Abstract
Background:
Stress is a commonly perceived cause of cancer, but the evidence to date is limited and inconclusive. We examined work-related stress in relation to cancer incidence in a population-based cohort, with outcome data from Swedish national registries.
Methods:
The study population included 113,057 participants in the Västerbotten Intervention Programme. HRs were estimated using Cox proportional hazards regression, for cancer overall and for types with ≥500 cases, and adjusting for several potential confounders. The primary exposure was prediagnostic work-related stress, using the well established Karasek job demand/control model. Demand and control variables were dichotomized at the median, and participants were classified according to combinations of these categories. We also considered social network and aspects of quality of life.
Results:
“High-strain” work (high demand/low control) was not associated with cancer risk compared with “low-strain” work (low demand/high control): multivariable HR 1.01 [95% confidence interval (CI), 0.94–1.08] for men and 0.99 (95% CI, 0.92–1.07) for women. Results were also null for most cancer types assessed: prostate, breast, colorectal, lung, and gastrointestinal (GI). The risk of GI cancer was lower for “passive” (low demand/low control) versus “low-strain” work, particularly for colorectal cancer in women: multivariable HR 0.71 (95% CI, 0.55–0.91), but statistical significance was lost after adjustment for multiple testing.
Conclusions:
The findings of this population-based, cohort study do not support a role for work-related stress in determining cancer risk.
Impact:
This study helps fill an important knowledge gap given the common concern about stress as a risk factor for cancer.
Introduction
Work-related stress, and especially job strain, is an established risk factor for cardiovascular disease (1), but is the same true for cancer? Notably, stress is one of the most commonly perceived causes of cancer not only in the general population (2), but also specifically among cancer survivors (3). A link between chronic work stress and cancer is also biologically plausible. Cardiovascular disease and cancer share many etiologic mechanisms and risk factors, some of which are also involved in the physiologic response to stress. Prolonged work stress leads to an allostatic load with dysregulation of nervous, endocrine, and immune systems (4), all of which predispose for atherosclerosis. Similarly, stress-related physiologic alterations such as activation of the sympathetic nervous system, dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, inflammation, and cellular immune suppression have all been implicated in carcinogenesis (5, 6).
However, despite potential pathogenic mechanisms for stress in cancer development, epidemiologic findings to date have been mixed. Meta-analyses of work stress and cancer risk have reported null results for cohort studies (7) and, more recently, an association between higher perceived work stress and increased risk of cancer (8). Although the latter result was driven largely by case–control studies based on retrospectively collected data, one large cohort study did report an increased risk of cancer in participants with higher perceived stress levels, particularly in men (9). A large register-based study including 284,257 Swedish men found an association between low adolescent stress resilience and an increased risk of liver and lung cancer, but also a decreased risk of prostate and melanoma skin cancer (10). Null results have been observed for sources of acute stress, such as posttraumatic stress disorder (11), in relation with cancer risk. Given the discrepancy between public perceptions of stress as a cause of cancer and the limited and inconsistent evidence to date, there is clearly a need for a stronger evidence base to help inform the public health message.
Sweden is a welfare state with a generally high standard of living. However, there has been a considerable increase in stress-related diseases and psychiatric problems in Sweden since the 1970s, which has been most striking health and social care, education, and the trade and service sector (12). Thus the Swedish population, being relatively homogeneous in many aspects but with a wide range of work stress, represents a relevant setting to investigate the relationship between work stress and cancer.
We investigated job strain, assessed by the well established Karasek demand-control model, in relation to future cancer risk using a large, population-based cohort (n = approximately 110,000), with extensive prospectively collected data, long follow-up, and a large number of cancer cases (n = approximately 11,000). We also considered estimates of social support and aspects of quality of life, which may modify effects of stress on health outcomes (13).
Materials and Methods
Study population
The study had a cohort design, including male and female participants in the population-based Västerbotten Intervention Programme (VIP; refs. 14, 15). The VIP is a publically funded, ongoing cardiometabolic risk screening program established in 1985. Residents of Västerbotten County are invited to the VIP the year they turn 40, 50, and 60 years of age (and 30 years during a period in the 1990s), and approximately a third of all participants have participated two or more times. Participation rates have generally been above 60% of the target population (15). At the health examination, anthropometric and blood pressure measurements are taken by a healthcare professional, oral glucose tolerance and blood cholesterol tests are done, and an extensive lifestyle questionnaire is filled out. Participants meet with a specially trained nurse to discuss the results of the health exam, including personalized advice for lifestyle modification, and when necessary, referrals are sent for additional work-up or therapy. At the health exam, blood samples are also collected and biobanked for research. All participants provided a signed informed consent at recruitment.
