Abstract
Background
Partial hospitalization programs (PHPs) are intensive outpatient mental health programs. During the COVID-19 pandemic, our PHP was converted from an in-person service to a completely virtual telehealth service. This study compared the outcomes of care between these two versions of our PHP.
Methods
In the live version of the program, care was provided to patients aged 18 to 65 years in person, five days a week, with five groups per day and additional services, such as family work. In the telehealth version, we attempted to provide the same services by HIPAA–secure videoconferencing and telephone, after educating staff and patients. The attendance at clinic, the hospitalization rate, and patient satisfaction with care were compared between the two program versions in the 12 months prior to and after the transition to virtual care.
Results
There were 4,821 patient visits in the in-person program, and 4,371 in the telehealth program. Compared to the in-person program, the telehealth program was associated with a higher attendance (84.5% vs. 89.5%, p = 0.0168), a lower hospitalization rate (16.5% vs. 8.9%, p = 0.02), without a difference in the patient satisfaction rate, and with 74.3% of patients reporting improvement in their condition.
Conclusions
A PHP completely delivered via telehealth was feasible to implement, and some outcomes with such a program were superior to those of a live PHP. Because this was a nonexperimental study, factors other than the method of service provision may have been responsible for the observed results.
This article examines the efficacy of virtual care for the subacute mental health population in an adult partial hospitalization program (PHP). The PHP is a short-term (up to 6 weeks), clinically intensive outpatient mental health care service designed to help high-risk individuals suffering from a subacute episode of mental illness to stabilize symptoms and transition back to their roles in the community. According to part 587.12 of the Codes, Rules and Regulations of the State of New York, “a partial hospitalization program shall provide active treatment designed to stabilize and ameliorate acute symptoms, to serve as an alternative to inpatient hospitalization, or to reduce the length of a hospital stay within a medically supervised program.”1 The PHP provides high-level services, similar to those found on inpatient units, but on an outpatient basis.2 , 3 A PHP serves a twofold purpose, as either a step-down service from inpatient psychiatric hospitalization, or as a higher level of care when referred from an outpatient or emergency room setting. The Zucker Hillside Hospital PHP provides care to patients aged 18 to 65 years from a wide variety of ethnic and cultural backgrounds with various mental health diagnoses. Services are historically provided exclusively in person, five days per week from 9:00 a.m. to 3:00 p.m., with an average length of stay of approximately 4.5 weeks. The program consists of five groups daily, twice weekly individual therapy, occupational therapy, diagnostic evaluation, medication management, case management, and family work.
Zucker Hillside Hospital PHP is located in Queens, New York, an area tremendously affected by the COVID-19 pandemic.4 In March 2020, cases of COVID-19 were rising rapidly in the region, and the program had to make swift decisions to ensure the safety of both patients and staff. Prepandemic, using telepsychiatry and a virtual care model for the PHP had not been considered, given the nature of the service delivery and patient profile. Here, virtual care was defined as treatment provided via video teleconferencing platform in which the patient is situated at a location outside of the clinical setting. It was believed that the PHP services were too labor intensive and complex to deliver virtually, and the patient cohort was considered too psychiatrically unstable to benefit from virtual care. Nonetheless, a virtual model of care was developed in the interest of patient and staff safety. Hospital administration, program management, and the clinical team worked to weigh the concerns related to providing virtual PHP services against the health risks of continuing in-person care along with anticipation of citywide stay-at-home orders. Ultimately, the decision to convert PHP to 100% virtual was made, and planning quickly began. In-house services were officially stopped, and PHP was fully virtual, as of March 19, 2020.
