Abstract
BACKGROUND:
To ascertain the effectiveness of a collaborative model between the Department of Community Medicine and state health department to improve MCH outcomes among the urban poor in Chandigarh.
MATERIALS AND METHODS:
A quasi-experimental study was conducted from 2011–12 to 2015–16 in the intervention and control areas. A collaboration was established between the state health department and the Department of Community Medicine of an autonomous institute. The intervention and control areas were mainly inhabited by the poor migrant population. Critical elements of an efficient collaboration such as the early engagement of partners, clearly stated purpose with common goals, effective communication, and no financial conflict were implemented in the intervention area. MCH program's implementation was strengthened through supportive supervision, enhanced community engagement, male partner involvement, tracking of high-risk pregnant women, and identification of problem families. Trend analysis of MCH indicators was done. The difference-in-difference (DID) analysis was done to measure the net effect of the intervention.
RESULTS:
All the MCH indicators improved significantly in the intervention area compared to the control area (P < 0.05). DID analysis depicted a net increase in the early registration of pregnancies by 18%, tetanus toxoid immunization by 9.2%, and fully immunized children by 8.6%. There was also an improvement in the maternal mortality ratio by 121.1 points, infant mortality rate by 2.2 points, and neonatal mortality rate by 2.6 points in the intervention area.
CONCLUSION:
An innovative, collaborative model between the state health department and the Department of Community Medicine effectively improved the MCH outcomes in Chandigarh.
Keywords: Community medicine, health planning, health policy, inter-sectoral collaboration, maternal-child health services, poverty
Introduction
Ensuring the well-being of all is difficult for the health sector; it needs to collaborate with other sectors of government and society to address various determinants of health and well-being. The role of collaboration in improving primary health care was first acknowledged in the Alma Ata declaration (1978) and then by WHO in 1986.[1] Collaborations can be explained as a relationship between parts of different sectors formed to take action on an issue and achieve health outcomes in a way that is more effective, efficient, and sustainable than can be achieved by the health sector acting alone.[2,3] Collaborations might be beneficial to reduce inequalities arising due to inadequate access and availability of health services, especially for the urban poor (slum population), or due to socio-cultural and geographical barriers like in rural or hard-to-reach areas. National health programs, such as the national rural health mission focusing on health system strengthening, have addressed these disparities to a certain extent in India.[4] However, inequalities persist within the urban areas.
Health inequalities within urban areas can be ascribed to rapid population growth and an unproportioned expansion of sanitation, health services, and livelihood opportunities.[5,6] Approximately 26.4% of the urban Indian population (102.5 million individuals) was below the poverty line in 2011–12.[7] Recent literature has documented substantial differences in maternal and child indicators between the urban and urban-poor of developing countries.[8,9,10,11,12] The differences are often linked to disparities in income, employment, educational level, living and working conditions, lifestyle, and accessibility to care services and lead to a range of health and well-being concerns of the deprived urban poor.[13,14]
To cater to these disparities, medical colleges can be potential stakeholders, especially the Department of Community Medicine (CM), whose origin can be traced back in India to a 1946 recommendation by the Bhore Committee report.[15] The primary aim of the CM specialist is to organize health and allied services in the community, set priorities in communities by using epidemiology and biostatistics, and address social determinants of the diseases prevalent in the community. CM in India has been pertinent in reaching out to the community through their urban and rural health and training centers (UHTCs/RHTCs).[16,17,18] In addition, CM experts use their expertise in the management of healthcare facilities, health-program implementation, monitoring and evaluation, health promotion, and surveillance of health information systems. Therefore, active collaboration of medical colleges with the public health system of the state government can be instrumental in improving health access for vulnerable populations, thus actualizing the concept of universal health coverage.[19] However, the effectiveness of such collaboration in improving health indicators needs to be assessed. Therefore, the objective of this study was to document the process of establishing a collaborative model between the public health system and the Department of CM of a medical college and to assess the effectiveness of this collaboration in improving the MCH indicators in North India.
Materials and Methods
Study design
Operational research with a quasi-experimental study design was conducted from April 2011–12 to March 2015–16.
Study settings
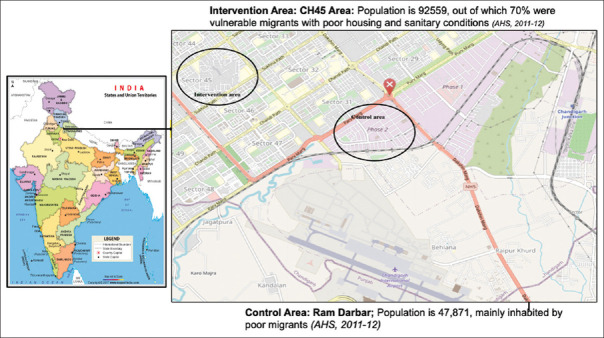
Intervention and control areas were selected purposively. The intervention area was the catchment area of a polyclinic in Sector 45, Chandigarh, with a population of 92,559 (as per the annual health survey data of the health center for the year 2011–12), and the control area was the catchment area of the civil dispensary (CD), Ram Darbar, which had a population of 47,871 [Figure 1].[20] Both the health facilities had one medical officer from 2011–12. The polyclinic was upgraded to a community health center in 2014–15 and a civil hospital (CH-45) in 2015–16, increasing human resources and providing indoor facilities. These two areas are located at different geographical locations in zone III (one of the administrative divisions of Chandigarh Union Territory health administration). They are naturally matched concerning the socioeconomic condition of the population and MCH indicators at the baseline. The majority of the population in both areas comprises poor migrants having low MCH indicators. The control area served as the control for 4 years (2011–12 to 2014–15). After that period, this area was also included in the intervention (during 2015–16).
