Abstract
Background
Hepatozoon canis is a protozoal agent that is known to be transmitted by oral uptake of H. canis-infected Rhipicephalus sanguineus sensu lato ticks in dogs. Vertical transmission of H. canis has only been described once in a study evaluating dogs from Japan. The aim of this study was to investigate the parasitological status of puppies from a bitch that had tested positive for Hepatozoon spp. prior to giving birth.
Findings
A 4-year-old, female, pregnant dog imported from Italy (Sardinia) to Germany showed clinical signs of lethargy and tachypnoea and tested positive for H. canis by PCR. The dog gave birth to eight puppies, one of which was stillborn and another that had to be reanimated. Haematology, buffy coat analysis and a biochemistry profile were performed for each dog. EDTA-blood of the surviving seven puppies and bone marrow, liver, spleen, amniotic fluid, and umbilical cord of the stillborn puppy was tested for the presence of Hepatozoon spp. by PCR.
The mother and the seven surviving puppies tested positive for H. canis by PCR at day 62 post-partum. Gamonts were detected in all dogs by buffy coat evaluation. Haematological and biochemistry results revealed mild abnormalities. In the stillborn puppy, spleen, umbilical cord, and amniotic fluid were positive for H. canis.
Conclusion
The results confirm that vertical transmission is a possible route of H. canis infection in dogs, demonstrated by molecular detection of the pathogen in the stillborn puppy. In the seven surviving puppies, vertical transmission was the most likely transmission route. A potential impact of the level of parasitaemia on the health of puppies, as well as its pathogenesis, should be investigated further.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s13071-022-05392-7.
Keywords: Hepatozoonosis, Canine, Transplacental, Infection, Hepatozoon canis
Main text
Hepatozoon canis, H. americanum and other Hepatozoon spp. are protozoal, apicomplexan agents. Blood-feeding arthropods are known as biological vectors for Hepatozoon spp., and their vertebrate hosts include dogs, cats, rodents, birds, reptiles and amphibians, which are susceptible to and affected by potential infection [1, 2]. In Germany, H. canis was previously detected by polymerase chain reaction (PCR) in 0–11% of dogs with a travel history [3–7]. In dogs in Europe, H. canis is thought to mainly be transmitted by the ingestion of Rhipicephalus sanguineus sensu lato (s.l.) ticks harbouring mature oocysts [8]. In northern Germany, a large proportion of the fox population tested positive for H. canis by PCR, with genotypes typically found in dogs [9]. Thus, foxes are thought to be potential pathogen reservoirs and alternative tick vectors, or alternative transmission routes are likely to be responsible for transmission within the fox population, as R. sanguineus s.l. ticks are not endemic in northern Germany [9]. Hepatozoon canis oocysts have also been detected in other tick species, including Rhipicephalus microplus, Haemaphysalis longicornis and Haemaphysalis flava [10, 11]. Amblyomma ovale was experimentally shown to be a suitable vector for H. canis in South America [12], but none of these tick species is endemic in Germany. Ixodes ricinus is widespread in Europe and H. canis DNA was detected in one I. ricinus tick collected from the environment in Italy [13], but additional studies suggested that this tick species does not act as a vector for H. canis [14]. Transstadial transmission of H. canis from R. sanguineus s.l. larvae to nymphs has been described [15].
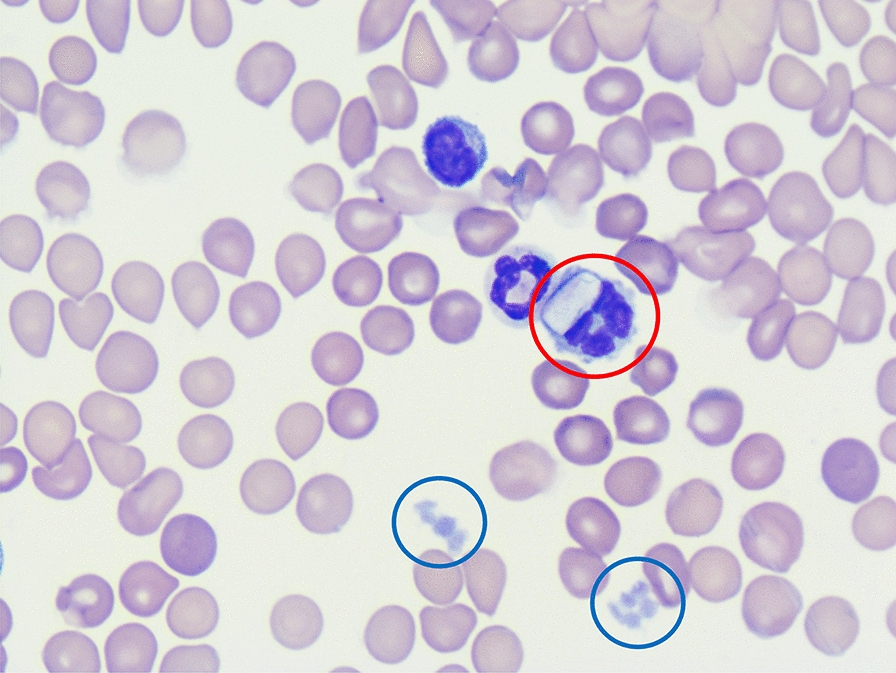
The life-cycle for all Hepatozoon spp. includes gamogony and sporogony in haematophagous invertebrate definitive hosts and merogony and gametogony in vertebrate hosts [1]. After ingestion of a tick harbouring oocytes that contain sporozoites, the infective sporozoites are released in the gastrointestinal tract of the vertebrate host and reach blood and lymph circulation by penetrating the gut wall. Merogony starts in lymphoid tissues such as the bone marrow and from 13 days post-infection onwards, merozoites penetrate neutrophilic granulocytes and monocytes to develop into gamonts [16]. During the tick’s blood meal on an infected host, the gamonts are ingested and gametogenesis takes place in the gut of the tick, followed by sporogony in the haemocoel [1]. Besides vectorial transmission, additional transmission pathways of Hepatozoon spp. have been described and include predation of infected animals, although this has not been described for H. canis [1, 17]. Intrauterine transmission of H. canis was previously demonstrated in a study from Japan, in which H. canis gamonts were observed in peripheral blood smears in 23 out of 29 puppies (79%) from a total of six deliveries at 16 to 60 days after birth [18].
