Abstract
Introduction
Patients with breast cancer with homologous recombination deficiency (HRD) such as germline BRCA1/2 mutations would respond to DNA-damaging drugs. Several clinical studies have revealed that HRD biomarkers were associated with the outcomes of patients with early breast cancer (EBC). However, no systematic review has determined the prognostic role of HRD biomarkers in patients with EBC. Therefore, this study will systematically combine and analyse the results of previous studies, to facilitate the clinical use of HRD detection in EBC.
Methods and analysis
We will search five databases including PubMed, Cochrane Library, EMBASE, OVID and Web of Science through December 2021, with no language restriction. Two reviewers will independently screen all records based on pre-established inclusion and exclusion criteria. The main outcomes include pathological complete response, disease-free survival and Ooerall survival. In addition, all studies included must contain the detection of HRD score, HRD status or HRD-related gene mutational status and protein expression. Data extraction will be carried out by two reviewers independently according to a self-designed template. The Newcastle-Ottawa Quality Assessment Scale and Jadad Scale will be used for quality assessment for cohort studies and randomised clinical trials, respectively. Review Manager V.5.3.5 will be used to perform meta-analysis. Both the Q test and I2 statistic will be used to assess heterogeneity. Subgroup and sensitivity analyses will be conducted if significant heterogeneity appears and cannot be reduced by using a random-effect model.
Ethics and dissemination
Ethical approval is not required for a systematic review. The results will be disseminated through international and national conferences or peer-reviewed publications.
PROSPERO registration number
CRD42021286522.
Keywords: breast tumours, adult oncology, cancer genetics
Strengths and limitations of this study.
This systematic review will follow the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Stringent inclusion and exclusion criteria will be used to select clinical studies assessing the impact of homologous recombination deficiency (HRD) biomarkers (HRD score, HRD status and HRD-related gene mutational status and protein expression) on outcomes of patients with early breast cancer.
Internationally recognised scales will be used for the quality assessment, to exclude low-quality studies and enhance the credibility of pooled results.
Differences in patient cohort, sample size, treatment regimen and measure of HRD biomarkers may yield significant heterogeneity.
Introduction
Cancer refers to a disease in which cells divide uncontrollably and invade normal tissues.1 In the pathogenesis of most cancers, normal cells need to undergo certain genetic changes to become cancerous such as activation of proto-oncogenes and inactivation of tumour suppressor genes.2 For example, the occurrence of retinoblastoma is often companied by the mutation of the tumour suppressor gene retinoblastoma gene (RB1).3 Endogenous (replication stress, oxygen radicals and cell metabolism) and exogenous (radiation, viral infection and chemotherapy) damaging factors continually act on the genome of cells and caused different degrees of DNA lesions,4 and what protects organisms from cancer is that cells have inherent repair mechanisms to eliminate these damaging events. DNA damages that occur on a single strand are to be dealt with by a number of simple repair pathways, including base-excision repair, nucleotide-excision repair, direct repair and mismatch repair. On the contrary, DNA double-strand break, which is the most severe DNA lesion and the main driver of cancer, requires sophisticated repair pathways such as non-homologous end joining (NHEJ) and homologous recombination (HR).5 The HR system uses a homologous sister chromatid (available in the S and G2 phases of cell cycle) as a template to copy and replace damaged DNA in a relatively error-free manner compared with NHEJ.6 A number of key genes including BRCA1/2, RAD51 and PALB2 will encode functional proteins and get involved in the process of repair.7 If these genes are mutated, the HR system will fail to perform the repair function, which is so-called HR deficiency (HRD), leading to the accumulation of somatic mutations, chromosomal aberrations and genomic scars (heritable genomic changes resulted from DNA repair defeat) as well as the development of cancer, especially breast cancer (BC).8 9
BC is a highly heterogeneous disease and treated mainly based on the receptor expression status. In recent years, with the development of sequencing technology and our further understanding of genetic variation of cancer, numerous genes are being used to screen for available therapeutic targets.10 For example, DNA-damaging drugs such as poly (ADP-ribose) polymerase inhibitors and platinums have been shown to significantly improve progression-free survival in patients with advanced triple-negative BC (TNBC) with germline BRCA1/2 mutations.11 12 Moreover, based on the latest data from phase III OlympliaA trial, adjuvant olaparib was shown to significantly improve the primary end point of invasive disease-free survival (DFS) versus placebo in patients with germline BRCA1/2-mutated high-risk early breast cancer (EBC) (3-year invasive DFS rate: 85.9% vs 77.1%; HR 0.58, 95% CI 0.41 to 0.82, p<0.001).13 Therefore, as key genes in the process of HR, BRCA1/2 are generally detected to determine the HRD status of patients with BC. However, only 4% and 22% HRD can be attributed to germline BRCA1/2 mutations in BC and TNBC, respectively.14–16 On this condition, biomarkers with wider coverage are needed to identify more patients with BC with HRD. The HRD score is an algorithmic assessment of three measures of loss of heterozygosity (LOH), large-scale transition (LST) and telomeric allelic imbalance (TAI).17 This kind of assessment along with BRCA mutation detection is now widely used to define the HRD status.
