Summary
Background
The elbow joint is sensitive to trauma from accidents, sports injuries, and surgical trauma. Some patients develop ossification or contracture of the medial collateral ligament (MCL) after elbow trauma. A less invasive reconstruction of the MCL can be performed after resection of diseased MCL. The biomechanical characteristics of this technique have been demonstrated and validated. However, its clinical effectiveness and safety require further confirmation in clinical practice.
Methods
This open-label, non-randomised, prospective, multicentre trial included consecutive patients with elbow stiffness from five orthopaedic centres in China. Patients willing to participate in the study, with elbow stiffness caused by traumatic injury, who had reached skeletal maturity, and who had a range of motion of <100° were eligible for inclusion. Patients with immunological or metabolic causes of elbow stiffness, burns, or central nervous system injuries were excluded. In addition, patients who did not require MCL release and reconstruction after intraoperative release of other structures were also excluded. All patients underwent resection of the diseased MCL part in an open arthrolysis. Medial stability of the elbow was reconstructed using a less invasive MCL reconstruction technique that uses fascia and tendon patches. In this study, the primary outcomes, including stability, Mayo Elbow Performance Score (MEPS), Amadio score, were used to comprehensively evaluate this technique. Outcomes were assessed at 6 weeks, 6 months, and 1 year postoperatively and annually thereafter. This study reports the results of one arm of the trial that has been registered with the Chinese Clinical Trial Registry (chictr.org.cn), ChiCTR-INC-16010019.
Findings
Between January 1, 2017 and March 1, 2020, 104 eligible patients were enrolled. The mean follow-up time was 43·47 (95% CI, 41·45 - 45·49) months. Among all 104 patients, 100 (96%) patients who underwent MCL reconstruction retained medial stability at the last follow-up. All outcomes from the last follow-up were used for comparison with the preoperative outcomes. No differences in preoperative and postoperative stability scores were observed (P = 0·7820). Extension, flexion, pronation, and supination of the injured elbow improved significantly (P < 0·0001, P < 0·0001, P < 0·0001, P < 0·0001). The mean range of motion (ROM) and forearm rotational range of motion (FRR) increased by 71·25° (152%) (P < 0·0001) and 30·83° (25%) (P < 0·0001), respectively. Additionally, the Mayo Elbow Performance Score (MEPS) and muscle strength had increased after evaluation at follow-ups (P < 0·0001, P < 0·0001). Drastic pain relief and nerve symptom reduction were observed, as evaluated using VAS scores and Amadio scores, respectively (P < 0·0001, P < 0·0001). Seventeen (16%) patients experienced a recurrence of elbow stiffness of varying severity, but only two patients had poor or fair results. Several common and non-severe complications, including infection in one (1%) patient, new nerve symptoms in seven (7%) patients, new pain in one (1%) patient, fracture in one (1%) patient, and valgus instability in four (4%) patients, were observed and properly treated in this study.
Interpretation
The less invasive MCL reconstruction technique using fascia and tendon patches is an effective method for restoring medial stability in patients with elbow stiffness after complete arthrolysis with certain safety. The technique shows prospects for elbow MCL reconstruction in clinical practice.
Funding
The study was supported by the National Key Research and Development Program of China (No. 2021YFC2400805), National Natural Science Foundation of China (No. 81830076), Young Elite Scientist Sponsorship Program by Cast (No. YESS20200153), Shanghai Sailing Program (No. 20YF1436000), Shanghai Municipal Science and Technology Commission Foundation (No.19ZR1439200), Municipal Hospital Newly-developing Cutting-edge Technologies Joint Research Program of Shanghai Shenkang Hospital Development Centre (No. SHDC12018130).
Keywords: Elbow stiffness, Valgus stability, Medial collateral ligament reconstruction, Fascia and tendon patches, Multicentre study
Research in context.
Evidence before this study
It is generally accepted that the elbow joint is sensitive to trauma. Currently, most medial collateral ligament (MCL) reconstruction techniques focus on reconstructing injured ligaments in athletes, while ligament reconstruction techniques for elbow stiffness patients who are more sensitive to trauma are rarely reported. We searched PubMed and Wanfang databases for studies on ligament reconstruction in patients with elbow stiffness. Apart from reports of suture anchors repairs and case reports of fascial reconstruction presented by our team for patients with elbow stiffness, there is only one case report of ligament reconstruction for patients with elbow stiffness. We focus on the treatment of elbow stiffness and propose a new less-invasive reconstruction technique for MCL that has been biomechanically validated. The clinical value and effectiveness of the new MCL reconstruction technique are not yet known.
Added value of this study
This study aimed to evaluate the clinical effectiveness and safety of the less-invasive technique. The results of this open-label, non-randomised, prospective, multicentre trial suggest that the new MCL technique using fascia and tendon patches can effectively rebuild medial stability in patients with elbow stiffness after complete arthrolysis. This study provided a valuable guide to ligament reconstruction in patients with elbow stiffness.
Implications of all the available evidence
The MCL reconstruction using suture anchors and soft tissue around the elbow helps to reduce damage to the elbow bone and avoids complications in other graft donor areas, reducing the recurrence of elbow stiffness caused by excessive surgical trauma. In addition, the new technique has the potential to guide ligament reconstruction in the general patient population.
Alt-text: Unlabelled box
Introduction
The elbow can develop various complications, such as pain, soft tissue contracture or ossification, nerve symptoms, and periarticular heterotopic ossification (HO), after trauma.1, 2, 3, 4, 5 Moreover, HO mostly occurs on the medial side of the elbow,3 causing contracture or ossification of medial soft tissues, including ligaments.6,7 These complications tend to restrict movement of the elbow. A 50° restriction of elbow motion in flexion-extension can result in an 80% loss of elbow function.8 Elbow stiffness limits most daily activities requiring a range of 30° - 130° in flexion-extension and 50° - 50° in pronation-supination.8
Open arthrolysis is an effective treatment for elbow stiffness and can significantly improve the mobility and function of the elbow.1,9, 10, 11, 12 To achieve optimal range of motion, the elbow release procedures involve removal of HO and release of contracted subcutaneous tissue, joint capsule, tendons, and ligaments. Previous studies encouraged the preservation of the anterior bundle of the medial collateral ligament (AMCL) because it is the primary structure for maintaining valgus stability.9,13 Additionally, the posterior bundle of the MCL (PMCL) plays a vital role in preventing elbow dislocation or subluxation and posteromedial rotational instability.14,15 However, the contracted or ossified AMCL and PMCL need to be released or excised to eliminate mobility restrictions in some patients.16,17 Therefore, maintaining elbow stability becomes challenging after releasing or removing the diseased ligaments.
Traditional ligamentous reconstructive techniques can provide excellent stability. However, they expose the elbow joint to further surgical trauma because these techniques disrupt the double layer of bone cortex when creating bone tunnels.18,19 Additionally, the elbow joint is sensitive to surgical trauma, which may facilitate the progression of elbow stiffness.20 Considering the greater sensitivity of the elbow to trauma and the critical roles of AMCL and PMCL, we propose a minimally invasive anatomical reconstruction technique that has been proven to be effective by biomechanical evaluation.21 Therefore, this study sought to investigate the clinical effectiveness and safety of the new technique to restore medial stability in patients with elbow stiffness. This study hypothesised that the new MCL reconstruction technique could effectively maintain medial stability in patients with elbow stiffness after an adequate release procedure.
