Abstract
Background:
Many children have experienced unprecedented levels of stress as a result of the COVID-19 pandemic due to school closures, strained resources, and excess morbidity and mortality. The current study examines change in children’s mental health and sleep during the early months of the US pandemic and identifies risk and protective factors.
Methods:
In May 2020, 225 parents reported on the mental health and sleep of each child (N=392 children) living in their household prior to the onset of the COVID-19 pandemic and about their functioning in the past month. McNemar’s test examined change in mental health and sleep disturbance across developmental stage. Bivariate and multivariate generalized estimating equations examined predictors of change in mental health and sleep.
Results:
Each age group showed a significant change in mental health and sleep outcomes, but the development of mental health problems was greater for older children. Parental caregiving strain (aOR:2.42, 95%CI:1.11–5.27) was identified as a risk factor associated with children developing anxiety and income loss was associated with developing sleep disturbances (aOR:2.34, 95%CI:1.06–5.17). Parental receipt of emotional support was identified as a protective factor for all child health outcomes.
Conclusion:
Policies and interventions that promote access to mental health services, provide financial safety nets, and strengthen social support networks for families are needed.
Keywords: child mental health, child sleep, social support, COVID-19
Introduction
Background
Although fewer cases of COVID-19 have been reported in children (0–17 years) than adults,1 children may be at high risk for psychological stress due to the pandemic. The Center for Disease Control and Prevention (CDC) identifies children as vulnerable to mental stress in the face of disasters as children may experience uncertainty, fear, disrupted routines, physical and social isolation, as well as high levels of parental stress.2 The COVID-19 pandemic has been a stressful experience for many children due to sickness and death as well as school closures and economic shutdowns, straining societal and household resources. School closures alone affected at least 55.1 million school-aged children during the 2019–2020 school year, and restrictions on social contact and gatherings further impinged on social support systems.3
While there is limited empirical evidence on the impact of COVID-19 on children’s mental health, a large body of research has identified anxiety, depression, and impaired sleep as common manifestations of psychological stress in children. In a study of primary school students in the Hubei province of China, where the pandemic originated, about a month into lockdown mandates in early Spring of 2020, 22.6% of children reported depressive symptoms, and 18.9% reported symptoms of anxiety, indicating a higher prevalence of symptoms than pre-pandemic studies of school-aged children in China.4 COVID-19 may also affect psychosomatic responses, such as sleep outcomes, as sleep patterns are linked with children’s emotional well-being. The presence of sleep disturbances has also been found to predict subsequent emotional and behavioral problems in children.5 The goal of this study is to examine changes in children’s mental health and sleep during the early months of the US COVID-19 pandemic and to assess risk and protective factors which can be the target for interventions supporting children’s mental health during the COVID-19 outbreak and future disaster response efforts.
Theoretical framework
This study is guided by the framework proposed by Norris and colleagues and assesses four categories of risk and protective factors for mental health outcomes among disaster-exposed children including exposure severity, personal characteristics, family context, and resource context.6 For example, the extent of exposure to a disaster has been found to be a strong predictor of child psychopathology.7,8 As for personal characteristics, some studies show that older children have greater psychological responses to stress and sleep disturbances than younger children and other studies find no effect of age.7–9 Many studies have found that girls exhibit more symptoms of stress than boys; however, not all studies have documented this relationship.7 Given that gender differences in internalizing symptoms generally emerge at puberty, it may be that gender effects are more pronounced among older children.7,10 A study on sleep outcomes following a natural disaster identified that female gender, younger age, and history of sleep problems heightened the risk of a sleep disturbance for children.11
A salient risk factor for children is strained or stressed family contexts.6 Children in the US usually rely on their parents to provide stable environments and may worry about their parents if they are stressed. The COVID-19 outbreak has caused excess sickness and death and isolated families at home. Additionally, many families are under tremendous emotional and financial stress and unable to receive in-person support. Due to these challenging circumstances, some parents may also experience mental health disorders, and studies conducted in the early months of the COVID-19 pandemic have found high levels of depressive symptoms among parents.12 Parent mental health can influence child health through parent-child relationships. A study conducted in late March 2020 found that approximately 50% of parents reported financial concerns and social isolation as “getting in the way of their parenting.”13 Major disruptive events, like the COVID-19 pandemic, can also heighten household violence and create unsafe environments which activate child stress responses.14
Additionally, psychosocial resources play a central role in mental health responses to a disaster.6 COVID-19 has impacted families’ financial, social, and caregiving resources. High levels of job loss associated with the pandemic have led to increased economic strain, which can limit children’s resources and cause food and housing insecurity. A systematic review of mental health following economic recessions found higher levels of sleep disturbances among children experiencing economic stress.15
Families’ social resources are another important element of risk and protection. Social supports can provide a major reservoir of resources and can limit the depletion of personal resources.16 For example, support systems can help buffer children from the impact of a negative event and provide a safe recovery environment through the provision of emotional and concrete support.17 A study of parental social networks found that parents with more social network members who could provide support were associated with reduced child behavior problems and increased prosocial behaviors.18 However, unlike other disasters, pandemics uniquely affect social interactions by demanding isolation and quarantine rather than the typical mobilization of social support, which involves convergence and gathering.19 These social distancing demands can impact child resilience and recovery by inhibiting peer and community support. A study of children in locales with high H1N1 prevalence found that children experiencing isolation or quarantine exhibited higher psychological distress than those who did not have these experiences.19
Research questions
The goal of the current study is to provide empirical evidence to understand how the COVID-19 pandemic has impacted child well-being and to examine predictors of child well-being guided by Norris and colleagues’ four-level framework.6 This study aims to understand inequalities in child well-being caused by the COVID-19 pandemic in order to inform public health programs. This study is guided by three research questions: How has children’s mental health and sleep changed during the early months of the US COVID-19 pandemic? Does the change in child mental health and sleep differ based on children’s age groups? and, What factors are associated with change in child psychological health and sleep during the early months of the COVID-19 pandemic?6
Methods
Study population
Study participants were drawn from the online longitudinal COVID-19 and Well-Being Study. This study is a longitudinal cohort study which began in March 2020 and aimed to examine individual, social, and societal-level fluctuations related to COVID-19 amid the rapidly changing landscape of the pandemic. Study periods occurred every few months and aimed to capture changes in COVID-19 related information, behaviors, and health status. Participants in the current analysis completed a baseline survey (March 24–27, 2020) and a follow-up survey (May 5–14, 2020). For context, the second wave of data collection occurred when a few states were beginning to reopen and/or lift restrictions on certain business types, but 31 states and the District of Columbia had mandatory Stay at Home Orders and 48 states and the District of Columbia, had recently announced that schools would be closed for the rest of academic year.3,20 The study was approved by the Johns Hopkins Bloomberg School of Public Health IRB.