Figure 1.
Geographical location of the intervention and the control area in Chandigarh, India
Study population
The study population included children aged less than 5 years and women in the reproductive age groups, including pregnant, postnatal, and lactating women in the catchment area.
Setting up the Collaborative model (The intervention)
The convergence mechanism was framed a priori, followed by a baseline assessment of the study areas. Nodal persons from each health sector, that is, Chandigarh Administration and the Department of Community Medicine, Postgraduate Institute of Medical Education and Research, were identified, and key roles and responsibilities of both the sectors were formulated. Administrative actions included signing a memorandum of understanding (MoU) between the two sectors by the respective heads of the organizations (directors). The roles and responsibilities for collaborators were clearly described and agreed upon as listed in Box 1. There was no financial liability on either organization. After finalizing the collaboration, specific facility-based and community-based activities were implemented that focused on improving MCH indicators in the intervention (CH-45) area. Details of the monthly activities performed are given in S1 File.
Box 1.
Responsibilities of the collaborative organizations
| Responsibilities of Department of Community Medicine, PGIMER, Chandigarh. |
| Provide technical assistance in strengthening the functioning of Civil Hospital, Sector 45, Chandigarh (CH-45) in conformity with guidelines by the Ministry of Health and Family Welfare, Government of India. |
| Provide overall supervision of the health services in the service area. |
| Post a Community Medicine faculty, resident doctor, and a paramedical staff in the service area. |
| Provide technical assistance for implementation, monitoring, and evaluation of National Health Programs of Government of India and Chandigarh Health Administration in the service area. |
| Carry out research and teaching/training of health care personnel of all categories in CH-45 and its service area. Primarily to conduct training of the staff nurses and the other staff in inter-personal communication/any other knowledge-based training. However, the skill-based training shall be imparted as per Government of India norms at various institutions. |
| Conduct monitoring and evaluation of health services within the service area. |
| Provide information of its staff and students posted in CH-45 and its service area, and submit a monthly report of their activities. Prepare an annual work plan to improve the health indicators of the service area in consultation with Director Health and Family Welfare, Chandigarh. |
| Responsibilities of the Chandigarh Administration |
| To provide sufficient office space clinic space to the staff and students of the collaborating Education and Research institution (PGIMER) at CH-45. |
| Allow the service area for teaching/training of its doctors and other staff and research. |
| Provide access to all health facilities, their records, monthly reports, and other health information to the staff and students designated by the director of PGIMER. |
| The ownership of the CH-45 building will be that of the Chandigarh Administration, and PGIMER shall be entitled only to use the same for the agreed period. |
| Chandigarh Administration will provide staff, equipment, and supplies as per requirement for a community health center in the service area, and PGIMER will not have financial liabilities of any kind. |
Baseline assessment phase: The data collected by auxiliary nurse midwives (ANMs) during annual health surveys were used to assess the baseline status of MCH indicators in the intervention and control area during 2011–12. An ANM is a ground-level worker usually posted at the health center and provides services related to maternal and child health, family planning, nutrition, universal immunization program, and communicable disease.
Intervention phase (Collaborative phase): Facility-based and community-based activities that focused on improving MCH indicators in the CH-45 area were implemented in the intervention area. In the control area (CD Ramdarbar), routine activities were carried out under the public health system. The duration of this phase was for three financial years, that is, from 2012–13 to 2014–15 in the intervention area.
Post-intervention phase: In this phase, that is, the year 2015–16, the intervention was extended to the control area. Weekly supportive supervision of the ANMs’ activities was done, along with weekly meetings with the control area's medical officer.
Data collection, validation, and quality assurance
The ANMs collected data in the routine health systems, and no separate staff was recruited to collect it in both areas. In the intervention area (CH 45), the annual health surveys were preceded by a refresher training of the ANMs. Resident doctors from the Department of CM, PGIMER, ensured that health workers had an in-depth understanding of the survey registers. Reference manuals provided explanatory text to accompany questionnaire sections and information about the coding and skip patterns. During survey implementation, a team of senior and junior residents and a medical social worker from PGIMER audited at least 10% of the households that ANMs had surveyed for any discrepancies in their records. This was followed by formal report writing and dissemination activities. In the control area (CD Ramdarbar), ANMs collected the survey data routinely without refresher training or monitoring and supervision by the PGIMER team. The survey reports of CD-Ram Darbar have been collected from the District Family Welfare (DFW) Bureau of Chandigarh Administration.
Data analysis and dissemination
The effectiveness of the collaboration was explained using a logic model approach [Table 1]. As per this model, it is assumed that there are inputs that lead to specific outputs through the set processes. These outputs further lead to specific outcomes related to a program (such as maternal and child health-related improvements) and ultimately the desired impacts. We have listed the inputs and processes of the collaborative model and related indicators in Table 1. Input, process, outputs, outcome, and impact indicators related to RCH (including maternal health, neonatal health, child health, and family planning) were defined as per the standard definitions and obtained from the review of the literature, including the National Family Health Survey reports, district-level household survey reports, and individual studies, and are mentioned in the footnotes of Table 2.[21,22] These indicators were compared in the study and control areas during the intervention period. Annual health survey reports were used to assess the impact on maternal and child health at the end of each financial year. Trend analysis of MCH indicators was done using the Chi-square test.
