Abstract
Background
Endoscopy has long been widely used to screen for esophageal varices (EV) in cirrhotic patients. Recurrent endoscopy is a significant burden for the healthcare system of the endoscopic unit as well as uncomfortable and high costs for patients. This study intended to prognosticate Right Liver Lobe Diameter/Serum Albumin Ratio (RLLD/Alb) as a non‐invasive approach in the early diagnosis of EV among chronic liver disease (CLD) Bangladeshi patients enrolled in a specific hospital.
Participants and Methods
A total of 150 admitted patients with CLD were included in the study. Patients were subjected through a comprehensive biochemical checkup and upper digestive endoscopic or ultrasonographic inspection. The correlation was evaluated between the RLLD/Alb ratio and esophageal varices grades.
Results
The upper digestive endoscopy demonstration among 150 patients resulted in no EV in 18%, while 24% of patients was identified as EV grade I, 20% as grade II, 20% as grade III, and 18% patients as grade IV. The mean value of the RLLD/Alb ratio was 4.89 ± 1.49 (range from 2.30 to 8.45). The RLLD/Alb ratio diagnosed the EV employing the cut‐off value of 4.01 with 85.3% sensitivity and 68.8% specificity. Furthermore, it was positively correlated with the grading of EV, when this ratio increased the grading of EV increases and vice versa (r = 0.630, p < 0.001).
Conclusion
The RLLD/Alb ratio is a non‐invasive parameter giving exact guidance relevant to the ascertainment of the existence of EV and their grading in chronic liver disease patients.
Keywords: esophageal varices (EV), liver cirrhosis, right liver lobe diameter/serum albumin ratio, ultrasonography, upper digestive endoscopy
Endoscopy, an invasive and expensive way of diagnosing esophageal varices (EV) in cirrhotic patients, which imposing a burden on the healthcare system due to the necessity of recurrent testing with unpleasant experiences. Here, we have assessed the potentiality of RLLD/Alb ratio, a non‐invasive and low cost method of precise predictability and reliability of classifying esophageal varices grade. The present study reveals RLLD/Alb ratio as a promising non‐invasive diagnostic marker of esophageal varices, which would be a fundamental tool for exhaustive variceal care.

1. INTRODUCTION
Chronic liver disease (CLD) eventually leads the way to develop liver cirrhosis for which portal hypertension is a major impediment. 1 , 2 Hepatocellular injury–mediated fibrosis and nodular formation cause liver cirrhosis, which has appeared to be a major burden in global health management. Inadequate information of CLD, liver diseases together with limited small‐scale institutional‐based studies, indicate that the number of people suffering from liver disease in Bangladesh is increasing at an alarming rate. Among them, 37%–69% of patients are suffering from CLD. As the burden of advanced liver disease is steadily rising, complications of cirrhosis and related rates of mortality are also increasing. 3 , 4
Esophageal varices (EV) is a serious complexity, happening in portal hypertension, with an incidence scenario of developing in cirrhotic patients is around 60%–80%. 5 Bleeding from EV happens in 20%–40% of liver cirrhotic patients, while that is highly correlated with morbidness and fatality. Initial bleeding from EV is reported to be fatal for up to 30% of cases, and 70% of patients face re‐bleeding episodes, those who are left untreated with a mortality rate of 35%. 6 , 7
Early detection and adequate treatment measures would be a great strategy to minimize a significant mortality rate due to EV‐mediated bleeding. Hence, the current guideline for all cirrhotic patients is to undergo an endoscopic examination to identify the plausibility of bleeding so that patients can be immediately treated with prophylactic therapy. 8 It is suggested that patients with proper liver function and without varices should be screened every 2 years and each year for patients with signs of deteriorated liver function endoscopically. 9 Resultantly, a substantial portion of patients may not have suffered from EV 10 years following the detection of cirrhosis. Therefore, repeated, uncomfortable, and costly endoscopy in cirrhotic patients would be a significant burden. 10 Additionally, endoscopy is an invasive procedure which involves some sedation effects that may further develop complications in cirrhotic patients. 