This cohort study evaluates the bidirectional, longitudinal associations between disturbed sleep and depressive symptoms in children and adolescents using cross-lagged models.
Key Points
Question
What are the bidirectional, longitudinal associations between disturbed sleep and depressive symptoms in children and adolescents?
Findings
In this cohort study including data on 1689 children and 1113 adolescents, cross-lagged analyses showed significant cascade processes (ie, bidirectional links carried forward across time) throughout childhood. In adolescence, significant bidirectional associations were found between ages 10 and 12 years, but after age 13 years, no significant cross-lagged estimates were found.
Meaning
These findings suggest disturbed sleep in childhood is an important target for early identification and intervention programs for depression.
Abstract
Importance
Understanding the longitudinal, bidirectional associations between disturbed sleep and depression in childhood and adolescence is crucial for the development of prevention and intervention programs.
Objective
To test for bidirectional associations and cascade processes between disturbed sleep and depressive symptoms covering both childhood and adolescence and to test for the moderating processes of sex and pubertal status in adolescence.
Design, Setting, and Participants
A prospective cohort study using the Québec Longitudinal Study of Child Development (QLSCD; 1997-ongoing). QLSCD’s objective is to identify early childhood factors associated with long-term psychosocial and academic adjustment. Data were collected across 8 waves between ages 5 years (2003) and 17 years (2015). Associations were tested through cross-lagged models in childhood (5, 7, and 8 years), and in adolescence (10, 12, 13, 15, and 17 years). Data were analyzed from February to October 2021.
Main Outcomes and Measures
Primary outcomes were disturbed sleep and depressive symptoms. Disturbed sleep was parent-reported and included sleep duration, time awake in bed, daytime sleepiness, sleep talking, sleepwalking, night terrors, and nightmares. Depressive symptoms were parent-reported in childhood (Child Behavior Checklist and Revised Ontario Child Health Study Scales), and self-reported in adolescence (Mental Health and Social Inadaptation Assessment for Adolescents).
Results
Data on 1689 children (852 female [50.4%]) and 1113 adolescents (595 female [53.5%]) were included in the analyses. In childhood, significant bidirectional associations between depressive symptoms and disturbed sleep at all time points were found, indicating cascade processes (range β = 0.07; 95% CI, 0.02-012 to β = 0.15; 95% CI, 0.10-0.19). In adolescence, significant bidirectional associations from depressive symptoms to disturbed sleep (β = 0.09; 95% CI, 0.04-0.14) and vice versa (β = 0.10; 95% CI, 0.04-0.16) between 10 and 12 years were found. Between 12 and 13 years, depressive symptoms were modestly associated with disturbed sleep (β = 0.05; 95% CI, 0.001-0.10) but the reverse association was not significant. Cross-lagged estimates were nonsignificant after 13 years. The associations did not vary as a function of either sex or puberty-by-sex.
Conclusions and Relevance
These findings suggest that disturbed sleep is associated with the consolidation of depressive symptoms starting in childhood, which, in turn, is associated with ongoing sleep problems. It is possible that timely and appropriate interventions for incipient disturbed sleep and depression prevent spiraling effects on both domains.
Introduction
Depression is the third leading cause of disability worldwide.1 It is an all-age disorder, and childhood is the time when it can first appear.2 The cumulative prevalence is low in childhood (2%-4%) and increases sharply during adolescence, peaking around 20% in early adulthood.3
Although girls are affected as often as boys in childhood, girls show a higher risk (approximately 2:1) from adolescence onward.4 Among other risk factors,4 earlier puberty is associated with an increased risk of depression and with the preponderance of affected girls in the transition from childhood to adolescence.5,6 Longitudinal epidemiological studies show that individuals with child-onset or adolescent-onset depression (compared with adult-onset depression) have a more chronic and recurring course, show worse functional outcomes,3,7,8 and have poorer response to treatment,9,10,11 suggesting that focusing on early prevention is important and could be key to reducing the overall lifetime burden of depression.
Prevention programs for depression in children and adolescents that rely on cognitive, coping, and emotional management skills are effective.12 However, their effects tend to decay over time,13,14 suggesting that further effort is needed. Modifiable risk factor management has proven effective in the prevention of various diseases15 and may be a complementary strategy to bolster depression prevention programs.
Disturbed sleep is one of the many modifiable risk factors for depression in children and adolescents.16,17 Previous research used a wide range of definitions for disturbed sleep, including insomnia symptoms,18,19,20,21,22,23 chronotype,24 daytime sleepiness,25 and broadly defined sleep disturbances, which include both insomnia and parasomnias (ie, nightmares, sleep talking, sleepwalking, and night terrors).26,27,28,29,30,31,32,33,34,35,36,37,38 A recent meta-analysis39 showed that the pooled estimates of the association between disturbed sleep and depression did not differ significantly between insomnia and broadly defined sleep disturbances.
Children and adolescents often report both disturbed sleep and depression, with co-occurrence rates equally distributed between boys and girls.40,41 Significant longitudinal, unidirectional associations have also been reported. A recent meta-analysis39 reported significant pooled estimates of the association between disturbed sleep and later depression controlling for baseline depression. Treating disturbed sleep has been effective in decreasing later depression in adolescence.42 However, whether analog prevention approaches in childhood will result in similar, or enhanced, outcomes is still unknown. There is also evidence of the prospective, unidirectional association between depression and later disturbed sleep in children and adolescents,31,43,44 although this finding is mixed, with some studies reporting nonsignificant associations.32,41,45
Several studies focused on bidirectional associations between disturbed sleep and depression in children and adolescents,46 with a minority testing 3 or more time points, therefore potentially looking at developmental cascades. Cascade processes occur when bidirectional links are carried forward across time, above and beyond within-time covariation and within-construct continuity.47 As of this writing and to our knowledge, 6 studies31,37,48,49,50,51 have tested 3 or more time points, and developmental cascades were found in adolescence only.48 Only 2 studies50,51 focused on childhood, and no studies covered both childhood and adolescence, which hinders a full understanding of the dynamics at play throughout these developmental stages.
Understanding the longitudinal, bidirectional associations and possible developmental cascades between disturbed sleep and depression has the potential to inform risk identification and prevention programs. The fact that disturbed sleep may lead to depression and, potentially, vice-versa, can trigger an unhealthy cycle. If set in motion in childhood, such a cycle would have time to amplify, resulting in developmental cascades that consolidate the 2 problems (ie, reciprocal effects build up over time, with long-lasting cumulative consequences for development).47
The primary goal of the current study was to replicate and expand this previous research by testing bidirectional associations and developmental cascades between disturbed sleep and depression using cross-lagged models and by extending the developmental window of investigation to cover both childhood and adolescence. We used data from the Québec Longitudinal Study of Child Development (QLSCD) collected across 8 waves between ages 5 and 17 years. Given the differences in risk between child-onset and adolescent-onset depression, particularly for girls,52 and the different assessment tools used in these developmental periods, we analyzed childhood and adolescence separately. In addition, given sex-related and puberty-related prevalence differences in both depression and disturbed sleep in adolescence,6,53 we conducted 2 multigroup analyses to examine the possible moderating role of sex and puberty in the cross-lagged model in adolescence. According to previous literature,31,37,49,51 we expected no sex difference. Given the lack of prior literature, the second multigroup analysis was considered exploratory.