Table 1.
Logic model showing the inputs, processes, outputs, outcomes, and impact of a collaborative model to improve reproductive maternal and child health services
| Inputs | Processes | Outputs | Outcomes | Impact |
|---|---|---|---|---|
| Increased human resources: A Community Medicine Faculty, Resident Doctor, and a Para Medical Staff posted in the Civil Hospital CH 45 [3–4 additional technical staff provided] | Conducting joint weekly meetings with MCH staff by the faculty of medical colleges and SMO in charge, civil hospital [4 meetings per month] | Increased early registration of antenatal cases | Increased institutional delivery | Reduced maternal mortality ratio |
| Quarterly meetings with the program officer RCH [4 meetings per year] | The health care staff follows up an increasing number of pregnant women and children to receive the MCH services. | Increased full immunization coverage | Reduced neonatal mortality, infant mortality, and under-five mortality [Table 2] | |
| Training the health personnel in Civil Hospital, Sector 45, Chandigarh (CH-45) in conformity with the Ministry of Health and Family Welfare guidelines, Government of India. [3-4 training per month] | Annual review meetings between Head of the department and Director Health services to monitor the progress and to lay down the plans for the next year | Increased four antenatal checkup | ||
| Assistance in daily indoor, outdoor, and emergency services [20% services delivered] | Increased immunization uptake by pregnant women and children | Increased contraception usage. [Table 2] | ||
| Increased postnatal checkups | ||||
| Identification of the high-risk pregnancies (HRP) and following till the time of safe delivery outcomes. Birth preparedness of the pregnant women in the antenatal period and tracking of high-risk pregnant women [90%–100% HRP followed up] | Increased contraception use rate | |||
| Early identification of danger signs in sick children and pregnant women and appropriate, timely referral to higher centers. [Table 2] | ||||
| Identification of problem families, problem-solving with cascade model (first level counseling with auxiliary nurse midwives (ANMs), social worker, and then with resident doctors in the field), and efficient referral system. [90%–100% problem houses identified and action taken] | ||||
| Data analysis and interpretation included using a mother-child tracking system and a health management information system. | ||||
| Health education through enhanced community engagement via interpersonal communication by the medical social worker | ||||
| Assisting in outbreak identification and investigations of all infectious diseases. [All outbreaks assisted] | ||||
| Providing work outputs to the MCH staff. | ||||
| Overall monitoring and supportive supervision of the health services in the service area by the PGI staff. Research activities included improving the skills of para-medical staff by innovative teaching methods such as microteaching. | ||||
| Liaison with the non-governmental organization to address different issues related to MCH |
Table 2.
The trend of demographic indicators in the areas under CH-45 (intervention area) and CD-Ram Darbar (control area)
| Indicators | CH-45 (Intervention area) | CD-Ram Darbar (Control area) | DID | P* | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||||
| 2011-12 (Baseline) | 2012-13 | 2013-14 | 2014-15 (End line) | 2015-16 | Diff | 2011-12 (Baseline) | 2012-13 | 2013-14 | 2014-15 (End line) | 2015-16 | Diff | |||
| Demographic Indicators | ||||||||||||||
| Population | 92,559 | 97,054 | 71,106 | 77,150 | 81,332 | - | 38,453 | 43,212 | 44,012 | 44,894 | 47,582 | - | - | 0.001 |
| Eligible couples1 | 13,826 | 15,430 | 11,724 | 11,710 | 11,276 | - | 6754 | 6801 | 6895 | 6987 | 7068 | - | - | 0.000 |
| Infant mortality rate2 | 25.6 | 15 | 13 | 7.1 | 5 | −18.5 | 18.4 | 17.9 | 15.4 | 12.2 | 8.6 | −6.2 | −2.2 | <0.001 |
| Neonatal mortality rate3 | 10.2 | 8.3 | 6.8 | 2.7 | 2.8 | −7.5 | 10.6 | 9.8 | 7.1 | 6.8 | 4.6 | −3.8 | −2.6 | <0.001 |
| Maternal mortality ratio4 | 192 | 294 | 0 | 89.7 | 0 | −102.3 | 591 | 468.4 | 485.4 | 367.6 | 221.1 | −223.4 | 121.1 | 0.000 |
| Maternal health indicators (%) | ||||||||||||||
| Early registration of pregnancy5 | 39.0 | 54.4 | 81.0 | 92.8 | 95.7 | 53.8 | 38.6 | 49.4 | 54.6 | 74.4 | 86.6 | 35.8 | 18 | 0.000 |
| Two doses of tetanus toxoid/Booster | 70.8 | 61.6 | 72.0 | 93.3 | 99.9 | 22.5 | 68.8 | 72.2 | 76.2 | 82.1 | 96.6 | 13.3 | 9.2 | 0.002 |
| Four antenatal visits | 82.7 | 78.3 | 94.0 | 96.9 | 99.7 | 14.2 | 64.6 | 71.2 | 74.3 | 90.6 | 96.4 | 26 | −11.8 | 0.000 |
| Iron folic acid provision to Antenatal mothers | 38.8 | 12.8 | 82.0 | 88.3 | 99.9 | 49.5 | 34.2 | 18.4 | 66.4 | 76.4 | 96.2 | 42.2 | 7.3 | 0.000 |
