Abstract
Objective
Healthcare provider (HCP) burnout is on the rise with electronic medical record (EMR) use being cited as a factor, particularly with the rise of the COVID-19 pandemic. Burnout in HCPs is associated with negative patient outcomes, and, therefore, it is crucial to understand and address each factor that affects HCP burnout. This study aims to (a) assess the relationship between EMR use and burnout and (b) explore interventions to reduce EMR-related burnout.
Methods
We searched MEDLINE (Ovid), CINAHL and SCOPUS on 29 July 2021. We selected all studies in English from any publication year and country that discussed burnout in HCPs (physicians, nurse practitioners and registered nurses) related to EMR use. Studies must have reported a quantitative relationship to be included. Studies that implemented an intervention to address this burnout were also included. All titles and abstracts were screened by two reviewers, and all full-text articles were reviewed by two reviewers. Any conflicts were addressed with a third reviewer and resolved through discussion. Quality of evidence of all included articles was assessed using the Quality Rating Scheme for Studies and Other Evidence.
Findings
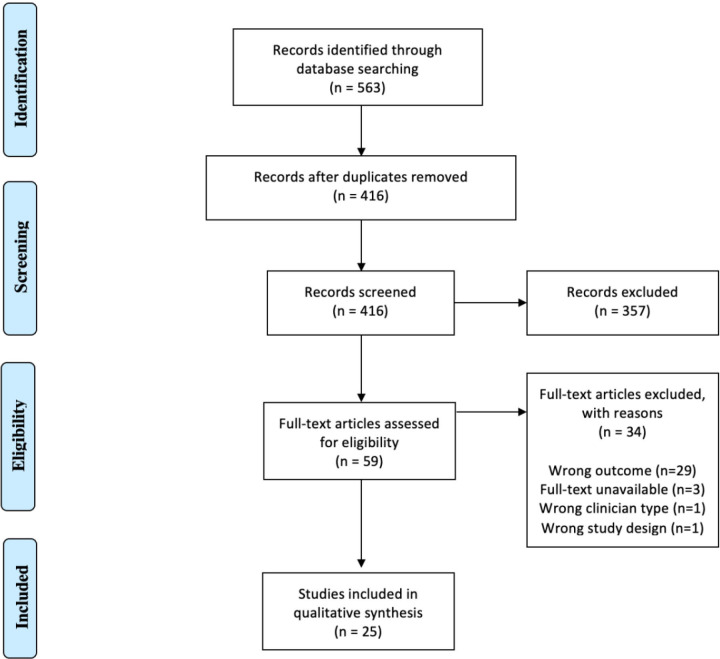
The search identified 563 citations with 416 citations remaining after duplicate removal. A review of abstracts led to 59 studies available for full-text assessment, resulting in 25 studies included in the scoping review. Commonly identified associations between EMR-related burnout in HCPs included: message and alert load, time spent on EMRs, organisational support, EMR functionality and usability and general use of EMRs. Two articles employed team-based interventions to improve burnout symptoms without significant improvement in burnout scores.
Conclusions and relevance
Current literature supports an association between EMR use and provider burnout. Very limited evidence exists for burnout-reducing interventions that address factors such as time spent on EMRs, organisational support or EMR design.
Keywords: health informatics, health & safety, organisational development
Strengths and limitations of this study.
This scoping review consisted of 25 studies representing 55 459 healthcare professionals (physicians, nurse practitioners and registered nurses).
This study used the WHO guidelines on scoping reviews and reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines to guide this scoping review.
Quality of evidence was assessed using the Quality Rating Scheme for Studies and Other Evidence.
Given the heterogeneity of data between the included studies, a meta-analysis was not appropriate and instead a narrative thematic analysis was performed to analyse the data.
This study explored electronic medical record-related burnout factors and situated them in the context of interventions and organisational supports.
Introduction
Electronic medical records (EMRs) are an important part of the way that health-related data are stored, accessed and managed, and, ultimately, how care is provided for patients across the world. EMRs are essential tools for healthcare that are continuously evolving and, therefore, the implementation of EMRs can have a significant impact on care delivery and the well-being of healthcare providers (HCPs).
Burnout is an occupation-related stress syndrome that accumulates through job-related stress. Several burnout indices have been developed to measure physician burnout, including the Mini Z survey, the Maslach Burnout Inventory (MBI), the Mayo Well Being Index and the Shirom-Melamed Burnout Measure (SMBM). The Mini Z is a ten-item survey to assess three outcomes (stress, burnout and satisfaction), and seven drivers of burnout (work control, work chaos, teamwork, values alignment with leadership, documentation time pressure, EMR use at home and EMR proficiency) with 5-point Likert scales. The MBI, the original type of survey, the MBI-Human Services Survey, is designed for professionals in human services, including HCPs. It contains 22 questions and three scales: emotional exhaustion, depersonalisation and personal accomplishment.1 The Mayo Well-Being Index is a 7 or 9 item instrument with yes or no response categories used to identify distress in a variety of dimensions including burnout, fatigue, low mental/physical quality of life, depression, anxiety and stress.2 Finally, the SMBM contains 14 items, which evaluate physical fatigue, emotional exhaustion and cognitive weariness.