Methods
Sample
This cohort study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for observational studies.54 The QLSCD is a representative birth cohort of infants born between 1997 and 1998 to mothers living in the province of Québec, Canada. Attrition rate and detailed cohort characteristics are reported in eMethods 1 in the Supplement and elsewhere.55 The study was approved by the ethics review boards of the Institut de la Statistique du Québec, the Centre Hospitalier Universitaire Sainte-Justine, the Louis-Hippolyte Lafontaine Hospital, and the Université de Montréal, Faculty of Medicine, and written informed consent was obtained from families at each assessment.55
For childhood analyses, data collected at ages 5, 7, and 8 years were considered, whereas for adolescent analyses, data at 10, 12, 13, 15, and 17 years were used. Of note, in the current study, we considered childhood the period between 5 and 9 years of age, and adolescence the period between 10 and 17 years.56 To allow for comparability across studies, given that the literature varies considerably in the definition of childhood and adolescence cutoffs, we tested 3 additional cross-lagged models: (1) 5, 7, 8, and 10 years; (2) 12, 13, 15, and 17 years; and (3) 5, 7, 8, 10, 12, 13, 15, and 17 years. Participants were included if they had 2 or fewer missing values for depression or disturbed sleep across all time points. For childhood assessments, mothers were asked to report on their child’s sleep and depression, whereas for adolescence, mothers reported on their child’s sleep, and depression was self-reported by adolescents.
Disturbed Sleep
For a wider scope, we opted for a broad definition of disturbed sleep, including both parasomnias and insomnia. Sleep was assessed through a questionnaire of 7 items that assessed sleep duration, time awake in bed, daytime sleepiness, sleep talking, sleepwalking, night terrors, and nightmares (eMethods 1 in the Supplement). The same measurement was used in previous research57 in the QLSCD cohort. A total score was computed, and the score was rescaled to range 0 to 10. The higher the score, the more disturbed the sleep. For comparability with previous research,18,19,20,21,22,23 cross-lagged analyses were repeated using an insomnia index—that is, the total score included sleep duration, time awake in bed, and daytime sleepiness.
Depressive Symptoms
Parents rated children on the well-validated Behavior Questionnaire, which was created for the Canadian National Longitudinal Study of Children and Youth58 and incorporates items from the Child Behavior Checklist59 and the Revised Ontario Child Health Study Scales.60 Eight items were used to depict depressive symptoms (eMethods 2 in the Supplement). Adolescents completed a 10-item questionnaire drawn from the Mental Health and Social Inadaptation Assessment for Adolescents. This measure has been validated in the QLSCD61 (eMethods 3 in the Supplement). A mean score was computed, and the score rescaled to range 0 to 10. The higher the score, the more depressive symptoms.
Covariates and Moderators
Sex, pubertal status, socioeconomic status (SES), and maternal depression were selected according to previous research.5,6,34,62,63 No data were available for sex. SES and maternal depression were entered as covariates at participant’s age 5 and 10 years in childhood and adolescence analyses, respectively. Sex and pubertal status were used as categorical moderators in multigroup analyses in adolescence. Measurements’ details for covariates and moderators are in eMethods 4 in the Supplement. Given that puberty-related risk for depression differs in boys and girls (ie, early pubertal status in girls, and early and late pubertal status in boys are associated with increased depression),5 pubertal status was categorized into 4 groups: early or late in boys/or girls (late = pubertal status lower than III; early = pubertal status equal or higher than III64).
Statistical Analysis
Descriptive statistics and Pearson correlations were computed using SPSS statistical software version 19.0 for Windows (SPSS Inc.). Missing data were examined by the missing value analysis module and the Little Missing Completely at Random test.65 Cross-lagged models were conducted using Mplus statistical software version 7 (Muthén & Muthén).66 Missing data were treated through full information maximum likelihood, which uses maximum likelihood to estimate model parameters using all available raw data.67,68 Overall model fit was tested by considering together the comparative fit index (CFI), the Tucker-Lewis index (TLI), the root mean square error of approximation (RMSEA), the χ2 statistic and the ratio of χ2 to degrees of freedom.69 A nonsignificant χ2 value, a CFI and a TLI value of 0.90 or higher, an RMSEA value below 0.06, and a ratio of χ2 to degrees of freedom less than 3 were considered indicators of good fit.70 Secondary analyses used a multigroup approach to test whether model estimates differed across sex or puberty-by-sex using a χ2test. The unconstrained model was compared against a model in which across-time, within-time, and cross-lagged paths were constrained to be equal across levels of the moderator. A deterioration of model fit would suggest that the associations may be different across levels of the moderator. All P values were 2-sided. P < .05 was considered to be significant. Data were analyzed from February to October 2021.
Results
A total of 1689 children (852 female [50.4%]) and 1113 adolescents (595 female [53.5%]) were included in the study. Missing data patterns for outcome variables in childhood and adolescence are reported in eResults 1, eTable 2, eTable 3, eTable 4, and eTable 5 in the Supplement.
Childhood
In the childhood analysis, 1689 children (49.6% male) were included (Table 1). Participants were from a higher SES and were more often girls compared with nonparticipants (431 participants; t2115 = −6.55, P < .001; and χ21 = 6.34, P = .011, respectively). Descriptive statistics across time points for the study variables are shown in Table 2.