Methods
At the outset, it was critical to develop a virtual service delivery plan that was consistent with the program's mission to help patients avoid or reduce hospitalization by stabilizing their subacute symptoms. It was a priority to ensure that patient care would not suffer from the decision to provide virtual care and that all New York State Office of Mental Health Clinic Standards of Care continued to be met.5 The planning was done collaboratively with clinical staff and leadership to ensure the most comprehensive plan possible. The team committed to providing a structured schedule of five groups each day, individual therapy twice weekly, occupational therapy, medication management, diagnostic evaluations, case management, family work, and daily safety check-ins. The virtual services were designed to mimic the care provided in person, but through a telehealth platform. To make this happen, plans were developed to use HIPAA–secure videoconferencing platforms and telephonic services.6 Platforms for group facilitation, individual sessions, and staff communication were identified and put into practice. Staff were given access and quickly trained on the proper use of these platforms prior to transitioning to virtual care. Support was provided to patients who struggled with accessing or using the technology necessary to participate in virtual care. Staff provided step-by-step instructions either via e-mail or by phone to assist patients with accessing the virtual care platform. Patients were offered practice sessions with the assistance of the referring provider prior to intake to help them learn the system and feel more comfortable with accessing care virtually.
Interventions
Many people experienced increased anxiety and depression as a result of changes brought about by COVID-19—such as job loss, social isolation, and bereavement—which greatly exacerbated symptoms for those with preexisting mental health conditions.7 The PHP team implemented support calls to provide added assistance to patients who were struggling. The support calls were an added service to what had been provided in person and typically occurred outside the scheduled program hours. These were not designed to be additional therapy sessions but rather brief phone calls to provide patients with encouragement and reinforce skills learned in group sessions.
Measures
As the virtual PHP was underway, it was critical to evaluate the ability of the program to keep patients safe and promote wellness in a virtual care environment. The team identified four specific criteria by which to evaluate the efficacy of the new model as compared to in-person care: attendance and participation, clinical progress, hospitalization rate, and patient satisfaction.
One metric we wanted to evaluate was the extent to which patients were still attending and participating in the program. Research suggests that patients who have poor program participation often experience an exacerbation of mental health symptoms.8 For PHP, the New York State Office of Mental Health9 counts a visit as services provided to a patient for a minimum of four hours in a given day. We compared the total patient visits for the 12 months prior to virtual care to the total patient visits during the first 12 months after providing virtual care. The rolling year data mitigated seasonal variance. We also examined patient attendance rates as a proportion of completed visits out of all possible visits based on the daily census for the same period.
To monitor clinical progress, we examined the patients’ Clinical Global Impressions (CGI) scales. The CGI is an evidence-based rating tool that evaluates various categories on a seven-point scale where 1 indicates no symptoms and 7 indicates the most severe symptoms.10 We examined the rating for severity of functioning, which is assessed by the clinician, as well as patient self-rating, which is evaluated by the patient directly. We compared the average change in rating from admission to discharge for each scale for 12 months pre and post virtual care.
We also closely monitored hospitalization rates as a clinical outcome metric. Because the purpose of PHP is to reduce or avoid inpatient hospitalizations,1 this has been a particularly important metric to evaluate. The number of hospitalizations per month from March 2019 to February 2020 was compared with the hospitalization numbers for March 2020 to February 2021. We examined the actual number of hospitalizations of patients enrolled in PHP as well as the rate as a percentage of all discharges in that period. We know that health systems in the region experienced a decrease in non-COVID medical hospitalizations during the height of the pandemic.11 We also anticipated hesitation from the community at large to go to emergency rooms or inpatient hospitals for behavioral health symptoms because of the pandemic. To account for this, we evaluated our change in hospitalization data trending with the volume in our hospital's behavioral health emergency department.
Finally, we used a patient satisfaction survey (Appendix 1, available in online article) to assess patients’ perception of the virtual care provided. The survey sought to obtain information regarding how the patient felt their condition improved, how well the staff worked together to provide care, and the team's ability to meaningfully include the patient in treatment decisions. The survey also evaluated the program's effectiveness based on an overall likelihood to recommend.