Dogs infected with H. canis usually do not show any clinical signs. Dogs may show clinical signs if a high level of parasitaemia is reached or if co-infections with other vector-borne infectious agents occur [19]. Clinical manifestation may be severe, e.g. lethargy, fever, anorexia, weight loss, lymphadenomegaly and anaemia (16, 17). In one study, 28 dogs younger than 18 months naturally infected with H. canis confirmed by PCR testing and cytology did not show any clinical signs [19], but haematological abnormalities were present in 26 out of the 28 dogs (93%); mainly eosinophilia (77%), leucocytosis (46%), lymphocytosis (31%), neutrophilia (23%), monocytosis (19%), thrombocytopenia (19%) and anaemia (4%). However, 13 out of these 26 dogs (50%) with haematological abnormalities were co-infected with other vector-borne pathogens [19].
The diagnosis of hepatozoonosis is most frequently based on PCR results [20, 21], as PCRs have higher sensitivity and specificity compared to other diagnostic tools such as microscopic evaluation [22]. Gamonts often are incidental findings when analysing blood smears. Additionally, histopathology may reveal meronts and/or monozoic cysts in different tissues [23]. Serological tests, such as the immunofluorescence antibody test (IFAT), detect antibodies against H. canis with high sensitivity mainly in dogs with chronic infections [24, 25], but are not used routinely.
To the best of the authors’ knowledge, vertical transmission of H. canis has not been reported from dogs in Europe until now. We therefore performed a follow-up on the history of a female pregnant bitch imported from Italy to Germany which previously tested positive for H. canis.
A 4-year-old, female mixed breed dog was presented to a veterinary practice in Ganderkesee, Germany, with lethargy and tachypnoea in the absence of fever (Fig. 1). The dog was pregnant and was imported from Sardinia (Italy) 2 months prior to the visit. All serological and PCR tests were performed at Laboklin (Bad Kissingen, Germany). The dog tested positive for Rickettsia spp. by IFAT (titre 1:512; RICKETTSIA CONORII IFA SLIDE, Viracell, Granada, Spain) and for H. canis by PCR (cycle threshold [Ct] 30.3; TaqMan® real-time PCR, in-house test, amplifying a ~ 664-base pair (bp) fragment of the 18S ribosomal [rRNA] gene). Negative test results were found for Babesia canis (Babesia ELISA Dog, Afosa, Blankenfelde-Mahlow, Germany), Ehrlichia canis (Ehrlichia ELISA Dog, Afosa, Blankenfelde-Mahlow, Germany), Leishmania infantum (Civtest® Canis Leishmania, ELISA, Hipra, Amer, Spain), Anaplasma platys (TaqMan® real-time PCR, in-house test), Dirofilaria spp. (TaqMan® real-time PCR, in-house test for detection of microfilariae) and antigen testing for Dirofilaria immitis (FASTest® HW Antigen, MegaCor GmbH, Hörbranz, Austria).
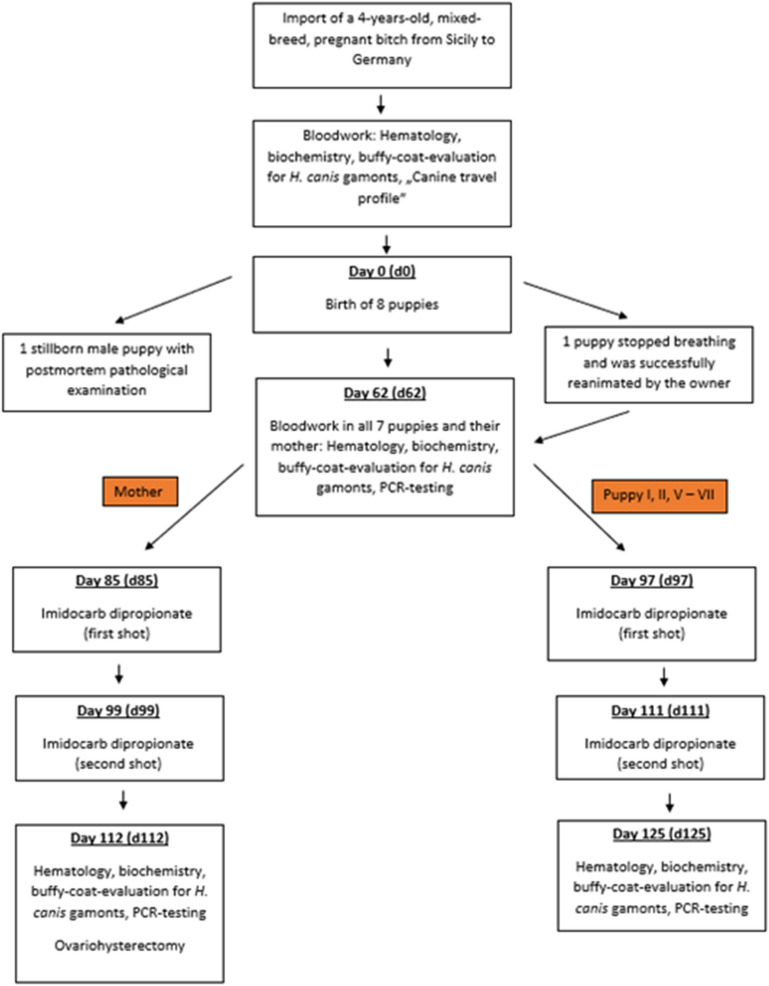
Fig. 1.
