Key Points
Question
What are the incubation periods of COVID-19 caused by different SARS-CoV-2 strains?
Findings
In this systematic review and meta-analysis of 141 articles, the pooled incubation period was 6.57 days. The incubation periods of COVID-19 caused by the Alpha, Beta, Delta, and Omicron variants were 5.00, 4.50, 4.41, and 3.42 days, respectively.
Meaning
These results suggest that with the evolution of mutant strains, the incubation period of COVID-19 decreased gradually from Alpha variant to Omicron variant.
This systematic review and meta-analysis estimates the incubation periods of COVID-19 caused by various strains of SARS-CoV-2.
Abstract
Importance
Several studies were conducted to estimate the average incubation period of COVID-19; however, the incubation period of COVID-19 caused by different SARS-CoV-2 variants is not well described.
Objective
To systematically assess the incubation period of COVID-19 and the incubation periods of COVID-19 caused by different SARS-CoV-2 variants in published studies.
Data Sources
PubMed, EMBASE, and ScienceDirect were searched between December 1, 2019, and February 10, 2022.
Study Selection
Original studies of the incubation period of COVID-19, defined as the time from infection to the onset of signs and symptoms.
Data Extraction and Synthesis
Following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline, 3 reviewers independently extracted the data from the eligible studies in March 2022. The parameters, or sufficient information to facilitate calculation of those values, were derived from random-effects meta-analysis.
Main Outcomes and Measures
The mean estimate of the incubation period and different SARS-CoV-2 strains.
Results
A total of 142 studies with 8112 patients were included. The pooled incubation period was 6.57 days (95% CI, 6.26-6.88) and ranged from 1.80 to 18.87 days. The incubation period of COVID-19 caused by the Alpha, Beta, Delta, and Omicron variants were reported in 1 study (with 6374 patients), 1 study (10 patients), 6 studies (2368 patients) and 5 studies (829 patients), respectively. The mean incubation period of COVID-19 was 5.00 days (95% CI, 4.94-5.06 days) for cases caused by the Alpha variant, 4.50 days (95% CI, 1.83-7.17 days) for the Beta variant, 4.41 days (95% CI, 3.76-5.05 days) for the Delta variant, and 3.42 days (95% CI, 2.88-3.96 days) for the Omicron variant. The mean incubation was 7.43 days (95% CI, 5.75-9.11 days) among older patients (ie, aged over 60 years old), 8.82 days (95% CI, 8.19-9.45 days) among infected children (ages 18 years or younger), 6.99 days (95% CI, 6.07-7.92 days) among patients with nonsevere illness, and 6.69 days (95% CI, 4.53-8.85 days) among patients with severe illness.
Conclusions and Relevance
The findings of this study suggest that SARS-CoV-2 has evolved and mutated continuously throughout the COVID-19 pandemic, producing variants with different enhanced transmission and virulence. Identifying the incubation period of different variants is a key factor in determining the isolation period.
Introduction
In December 2019, multiple cases of novel coronavirus disease (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), were reported in Wuhan, China.1 On March 11, 2020, the World Health Organization (WHO) declared that COVID-19 can be characterized as a pandemic. To date, the transmission of COVID-19 is still difficult to contain, as confirmed and death cases are still increasing. Up to March 16, 2022, 460 280 168 confirmed cases and 6 050 018 confirmed deaths have been reported to the WHO.2 Rapid spread of COVID-19 has had enormous social, economic, and health care system effects around the world. Effective treatment to block the spread of COVID-19 is not developed yet, so countries have implemented a series of nontreatment interventions such as social distancing, isolation, face mask mandates, and quarantining to reduce its rapid transmission.3 Existing evidence has shown that most of COVID-19 cases are missed by screening because infected persons are unaware they were exposed and have not developed symptoms yet.4,5,6
Incubation period is one of the most important epidemiological parameters of infectious diseases. Knowledge of the disease’s incubation period is of great significance for case definition, management of emerging threats, estimation of the duration of follow-up for contact tracing and secondary case detection, and the establishment of public health programs aimed at reducing local transmission.7 Previous studies8 have reported that the average serial interval of COVID-19 is shorter than the average incubation period, which suggests a substantial proportion of presymptomatic transmission. For diseases caused by different pathogens, the length of incubation period is the key factor to determine the isolation period of infected persons.
Since the beginning of the COVID-19 epidemic, SARS-CoV-2 has evolved and mutated continuously, producing variants with different transmissibility and virulence. SARS-CoV-2 variants are classified by the WHO into 2 types: variants of concern (VOC) and variants of interest (VOI).9 According to the US Center for Disease Control and Prevention (CDC), a VOC is a variant that has increased transmissibility, increased virulence, a resistance to vaccine or acquired immunity from previous infection, and has the ability to elude diagnostic detection.10 Several VOC have emerged from the original wild-type strain isolated in Wuhan since the outbreak first began in December 2019, such as Alpha (B.1.1.7), Beta (B.1.351), Gamma (P.1), Delta (B.1.617.2), and Omicron (B.1.1.529).9 The Alpha variant was first detected in the UK in September 2020; the Beta variant in South Africa in May 2020; and the Gamma variant in Brazil in September 2020. All 3 quickly became the main virus strains worldwide.
Globally, many studies were conducted to estimate the average incubation period of COVID-19. However, the reported estimates of incubation period in these fragmented studies vary depending on the number of study participants recruited, the type of design employed, the data collection period, and the country in which the study was conducted. In addition, with the spread of the Delta and Omicron variants, the current incubation period of COVID-19 is different from that in the outbreak of Wuhan. This meta-analysis was aimed to determine the overall pooled incubation period of COVID-19 and the incubation period of COVID-19 caused by different SARS-CoV-2 variants using available evidence, so as to adjust prevention and control strategies and better block the transmission of COVID-19.
Methods
Search Strategy
We conducted this meta-analysis following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline. This review was not registered. This study was exempted from ethics review board at Peking University because it used previously published literature in its analysis. A survey of the literature was implemented between December 1, 2019, and February 10, 2022. Publications on the electronic databases PubMed, Embase and ScienceDirect were searched using the keywords novel coronavirus, SARS-CoV-2, 2019-nCoV, or COVID-19 and either incubation period or incubation (eTable 1 in the Supplement). No restrictions on language or publication status were imposed so long as an English abstract was available. The initial searches were carried out by 3 of the investigators (Y.W., L.K., R.G.).
Inclusion and Exclusion Criteria
Inclusion criteria for selecting the studies were that the incubation period was one of the primary outcomes of the study and that, when the incubation periods of multiple groups were reported in the same study, only the group with the largest study population was included. Criteria for exclusion included articles not conducted as studies (ie, editorials, perspective articles, letters to the editor, reviews, article information, or comments), duplicate studies, and articles with overlapping study populations (ie, enrolling the same population in the same region around the same period).
Outcome Measures and Study Selection
The outcome variable was the mean estimate of the incubation period. Incubation period was defined as the time from when the infection occurred to the onset of signs and symptoms or the first positive test. It was measured with cases of a well-defined period of exposure and symptom onset.
Results of searches were screened in 2 stages. First, titles and abstracts were screened and only relevant articles retained. Next, articles were read in detail—studies were selected for meta-analysis if they reported either results fitting our primary parameters (with CIs) or sufficient information to facilitate calculation of those values.
After screening for inclusion and exclusion criteria, data extraction was carried out from the included studies. The name of the first author, area of study, time period for data collection, characteristics of the study population, strain type, and estimates for the incubation period with 95% CI were extracted from the selected studies. Ninety-five percent CIs were estimated for the studies reporting mean with standard deviation by using the following formula, which is generally used to calculate the 95% CI for any parameter:
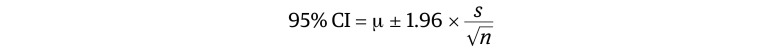 |
where μ indicates the mean incubation period, s the standard deviation, and n the sample size of the study. Some studies reported only median with interquartile range or range. Mean and the standard deviation were calculated for such studies by using an appropriate approximation for the consistency in synthesizing the results for meta-analysis.11,12
Quality Assessment
Once studies were shortlisted, 2 authors (Y.W., L.K.) independently conducted appraisals of study quality. We used a scale modified from the Newcastle-Ottawa scale13 by McAloon et al14 to assess the quality of observational studies in meta-analyses (eTable 2 in the Supplement). This scale consists of 2 parts with a full score of 5 stars. The first part is external validity, with a maximum of 1 star; the second part is internal validity, which includes exposure window (a maximum of 2 stars) and outcomes with (a maximum of 2 stars). Based on the combined score of these 2 parts, each paper was categorized as either weak (1 star or less), moderate (2 to 3 stars), or strong (4 stars or more). After the studies were evaluated by the 2 authors, the results were compared and differences in ratings were resolved by discussion until a consensus rating was agreed upon.
Statistical Analysis
A meta-analysis of continuous outcomes was employed for this study. We analyzed the data sets for the incubation period. After extracting all essential data using Excel 2021 (Microsoft Corporation), data were exported to Stata version 14.1 (StataCorp) statistical software for meta-analysis. A random-effect meta-analysis with an estimation of DerSimonian and Laird method was performed. Pooled mean estimates with 95% CIs were presented using forest plots. To determine the extent of variation between the studies, we conducted a heterogeneity test using the Higgins method, that was quantified by I2 value.15 Publication bias was also assessed using a funnel plot. A 2-sided P < .05 was considered statistically significant.