11 Furthermore, invasive procedures for diagnostic purposes like endoscopy can augment the onset of bacterial diseases in cirrhotic patients. 12 As a result, several non‐invasive approaches including right liver lobe diameter (RLLD)/albumin ratio, left liver lobe diameter (LLLD)/albumin ratio, and platelet count/spleen diameter (PC/SD) ratio have been investigated as a substitute to endoscopic examination in patients with a poor chance of developing varices. These methods for the prediction of EV are simple to perform, low cost, and non‐invasive due to their requirement of ultrasonography and biochemical tests, which can be regularly executed in patients with liver cirrhosis. 13
Alempijevic T et al. showed that RLLD/Alb ratio as a non‐invasive way to predict the EV which can easily obtained by performing an ultrasonography and measuring serum albumin concentration. 14 , 15 Afterward, several studies have been carried out to validate this ratio as a diagnostic tool which found to be same. 16 , 17 , 18 , 19 Since cirrhotic patients might have different clinical backgrounds prior to introducing a biological marker, the external validity and reproducibility should be evaluated in a cohort of the Bangladeshi population. However, to evaluate the reproducibility of the RLLD/serum albumin ratio as a non‐invasive strategy of diagnosing EV in cohorts of Bangladeshi patients is yet to be published. In this context, this study was performed to reinforce the RLLD/Alb as a promising tool of EV in the Bangladeshi CLD patients.
2. MATERIALS AND METHODS
A descriptive cross‐sectional study was executed at the Department of Gastroenterology, Chittagong Medical College Hospital, Chattogram‐4203, Bangladesh, throughout 1st January 2019 to 30th September 2021 with the approval from the Ethical Review Committee of CMCH and after getting approval from the Research and Training Monitoring Department of Bangladesh College of Physicians and Surgeons (BCPSs).
2.1. Patients, data collection, and experiment
Patients with previous variceal bleeding, hepatocellular carcinoma (HCC), renal disease, portal vein thrombosis, pulmonary disease, primary hematological diseases, unstable or critical cardiovascular disorders, HIV infection, coexistent illness or infection, history of undergoing band ligation/injection sclerotherapy/surgery for EV, history of receiving vasoactive agents or beta blockers, and contraindicated endoscopy for upper gastrointestinal tract (UGIT) were omitted from the study. Patients confirmed with clinical or biochemical examination and abdominal ultrasound evaluation were enrolled in the study. Consent was taken from the patients included in the study.
Non probability sampling techniques were applied in collecting data from all patients who were admitted to indoor gastroenterology ward of CMCH with defined liver cirrhosis. In the study, consecutive patients were enrolled considering the exclusion and inclusion criteria. After getting informed assent, all patients who were considered in our analysis were considered to be taking enumerated history and relevant clinical and laboratory examinations like concentration of serum albumin. Right liver lobe size in diameter (cm) was determined through the abdominal ultrasonography at the mid‐clavicular line by a consultant sonologist. Identification and grading of EV were carried out by UGIT endoscopy. 13 Child‐Pugh classification was also utilized to classify patients as A, B, and C grades. Data were accumulated employing a predetermined questionnaire.
2.2. Data processing and analysis
Acquired data were processed and further analyzed using either SPSS v23 or Microsoft Office Excel. Data were represented as range, frequency, percentage, mean ± standard deviation (SD), and proportion based on the types of variables, when appropriate. Chi‐square test and a one‐way analysis of variance (ANOVA) were executed for data analysis. A receiver operator characteristic (ROC) analysis was performed to classify the area under curve (AUC) and diagnostic marker–associated optimum cut off value for determining the sensitivity, specificity, and accuracy. The correlation between grading of EV and RLLD/Alb ratio was revealed by determining correlation coefficient ® using Spear’an's test (non‐parametric correlation). p value <0.05 was addressed as statistically meaningful.