The first EMR was developed in 1972, and, since then, has undergone massive strides in technological innovation and is a cornerstone of medical care provided all over the world. The COVID-19 pandemic has showcased the importance of generating real-time data for crisis response and planning, necessitating the use of carefully documented COVID-19 cases, to allow for ongoing tracking.
HCPs, in particular, are at higher risk for burnout,3 and this can have significant impacts on patient care and outcomes.4 Physician burnout through the Medscape National Physician Burnout and Suicide report was estimated to be 43%.5 Among nurses in the USA, 31.5% of registered nurses (RNs) who were leaving their job cited burnout as a reason.6 As mentioned, EMRs are an important aspect of health systems; however, they have been reported to contribute to HCP burnout. In a 2017 study analysing the influence of EMRs on physician burnout, 37% of practising physicians were experiencing at least one symptom of burnout, and 75% of these individuals attributed EMR as a contributor to their burnout.7
HCP burnout is a significant issue impacting our healthcare system today, and with quality improvement initiatives on the rise and the COVID-19 pandemic requiring large-scale data collection, it is crucial to investigate the relationship between EMRs and HCP burnout to consider its effects on the well-being of healthcare workers and patient outcomes. The objective of this study is to complete a scoping review of the literature assessing EMR-related burnout in HCPs. Specifically, to (1) explore the factors related to EMR that are associated with HCP burnout and (2) identify interventions to reduce these burdens. Other articles have attempted to explore the relationship between EMR use and HCP burnout;8 9 however, our article seeks to further understand interventions and organisational supports that have been implemented to address EMR-related HCP burnout and is not limited by publication year or location. To our knowledge, a study of this kind has not yet been published.
Methods
We conducted a scoping review in accordance with the International prospective register of systematic reviews (PROSPERO) Registration Standards10 and reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Search methods and information sources
We developed a search strategy (online supplemental appendix 1) by reviewing the search strategies of similar reviews on the effect of EMR on HCP burnout. For the purposes of this study, we have included all studies that evaluated the effect of electronic health records as well. The following electronic databases were searched: MEDLINE (Ovid), CINAHL and SCOPUS on 29 July 2021. Articles published at any time, in the English language, were included. Reference lists of included articles were also manually screened to identify additional studies.
bmjopen-2022-060865supp001.pdf (73.4KB, pdf)
Screening process
Titles and/or abstracts of studies retrieved using the search strategy and those from additional sources were screened independently by two review authors (CL and CP) to identify studies that met the inclusion criteria (table 1). The full text of these studies was retrieved and independently assessed for eligibility by two review team members (CL and CP). Any disagreement over the eligibility of particular studies was resolved through discussion with a third reviewer (DTK).
Table 1.
Eligibility criteria of studies
| Inclusion criteria | Exclusion criteria |
| Specific data on physicians, nurse practitioners and registered nurses Inclusion of quantitative data relating burnout to EMR use |
Not primary research (commentary, letters, conference abstracts, etc.) Wrong outcome (not EMR related, not burnout related) Not in English No full-text available |
EMR, electronic medical record.
Eligibility criteria
Eligibility criteria are included in table 1. Our study focused on the experiences of specific HCPs, which included physicians, nurse practitioners (NPs) and RNs. We included articles, published globally, that focused on burnout related to EMR use.
Data extraction
Data were extracted from studies into a predefined form. Data extracted included author, title, year of publication, country of origin, study design, number of participants (including breakdown according to sex), HCP type, burnout measurement, outcomes and grade of evidence. A review author (DTK) extracted data independently, and two review authors (CL and CP) reviewed the extracted results.
Rating of the quality of evidence
All included studies were graded according to the Quality Rating Scheme for Studies and Other Evidence11 by two reviewers independently (CL and CP), with discrepancies resolved after joint review and discussion.
Data synthesis
Given the significant heterogeneity of the data between studies, it was not possible to complete a meta-analysis. A narrative thematic analysis was performed to analyse the data.
Results
Search results
A total of 563 journal articles were identified using the search strategy. After duplicates were removed, there were 416 abstracts that underwent screening. Based on inclusion and exclusion criteria, 357 studies were excluded leaving 59 studies for full-text review. After full-text screening, 25 studies were included in the systematic review (figure 1). Table 2 outlines the characteristics of each included study.7 12–34
Figure 1.
PRISMA flow diagram outlining literature search and results of screening process. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 2.
