Abstract
This paper reports the history, background including politics, current status of Japan’s health imaging study and other information sharing. Its realization was slow until the Ministry of Health, Labour and Welfare (MHLW) started paying digital image storage at the same rate as films in 2008. Information sharing was initiated in early 2010s, which was before vendors became ready for Integrating the Healthcare Enterprise (IHE) cross-enterprise document sharing (XDS), with the result that most of 34 large regional sharing systems are in non-standardized protocol. One standardized example is the Hamamatsu area where inexpensive online PDI (portable data for imaging) was introduced.
Keywords: Healthcare information sharing, COVID-19, DICOM, IHE, XDS, XDS-I, PDI, netPDI, SS-MIX
Background
Digitization of Medical Images in Japan
Japan initialized the digitization of healthcare information for images before it did for medical records. In 1994, the Ministry of Health and Welfare issued a notification titled “Storage of Radiographs and Other Images on Optical Disks and Other Media.” Until then, while medical institutions had been required to store actual films for imaging examination results, for the first time in Japan, this notification paved the way for the storage of digitized data.
In Europe and the USA in 1994, development had been conducted on the storage of image data formatted in the Digital Imaging and Communications in Medicine (DICOM), an international standard for medical images, and the development of systems that would ensure interoperability of image data [1]. In Japan, the DICOM standard for format and transmission was also adopted, and studies on digital storage of image data in the Picture Archiving and Communication System (PACS) and clinical application of this system were conducted [2].
In 1999, to allow digital storage of not only images but also medical records, the Ministry of Health and Welfare issued a notification titled “Storage of Medical Records and Other Data in Electronic Media.” In 2000, the Japanese government announced the “e-Japan” strategy [3]. In this strategy, the government recommended digitization in healthcare and implemented policies to promote the introduction of an electric medical record (EMR) system. After this strategy was implemented, PACS was gradually introduced in real-world clinical practice. However, the introduction of PACS required a large initial investment. Thus, only a limited number of hospitals were able to introduce PACS. In Japan, the government controls the costs of medical services under a nationwide fixed fee-for-service system [4]. Regardless of the implementation status of PACS, the same fees were charged for diagnostic imaging, due to which no incentive was provided for digitization. However, the 2008 revision of medical service fees included a “management fee for electronic imaging.” When this fee enabled hospitals to recover the costs of introducing the PACS as a part of patient care costs, the number of hospitals introducing PACS suddenly increased.
For medical image data, the modalities that generate images have already been standardized to allow the output of images formatted in DICOM. The DICOM format has generally been adopted for the data stored in PACS. The wide adoption of PACS, as well as the development and adoption of recording media such as compact disks (CDs) for storage of music and data, led to the demand for sharing image data among hospitals by using portable media (e.g., CDs). At that time, the proprietary viewer application of PACS vendors was activated from the CD to view DICOM-formatted images that were stored on the CD. In other words, various existing systems are not designed for sharing the image data themselves, and furthermore, each disk usually contained its own proprietary viewer, a significant user interface and “usability” challenge.
Meanwhile, the MHLW devised the “Ministry of Health, Labour and Welfare Standards” in 2010 [5], and it initiated standards for the first time to promote appropriate informatization in healthcare. These standards clearly indicate that medical image data should be stored and exchanged in the DICOM format. The standards also included portable data for imaging (PDI), which is a profile for sharing medical images stored in portable media between facilities [6]. This profile was defined by the Integrating the Healthcare Enterprise (IHE), an international project organization that develops a workflow to determine how to apply these standards in accordance with clinical practice. The use of PDI laid the groundwork for sharing image data in the DICOM format and a uniform format for the DICOM directory.
Regional Healthcare Information Exchange Networks in Japan
When patients are transferred between medical institutions with PDI, physicians at the referred hospital can treat the patients while viewing images captured at the referring hospital. Hence, repetition of the same imaging examinations is unnecessary. The use of PDI has conferred significant benefits to patients and hospitals. However, sharing image data in the PDI format requires the import of data from a recording media, such as CD or DVD, to a hospital PACS. Importing image data may take time depending on the size of the image files and the queue that develops for large referral centers. The time during which healthcare professionals wait for completion of this process has been regarded as a cost for the healthcare system [7].
Japan comprises many isolated islands that have only small- to medium-sized hospitals or clinics and many settlements in the mountainous areas that are isolated from cities in lowland areas. To ensure a healthcare system that provides continuity of healthcare after emergency and acute phases, medical and image data between smaller medical institutions and large-sized hospitals must be shared in a more timely manner. To meet this requirement, a system that connects medical institutions online and allows them to share healthcare information should be developed. In Nagasaki Prefecture, which consists of multiple isolated islands, the Nagasaki Medical Association and Nagasaki University Hospital have been developing an online interoperable platform for sharing patient information since 2004 [8].
