Disruption of the outer segments of the photoreceptors on optical coherence tomography may be a pathognomonic sign of vitamin A deficiency. Early detection is especially important in patients with gastrointestinal disorders who may have other underlying deficiencies. Treatment leads to resolution of visual symptoms and improves the quality of life.
Key words: autofluorescence, gastrointestinal disorders, nyctalopia, OCT, vitamin A deficiency
Purpose:
To describe the optical coherence tomography features of vitamin A deficiency.
Methods:
Case series includes three male patients aged 50 to 66 years with vitamin A deficiency and visual symptoms ranging from 2 to 8 months. Examination included optical coherence tomography (OCT), fundus autofluorescence imaging, full-field electroretinography6 and laboratory work-up.
Results:
Patient 1 had inoperable pancreatic neuroendocrine tumor and presented with worsening nyctalopia. The electroretinography showed absent rod function 2 months after the onset of symptoms, followed by a decrease of the cone function eight months after the onset. Optical coherence tomography showed poorly distinguishable outer segments of the photoreceptors with the disappearance of the interdigitation zone. At that time, vitamin A deficiency along with several other deficiencies was confirmed. After the initiation of parenteral nutrition, a substantial improvement of the patient's overall well-being was noted and the OCT showed normalization of the retinal structure. Two other patients were diagnosed with vitamin A deficiency based on similar OCT features.
Conclusion:
Disruption of the outer segments of the photoreceptors and the disappearance of the interdigitation zone on OCT may be helpful in recognition of vitamin A deficiency. Early detection and malnutrition evaluation are especially important in patients with a history of gastrointestinal disorders who may have several other underlying deficiencies. Treatment with either enteral or parenteral nutrition not only leads to resolution of visual symptoms but vastly improves their general condition and quality of life.
Vitamin A is a fat-soluble vitamin involved in several physiological processes with its active compounds 11-cis-retinal and all-trans-retinoic acid.1 11-cis-retinal combines with opsins to form the visual pigments in photoreceptors and is important in phototransduction. All-trans-retinoic acid has a role in cell proliferation and differentiation, gene regulation, adaptive immunity, reproduction, embryonic growth, and normal brain function. It is also essential for epithelial cell RNA synthesis in the conjunctiva and cornea.1 Prolonged malnutrition, malabsorption, or abnormal metabolism can result in vitamin A deficiency. Functional deficiencies in the form of nyctalopia and rod or rod–cone dysfunction have been well recognized in association with vitamin A deficiency2–4; however, there are little data on the structural changes that occur in the retina. We describe optical coherence tomography (OCT) features of vitamin A deficiency observed in three patients.
Case Reports
The patients' characteristics and clinical details are shown in Table 1. Patient 1 was a 63-year-old man who presented to the Ljubljana University Eye Hospital with a 2-month history of worsening nyctalopia. The medical history included inoperable neuroendocrine pancreatic carcinoma treated with chemotherapy and radiotherapy 2 years before and a partial bowel resection with external biliary drainage because of small bowel obstruction two months before presentation. Prescribed medications included pancreatic digestive enzyme replacement (Creon) and insulin.
Table 1.
Patient Characteristics
| ID | Sex | Age | Systemic Diagnosis | Visual Symptoms | Duration of Symptoms | Examination Features | VA | OCT Features | FAF Features | Vit a Level (Normal 1.05-2.80 µmol/L) |
| 1 | M | 63 | Pancreatic adenocarcinoma | Nyctalopia | 8 months | Normal | RE 20/25; LE 20/200 (amblyopic) | poorly distinguishable OS | Normal | 0.15 |
| 2 | M | 66 | Liver transplantfailure | Nyctalopia;prolonged adaptation to dark;dry eye sensation | 3 months | Normal | RE 20/20; LE 20/20 | Poorlydistinguishable OS, drusen | Hypoautofluorescent dots | 0.20 |
| 3 | M | 50 | Chronic alcohol related pancreatitis | Decreased VA | 1 month | Dry eye; bilateral sterile corneal ulcer | RE CF; LE CF | Poorly distinguishable OS | N/A | 0.44 |
CF, counting fingers; LE, left eye; M, male; N/A, not available; RE, right eye; OS, photoreceptor outer segment layer.