Summary of all included articles
| First author | Year | Country | Study design | Quality of evidence | Number of participants | HCP type(s) | Intervention (if applicable) | Burnout measurement | Outcomes related to EMR and HCP burnout |
| Adler-Milstein12 | 2020 | USA | Cross-sectional survey | 4 | 87 | Physicians and NPs | None | MBI | 1. Higher quartiles of time spent on scheduled days after hours were associated with greater odds of exhaustion but not cynicism. Dose–response relationship noted. The higher quartile the more chance of exhaustion. 2. No correlation between time spent on unscheduled days and cynicism or exhaustion. 3. Highest quartile of message volume had OR 6.17 of exhaustion compared with first quartile. |
| Babbott23 | 2014 | USA | Cross-sectional survey | 4 | 379 | Physicians | None | Five-point scale measuring stress and burnout | Compared low, moderate and high function EMRs in clinics, and a trend toward higher burnout scores in moderate function group |
| Eschenroeder28 | 2021 | USA | Cross-sectional survey | 4 | 25 018 | Physicians | None | Single question from AMA Mini-Z Survey | 1. Physicians with 5 or fewer hours of weekly after-hours charting were twice as likely to report lower levels of burnout than those with 6 or more hours (OR 2.43; CI 2.3 to 2.57). 2. Those who agree that their organisation has done a great job with EHR implementation, training, and support were twice as likely to report lower levels of burnout than those that disagreed (OR 2.14; CI 2.01 to 2.28). |
| Gardner29 | 2019 | USA | Cross-sectional survey | 4 | 1792 | Physicians | None | Single question from AMA Mini-Z Survey | 1. 27.2% using EHR reported one or more symptoms of burnout. 2. Reporting moderately high or excessive time on EHR at home associated with burnout (OR 1.93; CI 1.36 to 2.75) compared with less time at home. 3. Physicians reporting insufficient time for documentation had 2.81 times the odds of burnout symptoms compared with those with sufficient time |
| Giess30 | 2020 | USA | Cross-sectional survey | 4 | 159 | Physicians (radiologists) | None | Stanford Wellness Survey | Reporting that ‘The amount of work I have to do in the EHR per patient is excessive.’ was associated with burnout in radiologists (1.47 (1.09 to 2.02)), and reporting ‘I have to spend too much time completing EHR tasks other team members could do.’ was not associated with burnout in radiologists (1.26 (0.92 to 1.74)) |
| Gregory31 | 2017 | USA | Cross-sectional survey | 4 | 16 | Primary care providers (physicians, NP, PA) | Hour-long semi-structured group discussions regarding attitudes towards alerts, facilitated by an experienced internal medicine physician. (4 sessions over 4 weeks—total 4 hours) | Subjected alert workload: Self-report questionnaire related to: organisational tenure, perceived alert burden, time spent responding to inbox-related alerts, burnout. Objective workload: hours they spent per day, on average, attending to alerts. Burnout: SMBM | Subjective alert load was strongly correlated with physical fatigue dimension of burnout. Objective alert load was not correlated with burnout. |
| Harris32 | 2018 | Canada | Cross-sectional survey | 4 | 371 | Advanced practice registered nurses | None | Mini Z Burnout Survey | Burnout was associated with agreement that EHR adds to daily frustration (unadjusted and adjusted OR: 3.60 (2.0 to 6.51) and 2.17 (1.02 to 4.65)), moderately high or excessive time on EMR at home (unadjusted and adjusted OR: 5.02 (2.64 to 9.56) and 2.66 (0.91 to 7.80)), and insufficient time for documentation (unadjusted and adjusted OR: 5.15 (2.84 to 9.33) and 3.72 (1.78 to 7.80)). |
| Hilliard et al33 | 2020 | USA | Cross-sectional survey | 4 | 422 | Physicians, APRN, PA | None | Mini Z Burnout Survey | Clinicians with highest volume of patient call messages had almost 4 times odds of burnout compared with clinicians with fewest (aOR 3.81, 95% CI 1.44 to 10.14, p=0.007). |
| Kroth34 | 2019 | USA | Cross-sectional survey | 4 | 282 | MD, PA, NP, DO | None | Novel instrument (including questions from previously validated instruments from Motowidlo, physician work-life survey; healthy workplace study; minimising error, maximising outcome (MEMO) | EHR design and use factors accounted for 12.5% of variance in measures of stress and 6.8% of variance in measures of burnout. |
| Kutney-Lee13 | 2021 | USA | Cross-sectional analysis | 4 | 12 004 | Nurses | None | Survey | Poorer EHR usability was associated with higher odds of burnout (OR 1.42; 95% CI 1.23 to 1.63, p<0.001), job dissatisfaction (OR 1.71; 95% CI 1.45 to 2.02 p<0.001), intention to leave (OR 1.30, 1.1 to 1.55, p=0.003). Poorer EHR usability had significantly higher odds of inpatient mortality and 30-day readmission. |
| McPeek-Hinz14 | 2021 | USA | Cross-sectional survey | 4 | 1310 | Attending physicians, Advanced practice providers, house staff (residents) | None | Well-being survey (5-item derivative of the MBI emotional exhaustion domain) | Increased number of days spent using the EHR system was associated with less likelihood of burnout (OR 0.966, 95% CI 0.937 to 0.996, p=0.03). |
| Melnick15 | 2020 | USA | Cross-sectional survey | 4 | 870 | Physicians | None | MBI | Physician-related EHR usability was independently associated with the odds of burnout with each one point more favourable System Usability Scale (measuring EHR usability) score associated with a 3% lower odds of burnout (OR 0.97, 95% CI 0.97 to 0.98; p<0.001) |