3. RESULTS
Out of 150 patients, 90 were males and the rest of the patients were female. The age of the study population ranged from 25–84 years, with a mean ± SD age of 55.11 ± 11.78 years, while older age patients belonged to half of them. The clinical outcomes of the study subjects are shown in Table 1. In our study population, patients with grade I EV were 36 (24.0%). In addition, patients with grade II, III, and IV found to be the same in number as 30 (20.0%) and grade 0 (no varices) was identified in 27 patients (18.0%).
TABLE 1.
Clinical and epidemiological outcomes in the study population (n = 150)
| Variables | Percentage (%) | |
|---|---|---|
| Age (years) | ||
| Ranges | 25–84 | ‐ |
| 25–40 | 15 | 10 |
| 41–59 | 66 | 44 |
| ≥60 | 69 | 46 |
| Mean ± SD | ||
| Gender | ||
| Male | 90 | 60 |
| Female | 60 | 40 |
| Aetiology of CLD | ||
| HBV | 105 | 70 |
| HCV | 15 | 10 |
| Non B Non C | 30 | 20 |
| Esophageal varices grade | ||
| Grade‐0 | 27 | 18 |
| Grade‐ I | 36 | 24 |
| Grade‐ II | 30 | 20 |
| Grade‐ III | 30 | 20 |
| Grade‐ IV | 27 | 18 |
| Child‐Pugh grades | ||
| Grade‐A | 72 | 48 |
| Grade‐B | 54 | 36 |
| Grade‐C | 24 | 16 |
| Right liver lobe diameter (cm) (Mean ± SD) | 11.44 ± 1.97 | ‐ |
| Serum albumin level (mg/dl) Mean ± SD | 3.02 ± 0.58 | ‐ |
Abbreviations: CLD, chronic liver disease; cm, centimeter; HBV& HCV, hepatitis B & C virus; mg/dl, milligram/deciliter; SD, standard deviation.
The number of patients with Child‐Turcotte‐Pugh (CTP) grades A, B, and C was observed to be 72 (48%), 54 (36%), and 24 (16%), respectively (Table 1). The RLLD (Mean ± SD) was 11.44 ± 1.97 cm with 7 cm and 16 cm as the minimum and maximum values, respectively (Table 1). Serum albumin (Mean ± SD) level was found 3.02 ± 0.58 mg/dl showing the minimum and maximum values like 1.5 and 4.5 mg/dl, respectively (Table 1).
The mean value of the RLLD/Alb ratio was 4.89 ± 1.49 (mean ± SD) with 2.30 as minimum and 8.45 as the maximum value (Ref. table). Grade 0/I/II/III/IV of EV in patients exhibited the mean RLLD/Serum albumin ratio value as 3.50 ± 0.59/4.12 ± 1.10/4.81 ± 1.04/5.63 ± 1.41/6.58 ± 1.12 (Table 2).
TABLE 2.
RLLD/Alb. ratio in different varices grade of CLD patients (n = 150)
| Esophageal varices (EV) grade | Mean ± SD | p value* |
|---|---|---|
| Grade 0 | 3.50 ± 0.59 | |
| Grade I | 4.12 ± 1.10 | |
| Grade II | 4.81 ± 1.04 | 0.001 |
| Grade III | 5.63 ± 1.41 | |
| Grade IV | 6.58 ± 1.12 |
Derived F (ANOVA) test.