Study participants were recruited through Amazon Mechanical Turk (MTurk), an online platform. MTurk allows for the study of real-time dynamics of large groups and data collected through MTurk has been found to be reliable.21,22 Study samples recruited through MTurk are not nationally representative but are often more representative than convenience- sampling.21,23 Compared to national samples, MTurk participants tend to be younger, more educated, and underemployed.22 MTurk study samples collected from US residents have been found to overrepresent Asians and underrepresent Black and Hispanics relative to the US population.22
Participants were eligible for the baseline study if they were adults who resided in the US, spoke and read English, and had heard of the coronavirus. MTurk best practices were used to design study protocols.24 During the follow-up survey, participants who reported having a child (<18 years) in their household were invited to participate in a Child Well-Being Supplement. The current study examines parents who participated in the supplement (N=225 parents; 392 children). Retention of participants who reported a child at baseline was 83% with twelve participants reporting a child at baseline but not at follow-up excluded from the sample. Parents who participated in the follow-up did not differ from parents who did not participate on gender, race, receipt of government assistance, and number of children in the household; however, non-respondents were significantly younger than respondents. Participation in the Child Well-Being Supplement was high (93%), and no demographic differences were identified between individuals who elected to participate in the supplement compared to those who did not.
Measures
Child mental health and sleep
Questions on child mental health and sleep were adapted from the National Survey of Children’s Health and the Gulf Coast Child and Family Health surveys.25,26 For each child, parents were asked if the child felt “sad or depressed,” “anxious or afraid,” and if they “had trouble sleeping” in the past month and before the COVID-19 pandemic. Each question was assessed for every child in the household, and response options were a dichotomous “yes” or “no.” To assess predictors of increased mental health or sleep troubles, a dichotomous variable was created for each of the three outcomes. The variable compared children whose symptomology increased (no symptomology before the COVID-19 pandemic to symptomology in May 2020) to children who did not experience change. The small number of children who transitioned from having symptomology before the COVID-19 pandemic to no symptomology in May 2020 (sad/depressed: n=2; anxious/afraid: n=0; trouble sleeping: n=5) were included in the no-change group.
Child and parent demographics
The age and gender were assessed for each child. Parents self-reported their own race as “White,” “Non-Hispanic Black,” “Hispanic,” “Asian,” “Mixed,” or “Other.” Due to the small sample size, “Hispanic” and “Mixed” responses were collapsed with “Other.” Educational attainment compared parents who had some college or above to those who had completed high school or less. Receiving government assistance was measured as reporting that any of their children qualified for free/reduced meals at school or anyone in your household received food stamps or checks from the government.
Family context
Two measures assessed family context. Household discord was assessed through the question from the Coronavirus Impact Scale, “Have you experienced stress or discord in your household?” Response options were: “No, none;” “Yes, household members occasionally short-tempered with one another; no physical violence;” “Yes, household members frequently short-tempered with one another; or children in the home getting in physical fights with one another;” “Yes, household members frequently short-tempered with one another and adults in the home throwing things at one another, knocking over furniture, hitting or harming.”27 To examine the presence versus absence of household discord, the measure was dichotomized to compare no discord with any household discord. Parental depression was examined using the ten-item Center for Epidemiologic Studies Depression scale (CES-D-10). The CES-D-10 scale was dichotomized at 10 or higher which indicates the presence of significant depressive symptoms.28
Severity of COVID-19 exposure
Three measures assessed severity of COVID-19 exposure. Norris and colleagues call for a need to assess both community and individual-level exposure to a disaster.29 Community-level COVID-19 exposure was assessed by the number of new COVID-19 cases per 100,000 using a 7-day rolling average from the start of the second wave of data collection.30 States with 10 or more new daily cases per 100,000 were considered high-risk as they represented dangerous community spread and were compared to states with lower incidence.31 Following Norris and colleagues’ suggestion, individual-level exposure was assessed as injury or threat of injury to self and peers. 29 Peers exposure to COVID-19 was assessed by asking participants the yes/no question, “Do you personally know anyone who has had the coronavirus?” At the time of the study, no individuals had themselves tested positive for COVID-19. Therefore, in addition, working outside of the home was used as a proxy for risk of COVID-19 exposure and participants were asked, “Are you currently required to report to work outside of your home?”