| Melnick15 | 2020 | USA | Cross-sectional survey | 4 | 848 | Physicians | None | MBI | Higher System Usability Scale associated with decrease in provider task load which in turn was associated with lower odds of burnout. |
| Tai-Seale22 | 2019 | USA | Cross-sectional survey | 4 | 934 | Physicians | None | One-item burnout measure (validated 5-point scale) | Receiving more than the average number of system-generated in-basket messages was associated with a 40% higher probability of burnout. |
| Olson16 | 2019 | USA | Cross-sectional survey | 4 | 475 | Practising physicians | None | Mini-Z Burnout Survey and MBI | Predictors of burnout included excessive EMR time at home (OR=1.99, (1.21 to 3.27). Odds of burnout associated with stressors were generally concordant via Mini-Z’s burnout metric vs the MBI. |
| Peccoralo17 | 2021 | USA | Cross-sectional survey | 4 | 1781 | All faculty (MD/DO, psychologists) | None | Maslach Burnout Inventory and Mayo Well-Being Index | EHR frustration (OR 1.64 to 1.66), spending>90 min on EHR outside the work day by self-report (OR=1.41 to 1.90) and >1 hour of self-reported clerical work/day (OR 1.39) were associated with burnout. |
| Robertson7 | 2017 | USA | Cross-sectional survey | 4 | 585 | Physicians (Residents/ Attendings) | None | Single-item 5-point burnout scale | 62 (75%) attributing burnout to EHR. Those who spent more than 6 hours weekly after hours in EHR work were 2.9 x (95% CI 1.9 to 4.4) more likely to report burnout and 3.9x (95% CI 1.9 to 8.2) more likely to attribute burnout to the EHR |
| Shanafelt26 | 2016 | USA | Cross-sectional survey | 4 | 6375 | Physicians | None | MBI | Physicians who used EHRs and CPOE had higher rates of burnout on univariate analysis. Use of CPOE associated with a higher risk of burnout after adjusting (OR 1.29, 1.12 to 1.48 p<0.001). Use of EHRs was not associated with burnout in adjusted models controlling for CPOE and other factors |
| Sharp18 | 2021 | USA | Cross-sectional survey | 4 | 502 | Fellows in pulmonary and critical care medicine | None | MBI | Burdens of EHR documentation were associated with higher odds of both burnout and depressive symptoms. Working more than 70 hours in an average clinical week (adjusted OR (aOR), 2.80; 95% CI, 1.78 to 4.40) was associated significantly with higher odds of burnout. Spending a moderately high or excessive amount of time at home on EHRs (aOR, 1.71; 95% CI, 1.11 to 2.63) were associated significantly with higher odds of depressive symptoms. |
| Sieja19 | 2019 | USA | Cohort study | 3 | 220 | MD, DO, NP, PA, midwife (clinicians) and RN, MA and clerk (clinical staff) | Sprint process (an intensive team-based intervention) to optimise EHR efficiency. The Sprint intervention included clinician and staff EHR training, building specialty-specific EHR tools and redesigning teamwork. Agile project management principles were used to prioritise and track optimisation requests. Clinicians were surveyed about EHR burden, satisfaction with EHR, teamwork and burnout 60 days before and 2 weeks after Sprint. | MBI (emotional exhaustion domain) | ‘Our clinic’s use of the EHR has improved,’ and ‘time spent charting’ all improved. We report clinician satisfaction with specific Sprint activities. The percentage of clinicians endorsing burnout was 39% (47/119) before and 34% (37/107) after the intervention. p=0.434 |
| Simpson20 | 2021 | USA | Cohort study | 3 | 18 | Advanced practice providers | An intensive 2 week inpatient EHR training, personalisation and system configuration, which we called sprint. | Emotional Thriving, Emotional Recovery (modified) and Emotional Exhaustion Scales, a modified subset of the MBI | The three-axis emotional thriving, emotional recovery and emotional exhaustion metrics did not show a significant change. By user log data, time spent in the EHR did not show a significant decrease; however, 40% of the APPs responded that they spent less time in the EHR. |
| Somerson21 | 2020 | USA | Cross-sectional survey | 4 | 203 | Physicians (orthopaedic residents) | None | MBI-HSS | On multivariable analysis use of EMR more than 20 hours per week (OR 2.1; range 1.0–4.5), was associated with physician burnout |
| Tajirian | 2020 | Canada | Cross-sectional survey | 4 | 208 | Physicians (attendings and learners) | None | Mini-Z Burnout Survey | 74.5% (155/208) of all respondents who reported burnout symptoms identified the EHR as a contributor. Lower satisfaction and higher frustration with the EHRs were significantly associated with perceptions of EHR contributing towards burnout. |
| Tiwari25 | 2020 | USA | Cross-sectional survey | 4 | 128 | Physicians (rheumatology) | None | MBI | Dissatisfaction with EHRs was associated with a 2.86-times increased likelihood of burnout (OR 2.86, 95% CI 1.23 to 6.65, p=0.015). |
| Zumbrunn35 | 2020 | Switzerland | Cross-sectional survey | 4 | 472 | Physicians (general internal medicine residents) | None | Physician Well-Being Index (PWBI) | Low satisfaction with the EMR was not associated with burnout (1.29 (0.72 to 2.30)) |
APRN - Advanced Practice Reigstered Nurse, NP - Nurse Practitioners, PA- Physician Assistant, MD- Medical Doctor, DO- Doctor of Osteopathic Medicine
CPOE, computerised physician order entry; EMR, electronic medical record; HCP, healthcare provider; MBI, Maslach Burnout Inventory; SMBM, Shirom-Melamed Burnout Measure.