Results
Using the in-person PHP data as a benchmark, the PHP team evaluated the success of the virtual program by assessing changes in patient attendance and participation rates; clinical outcome measures using the CGI scale; hospitalization rates for enrolled patients; and patient satisfaction scores. During the transition to virtual care, 24.1% of patients faced challenges using the necessary technology. As patients became more comfortable overall with virtual care, we noticed a decrease to 11.4% of patients having difficulty using the telehealth platform. Patients were encouraged to use their own devices to join virtual sessions. However, in rare instances, patients were offered temporary use of smartphones provided by the Zucker Hillside Hospital. Only 3 of the 296 patients were loaned smart phones to engage in care. All others already had access to the appropriate technology.
The demographic composite of our patient population remained relatively unchanged before and after moving to a virtual care model (Table 1 ). This allowed for a clear assessment of the effectiveness of the virtual care model implemented during this period.
Table 1.
Patient Demographics
| Pre-Telehealth (March 2019–Feb 2020) |
Post-Telehealth (March 2020–Feb 2021) |
|||
|---|---|---|---|---|
| n | % | n | % | |
| Mean age in years | 32 | 33 | ||
| Sex | ||||
| Male | 123 | 37.0 | 98 | 33.1 |
| Female | 209 | 63.0 | 198 | 66.9 |
| Race | ||||
| Asian | 35 | 10.5 | 18 | 6.1 |
| Black | 41 | 12.3 | 55 | 18.6 |
| Native American | 4 | 1.2 | 1 | 0.3 |
| White | 203 | 61.1 | 169 | 57.1 |
| Multiracial | 49 | 14.8 | 53 | 17.9 |
| Ethnicity | ||||
| Hispanic | 29 | 8.7 | 26 | 8.8 |
| Non-Hispanic | 303 | 91.3 | 270 | 91.2 |
| Marital Status | ||||
| Single | 227 | 68.4 | 167 | 56.4 |
| Married | 35 | 10.5 | 25 | 8.4 |
| Divorced | 7 | 2.1 | 12 | 4.1 |
| Unknown | 63 | 19.0 | 92 | 31.1 |
| Primary Insurance | ||||
| Medicaid | 101 | 30.4 | 103 | 34.8 |
| Medicare | 27 | 8.1 | 32 | 10.8 |
| Commercial | 201 | 60.5 | 160 | 54.1 |
| Self-Pay | 3 | 0.9 | 1 | 0.3 |
| Secondary Insurance | ||||
| Medicaid | 31 | 9.3 | 32 | 10.8 |
| Medicare | 4 | 1.2 | 1 | 0.3 |
| Commercial | 7 | 2.1 | 5 | 1.7 |
The PHP staff worked to develop innovative solutions to challenges that arose specific to providing services in a virtual care environment (Table 2 ).
Table 2.
Challenges and Solutions
| Challenge | Solution |
|---|---|
| Approximately 11% of patients have difficulty accessing and using the necessary technology to engage in the virtual platform. | The PHP team works closely with the referring clinicians to assess each patient's technology needs. The program manager provides patients with guidance and offers practice sessions prior to admission into the program. On the day of intake, the PHP team calls the patient and assists in logging on to the telehealth platform and walks them through the process. |
| Approximately 35% of PHP patients require bloodwork, EKGs, or long-acting injectable medications with program staff no longer on site. | PHP collaborated with other outpatient clinics at Zucker Hillside Hospital to establish a centralized lab and injection clinic for those patients in need of this valuable in-person service. The program also used a mobile lab service that provided patients the option to receive lab work from their homes. |
| Managing payers and appropriate reimbursement for virtual care was an unknown for a PHP level of service. | The medical record was modified to include virtual care indicators so billing could be accurately submitted to the payers. Services were provided and documented in accordance with federal and state regulation and state of emergency orders, as well as within the guidelines of managed care contracts. |
| Management of physical side effects and comorbid medical conditions in a virtual care setting for approximately 40% of patients | Patients and their family members were educated on monitoring symptoms and side effects at home, including use of home blood pressure monitoring devices. Patients were regularly encouraged to use their home monitoring devices during the telepsychiatry session to ensure proper use and accurate results. |
| Internal team member communication is more difficult because staff are not in one location. In-person meetings, daily briefs, and quick informal communication are not available. | A secure digital chat program is used for morning briefs as well as ongoing daily communication regarding patient care. Staff conduct twice weekly team meetings on a videoconferencing platform to discuss patient care and provide peer support for clinical issues. |
PHP, partial hospitalization program; EKG, electrocardiogram.