Resource context
Norris and colleagues highlight resource loss and social support as key domains of the resource context. 29 Three measures assessed loss of material and social resources. Income loss was assessed with the question, “My income has already been reduced by the coronavirus.” Responses of “A lot” or “A little” were compared to “Not at all.” Loss of social contact was probed with the yes/no question, “Are you trying to spend less time around other people to prevent getting the coronavirus?” Caregiving strain was assessed with the question, “I am worried about childcare because of the coronavirus.” Responses of “Strongly Agree” and “Agree” were compared to “Neither agree nor disagree,” “Disagree,” and “Strongly Disagree.” Two questions assessed received social support. The amount of childcare network support was elicited by the question, “How many family members or friends could provide childcare for your kids, if needed?” Received emotional support was assessed with “How many family or friends do you talk to weekly about things that are personal or private?” Responses of “0” were compared to all other responses to examine the presence of having at least one person available to provide support.
Analysis
To assess change in mental health and sleep disturbance across developmental stages from before the COVID-19 pandemic to May 2020, we used McNemar’s test. Bivariate and multivariable generalized estimating equations were used to examined predictors of increased mental health and sleep disturbances while accounting for clustering of children within families. Change in child mental health and sleep was assessed with three models: (1) change in sadness/depression, (2) change in anxiety/fear, (3) change in sleep. Covariates that were associated (p<0.10) with change in children’s depression, anxiety, or sleep disturbance were included in multivariable models.32 We modeled each child mental health and sleep outcome using the same covariates to assess specificity of risk and protective factors across models. In the sleep model, spending less time around others was omitted from the analysis as it was not possible to estimate the relationship because everyone who reported not trying to spend less time around others also reported no change in child sleep causing a zero-cell count. Analyses were conducted using Stata 14.33
Results
As seen in Table 1, the majority (41.58%) of children were between the ages of 5 and 11 years, with the remaining children being fairly equally distributed across the other age groups (0–4 years:23.98%; 12–14 years:17.60%; 15–17 years:16.84%). Half of the children were female (49.74%). Children lived in households with an average of 2.30 kids (SD: 1.28). Approximately half (55.10%) of children’s families experienced discord, and 40.31% received government assistance. More than 30% of children’s parents had depressive symptoms (37.76%). One in five children (22.19%) lived in states with high COVID-19 risk. Within the sample, 26% of children had a parent working outside of the home or a parent who knew someone infected with COVID-19. Children had differential access to resources, with 49.74% in households experiencing income loss since the onset of the COVID-19 pandemic, 93.11% in households where less time was spent around others, and 25.51% in households experiencing caregiving strain. A large number of parents had access to childcare support (77.55%) and received regular emotional support (89.29%).
Table 1.
Demographics & COVID-19 related economic and social changes (N=392 children)
| n (%) mean ± SD | |
|---|---|
| Child & parent demographics * | |
|
| |
| Child age (0–4 years) | 94 (23.98) |
| 5–11 | 163 (41.58) |
| 12–14 | 69 (17.60) |
| 15–17 | 66 (16.84) |
| Child sex (Female) | 195 (49.74) |
| Parent sex (Female) | 257 (65.56) |
| Parent race (White) | 305 (77.81) |
| Non-Hispanic Black | 35 (8.93) |
| Asian | 29 (7.40) |
| Other | 23 (5.87) |
| > High school education | 337 (85.97) |
| Government assistance | 158 (40.31) |
|
| |
| Family context | |
|
| |
| Household discord | 216 (55.10) |
| Parent depression | 148 (37.76) |
|
| |
| Severity of COVID-19 exposure | |
|
| |
| Live in high-risk state | 87 (22.19) |
| Parent works outside the home | 103 (26.28) |
| Know someone infected | 102 (26.02) |
|
| |
| Resource context | |
|
| |
| Income loss | 195 (49.74) |
| Caregiving strain | 100 (25.51) |
| Less time around others | 365 (93.11) |
| Childcare support (at least 1 person) | 304 (77.55) |
| Emotional support (at least 1 person) | 350 (89.29) |
Parent demographics were assessed in March 2020 (T1)
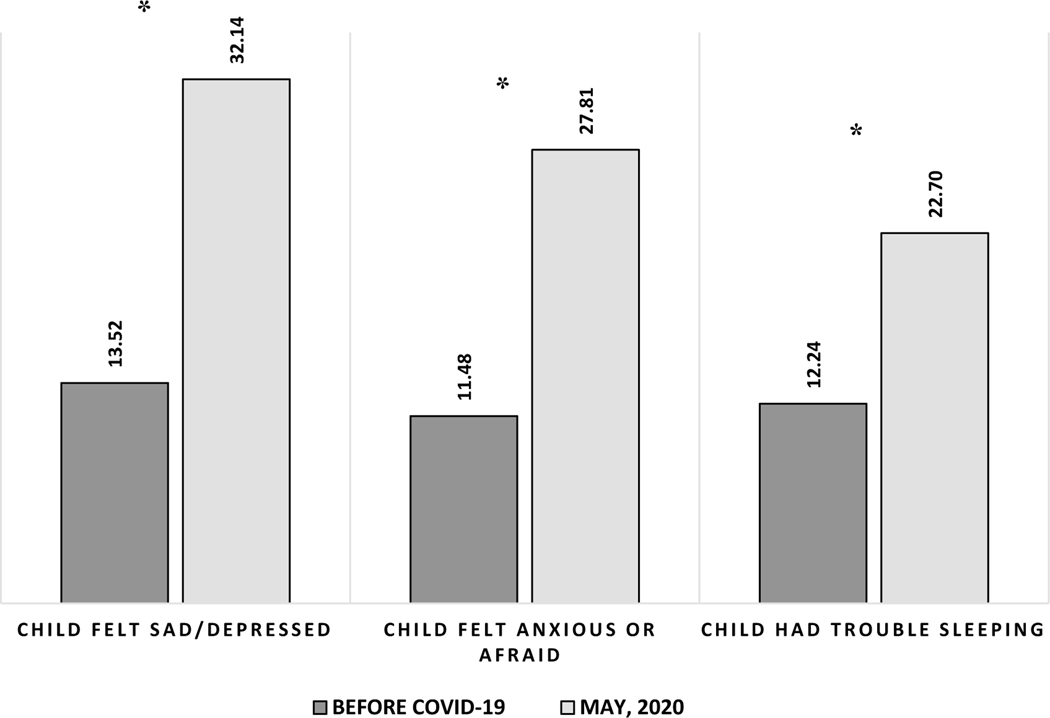
Children had significantly higher mental health and sleep disturbances during the early months of the COVID-19 pandemic (Figure 1; sad/depressed:32.14%; anxious/afraid:27.81%; sleep trouble:22.70%) compared to prior to the COVID-19 pandemic (sad/depressed:13.52%; anxious/afraid:11.48%; sleep trouble:12.24%). When change in mental health and sleep was assessed by age (Table 2), each age group showed a significant change in all outcomes. More older children changed from no anxiety and depression symptomology pre-COVID-19 pandemic to having symptomology during the early months of the COVID-19 pandemic compared to younger children (0–4 years). For example, 24.24% of children in the 15–17 years age group transitioned from no reports of sadness/depression pre-COVID-19 pandemic to having sadness/depression in early May, compared to only 9.57% of children 0–4 years making this same transition. However, change in sleep troubles was relatively equally distributed across age groups with approximately 10% of children in all age groups transitioning from no sleep troubles pre-COVID-19 pandemic to having sleep troubles in May 2020.