Results
Search Results
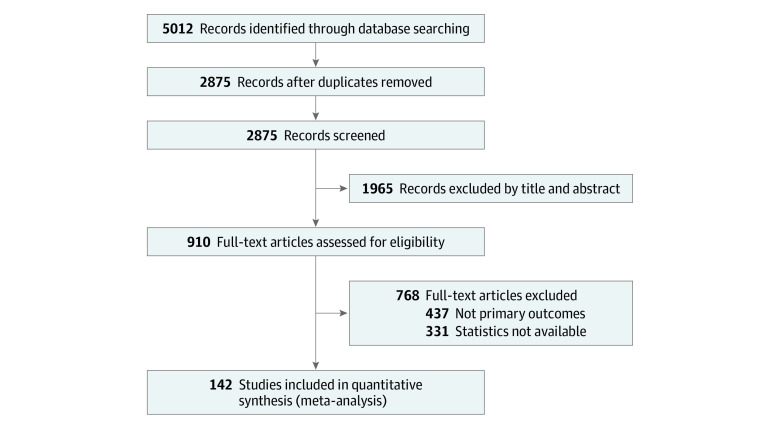
We identified 5012 records through PubMed, EMBASE, and Science Direct database searches, and documented the study selection process in a flowchart and showed the total numbers of retrieved references and the numbers of included and excluded studies (Figure 1). Based on the inclusion and exclusion criteria, 142 articles (8112 patients) were selected for analysis.16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157
Figure 1. Study Flow Diagram.
Study Characteristics
Over the 142 studies, the quality assessment gave 45 strong, 82 moderate, and 15 weak studies (eTable 3 in the Supplement). Most of the studies (93 [65.5%]) were conducted between January and March 2020 and most were conducted in China (108 [76.1%]). One study used case data from multiple countries around the world,81 6 studies were conducted in South Korea,37,46,51,52,59,124 4 in France,25,29,35,113 3 in Japan,80,105 2 in Singapore,87,111 2 in India,16,78,83,103 2 in Vietnam,21,58 and 2 in Australia.45,99 One hundred nineteen studies (83.8%) included patients infected with the wild-type strain, 5 (3.5%) with the multiple strains,17,26,35,80,112 and 11 (7.7%) with an unknown strain84,93,99,106,116,126,135,142,148,150,157 (eTable 4 in the Supplement).
Pooled Average Estimate of Incubation Period
The mean incubation period of COVID-19 was 6.57 days (95% CI, 6.26-6.88 days), ranging from 1.80 to 18.87 days (Table). There was substantial heterogeneity between the studies (I2 = 98.8%; P < .001). Our results suggested no potential publication bias in the included studies (eFigure 1 in the Supplement). The standard error for all the included studies in the meta-analysis was very low except for a 2020 study conducted by Xie134 where the highest standard error was observed.
Table. Mean Incubation Period of COVID-19 From Included Studies.
| Author | Mean incubation period (95% CI) | Weight |
|---|---|---|
| Areekal et al,16 2021 | 4.22 (3.71-4.65) | 0.81 |
| Backer et al,18.2020 | 6.4 (5.6-7.7) | 0.75 |
| Backer et al,17 2022 | 3.2 (2.93-3.47) | 0.82 |
| Bao et al,19 2020 | 5.4 (4.5-6.3) | 0.77 |
| Brandal et al,20 2021 | 3.33 (3.17-3.49) | 0.82 |
| Bui et al,21 2020 | 6.4 (4.89-8.5) | 0.64 |
| Chen et al,22 2020 | 8 (4.97-11.03) | 0.46 |
| Covid-Epidemiology Investigation Team,23 2021 | 8.75 (6.95-10.55) | 0.64 |
| Dai et al,24 2020 | 6.5 (5.9-7.1) | 0.80 |
| Del Águila-Mejía et al,26 2022 | 3.1 (2.82-3.38) | 0.82 |
| Deng et al,27 2021 | 8 (6.62-9.38) | 0.71 |
| Deng et al,28 2021 | 9.1 (7.86-9.66) | 0.77 |
| Denis et al,29 2021 | 4 (3.93-4.07) | 0.82 |
| Ding et al,30 2020 | 7.11 (5.24-8.98) | 0.63 |
| Dong et al,31 2020 | 7.25 (5.86-8.64) | 0.70 |
| Du et al,32 2020 | 5.28 (4.75-5.82) | 0.80 |
| Gao et al,34 2020 | 11.67 (9.46-13.87) | 0.58 |
| Gao et al,33 2020 | 7.33 (3.54-11.13) | 0.37 |
| Grant et al,35 2022 | 5 (4.95-5.05) | 0.82 |
| Guo et al,36 2020 | 9.33 (8.21-10.46) | 0.74 |
| Han et al,37 2020 | 6.63 (4.28-8.97) | 0.56 |
| Han et al,39 2020 | 7.67 (7.08-8.25) | 0.80 |
| Han et al,38 2020 | 5.5 (4.5-6.5) | 0.76 |
| Hong et al,40 2020 | 5.7 (4.95-6.45) | 0.78 |
| Hua et al,41 2020 | 9.1 (7.99-10.21) | 0.74 |
| Huang et al,43 2020 | 8 (7.57-8.43) | 0.81 |
| Huang et al,42 2020 | 5.5 (5.08-5.92) | 0.81 |
| Huang et al,44 2021 | 7.8 (7.4-8.5) | 0.80 |
| Je et al,45 2021 | 4.7 (3.21-6.19) | 0.69 |
| Jeong et al,46 2020 | 5 (4.38-5.62) | 0.79 |
| Jiang et al,47 2020 | 6.73 (5.97-7.48) | 0.78 |
| Jiang et al,48 2021 | 7.75 (7.1-7.99) | 0.81 |
| Jin et al,49 2020 | 5.33 (4.81-5.86) | 0.80 |
| Khonyongwa et al,50 2020 | 6 (5.5-7) | 0.78 |
| Ki et al,51 2020 | 5.39 (4.7-6.05) | 0.79 |
| Kim et al,52 2020 | 11.86 (7.59-16.13) | 0.32 |
| Kong et al,53 2020 | 6.33 (3.14-9.53) | 0.44 |
| Kong et al,55 2020 | 8.5 (7.8-9.2) | 0.79 |
| Kong et al,54 2020 | 7.25 (7.04-7.46) | 0.82 |
| Lai et al,56 2020 | 7.67 (7.02-8.31) | 0.79 |
| Lau et al,57 2021 | 4.75 (4.14-5.56) | 0.79 |
| Laval et al,25 2021 | 4.61 (3.2-6.02) | 0.70 |
| Le et al,58 2020 | 7 (4.87-9.13) | 0.59 |
| Lee et al,59 2021 | 4.6 (4.33-4.87) | 0.82 |
| Lei et al,60 2020 | 7.57 (3.95-11.19) | 0.39 |
| Leung et al,61 2020 | 1.8 (1.63-1.97) | 0.82 |
| Li et al,63 2020 | 5.33 (4.82-5.85) | 0.80 |
| Li et al,64 2022 | 6.5 (5.86-7.2) | 0.79 |
| Li et al,62 2020 | 5.2 (4.1-7) | 0.70 |
| Linton et al,65 2020 | 5.6 (5-6.3) | 0.79 |
| Liu et al,66 2021 | 13.5 (10.93-16.07) | 0.52 |
| Liu et al,68 2020 | 6.67 (5.38-7.95) | 0.72 |
| Liu et al,69 2020 | 6.02 (4.74-7.3) | 0.72 |
| Liu et al,70 2020 | 6 (4.83-7.17) | 0.73 |
| Liu et al,71 2020 | 8.8 (7.33-10.27) | 0.69 |
| Liu et al,72 2020 | 9 (7.79-10.21) | 0.73 |
| Liu et al,74 2021 | 8.4 (7.32-9.48) | 0.75 |
| Liu et al,67 2020 | 6.35 (6.28-6.42) | 0.82 |
| Liu et al,73 2020 | 7.67 (6.42-8.91) | 0.72 |
| Llaque-Quiroz et al,75 2020 | 8.67 (5.76-11.58) | 0.47 |
| Mao et al,76 2020 | 10.3 (8.18-12.42) | 0.59 |
| Moazzami et al,77 2021 | 1.91 (1.24-2.59) | 0.79 |
| Ng et al,78 2021 | 5.5 (4.99-6.01) | 0.80 |
| Nie et al,79 2020 | 5 (4.84-5.16) | 0.82 |
| Ogata et al,80 2022 | 3.7 (3.4-4) | 0.81 |
| Pak et al,81 2020 | 6.6 (5.4-7.8) | 0.73 |
| Pan et al,82 2020 | 6.11 (4.55-7.67) | 0.68 |
| Patrikar et al,83 2020 | 6.93 (6.11-7.75) | 0.78 |
| Paul et al,84 2021 | 6.74 (6.35-7.13) | 0.81 |
| Ping et al,85 2021 | 6.48 (5.58-7.38) | 0.77 |
| Pongpirul et al,86 2020 | 5.5 (4.69-6.31) | 0.78 |
| Pung et al,87 2020 | 4.33 (3.25-5.41) | 0.75 |
| Qi et al,88 2020 | 3.67 (2.87-4.46) | 0.78 |
| Qian et al,89 2020 | 5.67 (4.89-6.44) | 0.78 |
| Qiu et al,90 2020 | 11.25 (10.06-12.44) | 0.73 |
| Ratovoson et al,91 2021 | 4.1 (0.7-7.5) | 0.41 |