Attendance and Participation
A review of the attendance in the PHP from March 2019 to February 2020, prior to providing virtual care, showed a total of 4,821 visits. The attendance from March 2020 to February 2021, after the virtual care model was implemented, was 4,371 visits (Figure 1 ). However, 443 of the 450 visits lost were accounted for by the initial three months of virtual care which took place at the height of the COVID-19 pandemic in New York. A comparison of average visits of the following months, June through February, indicates a net loss of only 7 visits. This suggests that the number of patient visits was not greatly affected by the implementation of the virtual care model.
Figure 1.
This line graph compares in-person vs. virtual visits by month.
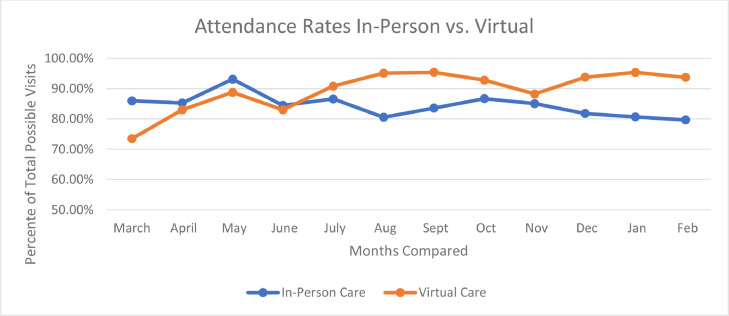
An evaluation of the attendance rate over the same period indicates a 5.9% average increase in the attendance of enrolled patients. Services provided in person yielded an average attendance rate of 84.5%, while services provided virtually yielded an average attendance rate of 89.5% (Figure 2 ). This is consistent with data found in other studies, suggesting that the use of telehealth services typically results in increased attendance rates.12 Patients enrolled in the program demonstrated improved utilization of services in a virtual environment.
Figure 2.
This line graph compares in-person and virtual attendance rates over the study period.
Clinical Global Impressions
Patients in the PHP are assessed using CGI scales as an outcome measure. For this project we focused on the CGI Severity of Functioning scores as well as the CGI Patient Self-Rating scores. The average change in CGI Severity of Functioning from admission to discharge on this scale remained unchanged comparing pre and post virtual care. In both conditions, patients typically demonstrated an improvement of 1.1 points on the rating scale. There was no change in this metric resulting from providing virtual care. The Patient Self-Rating scale showed an average improvement of 0.6 points for in-person care and an improvement of 0.5 points for virtual care. The difference in improvement variance was not statistically significant (p = 0.4541), indicating no adverse effect of providing care virtually.
Hospitalization of Enrolled Patients
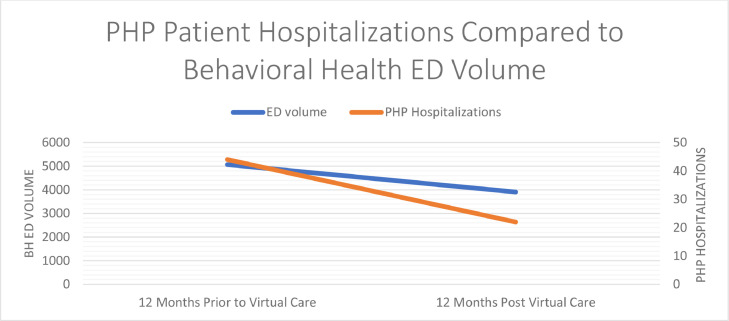
Patient hospitalizations were closely monitored as an outcome quality measure. During the 12-month period immediately prior to virtual care, the PHP had a total of 44 patients who were hospitalized while enrolled in the program. The 12-month period following the implementation of virtual services had only 22 hospitalizations of enrolled patient. This reduction in hospitalizations was significant based on an analysis of a two tailed t-test yielding a t value of 3.704, p = 0.0012.