Figure 1.
Percent of children experiencing mental health and sleep disturbance from before COVID-19 to May 2020 (N=392)
*p<0.05
Table 2.
Change in children’s mental health and sleep disturbance by age from before COVID-19 to May 2020 (N=392)
| n (%) | Change from pre-COVID-19 to May 2020 | ||||
|---|---|---|---|---|---|
|
| |||||
| Age | ‘No’ at both times | ‘Yes’ at both times | ‘Yes’ to ‘No’ | ‘No’ to ‘Yes’ | p-value |
| Child sad or depressed | |||||
|
| |||||
| 0–4 years | 83 (88.30) | 2 (2.13) | 0 (0.00) | 9 (9.57) | 0.003 |
| 5–11 years | 106 (65.03) | 20 (12.27) | 1 (0.61) | 36 (22.09) | <0.001 |
| 12–14 years | 37 (53.62) | 17 (24.64) | 1 (1.45) | 14 (20.29) | 0.001 |
| 15–17 years | 38 (57.58) | 12 (18.18) | 0 (0.00) | 16 (24.24) | 0.001 |
| All Ages (0–17 years) | 264 (67.34) | 51 (13.01) | 2 (0.51 ) | 75 (19.13) | <0.001 |
|
| |||||
| Child anxious or afraid | |||||
|
| |||||
| 0–4 years | 83 (88.30) | 3 (3.19) | 0 (0.00) | 8 (8.51) | 0.005 |
| 5–11 years | 108 (66.26) | 22 (13.50) | 0 (0.00) | 33 (20.25) | <0.001 |
| 12–14 years | 44 (63.77) | 13 (18.84) | 0 (0.00) | 12 (17.39) | 0.001 |
| 15–17 years | 48 (72.73) | 7 (10.61) | 0 (0.00) | 11 (16.67) | 0.001 |
| All Ages (0–17 years) | 283 (72.19) | 45 (11.48) | 0 (0.00) | 64 (16.33) | <0.001 |
|
| |||||
| Child has trouble sleeping | |||||
|
| |||||
| 0–4 years | 82 (87.23) | 3 (3.19) | 1 (1.06) | 8 (8.51) | 0.020 |
| 5–11 years | 122 (74.85) | 21 (12.88) | 1 (0.61) | 19 (11.66) | <0.001 |
| 12–14 years | 48 (69.57) | 13 (18.84) | 1 (1.45) | 7 (10.14) | 0.034 |
| 15–18 years | 46 (69.70) | 8 (12.12) | 2 (3.03) | 10 (15.15) | 0.021 |
| All Ages (0–17 years) | 298 (76.02) | 43 (10.97) | 5 (1.28) | 46 (11.73) | <0.001 |
Bivariate and multivariable generalized estimating models (Table 3) identified factors associated with change in child psychological and psychosomatic health. At the personal level, older child age was associated with higher odds of developing feelings of depression (5–11 years v. 0–4 years: aOR=3.00; 95%CI=1.46–6.15) and anxiety (5–11 years v. 0–4 years: aOR=2.96, 95%CI=1.24–7.01) during the early months of the COVID-19 pandemic. Family context factors also impacted child psychological health and sleep with parental depression increasing the odds of developing all three outcomes during the COVID-19 pandemic. In bivariate analysis, children in households experiencing discord were more likely to develop sleep trouble; however, this relationship did not remain significant in multivariable models. At the level of severity of COVID-19 exposure, no measures were associated with increased anxiety, depression, or sleep disturbances in this study. At the material and social resources level, the association differed depending on the child outcome measured. Receipt of parental emotional support was associated with reduced odds of children developing child psychological distress, with children whose parents reported receiving emotional support from at least one person having lower odds of developing depression (aOR=0.36, 95%CI=0.14–0.92), anxiety (aOR=0.20, 95%CI=0.07–0.58), and sleep trouble (aOR=0.29, 95%CI=0.11–0.78) compared to children whose parents reported no receipt of emotional support. Children in households experiencing caregiving strain had higher odds of developing anxiety symptoms (aOR=2.42, 95%CI=1.11–5.27) and children in households experiencing income loss were significantly associated with developing sleep disturbances (aOR=2.34, 95%CI=1.06–5.17).
Table 3.