Study characteristics
The majority of papers were written in the USA (22/25) with Canada contributing two papers and one study from Switzerland. The primary methodology for the included studies was cross-sectional surveys (23/25) with only two papers using a cohort of patients assessing interventions to reduce burnout related to EMR. The primary assessment of burnout was the MBI used in 12 studies followed by the Mini Z instrument (six studies), Mayo Clinic’s Well-Being Instrument (two studies) and Stanford Wellness Survey and SMBM used in one study each. Other non-validated instruments or single burnout screening questions were used in five studies. Physicians, including attendings, fellows and residents, were represented in 22 of the 25 studies followed by NPs in eight studies and RNs in two studies. Finally, 23 of the 25 included studies had a rating of 4 for the Quality Rating Scheme for Studies and Other Evidence, and the remaining 2 included studies had a rating of 3.
EMR factors and interventions related to burnout
General use of EMR
Eight included studies conducted cross-sectional surveys wherein burnout association with general use of EMRs was investigated.7 18 24–26 29 30 35 Five of the studies showed a positive association between burnout symptoms and EMR use.7 18 24 25 29 Sharp et al revealed 32% of fellows with positive results for either burnout depressive symptoms had positive results for burnout symptoms and 23% for both burnout and depressive symptoms.18 In contrast, the other three studies indicated no significant association between the use of EMRs and burnout symptoms or reduced well-being.26 30 35 Shanafelt et al showed that the use of EMRs was not associated with burnout in models adjusted for computerised physician order entry and other factors in a group of 6375 participants.26 In summary, a majority of the eight included articles reported a significant association between general EMR use and one or more positive burnout symptoms.
EMR functionality and usability
There were six studies that reviewed EMR functionality and usability as a contributor to burnout in clinicians.13 15 23 24 27 34 Each of these studies identified direct associations between the perceived functionality and usability of the EMR and levels of burnout among providers. Two of the studies compared the system usability scale (SUS), a measure of EMR usability, and found that higher SUS (ie, more usable) EMRs directly correlated with decreased odds of burnout in physicians using the MBI.15 27 A large cross-sectional study of more than 12 000 nurses by Kutney-Lee et al identified that nurses with poorer EMR usability reported statistically significant higher odds of burnout, job dissatisfaction and intention to leave their job. Furthermore, there was a direct correlation of poorer EMR usability to increased odds of inpatient mortality.13 Babbott et al reported that physicians with moderate function EMRs were associated with higher levels of stress and a non-statistically significant trend towards higher burnout in moderate function groups, which they concluded was related to hybrid paper and computer systems.23 Tajirian et al and Kroth et al both reported that EMR design and usability impacted provider frustration levels and led to variance in measures of stress and burnout in the survey respondents.24 34
Time spent on EMR
Ten studies examined the relationship between the actual or perceived amount of time spent on EMR (both after hours and in general). Eight studies focused on analysing burnout related to time spent on EMR documentation after hours,7 12 16–18 28 29 32 and two looked at general time spent on EMR and its association with HCP burnout.14 21 Of the eight studies examining after hours EMR use, all studies found a significant association between burnout and use of EMR after hours (spending a high amount of time on EMR at home, spending 6 or more hours weekly, or more than 1.5 hours on EMR outside the work day). Two studies examined the associations between general EMR use and burnout and demonstrated mixed results when assessing this relationship. Somerson et al found that use of EMRs for more than 20 hours per week was associated with higher burnout.21 On the other hand, McPeek-Hinz et al found that a higher number of days spent using the EMR system was associated with less likelihood of burnout.14 Finally, three studies evaluated the subjective marker of insufficient documentation time, and its association with burnout.16 29 32 All three papers found that HCPs who reported insufficient time for documentation were more likely to experience burnout.16 29 32 In general, most of the studies that examined the relationship between time spent on EMR and burnout found a strong association between the two.
Message and alert load
Four studies examined the relationship between in-basket messages and/or EMR alert load on HCP burnout. In-basket messages are a component of EMRs where HCPs can communicate with their colleagues, similar to an email platform. Messages can be sent to individual recipients as well as groups and can be associated with a specific patient chart. Tai-Seale et al found that receiving more than the average number of system generated in-basket messages was associated with a 40% higher probability of burnout.22 Two studies also found that a high volume of patient call messages was associated with higher odds of burnout. One study reported an adjusted OR (aOR) using general burnout (aOR 3.81, 95% CI 1.44 to 10.14, p=0.007),33 and the other reported there was an OR of 6.17 between the exhaustion dimension of burnout and the highest quartile of messaging volume.31 Subjective, or perceived, alert load was correlated with the physical fatigue dimension of burnout, but objective, or actual, alert load was not correlated with any dimensions of burnout.31 Despite the differences in study design and methodology, these four studies demonstrate a trend indicating that the alert or message load on EMR is generally associated with HCP burnout.