To account for any fluctuation in census, the hospitalizations were also calculated as a percentage of total discharges for the same time periods. In-person care had a hospitalization rate of 16.5% of all discharges. Virtual care had a hospitalization rate of 8.9% of all discharges (Figure 3 ). A chi-square test was performed to examine these data. The relationship between virtual care provided and hospitalization rate was significant, X 2 (1, N = 578) = 5.0896, p = 0.0241. Virtual PHP resulted in decreased hospitalizations to inpatient psychiatry.
Figure 3.
This bar graph compares in-person and virtual psychiatric hospitalization rate by month.
We further evaluated the hospitalization rates as they compared with the hospital's behavioral health emergency department volume to account for any hesitancy within the population to seek inpatient admission resulting from the pandemic. For the same time periods as above, the behavioral health emergency department had a 22.96% reduction in volume as compared with PHP having a 50.0% reduction in hospitalized patients (Figure 4 ). Prior to providing virtual care, PHP hospitalizations accounted for 0.87% of all emergency department visits. After providing care virtually, PHP hospitalizations accounted for 0.56% of all emergency department visits.
Figure 4.
This graph compares PHP (partial hospitalization program) hospitalizations with behavioral health (BH) emergency department (ED) volume over time.
This suggests the reduction in hospitalizations was not explained by patients avoiding emergency departments or inpatient hospitalizations.
Satisfaction Survey Results
Another area of study was the patient's perception of the care provided. Prior to providing virtual care, the program used the Press Ganey13 patient experience survey for behavioral health to collect patient satisfaction data. This survey was provided to patients as a hard copy and returned to Press Ganey for calculation of the aggregate data. Providing hard-copy surveys to patients amid the pandemic proved to be a significant barrier. As a result, the team developed an electronic survey targeting specific areas of interest related to patient perception of care in the virtual environment. We surveyed our patients at time of discharge to assess their satisfaction with the virtual care provided by eliciting responses to the following four items on a Likert scale: (1) “Since beginning this program I feel my condition is improving”; (2) “Staff worked together to care for you”; (3) “I feel included in my treatment decisions”; and (4) “Would you recommend this program to someone who is in need of treatment?” (See Appendix 1.)
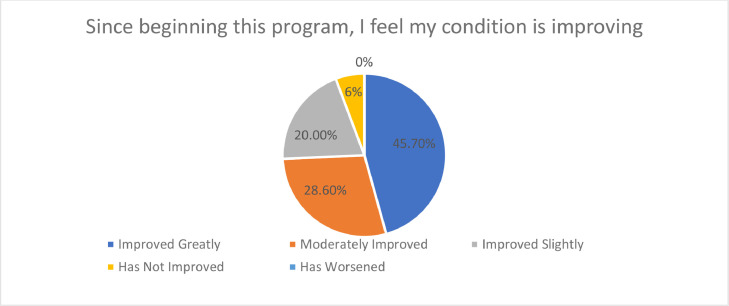
First, we wanted to learn if the patients felt their condition had improved. Of the 35 patients who returned survey responses, 74.3% reported that they felt their condition has moderately or greatly improved (Figure 5 ). No survey respondents reported their condition had worsened.
Figure 5.
This pie chart shows responses to the patient satisfaction survey item “I feel my condition is improving.”