At the cut-off date for inclusion in this study (November 18, 2016), the VIP included 123,602 participants. Participants diagnosed with cancer other than nonmelanoma skin cancer before recruitment to the cohort were excluded at baseline (n = 3,984). Observations with missing data on height or weight (n = 1,441) or with extreme anthropometric values (height < 130 or > 210 cm, weight < 35 kg, waist circumference < 60 cm, or BMI < 15 or > 70 kg/m2) were excluded (n = 100). After exclusions, 113,057 participants remained. The study protocol was approved by the Regional ethics review board in Umeå, Sweden, and the study was conducted in accordance with the Declaration of Helsinki.
Follow up
Participants were followed up from initial recruitment to the VIP project until November 1, 2017, by linkage to Swedish national registries (with essentially complete inclusion) for whatever occurred first of malignancy other than nonmelanoma skin cancer (northern Swedish branch of the Swedish Cancer Registry), death (Swedish Cause of Death Registry), or emigration (Swedish Registry of Total Population and Population Changes). We investigated associations with all cancer, as well as specific cancer sites with at least 500 incident cases in the cohort: prostate (C61), breast (C50), colorectal (C18-C20.9), and lung cancer (C34). For comparison with previous research, we also assessed gastrointestinal (GI) cancer, including esophagus (C15), gastric (C16), liver/intrahepatic bile ducts (C22), pancreas (C25), small intestine (C17), and colorectal cancer (C18–20.9).
Variables
The primary exposure was work-related stress risk, using indicators according to the well established and commonly used Karasek job demand/control model (16). Work demands and decision latitude (control) were measured using a validated 11-item questionaire (17), included in the VIP cohort questionnaire completed at baseline. Briefly, participants were asked to rate demand and control aspects at their current job on a four-point likert scale. In accordance with standard methodology for the Karasek model, each participant was categorized as “low” or “high” in demand and control defined as below or above to the study median of the two scales. The combination of these two variables were then used to categorize participants as having: ‘Low strain jobs’ (low demand/high control), ‘Passive jobs' (low demand/low control), ‘Active jobs' (high demand/high control), or ‘High strain jobs' (high demand/low control).
We also investigated indicators of social network and aspects of quality of life, which might modify relationships between work stress and health. To estimate the extent of social networks, we used the validated Interview schedule for social interaction (ISSI) indicators: the Availability of social interaction index (AVSI; score 0–14, in which higher scores indicate greater availability) and the Availability of attachment index (AVAT; score 0–12, in which higher scores indicate greater availability), based on 13 questionnaire items (18, 19). The two ISSI variables were each categorized into four groups (AVSI 0–3, 4–7, 8–10, 11–14, and AVAT 0–3, 4–6, 7–9, 10–12) to ensure an adequate number of incident cancer cases in each category. To estimate quality of life, we used the validated SF36 questionnaire (substituted from 2014 with RAND 36), including seven items related to satisfaction in various aspects of life (family, housing, work, finances, leisure time) and perceived appreciation outside and within the home. The variable scores range from 1 = very poor to 7 = excellent satisfaction. Quality-of-life variables were available from 1996 and onward, so these analyses were conducted on a subsample of the cohort (approximately 60% of the total cohort). In addition, questions from the Gothenburgh Quality of Life inventory were used (all D-questions in the questionnaire).
Other background variables and potential confounders considered in the analyses were baseline age and sex, as well as questionnaire-based variables: educational status (elementary school, junior secondary school, upper secondary school, and postsecondary education), smoking status (non-, former-, current smoker), long-term sick leave (yes or no, self-reported sick leave longer than 6 months, for any reason), body mass index (BMI) measured by a health professional (BMI, kg/m2), recreational physical activity (on a scale of 1–5, from never to >3 times/week), and alcohol intake (categorized as nonconsumers and questionnaire-version–specific quartiles among consumers).