Organisational support
One study assessed the impact of organisational support related to EMR.28 This study identified that physicians who reported that their organisation had done a great job with EMR implementation, training and support were two times as likely to report lower levels of burnout than those that disagreed.28
Interventions
Two included studies implemented interventions to address burnout related to EMR use. The first intervention in Sieja et al was team based, wherein 11-member teams worked with clinic leaders for 2 weeks to optimise onsite EMR and workflow.19 Teams were comprised of Medical Doctors, Doctors of Osteopathic Medicine, Nurse Practioners, Physician Asistants, midwifes, Registered Nurses, Medical Assistants and clinical staff, with results undelineated by profession. The intervention included EMR training for HCPs and staff, developing specialty-specific EMR tools and restructuring teamwork.19 Burnout was measured, using the MBI, 60 days before and 2 weeks after the completion.19 No significant reduction in burnout was seen after the intervention, with 47/119 (39%) of participants reporting burnout before and 37/107 (34%) after the intervention (p=0.434).19 The second study by Simpson et al similarly conducted 2 weeks of intensive EMR training, personalisation and system configuration in an inpatient setting.20 Baseline burnout was measured using questions from the Emotional Exhaustion Scale, Emotional Recovery Scale and Emotional Thriving Scale.20 Re-evaluation was completed 2 weeks after the 2-week training.20 A significant change was also not observed in these advanced providers in any of the three scales used.20
Discussion
In this scoping review, we explored the factors related to EMR that are related to burnout in HCPs (physicians, NPs and RNs) and interventions that have been implemented to address these factors. The research synthesised supports a positive correlation between EMR utilisation and perceived provider burnout, with no current intervention succeeding in reducing burnout symptoms related to use of EMRs.
Time spent on EMRs was found to be a strong indicator of burnout among providers. Despite this prevalent theme, there was no available data that discussed possible time-saving interventions, such as employing scribes, to decrease provider hours spent on EMR.36 Furthermore, only one included study addressed perceived support from their organisation in EMR implementation and training. Providers must be able to rely on organisations to provide the necessary resources to assist in administrative duties, to efficiently train clinicians and staff, and make improvements to increase workflow efficiency. Most importantly, providers must believe firmly that organisations value their health and well-being.37 In addition, evidence has shown that there is benefit in reducing burnout in individual-focused strategies such as engaging in mindfulness and small group discussions.38 However, no combined individual and organisational approach has not been studied, especially in the context of EMR-specific burnout in HCPs.39
Alert or message load on EMR was consistently associated with HCP burnout along with sentiments of poor EMR design. It is clear that the way providers use and interact with EMR interfaces and functions plays a crucial role in HCP burnout symptoms. It may then be hypothesised that EMR-related burnout may be mitigated by interventions that adopt a bottom-up model, which incorporate provider feedback, and empower clinician leaders to advance changes in EMR design, would certainly aid the expansion of EMR functionality and usability.39
The two included studies, which piloted team-based interventions, attempted to reduce burnout symptoms through additional intensive training of clinicians and staff. These studies found that there was no significant difference in participants’ reported burnout symptoms.
This study demonstrates the clear need for organisations to uncover the numerous factors that may be contributing to the burnout of their organisation’s HCPs, as each EMR system and organisation is nuanced and develop interventions that address these factors in full. It is not sufficient to approach one aspect of EMR-related burnout and not the others that are affecting provider wellness. This study reinforces the need for careful and innovative EMR development that actively works against the potential burnout that HCPs have experienced. Policy implications include ensuring HCPs are a large part of decision-making and prototyping of EMRs in healthcare organisations, in order to reduce the risk of EMR-related burnout before it occurs.
While other studies may have investigated similar associations as ours, we believe that our review has significant strengths, including highlighting the lack of research on the impact of organisation support on EMR-related HCP burnout and on the paucity of interventions attempted to address this issue. Wong et al’s rapid review focused on EMR-related burnout among HCPs in the USA and found similar results to this article but was not able to explore interventions proposed for this issue or the impact of organisational support on HCP burnout.8 Yan et al’s systematic review was also able to identify key EMR-related factors related to burnout, including insufficient time for documentation, high inbox volumes and negative perspectives.9 Both articles contributed significantly to the literature; however, they did not explore the association of interventions and organisational support on high levels of HCP burnout like ours. The EMR experience encompasses more than just time spent on the EMR or cumbersome EMR interfaces. Health and well-being are multifaceted for providers at all organisations, levels and stages of training. It was important for our team to call attention to the sparse data available on perceived organisational support, which, to our knowledge, has not previously been studied adequately.
Limitations of this paper include the heterogeneity of the reporting of the data precluding a formal meta-analysis. In addition, all included studies, aside from the two intervention studies, were cross-sectional surveys, which created inherent biases in the data including sampling bias, non-response bias and recall bias.40 Furthermore, the methods of these papers cannot imply causality. The data presented in this scoping review outline that EMR-related HCP burnout is a major problem across multiple fields, but there is a paucity of information on rigorous strategies to combat EMR-related HCP burnout.