| Ren et al,92 2020 | 5.3 (4.6-6) | 0.79 |
| Samrah et al,93 2021 | 6.33 (5.51-7.15) | 0.78 |
| Sanche et al,94 2020 | 4.2 (3.5-5.1) | 0.78 |
| Shen et al,95 2020 | 7.17 (3.34-11) | 0.36 |
| Shen et al,96 2020 | 7.57 (5.41-9.73) | 0.59 |
| Shi et al,97 2020 | 6.13 (2.95-9.32) | 0.44 |
| Shi et al,98 2020 | 4.77 (3.61-5.94) | 0.73 |
| Shiel et al,99 2021 | 5.33 (4.6-6.07) | 0.78 |
| Shu et al,100 2020 | 5.17 (2.75-7.59) | 0.55 |
| Song et al,101 2020 | 5.01 (4.31-5.69) | 0.79 |
| Song et al,102 2020 | 8.23 (6.73-9.73) | 0.69 |
| Song et al,103 2020 | 10 (8.54-11.46) | 0.69 |
| Su et al,104 2021 | 5.4 (4.42-6.38) | 0.76 |
| Sugano et al,105 2020 | 6.8 (5.57-8.03) | 0.73 |
| Sun et al,106 2021 | 6.5 (4.55-8.45) | 0.62 |
| Sun et al,107 2020 | 5.4 (4.88-5.92) | 0.80 |
| Sun et al,108 2020 | 8.1 (6.73-9.47) | 0.71 |
| Sun et al,109 2021 | 5.33 (1.93-8.73) | 0.41 |
| Sun et al,110 2020 | 13 (9.53-16.47) | 0.40 |
| Tan et al,111 2020 | 5.54 (5.18-5.9) | 0.81 |
| Tanaka et al,112 2022 | 2.87 (2.56-3.17) | 0.81 |
| The SARS-CoV-2 variant with line,113 2021 | 4.5 (1.83-7.17) | 0.51 |
| Tian et al,114 2020 | 6.7 (6.07-7.33) | 0.79 |
| Tindale et al,115 2020 | 8.68 (7.72-9.7) | 0.76 |
| Viego et al,116 2020 | 7.9 (4.6-11.1) | 0.43 |
| Wang et al,158 2021 | 10.64 (8.08-13.2) | 0.52 |
| Wang et al,117 2020 | 6.5 (5.86-7.14) | 0.79 |
| Wang et al,118 2020 | 6.3 (6-6.6) | 0.81 |
| Wang et al,119 2020 | 4.5 (3-6.4) | 0.66 |
| Wang et al,120 2020 | 6 (5.47-6.53) | 0.80 |
| Wei et al,123 2021 | 8.8 (6.77-10.83) | 0.61 |
| Wei et al,122 2020 | 5.67 (5.14-6.19) | 0.80 |
| Won et al,124 2021 | 5.53 (3.98-8.09) | 0.60 |
| Wong et al,125 2020 | 5.5 (4.05-6.95) | 0.70 |
| Wu et al,128 2021 | 8.75 (7.51-9.99) | 0.72 |
| Wu et al,127 2020 | 7 (4.9-9.1) | 0.60 |
| Wu et al,126 2020 | 7 (5.78-8.22) | 0.73 |
| Wu et al,129 2020 | 6.05 (4.87-7.23) | 0.73 |
| Xiao et al,131 2020 | 7.18 (5.84-8.52) | 0.71 |
| Xiao et al,133 2021 | 8.58 (7-9) | 0.76 |
| Xiao et al,132 2020 | 8.98 (7.98-9.9) | 0.76 |
| Xiao et al,130 2020 | 9.25 (8.78-9.72) | 0.81 |
| Xie et al,134 2020 | 18.87 (9.01-28.73) | 0.09 |
| Xin et al,135 2020 | 6.9 (6.3-7.5) | 0.80 |
| Xu et al,136 2020 | 11.67 (9.87-13.47) | 0.64 |
| Xu et al,137 2020 | 4 (3.6-4.4) | 0.81 |
| Yang et al,138 2020 | 8.75 (8.39-9.11) | 0.81 |
| Yang et al,139 2021 | 6.67 (5.64-7.7) | 0.75 |
| Yang et al,140 2020 | 4 (1.33-6.67) | 0.51 |
| You et al,141 2020 | 8 (7.28-8.72) | 0.79 |
| Yu et al,143 2022 | 16.6 (16.22-16.98) | 0.81 |
| Yu et al,142 2020 | 6.8 (6.23-7.37) | 0.80 |
| Zhang et al,146 2021 | 4.3 (2.73-5.87) | 0.68 |
| Zhang et al,144 2020 | 5.2 (1.8-12.4) | 0.24 |
| Zhang et al,145 2020 | 6.75 (4.27-9.23) | 0.54 |
| Zhang et al,147 2021 | 4.67 (3.92-5.41) | 0.78 |
| Zhang et al,148 2021 | 6.1 (5.73-6.47) | 0.81 |
| Zhao et al,151 2021 | 6.8 (6.2-7.5) | 0.79 |
| Zhao et al,152 2020 | 7 (5.43-8.57) | 0.68 |
| Zhao et al,153 2021 | 6.5 (5.6-7.4) | 0.77 |
| Zhao et al,150 2021 | 4 (3.52-4.48) | 0.80 |
| Zhao et al,149 2020 | 6.67 (4.86-8.48) | 0.64 |
| Zhong et al,154 2020 | 6.85 (5.74-7.96) | 0.74 |
| Zhu et al,156 2021 | 3.33 (2.81-3.85) | 0.80 |
| Zhu et al,155 2020 | 7.27 (6.76-7.78) | 0.80 |
| Zhu et al,157 2021 | 11.6 (10.6-12.7) | 0.75 |
| Overall a | 6.57 (6.26-6.88) | 100.00 |
I2 = 98.8%; P < .001.
Mean Incubation Periods of COVID-19 Infected by Different Strains
Across a total of 119 studies with data on the wild-type strain, the mean incubation period was 6.65 days (95% CI, 6.31-6.99) (eFigure 2 in the Supplement). For infections caused by the Alpha variant, an incubation period of 5.00 days (95% CI, 4.94-5.06) was reported in a single study.35 One study from France reported the incubation period of 4.50 days (95% CI, 1.83-7.17 days) for COVID-19 caused by the Beta variant.113 Another study reported the incubation period of COVID-19 caused by the Beta/Gamma variant was 5.10 days (95% CI, 4.87-5.33 days).35
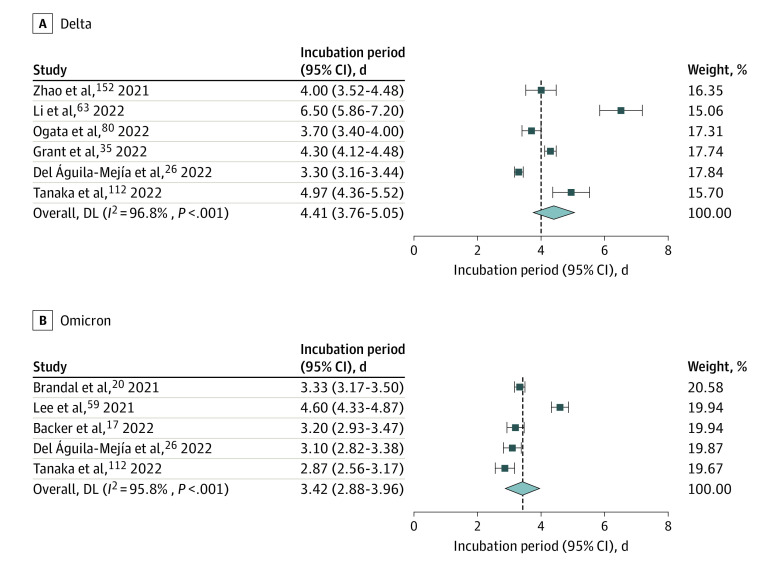
A total of 6 studies reported the incubation period of COVID-19 caused by the Delta variant, including 2 from China,63,152 2 from Japan,80,112 1 from France,35 and 1 from Spain,26 with a pooled incubation period of 4.41 days (95% CI, 3.76-5.05 days) (Figure 2). Five studies reported the incubation period of COVID-19 caused by the Omicron variant—1 each from Norway,20 Spain,26 Japan,112 the Netherlands,17 and South Korea59—with a pooled incubation period of 3.42 days (95% CI, 2.88-3.96 days) (Figure 2). With the evolution of the mutant strains, the incubation period of COVID-19 appeared to decrease gradually from the Alpha variant to Omicron variant, but there was no significant difference between the groups.
Figure 2. Forest Plot for Studies of Incubation Period of COVID-19 Caused by Different Variants.
Subgroup Analysis
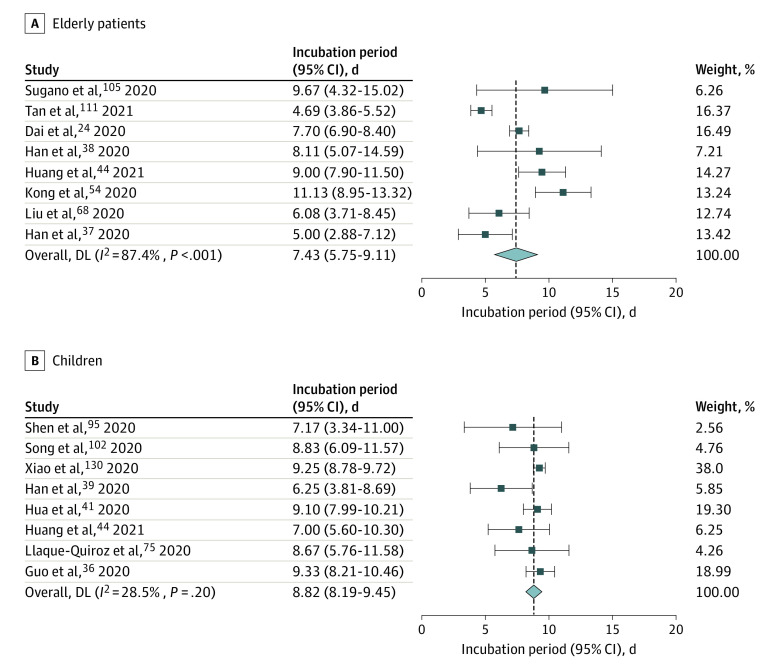
A total of 8 studies reported the incubation period of COVID-19 among older patients (ie, aged 60 years or more).24,37,38,44,54,68,105,111 The pooled mean incubation period for these studies was 7.43 days (95% CI, 5.75-9.11 days), which was slightly higher than the pooled incubation period of the general population (6.65 days; 95% CI, 6.34-6.96 days), but the difference was not significant (Figure 3).
Figure 3. Incubation Period for COVID-19 in Older Patients and Infected Children.
Infectious strains were original strains.
The mean incubation period of COVID-19 among infected children (under ages 18 years) was 8.82 days (95% CI, 8.19-9.45 days) across 8 studies,36,39,41,44,75,95,102,130 which was higher than the pooled incubation period of the general population (6.65 days; 95% CI, 6.34-6.96 days), and the difference was significant (P < .001) (Figure 3).