In the 2016 revision of medical service fees [4], the MHLW created a new fee that allowed specialized and large-sized hospitals to charge a certain amount of additional fee to patients visiting without a referral. This new fee helped address problems associated with patients with mild health conditions who unnecessarily visited large-sized hospitals for initial treatment because of free access to medical institutions. Consequently, general outpatients began to visit small- to medium-sized hospitals or clinics [9]. Ultimately, patients were referred from small- to medium-sized hospitals and clinics to specialized and large-sized hospitals and vice versa. Thus, the need to share healthcare information, prescription orders, test results, and image data has increased among hospitals and clinics throughout Japan.
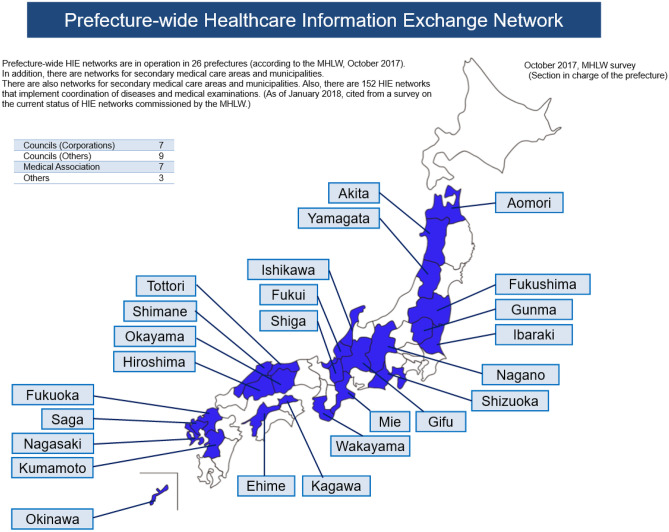
From the results of a survey conducted by the MHLW, prefecture-wide healthcare information exchange networks were established in 2017 in 26 prefectures, accounting for approximately half of all prefectures in Japan (Fig. 1) [10]. The distribution of these networks suggests possible increased need for online information exchange between medical institutions, mainly in rural regions where medical institutions are sparsely located, compared with the three metropolitan areas: Tokyo, Nagoya, and Osaka. The establishment of such a network is much more needed in prefectures in rural regions.
Fig. 1.
Distribution of areas with a Healthcare Information Exchange network for all prefectures (Ministry of Health, Labor and Welfare, October 2017) * English translation, partial modification of figure
MHLW introduced 34 regional healthcare information exchange networks, including the 26 networks on its special website [11]. We analyzed the data on the 34 networks that are available on this website, categorized the data into four categories (i.e., basic data, numeric data, exchange information, and system structure). Table 1 summarizes these data.
Table 1.
HIE networks (34) in MHLW website “Healthcare Information Exchange Network Support Navigation (Archive)”
| # | Basic data | Exchange information | System structure | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Name of HIE Network | Prefecture | Area | Since | EMR | Order | Study | Image | Dose | Server | Type | Protocol | + SSMIX | |
| 1 | Ajisai Net | Nagasaki | Pref | 2004 | ○ | ○ | ○ | ○ | Fa | Product | IDL, HB | ||
| 2 | Pika-Pika Link | Saga | Pref | 2010 | ○ | ○ | ○ | ○ | Fa + Cl | Product | IDL | ○ | |
| 3 | Azalea Net | Fukuoka | ? | 2012 | ○ | ○ | ○ | ○ | Fa | Product | IDL | ||
| 4 | Sado Himawari Net | Niigata | Oth | 2013 | ○ | ○ | ○ | ○ | Cl | SI | Original | ○ | |
| 5 | Hareyaka Net | Okayama | Pref | 2013 | ○ | ○ | ○ | ○ | ○ | Fa + Cl | Product | IDL, HB | ○ |
| 6 | Mame Net | Shimane | Pref | 2013 | ○ | ○ | ○ | ○ | ○ | Ce | SS-MIX | SS-MIX | ○ |
| 7 | Biwa lake Asagao Net | Shiga | Pref | 2014 | ○ | ○ | ○ | ○ | ○ | Fa | Product | IDL, HB | ○ |
| 8 | Yamashina Medical and Care Collaboration Network | Kyoto | ? | 2015 | ○ | ○ | ○ | Ce | Intl Std | IHE | ○ | ||
| 9 | Okinawa Shinryo Network | Okinawa | Pref | 2015 | ○ | ○ | ○ | ○ | Cl | SI | Original | ||
| 10 | To-Net | Saitama | Sec | 2012 | ○ | ○ | ○ | Cl | Product | IDL | ○ | ||
| 11 | HM Net | Hiroshima | Pref | 2013 | ○ | ○ | ○ | ○ | ○ | Fa | Intl Std | HL7 | ○ |
| 12 | Cyokai Net | Yamagata | Sec | 2012 | ○ | ○ | ○ | Ce | Product | IDL | |||
| 13 | Usuki Sekibutsu Net | Ooita | City | 2008 | ○ | ○ | ○ | ○ | Cl | Product | IDL | ||
| 14 | Ehime Medical Association HIE Network | Ehime | Pref | 2012 | ? | ? | ? | ? | ? | Ce | ? | ? | ? |
| 15 | Oshidori Net 3 | Tottori | Pref | 2009 | ○ | ○ | ○ | ○ | Cl | Intl Std | IHE | ○ | |
| 16 | Kiyosu Link | Wakayama | Pref | 2013 | ○ | ○ | ○ | ○ | ○ | Cl | SS-MIX | SS-MIX | ○ |
| 17 | Fuji-no-kuni Net | Shizuoka | Pref | 2011 | ○ | ○ | ○ | ○ | Fa + Cl | Product | HB | ○ | |