Statistical analysis
Baseline measurements and Cox proportional hazards regression were used to estimate HRs. Age was used as the time scale, and baseline age was the start of the time at risk for each participant. Primary analyses included work-related stress, social support, and quality of life variables in relation with the risk of cancer overall and of major cancer types (≥500 incident cases), in men and women, separately. In order to limit the number of statistical tests and the risk of chance findings, secondary analyses were planned only in the form of exploratory subgroup analyses of any associations revealed in the primary analyses. For each exposure variable, the category corresponding to the hypothetical low-risk situation was chosen as the reference category. Potential confounders to be included in the multivariable models were chosen a priori based on previous knowledge, focusing on available variables demonstrating broad associations across the most common types of cancer. The proportional hazards assumption was checked using statistical tests based on Schoenfeld residuals. There were no violations. To avoid spurious estimates, exposures were required to have more than 20 incident cancers in each category. For variables with categories containing less than 20 events, categories with the lowest numbers of cases were merged with adjacent categories until the requirement was met. For the HRs presented for each exposure variable, participants with missing values for that particular exposure were omitted from the model. Missing values for potential confounders included as covariates in the models were imputed with the mode among participants with observed values.
All tests were two-sided when applicable. Pvalues below an adjusted significance threshold of 0.001 were considered significant (Bonferroni correction approximated from 0.05/36 tests for 3 categories of exposures, 6 cancer sites, in men and women). All computations were conducted in R v.3.4.2 (R Foundation for Statistical Computing).
Results
Baseline characteristics
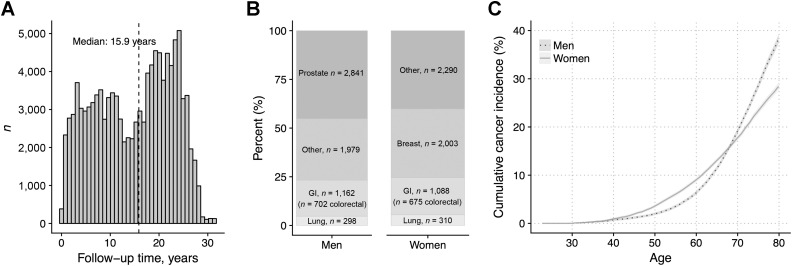
A total of 56,146 men and 56,911 women, both with a mean age at baseline of 46 (interquartile range: 40–50 years), were included. A total of 20% of men and 22% of women were current smokers, and the median BMI was 26 for men and 24 for women. During the follow-up of up to 31 years (median 16 years; Fig. 1A), 11,971 cohort participants were diagnosed with cancer (6,280 men, 5,691 women; Fig. 1B). The cumulative incidence of cancer at age 80 years was estimated to be 38% for men, and 28% for women (Fig. 1C).
Figure 1.
Västerbotten Intervention Programme (VIP) follow-up characteristics. A, Follow-up time distribution. B, Incident cancer cases distribution. C, Cumulative incidence of cancer estimated in the cohort by sex.
Baseline characteristics by Karasek's job-demand/control model categories are presented in Table 1. The low-strain and active categories, and the passive and high-strain categories, had similar baseline characteristics. The low-strain and active groups were characterized by a higher proportion of men and university-educated participants, and a lower proportion of current smokers, compared with the passive and high-strain groups. On average, they also had a lower proportion of reported sick leave, a slightly lower BMI, higher physical activity status, higher alcohol intake, as well as higher availability of social interaction and lower availability of attatchment scores, compared to the passive and high-strain groups. Women were overrepresented in the passive and high-strain categories, and underrepresented in the low-strain and active categories.
Table 1.
Baseline characteristics by work-related stress categories.