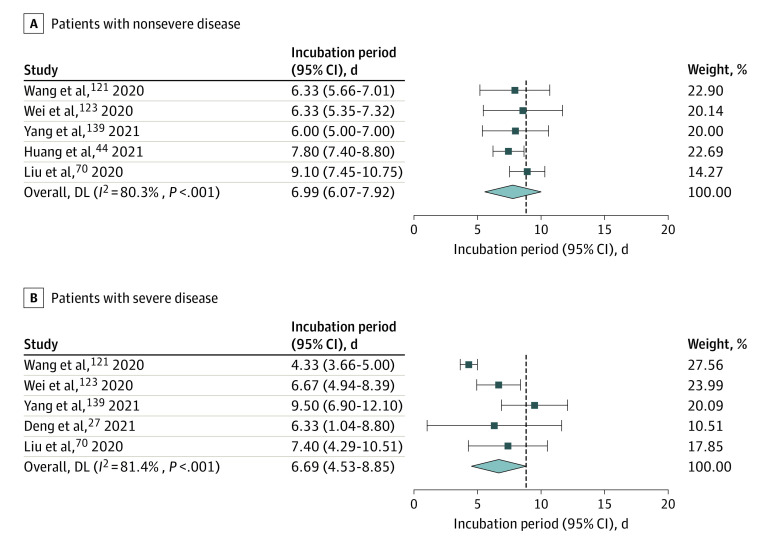
Five studies reported the incubation period in patients with nonsevere illness,44,70,121,123,139 with a pooled value of 6.99 days (95% CI, 6.07-7.92 days). Five studies analyzed the incubation period of patients with severe disease,27,70,121,123,139 with a pooled value of 6.69 days (95% CI, 4.53-8.85 days), which was slightly shorter than that of patients with nonsevere illness, but the difference was not significant (Figure 4).
Figure 4. Incubation Period for COVID-19 in Patients With Severe and Nonsevere Illness.
Infectious strains were original strains.
Discussion
Our findings suggested that COVID-19 had a mean incubation period of 6.57 days (95% CI, 6.26-6.88 days), which was similar to the results of Elias et al159 (6.38 days; 95% CI, 5.79-6.97 days) and McAloon et al14 (6.5 days, 95% CI, 5.9-7.1 days). COVID-19 seemed to have a longer incubation period than that of other acute respiratory viral infections such as human coronavirus (3.2 days), influenza A (1.43-1.64 days), parainfluenza (2.6 days), respiratory syncytial virus (4.4 days), and rhinovirus (1.4 days).160 Furthermore, the median incubation period for SARS in 2009 had been estimated as 4.0 days,160 which was lower than COVID-19. In this study, the shortest mean incubation reported was 1.8 days and the longest incubation was 18.87 days. At present, based on the assumption that the incubation period of COVID-19 is 1 to 14 days, the WHO still recommends that COVID-19 close contacts be isolated for 14 days.161
Our study found that the incubation period of COVID-19 caused by Alpha variant was 5.00 days (95% CI, 4.94-5.06 days), and the incubation period of COVID-19 caused by Beta variant was 4.50 days (95% CI, 1.83-7.17 days), which were similar to that of the wild-type strain in Wuhan, China (5.2 days).64,145
The Delta variant, which was first reported in India in October 2020, was dominant in the second wave of COVID-19 outbreak in India in May 2021.9 Our study revealed that the incubation period of COVID-19 caused by Delta variant was 4.41 days (95% CI, 3.76-5.05), which was shorter than the pooled incubation period of COVID-19 (6.26 days), and also shorter than that caused by Alpha variant and Beta variants.
On November 24, 2021, South Africa first discovered and reported a case of Omicron variant infection to the WHO. Since then, this variant has quickly become the main virus strain in South Africa and spread to many countries and regions around the world. The Omicron variant is exceptional for carrying over 30 mutations in the spike glycoprotein, which have been predicted to influence antibody neutralization and spike function.162 Our study revealed that the incubation period of COVID-19 caused by Omicron variant was 3.42 days (95% CI, 2.88-3.96 days), which was shorter than the Alpha, Beta, and Delta variants. The CDC released new quarantine and isolation policy on March 30, 2022, which stated that people exposed to COVID-19 should stay home and away from other people for at least 5 days.163 At present, some countries around the world require close contacts to be isolated for 14 days. However, with the shortening of the incubation period of new variants, the isolation period can be adjusted appropriately to reduce the pressure on the health system.
Eight studies reported the incubation period among older patients (ages 60 years and older), and the mean incubation period of older patients was about 7.43 days (95% CI, 5.75-9.11), which was slightly higher than the pooled incubation period among the general population. Although the difference between the incubation periods of older patients and the overall incubation period was not significant, there was still a lot of evidence to support the hypothesis of a longer incubation period in older populations due to a slower immune response among older patients. Cowling et al164 hypothesized about this in their report on SARS in 2007, where they demonstrated that older patients had longer incubation periods, suggesting that this might have resulted from a delayed immune response. A study by Chen et al165 revealed that several SARS-CoV nonstructural proteins that were shared by SARS-CoV-2 suppress the type 1 interferon response, and such suppression was shown to lead to poor CD8+ T-cell response to viral infection. Therefore, age-associated weaker type 1 interferon responses coupled with direct viral suppression could serve as a critical innate immune mechanism that leads to poor cell-mediated immunity and increased vulnerability of older adults to SARS-CoV-2 infection with therapeutic implication. Additionally, older patients were more likely to experience symptom minimization and be more likely to ignore early symptoms and only report later when symptoms become more severe or intolerable.111 The lack of a fever response in older patients, the nonspecific geriatric presentations in an infectious illness (such as falls and delirium), and multi-comorbidities might result in a delayed awareness of disease onset and its detection by a clinician.54
Additionally, our study also revealed that the mean incubation period for infected children (8.82 days; 95% CI, 8.19-9.45) was also shorter than the pooled incubation period among the general population (6.65 days). Infected children tend to present with mild clinical symptoms without the classic phenotype of lung pneumonia, and COVID-19 symptoms are easily confused with other influenza-like illnesses, which renders infected children difficult to identify.130 Second, previous studies found that children can be a source of transmission during the viral incubation period. Some infected children may have an incubation period of more than 14 days. Indeed, it is difficult for investigators to collect information about the symptoms of very young children because they cannot accurately express their symptoms.130
Previous studies on SARS indicated that the incubation period of patients was related to the severity of the disease, and the incubation period of fatal cases was shorter.166 Virlogeux et al167 also found that Middle East Respiratory Syndrome patients with a shorter incubation period proceeded to have more severe disease. However, there are few studies on the association between the length of COVID-19 incubation period and the severity of infection. Our study found that the incubation period of COVID-19 in patients with severe illness was shorter (6.69 days) than patients with nonsevere illness. Studies have indicated that shorter incubation periods are associated with more serious disease, and this is related to the number of cells initially infected by the virus.123
This study was the first meta-analysis of the incubation period of COVID-19 caused by SARS-CoV-2 variants. We compared the incubation period of COVID-19 caused by different variants and the wild-type strain, and the results may be helpful in changing public health guidance on duration of quarantine, outbreak investigation, and contact tracing.
Limitations
This study had several limitations. First, by definition, the required case data for the determination of individual incubation periods need to include both exposure (window) and onset of symptoms. In most studies, the data were collected retrospectively, resulting in a recall bias (uncertain exact dates of exposure) that would inevitably influence our assessment. Second, the estimate of the incubation period was computed with data with considerable heterogeneity. Possible sources of heterogeneity included difference in study population, data collection period, and method of analysis. Wild-type strain studies were mostly from Chinese patients; while variants studies were not. Population factors, especially those related to public policy and social behavior, may be confounding variables. In this study, we assumed that the incubation period was consistent across populations. Third, there were few studies on the incubation period of COVID-19 caused by SARS-CoV-2 variants. Because of the urgent timeline for data extraction and analysis, these studies have estimated the incubation period in a limited case number in a short period of time, which necessitates the cautious interpretation of the generalizability of our findings. The numbers were too small to detect systematic differences in incubation time in regards to age or sex.
Conclusions
Although variants such as Alpha, Beta, and Gamma are currently only prevalent in a few countries in Southeast Asia, South America, and Africa, the Delta and Omicron variants have become the dominant strains in many countries around the world. Identifying the incubation period of different variants is a key factor in determining the isolation period. The pooled incubation period of COVID-19 in this study was 6.57 days. The incubation period for COVID-19 caused by the Alpha and Beta variants was approximately 5 days. The incubation period of COVID-19 caused by the Delta and Omicron variants was significantly shorter than that of the other variants.
eTable 1. Search Strategies for Meta-analysis of Observational Studies Reporting the Incubation Period of COVID-19
eTable 2. Quality Assessment Scale
eTable 3. Quality Assessment of Final Studies Used in the Meta-analysis of Incubation Period
eTable 4. Characteristics of the Studies Included in the Systematic Review and Meta-analysis
eFigure 1. Funnel Plot with a 95% Confidence Interval for Included Studies in the Meta-analysis
eFigure 2. Forest Plot for the Meta-analysis of Incubation Period for COVID-19 Caused by Wild-type Strain
Reference
- 1.Guan W-J, Ni Z-Y, Hu Y, et al. ; China Medical Treatment Expert Group for Covid-19 . Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. doi: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . Coronavirus (COVID-19) Dashboard. 2022; https://covid19.who.int/.