This review suggests a strong association between EMRs and HCP burnout. Future research must now be focused on identifying strategies to effectively enhance coping strategies of HCP who are combating EMR-related burnout through large cohort studies and randomised controlled trials. Furthermore, our team was unable to distinguish burnout differences among different types of HCPs as this information was not delineated in the studies assessed, thus, future studies should explore HCP-specific burnout to allow for targeted interventions at each level. In addition, research is needed to focus on solutions that align with the patient-oriented goals that HCPs have, to ensure that EMRs serve their original purpose of improving and streamlining patient care, without acting as a significant burden on the mental health of HCPs.
Conclusion
EMR use should be considered a contributor to HCP burnout by organisational leaders and research scholars. With EMRs rapidly surpassing paper charting in most clinical settings, providers must feel confident that EMRs act as a helpful and comprehensive tool in their everyday practice, and not a burden that must be wielded ineffectively. Robust interventions are needed to address time spent on EMRs, EMR design and organisational support of clinicians and staff.
Supplementary Material
Footnotes
Twitter: @SriharanAbi
Contributors: CL and CP contributed equally to this publication and are listed as co-first authors. All authors conceptualised and designed the review. CL and CP reviewed titles, abstracts and full-text papers for eligibility. DTK extracted data, and all data extraction was verified by CL and CP. CL, CP and DK prepared the initial draft manuscript. AS reviewed and edited the manuscript and serves as the guarantor accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: This project is funded through a Knowledge Synthesis grant from the Canadian Institute for Health Research.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer-reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This scoping review was completed using secondary data and was, therefore, exempt from requiring research ethics board approval.
References
- 1.Schaufeli WB, Bakker AB, Hoogduin K, et al. On the clinical validity of the maslach burnout inventory and the burnout measure. Psychol Health 2001;16:565–82. 10.1080/08870440108405527 [DOI] [PubMed] [Google Scholar]
- 2.Dyrbye LN, Satele D, Shanafelt T. Ability of a 9-Item well-being index to identify distress and stratify quality of life in US workers. J Occup Environ Med 2016;58:810–7. 10.1097/JOM.0000000000000798 [DOI] [PubMed] [Google Scholar]
- 3.Qiao H, Schaufeli WB. The convergent validity of four burnout measures in a Chinese sample: a confirmatory factor-analytic approach 2010.
- 4.Halbesleben JRB, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev 2008;33:29–39. 10.1097/01.HMR.0000304493.87898.72 [DOI] [PubMed] [Google Scholar]
- 5.Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Available: https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460 [Accessed 24 Aug 2021].
- 6.Shah MK, Gandrakota N, Cimiotti JP, et al. Prevalence of and factors associated with nurse burnout in the US. JAMA Netw Open 2021;4:e2036469. 10.1001/jamanetworkopen.2020.36469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robertson SL, Robinson MD, Reid A. Electronic health record effects on work-life balance and burnout within the I3population collaborative. J Grad Med Educ 2017;9:479–84. 10.4300/JGME-D-16-00123.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong L. A rapid review of physician burnout secondary to electronic health records use in the United States from 2015 to 2020. Public Heal MPH Theses DrPH Diss 2020;276. [Google Scholar]
- 9.Yan Q, Jiang Z, Harbin Z, et al. Exploring the relationship between electronic health records and provider burnout: a systematic review. J Am Med Inform Assoc 2021;28:1009–21. 10.1093/jamia/ocab009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prospero . Registering a review on PROSPERO. Available: https://www.crd.york.ac.uk/prospero/#guidancenotes [Accessed 24 Aug 2021].
- 11.Jama Network Open . Instructions for authors, 2021. Available: https://jamanetwork.com/journals/jamanetworkopen/pages/instructions-for-authors#SecRatingsofQuality [Accessed 24 Aug 2021].