Study design and timeline of a mother dog imported from Sardinia (Italy) to Germany and giving birth to eight puppies, all infected with Hepatozoon canis
The first haematological examination (day 0; Vet abc Plus+, scil VET) of the mother was performed at the veterinary practice (Table 1) and showed mild anaemia and leucocytosis. All further analyses, including haematology (ADVIA 2120i, Siemens Healthineers) and a biochemistry profile (cobas 2 c 701, Roche Deutschland Holding GmbH) with kidney parameters, liver enzymes and electrolytes, as well as a buffy-coat analysis with quantification of H. canis-gamonts were carried out at Laboklin (Table 1). The Rickettsia conorii IFAT of the mother was repeated at day 62 and was still positive with a titre of 1:256. The dog also tested positive for H. canis by PCR on day 62 (Ct 30.8) and day 112 (Ct 31.8). On day 62, the anaemia had gone, but a mild leucocytosis with mild neutrophilia, lymphocytosis and eosinophilia was present (Table 1). Gamonts were detected in neutrophilic granulocytes on day 0 (4%), day 62 (2%) and day 112 (8%), indicating a moderate H. canis concentration in the peripheral blood (Table 1). On day 112, mild lymphocytosis and mild eosinophilia were seen. Biochemistry results were unremarkable apart from a mild initial decrease in iron on day 0 and day 112 as well as a mild hyperkalaemia on day 112 (Additional file 1). The dog was treated twice with imidocarb dipropionate (Carbesia® ad us. Vet., 0.5 ml/10 kg of body weight subcutaneously) on day 85 and day 99. On day 112, the H. canis PCR was still positive (Ct 31.8).
Table 1.
Complete blood count results of a female dog infected with Hepatozoon canis at the time of first presentation (day 0), 62 days post-partum and 112 days post-partum
| Parameter | Reference intervalsa | Day 0 | Reference intervalsb | Day 61 post-partum | Day 112 post-partum |
|---|---|---|---|---|---|
| RBC | 5.5–8.5 × 1012/l | 5.9 | 5.5–8.5 × 1012/l | 7.24 | 7.06 |
| HGB | 150–200 g/l | 133 | 150–190 g/l | 162 | 164 |
| HCT | 0.44–0.57 l/l | 0.36 | 0.44–0.52 l/l | 0.45 | 0.49 |
| MCV | 60.0–77.0 fl | 61.0 | 60.0–77.0 fl | 63.0 | – |
| MCH | 17.0–26.0 pg | 22.6 | 17.0–26.0 pg | 22.0 | – |
| MCHC | 31.0–38.0 g/dl | 37.0 | 31.0–38.0 g/dl | 36.0 | – |
| RET | – | – | < 110.0/nl | 58.6 | 205.4 |
| CHr | – | – | > 20.1 pg | 23.5 | 27.2 |
| WBC | 6.0–12.0 × 109/l | 13.3 | 6.0–12.0 × 109/l | 14.4 | 10.7 |
| Segc | – | – | 3.0–9.0 × 109/l | 9.5 | 5.4 |
| Lymphc | – | – | 1.0–3.6 × 109/l | 3.7 | 3.9 |
| Monoc | – | – | 0.04–0.5 × 109/l | 0.4 | 0.5 |
| Eoc | – | – | 0.04–0.6 × 109/l | 0.7 | 1.0 |
| Basoc | – | – | < 0.04 × 109/l | 0.0 | 0.0 |
| Bandsc | – | – | < 0.5 × 109/l | 0.0 | 0.0 |
| PLT | 200–460 × 109/l | 437 | 150–500 × 109/l | 201 | 157 |
| Hypochrc | – | – | Neg | Neg | Neg |
| Anisoc | – | – | Neg | Neg | Neg |
| Hepatozoon gamontsd | 0% | 4% | 0% | 2% | 8% |
| Hepatozoon spp. PCR | Negative | Positive (ct 30.3) | – |
Positive (ct 30.8) |
Positive (ct 31.8) |
Bold values demonstrate parameters out of the diagnostic thresholds
RBC red blood cells; HGB haemoglobin; HCT haematocrit; RET reticulocytes; CHr reticulocyte haemoglobin content; WBC white blood cells; Seg segmented neutrophilic granulocytes; Lymph lymphocytes; Mono monocytes; Eo eosinophilic granulocytes; Baso basophilic granulocytes; Bands banded neutrophilic granulocytes; PLT platelets; Hypochrom hypochromasia; Aniso anisocytosis
aIn-house laboratory of the veterinarian (Vet abc Plus+, scil VET, Germany)
bLaboklin GmbH & Co. KG. (ADVIA 2120i, Siemens Healthineers, Germany)
cManual differential count (Laboklin GmbH & Co. KG.)
dManual count out of buffy-coat smear (Laboklin GmbH & Co. KG.)