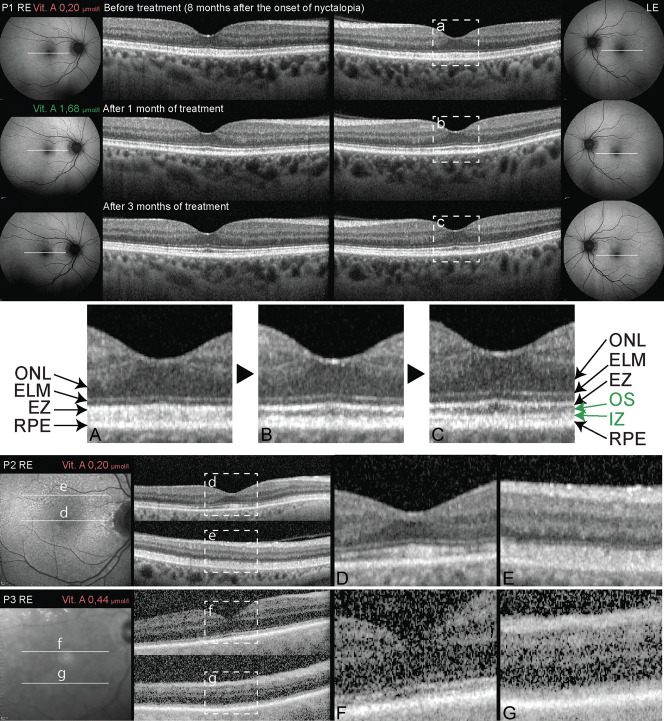
At presentation, the visual acuity was 20 of 25 on the right and 20 of 200 on the left, amblyopic eye. The anterior segment and fundoscopy were unremarkable. Full-field electroretinography (ERG) performed according to International Society for Clinical Electrophysiology of Vision (ISCEV) standards showed complete absence of the rod function confirming the symptoms of night blindness, whereas cone function was normally preserved (Figure 1). Based on these findings, vitamin A deficiency was suspected; however, the vitamin A level test performed by his general practitioner was reported normal. On a follow-up 6 months later, the patient complained of worsening visual symptoms. Slit-lamp examination and visual acuity were unchanged, whereas ERG revealed an additional reduction of the cone function (Figure 1). Macular spectral domain OCT (Heidelberg Engineering Spectralis) showed poorly distinguishable outer segments of the photoreceptors (OS) and unrecognizable interdigitation zone (IZ) (Figure 2). Fundus autofluorescence (FAF) was within normal limits. At that time, vitamin A deficiency was confirmed (0.15 µmol/L; normal 1.05–2.80 µmol/L). Further laboratory work-up revealed concomitant vitamin E deficiency, severe iron deficiency anemia, fat malabsorption, and decreased testosterone levels, consistent with secondary hypogonadism. The patient was referred to the clinical nutrition unit at the institute of oncology where further nutritional evaluation revealed gut failure requiring treatment with partial parenteral nutrition including vitamins and microelements supplementation (Vitalipid, Soluvit, and Addamel). Two weeks after the initiation of treatment, the patient's nutritional status improved (+5.7 kg of lean body mass) with normalization of the vitamin A level (1.68 µmol/L), and the patient reported improvement of his visual symptoms. OCT showed improved differentiation of the OS layer (Figure 2). Three months later, the patient reported complete resolution of visual symptoms and OCT showed a further improvement of the OS appearance as well as a reappearance of the interdigitation zone (Figure 2). In additin, the OCT showed an increase in macular thickness including the ganglion cell layer, when analyzed using the segmentation tool included in the Heidelberg Spectralis software. Electroretinography showed normalization of the rod and cone responses (Figure 1).
Fig. 1.