Bivariate and multivariable generalized estimating equations models assessing change in child mental health and sleep from before COVID-19 to May 2020 (N=392)
| Model 1: Child sad/depressed | Model 2: Child anxious or afraid | Model 3: Child has trouble sleeping | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | aOR | OR | aOR | OR | aOR | |
| Child & parent demographics | ||||||
|
| ||||||
| Child age (0–4 years) | REF | REF | REF | REF | REF | REF |
|
| ||||||
| 5–11 | 2.61 (1.28–5.30) | 3.00 (1.46–6.15) | 3.16 (1.37–7.25) | 2.96 (1.24–7.01) | 1.57 (0.75–3.26) | 1.43 (0.62–3.30) |
|
| ||||||
| 12–14 | 2.39 (1.03–5.51) | 2.72 (1.07–6.89) | 1.70 (0.53–5.46) | 2.20 (0.73–6.63) | 1.07 (0.34–3.36) | 0.87 (0.25–2.96) |
|
| ||||||
| 15–17 | 2.11 (0.74–5.96) | 2.64 (0.90–7.68) | 0.88 (0.14–5.49) | 1.66 (0.50–5.52) | 1.30 (0.42–4.07) | 1.53 (0.49–4.79) |
|
| ||||||
| Child sex (Male) | 1.23 (0.77–1.94) | -- | 1.28 (0.77–2.12) | -- | 0.87 (0.51–1.55) | -- |
|
| ||||||
| Parent sex (Female) | 1.16 (0.62–2.20) | -- | 0.83 (0.42–1.64) | -- | 1.19 (0.56–2.53) | -- |
|
| ||||||
| Parent race (White) | REF | REF | REF | REF | REF | REF |
|
| ||||||
| Non-Hispanic Black | 0.82 (0.26–2.61) | -- | 1.10 (0.34–3.51) | -- | 1.04 (0.27–3.80) | -- |
|
| ||||||
| Asian | 0.64 (0.21–1.90) | -- | 0.88 (0.24–3.26) | -- | 1.36 (0.43–4.35) | -- |
|
| ||||||
| Other | 1.83 (0.53–6.29) | -- | 2.15 (0.63–7.41) | -- | 0.95 (0.20–4.54) | -- |
|
| ||||||
| Parent > High school edu. | 4.12 (0.88–19.24) | 2.04 (0.41–10.12) | 4.90 (0.92–26.02) | 3.60 (0.78–16.60) | 2.28 (0.62–8.41) | 1.67 (0.46– 6.04) |
|
| ||||||
| Government assistance | 0.60 (0.30–1.18) | 0.39 (0.18–0.82) | 0.82 (0.41–1.65) | 0.51 (0.22–1.20) | 1.18 (0.57–2.46) | 0.66 (0.30–1.44) |
|
| ||||||
| Family Context | ||||||
|
| ||||||
| Household discord | 1.51 (0.81–2.79) | 1.01 (0.53–1.91) | 1.69 (0.86–3.31) | 0.88 (0.41–1.89) | 2.58 (1.15–5.80) | 1.74 (0.75–4.01) |
|
| ||||||
| Parent depression | 2.96 (1.62–5.39) | 2.61 (1.35–5.04) | 2.91 (1.50–5.62) | 2.54 (1.16–5.56) | 4.69 (2.23–9.88) | 3.14 (1.42–6.95) |
|
| ||||||
| Severity of COVID-19 Exposure | ||||||
|
| ||||||
| Live in high-risk state | 0.81 (0.40–1.66) | -- | 1.37 (0.67–2.82) | -- | 0.54 (0.21–1.40) | -- |
|
| ||||||
| Parent works outside home | 0.54 (0.26–1.12) | 0.71 (0.32–1.58) | 0.65 (0.30–1.42) | 0.93 (0.39–2.21) | 0.72 (0.31–1.68) | 1.17 (0.49–2.78) |
|
| ||||||
| Know someone infected | 1.48 (0.77–2.84) | -- | 1.39 (0.68–2.82) | -- | 1.23 (0.56–2.70) | -- |
|
| ||||||
| Resource Context | ||||||
|
| ||||||
| Income loss | 1.26 (0.70–2.29) | 1.10 (0.56–2.15) | 1.20 (0.63–2.31) | 1.21 (0.59–2.47) | 2.70 (1.27–5.70) | 2.34 (1.06–5.17) |
|
| ||||||
| Caregiving strain | 1.88 (0.99–3.58) | 1.90 (0.96–3.76) | 0.64 (0.30–1.36) | 2.42 (1.11–5.27) | 0.41 (0.19–0.87) | 1.71 (0.79–3.74) |
|
| ||||||
| Less time around others | 9.91 (1.41–69.54) | 5.25 (0.78–35.21) | 2.28 (0.46–11.24) | 1.47 (0.33–6.58) | xx | xx |
|
| ||||||
| Childcare support | 0.72 (0.35–1.46) | 1.02 (0.47–2.22) | 0.64 (0.30–1.36) | 0.97 (0.38–2.45) | 0.41 (0.19–0.87) | 0.62 (0.29–1.34) |
|
| ||||||
| Emotional support | 0.33 (0.14–0.77) | 0.36 (0.14–0.92) | 0.21 (0.08–0.51) | 0.20 (0.07–0.58) | 0.24 (0.09–0.64) | 0.29 (0.11–0.78) |
Bold : p≤0.05
not included in the model
omitted
Discussion
The current study examined changes in child mental health and sleep during the early months of the US COVID-19 pandemic and identified that a significant proportion of children experienced an increase in mental health and sleep issues compared to pre-COVID-19 pandemic functioning. This study identified demographic, family context, and resource-related risk and protective factors associated with child mental distress during the COVID-19 pandemic.6 We echo findings from studies in China and England that identified a higher prevalence of mental health symptomology among children during the COVID-19 pandemic than before.34,35 Experiencing elevated psychological sequelae is a normative response to stressful events; however, it is imperative to mitigate serious and lasting psychological problems following the waves of the COVID-19 pandemic. Identifying subgroups of children and families to target and intervening on these factors may help mitigate the long-term impact of COVID-19 on child psychological health.