Methods
Study design
This study was an open-label, non-randomised, prospective, multicentre trial of patients with elbow stiffness at five centres in China, three centres in Shanghai, one centre in Wenzhou, and one centre in Guangzhou. This study is one intervention subgroup of a trial of the establishment of a systemic elbow dysfunction treatment system. The entire treatment system consists of seven subgroups. We are reporting the results of this intervention group early because the treatment system for this subgroup has been completed and it does not affect the data collection and research for the other subgroups. The institutional review board of Shanghai Sixth People's Hospital approved the study. Shanghai Fengxian District Central Hospital, the Second Affiliated Hospital of Guangzhou Medical University, the Second Affiliated Hospital of Wenzhou Medical University, and Shanghai Tenth People's Hospital waived the need for ethics approval after quality assessment and recognition of the ethics approval granted by the institutional review board of Shanghai Sixth People's Hospital.
Participants
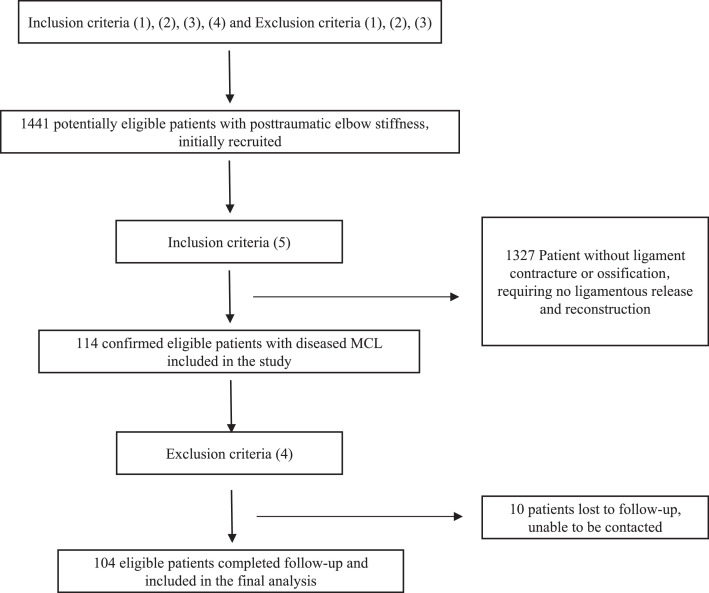
Patients with various types of elbow stiffness were consecutively seen at five centres from January 1, 2017 to March 1, 2020. Inclusion criteria were (1) willingness to participate in the study, (2) traumatic causes (i.e. traumatic factors that contribute to elbow stiffness, including fracture, dislocation, injury, and inappropriate surgical trauma), (3) skeletal maturity (considered to be generally at 18 years of age according to the Chinese standard for bone age, which was incorporated into the industry standard of the People's Republic of China [TY/T 3001-2006] in 200622), (4) ROM (i.e. elbow flexion and extension mobility) <100°(an extension-flexion arc of 100° [between 30° and 130°] is required for a relatively normal life8), and (5) MCL needing to be completely released and reconstructed during preoperative or intraoperative evaluation. In patients with post-traumatic elbow stiffness, some patients have ossification of the MCL, which can severely affect elbow mobility. The ossified ligament can be identified during preoperative imaging evaluation and needs to be completely released and reconstructed using a new MCL technique. Therefore, these anatomy-related patients can be included directly and do not need to be excluded intraoperatively. However, in some patients with post-traumatic elbow stiffness, they have developed a severe contracture of the MCL, which can also severely affect elbow mobility. A contracted MCL cannot be detected by preoperative imaging and requires further intraoperative evaluation of the MCL after release of other structures is completed. If the MCL contracture severely affects mobility, the contracted MCL will need to be released and then reconstructed, and these function-related patients will need to be formally included after intraoperative determination. If the MCL does not affect mobility after other structures have been released, these patients with elbow stiffness do not require ligament reconstruction and need to be excluded intraoperatively. Thus, the intraoperative criteria are that the contracted MCL affects joint mobility and needs to be completely released and reconstructed, and these patients need to be formally included. Those patients whose MCL does not affect joint mobility need to be excluded. Exclusion criteria were (1) immunological (e.g. rheumatoid arthritis or spondylitis) or metabolic conditions (e.g. osteoporosis, osteochondrosis, renal osteopathy, and Charcot arthropathy) that cause damage to bone structure, (2) elbow stiffness in patients with extensive scarring or contracture of soft tissues caused by burns, (3) central nervous system injuries (e.g. cranial trauma or cerebral haemorrhage), and (4) loss to follow-up. We prespecified a sample size of 50 for the ligament trial arm, and we estimated that 1400 patients were required to adequately meet the sample size for the entire trial according to protocol (number 2016-014). Initially, 1441 patients with posttraumatic elbow stiffness were recruited according to partial inclusion and exclusion criteria. After further preoperative or intraoperative evaluation, 114 patients had contracted or ossified MCL, which required complete release and reconstruction. These 114 patients underwent routine follow-up at 6 weeks, 6 months, 1 year postoperatively, and annually thereafter. Ten patients could not be contacted at final follow-up, and these patients were missing completely at random. The 8.77% (10/114) loss to follow-up rate in our study was below the 10% criterion which did not affect the statistical outcome of patients with orthopaedic trauma.23 Therefore, we excluded these 10 patients lost to follow-up and restricted analyses to participants with full outcome information (complete case analysis), which is a valid method when data are missing at complete randomization.24 Finally, 104 eligible patients were included in the primary analysis (Figure 1).
Figure 1.
Trial profile.
Inclusion criteria were (1) willingness to participate in the study, (2) traumatic causes, (3) skeletal maturity, (4) ROM <100°, and (5) MCL needing to be completely released and reconstructed during preoperative or intraoperative evaluation. Exclusion criteria were (1) immunological or metabolic causes, (2) burns, (3) central nervous system injuries, and (4) loss to follow-up.
All patients provided written informed consent. The trial was overseen by an institutional review board. The manuscript was written in accordance with the CONSORT recommendations.
Randomization and masking
This study is an open-label, non-randomised, prospective, multicentre trial. All eligible participants were informed about the use of the new ligament reconstruction technique for ligament reconstruction. Therefore, there is no randomization and masking method in this trial.