The mother gave birth to eight puppies on day 15 after her first presentation in the veterinary clinic. One of the puppies was stillborn (Fig. 1). A post-mortem examination of the stillborn puppy including histopathology showed that the animal was in a state of advanced autolysis and putrefaction, but the umbilical cord was normal, and no gross malformations were observed. The lungs were not ventilated, and the placenta was not available. As far as recognizable by routine histopathology, the lungs and kidneys showed immature morphology. There was no indication of inflammation in any of the examined organs (lungs, heart, liver, spleen, kidneys, brain). Due to the poor state of preservation, no pathogen-specific abnormalities were recognizable. DNA isolated from the umbilical cord (Ct 31.3), spleen (Ct 35.7) and amniotic fluid (Ct 32.3) were positive for H. canis by PCR, whereas the PCRs on the bone marrow and liver were negative.
Six out of the seven surviving puppies were alive at birth, but one dog stopped breathing immediately after birth and had to be reanimated by the owner. This animal (puppy VII) later became ill with fever (40.0–41.0 °C rectal temperature), inappetence and lethargy from day 95 onwards. The puppy presented in a lateral position and was unable to stand or walk on day 97 and received intensive care treatment with application of imidocarb dipropionate (Carbesia® ad us. vet., 0.5 ml/10 kg of body weight subcutaneously). The treatment was successful, and the clinical signs disappeared within 3 days after the first injection. All other four puppies of which the owner still took care were also treated with imidocarb dipropionate out of precaution, twice with a 12–14 day interval (Fig. 1) and have not developed clinical signs since. One puppy was adopted by new owners and therefore lost for further analysis.
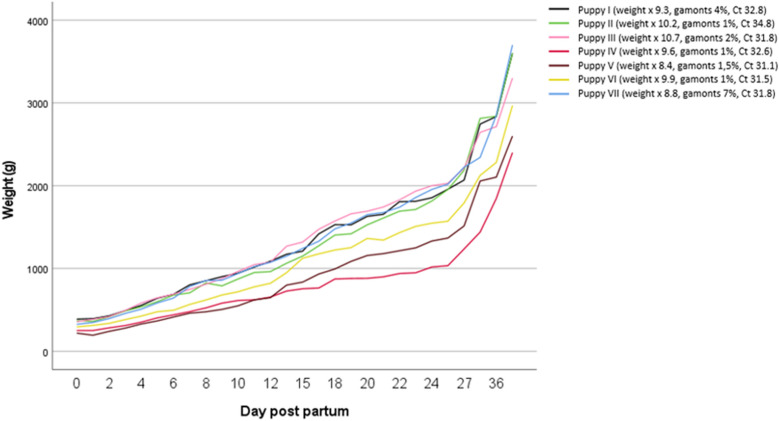
In all seven puppies that were alive at the time of writing, haematology was unremarkable, aside from a mild monocytosis in one puppy (Additional file 1). Gamonts of H. canis were detected in neutrophilic granulocytes of all puppies, with a range from 1 to 7% (median 1.5%), indicating a moderate concentration of H. canis in the peripheral blood. The puppy that had to be reanimated had the highest concentration of gamonts with 7% at day 62 and one of the lowest Ct in PCR testing (31.8; median 31.8, range 31.1–34.8). Biochemistry results revealed mild hyperproteinaemia, a mild increase in albumin and mild hyponatraemia in all puppies. In three out of seven puppies, a mild elevation of urea was seen as well as mild azotaemia in one puppy (Additional file 1: Table S3). At day 125, biochemistry results were available from five out of seven puppies. All five puppies showed a mild increase in creatine kinase and four out of five mild hyperkalaemia. In one puppy, mild elevation in C-reactive protein was recognized as well as decreased urea in another puppy (Additional file 1). The owner monitored the weight of all seven puppies from the day of birth to day 36 (Fig. 2), with the lowest weight gain percentage in dogs with the highest Ct values (puppy V: Ct 31.1, weight gain 8.4%; puppy VI: Ct 31.5, weight gain 9.9%; puppy VII: Ct 31.8, weight gain 8.8%; puppy III: Ct 31.8, weight gain: 10.2%; puppy IV: Ct 32.6, weight gain: 9.6%; puppy I: Ct 32.8, weight gain 9.3%; puppy II: Ct 34.8, weight gain 10.2%).
Fig. 2.
Overview of weight gain in the seven puppies tested positive for Hepatozoon canis by PCR from day 0 to day 36 post-partum with amounts of gamonts in buffy coat smears and cycle threshold (Ct) in polymerase chain reaction-testing on day 61 post-partum
A ~ 664 base pair fragment of the 18S rRNA gene from H. canis was amplified by PCR from samples collected from the bitch, all puppies, and the umbilical cord and amniotic fluid of the stillborn puppy [26]. The PCR products were subsequently sequenced (LGC Genomics, Berlin) and found to be identical to each other. A BLAST analysis of the sequence (GenBank Accession Number ON740944) showed 100% identity to previous H. canis entries from Europe, the Americas, and Asia, such as KX712129, MN393911 and MT107098.
To the best of the authors’ knowledge, this is the first study demonstrating the vertical transmission of H. canis in a dog in Europe. The diagnosis was made by PCR and detection of gamonts in peripheral blood smears. As the mother dog was imported only shortly before initial screening took place and R. sanguineus s.l. ticks are not considered to be endemic in Germany, an infection with H. canis of the mother in the country of origin, in this case Sardinia, seems most likely. Due to the absence of the vector and the early detection of the pathogen by PCR after 8 weeks of age (Fig. 1), the infection of the puppies born in Germany most likely occurred vertically. This is supported by the fact that the pathogen was also detected by PCR in the umbilical cord and the spleen of the stillborn puppy, where vector contact would not have been possible. However, an experimental study previously demonstrated that gamonts could be detected in canine blood as early as 28 days post-infection [16]. As the seven surviving puppies in our study were tested for Hepatozoon spp. at an age of 62 days for the first time, it cannot be fully excluded that they were infected with H. canis after birth. This does seem unlikely, as all puppies were predominantly kept indoors and tick attachment was not observed by the owner.