Our data show an increased ratio pattern in the patients with EV in comparison with the patients without EV (p < 0.001) (Ref. tab/fig). The RLLD/Alb ratio was also noticed to be substantially elevated with the increasing EV grades in the study population (Figure 1). Additionally, the RLLD/serum albumin ratio and grade of EV exhibited a substantial positive correlation (r = 0.630, p < 0.001). Notably, the RLLD/Alb ratio was found to be elevated as more progressed liver diseases, considering with the Child Pugh class scoring of the study population (Figure 2). Furthermore, a strong positive correction was found among RLLD/albumin ratio and grading of OV (r = 0.630, p < 0.001) (Figure 3). As an additional analysis, the receiver operating characteristic (ROC) curve was constructed to figure out the sensitivity, specificity, positive and negative predictive value (PPV & NPV), and accuracy of prediction of EV based on RLLD/Alb ratio (Figure 4), which was 85.3%, 68.8%, 85.3%, 68.8%, and 80.0%, respectively, at the best cut‐off value of 4.01 and area under ROC curve (AUC) was 0.777 (95% CI: 0.631–0.925; p ≤ 0.001).
FIGURE 1.
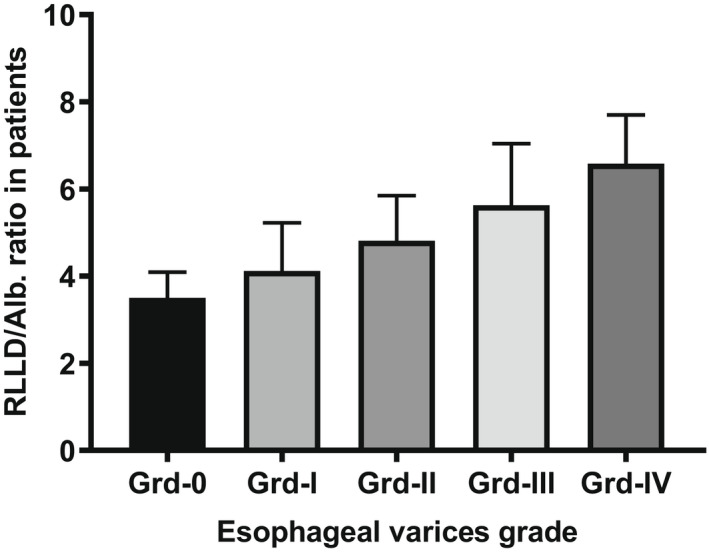
RLLD/Serum albumin ratio in patients with esophageal varices (p ≤ 0.001)
FIGURE 2.
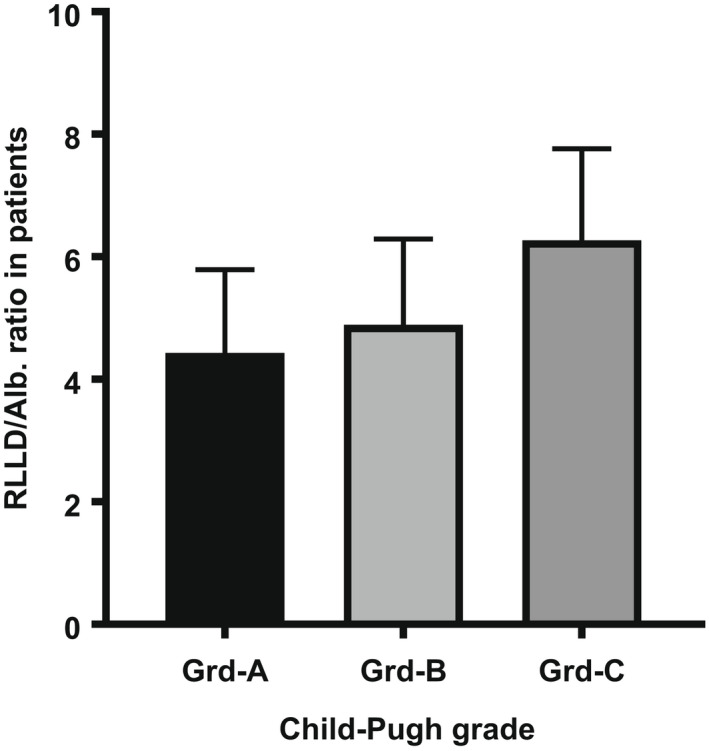
RLLD/Serum albumin ratio in patients with different Child‐Pugh classification (p = 0.008)
FIGURE 3.