Table 1. Characteristics of the Population Included in the Study.
| Characteristics | Participants, No. (%) | |
|---|---|---|
| Childhood sample (n = 1689) | Adolescence sample (n = 1113) | |
| Sex | ||
| Female | 852 (50.4) | 595 (53.5) |
| Male | 837 (49.6) | 518 (46.5) |
| Low birth weight (<2500 g) | 55 (3.3) | 30 (2.7) |
| Prematurity (<37 wk of gestation) | 84 (5.0) | 45 (4.0) |
| Sociodemographic characteristics | ||
| Parental age at child’s birth, mean (SD), y | ||
| Mother | 28.98 (5.18) | 29.21 (5.09) |
| Father | 31.82 (5.55) | 31.89 (5.35) |
| Low education (no high school diploma) | ||
| Maternal | 244 (14.5) | 139 (12.5) |
| Paternal | 258 (16.5) | 159 (15.2) |
| Nonintact family (single parent/blended) | 296 (17.6) | 183 (16.4) |
Table 2. Descriptive Statistics in the Childhood Samplea.
| Time point and variable | Children, No. (N = 1689) | Total score, mean (SD) [range] |
|---|---|---|
| 5 y | ||
| Disturbed sleep | 1438 | 1.50 (0.21) [0.00 to 10.00] |
| Depression | 1632 | 2.33 (1.47) [0.00 to 10.00] |
| Maternal depression | 1437 | 1.49 (1.69) [0.00 to 10.00] |
| Socioeconomic status | 1689 | 0.04 (0.95) [−2.91 to 2.90] |
| 6 y | ||
| Disturbed sleep | 1307 | 1.46 (0.20) [0.00 to 10.00] |
| Depression | 1428 | 2.44 (1.54) [0.00 to 10.00] |
| 8 y | ||
| Disturbed sleep | 1259 | 1.39 (0.20) [0.00 to 10.00] |
| Depression | 1392 | 2.52 (1.58) [0.00 to 10.00] |
Data are courtesy of the Quebec Institute of Statistics.
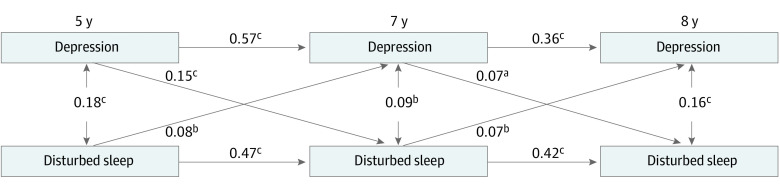
Bivariate correlations between depressive symptoms and disturbed sleep are reported in eTable 6 in the Supplement. Figure 1 shows the standardized path coefficients (β) and the fit indices of the cross-lagged model. The stability path estimates for disturbed sleep (range β = 0.42 [95% CI, 0.35-0.48] to β = 0.47 [95% CI, 0.42-0.52]) and depressive symptoms (range β = 0.36 [95% CI, 0.29-0.42] to β = 0.57 [95% CI, 0.53-0.61]) were fairly stable across time. The correlations between disturbed sleep and depressive symptoms were significant at each time point (r = 0.18 at 5 years, r = 0.09 at 7 years, and r = 0.16 at 8 years). Cross-lagged path estimates showed that depressive symptoms were significantly associated with later disturbed sleep, and disturbed sleep was associated with later depressive symptoms at all time points (range β = 0.07 [95% CI 0.02-0.12] to β = 0.15 [95% CI, 0.09-0.19]), suggesting a developmental cascade throughout childhood. Also, there were significant associations between depressive symptoms at 5 and 8 years (b = 0.27; SE = 0.038; β = 0.25 [95% CI, 0.19-0.32]; P < .001), and between disturbed sleep at 5 and 8 years (b = 0.23; SE = 0.031; β = 0.22 [95% CI, 0.17-0.29]; P < .001). Among covariates, only paths between maternal depression and both disturbed sleep and depressive symptoms were significant (β = 0.11 [95% CI, 0.06-0.17]; P < .001; and β = 0.22 [95% CI, 0.16-0.27]; P < .001).
Figure 1. Estimates From the Cross-Lagged Model for the Reciprocal Associations Between Disturbed Sleep and Depression Across Childhood.
All estimates are standardized. Fit statistics: χ216 = 52.449, P < .001; root mean square error of approximation = 0.037 (95% CI, 0.026-0.048); comparative fit index = 0.981; Tucker Lewis index = 0.961. Covariates were socioeconomic status and maternal depression. P < .05 was considered statistically significant. Data are courtesy of the Quebec Institute of Statistics.
aP < .05.
bP < .01.
cP < .001.
Adolescence
In the adolescent analysis, 1113 individuals were included (595 [53.5%] female) (Table 1). Participants were from a higher SES and were more often girls compared with the nonparticipants (1007 participants; t2115 = −7.11; χ21 = 18.17; P < .001). Descriptive statistics across time points for the study variables are shown in Table 3. Bivariate correlations between depressive symptoms and disturbed sleep are reported in eTable 7 in the Supplement. Figure 2 shows the β coefficients and the fit indices of the cross-lagged model. The stability path estimates for disturbed sleep (range β = 0.31 [95% CI, 0.23 to 0.39] to β = 0.63 [95% CI, 0.58 to 0.67]) and depressive symptoms (β = 0.37 [95% CI, 0.32 to 0.42] to β = 0.54 [95% CI, 0.49 t 0.60]) at baseline were fairly stable across all 5 time points. The correlation between depressive symptoms and disturbed sleep was significant at each time point (r range, 0.07 to 0.10). Cross-lagged path estimates were significant from depressive symptoms to disturbed sleep (β = 0.09 [95% CI, 0.04 to 0.14]; P < .001) and vice versa (β = 0.10 [95% CI, 0.04 to 0.16]; P = .001) between 10 and 12 years. Between 12 and 13 years, depressive symptoms were modestly associated with disturbed sleep (β = 0.05 [95% CI, 0.001 to 0.10], P = .04) but the reverse association was not significant. Cross-lagged estimates were nonsignificant after 13 years. Among covariates, significant paths were found between maternal depression and both disturbed sleep and depressive symptoms (β = 0.17 [95% CI, 0.11 to 0.24]; P < .001 and β = 0.08 [95% CI, 0.01 to 0.15]; P = .02, respectively), and between SES and depressive symptoms (β = −0.15 [95% CI, −0.21 to −0.09]; P < .001). Compared with the unconstrained model, the fit of either the sex-invariant or the puberty-by-sex-invariant model was not deteriorated (difference between 2 nested models, χ233 = 29.468; P = .64 and χ299 = 99.781; P = .46, respectively), indicating that the associations between depressive symptoms and disturbed sleep did not vary as a funciton of either sex or puberty-by-sex. Cross-lagged paths were identical when listwise deletion was used as an alternative missing data strategy, in both childhood and adolescence.
Table 3. Descriptive Statistics in the Adolescence Samplea.
| Time point and variable | Adolescents, No. (N = 1113) | Total score, mean (SD) [range] |
|---|---|---|
| 10 y | ||
| Disturbed sleep | 941 | 1.87 (0.76) [0.00 to 10.00] |
| Depression | 1024 | 2.81 (1.61) [0.00 to 10.00] |
| Maternal depression | 951 | 1.33 (1.28) [0.00 to 10.00] |
| Socioeconomic status | 1113 | 0.09 (0.91) [−2.59 to 2.78] |
| 12 y | ||
| Disturbed sleep | 1044 | 1.76 (0.74) [0.00 to 10.00] |
| Depression | 1080 | 2.33 (1.68) [0.00 to 10.00] |
| 13 y | ||
| Disturbed sleep | 950 | 1.76 (0.72) [0.00 to 10.00] |
| Depression | 1047 | 2.22 (1.82) [0.00 to 10.00] |
| 15 y | ||
| Disturbed sleep | 998 | 1.50 (0.69) [0.00 to 10.00] |
| Depression | 1082 | 3.28 (2.18) [0.00 to 10.00] |
| 17 y | ||
| Disturbed sleep | 894 | 1.42 (0.74) [0.00 to 10.00] |
| Depression | 976 | 3.67 (2.26) [0.00 to 10.00] |
Data are courtesy of the Quebec Institute of Statistics.