| 18 | Shinsyu Medical Net | Nagano | Pref | 2011 | ○ | ○ | ○ | ○ | Fa + Cl | Product | IDL, HB | ○ | |
| 19 | Ishikawa Medical Information Sharing Network | Ishikawa | Pref | 2014 | ○ | ○ | ○ | ○ | Fa | Product | IDL | ○ | |
| 20 | Tochimaru Net | Tochigi | Pref | 2013 | ○ | ○ | ○ | ○ | ○ | Cl | Product | IDL, HB | ○ |
| 21 | OKInet | Yamagata | Sec | 2011 | ○ | ○ | ○ | ○ | ○ | Fa + Ce | Product | IDL | |
| 22 | Mogami Net | Yamagata | Sec | 2013 | ○ | ○ | ○ | ○ | Ce | Product | IDL | ○ | |
| 23 | Benibana Net | Yamagata | Sec | 2014 | ○ | ○ | ○ | ○ | Fa | Product | IDL, HB | ||
| 24 | Akita Heartful Net | Akita | Pref | 2014 | ○ | ○ | ○ | Fa + Ce | Product | IDL, SI | |||
| 25 | Kumamoto Medical Network | Kumamoto | Pref | 2014 | ○ | ○ | ○ | ○ | ○ | Ce | Product | Original | ○ |
| 26 | Tobiume Net | Fukuoka | Pref | 2014 | ○ | ○ | ○ | ○ | Fa + Cl | Product | HB | ? | |
| 27 | K-MIX + | Kagawa | Pref | 2014 | ○ | ○ | ○ | ○ | ○ | Fa + Cl | Product | HB | ? |
| 28 | Mie Medical Safety Network | Mie | Pref | 2010 | ○ | ○ | ○ | ○ | ? | Product | IDL | ? | |
| 29 | Gifu Seiryu Net | Gifu | Pref | 2015 | ○ | ○ | ○ | ? | ? | ? | Product | IDL, HB | ? |
| 30 | Fukui Medical Net | Fukui | Pref | 2014 | ○ | ○ | ○ | ○ | ? | ? | Product | HB | ? |
| 31 | iSN: Ibaraki Safety Net | Ibaraki | Pref | 2015 | ○ | ? | ○ | ○ | ? | Ce | Product | Original | ? |
| 32 | Kibitan Health Net | Fukushima | Pref | 2015 | ○ | ? | ○ | ○ | ○ | ? | Product | IDL, HB | ? |
| 33 | MMWIN: Miyagi Net for everyone | Miyagi | Pref | 2013 | ○ | ○ | ○ | ○ | ○ | Ce | SS-MIX | SS-MIX | ○ |
| 34 | Aomori Medical Net | Aomori | Pref | 2015 | ○ | ○ | ○ | ○ | ? | Product | HB | ? | |
The data are as of the time of the MHLW survey and may not be current as of 2021.
For some of the HIE networks, there was almost no data other than the name and prefecture in the survey report.
Therefore, these were supplemented by manually collecting information from websites or other sources.
As for Yamagata, the entire prefecture is covered by four networks of secondary medical care areas on the list.
IDL ID Link proprietary HIE product of NEC Company, HB HumanBridge proprietary HIE product of Fujitsu Company, Original proprietary HIE protocol of Japanese vendor, SS-MIX Standardized Structured Medical Information eXchange, IHE Integrating the Healthcare Enterprise, SI System Integration, HL7 Health Level 7, Pref prefecture wide, Sec secondary medical area, City city wide, Oth other, Fa facility, Cl cloud, Ce data center
“?” is used to indicate that the information is unclear. A blank field means not applicable and is different from “?”.
As presented in Table 1, basic data and data in EMR are partially shared in all 34 networks, whereas image data and data on dispensed drugs are shared in 31 and 17 networks, respectively. The data-sharing systems used are proprietary products provided by major EMR vendors in 32 networks. Only two networks use the cross-enterprise document sharing (XDS), which is a profile developed by the IHE as a protocol for regional healthcare information exchange, and XDS for imaging (XDS-I), which is the image data version of XDS. In contrast, 17 networks concomitantly use standardized structured medical information exchange (SS-MIX) storage, which meets the MHLW Standards, as part of the information-sharing system. SS-MIX allows easy creation of a healthcare information archive for sharing healthcare information with other hospitals and backup of the data during disaster by using general operating system technology based on folder and file naming requirements [12]. In particular, many hospitals have introduced SS-MIX before introducing regional healthcare information exchange networks. It seems that this SS-MIX is used as a common interface for the proprietary products of the EMR vendors to suppress the introduction cost.