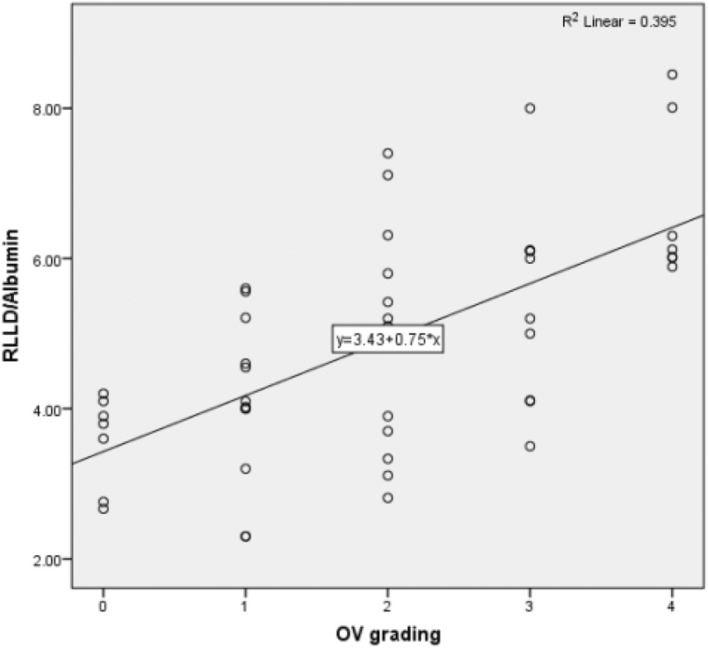
Correlation between RLLD/serum albumin ratios in 150 CLD patients
FIGURE 4.
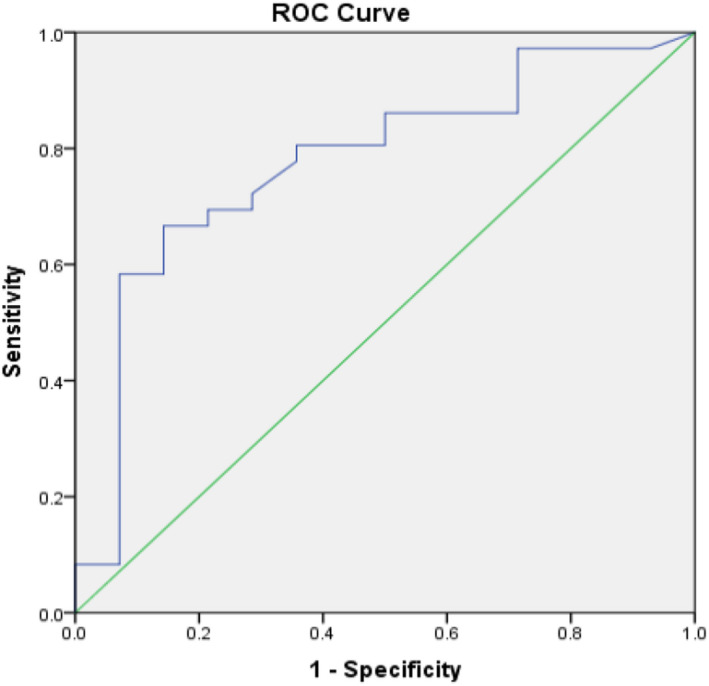
Evaluating the RLLD/Alb ratio as a diagnostic marker for ensuring the presence of EV through the analysis of ROC (Receiver Operating Characteristic) curve
4. DISCUSSION
Liver diseases including fatty liver, cirrhosis, or malignancy are being a major health burden in the developing world, and the rate of varices is raising because of alcohol intake, obesity, or some other causative reasons. Hazardous bleeding from varices is a serious complexity which is related with considerable disease activity and death. Also, this can negatively impact the health care system. Regardless of the improvement of endoscopic and clinical medicines, early mortality due to variceal draining remaining parts is high because of critical illness of the patient. Hence, the prevention of varices bleeding associated with EV is indispensable.