- 3.Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;323(18):1824-1836. doi: 10.1001/jama.2020.6019 [DOI] [PubMed] [Google Scholar]
- 4.Gostic K, Gomez AC, Mummah RO, Kucharski AJ, Lloyd-Smith JO. Estimated effectiveness of symptom and risk screening to prevent the spread of COVID-19. Elife. 2020;9:9. doi: 10.7554/eLife.55570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tawe Ngi AM, Johnston S, Albayat SS, et al. Pre-symptomatic and asymptomatic transmission of COVID-19: Implications for control measures in Qatar. Qatar Med J. 2021;2021(3):59-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganyani T, Kremer C, Chen D, et al. Estimating the generation interval for coronavirus disease (COVID-19) based on symptom onset data, March 2020. Euro Surveill. 2020;25(17):2000257. doi: 10.2807/1560-7917.ES.2020.25.17.2000257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nishiura H, Mizumoto K, Ejima K, Zhong Y, Cowling B, Omori R. Incubation period as part of the case definition of severe respiratory illness caused by a novel coronavirus. Euro Surveill. 2012;17(42):20296. [PMC free article] [PubMed] [Google Scholar]
- 8.Nishiura H, Linton NM, Akhmetzhanov AR. Serial interval of novel coronavirus (COVID-19) infections. Int J Infect Dis. 2020;93:284-286. doi: 10.1016/j.ijid.2020.02.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization . Tracking SARS-CoV-2 variants. Updated July 19, 2022. Accessed April 17, 2022. https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/
- 10.US Centers for Disease Control and Prevention . SARS-CoV-2 Variant Classifications and Definitions. Updated April 26, 2021. Accessed April 17, 2022. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html#anchor_1632158885160
- 11.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Published 2021. Accessed April 17, 2022. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 14.McAloon C, Collins Á, Hunt K, et al. Incubation period of COVID-19: a rapid systematic review and meta-analysis of observational research. BMJ Open. 2020;10(8):e039652-e039652. doi: 10.1136/bmjopen-2020-039652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Melsen WG, Bootsma MC, Rovers MM, Bonten MJ. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin Microbiol Infect. 2014;20(2):123-129. doi: 10.1111/1469-0691.12494 [DOI] [PubMed] [Google Scholar]
- 16.Areekal B, Vijayan SM, Suseela MS. Risk factors, epidemiological and clinical outcome of close contacts of COVID-19 cases in a tertiary hospital in southern India. J Clin Diagn Res. 2021;15(3):LC34-LC37. [Google Scholar]
- 17.Backer JA, Eggink D, Andeweg SP, et al. Shorter serial intervals in SARS-CoV-2 cases with Omicron BA.1 variant compared with Delta variant, the Netherlands, 13 to 26 December 2021. Euro Surveill. 2022;27(6):2200042. doi: 10.2807/1560-7917.ES.2022.27.6.2200042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travelers from Wuhan, China, 20-28 January 2020. Euro Surveill. 2020;25(5):2000062. doi: 10.2807/1560-7917.ES.2020.25.5.2000062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bao C, Pan E, Ai J, et al. COVID-19 outbreak following a single patient exposure at an entertainment site: an epidemiological study. Transbound Emerg Dis. 2021;68(2):773-781. doi: 10.1111/tbed.13742 [DOI] [PubMed] [Google Scholar]
- 20.Brandal LT, MacDonald E, Veneti L, et al. Outbreak caused by the SARS-CoV-2 Omicron variant in Norway, November to December 2021. Euro Surveill. 2021;26(50):2101147. doi: 10.2807/1560-7917.ES.2021.26.50.2101147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bui LV, Nguyen HT, Levine H, et al. Estimation of the incubation period of COVID-19 in Vietnam. PLoS One. 2020;15(12):e0243889-e0243889. doi: 10.1371/journal.pone.0243889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen G, Wu MZ, Qin CJ, et al. Epidemiological analysis of 18 patients with COVID-19. Eur Rev Med Pharmacol Sci. 2020;24(23):12522-12526. [DOI] [PubMed] [Google Scholar]
- 23.Zhang W; Covid-Epidemiology Investigation Team; Laboratory Testing Team . Local outbreak of COVID-19 in Shunyi District attributed to an asymptomatic carrier with a history of stay in Indonesia—Beijing municipality, China, December 23, 2020. China CDC Wkly. 2021;3(10):214-217. doi: 10.46234/ccdcw2020.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dai J, Yang L, Zhao J. Probable longer incubation period for elderly COVID-19 cases: analysis of 180 contact tracing data in Hubei Province, China. Risk Manag Healthc Policy. 2020;13:1111-1117. doi: 10.2147/RMHP.S257907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Laval F, Grosset-Janin A, Delon F, et al. Lessons learned from the investigation of a COVID-19 cluster in Creil, France: effectiveness of targeting symptomatic cases and conducting contact tracing around them. BMC Infect Dis. 2021;21(1):457-457. doi: 10.1186/s12879-021-06166-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Del Águila-Mejía J, Wallmann R, Calvo-Montes J, Rodríguez-Lozano J, Valle-Madrazo T, Aginagalde-Llorente A. Secondary attack rate, transmission and incubation periods, and serial interval of SARS-CoV-2 Omicron variant, Spain. Emerg Infect Dis. 2022;28(6):1224-1228. doi: 10.3201/eid2806.220158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deng L, Li Z, Liu Y, et al. Epidemiological and clinical findings of discharge patients infected with the 2019 novel coronavirus (SARS-CoV-2) in Changchun, Northeast China: a retrospective cohort study. Acta Med Mediter. 2021;37(2):1147-1153. [Google Scholar]
- 28.Deng Y, You C, Liu Y, Qin J, Zhou X-H. Estimation of incubation period and generation time based on observed length-biased epidemic cohort with censoring for COVID-19 outbreak in China. Biometrics. 2021;77(3):929-941. doi: 10.1111/biom.13325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Denis F, Septans AL, Le Goff F, Jeanneau S, Lescure FX. Analysis of COVID-19 transmission sources in France by self-assessment before and after the partial lockdown: observational study. J Med Internet Res. 2021;23(5):e26932. doi: 10.2196/26932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ding K, Yi B, Chen Y, et al. Epidemic cluster of novel coronavirus disease 2019 in Ningbo city of Zhejiang province. Article in Chinese. Chin J Publ Health. 2020;36(04):498-502. [Google Scholar]
- 31.Dong XC, Li JM, Bai JY, et al. [Epidemiological characteristics of confirmed COVID-19 cases in Tianjin]. Article in Chinese. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(5):638-641. [DOI] [PubMed] [Google Scholar]
- 32.Du ZC, Gu J, Li JH, et al. [Estimating the distribution of COVID-19 incubation period by interval-censored data estimation method]. Article in Chinese. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(7):1000-1003. [DOI] [PubMed] [Google Scholar]
- 33.Gao Y, Hou L, Li Y, et al. Epidemiological investigation and analysis of 137 confirmed cases of COVID-19. Article in Chinese. Chinese Journal of Critical Care Medicine. 2020;40(03):232-236. [Google Scholar]
- 34.Gao Y, Ma X, Bi J, et al. Epidemiological and clinical differences of coronavirus disease 2019 patients with distinct viral exposure history. Virulence. 2020;11(1):1015-1023. doi: 10.1080/21505594.2020.1802870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grant R, Charmet T, Schaeffer L, et al. Impact of SARS-CoV-2 Delta variant on incubation, transmission settings and vaccine effectiveness: results from a nationwide case-control study in France. Lancet Reg Health Eur. 2022;13:100278-100278. doi: 10.1016/j.lanepe.2021.100278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guo C-X, He L, Yin J-Y, et al. Epidemiological and clinical features of pediatric COVID-19. BMC Med. 2020;18(1):250-250. doi: 10.1186/s12916-020-01719-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Han T. Outbreak investigation: transmission of COVID-19 started from a spa facility in a local community in Korea. Epidemiol Health. 2020;42:e2020056-e2020056. doi: 10.4178/epih.e2020056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Han T, Hua L, He S, et al. The epidemiological characteristics of cluster transmission of coronavirus disease 2019 (COVID-19): a multi-center study in Jiangsu Province. Am J Transl Res. 2020;12(10):6434-6444. [PMC free article] [PubMed] [Google Scholar]
- 39.Han YN, Feng ZW, Sun LN, et al. A comparative-descriptive analysis of clinical characteristics in 2019-coronavirus-infected children and adults. J Med Virol. 2020;92(9):1596-1602. doi: 10.1002/jmv.25835 [DOI] [PubMed] [Google Scholar]
- 40.Hong H, Shi HB, Jiang HB, et al. [Epidemic dynamic model based evaluation of effectiveness of prevention and control strategies for COVID-19 in Ningbo]. Article in Chinese. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(10):1606-1610. [DOI] [PubMed] [Google Scholar]
- 41.Hua C-Z, Miao Z-P, Zheng J-S, et al. Epidemiological features and viral shedding in children with SARS-CoV-2 infection. J Med Virol. 2020;92(11):2804-2812. doi: 10.1002/jmv.26180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang J, Zhao Q, Xu K, et al. Analysis of COVID-19 epidemic characteristics based on network data. Article in Chinese. Chinese Journal of Disease Control & Prevention. 2020;24(11):1338. [Google Scholar]
- 43.Huang L, Zhang X, Xu A. Effectiveness of interventions as part of the One Health approach to control coronavirus disease 2019 and stratified case features in Anhui Province, China: a real-world population-based cohort study. One Health. 2021;12:100224-100224. doi: 10.1016/j.onehlt.2021.100224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huang S, Li J, Dai C, et al. Incubation period of coronavirus disease 2019: new implications for intervention and control. Int J Environ Health Res. 2021;32(8):1707-1715. [DOI] [PubMed] [Google Scholar]