Screening for co-infections is highly recommended in dogs infected with H. canis as clinical signs are mainly observed in animals with co-infections. In our study, we performed a so-called canine travel profile in the bitch. Positive titres in IFAT for Rickettsia spp. of 1:512 initially and 1:256 on day 61 were found. As there was no fourfold change in this titre during this period, the results were interpreted as being caused by a past pathogen contact, but a chronic or persistent infection could not be ruled out completely.
Although H. canis infections are usually subclinical, some case reports suggest that H. canis infections may cause systemic disease in canine puppies, with lethargy, fever, anorexia, weight loss and gastrointestinal signs being reported as the most prominent clinical signs [1, 27, 28]. In our study, immunosuppression due to pregnancy might have been responsible for the reported lethargy and tachypnoea in the mother dog.
The presence and severity of clinical signs is known to correlate with the degree of parasitaemia [22, 29, 30]. The puppy with the highest concentration of H. canis gamonts (7%) had to be reanimated, and another puppy with an unknown concentration of gamonts in the peripheral blood was stillborn. Additionally, there might be a correlation between percentage of weight gain and Ct values of the H. canis PCR with lowered percentages in dogs with higher concentrations of the pathogen (Fig. 2). However, Ct values are not necessarily proportionate to the level of parasitaemia. A quantitative PCR could not be performed, but quantification of H. canis gamonts in the buffy coat. To the best of the authors’ knowledge, it is so far unknown, if the parasitaemia level in puppies may be linked to stillbirth. Further experimental studies may be of interest to clarify this hypothesis.
Mild normochromic anaemia is thought to be the most common clinical abnormality in dogs with H. canis infections [1, 31, 32], which was present in the mother dog on day 0 (Table 1). The mild hyperkalaemia on day 112 is most likely linked to mild haemolysis. Lymphocytosis, monocytosis and eosinophilia were recognized in most of the dogs in our study (Tables 1, 2). These haematological findings are in accordance with another study evaluating haematology results in dogs younger than 18 months being infected with H. canis [19]. In this study, haematological abnormalities were present in 26 out of 28 dogs (93%), mainly eosinophilia (77%), leucocytosis (46%), lymphocytosis (31%), neutrophilia (23%), monocytosis (19%), thrombocytopenia (19%) and anaemia (4%) [19]. Because 13 out of the 26 dogs (50%) with available information regarding clinical signs and haematological results tested positive for other vector-borne pathogens, only a limited comparison of the mentioned study and our findings is possible. Higher leucocytic count was linked to a higher level of parasitaemia [1], but this was not seen in our study.
Table 2.
Complete blood count results of 7 puppies infected with Hepatozoon canis at day 62 post-partum performed with ADVIA 2120i [Siemens Healthineers] in the Laboklin laboratory (Bad Kissingen, Germany) with age-related reference intervals according to Rortveit et al. (2015)
| Parameter | Reference interval | Puppy I | Puppy II | Puppy III | Puppy IV | Puppy V | Puppy VI | Puppy VII |
|---|---|---|---|---|---|---|---|---|
| RBC | 4.0–5.5 × 1012/l | 4.55 | 4.71 | 4.58 | 4.54 | 4.39 | 4.47 | 5.0 |
| HGB | 86–177 g/l | 98 | 109 | 105 | 103 | 100 | 106 | 111 |
| HCT | 0.27–0.37 l/l | 0.32 | 0.36 | 0.34 | 0.32 | 0.31 | 0.32 | 0.36 |
| MCV | 63.0–74.0 fl | 70.0 | 77.1 | 74.0 | 70.0 | 72.0 | 71.0 | 71.6 |
| MCH | Pga | 22.0 | 23.1 | 23.0 | 23.0 | 23.0 | 24.0 | 22.2 |
| MCHC | 29.0–34.0 g/dl | 31.0 | 30.0 | 31.0 | 33.0 | 32.0 | 33.0 | 31.0 |
| RET | /nla | 177.5 | 203.5 | 188.2 | 205.2 | 180.9 | 138.6 | 187.0 |
| CHr | pga | 23.0 | 24.4 | 23.6 | 23.5 | 22.8 | 26.3 | 24.0 |
| WBC | 8.8–22.4 × 109/l | 13.6 | 20.5 | 17.3 | 15.6 | 18.9 | 17.3 | 17.5 |
| Segb | 4.1–12.2 × 109/l | 6.8 | 9.8 | 6.7 | 7.2 | 7.9 | 8.1 | 11.9 |
| Lymphb | 2.7–11.3 × 109/l | 4.8 | 8.6 | 8.0 | 7.0 | 9.1 | 6.9 | 3.9 |
| Monob | 0.5–1.6 × 109/l | 1.4 | 1.0 | 1.7 | 0.9 | 1.5 | 0.9 | 0.9 |
| Eob | 0.1–1.8 × 109/l | 0.7 | 1.0 | 0.7 | 0.5 | 0.4 | 1.4 | 0.9 |
| Basob | × 109/l | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Bandsb | < 0.5 × 109/l | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| PLT | 193–653 × 109/l | 241 | 399 | 367 | 429 | 280 | 393 | 307 |
| Hypochrb | Neg | Neg | Neg | Neg | Neg | Neg | Neg | Neg |
| Anisob | Neg | Neg | Neg | Neg | Pos | Neg | Neg | Neg |
| Hepatozoon gamontsc (day 62) (%) | 0 | 4 | 1 | 2 | 1 | 1.5 | 1 | 7 |
| Hepatozoon gamontsc (day 125) | 0% | 1% | 1% | – | – | 0% | 1% | 0% |
| Hepatozoon spp. PCR (day 62) | Negative | Positive (ct 32.8) | Positive (ct 34.8) | Positive (ct 31.8) | Positive (ct 32.6) | Positive (ct 31.1) | Positive (ct 31.5) | Positive (ct 31.8) |
| Hepatozoon spp. PCR (day 125) | Negative | Positive (ct 34.3) | Negative | – | – | Positive (ct 36.1) | Positive (ct 33.1) | Positive (ct 33.0) |
Bold values demonstrate parameters out of the diagnostic thresholds
RBC red blood cells; HGB haemoglobin; HCT haematocrit; RET reticulocytes; CHr reticulocyte haemoglobin content; WBC white blood cells; Seg segmented neutrophilic granulocytes; Lymph lymphocytes; Mono monocytes; Eo eosinophilic granulocytes; Baso basophilic granulocytes; Bands banded neutrophilic granulocytes; PLT platelets; Hypochrom hypochromasia; Aniso anisocytosis
aNo reference values provided by Rortveit et al. (2015)
bManual differential count (LABOKLIN GmbH & Co. KG.)