The distinguishing of patients with the beginning of variceal bleeding is a crucial stride in bleeding restrainment and categorize patients who should be given prophylactic treatment. Prediction of EV considering noninvasive approaches has obtained considerable attention, and numerous investigations have been carried out to invent noninvasive parameters to facilitate the anticipation of EV in CLD patients with an objective of declining cost and burden on endoscopy. 20 In our study, there were 123 (82%) patients with EV who were included, which was consistent with previously reported studies from different countries like Pakistan, India, Serbia, and Egypt. 14 , 18 , 21 , 22 In accordance with the previous study, 14 , 22 the grading of Child‐Turcotte‐Pugh, we noticed that patients with grade A were 72 (48%), which was followed by grade B (54, 36%), and grade C (24, 16%). Alempijevic et al. 15 identified 22.3%, 33%, 16%, and 4.3% of the patients with grade I, II, III, and IV esophageal varices, respectively, and 24.5% of the patients with no esophageal varices with an upper GI endoscopy examination. In contrast, in the present study, 36 (24.0%) patients had EV grade I, followed by 30 (20.0%) patients with grade II and grade III EV each. Grade IV EV was found in 27 (18.0%) patients along with that there were 27 (18.0%) of patients with grade 0 or no varices. In 2007, Alempijevic et al. 15 explored the RLLD/Alb ratio as a non‐invasive predictor of EV with the 83.1% and 73.9% as the sensitivity and specificity, respectively, using a cut‐off value of 44.25. In our investigation, the RLLD/Alb ratio also showed an increasing trend with the progressing grade of EV from I to IV, and a substantial positive correlation was also been seen among the ratio and grading. Sensitivity, specificity, positive and negative predictive value (PPV & NPV), and accuracy of the RLLD/Alb ratio were found to be 85.3%, 68.8%, 85.3%, 68.8% and 80.0%, respectively, at the best cut‐off value of 4.01. Several other studies 13 , 18 , 19 , 21 , 23 also investigated the potentiality of the RLLD/Alb ratio for noninvasively predicting the EV and explored a similar positive correlation, implying it as a promising noninvasive tool. Despite the promising outcomes and good correlation between the Right Liver Lobe Diameter/Serum Albumin Ratio (RLLD/Alb) ratio and grades of EV, endoscopy is yet the widely accepted and gold benchmark approach for diagnosing the EV, and the RLLD/Alb ratio yet cannot be an ideal alternative to endoscopy.
This prospective clinical study of non‐invasive diagnosis of esophageal varices (EV) using an ultrasound examination enables early prognosis of diseases and determination of safe and effective treatment strategies and appropriate follow‐up methods in hospital settings. In particular, the selection of proper treatment strategies as indicated by the consequences of the perception of esophageal varices should be carried out, which are believed to contribute in the advancement for patients with esophageal varices. Since this study was conducted in a territory‐based hospital, it does not represent the total scenario of the whole country. A multifaceted cohort study with large study populations is essential to find the health status regarding CLD patients with esophageal varices.
5. CONCLUSION
We found RLLD/Alb proportion and assessed simply serum albumin estimation and abdominal ultrasonography which enormously improved in the perception of esophageal varices, offering a promising, noninvasive approach by which diagnosis and quantitative grading might be accomplished. However, abdominal ultrasound examination has a few impediments, for example, operator reliance and a delay in absorbing information. Therefore, to completely apply the value of RLLD/Alb to clinical practice, it is important to standardize ultrasonography procedures and image interpretation. We believe that RLLD/Alb would be a fundamental tool for exhaustive variceal care.