- 45.Je D, O’Brolchain A, Ulett KB, et al. Demographics, clinical characteristics and outcomes among 197 patients with COVID-19 in the Gold Coast area. Intern Med J. 2021;51(5):666-672. doi: 10.1111/imj.15260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jeong TH, Pak C, Ock M, Lee SH, Son JS, Jeon YJ. Real asymptomatic SARS-CoV-2 infection might be rare: importance of careful interviews and follow-up. J Korean Med Sci. 2020;35(37):e333-e333. doi: 10.3346/jkms.2020.35.e333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jiang G, Wang C, Song L, et al. Aerosol transmission, an indispensable route of COVID-19 spread: case study of a department-store cluster. Front Environ Sci Eng. 2021;15(3):46. doi: 10.1007/s11783-021-1386-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jiang Z, Yang B, Qin J, Zhou Y. Enhanced empirical likelihood estimation of incubation period of COVID-19 by integrating published information. Stat Med. 2021;40(19):4252-4268. doi: 10.1002/sim.9026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jin X, Lian J-S, Hu J-H, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002-1009. doi: 10.1136/gutjnl-2020-320926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khonyongwa K, Taori SK, Soares A, et al. Incidence and outcomes of healthcare-associated COVID-19 infections: significance of delayed diagnosis and correlation with staff absence. J Hosp Infect. 2020;106(4):663-672. doi: 10.1016/j.jhin.2020.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ki HJ, Kim J, Kim S, Park J, Lee J, Kim Y-J. Statistical analysis of estimating incubation period distribution and case fatality rate of COVID-19. Korean Journal of Applied Statistics. 2020;33(6):777-789. [Google Scholar]
- 52.Kim SE, Jeong HS, Yu Y, et al. Viral kinetics of SARS-CoV-2 in asymptomatic carriers and presymptomatic patients. Int J Infect Dis. 2020;95:441-443. doi: 10.1016/j.ijid.2020.04.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kong D, Zheng Y, Wu H, et al. Pre-symptomatic transmission of novel coronavirus in community settings. Influenza Other Respir Viruses. 2020;14(6):610-614. doi: 10.1111/irv.12773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kong T-K. Longer incubation period of coronavirus disease 2019 (COVID-19) in older adults. Aging Med (Milton). 2020;3(2):102-109. doi: 10.1002/agm2.12114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kong W, Wang Y, Hu J, Chughtai A, Pu H; Clinical Research Collaborative Group of Sichuan Provincial People’s Hospital . Comparison of clinical and epidemiological characteristics of asymptomatic and symptomatic SARS-CoV-2 infection: a multi-center study in Sichuan Province, China. Travel Med Infect Dis. 2020;37:101754-101754. doi: 10.1016/j.tmaid.2020.101754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lai C, Yu R, Wang M, et al. Shorter incubation period is associated with severe disease progression in patients with COVID-19. Virulence. 2020;11(1):1443-1452. doi: 10.1080/21505594.2020.1836894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lau YC, Tsang TK, Kennedy-Shaffer L, et al. Joint estimation of generation time and incubation period for coronavirus disease (Covid-19). J Infect Dis. 2021;224(10):1664-1671. doi: 10.1093/infdis/jiab424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Le TQM, Takemura T, Moi ML, et al. Severe acute respiratory syndrome coronavirus 2 shedding by travelers, Vietnam, 2020. Emerg Infect Dis. 2020;26(7):1624-1626. doi: 10.3201/eid2607.200591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee JJ, Choe YJ, Jeong H, et al. Importation and transmission of SARS-CoV-2 B.1.1.529 (Omicron) variant of concern in Korea, November 2021. J Korean Med Sci. 2021;36(50):e346-e346. doi: 10.3346/jkms.2021.36.e346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lei D, Wang C, Li C, et al. Clinical characteristics of COVID-19 in pregnancy: analysis of nine cases. Article in Chinese. Chinese Journal of Perinatal Medicine. 2020;12:222-228. [Google Scholar]
- 61.Leung C. The difference in the incubation period of 2019 novel coronavirus (SARS-CoV-2) infection between travelers to Hubei and nontravelers: the need for a longer quarantine period. Infect Control Hosp Epidemiol. 2020;41(5):594-596. doi: 10.1017/ice.2020.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li J, Ding J, Chen L, et al. Epidemiological and clinical characteristics of three family clusters of COVID-19 transmitted by latent patients in China. Epidemiol Infect. 2020;148:e137-e137. doi: 10.1017/S0950268820001491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li L, Han Z-G, Qin P-Z, et al. Transmission and containment of the SARS-CoV-2 Delta variant of concern in Guangzhou, China: a population-based study. PLoS Negl Trop Dis. 2022;16(1):e0010048-e0010048. doi: 10.1371/journal.pntd.0010048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199-1207. doi: 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Linton NM, Kobayashi T, Yang Y, et al. Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: a statistical analysis of publicly available case data. J Clin Med. 2020;9(2):538. doi: 10.3390/jcm9020538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu C-X, Liu Z-H, Sun L-Y, Zhang K-Y, Sun Y-Z. A familial cluster of COVID-19 infection in a northern Chinese region. J Infect Public Health. 2021;14(9):1127-1132. doi: 10.1016/j.jiph.2021.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liu F, Ji C, Luo J, et al. Clinical characteristics and corticosteroids application of different clinical types in patients with corona virus disease 2019. Sci Rep. 2020;10(1):13689-13689. doi: 10.1038/s41598-020-70387-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu J, Liao X, Qian S, et al. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis. 2020;26(6):1320-1323. doi: 10.3201/eid2606.200239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu JY, Chen TJ, Hwang SJ. Analysis of community-acquired COVID-19 cases in Taiwan. J Chin Med Assoc. 2020;83(12):1087-1092. doi: 10.1097/JCMA.0000000000000411 [DOI] [PubMed] [Google Scholar]
- 70.Liu L, Du Y, Bai J, et al. Analysis of early characteristics of patients with novel coronavirus infection in Kunming City, Yunnan Province, China. Article in Chinese. Chinese Journal of Zoonoses. 2020;36(5):424-428. [Google Scholar]
- 71.Liu L, Jing L, Li Y, et al. Clustering of 2019 novel coronavirus disease cases in Liaoning province: reported data-base analysis. Article in Chinese. Chin J Publ Health. 2020;36(04):473-476. doi: 10.11847/zgggws1128823 [DOI] [Google Scholar]
- 72.Liu P, Niu R, Chen J, et al. Epidemiological and clinical features in patients with coronavirus disease 2019 outside of Wuhan, China: special focus in asymptomatic patients. PLoS Negl Trop Dis. 2021;15(3):e0009248-e0009248. doi: 10.1371/journal.pntd.0009248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Liu W, Zhou M, Yang S, et al. Epidemiological characteristics of cluster cases of coronavirus disease 2019 (COVID-19) in China. Acta Medicinae Universitatis Scientiae et Technologiae Huazhong. 2020;49(02):161-168. [Google Scholar]
- 74.Liu Y, Ding N, Zhou S, et al. Comparison of clinical characteristics between patients with coronavirus disease 2019 (COVID-19) who retested RT-PCR positive versus negative: a retrospective study of data from Nanjing. J Thorac Dis. 2020;12(11):6435-6445. doi: 10.21037/jtd.2020.04.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Llaque-Quiroz P, Prudencio-Gamio R, Echevarría-Lopez S, Ccorahua-Paz M, Ugas-Charcape C. Clinical and epidemiological characteristics of children with COVID-19 in a pediatric hospital in Peru. Rev Peru Med Exp Salud Publica. 2020;37(4):689-693. doi: 10.17843/rpmesp.2020.374.6198 [DOI] [PubMed] [Google Scholar]
- 76.Mao S, Huang T, Yuan H, et al. Epidemiological analysis of 67 local COVID-19 clusters in Sichuan Province, China. BMC Public Health. 2020;20(1):1525-1525. doi: 10.1186/s12889-020-09606-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Moazzami B, Moezedin Javad R, Samie S, et al. Is Computed tomography necessary for the diagnosis of coronavirus disease (COVID-19) in all suspected patients? a case series. J Kerman Univ Med Sci. 2021;2:187-193. [Google Scholar]
- 78.Ng T-C, Cheng H-Y, Chang H-H, et al. Comparison of estimated effectiveness of case-based and population-based interventions on COVID-19 containment in Taiwan. JAMA Intern Med. 2021;181(7):913-921. doi: 10.1001/jamainternmed.2021.1644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nie X, Fan L, Mu G, et al. Epidemiological characteristics and incubation period of 7015 confirmed cases with coronavirus disease 2019 outside Hubei Province in China. J Infect Dis. 2020;222(1):26-33. doi: 10.1093/infdis/jiaa211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ogata T, Tanaka H, Irie F, Hirayama A, Takahashi Y. Shorter incubation period among unvaccinated delta variant coronavirus disease 2019 patients in Japan. Int J Environ Res Public Health. 2022;19(3):1127. doi: 10.3390/ijerph19031127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pak D, Langohr K, Ning J, Cortés Martínez J, Gómez Melis G, Shen Y. Modeling the coronavirus disease 2019 incubation period: impact on quarantine policy. Mathematics. 2020;8(9):1631. doi: 10.3390/math8091631 [DOI] [Google Scholar]
- 82.Pan XX, Chen Y, Wang AH, et al. [Study on transmission dynamic of 15 clusters of COVID-2019 cases in Ningbo]. Article in Chinese. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(12):2010-2014. [DOI] [PubMed] [Google Scholar]
- 83.Patrikar SR, Kotwal A, Bhatti VK, et al. Incubation period and reproduction number for novel coronavirus 2019 (COVID-19) infections in India. Asia Pac J Public Health. 2020;32(8):458-460. doi: 10.1177/1010539520956427 [DOI] [PubMed] [Google Scholar]
- 84.Paul S, Lorin E. Distribution of incubation periods of COVID-19 in the Canadian context. Sci Rep. 2021;11(1):12569-12569. doi: 10.1038/s41598-021-91834-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ping K, Lei M, Gou Y, et al. Epidemiologic characteristics of COVID-19 in Guizhou Province, China. J Infect Dev Ctries. 2021;15(3):389-397. doi: 10.3855/jidc.12818 [DOI] [PubMed] [Google Scholar]