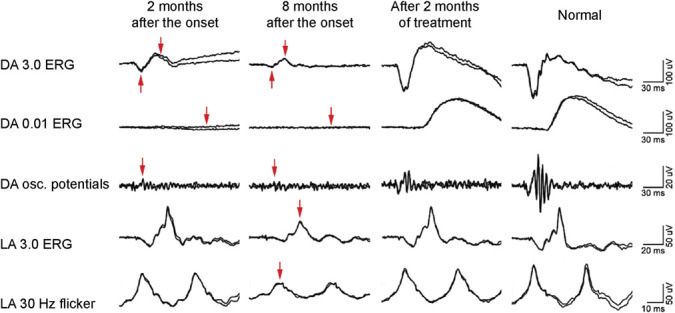
Full-field ERG of patient one before and after treatment. Findings were symmetrical on both eyes, traces from the right eye only are presented. At the first visit, there was a compete loss of rod function, followed by partial loss of cone function at the second visit and complete recovery of both after the treatment. Arrows indicate reduction of the ERG responses. DA, dark adapted; LA, light adapted.
Fig. 2.
Optical coherence tomography of three patients (P1–P3) with vitamin A deficiency. Locations of the OCT scans are noted on fundus autofluorescence images for patients P1 and P2 and infrared image for P3. The images in the dashed rectangles (A–G) are shown magnified and show poorly distinguishable outer segments of the photoreceptors and interdigitation zone. Note the improved delineation of the outer segments of the photoreceptors and the reappearance of the interdigitation zone after treatment in P1 (A–C). The poor quality of OCT image for P3 is due to keratopathy. ELM, external limiting membrane; EZ, ellipsoid zone of the photoreceptors; IZ, interdigitation zone; ONL, outer nuclear layer; OS, outer segments of the photoreceptors; RPE, retinal pigment epithelium. Normal serum vitamin A level: 1.05 µmol/L to 2.80 µmol/L.
After the retinal abnormalities in the first patient were recognized as possibly indicative of vitamin A deficiency, two other patients with gastrointestinal disorders were diagnosed with vitamin A deficiency based on the presence of similar OCT features. Patient 2 was a 66-year-old man with a history of liver transplantation 9 years before and jaundice because of biliary stent blockage, who presented with transitory visual disturbances including nyctalopia. Optical coherence tomography revealed poorly distinguishable OS, and there were hypoautofluorescent dots on FAF (Figure 2). Vitamin A deficiency was suspected and confirmed at 0.20 µmol/L. Electroretinography showed absent rod function and reduced cone function. He is currently awaiting liver transplantation. Patient 3 was a 50-year-old man with a history of chronic alcoholic pancreatitis and severe cachexia who presented with a 1-month history of bilaterally reduced visual acuity. Examination showed severe dry eye syndrome with keratomalacia, whereas OCT (attainable on one eye only because of corneal opacity) showed poorly distinguishable OS, especially in the peripheral parts of the macula (Figure 2). Laboratory work-up confirmed vitamin A deficiency (0.44 µmol/L). He is currently receiving palliative care because of poor general condition.
