Abstract
Histoplasma capsulatum is the most common cause of endemic mycosis in developing countries. It is a self-limited and asymptomatic disease in immunocompetent individuals but remains a frequent cause of opportunistic infection in patients with compromised immune status. Liver involvement as a part of disseminated histoplasmosis is well known. However, liver infection as a primary manifestation of histoplasmosis without evidence of primary lung involvement is rare. In conclusion, clinicians should be aware of isolated histoplasmosis affecting the hepatobiliary system, and careful evaluation is warranted to confirm the diagnosis. Given the appropriate clinical context, histoplasmosis should be considered in both immunocompetent and immunocompromised patients, regardless of pulmonary symptoms, in non endemic as well as endemic areas.
Keywords: Histoplasma capsulatum, Histoplasmosis, Hepatic manifestation, Mycosis
Introduction
Histoplasmosis is a systemic fungal disease that is caused by the dimorphic fungus Histoplasma capsulatum, which usually infects an individual by way of the respiratory tract. Cases comprise two distinct groups of conditions—the subcutaneous and systemic mycoses. The fungal infection has recently emerged as an important opportunistic infection among immunocompromised patients living in endemic areas for this fungus, and are prone to develop more severe disease.1
Epidemiology
Histoplasmosis is distributed worldwide but endemic in the Americas, Africa, and Asia. The actual incidence of histoplasmosis is not known, as the majority of the studies done on this subject have been limited to regions affected by outbreaks of the disease. Globally, about half a million people get infected with Histoplasma infection every year. However, approximately 100,000 people develop disseminated histoplasmosis,2 which is associated with high mortality rates (ranging between 30–50% if treated and 100% if not).3–5 In North America, the area of highest endemicity is in the Mississippi and Ohio River Valleys of the USA. In these areas, the incidence of histoplasmosis reaches up to an estimated 6.1 cases per 100,000.6,7 Through a 2011–2014 surveillance of cases in the USA, state-specific annual incidence rates were found to range from 0 to 4.3/100,000 population.8
A recent systematic literature review of both case volume and type of histoplasmosis in Southeast Asia, excluding the Indian sub-continent, found a total of 407 cases.9 Most cases (255 (63%)) were disseminated histoplasmosis.9 The highest burden of histoplasmosis was noted in Myanmar, Bali, and Surabaya in Indonesia, Ho ChiMinh City in Vietnam, southern Thailand, and north Luzon in the Philippines. In the East African region, a study from Northern Tanzania retrospectively identified 9 (0.9%) cases of probable histoplasmosis among 970 febrile in-patients.10
In Bangladesh, all variants of fungal infections are tracked and some studies have documented their frequency. In a study of 3,435 patients attending a dermatology clinic, 601 (17.5%) were diagnosed with superficial fungus infections.11 Deep mycoses are also an important evolving problem, as evidenced by reports of 16 cases of histoplasmosis with varying clinical manifestations.12,13 Isolated hepatic histoplasmosis is an uncommon condition; liver involvement is commonly associated with disseminated histoplasmosis. H. capsulatum has been recovered from soil of the Gangetic plains.14 When soil is disturbed by construction or excavation, the spores become airborne and are then inhaled.15 Considering the likeness of geo-climatic conditions, it is possible that many more cases of histoplasmosis occur in Bangladesh than are currently documented.