cManual count out of buffy-coat smear (LABOKLIN GmbH & Co. KG.)
The mild elevation of creatine kinase observed in the five puppies with complete follow-up on day 125 must be interpreted with caution. To the best of the authors’ knowledge, there are no published age-related reference intervals fitting with the age of the puppies. Therefore, an interpretation as age-related changes must be taken into consideration. Additionally, the formation of cysts in the muscular tissue of the puppies due to the H. canis infection [33] with subsequent elevation of enzyme activity in the blood can be discussed although no lameness or muscular pain was reported. Interestingly, elevated C-reactive protein was reported on day 125 2 weeks after the second shot of imidocarb dipropionate in the puppy with severe clinical signs, though not in any of the other puppies.
The therapeutic approach for canine H. canis infections is challenging, as no drug is officially labelled for treatment of this infection for dogs in Europe. Therefore, treatment options were discussed with the owner and the local veterinary authorities were asked for permission to apply imidocarb dipropionate. Previous reports indicated that treatment with imidocarb dipropionate did not sterilize H. canis infections at the standard recommended dose [34]. This was also demonstrated in our study, in which positive PCR results were still observed in the mother and four of the five treated puppies. However, in most of the dogs in our study, the Ct values of PCR tests revealed a lower parasitaemia after treatment. Clinical signs improved quickly in the diseased puppy and the mother was without clinical signs after treatment too. This is concordant with literature as the prognosis of dogs infected with H. canis is reportedly good in cases of low parasitaemia, although the decrease in the parasitaemia may be slow and may require several repeated treatments with imidocarb dipropionate [1].
Besides vector-based transmission, vertical transmission of H. canis from mother dogs to their puppies may present an important route of transmission. Dog breeders and veterinarians should be aware of this potential risk. As dogs usually do not show clinical signs or clinicopathological abnormalities upon H. canis infections, routine screening of dogs imported from endemic countries is important to identify infected animals. It is recommended to perform PCR-testing of both peripheral whole blood and buffy coat to increase the sensitivity. A possible link between stillbirth and H. canis infections has to be investigated further, as well as the routes of transmission from bitches to puppies. Our data suggest an impact of the umbilical cord (transmission via blood) while the impact of the amniotic fluid is in doubt. Additionally, further studies are required for evaluation of alternative treatment options in dogs infected with H. canis.
Supplementary Information
Additional file 1: Table S1: Biochemistry results of a female dog infected with Hepatozoon canis at the time of first presentation (day 0), 62 days post-partum and 112 days post-partum performed with cobas 2 c 701 (Roche Deutschland Holding GmbH) in the laboratory Laboklin (Bad Kissingen, Germany). Table S2: Complete blood count results for seven puppies infected with Hepatozoon canis at day 125 post-partum performed with ADVIA 2120i [Siemens Healthineers] in the laboratory Laboklin (Bad Kissingen, Germany). Table S3: Biochemistry results of 7 puppies infected with Hepatozoon canis at day 62 post-partum performed with cobas 2 c 701 (Roche Deutschland Holding GmbH) in the laboratory Laboklin (Bad Kissingen, Germany) with age-related reference intervals according to Rortveit et al. (2015). Table S4: Biochemistry results of seven puppies infected with Hepatozoon canis at day 125 post-partum performed with cobas 2 c 701 (Roche Deutschland Holding GmbH) in the laboratory Laboklin (Bad Kissingen, Germany).
Acknowledgements
Not applicable.
Abbreviations
- Ab-ELISA
Antibody enzyme-linked immunosorbent assay
- Ct
Cycle threshold in polymerase chain reaction-testing
- DNA
Deoxyribonucleic acid
- EDTA
Ethylenediaminetetraacetic acid
- IFAT
Immunofluorescence antibody test
- PCR
Polymerase chain reaction
Author contributions
The dogs included in the study were presented to SC. IS initiated the study, evaluated the data and wrote the manuscript. AMN, EM, SC, HAL, GL and TN supervised the study and edited the manuscript. All authors read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The owners of the mentioned dogs and the puppies agreed to publication of this study, figures and tables. Aside from testing indicated by the treating veterinarian, only surplus samples were used for further diagnostics.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ingo Schäfer, Email: i.schaefer@laboklin.com.
Elisabeth Müller, Email: mueller@laboklin.com.