| Karasek job/demand control categoryb | |||||
|---|---|---|---|---|---|
| Variablea | Low strain (%), n = 35,056 | Passive (%), n = 18,505 | Active (%), n = 15,278 | High strain (%), n = 33,277 | Missing (%) |
| Demand/control | low/high | low/low | high/high | high/low | 10,941 (10) |
| Women, n (%) | 15,015 (43) | 10,215 (55) | 7,009 (46) | 18,631 (56) | 0 (0) |
| Age, years | 45.8 (8.8) | 47.4 (9.6) | 45.0 (8.5) | 45.2 (9.0) | 0 (0) |
| Postsecondary education, n (%) | 15,372 (44) | 2,979 (16) | 6,240 (41) | 5,621 (17) | 1,877 (2) |
| Current smokers, n (%) | 6,157 (18) | 4,036 (22) | 2,943 (19) | 7,614 (23) | 235 (<1) |
| Any sick leave >6 months, n (%) | 4,077 (13) | 3,617 (23) | 1,855 (14) | 5,211 (18) | 15,689 (14) |
| BMI, kg/m2 | 25.7 (4.0) | 26.0 (4.4) | 25.8 (4.1) | 26.0 (4.4) | 0 (0) |
| Recreational physical activity, scale 1–5c | 2.4 (1.3) | 2.2 (1.3) | 2.3 (1.3) | 2.2 (1.3) | 2,735 (2) |
| Alcohol intake, g/day | 4.9 (5.3) | 3.4 (4.3) | 4.8 (5.6) | 3.5 (4.9) | 9,796 (9) |
| ISSIc | |||||
| AVSI, score 0–14 | 8.5 (1.5) | 8.1 (1.7) | 8.4 (1.6) | 8.0 (1.7) | 8,507 (8) |
| AVAT, score 0–12 | 2.8 (1.7) | 3.0 (2.0) | 2.8 (1.8) | 3.1 (2.1) | 8,717 (8) |
| Quality of lifec, score 1–7 | |||||
| Satisfaction: family | 6.2 (1.1) | 6.1 (1.2) | 6.0 (1.3) | 5.9 (1.3) | 47,006 (42) |
| Satisfaction: housing | 6.3 (1.0) | 6.2 (1.1) | 6.2 (1.1) | 6.0 (1.2) | 46,893 (41) |
| Satisfaction: work | 5.6 (1.4) | 5.2 (1.7) | 4.9 (1.5) | 4.7 (1.6) | 48,263 (43) |
| Satisfaction: finances | 5.7 (1.3) | 5.3 (1.5) | 5.3 (1.4) | 5.1 (1.5) | 47,019 (42) |
| Satisfaction: leisure time | 5.7 (1.3) | 5.7 (1.4) | 5.3 (1.5) | 5.3 (1.5) | 47,083 (42) |
| Feel appreciated outside home | 6.0 (1.0) | 5.5 (1.2) | 5.7 (1.1) | 5.3 (1.3) | 47,035 (42) |
| Feel appreciated inside home | 6.3 (1.0) | 6.1 (1.1) | 6.1 (1.1) | 5.9 (1.2) | 47:619 (42) |
a N (%) or mean (SD).
b χ 2 or ANOVA tests of difference in distribution of all variables in the table by work-related stress categories were performed, with all P < 0.001.
cRanging from never to ≥3 times per week.
dQuestionnaire items, higher score indicates a higher availability, satisfaction, or degree of appreciation. Collected for the subset of participants sampled from 1996 and onward.
Among the participants, 43,070 had repeated sampling occasions at 10-year intervals, of which 37,099 had a valid measurement of Karasek job demand/control model at both visits. Among these participants, 18,685 (50.4%) reported the same category at both visits, indicating a moderate intraindividual agreement of the instrument over time (Cohen kappa, 0.35).
Work-related stress and cancer risk
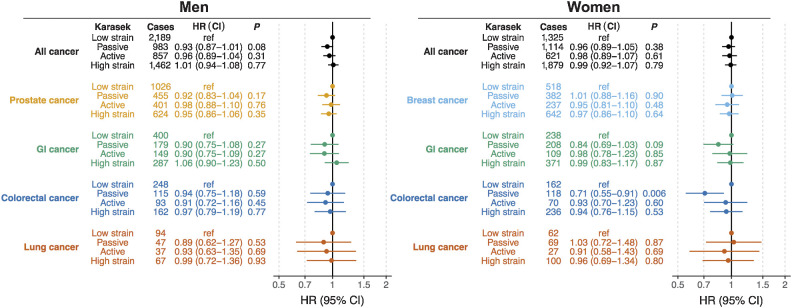
High strain work according to Karasek job demand/control model, was not associated with the overall risk of cancer in men or women (high strain vs. low strain HR 1.01; 95% CI, 0.94–1.08 and HR 0.99; 95% CI, 0.92–1.07, respectively; Fig. 2). The results were also null for major cancer sites in men and women (cases in men/women: prostate, n = 2,841/0; breast, n = 0/2,003; colorectal, n = 702/675; lung, n = 298/310; and GI, n = 1,162/1,088), with the exception of a slightly lower risk of GI cancer, in particular colorectal cancer, in women in the “passive” work category compared with the “low-strain” group (HR 0.71; 95% CI, 0.55–0.91). However, the association was not significant when adjusted for multiple testing (P = 0.006, above the threshold of 0.001). Given the overall null results, no secondary subgroup analyses were conducted.