Figure 2. Estimates From the Cross-Lagged Model for the Reciprocal Association Between Disturbed Sleep and Depression Across Adolescence.
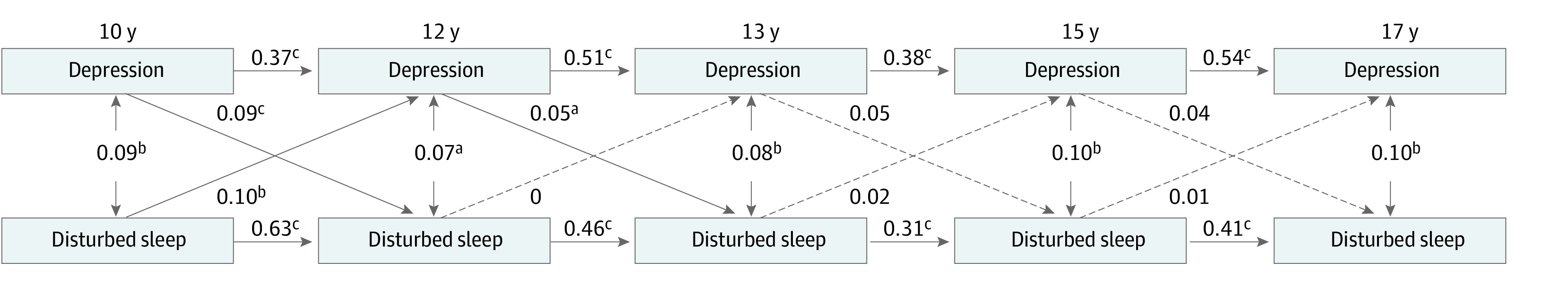
All estimates are standardized. Dashed arrows indicate nonsignificant paths. Fit statistics: χ228 = 48.842; P = .009; root mean square error of approximation = 0.026 (95% CI, 0.013-0.038); comparative fit index = 0.993; Tucker Lewis index = 0.985. Covariates were socioeconomic status and maternal depression. P < .05 was considered statistically significant. Data are courtesy of the Quebec Institute of Statistics.
aP < .05.
bP < .01.
cP < .001.
Cross-lagged paths using the insomnia index are reported in eResults 2, eFigure 1, and eFigure 2 in the Supplement. Results from the cross-lagged models (1) 5, 7, 8, and 10 years; (2) 12, 13, 15, and 17 years; and (3) 5, 7, 8, 10, 12, 13, 15, and 17 years are reported in eResults 3, eFigure 3, eFigure 4, and eFigure 5 in the Supplement.
Discussion
To our knowledge, this cohort study is the first to report developmental cascades between disturbed sleep and depressive symptoms throughout childhood and early adolescence. Our finding suggests that disturbed sleep makes a significant contribution to the stability over time of depressive symptoms across childhood and early adolescence, which, in turn, is associated with ongoing disturbed sleep.
To date, 2 studies50,51 that we know of have tested cross-lagged associations over 3 or more time points in childhood and developmental cascades were not reported. Quach et al50 found that disturbed sleep is consistently associated with increased depression from preschool to 12 years, and bidirectionality was found only from 6 to 7 years. Although the study sample and measurements were similar to ours, analyses were not controlled for any covariates, which could plausibly account for the discrepancy of the results. Foley et al51 found no bidirectional effects but only a unidirectional association from disturbed sleep to depression between preschool and grade 1. Differently from our study, the authors tested the reciprocal effects of disturbed sleep, depression, and social competence, therefore adding 1 construct in the cross-lagged model, which could partly explain the discrepancy of the results. In adolescence, we found no developmental cascades, which was in line with 331,37,49 previous studies but differed from a fourth study,48 and a bidirectional association between 10 and 12 years in line with 1 previous study.37 Starting at 13 years, cross-lagged associations were not significant at any time points. Finally, effects held across sexes in line with previous results31,37,49,51 and were unaffected by including pubertal status as a moderator in the model.
Taken together, our findings suggest that there might be a sensitive window between 5 and 12 years for sleep interventions to mitigate the emergence and/or growth of later depressive symptoms. Up to now, randomized clinical trials of sleep interventions in depressed adolescents have targeted mid adolescence (ie, 15 years)42,71 and yielded small effect sizes (pooled standardized mean difference = −0.27 [95% CI, −0.50 to −0.04]).42 Starting prevention efforts in childhood may have a similar, or even greater impact on depression compared with treatment initiated in adolescence,42,71 because it would reduce the risk before depression consolidates. To date, we are not aware of any randomized clinical trials of sleep interventions specifically addressing depressed children. To expand our understanding, randomized clinical trials with long-term follow-up and in children with different levels of baseline depression are needed. According to our findings, a sample of 100 individuals would be adequately powered for a sleep intervention for the prevention of depression in a children community sample.
The magnitude of the cross-lagged estimates that we found was overall small (β range, 0.05-0.15), but quite in line with previous reports39 and with etiological models of depression. Indeed, multiple risk factors, each with a small effect, underlie the vulnerability to depression,72 and this may partly explain why sleep interventions, albeit having a significant effect, are limited in preventing depression in adolescents.42,71 The potential for a larger impact could be achieved by simultaneously addressing multiple risk factors of depression. Disturbed sleep often co-occurs with other lifestyle risk behaviors associated with depression, including poor diet,73 poor physical activity,74 and excessive recreational screen time.75 Future research should examine whether a multiple health behavior change approach could be a viable option for depression prevention.76
Understanding the biological mechanisms underlying the developmental cascade linking disturbed sleep and depression is of paramount importance. Key outstanding questions include whether an early sensitive window of vulnerability can be identified, which could explain why cascade processes concentrate in early childhood and fade in adolescence. Both conditions77 are heritable4 and share common genetic risk factors.78 Both disturbed sleep79 and depression80 have been associated bidirectionally with inflammatory processes, suggesting that inflammation may be one mechanism driving the spiraling process. Interestingly, treating disturbed sleep and depression attenuates inflammation,81,82 and using anti-inflammatory medications to treat depression seems promising in adults.83 Future research is needed to determine whether patterns of proinflammatory responses may be one of the biological mechanisms through which disturbed sleep accelerates depression and whether it can be targeted for depression prevention in children and adolescents.