Ard M. Nijhof, Email: ard.nijhof@fu-berlin.de
Heike Aupperle-Lellbach, Email: aupperle@laboklin.com.
Gerhard Loesenbeck, Email: loesenbeck@laboklin.com.
Sybille Cramer, Email: Sybille.cramer@icloud.com.
Torsten J. Naucke, Email: naucke@laboklin.com
References
- 1.Baneth G. Perspectives on canine and feline hepatozoonosis. Vet Parasitol. 2011;181:3–11. doi: 10.1016/j.vetpar.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 2.Smith TG. The genus Hepatozoon (Apicomplexa: Adeleina) J Parasitol. 1996;82:565–585. doi: 10.2307/3283781. [DOI] [PubMed] [Google Scholar]
- 3.Menn B, Lorentz S, Naucke TJ. Imported and travelling dogs as carriers of canine vector-borne pathogens in Germany. Parasit Vectors. 2010;3:34. doi: 10.1186/1756-3305-3-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Röhrig E, Hamel D, Pfister K. Retrospective evaluation of laboratory data on canine vector-borne infections from the years 2004–2008. Berl Munch Tierarztl Wochenschr. 2011;124:411–418. [PubMed] [Google Scholar]
- 5.Hamel D, Röhrig E, Pfister K. Canine vector-borne disease in travelled dogs in Germany–a retrospective evaluation of laboratory data from the years 2004–2008. Vet Parasitol. 2011;181:31–36. doi: 10.1016/j.vetpar.2011.04.020. [DOI] [PubMed] [Google Scholar]
- 6.Schäfer I, Volkmann M, Beelitz P, Merle R, Müller E, Kohn B. Retrospective evaluation of vector-borne infections in dogs imported from the Mediterranean region and southeastern Europe (2007–2015) Parasit Vectors. 2019;12:30. doi: 10.1186/s13071-018-3284-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schafer I, Volkmann M, Beelitz P, Merle R, Muller E, Kohn B. Retrospective analysis of vector-borne infections in dogs after travelling to endemic areas (2007–2018) Vet Parasitol. 2019;276:100015. doi: 10.1016/j.vpoa.2019.100015. [DOI] [PubMed] [Google Scholar]
- 8.Baneth G, Bourdeau P, Bourdoiseau G, Bowman D, Breitschwerdt E, Capelli G, et al. Vector-borne diseases–constant challenge for practicing veterinarians: recommendations from the CVBD World Forum. Parasit Vectors. 2012;5:55. doi: 10.1186/1756-3305-5-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Helm CS, Samson-Himmelstjerna GV, Liesner JM, Kohn B, Muller E, Schaper R, et al. Identical 18S rRNA haplotypes of Hepatozoon canis in dogs and foxes in Brandenburg, Germany. Ticks Tick Borne Dis. 2020;11:101520. doi: 10.1016/j.ttbdis.2020.101520. [DOI] [PubMed] [Google Scholar]
- 10.Murata T, Inoue M, Taura Y, Nakama S, Abe H, Fujisaki K. Detection of Hepatozoon canis oocyst from ticks collected from the infected dogs. J Vet Med Sci. 1995;57:111–112. doi: 10.1292/jvms.57.111. [DOI] [PubMed] [Google Scholar]
- 11.de Miranda RL, de Castro JR, Olegario MM, Beletti ME, Mundim AV, O'Dwyer LH, et al. Oocysts of Hepatozoon canis in Rhipicephalus (Boophilus) microplus collected from a naturally infected dog. Vet Parasitol. 2011;177:392–396. doi: 10.1016/j.vetpar.2011.01.044. [DOI] [PubMed] [Google Scholar]
- 12.Rubini AS, Paduan KS, Martins TF, Labruna MB, O'Dwyer LH. Acquisition and transmission of Hepatozoon canis (Apicomplexa: Hepatozoidae) by the tick Amblyomma ovale (Acari: Ixodidae) Vet Parasitol. 2009;164:324–327. doi: 10.1016/j.vetpar.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 13.Gabrielli S, Kumlien S, Calderini P, Brozzi A, Iori A, Cancrini G. The first report of Hepatozoon canis identified in Vulpes vulpes and ticks from Italy. Vector Borne Zoonotic Dis. 2010;10:855–859. doi: 10.1089/vbz.2009.0182. [DOI] [PubMed] [Google Scholar]
- 14.Giannelli A, Ramos RA, Dantas-Torres F, Mencke N, Baneth G, Otranto D. Experimental evidence against transmission of Hepatozoon canis by Ixodes ricinus. Ticks Tick Borne Dis. 2013;4:391–394. doi: 10.1016/j.ttbdis.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Giannelli A, Ramos RA, Di Paola G, Mencke N, Dantas-Torres F, Baneth G, et al. Transstadial transmission of Hepatozoon canis from larvae to nymphs of Rhipicephalus sanguineus. Vet Parasitol. 2013;196:1–5. doi: 10.1016/j.vetpar.2013.02.017. [DOI] [PubMed] [Google Scholar]
- 16.Baneth G, Samish M, Shkap V. Life cycle of Hepatozoon canis (Apicomplexa: Adeleorina: Hepatozoidae) in the tick Rhipicephalus sanguineus and domestic dog (Canis familiaris) J Parasitol. 2007;93:283–299. doi: 10.1645/GE-494R.1. [DOI] [PubMed] [Google Scholar]
- 17.Johnson EM, Panciera RJ, Allen KE, Sheets ME, Beal JD, Ewing SA, et al. Alternate pathway of infection with Hepatozoon americanum and the epidemiologic importance of predation. J Vet Intern Med. 2009;23:1315–1318. doi: 10.1111/j.1939-1676.2009.0375.x. [DOI] [PubMed] [Google Scholar]
- 18.Murata T, Inoue M, Tateyama S, Taura Y, Nakama S. Vertical transmission of Hepatozoon canis in dogs. J Vet Med Sci. 1993;55:867–868. doi: 10.1292/jvms.55.867. [DOI] [PubMed] [Google Scholar]