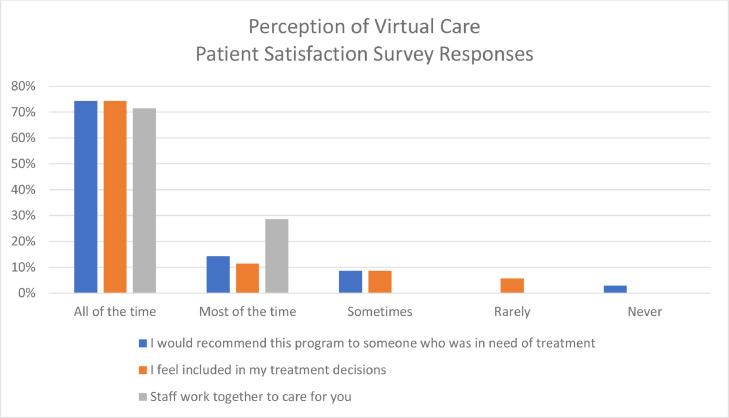
We also evaluated the patients’ perception of staff's ability to work together to provide care in a virtual environment. All 35 patients who completed the survey reported staff worked together all or most of the time; 58.7% of patients felt included in their treatment decisions all or most of the time. Further, 88.6% of survey respondents stated they would recommend the virtual PHP to someone in need of treatment all or most of the time (Figure 6 ).
Figure 6.
This bar graph shows responses to the patient satisfaction survey item measuring perception of virtual care.
This clearly indicates that the majority of patients who responded to the survey were satisfied with their care in the virtual program.
Discussion
This study demonstrates that the provision of PHP services via telehealth produces positive clinical outcomes and high patient satisfaction. Furthermore, there was no interruption in service delivery at a time of high demand given psychosocial stressors pertaining to the COVID-19 pandemic. The overall program census was relatively unaffected by the transition to virtual care, and the overall utilization of the program increased as a result. The CGI scores of patients receiving virtual care were observed to be on par with the scores of those who had received care in person. The aggregate findings of this standardized outcome measure tool indicate no negative effects resulting from virtual care. Further, psychiatric hospitalizations decreased significantly when services were provided in a telehealth treatment environment. Last, patients in the PHP reported satisfaction with the care they received virtually across a variety survey items.
Limitations
This study has some limitations. First, the study was conducted during the COVID-19 pandemic, during a time of unprecedented societal behavioral changes, including a preference for social distancing, which may have increased willingness of individuals to engage in telehealth and influenced their satisfaction with this modality. Furthermore, the COVID-19 pandemic may have affected patient attendance rates, as access to many leisure and entertainment options in the community were restricted, reducing the likelihood patients would choose to miss the program to engage in other types of activities. In addition, patient satisfaction during the study could not be directly compared to satisfaction scores for in-person care, as the survey tool was changed to meet the need for electronic surveying. Furthermore, the additional support calls added to the program structure that provided assistance to those struggling as a result of the pandemic may have contributed to the positive outcomes observed in the study. Last, demographic and socioeconomic data were not collected and analyzed as a potential factor related to challenges accessing and using technology
Conclusion
The evidence supports the ongoing use of telehealth for a PHP level of care. By providing care virtually, the PHP has been able to prevent psychiatric hospitalizations and support patients in achieving symptom stability equivalent to—and in some cases superior to—services provided in person. This is consistent with previous research focusing on telepsychiatry more broadly.14 Clinical outcomes and patient engagement are clearly not barriers to providing PHP level of care in a virtual setting. Providing PHP services virtually allows programs to expand the services offered to patients who may not otherwise be able to receive this level of care. Distance, access to transportation, and cost of transportation are no longer obstacles to participate in treatment. This, coupled with increasingly strong evidence that telehealth is an effective mode of treatment,15 suggests that virtual care for PHP level of service should be continued after the risk of COVID-19 infection is diminished.