| Institutional delivery | 78.7 | 87.9 | 96.0 | 97.3 | 99.4 | 18.6 | 61.2 | 66.4 | 78.6 | 86.2 | 94.6 | 25 | -6.4 | 0.004 |
| Three postnatal visits | 47.5 | 80.2 | 65.0 | 87.5 | 95.5 | 40 | NA | NA | 76.4 | 78.1 | 84.2 | - | - | 0.000 |
| Child health indicators (%) | ||||||||||||||
| BCG coverage | 92 | 93 | 94 | 99.6 | 99.9 | 7.6 | 82 | 82.4 | 85.8 | 88.6 | 94.2 | 6.2 | 0.4 | 0.7 |
| Measles coverage | 79 | 80 | 82 | 94 | 97.5 | 15 | 80 | 81.4 | 82.4 | 86.2 | 93.2 | 6.2 | 9.2 | 0.4 |
| Fully immunized children 12-23 months6 | 83.0 | 80.2 | 82.2 | 93.6 | 97.5 | 10.6 | 80.1 | 81.4 | 82.4 | 86.2 | 93.2 | 6.1 | 8.6 | 0.6 |
| Family planning indicators (%) | ||||||||||||||
| Contraceptive prevalence Rate7 | 69.4 | 71.6 | 72 | 76.9 | 76.9 | 7.5 | 64.6 | 65.4 | 67.4 | 69.6 | 72.6 | 5 | 2.5 | 0.000 |
| Condom | 18.3 | 38.5 | 43.0 | 57.7 | 52 | 39.4 | 39.9 | 40.1 | 41.4 | 41.6 | 42.1 | 1.7 | 37.7 | 0.000 |
| Oral contraceptive pills | 18.6 | 3.9 | 6.8 | 3.6 | 4.1 | -15 | 2.1 | 2.3 | 2.2 | 2.4 | 2.5 | 0.3 | -15.3 | 0.000 |
| Copper-T | 4.7 | 5.3 | 1.6 | 4.6 | 7.2 | -0.1 | 6.7 | 7.1 | 6.8 | 7.2 | 8.3 | 0.5 | -0.6 | 0.002 |
*Chi-square for trends of indicators between study and control area; Diff: Difference of indicators between endline and baseline in the intervention and control areas; DID: Difference in difference analysis. Operational definitions: 1Eligible couples: It refers to a currently married couple wherein the age of the wife is in the age group of 15-44 years (child-bearing age); 2Infant mortality rate: The ratio of infant deaths registered in a given year to the total number of live births registered in the same year, usually expressed as a rate per 1000 live births; 3Neonatal mortality rate: Neonatal mortality rate is the number of neonatal deaths in a given year per 1000 live births in that year; 4Maternal mortality ratio: Number of maternal deaths during a given time period per 100,000 live births during the same time-period; 5Early registration of pregnancy (%): Percentage of total pregnant women who got themselves registered during the 1st trimester of pregnancy; 6Fully immunized children 12-23 months (%): Children aged 12-23 months who received at least one dose of BCG vaccine, three doses of DPT vaccine, three doses of polio vaccine, and one dose of measles vaccine; 7Contraceptive prevalence rate (%): Percentage of married women aged 15-49, who are currently using, or whose sexual partner is currently using at least one method of contraception, regardless of the method used
The difference-in-difference (DID) analysis was done to measure the effectiveness of the collaborative model intervention in improving the MCH indicators in the study area. DID includes first estimating the difference in a particular indicator before and after the intervention period in the intervention and control group, respectively, and then estimating the DID between these two differences for a particular indicator. DID analysis was done to estimate the net effect of interventions from 2011–12 to 2014–15. We could not estimate the significance of the DID values because of the unavailability of individual-level data for the control area. A joint review meeting was held every year to share the findings of the annual health surveys with the officials from both the sectors under the chairmanship of Director Health Services, Chandigarh Administration. A joint annual health action plan was developed for the next financial year based on the results.
Ethics statement
No individual patient-level data were utilized for this study, and the data were fully anonymized before final analysis. The intervention was implemented at the population level through the existing public health care delivery system to improve maternal and child health outcomes by establishing a formal collaboration between the public health system and the Department of Community Medicine and School of Public Health of a tertiary care teaching hospital. Thus, the ethical approval was exempted.
Results
Benefits of collaboration to the community
The trend of demographic indicators: The baseline maternal and child health indicators were comparable in both the areas during 2011–12 except for institutional delivery rate, as shown in Table 2. The trend of demographic indicators depicts that the population in the two areas had never been stable owing to a large number of the migrant population residing in these areas. In the CH-45 catchment area, there was a large slum (colony number 5) with a population of approximately 25,000 during 2011–13. This population was later rehabilitated and shifted to another area in Chandigarh. Thus, there was a decline in the total population. The infant mortality, neonatal mortality, and maternal mortality ratio exhibited significant improvements in the study area (P < 0.001).