Figure 2.
HRs for cancer risk by work-related stress categories (Karasek) in men and women. Estimates from Cox proportional hazard models using age as time scale, adjusted for educational status, smoking status, BMI, recreational physical activity, and alcohol intake.
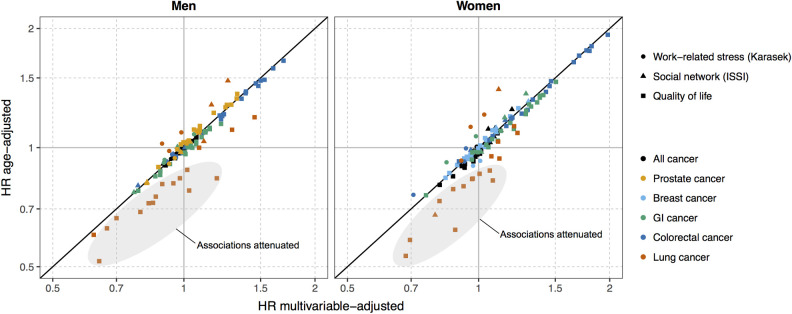
Associations between possible modifiers of psychosocial stress and cancer risk, available for the subset of participants (approximately 60%) recruited from 1996 and onward, are presented in Supplementary Table S1. There were no associations with a P value below the adjusted threshold of 0.001 for any major cancer in men or women for availability of social interaction, availability of attachment, or estimates of quality of life. For colorectal cancer, and GI cancer in women, HRs tended to be above 1, whereas for all cancer and other common types of cancer results HRs were more evenly distributed. Adjusting for potential confounders generally had little effect on the HR estimates, except for lung cancer, for which multivariable adjustment attenuated the associations, in particular for quality of life variables (Fig. 3).
Figure 3.
Comparison of age-adjusted and multivariable adjusted HR for cancer risk by work-related stress (Karasek), social network, and quality of life indicators. Estimates from Cox proportional hazard models using age as time scale. Multivariable adjusted estimates were adjusted for educational status, smoking status, BMI, recreational physical activity, and alcohol intake. HRs are interpreted as the relative hazard of cancer at higher scores (indicating a higher risk of work-related stress, larger social network, and better quality of life), compared with lower scores. HRs differing from 1 with an unadjusted P < 0.05 are labelled.
Discussion
In this population-based cohort study, including more than 110,000 participants and 11,000 incident cancer cases, work-related stress according to Karasek job/demand control model was not associated with the overall risk of cancer. Results were also null for breast cancer, GI cancer, colorectal cancer, prostate cancer, and lung cancer in men and women.
These findings confirm and expand upon the results of a smaller meta-analysis of work stress and cancer risk, using individual-level data from 12 cohort studies but with a total of 116,000 participants and 5,700 cancer incident cases (7). That meta-analysis focused on studies with prospectively collected data on high-strain low-control exposures. In contrast, a meta-analysis published by Yang and colleagues in 2019 (8) reported an association between higher work-stress exposure and increased cancer risk, but the result was driven largely by case–control studies with retrospectively collected exposure data.