Procedures
Surgical techniques
Contraindications to surgery were ruled out preoperatively. All operations were performed by highly qualified surgeons from five centres with extensive experience in elbow release and rigorous training in new ligament reconstruction techniques. Sterile tourniquets were routinely used after brachial plexus anaesthesia or general anaesthesia. The choice of incision was based on previous surgical incisions. A combined medial and lateral incision or posterior median incision was most commonly used. Open arthrolysis of elbow stiffness was performed, as in previous studies.9,12,25,26
The lateral approach was used to expose contracted soft tissues and hyperplastic HO in the lateral and anterior aspects of the elbow. Contracture of the common extensor tendon of the elbow occasionally occurred, which required punctate release in some patients. Thick scar tissues formed after the previous surgeries were removed because they restricted elbow movement. Additionally, contracted capsules and hyperplastic HO in the anterior aspect of the elbow had to be removed. Along with the removal of the HO, some patients required coronal fossa and coronal osteoplasty. The annular ligament (AL) and radial collateral ligament (RCL) had to be released in some patients with rotational dysfunction. The lateral ulnar collateral ligament (LUCL) needs to be protected because it is an important structure for lateral stability.27 The LUCL was not found to impede movement in our study. Additionally, the radial nerve was released in some patients with severe restriction of movement, long duration of stiffness, or previous radial nerve symptoms.
The medial approach was used to expose the ulnar nerve, contracted tissue, and HO in the medial and posterior aspects of the elbow. Ulnar nerve release and anteriorization were performed in all patients. Additionally, the medial scar tissue was removed. The PMCL had to be excised to expose the posterior aspect of the elbow. However, the AMCL required preservation unless ossification had occurred. Thereafter, contracted capsules and HO in the posterior aspect of the elbow were removed. After HO excision, olecranon fossa and olecranon osteoplasty were performed in some patients to maximise extension improvement.
After routine surgical release, elbow flexion and extension movements were assessed again during the operation. We found that contracture of the triceps tendon occurred in some patients. Therefore, a pie-crusting technique for triceps tendon release was performed to improve flexion function.12 Additionally, we found that contracture or ossification of the AMCL occurred in some patients. The contracted or ossified AMCL had to be resected to maximise mobility. After a complete surgical release, the valgus instability of the elbow was identified during intraoperative evaluation in these patients. Therefore, these patients with valgus instability were finally included in the study, and MCL reconstructions were performed. Before MCL reconstruction, metal implants from previous surgeries were removed if the fracture had healed.
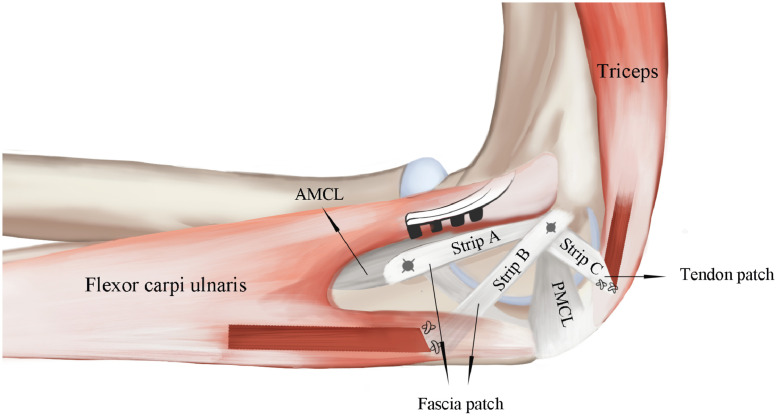
MCL reconstruction included AMCL reconstruction with the flexor carpi ulnaris fascia patch and PMCL reconstruction with the triceps tendon patch.21 The fascia patch was released from three sides of the muscle surface, retained on the proximal side 2 cm distal to the joint line, and fabricated to be 6 cm long, 1 cm wide, and 2 mm thick. The tendon patch was released from three sides with the distal end at the insertion and fabricated to be 3 cm long, 0·5 cm wide, and 2 mm thick. After preparing the patches, MCL reconstruction was performed at 90° of elbow flexion. The patches were sutured to their terminals using absorbable sutures to prevent further tearing. The fascia patch was folded along the long axis and pulled towards the medial condyle by passing underneath the flexor carpi ulnaris muscle to fit snugly over the bone surface. The patch was first fixed at the origin of the AMCL using a suture anchor (Twinfix; Smith & Nephew, Andover, MA, USA). Thereafter, the patch was reversed and tensioned toward the ulnar ridge. Finally, the patch was fixed at the centre of the ulnar attachments of the AMCL using a suture anchor. The triceps tendon patch was tensioned toward the medial epicondyle and fixed at the same point as the fascial patch. This new MCL reconstruction technique consisted of strips A, B, and C (Figure 2). Ensuring proper tension of the three strips was essential for a successful reconstruction. After MCL reconstruction, the remaining flexor carpi ulnaris fascia patch and common flexor tendons were intermittently sutured. The lateral collateral ligaments were repaired to their origins by a suture anchor. The two drainage tubes were placed anteriorly and posteriorly to the elbow to drain the hemorrhagic exudate adequately. Finally, hinged external fixation (Orthofix, Verona, Italy) was used to keep the elbow stability for soft tissue healing during the early rehabilitation phase.16
Figure 2.
Schematic diagram of the ligaments.
Schematic diagram shows position of reconstructed ligaments in relation to original ligaments. AMCL, the anterior bundle of the medial collateral ligament; PMCL, the posterior bundle of the medial collateral ligament.
Postoperative rehabilitation and treatment
Elbow rehabilitation exercises followed a uniform standard.9,28 Rehabilitation exercises started on the first postoperative day, and rehabilitation exercises were mainly passive exercises supplemented by active exercises. Thirty sets of rehabilitation exercises were conducted on the first postoperative day and then increased by 30 sets per day until 300 sets. Maximum flexion and extension were considered as one set, and the elbow could be locked at a maximum angle using the hinged external fixation until maximum tolerance. Concurrently, medications were used to promote swelling and pain relief. The hinged external fixation was removed at 6 weeks postoperatively. Meanwhile, the rotational function could be trained by performing 10 sets of passive pronation-supination exercises per day. All patients were encouraged to continue rehabilitation exercises along with muscle strength training. The duration of rehabilitation was determined by elbow function.
The elbow joint is prone to HO or HO recurrence after bone damage.1,2,29 Additionally, postoperative rehabilitation often accompanies pain. Therefore, celecoxib (Pfizer Pharmaceuticals LLC, Vega Baja, Puerto Rico; 200 mg orally, twice daily) was frequently used for analgesia and prevention of HO from postoperative day 1 to 6 weeks.30
Outcomes
Demographic data included age, sex, diseased side, body mass index (BMI), dominant side, and basic diseases. Clinical characteristics included duration of stiffness, follow-up time, preoperative nerve symptoms, moderate preoperative instability, type of original injury, mechanism of injury, and grading of stiffness severity (Table 1). Patients with elbow stiffness were classified using a stiffness grading scale (Table 2).31 The Mayo Elbow Performance Score (MEPS) was used to evaluate elbow mobility, pain, stability, and daily function.32 The visual analogue scale (VAS) score33 for quantifying elbow pain and Amadio score34 for describing nerve symptoms were recorded. Grip strength was used to evaluate the patient's upper extremity strength status. Among the evaluation indices mentioned above, stability, MEPS, and Amadio score were the primary index examined in this study. The other indices were used as auxiliary assessments of elbow joint function. The stability of the elbow joint was tested by using the modified milking manoeuvre and moving valgus stress tests. A modified milking test was performed by pulling the thumb to apply valgus stress at 70° of elbow flexion, which is the most unstable position of the elbow.35 The moving valgus stress test applied elbow valgus forces from maximum flexion to 30° flexion in the shoulder abduction and external rotation positions. It has a 100% sensitivity and 75% specificity for MCL injuries.36 Instability was defined as medial elbow pain or an increase in medial elbow opening during the valgus test. Valgus laxity ≤ 10° indicated moderate instability, whereas laxity > 10° indicated severe instability.32 All data were recorded by independent senior surgeons. Safety outcomes include adverse events and changes in muscle strength, stability and nerve symptoms.