The trend of maternal health indicators: Maternal health indicators improved significantly in the study area compared to the control area [Table 2]. Early registration of pregnant women (registration within 12 weeks of pregnancy) significantly increased more in the intervention area compared to the control area (P < 0.001). Similar significant trends were observed for coverage of tetanus toxoid immunization during pregnancy, at least four antenatal checkups during the antenatal period, iron-folic acid supplementation coverage to the antenatal mothers, institutional deliveries, and at least three postnatal checkups in the intervention and control area. DID analysis depicted a net increase in the early registration of pregnancies by 18%, tetanus toxoid immunization by 9.2%, provision of iron-folic acid supplementation by 7.3%, and improvement in the maternal mortality ratio by 121.1 points. In comparison, the net effect declined by 11.8% regarding four antenatal visits and 6.4% in the institutional delivery.
The trend of child health indicators: Child health indicators also exhibited specific improvements [Table 2]. The changes in the proportion of babies born with low birth weight in the two areas were non-significant (P = 0.2). Similar trends were observed in the proportion of children with full immunization individual vaccine coverage. DID analysis revealed a net increase in children who were fully immunized by 8.6%, and an increase in coverage of all the vaccines available under the universal immunization program (BCG by 0.4%, DPT 1st dose + Pentavalent vaccine first dose by 0.6%, DPT 3rd dose + Pentavalent vaccine third dose by 3.5%, and measles by 9.2%). As per-DID analysis, there was also an improvement in the infant mortality rate by 2.2 points and in the neonatal mortality rate by 2.6 points.
The trend of family planning indicators: There was a decline in the total number of eligible couples residing in the study area, while an increase was observed in the control area [Table 2]. The contraceptive use rate increased more in the intervention area compared to the control area. Different family planning methods exhibited no specific trends during five years, but the differences were statistically significant (P < 0.001). DID analysis revealed a 2.5% improvement in contraceptive usage. There was a 37.7% improvement in condom usage and 0.46% improvement in vasectomy rates. In comparison, a 15.3% decrease was observed in oral contraceptive usage, a 2.3% decrease in tubectomy rates, and a 0.6% decrease in Cu-T (an intrauterine contraceptive device) insertions in the intervention area compared to the control area.
Problems identification and problem-solving
Problems identified in delivering adequate services included the availability of the drugs and logistics, inability to do ultrasonography of the migrant pregnant women who did not have residence proof such as Aadhar card (an identification document), and recruitment of Accredited Social Health Activist (ASHA) workers in vulnerable areas to work with the migrant population. These issues were presented to the Director of Health Services in the review meetings so that necessary actions could be taken at the earliest, and a regular supply of drugs and logistics was assured immediately. For availing of the ultrasonography services, an alternative option was tried that required minimum paperwork. However, ensuring the availability of ASHA workers was still a challenge. The strengths and limitations of the MCH program implemented in CH 45 were examined through SWOT analysis at the end of each year so that appropriate actions could be taken to strengthen the program further.
Benefits of collaboration to the medical college
Residents posted in the community benefitted from the community-based teaching and learning and first-hand exposure to the public health care delivery system in urban settings. More emphasis was given on understanding the implementation process of national health programs at a secondary care hospital and community. As CM postgraduates, they remained updated regarding recent changes in the program implementation and were aware of various challenges in implementing the programs. Concurrent evaluation, monitoring, and supervision of the RCH program trained the residents in core principles of health management, and community level research activities related to program implementation trained them in the operational research. Visiting the problem families acquainted the students to develop a problem-solving approach through a broad perspective. Contributions of and benefits to each organization, key challenges, and lessons learned are summarized in Figure 2.
Figure 2.
Diagram showing the contribution, benefits, challenges, and lessons learned using a collaborative model to improve MCH services
Discussion
The present study highlighted that collaboration between different organizations (Chandigarh Health Administration and Department of CM of a medical college) can significantly improve the health indicators and offer pertinent help in realizing the sustainable development goals related to MCH, especially among the urban poor. This study also provided evidence that CM can play an apposite role in strengthening the routine healthcare delivery system apart from teaching undergraduate and postgraduate medical students.[17,23,24]
Currently, CM departments restrict their participation in strengthening the health care delivery system to their primary health centers in rural areas and urban health centers in most medical colleges.[24,25] However, the true potential of the department in strengthening health care delivery remains unutilized.[26] A large workforce (including professors, associates professors, assistant professors, residents, medical officers, and other para-medical staff members) was recruited in CM departments of about 497 medical colleges of India.[27] The Government of India is promoting such associations by the department of CM, Pediatrics, and Gynecology/Obstetrics in medical colleges and contributing to the effective implementation of the National Urban Health Mission in urban areas.[5] This study provides evidence that such a partnership can successfully achieve these goals. However, only limited empirical evidence exists on their effectiveness in improving community-level outcomes as studies similar to ours are limited and difficult to find, particularly from developing countries.
In our study, the logic model used for evaluating the effectiveness indicates that inputs in the health system can improve visible changes in the outcomes and impact the maternal and child health indicators, which can be generalized to other health indicators. This collaboration was successful, and it had almost all the vital elements of inter-sectoral collaboration.[28] It had the early engagement of potential partners (administrative hierarchy of both the organizations), and nodal officers to collaborate were identified. There was a clearly stated purpose with crucial roles and responsibilities laid out, and a formal mechanism (signing of a MoU between the parties) was established where everyone benefitted and was accountable. There was no financial conflict as health staff used finances available within the health system whereas Department of CM staff got the salary from their institute. They only used the existing staff and infrastructure to improve the performance of health staff. The Department of CM also trained their resident doctors in family medicine, health management, health promotion, and epidemiology and conducted community-based research in these study areas. There was a common goal of improving the health of the vulnerable population in the service area. Review meetings kept the communication channel open between the two organizations and built trust in the collaboration [Figure 3]. Such a win-win situation, created for everyone, resulted in effective collaboration.