- 86.Pongpirul WA, Wiboonchutikul S, Charoenpong L, et al. Clinical course and potential predictive factors for pneumonia of adult patients with Coronavirus Disease 2019 (COVID-19): a retrospective observational analysis of 193 confirmed cases in Thailand. PLoS Negl Trop Dis. 2020;14(10):e0008806-e0008806. doi: 10.1371/journal.pntd.0008806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pung R, Chiew CJ, Young BE, et al. ; Singapore 2019 Novel Coronavirus Outbreak Research Team . Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395(10229):1039-1046. doi: 10.1016/S0140-6736(20)30528-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Qi B, Peng H, Shou K, et al. Protecting healthcare professionals during the COVID-19 pandemic. Biomed Res Int. 2020;2020:8469560-8469560. doi: 10.1155/2020/8469560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Qian GQ, Yang NB, Ding F, et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: a retrospective, multi-centre case series. QJM. 2020;113(7):474-481. doi: 10.1093/qjmed/hcaa089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Qiu C, Deng Z, Xiao Q, et al. Transmission and clinical characteristics of coronavirus disease 2019 in 104 outside-Wuhan patients, China. J Med Virol. 2020;92(10):2027-2035. doi: 10.1002/jmv.25975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ratovoson R, Razafimahatratra R, Randriamanantsoa L, et al. Household transmission of COVID-19 among the earliest cases in Antananarivo, Madagascar. Influenza Other Respir Viruses. 2022;16(1):48-55. doi: 10.1111/irv.12896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ren X, Li Y, Yang X, et al. Evidence for pre-symptomatic transmission of coronavirus disease 2019 (COVID-19) in China. Influenza Other Respir Viruses. 2021;15(1):19-26. doi: 10.1111/irv.12787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Samrah SM, Al-Mistarehi A-H, Kewan T, et al. Viral clearance course of COVID-19 outbreaks. J Multidiscip Healthc. 2021;14:555-565. doi: 10.2147/JMDH.S302891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470-1477. doi: 10.3201/eid2607.200282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shen Q, Guo W, Guo T, et al. Novel coronavirus infection in children outside of Wuhan, China. Pediatr Pulmonol. 2020;55(6):1424-1429. doi: 10.1002/ppul.24762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shen Y, Xu W, Li C, et al. A cluster of novel coronavirus disease 2019 infections indicating person-to-person transmission among casual contacts from social gatherings: an outbreak case-contact investigation. Open Forum Infect Dis. 2020;7(6):ofaa231. doi: 10.1093/ofid/ofaa231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shi J-C, Yu Z-J, He G-Q, et al. Epidemiological features of 105 patients infected with the COVID-19. J Natl Med Assoc. 2021;113(2):212-217. doi: 10.1016/j.jnma.2020.09.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shi P, Gao Y, Shen Y, et al. Characteristics and evaluation of the effectiveness of monitoring and control measures for the first 69 patients with COVID-19 from 18 January 2020 to 2 March in Wuxi, China. Sustain Cities Soc. 2021;64:102559-102559. doi: 10.1016/j.scs.2020.102559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shiel E, Miyakis S, Tennant E, et al. Clinical characteristics and outcomes of COVID-19 in a low-prevalence, well resourced setting, Sydney, Australia. Intern Med J. 2021;51(10):1605-1613. doi: 10.1111/imj.15445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Shu Y, Deng Z, Wang H, et al. Epidemiological and clinical characteristics of 32 patients with COVID-19. Can J Infect Control. 2020;19(08):679-686. [Google Scholar]
- 101.Song Q, Zhao H, Fang L, Liu W, Zheng C, Zhang Y. Study on assessing early epidemiological parameters of coronavirus disease epidemic in China. Article in Chinese. Chinese Journal of Epidemiology. 2020;41(4):461-465. doi: 10.3760/cma.j.cn112338-20200205-00069 [DOI] [PubMed] [Google Scholar]
- 102.Song R, Han B, Song M, et al. Clinical and epidemiological features of COVID-19 family clusters in Beijing, China. J Infect. 2020;81(2):e26-e30. doi: 10.1016/j.jinf.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Song YS, Hao YB, Liu WW, Zhang SS, Wang P, Fan TL. Clinical features of 17 patients with 2019-nCoV. Eur Rev Med Pharmacol Sci. 2020;24(20):10896-10901. [DOI] [PubMed] [Google Scholar]
- 104.Su YJ, Kuo KC, Wang TW, Chang CW. Gender-based differences in COVID-19. New Microbes New Infect. 2021;42:100905-100905. doi: 10.1016/j.nmni.2021.100905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sugano N, Ando W, Fukushima W. Cluster of severe acute respiratory syndrome coronavirus 2 infections linked to music clubs in Osaka, Japan. J Infect Dis. 2020;222(10):1635-1640. doi: 10.1093/infdis/jiaa542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sun B, Qi Y, Chen H, et al. Epidemiological profile of a cluster of COVID-19 caused by an imported case. Article in Chinese. Chin J Prev Med. 2021;22(04):246-249. [Google Scholar]
- 107.Sun C, Zhang XB, Dai Y, Xu XZ, Zhao J. [Clinical analysis of 150 cases of 2019 novel coronavirus infection in Nanyang City, Henan Province]. Article in Chinese. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(6):503-508. [DOI] [PubMed] [Google Scholar]
- 108.Sun L, Shen L, Fan J, et al. Clinical features of patients with coronavirus disease 2019 from a designated hospital in Beijing, China. J Med Virol. 2020;92(10):2055-2066. doi: 10.1002/jmv.25966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sun YM, Liu F, Cai W, et al. [Transmission chains of clusters of COVID-19 associated with a market in Beijing]. Article in Chinese. Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42(3):427-432. [DOI] [PubMed] [Google Scholar]
- 110.Sun Y, Tian L, Du X, Wang H, Li Y, Wu R. Epidemiological and clinical characteristics of a familial cluster of COVID-19. Epidemiol Infect. 2020;148:e145-e145. doi: 10.1017/S0950268820001521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Tan WYT, Wong LY, Leo YS, Toh MPHS. Does incubation period of COVID-19 vary with age? a study of epidemiologically linked cases in Singapore. Epidemiol Infect. 2020;148:e197-e197. doi: 10.1017/S0950268820001995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Tanaka H, Ogata T, Shibata T, et al. Shorter incubation period among COVID-19 cases with the BA.1 Omicron variant. Int J Environ Res Public Health. 2022;19(10):6330. doi: 10.3390/ijerph19106330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.SARS-CoV-2 variant with lineage B.1.351 clusters investigation team . Linked transmission chains of imported SARS-CoV-2 variant B.1.351 across mainland France, January 2021. Euro Surveill. 2021;26(13):2100333. doi: 10.2807/1560-7917.ES.2021.26.13.2100333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Tian S, Hu N, Lou J, et al. Characteristics of COVID-19 infection in Beijing. J Infect. 2020;80(4):401-406. doi: 10.1016/j.jinf.2020.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tindale LC, Stockdale JE, Coombe M, et al. Evidence for transmission of COVID-19 prior to symptom onset. Elife. 2020;9:e57149. doi: 10.7554/eLife.57149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Viego V, Geri M, Castiglia J, Jouglard E. Incubation period and serial interval of Covid-19 in a chain of infections in Bahia Blanca (Argentina). Cien Saude Colet. 2020;25(9):3503-3510. doi: 10.1590/1413-81232020259.20852020 [DOI] [PubMed] [Google Scholar]
- 117.Wang J, Wang S, Yang S, et al. Epidemiological characteristics of 17 coronavirus disease 2019 in Puyang, Henan. Article in Chinese. Chinese Journal of Disease Control & Prevention. 2021;25(04):416-420. [Google Scholar]
- 118.Wang X, Gao J, Wang X, Hu W, Liu H. Clinical and epidemiological characteristics of patients with COVID. Can J Infect Control. 2020;19(03):223-226. doi: 10.3389/fpubh.2020.00244 [DOI] [Google Scholar]
- 119.Wang X, Pan Y, Zhang D, et al. Basic epidemiological parameter values from data of real-world in mega-cities: the characteristics of COVID-19 in Beijing, China. BMC Infect Dis. 2020;20(1):526-526. doi: 10.1186/s12879-020-05251-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang X, Zhou Q, He Y, et al. Nosocomial outbreak of COVID-19 pneumonia in Wuhan, China. Eur Respir J. 2020;55(6):2000544. doi: 10.1183/13993003.00544-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wang Y, Liao B, Guo Y, et al. Clinical characteristics of patients infected with the novel 2019 coronavirus (SARS-Cov-2) in Guangzhou, China. Open Forum Infect Dis. 2020;7(6):ofaa187. doi: 10.1093/ofid/ofaa187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wei X. Analysis of clinical characteristics of 28 cases of COVID-19. Article in Chinese. Chinese Journal of Integrated Traditional and Western Medicine. 2021;28(3). [Google Scholar]
- 123.Wei Y, Zeng W, Huang X, et al. Clinical characteristics of 276 hospitalized patients with coronavirus disease 2019 in Zengdu District, Hubei Province: a single-center descriptive study. BMC Infect Dis. 2020;20(1):549-549. doi: 10.1186/s12879-020-05252-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Won YS, Kim J-H, Ahn CY, Lee H. Subcritical transmission in the early stage of COVID-19 in Korea. Int J Environ Res Public Health. 2021;18(3):1265. doi: 10.3390/ijerph18031265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wong J, Chaw L, Koh WC, et al. Epidemiological investigation of the first 135 COVID-19 cases in Brunei: implications for surveillance, control, and travel restrictions. Am J Trop Med Hyg. 2020;103(4):1608-1613. doi: 10.4269/ajtmh.20-0771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wu J, Chen X, Gong L, et al. Epidemiological and clinical features of SARS-CoV-2 cluster infection in Anhui Province, Eastern China. Int J Infect Dis. 2021;117:372-377. doi: 10.1016/j.ijid.2021.04.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wu J, Xia J, Yang Q, et al. Clinical characteristics of SARS-CoV-2 infection at early stage. Article in Chinese. Chinese Journal of Infection and Chemotherapy. 2020;20(05):521-524. [Google Scholar]
- 128.Wu W, Liu Y, Wei Z, et al. Investigation and analysis on characteristics of a cluster of COVID-19 associated with exposure in a department store in Tianjin. Article in Chinese. Chin J Epidemiol. 2020;41(4):489-493. doi: 10.3760/cma.j.cn112338-20200221-00139 [DOI] [PubMed] [Google Scholar]