Several studies have investigated the prognostic role of HRD score in early BC (EBC).18–21 Telli et al18 assessed the HRD score in three neoadjuvant TNBC trials and found that a HRD score ≥42 or the presence of BRCA1/2 mutations were correlated with the objective response rate to platinum-based therapy. SWOG S9313 is a phase III randomised study, comparing the efficacy of simultaneous anthracycline (A) and cyclophosphamide (C) and sequential A→C in more than 3000 stage I/II patients with BC. Sharma et al19 investigated the prognostic role of HRD status in a subset of patients from SWOG S9313. The results indicated that HRD-positive status was associated with better DFS (HR 0.72, 95% CI 0.51 to 1.00, p=0.049). Significant associations between HRD-positive status and higher pathological complete response (pCR) rates of patients with EBC were also revealed in two studies by Loibl et al20 and Telli et al,21 respectively. Despite all the above efforts, the detection of HRD biomarkers has not been incorporated into the clinical practice of BC. In addition, no systematic review has explored the relationship between HRD biomarkers and the prognosis of patients with EBC. Therefore, we will first systematically combine and analyse the results of previous studies in this study, to facilitate the clinical use of HRD detection in EBC.
Methods and analysis
This systematic review is expected to begin on 1 December 2021 and end on 30 June 2022 and will be conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 statement.22 This review’s protocol has been registered in the International Prospective Register of Systematic Reviews.
Search strategy
Five databases including PubMed, Cochrane Library, EMBASE, OVID and Web of Science will be searched from 1 December 2021 to 31 March 2022, with no language restriction. Medical Subject Headings and free text will be combined to search for concepts such as ‘Breast Neoplasms’ and ‘Early’ and ‘Recombinational DNA Repair’ and ‘Biomarkers’. The detailed example of the search strategy applied in PubMed is available in online supplemental file 1. In addition, we will search the reference lists of recognised studies to identify additional papers.
bmjopen-2021-059538supp001.pdf (55.9KB, pdf)
Study selection
All records identified through database searching will be imported into EndNote V.9.1 software. First, duplicates will be removed using the built-in recognition function of the software by the lead author. Then, all records will be screened by two reviewers independently according to the title and abstracts. After that, the potentially relevant full-text articles will be reviewed by the same two reviewers independently based on pre-established inclusion and exclusion criteria. Finally, the remaining full-text articles will be assessed for eligibility by the team. Disagreements between the two reviewers will be settled by discussion. The particular reason for exclusion of each reviewed article will be recorded and presented in the final manuscript. In addition, the reference lists of recognised studies will be searched to make sure that no potentially eligible article is missed.
Inclusion criteria
Types of studies
Clinical studies investigating the impact of HRD biomarkers (HRD score, HRD status and HRD-related gene mutational status and protein expression) on outcomes in patients with EBC will be included. Concretely, the HRD-related genes/proteins mainly include ATM, ATR, BARD1, BLM, BRCA1, BRCA2, BRIP1, CHEK2, MRE11A, NBN, PALB2, RAD51C, RAD51D, RBBP8, SLX4 and XRCC2.23 This review will include articles published in any language, with no restriction of date. Non-English articles potentially eligible for inclusion will be translated to obtain enough data. The rationality of treatment regimens in all included studies will be confirmed by the lead author based on the recommendations of National comprehensive cancer network clinical practice guidelines.24 For studies involving grouping, the treatment regimen received by patients in each group should be comparable.