Table 1.
Demographic and clinical characteristics of patients.
| Characteristic | Values or proportions |
|---|---|
| Number of patients (n) | 104 |
| Male (n) | 71 (68%) |
| Female (n) | 33(32%) |
| Age (years) | 34.60 ± 11.70 (18 - 68) |
| Diseased side (Right/Left) | 61/43 |
| Body mass index (kg/m2) | 23.01 ± 3.44 (16.26 – 32.41) |
| Dominant side (Right/Left) | 64/40 |
| Duration of elbow stiffness (months) | 29.65 ± 51.23 (6 - 324) |
| Follow-up time (months) | 43.47 ± 10.39 (26 - 62) |
| Preoperative pain (n) | 45 (43%) |
| Preoperative nerve symptoms (n) | 24 (23%) |
| Preoperative moderate instability (n) | 5 (5%) |
| Original injury types (n) | |
| Distal humerus fracture | 31 (30%) |
| Olecranon fracture | 14 (13%) |
| Radial head fracture | 10 (10%) |
| Elbow dislocation | 13 (13%) |
| Multiple fractures/injuries | 23 (22%) |
| Terrible triad | 11 (10%) |
| Monteggia fracture | 1 (1%) |
| Coronoid process fracture | 1 (1%) |
| Mechanism of injury (n) | |
| Low energy | 58 (56%) |
| High energy | 46 (44%) |
| Severity of stiffness | |
| Minimum or functional stiffness | 0 (0%) |
| Moderate stiffness | 30 (29%) |
| Severe stiffness | 43 (41%) |
| Very severe stiffness | 31 (30%) |
| Diabetes | 1 (1%) |
| Hypertension | 4(4%) |
Table 2.
Severity of elbow stiffness.
| Grade | Description |
|---|---|
| Minimum or functional stiffness | ≥91° |
| Moderate stiffness | 61° to 90° |
| Severe stiffness | 31° to 60° |
| Very severe stiffness | ≤30° |
Statistical analysis
This trial arm aimed to assess the efficacy and safety of a less-invasive ligament reconstruction technique, and the arm lacked a matched control group. Therefore, we doubled the prespecified sample size to reduce bias in practice. To our knowledge, there are no objective data on the efficacy of reconstructing medial stability in patients with elbow stiffness. Sample size will not be stipulated in advance for this study. Therefore, the sample size is not determined by power calculations.
The continuous variables were summarised as mean ± standard deviation, and the categorical variables were summarised as frequency (percentage). All data were checked for normality before analysis. The skewed data were statistically analysed using the nonparametric Wilcoxon signed-rank test. The normally distributed data were assessed for equality of variances using Levene's test, and then, statistical analysis was performed using a paired t-test. A p-value < 0·05 was considered to indicate significant differences. Statistical analysis was performed using IBM SPSS software (version 23·0; IBM, Armonk, NY, USA).
Chinese Clinical Trial Registry (chictr.org.cn), ChiCTR-INC-16010019.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors had access to the dataset, and WL, HX, WW, JZ, YQ, and CF were responsible for the decision to submit the manuscript.
Results
Demographic and clinical characteristics of patients
Between January 1, 2017 and March 1, 2020, 104 eligible patients were eventually enrolled in this study. The demographic and clinical characteristics of the patients are presented in Table 1. These patients had different types of previous elbow injuries caused by low or high energy trauma. Among these patients, 74 (71%) patients had severe or very severe elbow stiffness. The duration of elbow stiffness varies widely from 6 months to 324 months. All patients underwent regular follow-up with a final mean follow-up time of 43·47 (95% CI, 41·45 - 45·49) months (Table 1).
Stability
Preoperatively, five patients had moderate valgus instability caused by treatment of previous trauma. The valgus instability in these five patients was resolved by MCL reconstruction. However, four patients developed a new onset of moderate valgus instability at 6 weeks postoperatively with the removal of the hinged external fixation. One hundred (96%) patients who underwent MCL reconstruction maintained medial stability at the last follow-up. No significant differences in the preoperative and postoperative stability scores were observed (P = 0·7820).
Mayo Elbow performance score and nerve symptoms
The mean MEPS increased from 63·27 (95% CI, 67·34 – 73·91) points to 95·05 (95% CI, 93·27 – 96·83) points at the final follow-up (P < 0·0001). At the final follow-up, 85 (82%) patients had excellent results, 17 (16%) patients had good results, 1 (1%) patient had fair results, and 1 (1%) patient was poor results. Twenty-four patients had preoperative nerve symptoms, including 22 ulnar nerve symptoms and two radial nerve symptoms. The ulnar nerve symptoms included numbness, claw deformity, and muscular atrophy, whereas the radial nerve symptoms included numbness only. Postoperatively, 12 patients still had nerve symptoms despite the relief of nerve symptoms, and seven patients had new-onset ulnar nerve numbness. After ulnar nerve release and anteriorization, seven patients with preoperative amyotrophy were relieved. However, one of them still had claw deformity. Overall, the nerve symptoms were significantly relieved, and the Amadio score increased from 8·07 (95% CI, 7·82 – 8·31) points to 8.56 (95% CI, 8·41 – 8·71) points (P < 0·0001).
Range of elbow motion
At the final follow-up, elbow extension had improved from a mean of 40·62° (95% CI, 37·38° - 43·87°) preoperatively to 10·77° (95% CI, 8·46° - 13·08°) postoperatively (P < 0·0001) (Table 3). Elbow flexion had increased considerably from 87·31° (95% CI, 83·80° – 90·82°) to 128·89° (95% CI, 126·52° – 131·27°) after surgery (P < 0·0001). As a result, the ROM was considerably modified from 46·88° (95% CI, 42·62° – 51·13°) to 118·13° (95% CI, 113·91° – 122·34°) (P < 0·0001). Preoperative pronation and supination increased from 54·18° (95% CI, 48·78° - 59·59°) and 68·94° (95% CI, 63·05° – 74·84°) to 70·62° (95% CI, 67·34° – 73·91°) and 83·51° (95% CI, 80·82° – 86·20°), respectively, after surgery (P < 0·0001 and P < 0·0001, respectively). Therefore, the rotational function of the forearm was improved (P < 0·0001).
Table 3.