Methods
This paper is intended to report two regional information sharing; Fuji-no-kuni network as a non-standardized approach but common to find in Japan, versus Hamamatsu area netPDI as IHE PDI standardized method.
Results
Common Networks for Regional Healthcare Information Exchange
A typical example of the operational performance of a common regional healthcare information network in Japan, is that of data from the “Fuji-no-kuni Net,” one of Japan’s 34 networks that is operated throughout Shizuoka Prefecture. This network became operational in fiscal year 2011 and connects a total of 145 facilities, including 34 hospitals (i.e., 18 hospitals are showing and receiving data, and 16 hospitals only view data), 75 clinics (i.e., 1 clinic discloses data, and 74 clinics only request data), 30 pharmacies, 1 care facility, and 5 others, as of the end of June 2021 (Fuji-no-kuni Net Survey, June 2021). The number of registered patients was 2500 (MHLW survey, March 2020). The shared data included basic patient information, disease name, summary, operative notes, various test orders, laboratory test results, and images.
The information exchange system is built on the systems provided by major Japanese vendors developing and selling EMR products. The proprietary communication protocols of the vendors were used (Fig. 2). In order to interoperate in accordance with international standards, medical information is shared among facilities using data templates such as the IHE XDS profile. Conversely, this network uses a system in which healthcare information is disclosed by hospitals through a management system that is installed in the cloud servers managed by the vendors, and the information is requested by participating facilities when needed.
Fig. 2.
Fuji-no-kuni Net system configuration (from homepage) *English translation
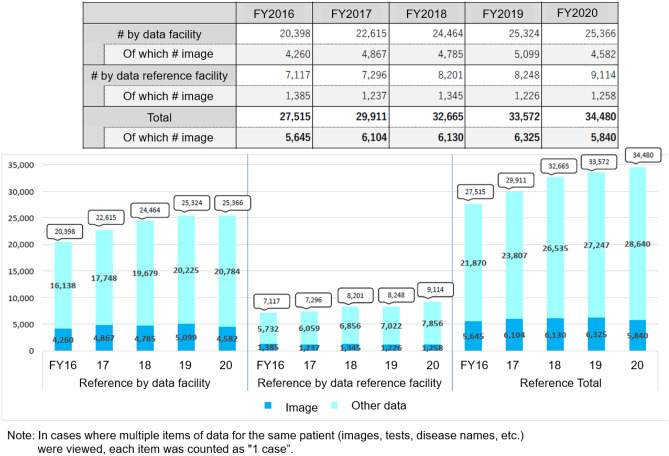
In the fiscal year 2020, the participating facilities requested 34,480 cases, including 5840 imaging studies (approximately 17%) (Fig. 3). In the past 5 years, the total number of requested cases increased by 25% from 27,515 cases in the fiscal year 2016. In contrast, the number of requested imaging studies increased slightly until the fiscal year 2019 (12% increase), compared with 5645 imaging studies in the fiscal year 2016. However, this number decreased by 8% in the fiscal year 2020, compared with the number in the previous fiscal year. In the Fuji-no-kuni Net, medical institutions, pharmacies, care facilities, and visiting nursing care providers participate. Given the current aging population of Japan, we can assume that the need to share information among these medical and welfare facilities will increase in Shizuoka Prefecture. In contrast, image data are often requested mainly by medical institutions. We surmise that the decrease in the number of requested imaging studies in the fiscal year 2020 indicated the decreased need of medical institutions for sharing information. In the fiscal year 2020, the number of patients visiting hospitals presumably decreased because the government imposed travel restrictions in a nationwide attempt to control novel coronavirus disease 2019 (COVID-19) [13].
Fig. 3.