- 129.Wu Y. Epidemiological and clinical characteristics of 41 patients with COVID-19. Article in Chinese. Chinese Journal of Integrated Traditional and Western Medicine. 2020;27(4). [Google Scholar]
- 130.Xiao F, Chen B, Xiao T, Lee SK, Yan K, Hu L. Children with SARS-CoV-2 infection during an epidemic in China (outside of Hubei province). Ann Transl Med. 2020;8(14):849-849. doi: 10.21037/atm-20-2908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Xiao M, Hou M, Liu X, Li Z, Zhao Q. Clinical characteristics of 71 patients with coronavirus disease 2019. Article in Chinese. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2020;45(7):790-796. doi: 10.11817/j.issn.1672-7347.2020.200187 [DOI] [PubMed] [Google Scholar]
- 132.Xiao Z, Guo W, Luo Z, Liao J, Wen F, Lin Y. Examining geographical disparities in the incubation period of the COVID-19 infected cases in Shenzhen and Hefei, China. Environ Health Prev Med. 2021;26(1):10-10. doi: 10.1186/s12199-021-00935-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Xiao Z, Xie X, Guo W, et al. Examining the incubation period distributions of COVID-19 on Chinese patients with different travel histories. J Infect Dev Ctries. 2020;14(4):323-327. doi: 10.3855/jidc.12718 [DOI] [PubMed] [Google Scholar]
- 134.Xie S, Zhang G, Yu H, et al. The epidemiologic and clinical features of suspected and confirmed cases of imported 2019 novel coronavirus pneumonia in north Shanghai, China. Ann Transl Med. 2020;8(10):637-637. doi: 10.21037/atm-20-2119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Xin H, Li Y, Wu P, et al. Estimating the latent period of coronavirus disease 2019 (COVID-19). Clin Infect Dis. 2022;74(9):1678-1681. doi: 10.1093/cid/ciab746 [DOI] [PubMed] [Google Scholar]
- 136.Xu T, Chen C, Zhu Z, et al. Clinical features and dynamics of viral load in imported and non-imported patients with COVID-19. Int J Infect Dis. 2020;94:68-71. doi: 10.1016/j.ijid.2020.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Xu X-W, Wu X-X, Jiang X-G, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606-m606. doi: 10.1136/bmj.m606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yang HY, Xu J, Li Y, et al. [The preliminary analysis on the characteristics of the cluster for the COVID-19]. Article in Chinese. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(5):623-628. [DOI] [PubMed] [Google Scholar]
- 139.Yang J, Wu K, Ding A, et al. Clinical characteristics, treatment, and prognosis of 74 2019 novel coronavirus disease patients in Hefei: a single-center retrospective study. Medicine (Baltimore). 2021;100(21):e25645-e25645. doi: 10.1097/MD.0000000000025645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yang N, Shen Y, Shi C, et al. In-flight transmission cluster of COVID-19: a retrospective case series. Infect Dis (Lond). 2020;52(12):891-901. doi: 10.1080/23744235.2020.1800814 [DOI] [PubMed] [Google Scholar]
- 141.You C, Deng Y, Hu W, et al. Estimation of the time-varying reproduction number of COVID-19 outbreak in China. Int J Hyg Environ Health. 2020;228:113555-113555. doi: 10.1016/j.ijheh.2020.113555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Yu S, Cui S, Rui J, et al. Epidemiological characteristics and transmissibility for SARS-CoV-2 of population level and cluster level in a Chinese city. Front Public Health. 2022;9:799536-799536. doi: 10.3389/fpubh.2021.799536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yu X, Sun X, Cui P, et al. Epidemiological and clinical characteristics of 333 confirmed cases with coronavirus disease 2019 in Shanghai, China. Transbound Emerg Dis. 2020;67(4):1697-1707. doi: 10.1111/tbed.13604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Zhang H, Song S, Chen Z, et al. A Cluster transmission of coronavirus disease 2019 and the prevention and control measures in the early stage of the epidemic in Xi’an, China, 2020. Med Sci Monit. 2021;27:e929701-e929701. doi: 10.12659/MSM.929701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zhang J, Litvinova M, Wang W, et al. Evolving epidemiology and transmission dynamics of coronavirus disease 2019 outside Hubei province, China: a descriptive and modelling study. Lancet Infect Dis. 2020;20(7):793-802. doi: 10.1016/S1473-3099(20)30230-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zhang K, Zhang Y, Li M, Yu M, Cha L, Ruan L. Comparative analysis of clinical characteristics of imported and local family clusters of novel coronavirus pneumonia. Article in Chinese. Chinese Journal of Integrated Traditional and Western Medicine. 2020;27(4):385-389. [Google Scholar]
- 147.Zhang Q, Zhu J, Jia C, Xu S, Jiang T, Wang S. Epidemiology and clinical outcomes of COVID-19 patients in northwestern China who had a history of exposure in Wuhan City: departure time-originated pinpoint surveillance. Front Med (Lausanne). 2021;8:582299-582299. doi: 10.3389/fmed.2021.582299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zhang T, Ding S, Zeng Z, et al. Estimation of incubation period and serial interval for SARS-CoV-2 in Jiangxi, China, and an updated meta-analysis. J Infect Dev Ctries. 2021;15(3):326-332. doi: 10.3855/jidc.14025 [DOI] [PubMed] [Google Scholar]
- 149.Zhao C, Xu Y, Zhang X, et al. Public health initiatives from hospitalized patients with COVID-19, China. J Infect Public Health. 2020;13(9):1229-1236. doi: 10.1016/j.jiph.2020.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zhao H, Zhang Z, Lun W, et al. Transmission dynamics and successful control measures of SARS-CoV-2 in the mega-size city of Guangzhou, China. Medicine (Baltimore). 2021;100(48):e27846. doi: 10.1097/MD.0000000000027846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zhao S, Tang B, Musa SS, et al. Estimating the generation interval and inferring the latent period of COVID-19 from the contact tracing data. Epidemics. 2021;36:100482-100482. doi: 10.1016/j.epidem.2021.100482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhao WH, Ma Y, Wang H, et al. [Epidemiological characteristics of three local epidemics of COVID-19 in Guangzhou]. Article in Chinese. Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42(12):2088-2095. [DOI] [PubMed] [Google Scholar]
- 153.Zhao Z, Yin M, Yin S, et al. Analysis of clinical characteristics of 26 cases of COVID-19. Article in Chinese. Chinese Journal of Disease Control & Prevention. 2020;24(05):539-542. [Google Scholar]
- 154.Zhong S, Lin F, Shi L. Clinical characteristics and outcomes of the patients with COVID-19: a report of 62 cases. Article in Chinese. Medical Journal of Chinese People’s Liberation Army. 2020;45(04):370-374. [Google Scholar]
- 155.Zhu J, Zhang Q, Jia C, et al. Challenges caused by imported cases abroad for the prevention and control of COVID-19 in China. Front Med (Lausanne). 2021;8:573726-573726. doi: 10.3389/fmed.2021.573726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zhu N, Chen S, Yang G, et al. Analysis of the path from discovery of novel coronavirus disease 2019 cases to its diagnosis in Shaanxi Province. Article in Chinese. Xi’an Jiaotong Daxue Xuebao Yixue Ban. 2020;41(06):923-926. [Google Scholar]
- 157.Zhu W, Zhang M, Pan J, Yao Y, Wang W. Effects of prolonged incubation period and centralized quarantine on the COVID-19 outbreak in Shijiazhuang, China: a modeling study. BMC Med. 2021;19(1):308-308. doi: 10.1186/s12916-021-02178-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Wang Y, Liao B, Guo Y, et al. Clinical characteristics of patients infected with the novel 2019 coronavirus (SARS-Cov-2) in Guangzhou, China. Open Forum Infect Dis. 2020;7(6):ofaa187. doi: 10.1093/ofid/ofaa187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Elias C, Sekri A, Leblanc P, Cucherat M, Vanhems P. The incubation period of COVID-19: a meta-analysis. Int J Infect Dis. 2021;104:708-710. doi: 10.1016/j.ijid.2021.01.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Lessler J, Reich NG, Brookmeyer R, Perl TM, Nelson KE, Cummings DA. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis. 2009;9(5):291-300. doi: 10.1016/S1473-3099(09)70069-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.World Health Organization . Coronavirus disease (COVID-19). Updated May 13, 2021. Accessed April 17, 2022. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19
- 162.Cao Y, Wang J, Jian F, et al. Omicron escapes the majority of existing SARS-CoV-2 neutralizing antibodies. Nature. 2022;602(7898):657-663. doi: 10.1038/s41586-021-04385-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.US Centers for Disease Control and Prevention . Quarantine and Isolation. Updated March 30, 2022. Accessed April 17, 2022. https://www.cdc.gov/coronavirus/2019-ncov/your-health/quarantine-isolation.html
- 164.Cowling BJ, Muller MP, Wong IO, et al. Alternative methods of estimating an incubation distribution: examples from severe acute respiratory syndrome. Epidemiology. 2007;18(2):253-259. doi: 10.1097/01.ede.0000254660.07942.fb [DOI] [PubMed] [Google Scholar]
- 165.Chen Y, Klein SL, Garibaldi BT, et al. Aging in COVID-19: vulnerability, immunity and intervention. Ageing Res Rev. 2021;65:101205-101205. doi: 10.1016/j.arr.2020.101205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Virlogeux V, Fang VJ, Wu JT, et al. Brief report: incubation period duration and severity of clinical disease following severe acute respiratory syndrome coronavirus infection. Epidemiology. 2015;26(5):666-669. doi: 10.1097/EDE.0000000000000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Virlogeux V, Park M, Wu JT, Cowling BJ. Association between severity of MERS-CoV infection and incubation period. Emerg Infect Dis. 2016;22(3):526-528. doi: 10.3201/eid2203.151437 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Search Strategies for Meta-analysis of Observational Studies Reporting the Incubation Period of COVID-19
eTable 2. Quality Assessment Scale
eTable 3. Quality Assessment of Final Studies Used in the Meta-analysis of Incubation Period
eTable 4. Characteristics of the Studies Included in the Systematic Review and Meta-analysis
eFigure 1. Funnel Plot with a 95% Confidence Interval for Included Studies in the Meta-analysis
eFigure 2. Forest Plot for the Meta-analysis of Incubation Period for COVID-19 Caused by Wild-type Strain