AUTHOR CONTRIBUTION
Conceptualization: Md Faisal Fahad Chowdhury, Ashekul Islam, PhD; Pulak Kanti Palit. Supervision: Ashekul Islam, PhD. Investigation: Md Faisal Fahad Chowdhury, Ashekul Islam, PhD; Pulak Kanti Palit, Md. Mozibullah. Formal Analysis: Md Faisal Fahad Chowdhury, Ashekul Islam, PhD; Pulak Kanti Palit. Writing‐Original Draft Preparation: Md Faisal Fahad Chowdhury, Ashekul Islam, PhD; Pulak Kanti Palit, Md. Mozibullah, Md Sohel, Mst. Mahmuda Khatun. Writing‐Review & Editing: Md Faisal Fahad Chowdhury, Ashekul Islam, Pulak Kanti Palit, Md. Mozibullah, Md Sohel, Mst. Mahmuda Khatun, Mohammed Mehadi Hassan Chowdhury, Mohammod Johirul Islam, Joyonti Datta, Suman Dhar, Pradip Kumar Nath, Sabuj Kanti Nath. All authors have read and approved the final version of the manuscript, and the corresponding author had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
CONFLICT OF INTEREST
The author did not expose any conflict of interest.
TRANSPARENCY STATEMENT
The lead author confirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
ACKNOWLEDGEMENTS
We would like to thanks all the members of Gastroenterology and Medicine Department, Chittagong Medical College and Hospital, Chattogram‐4203, Bangladesh; for their cordial support.
Chowdhury MFF, Islam A, Palit PK, et al. RLLB/Alb ratio: a promising noninvasive diagnostic marker in assessing esophageal varices in cirrhotic patients. J Clin Lab Anal. 2022;36:e24589. doi: 10.1002/jcla.24589
Md Faisal Fahad Chowdhury and Ashekul Islam have contributed equally in the study
Funding information
There are no funding sources.
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the qualitative findings of this study are available within the article.
REFERENCES
- 1. Rye K, Scott R, Mortimore G, Lawson A, Austin A, Towards FJ. Noninvasive detection of oesophageal varices. Int J Hepatol. 2012;2012:343591. doi: 10.1155/2012/343591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ahmed S, Mumtaz K, Ahmed US, et al. Frequency and characteristic features of portal hypertensive gastropathy in patients with viral cirrhosis. J Coll Physicians Surg Pak. 2010;20(11):714‐718. [PubMed] [Google Scholar]
- 3. Rahman S, Faroque Ahmed M, Jamshed Alam M, et al. Distribution of liver disease in Bangladesh: a cross‐country study. Euroasian J Hepatogastroenterol. 2014;4(1):25‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mahtab M‐A. Epidemiology of viral hepatitis and liver diseases in Bangladesh. Euroasian J Hepatogastroenterol. 2015;5(1):26‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jensen DM. Endoscopic screening for varices in cirrhosis: findings, implications, and outcomes. Gastroenterology. 2002;122(6):1620‐1630. [DOI] [PubMed] [Google Scholar]
- 6. Stefanescu H, Procopet B. Noninvasive assessment of portal hypertension in cirrhosis: liver stiffness and beyond. World J Gastroenterol. 2014;20(45):16811‐16819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Of NH, Bleeding V, Of P, Bleeding V. Review indication of treatment for esophageal varices: who and when? 2006;(September 2005):10–5.