Changes in the number of references between participating facilities of Fuji-no-kuni Net (FY2016–20)
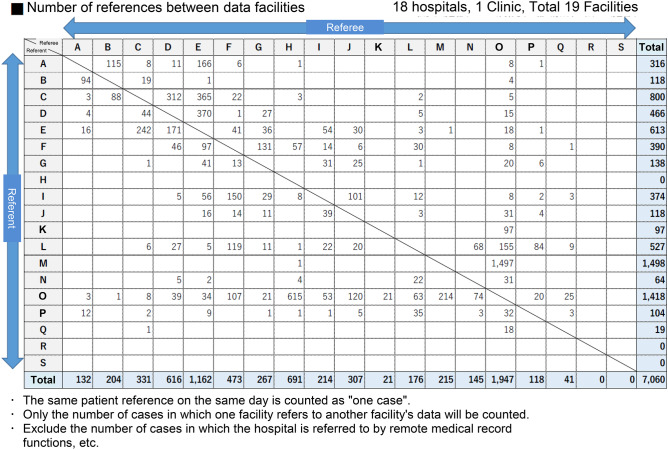
In addition, to demonstrate which hospitals were asked to disclose its patient data by each facility, we tabulated the volume of patient data requested from 19 facilities disclosing data in the fiscal year 2020 in a round-robin manner (Fig. 4). At facility O, which is a core hospital in Shizuoka Prefecture, the volume of data requested by other hospitals (1947 cases) and data disclosed to other hospitals (1418 cases) markedly exceeded the mean values. Among the data requested by other hospitals, 1497 cases were requested by facility M, accounting for approximately 77%. This indicates that facility M tends to accept patients receiving primary treatment at facility O. Figure 5 shows how individual facilities share their data. The rectangle with a letter represents a facility. The arrow indicates the direction of data-sharing. The number in a rectangle indicates the volume of shared data. The red arrow indicates the sharing of more than 100 cases. Except facilities R and S, which do not share any data, the associations among the other facilities largely overlap with their geographical positional relations in Shizuoka Prefecture. Facility O shares information with surrounding facilities and serves as the core hospital in the eastern region of the prefecture. In contrast, although a large volume of data (red arrows) is exchanged at facility E, it tends to exchange data more intensively with facilities A, C, and D in the surrounding area, unlike facility O. This seems to indicate that facility E serves as the core hospital in the western region of the Shizuoka Prefecture. In the future, such data may be useful for determining the distribution of hospitals according to their functions and strategically promoting the sharing of healthcare information among facilities in Shizuoka Prefecture.
Fig. 4.
Volume of data requested by facilities disclosing healthcare information (fiscal year 2020)
Fig. 5.
Reference trends and number of references among disclosure facilities (FY2020)
Interoperability of Medical Image Data in the IHE PDI and the New netPDI Method
Hamamatsu University Hospital founded a regional cooperation office in 2005 and has contributed to regional healthcare through hospital–hospital and hospital–clinic cooperation. To develop an information system that supports regional cooperation, the office has devised a system using the SS-MIX storage for regional healthcare information exchange and built an information-sharing network that meets Health Level 7 (HL7) V2.5, an international standard to ensure the interoperability of non-imaging healthcare information [12]. In addition, the IHE PDI profile, an international standard, is actively used to ensure the interoperability of medical image data. The office devised the netPDI protocol from the IHE PDI and XDS protocols, and the netPDI protocol is used to share image data online with two neighboring hospitals currently.
According to the original IHE PDI protocol, image data to be shared are saved in external media (e.g., CDs and digital versatile disks [DVDs]) at a hospital that captured the images, and patients bring the external media to referred hospitals that use the image data. This protocol is associated with the previously mentioned problems owing to the time required to import image data from external media to the PACS of referred hospitals, as well as security issues. Because patients, transport external media, (CDs and DVDs), the external media may be lost or damaged, which may result in loss of image data and consequently failure to share the data.
In contrast, in the netPDI protocol, image data are uploaded to a delivery storage server, rather than being saved in external storage media (Fig. 6). Patients receive “token” information that allows secure access to the delivery storage server, rather than physical storage media containing image data. At Hamamatsu University Hospital, considering the level of information technology literacy of patients, including the elderly, we provide them with paper on which the token information is printed. We also envision a future wherein token information will be shared as digital data through e-mails and other means on smartphones and other devices, for example QR codes. Patients bring and present this token information to the referred hospitals where the image data can be safely downloaded from the delivery storage server and imported to the systems of the referred hospitals. Even if patients lose the token information, regardless of whether they are printed on paper or stored in a smartphone, the image data themselves will not be leaked or lost unless the procedure to access the delivery storage server that only the referred hospitals know is exposed. The token information can be electronically recorded at hospitals that store images. Thus, even when loss of token information or other problems occur, the information can be delivered to the referred hospitals by passing the token by reprinting it on paper or sending it through e-mail or other means.
Fig. 6.
Operational procedures for netPDI using tokens
The netPDI was implemented according to the communication protocol used for the IHE XDS profile [6] (Fig. 7). The IHE Information Technology Infrastructure (ITI) 41 transaction (Provide & Register Document Set-b), which is developed in the ITI domain, is used when hospitals must upload image data to the delivery storage server. The token information that is transported to the referred hospitals by patients can substitute for the ITI-18 transaction (Registry Stored Query). It is pretend on paper as a barcode and the referred hospital can identified the token easily using barcode reader in Hamamatsu example. Because no referred hospital name is printed on paper, even if someone else picks up the paper which was lost by the patient, he/she cannot use it. When the referred hospitals download images from the delivery storage server, the ITI-43 transaction (Retrieve Document Set) is used. Because the IHE ITI transaction is used in the communication protocol, as described previously, netPDI is easier to implement with products equipped with communication functions that meet international standards than proprietary communication systems provided by EMR vendors. When hospitals transferring and receiving images are clearly known, netPDI may be a system that allows easy and secure sharing of data, because hospitals just ask for the patient’s data, as token shows that repository must have the patient’s data.