Acknowledgments
Conflicts of Interest
All authors report no conflicts of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jcjq.2022.04.007.
Appendix. Supplementary materials
References
- 1.Westlaw. New York Codes, Rules and Regulations. Part 587.12: Partial Hospitalization Programs. Feb 15, 2021. Accessed May 13, 2022. https://govt.westlaw.com/nycrr/Document/I503782c9cd1711dda432a117e6e0f345?viewType=FullText&originationContext=documenttoc&transitionType=CategoryPageItem&contextData=%28sc.Default%29.
- 2.Horvitz-Lennon M, et al. Partial versus full hospitalization for adults in psychiatric distress: a systematic review of the published literature (1957–1997) Am J Psychiatry. 2001;158:676–685. doi: 10.1176/appi.ajp.158.5.676. [DOI] [PubMed] [Google Scholar]
- 3.Granello DH, Granello PF, Lee F. Measuring treatment outcomes and client satisfaction in a partial hospitalization program. J Behav Health Serv Res. 1999;26:50–63. doi: 10.1007/BF02287794. [DOI] [PubMed] [Google Scholar]
- 4.Thompson CN, et al. COVID-19 Outbreak—New York City, February 29–June 1, 2020. MMWR Morb Mortal Wkly Rep. 2020 Nov 20;69:1725–1729. doi: 10.15585/mmwr.mm6946a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.New York State Office of Mental Health, Bureau of Inspection and Certification. Clinic Standards of Care Anchor Element. May 2021. Accessed May 13, 2022. https://omh.ny.gov/omhweb/clinic_restructuring/docs/standards-of-care-anchor-tool-clinic.pdf.
- 6.US Congress. Health Insurance Portability and Accountability Act of 1996. Public Law 104–191. Accessed May 13, 2022. https://www.congress.gov/104/plaws/publ191/PLAW-104publ191.pdf.
- 7.Kaiser Family Foundation. The Implications of COVID-19 for Mental Health and Substance Use. Panchal N, et al. Feb 10, 2021. Accessed May 13, 2022. https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/.
- 8.Sparr LF, Moffitt MC, Ward MF. Missed psychiatric appointments: who returns and who stays away. Am J Psychiatry. 1993;150:801–805. doi: 10.1176/ajp.150.5.801. [DOI] [PubMed] [Google Scholar]
- 9.New York State Office of Mental Health. Medicaid Reimbursement Rates. (Updated: May 9, 2022.) Accessed May 13, 2022. https://omh.ny.gov/omhweb/medicaid_reimbursement/.
- 10.Busner J, Targum SD. The Clinical Global Impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont) 2007;4(7):28–37. [PMC free article] [PubMed] [Google Scholar]
- 11.Kaiser Family Foundation. Trends in Overall and Non-COVID-19 Hospital Admissions. Schwartz KS, Heist T. Feb 18, 2021. Accessed May 13, 2022. https://www.kff.org/health-costs/issue-brief/trends-in-overall-and-non-covid-19-hospital-admissions/.
- 12.Childs AW, et al. Showing up is half the battle: the impact of telehealth on psychiatric appointment attendance for hospital-based intensive outpatient services during COVID-19. Telemed J E Health. 2021;27:835–842. doi: 10.1089/tmj.2021.0028. [DOI] [PubMed] [Google Scholar]
- 13.Press Ganey. Patient Experience [survey portal]. Accessed May 13, 2022. https://www.pressganey.com/products/patient-experience.
- 14.Hubley S, et al. Review of key telepsychiatry outcomes. World J Psychiatry. 2016 Jun 22;6:269–282. doi: 10.5498/wjp.v6.i2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guinart D, et al. Mental health care providers’ attitudes toward telepsychiatry: a systemwide, multisite survey during the COVID-19 pandemic. Psychiatr Serv. 2021;72:704–707. doi: 10.1176/appi.ps.202000441. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.