A key finding from this study is that the COVID-19 pandemic has differentially affected children’s mental health and sleep based on age. Study findings indicate that older children may be at higher risk of developing mental health symptoms during the COVID-19 pandemic compared to younger children. This could be the result of parents being better able to detect symptomology in older children compared to younger children.36 However, the finding is consistent with a study conducted in China using child-reported outcomes which found that anxiety levels in adolescents during the COVID-19 pandemic were significantly higher than those of younger children.34 The higher level of mental health symptoms in older children during the early months of the COVID-19 pandemic may be attributable to the fact that school-aged children are more likely to have disrupted routines because of school closures compared to younger children. Interestingly, our research did not identify a relationship between the onset of sleep disturbances and age. Perhaps this lack of age-related differences in sleep was because, among children, sleep disturbances are highly prevalent in all age groups, whereas mental health disturbances are more often identified in older children.36,37
Another key finding from this study was that parental depression was identified as a strong and consistent risk factor for child mental health and sleep disturbances during the early months of the COVID-19 pandemic. It may be that parents with depression are more sensitive to their children’s well-being and more apt to identify when they are distressed.38 However, it has also been argued that parents with depression who are withdrawn and hopeless may have decreased effectiveness at identifying child depression.38 This finding of a significant relationship between parental and child depression, is consistent with previous studies that identify parental post-traumatic stress as significantly associated with child distress after a disaster using independent reports from parents and children.39
These findings of elevated psychological distress among children have several public health implications. Previous research has identified that there is limited access to and underutilization of mental health services among children and families.40 To address this gap, access to affordable and convenient mental health services must be expanded for families. During the COVID-19 pandemic, when access to in-person services is limited, expansion of tele-mental health services for children and parents can help reduce psychological stress because telemedicine has been found to be similarly effective as compared to in-person services.41 However, provision of telemedicine care can heighten disparities as not all families have access to the needed technology. In this study, four of ten children lived with at least one parent with depression, indicating a need for coordinated mental health services that integrate child and parent health. Furthermore, due to the high levels of distress identified among both children and parents, universal prevention strategies should also be considered. As schools and workplaces re-open, organizations should embed services and policies which promote mental well-being. One strategy is for school systems to integrate social and emotional learning (SEL) for all students to provide universal socioemotional support.42 SEL refers to the capacity to recognize and manage emotions, solve problems effectively, and establish positive relationships with others.42
Another finding from this study was that family’s resources were consistently associated child well-being outcomes during the early months of the COVID-19 pandemic. The study identified economic and caregiving strain as risk factors associated with child mental health and sleep during the COVID-19 pandemic. These factors have also been found to be associated with poor parent mental health in previous research.43 Provision of weekly emotional support from at least one person to parents was identified as a protective factor for all child mental health and sleep outcomes. Additionally, having at least one person in the network who could provide caregiving support was associated with reduced change in sleep troubles. Identifying the intertwined relationship between family resources and child well-being during the early months of the COVID-19 pandemic suggests the need for public health interventions focused on supporting family social and economic resources to protect child well-being. For example, socioeconomic safety nets and caregiving supports should be strengthened to address the causes of stress during the COVID-19 pandemic. Comprehensive care teams can administer online screening tools to assess economic hardship and provide lists of aligned resources.44 Some parents have been pushed out of work because they need to provide childcare.45 To support caregiving, policies such as paid parental leave and practices for parents that allow for flexible work arrangements are needed. Our research also indicates that during the COVID-19 pandemic many social relationships and caregiving structures have been disrupted. This finding highlights the importance of support networks for parents and their potential for enhancing child well-being. COVID-19 vaccinations have allowed many families to reconnect; however, new variants can pose additional risks and the reinstatement of distancing recommendations. From an intervention perspective, communication campaigns that encourage families and peers to connect via social media, phone, or through socially distanced interactions could promote child well-being.
In contrast to previous research,34 no association was identified between severity of COVID-19 exposure and change in child mental health outcomes. These contrasting findings may be a product of the outcome measure as this study examines change in child anxiety, whereas Duan and colleagues looked at child anxiety at one time point. Alternatively, it may be that the other factors that were included in the models have more valence in relation to child mental health than does severity of exposure to COVID-19. Our findings are aligned with Jiao and colleagues (2020), who found that living in a state with a high level of epidemic risk was not significantly associated with child well-being outcomes.46
This study adds to the limited body of research on child mental health during the early months of the US COVID-19 pandemic. Study findings have identified both risk and protective factors which can be the target of interventions to address child well-being during the pandemic. Additionally, through collecting data on all children in the household, we were able to assess age-related changes in child mental health and sleep and identify age-related differences in the impact of COVID-19 on child health. There are a few limitations to this study. First, this study uses parent-reported outcomes. Parental report only has moderate concordance with child-reported mental health outcomes.47 With school closures and children’s vulnerability status, it was difficult to access samples of children and to ensure parental consent during the early stages of the COVID-19 pandemic. Future studies should work with schools to educate families about the importance of including the perspective of children to collect information from both parents and children. Additionally, alternative methods of severity of COVID-19 exposure, which is a multidimensional construct, should be utilized. For example, this study used a state-level measure of community risk and more localized measures may have different relationships with child mental health. Additionally, this study assessed parents working outside the home as measure of risk exposure however, not all work environments may have heightened risk of exposure in the early months of the pandemic. Future research should also utilize CDC criteria to assess risk exposure and frequency. Our study’s findings may also have been affected by social desirability and recall bias. We asked parents to think retrospectively about their children’s mental health pre-COVID-19 pandemic; this approach may provide differential estimates as compared to data collected prior to the COVID-19 pandemic. Additionally, future studies should use scale measures of child mental health and sleep to increase specificity. The purpose of the questionnaire used in this study was not to establish a final diagnosis of a mental health or sleep disorder but to screen for initial signs of emotional and psychosomatic disturbances.