Limitations
There are some limitations in this study. First, participants were from a higher SES and more often girls than nonparticipants, which potentially limits the generalizability of our results. Second, the questionnaire for depression did not rate symptoms’ severity. Furthermore, depressive symptoms were parent-reported in childhood and self-reported in adolescence, which may have accounted for the differences found between childhood and adolescent findings. However, the high stability of scores suggests that both adolescent and parent-report measures tapped into the same constructs. Third, in childhood, parents reported on both disturbed sleep and depressive symptoms, which might have implied perception bias. Fourth, the questionnaire for disturbed sleep was not validated. Furthermore, it was parent-reported, which have been shown to be less accurate compared with self-report and objective measurements of sleep.84 Results may need to be replicated with objective measurements and/or validated questionnaires. However, self-reports remain the measure of choice in community surveys. Additionally, for disturbed sleep during childhood, there was a slight difference in the pattern of missing data related to time since enrollment. Although the analytical strategy that was used to deal with missing data mitigates the effects of attrition, we cannot exclude that missing data may have affected the results in the childhood analysis.
Conclusions
In conclusion, bidirectional and developmental cascades linking disturbed sleep and depressive symptoms in childhood and early adolescence emphasize the importance of identifying and treating incipient disturbed sleep as early as possible to prevent spiraling effects on depression. More randomized clinical trials testing interventions possibly targeting common pathways are needed to bolster depression prevention. Because of the reliance on self-report data, results should be interpreted with caution.
eMethods 1. Characteristic of the Quebec Longitudinal Study of Child Development (QLSCD)
eMethods 2. Seven-Item Parent-Reported Questionnaire to Assess Disturbed Sleep in Children and Adolescents
eMethods 3. Eight-Item Parent-Reported Questionnaire to Assess Depression in Children
eMethods 4. Ten-Item Self-Reported Questionnaire to Assess Depression in Adolescents
eMethods 5. Measurements’ Details for Covariates/Moderators, i.e. Socioeconomic Status (SES), Maternal Depression and Pubertal Status
eResults 1. Missing Data Pattern for Outcome Variables in Childhood and Adolescence
eResults 2. Cross-Lagged Paths Between the Insomnia Index and Depressive Symptoms in Childhood and Adolescence
eResults 3. Cross-Lagged Paths Between the Disturbed Sleep and Depressive Symptoms Including the Following Time-Points: (1) 5, 7, 8, 10 years, (2) 12, 13, 15 and 17 years, and (3) 5, 7, 8, 10, 12, 13, 15 and 17 Years
eTable 1. Tanner Stage Distribution for Adrenarche and Gonadarche for Males and Females
eTable 2. Rates of Missingness for Depression and Disturbed Sleep in Childhood
eTable 3. Characteristics of the Study Variables at Each Time Point in the Complete Versus With-Missing-Data Subgroups in the Childhood Sample
eTable 4. Rates of Missingness for Depression and Disturbed Sleep in Adolescence
eTable 5. Characteristics of the Study Variables at Each Time Point in the Complete Versus With-Missing-Data Subgroups in the Adolescence Sample
eTable 6. Correlation Matrix Between Disturbed Sleep and Depression in Childhood
eTable 7. Correlation Matrix Between Disturbed Sleep and Depression in the Adolescence Sample
eFigure 1. Estimates From the Cross-Lagged Model for the Reciprocal Associations Between the Insomnia Index and Depression Across Childhood (n=1689)
eFigure 2. Estimates From the Cross-Lagged Model for the Reciprocal Association Between the Insomnia Index and Depression Across Adolescence (n=1113)
eFigure 3. Estimates From the Cross-Lagged Model for the Reciprocal Associations Between Disturbed Sleep and Depression Across Childhood Including Time-Points 5, 7, 8 and 10 Years (n=1689)
eFigure 4. Estimates From the Cross-Lagged Model for the Reciprocal Association Between Disturbed Sleep and Depression Across Adolescence Including Time-Points 12, 13, 15 and 17 Years (n=1113)
eFigure 5. Estimates From the Cross-Lagged Model for the Reciprocal Associations Between Disturbed Sleep and Depression From 5 to 17 Years of Age (n=1085)
References
- 1.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-1858. doi: 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luby JL, Gaffrey MS, Tillman R, April LM, Belden AC. Trajectories of preschool disorders to full DSM depression at school age and early adolescence: continuity of preschool depression. Am J Psychiatry. 2014;171(7):768-776. doi: 10.1176/appi.ajp.2014.13091198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety. 1998;7(1):3-14. doi: [DOI] [PubMed] [Google Scholar]
- 4.Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. 2012;379(9820):1056-1067. doi: 10.1016/S0140-6736(11)60871-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Graber JA. Pubertal timing and the development of psychopathology in adolescence and beyond. Horm Behav. 2013;64(2):262-269. doi: 10.1016/j.yhbeh.2013.04.003 [DOI] [PubMed] [Google Scholar]
- 6.Angold A, Costello EJ. Puberty and depression. Child Adolesc Psychiatr Clin N Am. 2006;15(4):919-937. doi: 10.1016/j.chc.2006.05.013 [DOI] [PubMed] [Google Scholar]
- 7.Copeland WE, Alaie I, Jonsson U, Shanahan L. Associations of childhood and adolescent depression with adult psychiatric and functional outcomes. J Am Acad Child Adolesc Psychiatry. 2021;60(5):604-611. doi: 10.1016/j.jaac.2020.07.895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kessler RC, Avenevoli S, Ries Merikangas K. Mood disorders in children and adolescents: an epidemiologic perspective. Biol Psychiatry. 2001;49(12):1002-1014. doi: 10.1016/S0006-3223(01)01129-5 [DOI] [PubMed] [Google Scholar]
- 9.Cipriani A, Zhou X, Del Giovane C, et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet. 2016;388(10047):881-890. doi: 10.1016/S0140-6736(16)30385-3 [DOI] [PubMed] [Google Scholar]
- 10.Eckshtain D, Kuppens S, Ugueto A, et al. Meta-analysis: 13-year follow-up of psychotherapy effects on youth depression. J Am Acad Child Adolesc Psychiatry. 2020;59(1):45-63. doi: 10.1016/j.jaac.2019.04.002 [DOI] [PubMed] [Google Scholar]