Fig. 7.
NetPDI implementation was based on application of IHE XDS transactions
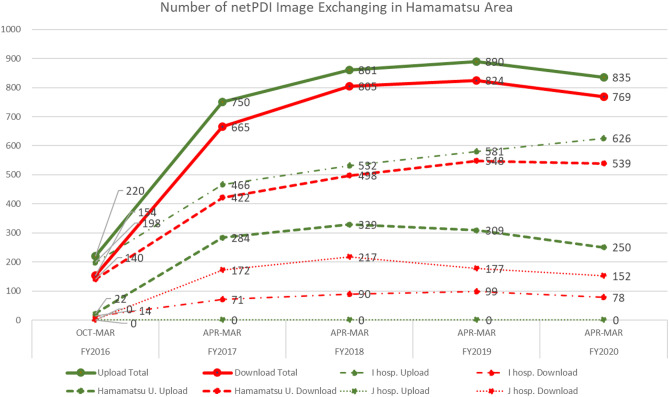
In October 2016, Hamamatsu University Hospital and two neighboring hospitals (i.e., facilities I and J) started sharing image data through the netPDI system. Tracking changes in the volume of shared data (fiscal year 2016–2020: Fig. 8), the total volume of uploaded and downloaded data increased until the fiscal year 2019, despite the differences in the types of data shared among the three hospitals. In the fiscal year 2020, the total volume of shared data decreased slightly. Because the volume of PDI data transferred and received by Hamamatsu University Hospital also decreased (Fig. 9), the total volume of shared image data is assumed to decrease as well. This suggests that patients tended to refrain from visiting hospitals because of the spread of COVID-19, as discussed in the Fuji-no-kuni Net [13].
Fig. 8.
Changes in the number of image exchange on netPDI by 3 hospitals in the Hamamatsu area (FY2016–20)
Fig. 9.
Number of image exchanging using the IHE PDI method at Hamamatsu University Hospital (CD creation/import)
For the exchange of image data among the three hospitals, the PDI system has been replaced with the netPDI system. In the fiscal year 2019, the volume of exchanged image data peaked at 890 uploaded cases and 824 downloaded cases, indicating a transition from the exchange of image data on CDs to online exchange. The volume of uploaded and downloaded data differed by 66 cases, which suggests that some patients did not visit the referred hospitals for some reason.
Hamamatsu University Hospital used the IHE PDI system to share healthcare information and image data stored on CDs before 2016, when netPDI was introduced. Currently, the IHE PDI system is still used to exchange image data with hospitals, in addition to the two hospitals participating in the netPDI-based network. At Hamamatsu University Hospital from the fiscal year 2017 to 2020, the total number of exported (output) and imported (input) CDs prepared in the PDI format changed in an almost similar manner to the volume of uploaded (output) and downloaded (input) netPDI data (Table 2). When we calculated the ratios of the exchanged netPDI data to the total volume of the exchanged PDI and netPDI data for input and output in each fiscal year, the differences in the ratios of the exchanged netPDI data throughout the period were 1.1% (1) (minimum 6.5% (2) to maximum 7.6% (3)) for output and 1.3% (4) (minimum 9.9% (5) to maximum 11.1% (6)) for input. These values also suggest similar changes observed in the PDI and netPDI data. The average ratio of the exchanged netPDI data for output was 10.4% (7). When more facilities replace the PDI system with the netPDI system and reduce the time required for importing data from CDs in the future, data are expected to be more efficiently exchanged online.
Table 2.
Comparison of the number of image exchanges between PDI and netPDI method at Hamamatsu University Hospital
| Fiscal year (Apr to Mar) | PDI (number) | netPDI (number) | PDI—> net PDI (netPDI / PDI + netPDI) | |||
|---|---|---|---|---|---|---|
| Create CD | Import CD | Upload | Download | Output | Input | |
| 2017 | 2264 | 6062 | 284 | 422 | 11.1% | 6.5% |
| 2018 | 2739 | 6646 | 329 | 498 | 10.7% | 7.0% |
| 2019 | 2824 | 7076 | 309 | 548 | 9.9% | 7.2% |
| 2020 | 2258 | 6577 | 250 | 539 | 10.0% | 7.6% |
| 1172 | 2007 | 10.4% | 7.1% | |||
| Total | Average PDI—> netPDI | |||||
| (4) 1.3% | (1) 1.1% | |||||
| Range of max–min of output/input 2017–20 | ||||||
Discussion
We considered differences in the establishment of regional healthcare information exchange networks between Japan and other countries and future prospects of exchanging image data.
Table 1 indicates that 25 out of 26 regional healthcare information exchange networks in Japan are implemented on proprietary systems provided by EMR vendors or systems uniquely developed and built by system integrators. In other countries (e.g., the USA, Canada, and Austria), healthcare information networks are built on the basis of international standards, such as IHE, HL7, and DICOM [14].