The ongoing trajectory of the COVID-19 pandemic is uneven, and children may continue to experience household stress, the loss of socioeconomic resources, and fear of becoming infected or losing a loved one. Based on these results, we advocate for policies that provide a financial safety net to families and for interventions that strengthen social support networks. To address distress, more comprehensive care systems are needed that integrate primary care, psychiatric care, and socioeconomic support resources to identify and address children and family needs. Widespread uptake of COVID-19 vaccination is essential to help reestablish social networks. Continued longitudinal research on child and family psychological health and access to psychosocial resources is imperative to inform tailored and developmentally appropriate interventions.
Acknowledgements & Study Support:
This study was supported by R01 DA040488 and Alliance for a Healthier World
Footnotes
Conflict of interest/Competing interests: The authors do not have any conflicts of interests to declare
References
- 1.Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus Disease 2019 Case Surveillance — United States, January 22–May 30, 2020. MMWR. 2020;69(24):759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Charing for children in disasters: How are children different from adults? https://www.cdc.gov/childrenindisasters/differences.html. Updated 2020. Accessed September 2, 2020.
- 3.Education Week. Map: Coronavirus and School Closures in 2019–2020. https://www.edweek.org/ew/section/multimedia/map-coronavirus-and-school-closures.html. Updated 2020. Accessed September 22, 2020.
- 4.Xie X, Xue Q, Zhou Y, et al. Mental Health Status Among Children in Home Confinement During the Coronavirus Disease 2019 Outbreak in Hubei Province, China. JAMA Pediatrics. 2020;174(9):898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ivanenko A, Crabtree VM, Obrien LM, Gozal D. Sleep complaints and psychiatric symptoms in children evaluated at a pediatric mental health clinic. Journal of Clinical Sleep Medicine. 2006;2(1):42–48. doi: 10.5664/jcsm.26434. [DOI] [PubMed] [Google Scholar]
- 6.Norris FH, Friedman MJ, Watson PJ. 60,000 Disaster Victims Speak: Part II. Summary and Implications of the Disaster Mental Health Research. Psychiatry. 2002;65(3):240–260. doi: 10.1521/psyc.65.3.240.20169. [DOI] [PubMed] [Google Scholar]
- 7.Furr JM, Comer J, Edmunds JM, Kendall PC. Disasters and youth: A meta-analytic examination of posttraumatic stress. Journal of Consulting and Clinical Psychology. 2010;78(6):765–780. doi: 10.1037/a0021482. [DOI] [PubMed] [Google Scholar]
- 8.Tang B, Liu X, Liu Y, Xue C, Zhang L. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health. 2014;14(1):623. doi: 10.1186/1471-2458-14-623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Camhi S. Factors affecting sleep disturbances in children and adolescents. Sleep medicine. 2000;1(2):117–123. doi: 10.1016/s1389-9457(99)00005-2. [DOI] [PubMed] [Google Scholar]
- 10.Angold A, Costello EJ. Puberty and Depression. Child and Adolescent Psychiatric Clinics of North America. 2006;15(4):919–937. doi: 10.1016/j.chc.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 11.Lai BS, La Greca AM, Colgan CA, et al. Sleep Problems and Posttraumatic Stress: Children Exposed to a Natural Disaster. Journal of Pediatric Psychology. 2020;45(9):1016–1026. doi: 10.1093/jpepsy/jsaa061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee S, Ward K. Mental health, relationships, and coping during the coronavirus pandemic. Parenting in Context Research Lab. 2020. [Google Scholar]
- 13.Lee S, Ward K. Stress and parenting during the coronavirus pandemic. Parenting in Context Research Lab. 2020. [Google Scholar]
- 14.Curtis T, Miller BC, Berry EH. Changes in reports and incidence of child abuse following natural disasters. Child Abuse & Neglect. 2000;24(9):1151–1162. doi: 10.1016/S0145-2134(00)00176-9. [DOI] [PubMed] [Google Scholar]
- 15.Frasquilho D, Matos MG, Salonna F, et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health. 2016;16(1):115. doi: 10.1186/s12889-016-2720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hobfoll S, Freedy J, Lane C, Geller P. Conservation of social resources: Social support resource theory. Journal of Social and Personal Relationships. 1990;7:465–478. [Google Scholar]
- 17.Sprague C, Sprague C, Kia-Keating M, et al. Youth Psychosocial Adjustment Following Wildfire: The Role of Family Resilience, Emotional Support, and Concrete Support. Child Youth Care Forum. 2015;44(3):433–450. doi: 10.1007/s10566-014-9285-7. [DOI] [Google Scholar]
- 18.Koyama Y, Fujiwara T, Isumi A, Doi S. Association of parental social network diversity with behaviour problems and resilience of offspring in a large population-based study of Japanese children. BMJ Open. 2020;10(e035100). doi: 10.1136/bmjopen-2019-035100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sprang G, Silman M. Posttraumatic Stress Disorder in Parents and Youth After Health-Related Disasters. Disaster Medicine and Public Health Preparedness. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- 20.Moreland A, Herlihy C, Tynan MA, et al. Timing of State and Territorial COVID-19 Stay-at-Home Orders and Changes in Population Movement — United States, March 1–May 31, 2020. Morbidity and Mortality Weekly Report. 2020;69(35):1198–1203. doi: 10.15585/mmwr.mm6935a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berinsky AJ, Huber GA, Lenz GS. Evaluating Online Labor Markets for Experimental Research: Amazon.com‘s Mechanical Turk. Political Analysis. 2012;20(3):351–368. doi: 10.1093/pan/mpr057. [DOI] [Google Scholar]
- 22.Paolacci G, Chandler J. Inside the Turk: Understanding Mechanical Turk as a Participant Pool. Current Directions in Psychological Science. 2014;23(3):184–188. doi: 10.1177/0963721414531598. [DOI] [Google Scholar]
- 23.Huff C, Tingley D. “Who are these people?” Evaluating the demographic characteristics and political preferences of MTurk survey respondents. Research & Politics. 2015;2(3):205316801560464. doi: 10.1177/2053168015604648. [DOI] [Google Scholar]
- 24.Young J, Young K. Don’t Get Lost in the Crowd: Best Practices for Using Amazon’s Mechanical Turk in Behavioral Research. Journal of the Midwest Association for Information Systems. 2019(2):7–34. doi: 10.17705/3jmwa.000050. [DOI] [Google Scholar]
- 25.U.S. Department of Health and Human Services. National Survey of Children’s Health. 2019.