- 11.Weisz JR, Kuppens S, Ng MY, et al. Are psychotherapies for young people growing stronger? tracking trends over time for youth anxiety, depression, attention-deficit/hyperactivity disorder, and conduct problems. Perspect Psychol Sci. 2019;14(2):216-237. doi: 10.1177/1745691618805436 [DOI] [PubMed] [Google Scholar]
- 12.Li J, Liang JH, Li JY, et al. Optimal approaches for preventing depressive symptoms in children and adolescents based on the psychosocial interventions: a bayesian network meta-analysis. J Affect Disord. 2021;280(Pt A):364-272. doi: 10.1016/j.jad.2020.11.023 [DOI] [PubMed] [Google Scholar]
- 13.Ssegonja R, Nystrand C, Feldman I, Sarkadi A, Langenskiöld S, Jonsson U. Indicated preventive interventions for depression in children and adolescents: a meta-analysis and meta-regression. Prev Med. 2019;118:7-15. doi: 10.1016/j.ypmed.2018.09.021 [DOI] [PubMed] [Google Scholar]
- 14.Loechner J, Starman K, Galuschka K, et al. Preventing depression in the offspring of parents with depression: a systematic review and meta-analysis of randomized controlled trials. Clin Psychol Rev. 2018;60:1-14. doi: 10.1016/j.cpr.2017.11.009 [DOI] [PubMed] [Google Scholar]
- 15.Gapstur SM, Drope JM, Jacobs EJ, et al. A blueprint for the primary prevention of cancer: targeting established, modifiable risk factors. CA Cancer J Clin. 2018;68(6):446-470. doi: 10.3322/caac.21496 [DOI] [PubMed] [Google Scholar]
- 16.Cairns KE, Yap MB, Pilkington PD, Jorm AF. Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2014;169:61-75. doi: 10.1016/j.jad.2014.08.006 [DOI] [PubMed] [Google Scholar]
- 17.Mewton L, Champion K, Kay-Lambkin F, Sunderland M, Thornton L, Teesson M. Lifestyle risk indices in adolescence and their relationships to adolescent disease burden: findings from an Australian national survey. BMC Public Health. 2019;19(1):60. doi: 10.1186/s12889-019-6396-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luo C, Zhang J, Pan J. One-year course and effects of insomnia in rural Chinese adolescents. Sleep. 2013;36(3):377-384. doi: 10.5665/sleep.2454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31(10):1351-1356. [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts RE, Duong HT. Depression and insomnia among adolescents: a prospective perspective. J Affect Disord. 2013;148(1):66-71. doi: 10.1016/j.jad.2012.11.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31(4):473-480. doi: 10.1093/sleep/31.4.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alvaro PK, Roberts RM, Harris JK, Bruni O. The direction of the relationship between symptoms of insomnia and psychiatric disorders in adolescents. J Affect Disord. 2017;207:167-174. doi: 10.1016/j.jad.2016.08.032 [DOI] [PubMed] [Google Scholar]
- 23.Urrila AS, Karlsson L, Kiviruusu O, et al. ; Adolescent Depression Study group . Sleep complaints in adolescent depression: one year naturalistic follow-up study. BMC Psychiatry. 2014;14:283. doi: 10.1186/s12888-014-0283-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haraden DA, Mullin BC, Hankin BL. The relationship between depression and chronotype: a longitudinal assessment during childhood and adolescence. Depress Anxiety. 2017;34(10):967-976. doi: 10.1002/da.22682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luo C, Zhang J, Chen W, Lu W, Pan J. Course, risk factors, and mental health outcomes of excessive daytime sleepiness in rural Chinese adolescents: a one-year prospective study. J Affect Disord. 2018;231:15-20. doi: 10.1016/j.jad.2018.01.016 [DOI] [PubMed] [Google Scholar]
- 26.Fan F, Zhou Y, Liu X. Sleep disturbance predicts posttraumatic stress disorder and depressive symptoms: a cohort study of Chinese adolescents. J Clin Psychiatry. 2017;78(7):882-888. doi: 10.4088/JCP.15m10206 [DOI] [PubMed] [Google Scholar]
- 27.Kouros CD, Morris MC, Garber J. Within-person changes in individual symptoms of depression predict subsequent depressive episodes in adolescents: a prospective study. J Abnorm Child Psychol. 2016;44(3):483-494. doi: 10.1007/s10802-015-0046-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shanahan L, Copeland WE, Angold A, Bondy CL, Costello EJ. Sleep problems predict and are predicted by generalized anxiety/depression and oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry. 2014;53(5):550-558. doi: 10.1016/j.jaac.2013.12.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson EO, Chilcoat HD, Breslau N. Trouble sleeping and anxiety/depression in childhood. Psychiatry Res. 2000;94(2):93-102. doi: 10.1016/S0165-1781(00)00145-1 [DOI] [PubMed] [Google Scholar]
- 30.Becker SP, Langberg JM, Evans SW. Sleep problems predict comorbid externalizing behaviors and depression in young adolescents with attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry. 2015;24(8):897-907. doi: 10.1007/s00787-014-0636-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Doane LD, Gress-Smith JL, Breitenstein RS. Multi-method assessments of sleep over the transition to college and the associations with depression and anxiety symptoms. J Youth Adolesc. 2015;44(2):389-404. doi: 10.1007/s10964-014-0150-7 [DOI] [PubMed] [Google Scholar]
- 32.Gregory AM, Rijsdijk FV, Lau JY, Dahl RE, Eley TC. The direction of longitudinal associations between sleep problems and depression symptoms: a study of twins aged 8 and 10 years. Sleep. 2009;32(2):189-199. doi: 10.1093/sleep/32.2.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chang LY, Chang HY, Wu WC, Lin LN, Wu CC, Yen LL. Body mass index and depressive symptoms in adolescents in Taiwan: testing mediation effects of peer victimization and sleep problems. Int J Obes (Lond). 2017;41(10):1510-1517. doi: 10.1038/ijo.2017.111 [DOI] [PubMed] [Google Scholar]
- 34.El-Sheikh M, Kelly RJ, Buckhalt JA, Benjamin Hinnant J. Children’s sleep and adjustment over time: the role of socioeconomic context. Child Dev. 2010;81(3):870-883. doi: 10.1111/j.1467-8624.2010.01439.x [DOI] [PubMed] [Google Scholar]
- 35.Ksinan Jiskrova G, Vazsonyi AT, Klánová J, Dušek L. Sleep quantity and problems as mediators of the eveningness-adjustment link during childhood and adolescence. J Youth Adolesc. 2019;48(3):620-634. doi: 10.1007/s10964-018-0965-8 [DOI] [PubMed] [Google Scholar]
- 36.Schneiderman JU, Ji J, Susman EJ, Negriff S. Longitudinal relationship between mental health symptoms and sleep disturbances and duration in maltreated and comparison adolescents. J Adolesc Health. 2018;63(1):74-80. doi: 10.1016/j.jadohealth.2018.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mulraney M, Giallo R, Lycett K, Mensah F, Sciberras E. The bidirectional relationship between sleep problems and internalizing and externalizing problems in children with ADHD: a prospective cohort study. Sleep Med. 2016;17:45-51. doi: 10.1016/j.sleep.2015.09.019 [DOI] [PubMed] [Google Scholar]