This difference is assumed to be broadly attributable to four factors:
Adaptation to the Higher Requirements Specifications by Free Access System
The Japanese healthcare system is primarily characterized by “free access” to any medical institution [9]. Patients have the option to visit any type of hospital or clinic that they prefer. Thus, patients can visit different hospitals for each episode at their discretion, based on the symptoms they experience and information they collect. In this system, patients are always free to choose hospitals, and the flow of patients among hospitals is complex. The requirement specifications for the needs of hospitals to share information have originally tended to be complicated. Because EMR vendors have independently developed entire systems to meet these requirements, each vendor has developed a system that is easy for the vendor to provide.
Technological Maturity of EMR Vendors and an Oligopoly Situation with Regard to Introduction into Large Hospitals
In 2001, the MHLW released the “Grand Design for Informatization in the Healthcare Field” [15]. In this design, the government set a target to achieve implementation of EMRs at 60% of hospitals with 400 beds or more by 2006, and it provided hospitals as a support for the introduction of EMRs. Although this target was not achieved, EMRs had already been introduced and used in 38.8% of large-sized hospitals by 2008 (Survey of Medical Institutions: MHLW) [5]. The technical and business driving force for this promotion of EMRs is major EMR vendors, which appear to have had sufficient ability to independently develop a regional healthcare information exchange system at that time. According to a survey conducted by a Japanese EMR vendor (fiscal year 2015), the operating hospital-use EMRs of four Japanese vendors accounted for 76% of all operating EMRs. In particular, the EMR market is an oligopoly. In this circumstance, EMR products from the same vendor are often used at multiple hospitals in a region. Thus, regional networks were relatively easy to build on the proprietary system of vendors.
Establishment of a Regional Healthcare Information Exchange Network and Preparation of Standard Procedures
With regard to the timing of the establishment of regional healthcare information exchange networks in Japan, 33 out of the 34 networks posted on the website of the MHLW, excluding the network in Nagasaki Prefecture, became operational between 2008 and 2015. This was partially attributed to the relative ease of receiving financial aid from the government because such networks were considered to serve the public interest. However, because protocols based on IHE (e.g., XDS and cross-community access [XCA]) were added to the MHLW Standards in 2016 [5], the demand for the establishment of the network appears to have peaked before this addition. Because the Japan IHE Association recorded the implementation of the XDS and XDS-I in 2006 in the results from the Connectathon, EMR vendors should already know the presence of international standard procedures. However, they had already established their own proprietary networking technology. Because adaptation to international standards would impose additional costs, vendors seem to have actively promoted the introduction of their own technology.
Unique Evolution into a Multivendor of the Information-Exchange Portal and Others
In 2018, the “Hareyaka Net,” the prefecture-wide healthcare information exchange network in Okayama Prefecture, reported the development of a portal server for transparent requests for information stored in EMR products from different vendors. This server allows local small- to medium-sized hospitals and clinics to request healthcare information stored in hospitals that had introduced EMRs from various vendors [16]. Previously, developing a new regional healthcare information exchange network from scratch had been attempted after securing project funds from the Ministry of Internal Affairs and Communications and the MHLW. Currently, regional healthcare information exchange networks are commonly implemented by expanding already established regional healthcare networks, that is, the proprietary networks of EMR vendors.
For EMR vendors, maintaining a regional healthcare information exchange network with their proprietary systems is fundamentally and strategically beneficial with regard to the introduction and upgrading of EMR products in the region in the future. In contrast, networking technology that allows requests for data stored in products of different vendors has been developed, as indicated in the “Hareyaka Net.” It is unlikely that EMR vendors will voluntarily spend additional costs to replace already established regional healthcare information exchange networks with those meeting international standards, such as IHE XDS and XCA.
However, the prefecture-wide healthcare information exchange networks that are currently in development will eventually be developed into a nationwide network. As discussed previously, the MHLW Standards recommend the establishment of a healthcare information exchange network that meets international standards, such as IHE, HL7, and DICOM, as with other countries. In 2021, the government founded a new digital agency to implement a policy to accelerate digitization in Japan [17, 18]. The government may plan to develop current prefecture-wide healthcare information exchange networks into a nationwide network. Nevertheless, the necessity of information exchange with other countries must be considered when such a nationwide network is built. In addition, the implementation of international standards should be essential for establishing new networks between Japan and other countries.
In contrast, when image data are exchanged, the use of images formatted in DICOM is common. In terms of sharing information, importing image data from other facilities into PACS and using the data are not as complex as importing non-image data. In addition, for systems to share image data, the PDI system using CDs and other external media to exchange image data is still widely used by hospitals that do not participate in any regional healthcare information exchange networks in Japan. When the need for prompt online requests for image data increases in the future, the netPDI, which can be introduced more easily than a full-scale network using IHE XDS-I, may be a beneficial option. We expect that the promotion of information exchange networks based on netPDI using IHE ITI-based communication will allow easy implementation of international standards (e.g., IHE XDS-I and XCA-I) when the exchange of data meeting these international standards becomes necessary.