- 26.Abramson D, Stehling-Ariza T, Garfield R, Redlener I. Prevalence and Predictors of Mental Health Distress Post-Katrina: Findings From the Gulf Coast Child and Family Health Study. Disaster Medicine and Public Health Preparedness. 2008;2(2):77–86. doi: 10.1097/DMP.0b013e318173a8e7. [DOI] [PubMed] [Google Scholar]
- 27.Stoddard J, Kaufman J. Coronavirus Impact Scale. Johns Hopkins University. 2020. [Google Scholar]
- 28.Zhang W, O’Brien N, Forrest JI, et al. Validating a Shortened Depression Scale (10 Item CES-D) among HIV-Positive People in British Columbia, Canada. PloS One. 2012;7(7):e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 Disaster Victims Speak: Part I. An Empirical Review of the Empirical Literature, 1981–2001. Psychiatry. 2002;65(3):207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- 30.USAFacts . US Coronavirus Cases and Deaths Track COVID-19 data daily by state and county https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/. Updated 2020. Accessed Sept 6, 2020.
- 31.Harvard Global Health Institute and Harvard’s Edmond J. Safra Center for Ethics. Key Metrics for COVID Suppression. 2020. [Google Scholar]
- 32.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code for Biology and Medicine. 2008;3(1):17. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.StataCorp. Stata Statistical Software: Release 14. 2015. [Google Scholar]
- 34.Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. Journal of Affective Disorders. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Newlove-Delgado T, McManus S, Sadler K, et al. Child mental health in England before and during the COVID-19 lockdown. Lancet Psychiatry. 2021. doi: 10.1016/S2215-0366(20)30570-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dopheide J. Recognizing and treating depression in children and adolescents. American Journal of Health-System Pharmacy. 2006;63(3):233–243. doi: 10.2146/ajhp050264. [DOI] [PubMed] [Google Scholar]
- 37.Ohayon A, Roberts R, Zulley J, Smirne S, Priest R. Prevalence and Patterns of Problematic Sleep Among Older Adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(12):1549–1556. doi: 10.1097/00004583-200012000-00019. [DOI] [PubMed] [Google Scholar]
- 38.Logan D, King C. Parental identification of depression and mental health service use among depressed adolescents. J. Am. Acad. Child Adolesc. Psychiatry. 2002;41(3):296–303. [DOI] [PubMed] [Google Scholar]
- 39.Juth V, Silver RC, Seyle DC, Widyatmoko CS, Tan ET. Post-Disaster Mental Health Among Parent–Child Dyads After a Major Earthquake in Indonesia. J Abnorm Child Psychol. 2015;43(7):1309–1318. doi: 10.1007/s10802-015-0009-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Owens P, Hoagwood K, Horwitz S, et al. Barriers to children’s mental health services. J. Am. Acad. Child Adolesc. Psychiatry. 2002;41(6):731–738. [DOI] [PubMed] [Google Scholar]
- 41.Bashshur RL, Shannon GW, Bashshur N, Yellowlees PM. The Empirical Evidence for Telemedicine Interventions in Mental Disorders. Telemedicine Journal and e-Health. 2016;22(2):87–113. doi: 10.1089/tmj.2015.0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zins JE, Elias MJ. Social and Emotional Learning: Promoting the Development of All Students. Journal of educational and psychological consultation. 2007;17(2–3):233–255. doi: 10.1080/10474410701413152. [DOI] [Google Scholar]
- 43.American Psychological Association. Stress in the Time of COVID-19, Volume One. 2020. [Google Scholar]
- 44.Fallon B, Lefebvre R, Collin-Vézina D, et al. Screening for economic hardship for child welfare-involved families during the COVID-19 pandemic: A rapid partnership response. Child Abuse & Neglect. in press:104706. doi: 10.1016/j.chiabu.2020.104706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alon T, Doepke M, Olmstead-Rumsey J, Tertilt M. The impact of Covid-19 on gender equality. National Bureau of Economic Research. 2020. [Google Scholar]
- 46.Jiao WY, Wang LN, Liu J, et al. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. Euorpean Paediatric Association. 2020;17(3):230–233. doi: 10.15690/pf.v17i3.2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.De Los Reyes A, Kazdin AE. Measuring Informant Discrepancies in Clinical Child Research. Psychological Assessment. 2004;16(3):330–334. doi: 10.1037/1040-3590.16.3.330. [DOI] [PubMed] [Google Scholar]