Clinical evaluation of patients: preoperative and postoperative data.
| Characteristic | pre-operation | post-operation | P value |
|---|---|---|---|
| Extension (°) | 40.62 ± 16.70 (37.38 - 43.87) | 10.77 ± 11.86 (8.46 - 13.08) | < 0.0001 |
| Flexion (°) | 87.31 ± 18.05 (83.80 – 90.82) | 128.89 ± 12.23 (126.52 – 131.27) | < 0.0001 |
| ROM (°) | 46.88 ± 21.87 (42.62 – 51.13) | 118.13 ± 21.68 (113.91 – 122.34) | < 0.0001 |
| Pronation (°) | 54.18 ± 27.80 (48.78 - 59.59) | 70.62 ± 16.88 (67.34 – 73.91) | < 0.0001 |
| Supination (°) | 68.94 ± 30.31 (63.05 – 74.84) | 83.51 ± 13.83 (80.82 – 86.20) | < 0.0001 |
| FRR (°) | 123.21 ± 48.75 (113.73 – 132.69) | 154.04 ± 25.08 (149.16 – 158.92) | < 0.0001 |
| Stability (points) | 9.76 ± 1.07 (9.55 – 9.97) | 9.71 ± 1.36 (9.45 – 9.98) | 0.7820 |
| MEPS (points) | 63.27 ± 14.89 (60.37 – 66.17) | 95.24 ± 8.82 (93.52 – 96.96) | < 0.0001 |
| VAS (points) | 1.38 ± 1.77 (1.04 – 1.73) | 0.32 ± 0.77 (0.17 – 0.47) | < 0.0001 |
| Grip strength (kg) | 23.95 ± 10.39 (21.92 – 25.97) | 27.25 ± 9.47 (25.41 – 29.09) | < 0.0001 |
| Amadio score (points) | 8.07 ± 1.26 (7.82 – 8.31) | 8.56 ± 0.76 (8.41 – 8.71) | < 0.0001 |
ROM, range of motion; FRR, forearm rotational range of motion; MEPS, Mayo Elbow Performance Score; VAS, visual analog scale; Data are presented as the mean ± standard deviation (95% CI).
Pain and grip strength
Forty-five (43%) patients suffered preoperative pain with a VAS score of 1·38 points (95% CI, 1·04 – 1·73), and 19 (18%) patients had postoperative pain with a VAS score of 0·32 points (95% CI, 0·17 – 0·47) (P < 0·0001). Of these 19 patients, 16 patients had pain relief, two patients had no significant relief in pain, and unfortunately, one patient had new mild pain after surgery. After surgical treatment and rehabilitation exercises, the muscle strength of patients improved from 23·95 (95% CI, 21·92 – 25·97) kg to 27·25 (95% CI, 25·41 – 29·09) kg (P < 0·0001).
Recurrence of stiffness
Elbow stiffness recurred in 17 (16%) patients, including two with mild, 11 with moderate, and four with severe stiffness (Table 4). Of the four patients with severe stiffness, stiffness in three patients was due to recurrent HO, and that of one patient was due to the development of olecranon fracture. Although recurrence of elbow stiffness occurred in 17 patients, nine patients had excellent results, six patients had good results, one patient had a fair result, and one patient had a poor result. The poor or fair results in two patients were caused by a recurrence of HO; they still had mild pain despite some relief. Pain and HO recurrence may be important factors contributing to renewed elbow stiffness.
Table 4.
Recurrence of elbow stiffness.
| Variables | Values or proportions |
|---|---|
| Minimum or functional stiffness | 2 (2%) |
| Moderate stiffness | 11(10%) |
| Severe stiffness | 4 (4%) |
Postoperative complications
One patient developed an infection at the nail tract of hinged external fixation; the patient underwent antibiotic treatment (Table 5). One patient experienced a fracture caused by violent rehabilitation exercises after the removal of a metal implant in release surgery; the patient underwent conservative treatment. One patient with no previous pain developed mild pain after the release procedure, and the pain was slightly relieved at the last follow-up. Seven patients had new-onset ulnar nerve numbness, which was not relieved significantly after conservative treatment. Four patients still had moderate valgus instability of the elbow after conservative treatment.
Table 5.
Distribution of postoperative complications.
| Variables | Values or proportions |
|---|---|
| Infection, n (%) | 1 (1%) |
| New onset of nerve symptoms, n (%) | 7 (7%) |
| New onset of pain | 1 (1%) |
| Fracture, n (%) | 1 (1%) |
| Moderate valgus instability, n (%) | 4 (4%) |
Discussion
The elbow joint is sensitive to trauma and even surgical trauma.2,20,29,37 Elbow stiffness is a common complication of trauma. A variety of factors can cause restriction in elbow movement, and MCL ossification or contracture is one of the important factors which need to be removed.6,7,16 Therefore, reduced invasion of the elbow joint is essential for MCL reconstruction in patients with elbow stiffness. To our knowledge, this study is the first to use a minimally invasive MCL reconstruction technique to reconstruct valgus stability and evaluate its effectiveness in patients with elbow stiffness. We conducted this prospective study to investigate whether the technique could be effective in restoring valgus stability in patients with elbow stiffness after complete open arthrolysis. In this study, all patients developed elbow stiffness after trauma, and their MCLs underwent ossification or severe contracture. We used fascia and tendon patches to reconstruct the medial stability of the elbow in all patients after resection or excision of the MCL. Our results showed that the new technique could effectively restore valgus stability. Additionally, surgical treatment combined with rehabilitation exercises proved to be a reliable procedure for elbow stiffness.
In our study, the MCL reconstruction technique consisted of three strips A, B, and C (Figure 2).21 This new MCL technique is a modification of the previous fascia reconstruction technique.17 In the new MCL reconstruction technique, we used a longer fascia patch than before, and the fascia patch passed underneath the ulnar carpal flexor and fitted snugly over the bone surface. The fascia was first fixed at the origin of the AMCL, then reversed and fixed at the centre of the ulnar attachments of the AMCL, forming strands A and B. The two-strand fascial reconstruction has advantages over the previous single-strand reconstruction, and the fascia adhered to the bone surface can maintain stable tension more effectively than in the previous fascia reconstruction. Previous literature has reported that the proximal and distal parts of the insertion of the AMCL played different roles in maintaining medial elbow stability.38,39 Frangiamore argued that proximal insertion is important for maintaining stability at higher elbow flexion angles, whereas distal insertion is important at lower flexion angles.38 In biomechanical studies, Hassan concluded that the proximal half insertion has a significant role in maintaining posteromedial stability of the elbow, whereas the distal half has no significance.39 Our study used strips A and B to replace the AMCL. Strip A was reconstructed at the centre of the original AMCL insertion, simulating the role of the proximal half of the original insertion. Strip B was proximal to the proximal half of the insertion, reinforcing the role of the proximal half of the original insertion. The existing Jobe and Docking techniques converge the two strands on the ulna into one strand on the medial condyle.40 The shape of the reconstructed ligament is similar to that in our AMCL reconstruction, but our technique is performed more closely to the functional area of the proximal insertion. The interference technique and the internal bracing technique use a single strand reconstruction, whose position is similar to that of strip A in our AMCL reconstruction. Therefore, we believe that our AMCL reconstruction technique has advantages over the traditional technique in terms of reconstructed functional areas and the number of reconstructed ligaments. Additionally, the new technique involves a PMCL reconstruction using the triceps tendon, forming a C-strand, which is different from the previous fascia reconstruction.17 The PMCL was considered to play an important role in maintaining the posteromedial stability of the elbow, and reconstruction of the PMCL after injury was recommended.14,41 Additionally, the medial and central portions of the triceps tendon are thicker and stiffer than the lateral portion, and the medial portion of the tendon can be used as a graft for ligament reconstruction.42 Therefore, we used the medial part of the triceps tendon for PMCL reconstruction. The new reconstruction technique formed a fan-shaped structure, which covered a wider area than the previous technique to maintain the stability of the medial elbow. Additionally, biomechanical studies confirmed that the new technique has certain advantages in maintaining elbow valgus stability.21 Therefore, from the perspective of structural and biomechanical characteristics, we believe that the new technique has an advantage over the traditional technique in maintaining the valgus stability of the elbow.
