Recently, with the SARS-CoV-2 vaccination campaign progress, evidence of possible alteration of blood pressure (BP) associated with vaccination has increased [1]. BP changes occurred in two directions, as shown by evidence of hyper- and hypotensive episodes, which lead many authors to monitor and report the most striking cases they have treated [2], [3], [4], [5].
Since during the vaccination period we revealed a general increase of requests for a BP control and consequent changes in therapy following vaccine administration, we designed a dedicated survey to monitor this phenomenon and address it to internal healthcare workers only. This choice was considered the most appropriate due to two reasons: from one side the level of health literacy was more homogeneous among healthcare workers, which is fundamental in controlling individual heterogeneity in answers provided by self-administrated questionnaires. Second, we could have rapid access to a population with very homogenous vaccination periods, independently by age, gender, and other factors that in the general population are used to stratify different vaccination administration time. Moreover, this enhances the usefulness of these results for future studies, where crossing survey results with more clinical individual information may be possible due to the existence of internal biobank, that include clinical data on institutional workers.
RESULTS: A total of 1870 subjects (69% female, 31% male) answered the questionnaire. 1866 subjects underwent the anti-SARS-CoV-2 vaccination course (mostly with Comirnaty® Pfizer (93% 1st dose, 94% 2nd dose, and 75% for the booster dose; Spikevax® Moderna was only significantly used for 23% of booster doses)
Only 16% of the subjects declared a previous diagnosis of hypertension and 32% of respondents reported a regular BB control (mostly 1/month).
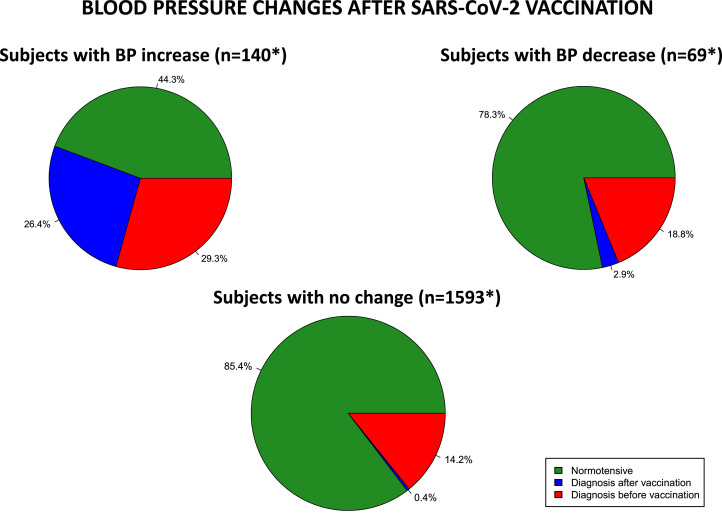
153 subjects (8%) reported an increase in BP values after vaccination and 70 subjects (4%) observed a decrease in blood pressure. BP alterations presented with greater frequency at the 2nd or booster dose. Associated symptoms were headache (39%), general malaise (34%), and dizziness (18%). Only in 39 subjects (2%), a conclamant diagnosis of hypertension was done after this discovery of BP alteration ( Fig. 1). Among the 281 subjects already on antihypertensive therapy, 13% declared a change in antihypertensive therapy (11% had to increase therapy, 2% reduced it).
Fig. 1.
Reported BP changes after mRNA SARS-CoV-2 vaccination according to known history of hypertension. ' = 64 patients omitted hypertension history. GREEN: No history of hypertension; RED: history of hypertension already known before vaccination; BLUE: new diagnosis of hypertension done after vaccination. BP= blood pressure.
From an epidemiological point of view, 36% had COVID-19 disease (50% before vaccination, 39% after the booster dose).
Although the theory of pandemic evolution is still under an ongoing debate, this data supports the recommendation of a high level of active surveillance on BP measurements after vaccination, especially if a further dose should be required in fragile patients.
These results show how up to 10% of the general population may have an alteration in blood pressure values after the completion of a vaccination course. So, our aim is to focus the attention of the operators, who are dealing with the daily treatment of BP disorders, on short-medium term the consequences that a new vaccination campaign could expose.
How mRNA vaccines could affect blood pressure is not known and there are many hypothesized mechanisms. The identification and discussion of such routes are beyond the aim of this letter; however, it would be very helpful in understanding the underlying pathways of the disease to monitor these BP changes over a longer period.
Declaration of Competing Interest
The authors declare they have no conflict of interest.
Acknowledgments
Hayden Carl Nortje (RSA) for English supervision. Members of the Multidisciplinary Epidemiological Research Team Study Group: Prof. Clelia Di Serio1, Dr. Matteo Moro2
1Vita-Salute San Raffaele University, Milan, Italy.
2Infection Control, Chief Medical Office, IRCCS San Raffaele Scientific Institute, Milan, Italy.
Contributor Information
Multidisciplinary Epidemiological Research Team Study Group:
References
- 1.Angeli F., Reboldi G., Trapasso M., Santilli G., Zappa M., Verdecchia P. Blood pressure increase following COVID-19 vaccination: a systematic overview and meta-analysis. J Cardiovasc Dev Dis. 2022;9:150. doi: 10.3390/jcdd9050150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zappa M., Verdecchia P., Spanevello A., Visca D., Angeli F. Blood pressure increase after Pfizer/BioNTech SARS-CoV-2 vaccine. Eur J Intern Med. 2021;90:111–113. doi: 10.1016/j.ejim.2021.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bouhanick B., Montastruc F., Tessier S., Brusq C., Bongard V., Senard J.M., Montastruc J.L., Herin F. Hypertension and Covid-19 vaccines: are there any differences between the different vaccines? A safety signal. Eur J Clin Pharmacol. 2021;77:1937–1938. doi: 10.1007/s00228-021-03197-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sanidas E., Anastasiou T., Papadopoulos D., Velliou M., Mantzourani M. Short term blood pressure alterations in recently COVID-19 vaccinated patients. Eur J Intern Med. 2022;96:115–116. doi: 10.1016/j.ejim.2021.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meylan S., Livio F., Foerster M., Genoud P.J., Marguet F., Wuerzner G., Center C.C.V. Stage III hypertension in patients after mRNA-based SARS-CoV-2 vaccination. Hypertension. 2021;77:e56–e57. doi: 10.1161/HYPERTENSIONAHA.121.17316. [DOI] [PMC free article] [PubMed] [Google Scholar]