Pathogenesis
Upon inhalation of airborne spores, once they reach the alveoli, they convert to a yeast form, which is the tissue-invasive form. The current multiplying yeasts are then phagocytosed by alveolar macrophages, that are initially incapable of killing the fungus. The ingested yeasts multiply inside the macrophages and during the pre-immune phase of the illness, and they are then spread throughout the body via the lymphatics to organs rich in reticuloendothelial cells.16 Hematogenous dissemination usually occurs before cellular immunity develops, during the first 2 weeks.17 In an immunocompetent host, once sufficient cell-mediated immunity develops, the infection is eliminated by cytokines (e.g., interferon-γ and interleukin-12) which aid macrophages in either killing the organism or halting their progression by forming a calcified granuloma.18 In immunosuppressed patients, especially those with defective cell-mediated immunity, these defense mechanisms are impaired, causing reactivation of old foci or a progressive dissemination involving the extra-pulmonary tissues.19 The typical incubation period is 7–21 days.15
Predisposing factors
A variety of conditions can predispose to disseminated histoplasmosis, such as immunocompromised condition (i.e. acquired immune deficiency syndrome (AIDS)), taking of immunosuppressive medications (i.e. glucocorticoids, anti-rejection therapies in solid organ transplantation, or TNF-α inhibitor therapies), primary immunodeficiency, and extremes of age.20–22
Clinical features
Histoplasmosis can present in various forms, including:
Asymptomatic primary infection
Acute pulmonary histoplasmosis
Sequelae: mediastinal granuloma, rheumatologic syndromes, pericarditis
Chronic pulmonary histoplasmosis
Disseminated histoplasmosis
Other: mediastinal fibrosis, broncholithiasis, central nervous system histoplasmosis, gastrointestinal histoplasmosis, hepatic histoplasmosis.19,23
The most common symptoms of the disseminated forms are fever (89.1%), respiratory symptoms (38.1%), weight loss (37.4%), and various common signs, including splenomegaly (72%), hepatomegaly (68.1%) and lymphadenopathy (41.2%).24 Initial infection occurs in the lung alveoli, and then is transformed by the reticuloendothelial system and spread to various organs, resulting in progressive disseminated histoplasmosis.23
Hepatic histoplasmosis
Hepatic histoplasmosis can occur both in children and adults, in immunocompetent and immunocompromised patients, and in endemic and nonendemic areas.24 Hepatic involvement is frequent in disseminated histoplasmosis. The liver is reportedly involved in about 90% of patients with disseminated histoplasmosis.25 However, liver histoplasmosis as a primary sign of histoplasmosis without lung involvement is uncommon. Patients with primary liver involvement usually present with nonspecific symptoms, such as fever, fatigue, nausea, vomiting, weight loss, and elevation of liver enzymes. They may present with stigmata of chronic liver disease, portal hypertension, ascites, and/or varices. These features may be due to chronic parenchymal liver disease resulting from histoplasma-induced liver injury. The full spectrum of hepatic manifestations of this disease is unknown but spans the range in the literature from mildly abnormal liver enzymes to severe icteric cholestasis with fever and pain.24–26
H.capsulatum is an uncommon cause of granulomatous liver disease. There are few case reports on hepatic histoplasmosis with atypical presentations. Sartin et al.27 from the Mayo Clinic (Rochester, MN, USA) found histoplasmosis comprised 4.5% (4 of 88) of cases of idiopathic granulomatous disease. Cholestasis due to H. capsulatum in the setting of primary liver manifestation has been rarely detected. Only a few case reports of liver biopsy-proven histoplasmosis have reported associated cholestasis.25,28–30
The typical clinical presentations are fever and jaundice in the setting of immunosuppression. Right upper quadrant pain might be confused with biliary colic in cases of cholestatic hepatitis secondary to disseminated histoplasmosis.24 Clinically, these patients are usually symptomatic with elevated liver enzymes and pyrexia of unknown origin.31 There is one case report in the publicly available literature that describes a patient with acute cholestatic granulomatous hepatitis with disseminated histoplasmosis.24 Obstruction by peri-portal lymph nodes results in obstructive jaundice.20 Two case reports by Park et al.24 and Kothadia et al.30 describe patients who underwent laparoscopic cholecystectomy for uncertain etiology shortly before being diagnosed with disseminated histoplasmosis. Nahar et al.28 reported a patient with disseminated histoplasmosis that presented as chronic liver disease with portal hypertension.
Diagnosis
Disseminated histoplasmosis can be diagnosed using various methods, like antigen detection, cultures, serology, or direct microscopy. Recovery of the organism from a biologic extra-pulmonary specimen is the gold standard.16
Laboratory values are highly variable for this disease. Transaminase levels are usually above the upper limit of normal, and the elevated alkaline phosphatase level is often as high as >2,100 U/L. In addition, high total bilirubin is usually associated with a concomitant rise in direct bilirubin, and γ-glutamyl transpeptidase (GGT) is significantly elevated as demonstrated by the case reported by Gill et al.31 A liver biopsy is often obtained in conjunction with serum and urine antigen studies to establish the diagnosis.