In this study, four (4%) patients were found to have moderate elbow valgus instability when the hinged external fixation was removed at 6 weeks postoperatively. The valgus instability may be related to partial healing of the soft tissues. Moreover, they still remained unstable after conservative treatment at the final follow-up. Reconstruction failure may be related to insufficient tension of the fascia and triceps tendon patches during fixation of the patches. The overall stability did not change before and after surgery (P = 0·7820). Our MCL reconstruction technique used soft tissues around the elbow joint and eliminated the need to obtain grafts from other donor areas, avoiding the dysfunction and complications associated with donor areas.43 In this study, MCL reconstruction was applied to patients with post-traumatic elbow stiffness who were more sensitive to trauma or even surgical trauma and were more prone to contracture and heterotopic ossification. Patients without elbow stiffness may have better clinical outcomes with less invasive ligament reconstruction. The results of MCL reconstruction in patients with post-traumatic elbow stiffness may be better than in patients with immune or metabolic elbow stiffness because the immune or metabolic disease may have an inflammatory response in the ulnar carpal flexor fascia and triceps tendon.
Numerous research studies have confirmed that open elbow release is an ideal treatment for elbow stiffness.1,9, 10, 11, 12,16,17 In our study, patients had different severities of elbow stiffness caused by various original injuries in high or low energy trauma. The MCL of all patients was confirmed to be ossified or severely contracted during the release procedure. All patients had moderate stiffness or above, and the severity of stiffness may have affected contracture or ossification of the elbow MCL. By complete release, including removal of the diseased MCL, all patients achieved excellent elbow mobility in intraoperative evaluation. The results of our study showed that ROM and FRR improved significantly in 87 (84%) patients. The average extension, flexion, and ROM increased by 29·83° (73%), 41.58° (47%), and 71·25° (152%), respectively. The mean protonation, supination, and FRR increased by 16·44° (30%), 14.57° (21%), and 30.83° (25%), respectively. The average MEPS significantly increased by 31·97 points (51%). The results indicated that open release was an excellent method for improving mobility and function for patients with elbow stiffness, which was consistent with findings from previous studies.1,9, 10, 11, 12,16,17 Most patients' preoperative pain was relieved after arthrolysis and rehabilitation. Therefore, we concluded that arthrolysis and rehabilitation exercises are reliable approaches for treating posttraumatic pain. However, mild postoperative pain remained in 19 patients. The residual pain may be related to healing of the postoperative scar, re-contraction of the soft tissue, or joint deformity.
In this study, most patients had relief of nerve symptoms after nerve release. Two patients had slight relief of radial nerve symptoms after radial nerve release. One patient with preoperative nerve symptoms still had claw deformity despite some relief of ulnar nerve symptoms, which may be related to the loss of neurotrophy of the muscle. Seven patients newly developed ulnar nerve numbness after surgery. The new emerging ulnar nerve symptoms may be associated with contracture of the soft tissues and complete improvement in mobility, which results in compression or strain on the ulnar nerve. We routinely performed ulnar nerve release and anteriorization. Overall, nerve symptoms were relieved, and the mean Amadio score improved (P < 0·0001).
All patients accepted uniform postoperative rehabilitation exercises with enhanced recovery after surgery (ERAS).28 Scientific rehabilitation exercises have been verified to remarkably improve joint mobility and function.9,25,28 Additionally, all patients were encouraged to perform muscle strength training after removing the hinged external fixation. The average grip strength of the patients was improved by 3·3 kg, which was a 14% increase in muscle strength (P < 0·0001). The increase in muscle strength was significantly lower than the 95% increase in patients with rheumatoid stiffness,9 which may be related to the lower pain profile in patients with preoperative posttraumatic stiffness compared to rheumatoid patients. However, the overall level of postoperative muscle strength was higher than in rheumatoid patients. Therefore, we believe that postoperative rehabilitation and strength training has a positive effect on improving muscle strength and elbow function in patients with elbow stiffness.
In our study, 17 (16%) patients had recurrent elbow stiffness, ranging from mild to severe stiffness. Although the recurrence rate of elbow stiffness was relatively high as previously reported,1 15 patients had excellent or good results, and only two patients had fair or poor results. Although 15 patients had recurrent elbow stiffness caused by soft tissue contracture or pain, they were allowed to continue with their daily lives. The two (2%) patients with fair or poor results had a recurrence of HO on the posterior and medial sides of the elbow, but no ossification occurred in the reconstructed MCL. The recurrent HO affected the elbow joint function and was therefore named function-related HO. The 2% HO recurrence rate was lower than the 4% reported in previous studies.25 However, the function-related HO is not representative of HO recurrence in all patients, as some patients have recurrent HO that does not affect function and refuse to retest radiographic imaging. Therefore, the actual rate of HO recurrence may be underestimated, and the results should be interpreted with caution. We believe that less invasive reconstruction after effective release is beneficial in reducing the recurrence of function-related HO.
Several common complications were observed in the present study. The patient with superficial infection underwent antibiotic therapy. After treatment with non-steroidal anti-inflammatory drugs (NSAIDs) and reduced activity, the patient with new-onset pain was slightly relieved but still had mild pain. Seven patients with new-onset ulnar nerve symptoms were slightly relieved but still had numbness after nerve nutrition therapy, which may be related to compression caused by postoperative contracture of the soft tissue. The patient with the fracture refused surgical treatment and experienced a recurrence of elbow stiffness. Four patients with instability remained unstable after conservative treatment. The four patients accepted the current joint function and refused another ligament reconstruction treatment.
This study is a multicentre study. To minimise central effects, we ensured strict standardisation and consistency in trial management, subject baseline characteristics, and clinical practice. In order to achieve multicentre homogeneity, we have developed several measures. First, we developed a multiparty-approved trial protocol, which guided the entire trial and ensured strict adherence to the protocol during the actual operation of each study centre. Second, we required each centre to strictly comply with the inclusion and exclusion criteria and select subjects who met the criteria. Third, the surgeries at each centre were operated by a regular surgeon who had undergone rigorous standardised training at our main centre (Shanghai Sixth People's Hospital). Their surgical skills and abilities were basically at the same level, and they all followed the same operational procedures for surgery as well as perioperative management. Fourth, we had uniformly trained senior surgeons from each centre for data collection, and developed a uniform rating scale. The main centre made the final assessment when ambiguity occurred. We acknowledge that even though we controlled for variations in surgical performance between centres, some heterogeneity may have existed between centres in terms of differences in trial management, patient selection, and clinical practices.