- 38.Reynolds KC, Alfano CA. Childhood bedtime problems predict adolescent internalizing symptoms through emotional reactivity. J Pediatr Psychol. 2016;41(9):971-982. doi: 10.1093/jpepsy/jsw014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marino C, Andrade B, Campisi SC, et al. Association between disturbed sleep and depression in children and youths: a systematic review and meta-analysis of cohort studies. JAMA Netw Open. 2021;4(3):e212373. doi: 10.1001/jamanetworkopen.2021.2373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lovato N, Short MA, Micic G, Hiller RM, Gradisar M. An investigation of the longitudinal relationship between sleep and depressed mood in developing teens. Nat Sci Sleep. 2017;9:3-10. doi: 10.2147/NSS.S111521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gregory AM, O’Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41(8):964-971. doi: 10.1097/00004583-200208000-00015 [DOI] [PubMed] [Google Scholar]
- 42.Gee B, Orchard F, Clarke E, Joy A, Clarke T, Reynolds S. The effect of non-pharmacological sleep interventions on depression symptoms: a meta-analysis of randomised controlled trials. Sleep Med Rev. 2019;43:118-128. doi: 10.1016/j.smrv.2018.09.004 [DOI] [PubMed] [Google Scholar]
- 43.Kaneita Y, Yokoyama E, Harano S, et al. Associations between sleep disturbance and mental health status: a longitudinal study of Japanese junior high school students. Sleep Med. 2009;10(7):780-786. doi: 10.1016/j.sleep.2008.06.014 [DOI] [PubMed] [Google Scholar]
- 44.Meijer AM, Reitz E, Deković M, van den Wittenboer GL, Stoel RD. Longitudinal relations between sleep quality, time in bed and adolescent problem behaviour. J Child Psychol Psychiatry. 2010;51(11):1278-1286. doi: 10.1111/j.1469-7610.2010.02261.x [DOI] [PubMed] [Google Scholar]
- 45.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40(8):700-708. doi: 10.1016/j.jpsychires.2006.07.008 [DOI] [PubMed] [Google Scholar]
- 46.Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. 2013;36(7):1059-1068. doi: 10.5665/sleep.2810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Masten AS, Cicchetti D. Developmental cascades. Dev Psychopathol. 2010;22(3):491-495. doi: 10.1017/S0954579410000222 [DOI] [PubMed] [Google Scholar]
- 48.Hayley AC, Skogen JC, Sivertsen B, et al. Symptoms of depression and difficulty initiating sleep from early adolescence to early adulthood: a longitudinal study. Sleep. 2015;38(10):1599-1606. doi: 10.5665/sleep.5056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kelly RJ, El-Sheikh M. Reciprocal relations between children’s sleep and their adjustment over time. Dev Psychol. 2014;50(4):1137-1147. doi: 10.1037/a0034501 [DOI] [PubMed] [Google Scholar]
- 50.Quach JL, Nguyen CD, Williams KE, Sciberras E. Bidirectional associations between child sleep problems and internalizing and externalizing difficulties from preschool to early adolescence. JAMA Pediatr. 2018;172(2):e174363. doi: 10.1001/jamapediatrics.2017.4363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Foley JE, Weinraub M. Sleep, affect, and social competence from preschool to preadolescence: distinct pathways to emotional and social adjustment for boys and for girls. Front Psychol. 2017;8:711. doi: 10.3389/fpsyg.2017.00711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shanahan L, Copeland WE, Costello EJ, Angold A. Child-, adolescent- and young adult-onset depressions: differential risk factors in development? Psychol Med. 2011;41(11):2265-2274. doi: 10.1017/S0033291711000675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang J, Chan NY, Lam SP, et al. Emergence of sex differences in insomnia symptoms in adolescents: a large-scale school-based study. Sleep. 2016;39(8):1563-1570. doi: 10.5665/sleep.6022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. doi: 10.1016/j.ijsu.2014.07.013 [DOI] [PubMed] [Google Scholar]
- 55.Orri M, Boivin M, Chen C, et al. Cohort profile: Quebec Longitudinal Study of Child Development (QLSCD). Soc Psychiatry Psychiatr Epidemiol. 2021;56(5):883-894. doi: 10.1007/s00127-020-01972-z [DOI] [PubMed] [Google Scholar]
- 56.Bundy DAP, de Silva N, Horton S, et al. Investment in child and adolescent health and development: key messages from Disease Control Priorities, 3rd Edition. Lancet. 2018;391(10121):687-699. doi: 10.1016/S0140-6736(17)32417-0 [DOI] [PubMed] [Google Scholar]
- 57.Shen C, Luo Q, Chamberlain SR, et al. What Is the link between attention-deficit/hyperactivity disorder and sleep disturbance? a multimodal examination of longitudinal relationships and brain structure using large-scale population-based cohorts. Biol Psychiatry. 2020;88(6):459-469. doi: 10.1016/j.biopsych.2020.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.National Longitudinal Survey of Children and Youth (NLSCY) . May 14, 2009. Accessed August 3, 2022. https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=4504
- 59.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. ASEBA; 2001. [Google Scholar]
- 60.Boyle MH, Offord DR, Racine Y, Fleming JE, Szatmari P, Sanford M. Evaluation of the revised Ontario Child Health Study scales. J Child Psychol Psychiatry. 1993;34(2):189-213. doi: 10.1111/j.1469-7610.1993.tb00979.x [DOI] [PubMed] [Google Scholar]
- 61.Côté SM, Orri M, Brendgen M, et al. Psychometric properties of the Mental Health and Social Inadaptation Assessment for Adolescents (MIA) in a population-based sample. Int J Methods Psychiatr Res. 2017;26(4):e1566. doi: 10.1002/mpr.1566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. 2015;54(1):37-44.e2. doi: 10.1016/j.jaac.2014.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stein A, Pearson RM, Goodman SH, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800-1819. doi: 10.1016/S0140-6736(14)61277-0 [DOI] [PubMed] [Google Scholar]
- 64.Royal College of Pediatrics and Child Health . Fact sheet: UK 2-18 years growth chart. Accessed August 3, 2022. https://www.rcpch.ac.uk/resources/uk-who-growth-charts-2-18-years
- 65.Little RJ, Rubin DB. The analysis of social science data with missing values. Sociol Methods Res. 1989;18(2-3):292–326. doi: 10.1177/0049124189018002004 [DOI] [Google Scholar]
- 66.Muthen LK, Muthen BO. Mplus users’ guide. 7th ed. 2015. Accessed August 3, 2022. https://www.statmodel.com/download/usersguide/MplusUserGuideVer_7