The tissue response in histoplasmosis causes granulomas that are visible by histopathologic examinations. Grocott-Gomorimethenamine-silver nitrate and periodic acid-Schiff stains are useful for visualizing Histoplasma organisms in tissues. The early lesions in the tissue specimen contain a large number of macrophages and lymphocytes, with occasional epithelioid cells and multinucleated giant cells. Histological examination shows varying degrees of central caseation and occasionally calcification. Areas of caseous necrosis with a surrounding fibrous capsule which prevents the spread of the organism are characteristic. H. capsulatum may also be seen in tissues inside macrophages (Fig. 1).29 If features of portal hypertension are present, then esophagogastrodudenoscopy should be performed to identify and evaluate varices (Fig. 2).28
Fig. 1. Histopathological examination.
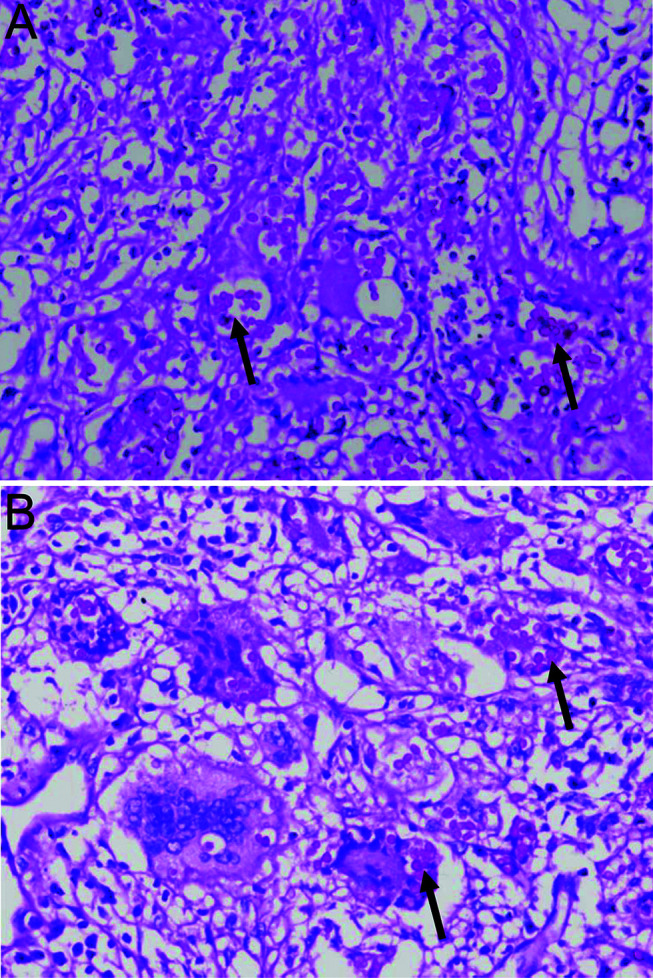
(A, B) Representative staining samples. Arrows indicate H. capsulatum.
Fig. 2. Large esophageal varices in a child with disseminated histoplasmosis.

Treatment
Prompt diagnosis and initiation of antifungal therapy are crucial in immunocompromised, who otherwise have a fatality rate of 100% if left untreated,8 The agents most commonly used for the treatment of histoplasmosis are amphotericin B and itraconazole. For moderately severe to severe disease, liposomal amphotericin B (3mg/kg/day) is suggested for 1–2 weeks, followed by oral itraconazole (200mg thrice daily for 3 days and then 200mg twice daily for a total of at least 12 months). Liposomal formulation is preferred to deoxycholate, due to its superior side effect profile, better response rate, and survival benefit. Patients with mild-to-moderate disease can be treated with itraconazole.30
Monitoring
Antigen levels in urine can be used to monitor the response to treatment. Antigen levels usually decline by the end of 12 weeks, and more rapidly in serum than in urine. Most of the decline in antigen level was seen in the first 2 weeks of therapy.32 An increase in antigen concentration indicates relapse or treatment failure, and further evaluation of the adequacy of treatment is needed.22
Conclusions
The liver is involved in about 90% of patients with disseminated histoplasmosis. Hepatic histoplasmosis can present as granulomatous hepatitis, as stigmata of chronic liver disease, portal hypertension, comprising ascites or varices, or with elevated liver enzymes. The most common hepatic finding seen on liver biopsy is portal lymphohistiocytic inflammation. Discrete hepatic granulomas are found in less than 20% cases of involved livers. There are limited case reports of disseminated histoplasmosis presenting as primary hepatic histoplasmosis. A high clinical suspicion is warranted in patients who present with stigmata of chronic liver disease and portal hypertension with no evidence of cirrhosis, especially if the person lives in or has visited an endemic area.28
Abbreviations
- AIDS
acquired immune deficiency syndrome
- GGT
γ-glutamyl transferase
References
- 1.Cano MV, Hajjeh RA. The epidemiology of histoplasmosis: a review. Semin Respir Infect. 2001;16(2):109–118. doi: 10.1053/srin.2001.24241. [DOI] [PubMed] [Google Scholar]