This study has several limitations. First, the study sample size was small and lacked a control group. Randomized controlled clinical trials recruiting patients undergoing the new MCL reconstruction technique matched with patients undergoing other reconstruction techniques are needed. However, they are difficult to execute due to the low prevalence of MCL ossification or contracture. Second, this study's evaluation of valgus stability used physical examinations and simple stability scores in MEPS, which lacked detailed quantification of valgus stability. A more detailed elbow valgus instability scoring system needs to be created and introduced to evaluate elbow valgus stability. Third, radiographic imaging was not performed for all patients at the last follow-up, which may underestimate the recurrence of HO. Fourth, obesity and diabetes affected functional recovery after surgery in patients with elbow joint stiffness. There was only one diabetic patient and seven obese patients in our study, and the number of patients was too small to perform an accurate subgroup statistical analysis.
In conclusion, the new less-invasive MCL reconstruction technique can effectively rebuild medial stability in patients with elbow stiffness after complete arthrolysis.
Contributors
WL, HX, WW, YQ wrote the draft manuscript. WL, HX, WW, YQ and JL revised manuscript. WL, HX, WW, SC, FL, HY, YQ collected the data. WL, YQ analyzed the data. JZ, YQ, and CF conducted the study design and quality control. All authors including YQ, WL, HX, WW, SC, FL, HY, JZ, JL, and CF have accessed and verified the study data
Data sharing statement
The data associated with this study are present in the paper. The raw data is also available from the corresponding authors upon reasonable request.
Declaration of interests
All authors declare no competing interests.
Funding
The study was supported by the National Key Research and Development Program of China (No. 2021YFC2400805), National Natural Science Foundation of China (No. 81830076), Young Elite Scientist Sponsorship Program by Cast (No. YESS20200153), Shanghai Sailing Program (No. 20YF1436000), Shanghai Municipal Science and Technology Commission Foundation (No.19ZR1439200), Municipal Hospital Newly-developing Cutting-edge Technologies Joint Research Program of Shanghai Shenkang Hospital Development Centre (No. SHDC12018130).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101616.
Contributor Information
Jingwei Zhang, Email: zx12orthopaedics@163.com.
Yun Qian, Email: lollipopcloudland@foxmail.com.
Cunyi Fan, Email: cyfan@sjtu.edu.cn.
Appendix. Supplementary materials
References
- 1.Yu S, Chen M, Fan C. Team approach: elbow contracture due to heterotopic ossification. JBJS Rev. 2017;5(1) doi: 10.2106/JBJS.RVW.16.00008. 01874474-201701000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Foruria AM, Augustin S, Morrey BF, Sánchez-Sotelo J. Heterotopic ossification after surgery for fractures and fracture-dislocations involving the proximal aspect of the radius or ulna. J Bone Joint Surg Am. 2013;95(10):e66. doi: 10.2106/JBJS.K.01533. [DOI] [PubMed] [Google Scholar]
- 3.Foruria AM, Lawrence TM, Augustin S, Morrey BF, Sanchez-Sotelo J. Heterotopic ossification after surgery for distal humeral fractures. Bone Joint J. 2014;96-B(12):1681–1687. doi: 10.1302/0301-620X.96B12.34091. [DOI] [PubMed] [Google Scholar]
- 4.Kodde IF, van Rijn J, van den Bekerom MP, Eygendaal D. Surgical treatment of post-traumatic elbow stiffness: a systematic review. J Shoulder Elbow Surg. 2013;22(4):574–580. doi: 10.1016/j.jse.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Ranganathan K, Loder S, Agarwal S, et al. Heterotopic ossification: basic-science principles and clinical correlates. J Bone Joint Surg Am. 2015;97(13):1101–1111. doi: 10.2106/JBJS.N.01056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morrey BF. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Joint Surg Am. 1990;72(4):601–618. [PubMed] [Google Scholar]
- 7.Beck CM, Gluck MJ, Zhang Y, et al. Outcomes of arthroscopic elbow contracture release: improvement for severe prosupination and flexion contracture. Arthroscopy. 2022;38(2):315–322. doi: 10.1016/j.arthro.2021.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63(6):872–877. [PubMed] [Google Scholar]
- 9.Liu W, Zhang J, Liu J, et al. Clinical results of a 10-year follow-up of surgical treatment for elbow stiffness in rheumatoid arthritis: a case series. Int J Surg. 2022;99 doi: 10.1016/j.ijsu.2022.106590. [DOI] [PubMed] [Google Scholar]
- 10.Haglin JM, Kugelman DN, Christiano A, Konda SR, Paksima N, Egol KA. Open surgical elbow contracture release after trauma: results and recommendations. J Shoulder Elbow Surg. 2018;27(3):418–426. doi: 10.1016/j.jse.2017.10.023. [DOI] [PubMed] [Google Scholar]
- 11.Salazar D, Golz A, Israel H, Marra G. Heterotopic ossification of the elbow treated with surgical resection: risk factors, bony ankylosis, and complications. Clin Orthop Relat Res. 2014;472(7):2269–2275. doi: 10.1007/s11999-014-3591-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang W, Zhan YL, Yu SY, Zheng XY, Liu S, Fan CY. Open arthrolysis with pie-crusting release of the triceps tendon for treating post-traumatic contracture of the elbow. J Shoulder Elbow Surg. 2016;25(5):816–822. doi: 10.1016/j.jse.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 13.Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11(5):315–319. doi: 10.1177/036354658301100506. [DOI] [PubMed] [Google Scholar]
- 14.Shukla DR, Golan E, Nasser P, Culbertson M, Hausman M. Importance of the posterior bundle of the medial ulnar collateral ligament. J Shoulder Elbow Surg. 2016;25(11):1868–1873. doi: 10.1016/j.jse.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Golan EJ, Shukla DR, Nasser P, Hausman M. Isolated ligamentous injury can cause posteromedial elbow instability: a cadaveric study. J Shoulder Elbow Surg. 2016;25(12):2019–2024. doi: 10.1016/j.jse.2016.04.022. [DOI] [PubMed] [Google Scholar]
- 16.Zhou Y, Cai JY, Chen S, Liu S, Wang W, Fan CY. Application of distal radius-positioned hinged external fixator in complete open release for severe elbow stiffness. J Shoulder Elbow Surg. 2017;26(2):e44–e51. doi: 10.1016/j.jse.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 17.Chen S, Yan H, Wang W, Zhang M, Hildebrand KA, Fan CY. Reconstruction of medial collateral ligament defects with a flexor-pronator fascia patch in complete open release of stiff elbows. J Shoulder Elbow Surg. 2017;26(1):133–139. doi: 10.1016/j.jse.2016.09.030. [DOI] [PubMed] [Google Scholar]