- 19.Otranto D, Dantas-Torres F, Weigl S, Latrofa MS, Stanneck D, Decaprariis D, et al. Diagnosis of Hepatozoon canis in young dogs by cytology and PCR. Parasit Vectors. 2011;4:55. doi: 10.1186/1756-3305-4-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baneth G, Barta JR, Shkap V, Martin DS, Macintire DK, Vincent-Johnson N. Genetic and antigenic evidence supports the separation of Hepatozoon canis and Hepatozoon americanum at the species level. J Clin Microbiol. 2000;38:1298–1301. doi: 10.1128/JCM.38.3.1298-1301.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Y, Wang C, Allen KE, Little SE, Ahluwalia SK, Gao D, et al. Diagnosis of canine Hepatozoon spp. infection by quantitative PCR. Vet Parasitol. 2008;157:50–58. doi: 10.1016/j.vetpar.2008.06.027. [DOI] [PubMed] [Google Scholar]
- 22.Karagenc TI, Pasa S, Kirli G, Hosgor M, Bilgic HB, Ozon YH, et al. A parasitological, molecular and serological survey of Hepatozoon canis infection in dogs around the Aegean coast of Turkey. Vet Parasitol. 2006;135:113–119. doi: 10.1016/j.vetpar.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 23.Baneth G, Shkap V. Monozoic cysts of Hepatozoon canis. J Parasitol. 2003;89:379–381. doi: 10.1645/0022-3395(2003)089[0379:MCOHC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Baneth G, Shkap V, Samish M, Pipano E, Savitsky I. Antibody response to Hepatozoon canis in experimentally infected dogs. Vet Parasitol. 1998;74:299–305. doi: 10.1016/S0304-4017(97)00160-X. [DOI] [PubMed] [Google Scholar]
- 25.Shkap V, Baneth G, Pipano E. Circulating antibodies to Hepatozoon canis demonstrated by immunofluorescence. J Vet Diagn Invest. 1994;6:121–123. doi: 10.1177/104063879400600127. [DOI] [PubMed] [Google Scholar]
- 26.Schäfer I, Kohn B, Nijhof AM, Müller E. Molecular detection of Hepatozoon species infections in domestic cats living in Germany. J Feline Med Surg. 2021 doi: 10.1177/1098612X211055680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Bonis A, Colombo M, Terragni R, Bacci B, Morelli S, Grillini M, et al. Potential role of Hepatozoon canis in a fatal systemic disease in a puppy. Pathogens. 2021;10:1193. doi: 10.3390/pathogens10091193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baker JL, Craig TM, Barton CL, Scott DW. Hepatozoon canis in a dog with oral pyogranulomas and neurologic disease. Cornell Vet. 1988;78:179–183. [PubMed] [Google Scholar]
- 29.Skeldon N, Klaassen J, Hinds M. Diagnosis of Hepatozoon canis. Vet Rec. 2017;180:124. doi: 10.1136/vr.j549. [DOI] [PubMed] [Google Scholar]
- 30.Gavazza A, Bizzeti M, Papini R. Observations on dogs found naturally infected with Hepatozoon canis in Italy. Rev Méd Vét. 2003;154:565–571. [Google Scholar]
- 31.Kwon SJ, Kim YH, Oh HH, Choi US. First case of canine infection with Hepatozoon canis (Apicomplexa: Haemogregarinidae) in the Republic of Korea. Korean J Parasitol. 2017;55:561–564. doi: 10.3347/kjp.2017.55.5.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Voyvoda H, Pasa S, Uner A. Clinical Hepatozoon canis infection in a dog in Turkey. J Small Anim Pract. 2004;45:613–617. doi: 10.1111/j.1748-5827.2004.tb00184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baneth G. Hepatozoon canis infection. In: Greene CE, editor. Infectious Diseases of the Dog and the Cat. 4. Oxford: Elsevier; 2012. [Google Scholar]
- 34.Sasanelli M, Paradies P, Greco B, Eyal O, Zaza V, Baneth G. Failure of imidocarb dipropionate to eliminate Hepatozoon canis in naturally infected dogs based on parasitological and molecular evaluation methods. Vet Parasitol. 2010;171:194–199. doi: 10.1016/j.vetpar.2010.03.042. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1: Biochemistry results of a female dog infected with Hepatozoon canis at the time of first presentation (day 0), 62 days post-partum and 112 days post-partum performed with cobas 2 c 701 (Roche Deutschland Holding GmbH) in the laboratory Laboklin (Bad Kissingen, Germany). Table S2: Complete blood count results for seven puppies infected with Hepatozoon canis at day 125 post-partum performed with ADVIA 2120i [Siemens Healthineers] in the laboratory Laboklin (Bad Kissingen, Germany). Table S3: Biochemistry results of 7 puppies infected with Hepatozoon canis at day 62 post-partum performed with cobas 2 c 701 (Roche Deutschland Holding GmbH) in the laboratory Laboklin (Bad Kissingen, Germany) with age-related reference intervals according to Rortveit et al. (2015). Table S4: Biochemistry results of seven puppies infected with Hepatozoon canis at day 125 post-partum performed with cobas 2 c 701 (Roche Deutschland Holding GmbH) in the laboratory Laboklin (Bad Kissingen, Germany).
Data Availability Statement
All data generated or analysed during this study are included in this published article.