Work-related stress and general stress are correlated (20), and research on other types of psychosocial stress may, therefore, also have relevance here. Higher perceived general stress levels were reported to associate with a small increased risk of cancer, particularly liver cancer, in a Japanese population (9). Notably, general stress was assessed using a single-item questionnaire measure which may be more vulnerable to measurement error and misclassification than the validated multi-item job-strain index used in our study and in the previous meta-analysis (7). Similar to the Japanese study, a higher future risk of cancer, specifically liver and lung cancer, was observed in Swedish adolescents with lower stress resilience (10). The authors suggested that low stress resilience could lead to unfavorable adult lifestyle decisions, which, rather than stress itself, might cause a higher risk of cancer. We were able to account for several potential confounders, such as smoking status, BMI, and alcohol intake. Furthermore, the similar null results in the age-adjusted and multivariable analyses suggest no mediation by lifestyle factors, with the possible exception of the quality of life factors in lung cancer. Although we cannot exclude residual confounding, any such factor not assessed or inadequately captured in the analyses would need to be directly associated with work-related stress and inversely related to cancer risk to mask a causal relationship between job stress and cancer. Furthermore, the relatively homogeneous nature of the Swedish population with respect to potentially important confounders such as socioeconomic conditions minimizes the risk of residual confounding. Work stress, on the other hand, displays a wider gradient in Sweden and thus should not have hindered detection of a risk relationship, but rather lends support to the observed null association between job strain and cancer risk. Studies of other sources of major stress in relation to cancer risk, such as stress induced by major life events or posttraumatic stress disorder (PTSD), have been inconclusive (11, 21, 22). Psychologic stress due to discrimination, related gender, ethnicity, or racism for example, could be closely intertwined with work-related stress. For example, workplace bullying has reported to be higher in immigrants in Sweden compared with native Swedes (23). To our knowledge, stress due to discrimination has not been studied in relation to cancer risk.
Given the many shared risk factors and etiologic mechanisms in cardiovascular diseases and cancer, it might seem surprising that work-related stress could have an established role in one but not the other. Indeed, mechanistic studies show a direct impact of increased neuroendocrine activity on increased neuroendocrine activity on stress on tumor growth, including increased angiogenesis and altered immunologic response. This has been suggested to occur through activation of ß2-adrenergic receptors leading to subsequent activation of the tumor cell cyclic (cAMP)–protein kinase signaling pathway as well as enhanced expression of VEGF and matrix metalloproteinases (MMP)–2 and −9 (24, 25). Furthermore, increased glucocorticoid receptor activation may lead to inhibition of tumor cell apoptosis (26), and concomitant activation of both the sympathetic nervous system and the HPA axis can regulate inflammatory responses by immune cells as shown in both human and animal studies (27). It is possible that a potential role of work-related stress in cancer development may be too weak to be detectable in this type of study. Analogously, the importance of modifiable risk factors such as lifestyle is generally greater for cardiovascular disease than cancer (28–30).
A main strength of our study is the population-based cohort design. The VIP cohort is based on cardiometabolic health screening, integrated within primary health care in the Swedish county of Västerbotten. The high participation rate (approximately 70%) and low selection bias in the VIP (15, 31) make our results more generalizable to the overall Swedish population compared with most previous studies, which were based on more selected cohort populations (7). Work-related stress was assessed using the validated, robust, and well established Karasek job strain/demand-control model. The Karasek demand-control model has been used extensively, mainly in the Scandinavian countries, for analyses of work stress in relation to health outcomes (Theorell, Jood, and colleagues 2016). In this present study, high-quality data were thus collected prospectively according to a standardized protocol, and cohort participants were followed for up to 30 years (median 15.9 years) for cancer endpoints. The prediagnostic exposure data and long followup avoided recall bias and reverse causation. Furthermore, use of the Swedish Cancer Registry to identify cancer cases ensures complete follow up. Finally, our analyses included twice the number of cancer cases as the one previous meta-analysis of work stress and cancer risk, combining, to the best of our knowledge, all previous cohort studies (7).
Limitations of the study are that even though Karasek's job demand/control model entails a validated questionnaire, it is based on self-reported, perceived work stress. Also, we were unable to take into consideration some potential sources of selection bias, such as possible lower recruitment of people on stress leave or with higher work stress at baseline. We did not address work history prior to baseline, to what degree participants worked at baseline, career stage or changes, or specific reasons for not working (e.g., unemployment, sick leave or full time homemaking, the latter being rare in Sweden even during the early recruitment years for this study; ref. 32). The 10% of participants with missing data for the work-stress variables provides some estimation of nonemployed, as it includes participants who probably did not work at baseline. Over the recruitment period for the study (1985–2016), the work force in Sweden included approximately 70% to 75% of the population 20 to 74 years of age, and unemployment rates have generally been 5% to 10% (33). We were unable to take into consideration work stress during the first decades of working life. The study also lacks information about the participants' ethnic and racial origin, as these variables are not recorded at baseline. Additional studies on other populations, ensuring inclusion of minority groups, would be needed to draw a more general conclusion. We lacked data on cancer-related factors such as reproductive factors, family history, and cancer screening history, but of the major cancer types addressed in the analyses, only breast cancer had a general population-based screening program during the recruitment period. Finally, our risk estimates were based on a single measurement of work-related stress and covariates, though analyses of the subsample of 37,099 participants with repeated measures 10 years apart suggested moderately stable work-related stress variables over time.