Types of participants
Patients with histologically confirmed EBC.
Interventions/exposures
High HRD score, positive HRD status, positive gene mutational status and positive protein expression. Specifically, the assessment of HRD score should include three measures of tumour genomic instability (LOH, LST and TAI), with a cut-off of 42.18
Comparators/control
Low HRD score, negative HRD status, negative gene mutational status and loss of protein expression.
Main outcomes
Each study should contain at least one of the following outcomes:
pCR: no invasive carcinoma in primary site and negative regional lymph node (ypT0/ypTis ypN0) after neoadjuvant therapy.25
DFS: the time from randomisation to disease recurrence or death due to disease progression.
Overall survival (OS): the time from randomisation to death from any cause.
Exclusion criteria
Articles that meet the following criteria will be excluded:
Non-clinical studies including reviews, conference abstracts, case reports and series and comments.
Patients with metastatic or advanced BC.
No detection of HRD, wrong evaluation methods of HRD score or other cut-off values.
Non-human experiments.
Data extraction
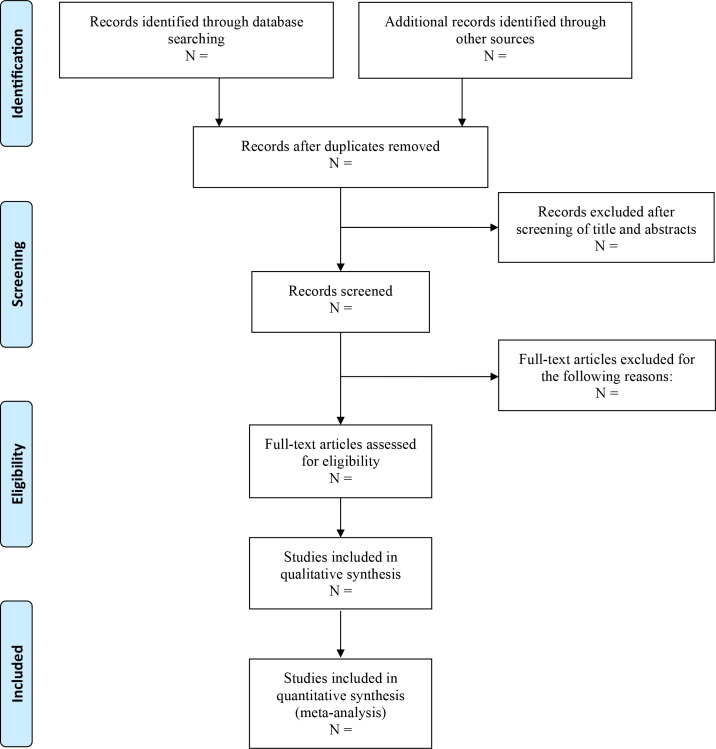
Two reviewers will independently extract data from the included studies into a self-designed data extraction template. If some important data are not available in the articles, we will make contact with the first or corresponding authors for potential support. Differences in opinion between the two reviewers will be settled by discussion. The study selection process is shown in figure 1. The following study characteristics will be collected:
Figure 1.
Flow diagram of study selection process.
Study details
First author, year of publication, country/region, study design and setting (neoadjuvant and adjuvant).
Patients characteristics
Patient subtype (hormone receptor-positive, human epidermal growth factor receptor 2-positive and TNBC), number of patients and treatment regimen.
Evaluation indicators
Main outcomes (pCR, DFS and OS), HRD biomarkers (HRD score, HRD status and HRD-related gene mutational status and protein expression) and score of quality assessment.