Conclusion
Japan initiated development of digital medical information exchange before international standards were stated. Health information sharing started development by MHLW subsidy, before IHE XDS. This resulted in Japan vendors’ proprietary protocol sharing system scattered in more than 200 networks. Some of them are well designed as they are really used daily, such as Fuji-no-kuni described here. However, naturally, no inter-community exchange between typical active 34 regions is realized.
Images themselves are, of course, standardized in DICOM. IHE PDI based exchange with ISO standardized token is a solution for inter-community and international sharing.
In either case, based on free access healthcare providing system in Japan, the fact that no policy headquarter exists, is another obstacle for interoperability.
Funding
This research is partially supported by the Ministry of Health Labour and Welfare grant-in-aid, Research on Application Promotion of Healthcare Information Database (20KC2007).
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Declarations
Conflict of Interest
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yasunari Shiokawa, Email: yasunari.shiokawa@medical.canon.
Noriko Mori, Email: noriko-mori@i.shizuoka-pho.jp.
Takaya Sakusabe, Email: scsb@fujita-hu.ac.jp.
Takeshi Imai, Email: ken@hcc.h.u-tokyo.ac.jp.
Hiroshi Watanabe, Email: hiroshiw@ncgg.go.jp.
Michio Kimura, Email: kimura@mi.hama-med.ac.jp.
References
- 1.Ratib O, Hoehn H, Girard C, Parisot C: PAPYRUS 3.0: DICOM-compatible file format. Med Infor (Lond). 19(2):171–8. 1994 [DOI] [PubMed]
- 2.Sakusabe T, Onogi Y, Kimura M, Ohe K, Sasaki Y: DICOM image server linked with hospital information system. The 16th Joint Conference on Medical Informatics (JAMI). 124–125, 1996
- 3.e-Japan Strategy. https://japan.kantei.go.jp/it/network/0122full_e.html. Accessed 2 July 2021
- 4.The Medical Service Fee System. https://japanhpn.org/en/section-7-2/. Accessed 2 July 2021
- 5.Promotion of computerization in the medical field (Japanese). https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/iryou/johoka/index.html. 2 July 2021
- 6.IHE IT Infrastructure Technical Framework. https://www.ihe.net/resources/technical_frameworks/#IT. Accessed 27 June 2021
- 7.Hagiwara H, Nemoto A, Inoue T. Burden on university hospitals of handling portable data for imaging (PDI) media. Appl Clin Inform. 2014;05(01):46–57. doi: 10.4338/ACI-2013-07-RA-0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matsumoto T, Honda M. The evaluation of the health information exchange with the number of usage and the introduction of outpatient to the hospitals at Nagasaki Japan. Stud Health Technol Inform. 2017;254:1373. [PubMed] [Google Scholar]
- 9.Japan’s Health Insurance System. http://japanhpn.org/en/section-3-1/. Accessed 2 July 2021
- 10.Prefecture-wide Healthcare Information Exchange Network (Japanese). https://www.mhlw.go.jp/content/10808000/000613012.pdf. Accessed 27 June 2021
- 11.Healthcare Information Exchange Network Support Navigation (Archive) home page (Japanese). https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/iryou/johoka/renkei-support.html. Accessed 2 July 2021
- 12.Kimura M, Nakayasu K, Ohshima Y, Fujita N, Nkashima N, Jozaki H, Numano T, Shimizu T, Shimomura M, Sasaki F, Fujiki T, Nakashima T, Toyoda K, Hoshi H, Sakusabe T, Naito Y, Kawaguchi K, Watanabe H, Tani S. SS-MIX - a ministry project to promote standardized healthcare information exchange. Methods Inf Med. 2011;50(02):131–139. doi: 10.3414/ME10-01-0015. [DOI] [PubMed] [Google Scholar]
- 13.[COVID-19] Declaration of a state of emergency in response to the novel coronavirus disease (April 7) https://japan.kantei.go.jp/ongoingtopics/_00018.html. Accessed 2 July 2021
- 14.Persons KR, Nagels J, Carr C, Mendelson DS, Primo HR, Fischer B, Doyle M: Interoperability and considerations for standards-based exchange of medical images: HIMSS-SIIM Collaborative White Paper, J Digit Imaging, Feb;33(1):6–16, 2020 [DOI] [PMC free article] [PubMed]
- 15.Grand design for computerization in the medical field (Japanese). https://www.mhlw.go.jp/shingi/0112/s1226-1a.html. Accessed 2 July 2021
- 16.Challenges and responses to the national health and medical information network and health record sharing service (Japanese). https://www.mhlw.go.jp/content/12601000/000342743.pdf. Accessed 27 June 2021
- 17.Speeches and statements by the Prime Minister. https://japan.kantei.go.jp/99_suga/statement/202106/_00008.html. Accessed 2 July 2021
- 18.Digital Agency. https://www.digital.go.jp/en. Accessed 13 March 2022
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.