Figure 3.
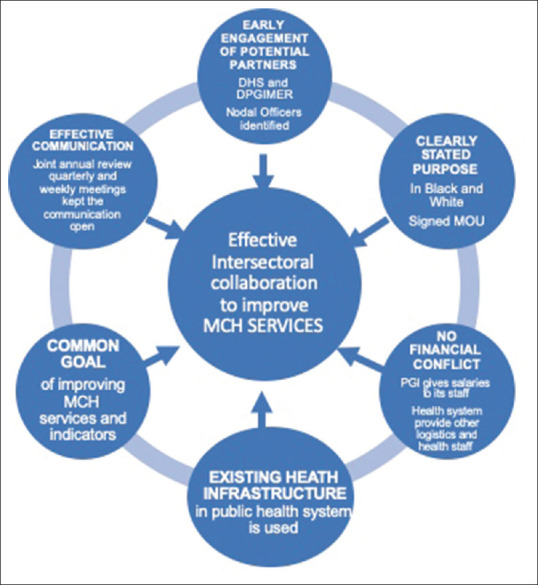
Model leading to effective collaboration to improve MCH services
Similar collaborations have been tried in specific fields in supportive supervision clinical audits, but none of the studies has tried it in such a comprehensive manner, with the whole community being a party to this activity.[29,30] Previous studies have presented population-level outcomes with some improvements that can be potentially attributed to activities of the collaborative partnership. A case study of an initiative to reduce infant mortality in Boston, which then had one of the highest rates in the nation, found a 50% reduction in Boston's infant mortality rate among African-Americans within 2 years after the start of the partnership.[31] In a systematic replication of the South Carolina program in three intervention communities, the School/Community Adolescent Pregnancy Prevention Partnerships in Kansas found a 9%–12% decrease in estimated pregnancy rates and a 13% decrease in birth rates in 14–17-year-olds within 2 years.[32] Prybil et al. (2014)[33] also demonstrated a successful collaboration between hospitals and the community with favorable outcomes. Gupta et al. (2017)[34] earlier reported improving the quality of home-based postnatal care by microteaching of multipurpose workers in Chandigarh's rural and urban slum areas through intersectoral collaboration.
In general, specific challenges were observed during the collaboration study. Most important was effective community engagement in implementing sustainable study components by the health facility even after the collaboration. Increased community participation is pertinent in the decision-making process through enhanced ownership and effective implementation of particular interventions. In the early period of collaboration, various challenges were faced, including non-cooperation of MCH staff, mainly with the PGI's team, which were later resolved after the facilitation of the Senior Medical Officer in charge of the health facility, and improved over time when they realized the benefits of support provided the collaborating institute. While analyzing this type of simple pre-and post-intervention comparisons, results may be affected by time or by other events that may have occurred between the two periods. Therefore, DID analysis was used to measure the effects of interventions related to improvement in MCH indicators of the intervention and the control areas. “Parallel trend” is a key assumption of DID that accounts for certain unobserved confounding variables that remain constant over time. It considers that without intervention, the end-line indicators of the intervention group and control group would follow parallel paths over the period.[35,36]
The major strength of this study was the implementation of the preexisting knowledge of collaboration while providing routine services to the community in a systematic and predefined manner. Identification of the need for outside help in the intervention area and support at every stage of the implementation by the health administration was another strength of the study. Further, we used the DID analysis in this study to measure the effectiveness of the collaborative model intervention in improving the MCH indicators in the study area. Effectiveness was measured by calculating the DID proportion change in MCH indicators between the intervention and control groups. Wing et al. mentioned that DID is often used to study the causal relationships in public health settings where randomized control trials may not be feasible or unethical. Although DID may not be the perfect substitute for randomized control trials, it is feasible for understanding causal relationships between the intervention and outcome, as stated by Wing et al.[37] This type of analysis was also considered in measuring the net effect of the nutrition-based intervention to estimate the change in dietary intake from baseline to end-line in the intervention and control arm in the study by Kaur et al.[38]
There are certain limitations to the study. The exact details regarding the social and economic factors were not obtained routinely in the annual health surveys by the ANMs. Thus, we could not match the intervention and control area on that basis that might influence the effectiveness of the intervention. The role of residual biases due to baseline differences cannot be ruled out. However, the fact that the control area was also inhabited by migrants who primarily worked as daily wagers/laborers was similar to the intervention area, and with our experience, we assumed that these would be similar. We could only depict the changes in the maternal and child health indicators as their improvement was the primary objective of the collaboration, and only these indicators could be religiously monitored with the available human resources. However, indicators from other pertinent national health programs could also have been monitored to make this a holistic, collaborative model. Being a quasi-experimental study, there are certain threats to internal validity which may limit generalizability.