Discussion
Single reports of patients with vitamin A deficiency have described white dotted fundus, circular hypoautofluorescent dots on FAF, and hyper-reflective material beneath the ellipsoid zone on OCT4–9; however, neither of these features were consistently observed in a larger patient cohort making this case series the largest so far. Contrary to the previous reports, none of our patients exhibited white dotted fundus; moreover, hypoautofluorescent dots on FAF were noted in only one patient. Nevertheless, all patients displayed abnormalities of the OS layer on OCT. Although a more prominent OS disruption with an accumulation of hyper-reflective material under the ellipsoid zone of the photoreceptors5,6,9 has been noted in most of the previous case reports, the OCT features seen in our patients were subtler, consisting only of poorly distinguishable OS and an absent IZ; closest to the case published by de Carvalho et al.8 Interestingly, Hansen et al described a “normal OCT” of a patient with vitamin A deficiency and decreased ERG4; however, on review, the IZ is not clearly recognizable in the published OCT figure. This highlights the subtlety of the vitamin A related OCT features and the need for improvement of their recognition. The reason for the variability of the OCT features is unclear. Potential factors include the length and degree of vitamin A deficiency or other anatomical and physiological variations in the retina. We suspect that the OS abnormalities on OCT are related to the slowed production of the photoreceptor outer segments, which had been previously demonstrated in an animal model of vitamin A deficiency.10 Normalization of the OS and IZ reappearance after treatment support the association of these features with vitamin A deficiency (Figure 2, Patient 1) and are also consistent with an improvement of the photoreceptor morphology after treatment in the animal model.10 The improvement of the ganglion cell layer thickness observed after treatment in Patient 1 is in accordance with a previous observation5 and may reflect other less known roles of vitamin A in the retina. This study supports the association between subtle but relatively specific OCT features and vitamin A deficiency, thereby recognizing the role of OCT in ensuring earlier diagnosis and treatment. It is important to note that the OCT of the normal retina has some variation; therefore, the OCT abnormalities should be evaluated with caution and in light of the patients' visual symptoms and medical history. Vitamin A level testing is an easily accessible method for assessment of patients with suspected vitamin A deficiency based on OCT features, before classical evaluation such as ERG is performed to confirm photoreceptor dysfunction. Vitamin A deficiency may also be associated with other vitamin deficiencies and/or gut failure and should prompt full nutritional evaluation, especially in patients with a history of gastrointestinal disorders who may vastly benefit from either enteral or parenteral nutrition.
Footnotes
None of the authors has any financial/conflicting interests to disclose.
References
- 1.Alvarez R, Vaz B, Gronemeyer H, de Lera AR. Functions, therapeutic applications, and synthesis of retinoids and carotenoids. Chem Rev 2014;114:1–125. [DOI] [PubMed] [Google Scholar]
- 2.Kontos A, Kayhanian H, El-Khouly F, Gillmore R. Night blindness due to vitamin A deficiency associated with resected adenocarcinoma of the pancreas. Int J Ophthalmol 2015;8:206–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singer JR, Bakall B, Gordon GM, Reddy RK. Treatment of vitamin A deficiency retinopathy with sublingual vitamin A palmitate. Doc Ophthalmol 2016;132:137–145. [DOI] [PubMed] [Google Scholar]
- 4.Hansen BA, Mendoza-Santiesteban CE, Hedges TR, III. Reversible nyctalopia associated with vitamin a deficiency after resected malignant ileal carcinoid and pancreatic adenocarcinoma. Retin Cases Brief Rep 2018;12:127–130. [DOI] [PubMed] [Google Scholar]
- 5.Saenz-de-Viteri M, Sadaba LM. Optical coherence tomography assessment before and after vitamin supplementation in a patient with vitamin A deficiency: a case report and literature review. Medicine 2016;95:e2680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aleman TS, Garrity ST, Brucker AJ. Retinal structure in vitamin A deficiency as explored with multimodal imaging. Doc Ophthalmol 2013;127:239–243. [DOI] [PubMed] [Google Scholar]
- 7.Apushkin MA, Fishman GA. Improvement in visual function and fundus findings for a patient with vitamin A-deficient retinopathy. Retina 2005;25:650–652. [DOI] [PubMed] [Google Scholar]
- 8.Lima de Carvalho JR, Jr, Tsang SH, Sparrow JR. Vitamin a deficiency monitored by quantitative short wavelength fundus autofluorescence in a case of bariatric surgery. Retin Cases Brief Rep 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chow CC, Mieler WF. Vitamin A deficiency and xerophthalmic fundus in autoimmune hepatitis and cirrhosis. Retin Cases Brief Rep 2014;8:164–166. [DOI] [PubMed] [Google Scholar]
- 10.Herron WL, Jr, Riegel BW. Production rate and removal of rod outer segment material in vitamin A deficiency. Invest Ophthalmol 1974;13:46–53. [PubMed] [Google Scholar]