Quality assessment
Two reviewers will independently conduct quality assessment using the Newcastle-Ottawa Quality Assessment Scale (NOS) for cohort studies and Jadad scale for randomised clinical trials, respectively.26 27 The NOS consists of three key items: (1) selection, (2) comparability and (3) outcome. One point will be added when there is enough support information for an item. One study that obtains at least 6 points will be considered as high quality, with a full score of 9 points.26 The Jadad Scale includes four key items: (1) randomisation, (2) double blinding, (3) concealment of allocation and (4) withdrawals and dropouts. If the description of one item is described and appropriate, two points will be added to this item. On the contrary, if the description is not described or inappropriate, the score for this item will be 0. If the rating falls between the two situations, one point will be added. Specially, for the item of withdrawals and dropouts, only 1 and 0 point can be chosen. The full score of Jadad scale is 7 points, and a score of more than 3 points means high quality.27
Statistical analysis
Data synthesis
All data will be synthesised narratively and quantitatively. If there are more than two studies for one outcome, meta-analysis will be further conducted.28 Otherwise, we will only carry out systematic review with descriptive analysis. Review Manager V.5.3.5 (Cochrane Collaboration, Oxford, UK) will be used to pool the results. ORs and HRs along with 95% CIs will be calculated using the Mantel–Haenszel method and inverse variance method, respectively. Forest plots will be used to present the pooled results. For all statistical tests, a two-tailed p value of <0.05 will be considered statistically significant.
Heterogeneity assessment
Before pooling the results, both the Q test and I2 statistic will be used to assess heterogeneity. A p value of <0.1 and an I2 value of >50% indicate significant heterogeneity across studies. A fixed-effect model will be used unless considerable heterogeneity arises. Alternatively, a random-effect model will be used.
Subgroup and sensitivity analysis
If significant heterogeneity appears and cannot be reduced by using a random-effect model, subgroup analysis or sensitivity analysis will be conducted to find possible source of heterogeneity. The grouping methods of subgroup analysis will be based on the study characteristics, patient subtypes, chemotherapy regimens or HRD detection methods, while the sensitivity analysis will be conducted by omitting the data of individual studies. The potential source of heterogeneity can be identified if the heterogeneity decreases significantly when carrying out subgroup analysis based on one factor or discarding data from one study.
Publication bias
Stata V.12.0 (Stata Corporation, College Station, Texas) will be used to evaluate potential publication bias using Egger’s and Begg’s test. A p value of<0.05 will be considered a significant publication bias.
Supplementary Material
Footnotes
HL and WP contributed equally.
Contributors: HaL, WP and JZ were responsible for the conception of the study plan, and preparation of the manuscript. HuL reviewed the study plan and manuscript and offered comments and edits.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell 2011;144:646–74. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 2.Lee EYHP, Muller WJ. Oncogenes and tumor suppressor genes. Cold Spring Harb Perspect Biol 2010;2:a003236. 10.1101/cshperspect.a003236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamihara J, Bourdeaut F, Foulkes WD, et al. Retinoblastoma and neuroblastoma predisposition and surveillance. Clin Cancer Res 2017;23:e98–106. 10.1158/1078-0432.CCR-17-0652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Di Micco R, Krizhanovsky V, Baker D, et al. Cellular senescence in ageing: from mechanisms to therapeutic opportunities. Nat Rev Mol Cell Biol 2021;22:75–95. 10.1038/s41580-020-00314-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jackson SP, Bartek J. The DNA-damage response in human biology and disease. Nature 2009;461:1071–8. 10.1038/nature08467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ward JF. Radiation mutagenesis: the initial DNA lesions responsible. Radiat Res 1995;142:362–8. 10.2307/3579145 [DOI] [PubMed] [Google Scholar]
- 7.Easton DF, Pharoah PDP, Antoniou AC, et al. Gene-panel sequencing and the prediction of breast-cancer risk. N Engl J Med 2015;372:2243–57. 10.1056/NEJMsr1501341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawrence MS, Stojanov P, Mermel CH, et al. Discovery and saturation analysis of cancer genes across 21 tumour types. Nature 2014;505:495–501. 10.1038/nature12912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ali RMM, McIntosh SA, Savage KI. Homologous recombination deficiency in breast cancer: implications for risk, cancer development, and therapy. Genes Chromosomes Cancer 2021;60:358–72. 10.1002/gcc.22921 [DOI] [PubMed] [Google Scholar]