- 12.Adler-Milstein J, Zhao W, Willard-Grace R, et al. Electronic health records and burnout: time spent on the electronic health record after hours and message volume associated with exhaustion but not with cynicism among primary care clinicians. J Am Med Informatics Assoc 2020;27:531–8. 10.1093/jamia/ocz220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kutney-Lee A, Brooks Carthon M, Sloane DM, et al. Electronic health record usability: associations with nurse and patient outcomes in hospitals. Med Care 2021;59:625–31. 10.1097/MLR.0000000000001536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McPeek-Hinz E, Boazak M, Sexton JB, et al. Clinician burnout associated with sex, clinician type, work culture, and use of electronic health records. JAMA Netw Open 2021;4:e215686. 10.1001/jamanetworkopen.2021.5686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Melnick ER, Dyrbye LN, Sinsky CA, et al. The association between perceived electronic health record usability and professional burnout among US physicians. Mayo Clin Proc 2020;95:476–87. 10.1016/j.mayocp.2019.09.024 [DOI] [PubMed] [Google Scholar]
- 16.Olson K, Sinsky C, Rinne ST, et al. Cross-sectional survey of workplace stressors associated with physician burnout measured by the Mini-Z and the Maslach burnout inventory. Stress Health 2019;35:157–75. 10.1002/smi.2849 [DOI] [PubMed] [Google Scholar]
- 17.Peccoralo LA, Kaplan CA, Pietrzak RH, et al. The impact of time spent on the electronic health record after work and of clerical work on burnout among clinical faculty. J Am Med Inform Assoc 2021;28:938–47. 10.1093/jamia/ocaa349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharp M, Burkart KM, Adelman MH, et al. A national survey of burnout and depression among fellows training in pulmonary and critical care medicine: a special report by the association of pulmonary and critical care medicine program directors. Chest 2021;159:733–42. 10.1016/j.chest.2020.08.2117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sieja A, Markley K, Pell J, et al. Optimization Sprints: improving clinician satisfaction and teamwork by rapidly reducing electronic health record burden. Mayo Clin Proc 2019;94:793–802. 10.1016/j.mayocp.2018.08.036 [DOI] [PubMed] [Google Scholar]
- 20.Simpson JR, Lin C-T, Sieja A, et al. Optimizing the electronic health record: an inpatient sprint addresses provider burnout and improves electronic health record satisfaction. J Am Med Inform Assoc 2021;28:628–31. 10.1093/jamia/ocaa231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Somerson JS, Patton A, Ahmed AA, et al. Burnout among United States orthopaedic surgery residents. J Surg Educ 2020;77:961–8. 10.1016/j.jsurg.2020.02.019 [DOI] [PubMed] [Google Scholar]
- 22.Tai-Seale M, Dillon EC, Yang Y, et al. Physicians’ Well-Being Linked To In-Basket Messages Generated By Algorithms In Electronic Health Records. Health Aff 2019;38:1073–8. 10.1377/hlthaff.2018.05509 [DOI] [PubMed] [Google Scholar]
- 23.Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO study. J Am Med Inform Assoc 2014;21:e100–6. 10.1136/amiajnl-2013-001875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tajirian T, Stergiopoulos V, Strudwick G, et al. The influence of electronic health record use on physician burnout: cross-sectional survey. J Med Internet Res 2020;22:e19274. 10.2196/19274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tiwari V, Kavanaugh A, Martin G, et al. High burden of burnout on rheumatology practitioners. J Rheumatol 2020;47:1831–4. 10.3899/jrheum.191110 [DOI] [PubMed] [Google Scholar]
- 26.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016;91:836–48. 10.1016/j.mayocp.2016.05.007 [DOI] [PubMed] [Google Scholar]
- 27.Melnick ER, Harry E, Sinsky CA, et al. Perceived electronic health record usability as a predictor of task load and burnout among US physicians: mediation analysis. J Med Internet Res 2020;22:e23382. 10.2196/23382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eschenroeder HC, Manzione LC, Adler-Milstein J, et al. Associations of physician burnout with organizational electronic health record support and after-hours charting. J Am Med Inform Assoc 2021;28:960–6. 10.1093/jamia/ocab053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc 2019;26:106–14. 10.1093/jamia/ocy145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Giess CS, Ip IK, Cochon LR, et al. Predictors of self-reported burnout among radiology faculty at a large academic medical center. J Am Coll Radiol 2020;17:1684–91. 10.1016/j.jacr.2020.01.047 [DOI] [PubMed] [Google Scholar]
- 31.Gregory ME, Russo E, Singh H. Electronic health record alert-related workload as a predictor of burnout in primary care providers. Appl Clin Inform 2017;8:686–97. 10.4338/ACI-2017-01-RA-0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harris DA, Haskell J, Cooper E, et al. Estimating the association between burnout and electronic health record-related stress among advanced practice registered nurses. Appl Nurs Res 2018;43:36–41. 10.1016/j.apnr.2018.06.014 [DOI] [PubMed] [Google Scholar]
- 33.Hilliard RW, Haskell J, Gardner RL. Are specific elements of electronic health record use associated with clinician burnout more than others? J Am Med Inform Assoc 2020;27:1401–10. 10.1093/jamia/ocaa092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kroth PJ, Morioka-Douglas N, Veres S, et al. Association of electronic health record design and use factors with clinician stress and burnout. JAMA Netw Open 2019;2:e199609. 10.1001/jamanetworkopen.2019.9609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zumbrunn B, Stalder O, Limacher A, et al. The well-being of Swiss general internal medicine residents. Swiss Med Wkly 2020;150:w20255. 10.4414/smw.2020.20255 [DOI] [PubMed] [Google Scholar]
- 36.Corby S, Ash JS, Mohan V, et al. A qualitative study of provider burnout: do medical scribes hinder or help? JAMIA Open 2021;4:1–8. 10.1093/jamiaopen/ooab047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rhoades L, Eisenberger R. Perceived organizational support: a review of the literature. J Appl Psychol 2002;87:698–714. 10.1037/0021-9010.87.4.698 [DOI] [PubMed] [Google Scholar]
- 38.West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016;388:2272–81. 10.1016/S0140-6736(16)31279-X [DOI] [PubMed] [Google Scholar]
- 39.O'Malley AS, Grossman JM, Cohen GR, et al. Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med 2010;25:177–85. 10.1007/s11606-009-1195-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mann CJ. Observational research methods. Research design II: cohort, cross sectional, and case-control studies. Emerg Med J 2003;20:54–60. 10.1136/emj.20.1.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-060865supp001.pdf (73.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.