Nevertheless, it was the most suitable research design that could have been implemented without disrupting the preexisting service delivery pathway. We also do not have data on pre-intervention periods. This could have been more useful in comparing the trends before and after the intervention done by the study. Secular trends driving the overall improvement in the social and economic standards of the community throughout the study that may have occurred were not addressed in the analysis.
The lessons learned through this study will help formulate the ways to enhance collaborations that may help improve the health indicators at the community level. This paper provides a replicable collaboration model for medical colleges and stresses the need for active role-play by the Department of CM to strengthen the existing health care systems under their jurisdiction. In our case, collaboration was between an autonomous institute and the union-territory administration. However, such collaborations can be even more smooth between state-run medical colleges and health departments. Future research should focus on the impact of such collaborations in improving health outcomes at the community level.
Conclusions
To conclude, the current collaborative model between the department of CM of an autonomous medical and research institute and state health department demonstrated a win-win situation for both the parties as evidenced through the improvement in the MCH indicators in the intervention area with simultaneous training of residents doctors of the medical institute. The health sector needs to be prepared to take the lead in such inter-sectoral collaborations to boost their performance further and improve the health indicators.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We are thankful to Dr. G Dewan, Director of Health Services, Chandigarh Administration, for providing the opportunity to carry out the collaborative work in their health facilities.
References
- 1.World Health Organization. The vital role of law Advancing the Right to health : International Development Law Organization. Geneva, Switzerland: 2017. [Google Scholar]
- 2.Kriesel W. Intersectorial action for health. A cornerstone for health-for-all in the twenty-first century. Report of the International Conference. Vol 51, World Health Statistics Quarterly. Halifax, Nova Scotia, Canada. 1997 [Google Scholar]
- 3.Adeleye OA, Ofili AN. Strengthening intersectoral collaboration for primary health care in developing countries: Can the health sector play broader roles? J Environ Public Health 2010. 2010 doi: 10.1155/2010/272896. 272896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta M, Bosma H, Angeli F, Kaur M, Chakrapani V, Rana M, et al. A mixed methods study on evaluating the performance of a multi-strategy national health program to reduce maternal and child health disparities in Haryana, India. BMC Public Health. 2017;17:698. doi: 10.1186/s12889-017-4706-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Government of India. National Urban Health Mission. : Framework For Implementation. New Delhi. 2013 [Google Scholar]
- 6.United Nations Human Settlements Programme. The Challenge of Slums; Global Report on Human Settlements 2003. London and Sterling, VA: 2003. [Google Scholar]
- 7.Rangarajan C. Rangarajan Report on Poverty. Press Information Bureau. 2014. [Last accessed on 2019 Jul 03]. Available from: http://pib.nic.in/newsite/PrintRelease.aspx?relid=108291 .
- 8.Arokiasamy P, Jain K, Goli S, Pradhan J. Health inequalities among urban children in India: A comparative assessment of Empowered Action Group (EAG) and South Indian states Environmental medicine: Social and medical aspects View project Assessing Inequity, and Impoverishment in Healthcare Expenditure in India View project. Artic J Biosoc Sci. 2013;45:167–85. doi: 10.1017/S0021932012000211. [DOI] [PubMed] [Google Scholar]
- 9.Fotso JC, Ezeh AC, Madise NJ, Ciera J. Progress towards the child mortality millennium development goal in urban sub-Saharan Africa: The dynamics of population growth, immunization, and access to clean water. BMC Public Health. 2007;7:218. doi: 10.1186/1471-2458-7-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu X, Cook S, Salazar MA. Internal migration and health in China. Lancet. 2008;372:1717–9. doi: 10.1016/S0140-6736(08)61360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Urban health Division. Meeting the health challenges of Urban Population especially the urban poor. New Delhi. 2008. [Last accessed on 2022 Apr 30]. p. 159. Available from: http://www.uhrc.in/downloads/Reports/NUHM-Draft.pdf .
- 12.Ministry of Health and Family Welfare (Government of India). National Urban Health Mission: Orientation Module for Planners, Implementers and Partners. 2013. [Last accessed on 2019 Apr 15]. Available from: https://nhm.gov.in/images/pdf/NUHM/Orientation_module_for_planners_implementers_and_partners.pdf .
- 13.Storm I, den Hertog F, van Oers H, Schuit AJ. How to improve collaboration between the public health sector and other policy sectors to reduce health inequalities?-A study in sixteen municipalities in the Netherlands. Int J Equity Health. 2016;15:97. doi: 10.1186/s12939-016-0384-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. The urban Health Crisis; Strategies for health for all in the face of rapid urbanization. Report of the Technical Discussions at the Forty-fourth World Health Assembly. Geneva, Switzerland: 1993. [Last accessed on 2022 Apr 30]. Available from: https://apps.who.int/iris/handle/10665/37434 . [Google Scholar]
- 15.Bhore committee, 1946 | National Health Portal Of India. [Last accessed on 2019 Apr 15]. Available from: https://www.nhp.gov.in/bhore-committee-1946_pg .