- 67.Wothke W. Longitudinal and multi-group modeling with missing data. In: Little TD, Schnabel KU, Baumert J, eds. Modeling Longitudinal and Multiple Group Data: Practical Issues, Applied Approaches, and Specific Examples. Lawrence Erlbaum Associates, Inc; 1996: 219–240. [Google Scholar]
- 68.Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, eds. Advanced Structural Equation Modeling. Lawrence Erlbaum Associates, Inc; 1996: 243–277. [Google Scholar]
- 69.McDonald RP, Ho MH. Principles and practice in reporting structural equation analyses. Psychol Methods. 2002;7(1):64-82. doi: 10.1037/1082-989X.7.1.64 [DOI] [PubMed] [Google Scholar]
- 70.Ullman JB. Structural equation modeling. In: Tabachnick BG, Fidell LS, eds. Using Multivariate Statistics. 4th ed. Allyn & Bacon; 2001. [Google Scholar]
- 71.de Bruin EJ, Bögels SM, Oort FJ, Meijer AM. Improvements of adolescent psychopathology after insomnia treatment: results from a randomized controlled trial over 1 year. J Child Psychol Psychiatry. 2018;59(5):509-522. doi: 10.1111/jcpp.12834 [DOI] [PubMed] [Google Scholar]
- 72.Köhler CA, Evangelou E, Stubbs B, et al. Mapping risk factors for depression across the lifespan: an umbrella review of evidence from meta-analyses and Mendelian randomization studies. J Psychiatr Res. 2018;103:189-207. doi: 10.1016/j.jpsychires.2018.05.020 [DOI] [PubMed] [Google Scholar]
- 73.Lassale C, Batty GD, Baghdadli A, et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry. 2019;24(7):965-986. doi: 10.1038/s41380-018-0237-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Korczak DJ, Madigan S, Colasanto M. Children’s physical activity and depression: a meta-analysis. Pediatrics. 2017;139(4):e20162266. doi: 10.1542/peds.2016-2266 [DOI] [PubMed] [Google Scholar]
- 75.Wang X, Li Y, Fan H. The associations between screen time-based sedentary behavior and depression: a systematic review and meta-analysis. BMC Public Health. 2019;19(1):1524. doi: 10.1186/s12889-019-7904-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Prochaska JJ, Spring B, Nigg CR. Multiple health behavior change research: an introduction and overview. Prev Med. 2008;46(3):181-188. doi: 10.1016/j.ypmed.2008.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Barclay NL, Gehrman PR, Gregory AM, Eaves LJ, Silberg JL. The heritability of insomnia progression during childhood/adolescence: results from a longitudinal twin study. Sleep. 2015;38(1):109-118. doi: 10.5665/sleep.4334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gregory AM, Rijsdijk FV, Dahl RE, McGuffin P, Eley TC. Associations between sleep problems, anxiety, and depression in twins at 8 years of age. Pediatrics. 2006;118(3):1124-1132. doi: 10.1542/peds.2005-3118 [DOI] [PubMed] [Google Scholar]
- 79.Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80(1):40-52. doi: 10.1016/j.biopsych.2015.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Colasanto M, Madigan S, Korczak DJ. Depression and inflammation among children and adolescents: a meta-analysis. J Affect Disord. 2020;277:940-948. doi: 10.1016/j.jad.2020.09.025 [DOI] [PubMed] [Google Scholar]
- 81.Irwin MR, Olmstead R, Breen EC, et al. Cognitive behavioral therapy and tai chi reverse cellular and genomic markers of inflammation in late-life insomnia: a randomized controlled trial. Biol Psychiatry. 2015;78(10):721-729. doi: 10.1016/j.biopsych.2015.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cho JH, Bhutani S, Kim CH, Irwin MR. Anti-inflammatory effects of melatonin: a systematic review and meta-analysis of clinical trials. Brain Behav Immun. 2021;93:245-253. doi: 10.1016/j.bbi.2021.01.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Köhler O, Benros ME, Nordentoft M, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71(12):1381-1391. doi: 10.1001/jamapsychiatry.2014.1611 [DOI] [PubMed] [Google Scholar]
- 84.Short MA, Gradisar M, Lack LC, Wright HR, Chatburn A. Estimating adolescent sleep patterns: parent reports versus adolescent self-report surveys, sleep diaries, and actigraphy. Nat Sci Sleep. 2013;5:23-26. doi: 10.2147/NSS.S38369 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods 1. Characteristic of the Quebec Longitudinal Study of Child Development (QLSCD)
eMethods 2. Seven-Item Parent-Reported Questionnaire to Assess Disturbed Sleep in Children and Adolescents
eMethods 3. Eight-Item Parent-Reported Questionnaire to Assess Depression in Children
eMethods 4. Ten-Item Self-Reported Questionnaire to Assess Depression in Adolescents
eMethods 5. Measurements’ Details for Covariates/Moderators, i.e. Socioeconomic Status (SES), Maternal Depression and Pubertal Status
eResults 1. Missing Data Pattern for Outcome Variables in Childhood and Adolescence
eResults 2. Cross-Lagged Paths Between the Insomnia Index and Depressive Symptoms in Childhood and Adolescence
eResults 3. Cross-Lagged Paths Between the Disturbed Sleep and Depressive Symptoms Including the Following Time-Points: (1) 5, 7, 8, 10 years, (2) 12, 13, 15 and 17 years, and (3) 5, 7, 8, 10, 12, 13, 15 and 17 Years
eTable 1. Tanner Stage Distribution for Adrenarche and Gonadarche for Males and Females
eTable 2. Rates of Missingness for Depression and Disturbed Sleep in Childhood
eTable 3. Characteristics of the Study Variables at Each Time Point in the Complete Versus With-Missing-Data Subgroups in the Childhood Sample
eTable 4. Rates of Missingness for Depression and Disturbed Sleep in Adolescence
eTable 5. Characteristics of the Study Variables at Each Time Point in the Complete Versus With-Missing-Data Subgroups in the Adolescence Sample
eTable 6. Correlation Matrix Between Disturbed Sleep and Depression in Childhood
eTable 7. Correlation Matrix Between Disturbed Sleep and Depression in the Adolescence Sample
eFigure 1. Estimates From the Cross-Lagged Model for the Reciprocal Associations Between the Insomnia Index and Depression Across Childhood (n=1689)
eFigure 2. Estimates From the Cross-Lagged Model for the Reciprocal Association Between the Insomnia Index and Depression Across Adolescence (n=1113)
eFigure 3. Estimates From the Cross-Lagged Model for the Reciprocal Associations Between Disturbed Sleep and Depression Across Childhood Including Time-Points 5, 7, 8 and 10 Years (n=1689)
eFigure 4. Estimates From the Cross-Lagged Model for the Reciprocal Association Between Disturbed Sleep and Depression Across Adolescence Including Time-Points 12, 13, 15 and 17 Years (n=1113)
eFigure 5. Estimates From the Cross-Lagged Model for the Reciprocal Associations Between Disturbed Sleep and Depression From 5 to 17 Years of Age (n=1085)