- 2.Denning DW. Minimizing fungal disease deaths will allow the UNAIDS target of reducing annual AIDS deaths below 500 000 by 2020 to be realized. Philos Trans R Soc Lond B Biol Sci. 2016;371(1709):20150468. doi: 10.1098/rstb.2015.0468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adenis A, Nacher M, Hanf M, Vantilcke V, Boukhari R, Blachet D, et al. HIV-associated histoplasmosis early mortality and incidence trends: from neglect to priority. PLoS Negl Trop Dis. 2014;8(8):e3100. doi: 10.1371/journal.pntd.0003100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012;4(165):165rv13. doi: 10.1126/scitranslmed.3004404. [DOI] [PubMed] [Google Scholar]
- 5.Almeida MA, Almeida-Silva F, Guimarães AJ, Almeida-Paes R, Zancopé-Oliveira RM. The occurrence of histoplasmosis in Brazil: A systematic review. Int J Infect Dis. 2019;86:147–156. doi: 10.1016/j.ijid.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Manos NE, Ferebee SH, Kerschbaum WF. Geographic variation in the prevalence of histoplasmin sensitivity. Dis Chest. 1956;29(6):649–668. doi: 10.1378/chest.29.6.649. [DOI] [PubMed] [Google Scholar]
- 7.Baddley JW, Winthrop KL, Patkar NM, Delzell E, Beukelman T, Xie F, et al. Geographic distribution of endemic fungal infections among older persons, United States. Emerg Infect Dis. 2011;17(9):1664–1669. doi: 10.3201/eid1709.101987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Armstrong PA, Jackson BR, Haselow D, Fields V, Ireland M, Austin C, et al. Multistate epidemiology of histoplasmosis, United States, 2011-2014. Emerg Infect Dis. 2018;24(3):425–431. doi: 10.3201/eid2403.171258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baker J, Setianingrum F, Wahyuningsih R, Denning DW. Mapping histoplasmosis in South East Asia - implications for diagnosis in AIDS. Emerg Microbes Infect. 2019;8(1):1139–1145. doi: 10.1080/22221751.2019.1644539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lofgren SM, Kirsch EJ, Maro VP, Morrissey AB, Msuya LJ, Kinabo GD, et al. Histoplasmosis among hospitalized febrile patients in northern Tanzania. Trans R Soc Trop Med Hyg. 2012;106(8):504–507. doi: 10.1016/j.trstmh.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rehman MH, Hadiuzzaman Md, Bhuiyan MKJ, Islam N, Ansari NP, Mumu SA, et al. Prevalence of superficial fungal infections in the rural areas of Bangladesh. Iran Journal of Dermatology. 2011;14(3):86–91. [Google Scholar]
- 12.Parvin R, Amin R, Mahbub MS, Hasnain M, Arif KM, Miah MT, et al. Deep fungal infection-an emerging problem in Bangladesh. J Medicine. 2010;11(2):170–175. doi: 10.3329/jom.v11i2.5466. [DOI] [Google Scholar]
- 13.Mahbub MS, Ahasan HN, Miah MT, Alam MB, Gupta RD, Arif KM, et al. Disseminated histoplasmosis. J Medicine. 2010;11(1):70–73. doi: 10.3329/jom.v11i1.4278. [DOI] [Google Scholar]
- 14.Antinori S. Histoplasma capsulatum: more widespread than previously thought. Am J Trop Med Hyg. 2014;90(6):982–983. doi: 10.4269/ajtmh.14-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deepe GS. 265 - Histoplasma capsulatum (Histoplasmosis) In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases (Eighth Edition) Philadelphia: Content Repository Only; 2015. pp. 2949–2962.e1. [Google Scholar]
- 16.Schlossberg D. Clinical infectious disease. Cambridge University Press; 2008. [Google Scholar]