- 18.Bodendorfer BM, Looney AM, Lipkin SL, et al. Biomechanical comparison of ulnar collateral ligament reconstruction with the docking technique versus repair with internal bracing. Am J Sports Med. 2018;46(14):3495–3501. doi: 10.1177/0363546518803771. [DOI] [PubMed] [Google Scholar]
- 19.Looney AM, Wang DX, Conroy CM, et al. Modified jobe versus docking technique for elbow ulnar collateral ligament reconstruction: a systematic review and meta-analysis of clinical outcomes. Am J Sports Med. 2021;49(1):236–248. doi: 10.1177/0363546520921160. [DOI] [PubMed] [Google Scholar]
- 20.Qian Y, Yu S, Shi Y, Huang H, Fan C. Risk factors for the occurrence and progression of posttraumatic elbow stiffness: a case-control study of 688 cases. Front Med (Lausanne) 2020;7 doi: 10.3389/fmed.2020.604056. Published 2020 Dec 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu W, Xiong H, Chen S, et al. Biomechanical evaluation of a low-invasive elbow medial collateral ligament reconstruction technique with fascia and tendon patches. Front Bioeng Biotechnol. 2022;10 doi: 10.3389/fbioe.2022.831545. Published 2022 Mar 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.General Administration of Sport of China. 2006. Skeletal maturity and assessment methods of hand and wrist for Chinese: TY/T 3001-2006.https://d.wanfangdata.com.cn/standard/ChxTdGFuZG FyZE5ld1MyMDIwMDkxODIwMjIwNTMwEg5UWS9UIDMwM DEtMjAwNhoIczlkODljZG8%3D [Google Scholar]
- 23.Zelle BA, Bhandari M, Sanchez AI, Probst C, Pape HC. Loss of follow-up in orthopaedic trauma: is 80% follow-up still acceptable? J Orthop Trauma. 2013;27(3):177–181. doi: 10.1097/BOT.0b013e31825cf367. [DOI] [PubMed] [Google Scholar]
- 24.Akl EA, Briel M, You JJ, et al. Potential impact on estimated treatment effects of information lost to follow-up in randomised controlled trials (LOST-IT): systematic review. BMJ. 2012;344:e2809. doi: 10.1136/bmj.e2809. Published 2012 May 18. [DOI] [PubMed] [Google Scholar]
- 25.Sun Z, Cui H, Ruan J, Li J, Wang W, Fan C. What range of motion and functional results can be expected after open arthrolysis with hinged external fixation for severe posttraumatic elbow stiffness? Clin Orthop Relat Res. 2019;477(10):2319–2328. doi: 10.1097/CORR.0000000000000726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang W, Jiang SC, Liu S, Ruan HJ, Fan CY. Stability of severely stiff elbows after complete open release: treatment by ligament repair with suture anchors and hinged external fixator. J Shoulder Elbow Surg. 2014;23(10):1537–1544. doi: 10.1016/j.jse.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 27.O'Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73(3):440–446. [PubMed] [Google Scholar]
- 28.Cui H, Sun Z, Ruan J, Yu Y, Fan C. Effect of enhanced recovery after surgery (ERAS) pathway on the postoperative outcomes of elbow arthrolysis: a randomized controlled trial. Int J Surg. 2019;68:78–84. doi: 10.1016/j.ijsu.2019.06.010. [DOI] [PubMed] [Google Scholar]
- 29.Andrachuk JS, Scillia AJ, Aune KT, Andrews JR, Dugas JR, Cain EL. Symptomatic heterotopic ossification after ulnar collateral ligament reconstruction: clinical significance and treatment outcome. Am J Sports Med. 2016;44(5):1324–1328. doi: 10.1177/0363546515626185. [DOI] [PubMed] [Google Scholar]
- 30.Sun Y, Cai J, Li F, Liu S, Ruan H, Fan C. The efficacy of celecoxib in preventing heterotopic ossification recurrence after open arthrolysis for post-traumatic elbow stiffness in adults. J Shoulder Elbow Surg. 2015;24(11):1735–1740. doi: 10.1016/j.jse.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 31.Mansat P, Morrey BF. The column procedure: a limited lateral approach for extrinsic contracture of the elbow. J Bone Joint Surg Am. 1998;80(11):1603–1615. [PubMed] [Google Scholar]
- 32.Morrey BF, Bryan RS, Dobyns JH, Linscheid RL. Total elbow arthroplasty. A five-year experience at the Mayo Clinic. J Bone Joint Surg Am. 1981;63(7):1050–1063. [PubMed] [Google Scholar]
- 33.Huskisson EC. Measurement of pain. Lancet. 1974;2(7889):1127–1131. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 34.Amadio PC. Anatomical basis for a technique of ulnar nerve transposition. Surg Radiol Anat. 1986;8(3):155–161. doi: 10.1007/BF02427843. [DOI] [PubMed] [Google Scholar]
- 35.Hariri S, Safran MR. Ulnar collateral ligament injury in the overhead athlete. Clin Sports Med. 2010;29(4):619–644. doi: 10.1016/j.csm.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 36.O'Driscoll SW, Lawton RL, Smith AM. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am J Sports Med. 2005;33(2):231–239. doi: 10.1177/0363546504267804. [DOI] [PubMed] [Google Scholar]
- 37.Dunham CL, Castile RM, Havlioglu N, Chamberlain AM, Lake SP. Temporal patterns of motion in flexion-extension and pronation-supination in a rat model of posttraumatic elbow contracture. Clin Orthop Relat Res. 2018;476(9):1878–1889. doi: 10.1097/CORR.0000000000000388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Frangiamore SJ, Lynch TS, Vaughn MD, et al. Magnetic resonance imaging predictors of failure in the nonoperative management of ulnar collateral ligament injuries in professional baseball pitchers. Am J Sports Med. 2017;45(8):1783–1789. doi: 10.1177/0363546517699832. [DOI] [PubMed] [Google Scholar]
- 39.Hassan SE, Parks BG, Douoguih WA, Osbahr DC. Effect of distal ulnar collateral ligament tear pattern on contact forces and valgus stability in the posteromedial compartment of the elbow. Am J Sports Med. 2015;43(2):447–452. doi: 10.1177/0363546514557239. [DOI] [PubMed] [Google Scholar]
- 40.Langer P, Fadale P, Hulstyn M. Evolution of the treatment options of ulnar collateral ligament injuries of the elbow. Br J Sports Med. 2006;40(6):499–506. doi: 10.1136/bjsm.2005.025072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shukla DR, Golan E, Weiser MC, Nasser P, Choueka J, Hausman M. The posterior bundle's effect on posteromedial elbow instability after a transverse coronoid fracture: a biomechanical study. J Hand Surg Am. 2018;43(4):381. doi: 10.1016/j.jhsa.2017.09.018. .e1–8. [DOI] [PubMed] [Google Scholar]
- 42.Baumfeld JA, van Riet RP, Zobitz ME, Eygendaal D, An KN, Steinmann SP. Triceps tendon properties and its potential as an autograft. J Shoulder Elbow Surg. 2010;19(5):697–699. doi: 10.1016/j.jse.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 43.Cain EL, Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: Results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. doi: 10.1177/0363546510378100. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.