- 16.Nongkynrih B, Anand K, Kusuma YS, Rai SK, Misra P, Goswami K. Linking undergraduate medical education to primary health care. Indian J Public Heal. 2008;52:28–32. [PubMed] [Google Scholar]
- 17.Zodpey S, Negandhi H, Sharma K. How can departments of community medicine shape the future of Public Health Education in India? Indian J Public Health. 2010;54:184. doi: 10.4103/0019-557X.77257. [DOI] [PubMed] [Google Scholar]
- 18.Kumar R. Clinical practice in community medicine: Challenges and opportunities. Indian J Community Med. 2017;42:131. doi: 10.4103/ijcm.IJCM_18_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Devadasan N, Ghosh S, Nandraj S, Sundararaman T. Monitoring and Evaluating Progress towards Universal Health Coverage in India. PLoS Med. 2014;11:e1001697. doi: 10.1371/journal.pmed.1001697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.OpenStreetMap. [Last accessed on 2019 Aug 01]. Available from: https://www.openstreetmap.org/#map=14/30.6980/76.7788&layers=N .
- 21.International Institute of Population Sciences (IIPS). District Level Household & Facility Survey (2012-13) [Last accessed on 2021 Jan 11]. Available from: http://rchiips.org/
- 22.International Institute of Population Sciences (IIPS). National Family Health Survey-IV (2015-16) [Last accessed on 2021 Jan 11]. Available from: http://rchiips.org/nfhs/
- 23.Lal S. Scenario of post graduate medical education in community medicine in India. Indian J Community Med. 2005;25:56–61. [Google Scholar]
- 24.Garg R, Gupta S. Are we really producing public health experts in India? Need for a paradigm shift in postgraduate teaching in community medicine. Indian J Community Med. 2011;36:93. doi: 10.4103/0970-0218.84124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shewade H, Jeyashree K, Chinnakali P. Reviving community medicine in India: The need to perform our primary role. Int J Med Public Heal. 2014;4:29. [Google Scholar]
- 26.Pandav CS. Role of faculty of medical colleges in national health policy and program development. Indian J Community Med. 2010;35:3–6. doi: 10.4103/0970-0218.62544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Medical Council of India. List of College Teaching MBBS | MCI India. 2019. [Last accessed on 2019 Apr 15]. Available from: https://www.mciindia.org/CMS/information-desk/for-students-to-study-in-india/list-of-college-teaching-mbbs .
- 28.Key Element 6: Collaborate Across Sectors and Levels | Canadian Best Practices Portal-CBPP. [Last accessed on 2019 Apr 15]. Available from: http://cbpp-pcpe.phac-aspc.gc.ca/population-health-approach-organizing-framework/key-element-6-collaborate-sectors-levels/
- 29.Mittelmark MB, Hunt MK, Heath GW, Schmid TL. Realistic outcomes: Lessons from community-based research and demonstration programs for the prevention of cardiovascular diseases. J Public Health Policy. 1993;14:437–62. [PubMed] [Google Scholar]
- 30.Aggarwal A, Gupta R, Das D, Dhakar A, Sharma G, Anand H, et al. An alternative approach for supportive supervision and skill measurements of health workers for integrated management of neonatal and childhood illnesses program in 10 districts of Haryana. Indian J Community Med. 2018;43:40. doi: 10.4103/ijcm.IJCM_402_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Plough A, Olafson F. Implementing the Boston Healthy Start Initiative: A case study of community empowerment and public health. Health Educ Q. 1994;21:221–34. doi: 10.1177/109019819402100207. [DOI] [PubMed] [Google Scholar]
- 32.Paine-Andrews A, Harris KJ, Fisher JL, Lewis RK, Williams EL, Fawcett SB, et al. Effects of a replication of a multicomponent model for preventing adolescent pregnancy in three Kansas communities. Fam Plann Perspect. 1999;31:182–9. [PubMed] [Google Scholar]
- 33.Prybil L, Scutchfield FD, Mays GP. Improving Community Health through Hospital- Public Health Collaboration : Insights and Lessons learned from successful partnerships [Internet] Health management and Policy faculty book. 2014. [cited 2022 May 9]. pp. 1–110. Available from: https://uknowledge.uky.edu/hsm_book .
- 34.Gupta M, Tripathy JP, Jamir L, Sarwa A, Sinha S, Bhag C. Improving quality of home-based postnatal care by microteaching of multipurpose workers in rural and urban slum areas of Chandigarh, India: A pilot study. Adv Med Educ Pract. 2017;8:1–8. doi: 10.2147/AMEP.S111697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abadie A. Oxford University Press; 2005. Semiparametric Difference-in-Differences Estimators. Vol. 72, The Review of Economic Studies; pp. 1–19. [Google Scholar]
- 36.Crown WH. Propensity-score matching in economic analyses: Comparison with regression models, instrumental variables, residual inclusion, differences-in-differences, and decomposition methods. Appl Health Econ Health Policy. 2014;12:7–18. doi: 10.1007/s40258-013-0075-4. [DOI] [PubMed] [Google Scholar]
- 37.Wing C, Simon K, Bello-Gomez RA. Designing difference in difference studies: Best Practices for Public Health Policy Research. Vol. 39, Annual Review of Public Health. Annual Reviews Inc. 2018:453–69. doi: 10.1146/annurev-publhealth-040617-013507. [DOI] [PubMed] [Google Scholar]
- 38.Kaur J, Kaur M, Webster J, Kumar R. Protocol for a cluster randomised controlled trial on information technology-enabled nutrition intervention among urban adults in Chandigarh (India): SMART eating trial. Glob Health Action. 2018;11:1419738. doi: 10.1080/16549716.2017.1419738. [DOI] [PMC free article] [PubMed] [Google Scholar]