- 17.Fojtasek MF, Sherman MR, Garringer T, Blair R, Wheat LJ, Schnizlein-Bick CT. Local immunity in lung-associated lymph nodes in a murine model of pulmonary histoplasmosis. Infect Immun. 1993;61(11):4607–4614. doi: 10.1128/iai.61.11.4607-4614.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou P, Sieve MC, Tewari RP, Seder RA. Interleukin-12 modulates the protective immune response in SCID mice infected with Histoplasma capsulatum. Infect Immun. 1997;65(3):936–942. doi: 10.1128/IAI.65.3.936-942.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wheat J. Histoplasmosis. Experience during outbreaks in Indianapolis and review of the literature. Medicine (Baltimore) 1997;76(5):339–354. doi: 10.1097/00005792-199709000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Assi MA, Sandid MS, Baddour LM, Roberts GD, Walker RC. Systemic histoplasmosis: a 15-year retrospective institutional review of 111 patients. Medicine (Baltimore) 2007;86(3):162–169. doi: 10.1097/md.0b013e3180679130. [DOI] [PubMed] [Google Scholar]
- 21.Wheat LJ, Slama TG, Norton JA, Kohler RB, Eitzen HE, French ML, et al. Risk factors for disseminated or fatal histoplasmosis. Analysis of a large urban outbreak. Ann Intern Med. 1982;96(2):159–163. doi: 10.7326/0003-4819-96-2-159. [DOI] [PubMed] [Google Scholar]
- 22.Kauffman CA. Histoplasmosis: a clinical and laboratory update. Clin Microbiol Rev. 2007;20(1):115–132. doi: 10.1128/CMR.00027-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wheat J, Sarosi G, McKinsey D, Hamill R, Bradsher R, Johnson P, et al. Practice guidelines for the management of patients with histoplasmosis. Infectious Diseases Society of America. Clin Infect Dis. 2000;30(4):688–695. doi: 10.1086/313752. [DOI] [PubMed] [Google Scholar]
- 24.Lamps LW, Molina CP, West AB, Haggitt RC, Scott MA. The pathologic spectrum of gastrointestinal and hepatic histoplasmosis. Am J Clin Pathol. 2000;113(1):64–72. doi: 10.1309/X0Y2-P3GY-TWE8-DM02. [DOI] [PubMed] [Google Scholar]
- 25.Goodwin RA, Jr, Shapiro JL, Thurman GH, Thurman SS, Des Prez RM. Disseminated histoplasmosis: clinical and pathologic correlations. Medicine (Baltimore) 1980;59(1):1–33. [PubMed] [Google Scholar]
- 26.Rihana NA, Kandula M, Velez A, Dahal K, O’Neill EB. Histoplasmosis presenting as granulomatous hepatitis: case report and review of the literature. Case Rep Med. 2014;2014:879535. doi: 10.1155/2014/879535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wood A, Abushamma S, Esfeh JM. Extrapulmonary hepatic histoplasmosis presenting as chronic liver disease: A case report. American Journal of Gastroenterology. 2018;113:S1275–S1276. [Google Scholar]
- 28.Nahar L, Benzamin M, Sarkar N, Roy U, Nahar K, Rukunuzzaman M, et al. A 8- year Bangladeshi girl with disseminated histoplasmosis, presented as chronic liver disease with portal hypertension: a rare case report. BMC Pediatr. 2020;20(1):284. doi: 10.1186/s12887-020-02189-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wheat LJ. Laboratory diagnosis of histoplasmosis: update 2000. Semin Respir Infect. 2001;16(2):131–140. doi: 10.1053/srin.2001.24243. [DOI] [PubMed] [Google Scholar]
- 30.Wheat LJ, Freifeld AG, Kleiman MB, Baddley JW, McKinsey DS, Loyd JE, et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45(7):807–825. doi: 10.1086/521259. [DOI] [PubMed] [Google Scholar]
- 31.Gill D, Dean R, Virk J, Lyons M, Hess M. Unusual presentation of disseminated histoplasmosis. Am J Emerg Med. 2017;35(4):668.e3–668.e4. doi: 10.1016/j.ajem.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 32.Hage CA, Kirsch EJ, Stump TE, Kauffman CA, Goldman M, Connolly P, et al. Histoplasma antigen clearance during treatment of histoplasmosis in patients with AIDS determined by a quantitative antigen enzyme immunoassay. Clin Vaccine Immunol. 2011;18(4):661–666. doi: 10.1128/CVI.00389-10. [DOI] [PMC free article] [PubMed] [Google Scholar]