- 8. Garcia‐Tsao G, Bosch J, Groszmann RJ. Portal hypertension and variceal bleeding‐‐Unresolved issues. Summary of an American association for the study of liver diseases and European association for the study of the liver single‐topic conference. Hepatology. 2008;47:1764‐1772. [DOI] [PubMed] [Google Scholar]
- 9. Grace ND, Groszmann RJ, Garcia‐Tsao G, et al. Portal hypertension and variceal bleeding: an AASLD single topic symposium. Hepatology. 1998;28:868‐880. [DOI] [PubMed] [Google Scholar]
- 10. D'Amico G, Morabito A. Noninvasive markers of esophageal varices: another round, not the last. Hepatology. 2004;39:30‐34. [DOI] [PubMed] [Google Scholar]
- 11. McGuire BM. Safety of endoscopy in patients with end‐stage liver disease. Gastrointest Endosc Clin N Am. 2001;11(1):111‐130. [PubMed] [Google Scholar]
- 12. Almeida D, Lopes AA, Santos‐Jesus R, Paes I, Bittencourt H, Paraná R. Comparative study of bacterial infection prevalence between cirrhotic patients with and without upper gastrointestinal bleeding. Braz J Infect Dis. 2001;5(3):136‐142. [DOI] [PubMed] [Google Scholar]
- 13. Charan S, Garg R, Chander R, et al. A comparative evaluation of liver lobe size/albumin ratio and platelet count/spleen diameter ratio as non‐invasive predictors of oesophageal varices in patients with liver cirrhosis. J Evol Med Dent Sci. 2017;6(23):1858‐1867. [Google Scholar]
- 14. Alempijevic T, Bulat V, Djuranovic S, et al. Right liver lobe/albumin ratio: contribution to non‐invasive assessment of portal hypertension. World J Gastroenterol. 2007;13(40):5331‐5335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alempijevic T, Kovacevic N. Right liver lobe diameter: albumin ratio: a new non‐invasive parameter for prediction of oesophageal varices in patients with liver cirrhosis (preliminary report). Gut. 2007;56(8):1166‐1167. [PMC free article] [PubMed] [Google Scholar]
- 16. Ahmed S, Sarwar N, Hafeez S, Abbas N, Akram N, Ahmed R. Diagnostic accuracy of right liver lobe diameter/albumin ratio for non‐invasive detection of oesophageal varices in hepatitis C related cirrhosis. Age (in years). 18(50):51–80. [Google Scholar]
- 17. El Ray A, Azab MM, El‐Aziz IM, et al. Non‐invasive predictors for the presence, grade and risk of bleeding from esophageal varices in patients with post‐hepatitic cirrhosis. J Egypt Soc Parasitol. 2015;45(2):421‐428. [DOI] [PubMed] [Google Scholar]
- 18. Esmat S, Omarn D, Rashid L. Can we consider the right hepatic lobe size/albumin ratio a noninvasive predictor of oesophageal varices in hepatitis C virus‐related liver cirrhotic Egyptian patients? Eur J Intern Med. 2012;23(3):267‐272. [DOI] [PubMed] [Google Scholar]
- 19. Nouh MA, El‐Hamouly MS, Mohamed SA, Metwally AYH. Right liver lobe diameter/serum albumin ratio in the prediction of esophageal varices in cirrhotic patients. Menoufia Med J. 2019;32(3):1113. [Google Scholar]
- 20. Giannini E, Botta F, Borro P, et al. Platelet count/spleen diameter ratio: proposal and validation of a non‐invasive parameter to predict the presence of oesophageal varices in patients with liver cirrhosis. Gut. 2003;52(8):1200‐1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Akram M, Soomro MH, Magsi M. The right liver lobe size/albumin concentration ratio in identifying esophageal varices among patients with liver cirrhosis. Middle East J Dig Dis. 2019;11(1):32‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mandhwani R, Hanif FM, Haque MMU, Wadhwa RK, Luck NH, Mubarak M. Noninvasive clinical predictors of portal hypertensive gastropathy in patients with liver cirrhosis. J Transl Int Med. 2017;5(3):169‐173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Salem MNE, Elhawary MAA, Abdallah SR, Khedr MAHB. Role of right liver lobe diameter/serum albumin ratio in esophageal varices assessment in cirrhotic patients. Egypt J Hosp Med. 2018;73(7):7112‐7118. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the qualitative findings of this study are available within the article.