- 10.Liao H, Li H. Advances in the detection technologies and clinical applications of circulating tumor DNA in metastatic breast cancer. Cancer Manag Res 2020;12:3547–60. 10.2147/CMAR.S249041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robson ME, Tung N, Conte P, et al. OlympiAD final overall survival and tolerability results: olaparib versus chemotherapy treatment of physician's choice in patients with a germline BRCA mutation and HER2-negative metastatic breast cancer. Ann Oncol 2019;30:558–66. 10.1093/annonc/mdz012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tutt A, Tovey H, Cheang MCU, et al. Carboplatin in BRCA1/2-mutated and triple-negative breast cancer BRCAness subgroups: the TNT trial. Nat Med 2018;24:628–37. 10.1038/s41591-018-0009-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tutt ANJ, Garber JE, Kaufman B, et al. Adjuvant Olaparib for Patients with BRCA1- or BRCA2-Mutated Breast Cancer. N Engl J Med 2021;384:2394–405. 10.1056/NEJMoa2105215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pellegrino B, Cavanna L, Boggiani D, et al. Phase II study of eribulin in combination with gemcitabine for the treatment of patients with locally advanced or metastatic triple negative breast cancer (ERIGE trial). Clinical and pharmacogenetic results on behalf of the Gruppo Oncologico Italiano di Ricerca clinica (GOIRC). ESMO Open 2021;6:100019. 10.1016/j.esmoop.2020.100019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baretta Z, Mocellin S, Goldin E, et al. Effect of BRCA germline mutations on breast cancer prognosis: a systematic review and meta-analysis. Medicine 2016;95:e4975. 10.1097/MD.0000000000004975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akashi-Tanaka S, Watanabe C, Takamaru T, et al. Brcaness predicts resistance to taxane-containing regimens in triple negative breast cancer during neoadjuvant chemotherapy. Clin Breast Cancer 2015;15:80–5. 10.1016/j.clbc.2014.08.003 [DOI] [PubMed] [Google Scholar]
- 17.Marquard AM, Eklund AC, Joshi T, et al. Pan-Cancer analysis of genomic scar signatures associated with homologous recombination deficiency suggests novel indications for existing cancer drugs. Biomark Res 2015;3:9. 10.1186/s40364-015-0033-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Telli ML, Timms KM, Reid J, et al. Homologous recombination deficiency (HRD) score predicts response to Platinum-Containing neoadjuvant chemotherapy in patients with triple-negative breast cancer. Clin Cancer Res 2016;22:3764–73. 10.1158/1078-0432.CCR-15-2477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma P, Barlow WE, Godwin AK, et al. Impact of homologous recombination deficiency biomarkers on outcomes in patients with triple-negative breast cancer treated with adjuvant doxorubicin and cyclophosphamide (SWOG S9313). Ann Oncol 2018;29:654–60. 10.1093/annonc/mdx821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Loibl S, Weber KE, Timms KM, et al. Survival analysis of carboplatin added to an anthracycline/taxane-based neoadjuvant chemotherapy and HRD score as predictor of response-final results from GeparSixto. Ann Oncol 2018;29:2341–7. 10.1093/annonc/mdy460 [DOI] [PubMed] [Google Scholar]
- 21.Telli ML, Hellyer J, Audeh W, et al. Homologous recombination deficiency (HRD) status predicts response to standard neoadjuvant chemotherapy in patients with triple-negative or BRCA1/2 mutation-associated breast cancer. Breast Cancer Res Treat 2018;168:625–30. 10.1007/s10549-017-4624-7 [DOI] [PubMed] [Google Scholar]
- 22.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Norquist BM, Brady MF, Harrell MI, et al. Mutations in homologous recombination genes and outcomes in ovarian carcinoma patients in GOG 218: an NRG Oncology/Gynecologic Oncology Group study. Clin Cancer Res 2018;24:777–83. 10.1158/1078-0432.CCR-17-1327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gradishar WJ, Anderson BO, Abraham J, et al. Breast cancer, version 3.2020, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Ne 2020;18:452–78. 10.6004/jnccn.2020.0016 [DOI] [PubMed] [Google Scholar]
- 25.Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 2014;384:164–72. 10.1016/S0140-6736(13)62422-8 [DOI] [PubMed] [Google Scholar]
- 26.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 27.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–12. 10.1016/0197-2456(95)00134-4 [DOI] [PubMed] [Google Scholar]
- 28.Valentine JC, Pigott TD, Rothstein HR. How many studies do you need?: a primer on statistical power for meta-analysis. J Educ Behav Stat 2010;35:215–47. 10.3102/1076998609346961 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059538supp001.pdf (55.9KB, pdf)