In this population-based cohort study of 113,057 men and women and 11,971 cancer cases, we found a null association between work-related stress and future risk of cancer. Our findings are an important contribution to a relatively underresearched topic of considerable public and patient interest, and suggest that work-related stress is unlikely to have any substantial causal effect in cancer development.
Authors' Disclosures
J. Hadrévi reports grants from The Swedish Research Council during the conduct of the study. R. Myte reports personal fees from AstraZeneca outside the submitted work. B. Van Guelpen reports grants from Cancer Research Foundation in Northern Sweden during the conduct of the study. No disclosures were reported by the other authors.
Disclaimer
The funders had no role in the study design, collection of data, writing, or decision to submit the paper for publication. The researchers are independent from the funders, and all authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Acknowledgments
We thank the Biobank Research Unit at Umeå University, Västerbotten Intervention Programme, and the County Council of Västerbotten for providing data and samples and we acknowledge the contribution from Biobank Sweden, supported by the Swedish Research Council (VR 2017-00650), as well as the scientists involved in the Northern Sweden Diet Database, for excellent assistance. The study was also supported by the Cancer Research Foundation in Northern Sweden.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
This article is featured in Highlights of This Issue, p. 1
Footnotes
Note: Supplementary data for this article are available at Cancer Epidemiology, Biomarkers & Prevention Online (http://cebp.aacrjournals.org/).
Authors' Contributions
J. Hadrévi: Validation, investigation, visualization, writing–original draft, project administration, writing–review and editing. R. Myte: Data curation, formal analysis, validation, investigation, visualization, methodology, writing–original draft, project administration. T. Olsson: Conceptualization, funding acquisition, validation, methodology, writing–original draft. R. Palmqvist: Conceptualization, validation, investigation, methodology, writing–original draft. L. Slunga Järvholm: Conceptualization, formal analysis, validation, investigation, writing–original draft. B. Van Guelpen: Conceptualization, resources, formal analysis, supervision, funding acquisition, validation, methodology, writing–original draft, project administration.
References
- 1. Kivimaki M, Kawachi I. Work stress as a risk factor for cardiovascular disease. Curr Cardiol Rep 2015;17:630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shahab L, McGowan JA, Waller J, Smith SG. Prevalence of beliefs about actual and mythical causes of cancer and their association with socio-demographic and health-related characteristics: findings from a cross-sectional survey in England. Eur J Cancer 2018;103:308–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thomson AK, Heyworth JS, Girschik J, Slevin T, Saunders C, Fritschi L. Beliefs and perceptions about the causes of breast cancer: a case-control study. BMC Res Notes 2014;7:558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McEwen BS. Stressed or stressed out: what is the difference? J Psychiatry Neurosci 2005;30:315–8. [PMC free article] [PubMed] [Google Scholar]
- 5. Andersen BL, Thornton LM, Shapiro CL, Farrar WB, Mundy BL, Yang HC, et al. Biobehavioral, immune, and health benefits following recurrence for psychological intervention participants. Clin Cancer Res 2010;16:3270–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Armaiz-Pena GN, Cole SW, Lutgendorf SK, Sood AK. Neuroendocrine influences on cancer progression. Brain Behav Immun 2013;30:S19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Heikkila K, Nyberg ST, Theorell T, Fransson EI, Alfredsson L, Bjorner JB, et al. Work stress and risk of cancer: meta-analysis of 5700 incident cancer events in 116,000 European men and women. BMJ 2013;346:f165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yang T, Qiao Y, Xiang S, Li W, Gan Y, Chen Y. Work stress and the risk of cancer: a meta-analysis of observational studies. Int J Cancer 2019;144:2390–400. [DOI] [PubMed] [Google Scholar]
- 9. Song H, Saito E, Sawada N, Abe SK, Hidaka A, Shimazu T, et al. Perceived stress level and risk of cancer incidence in a Japanese population: the Japan Public Health Center (JPHC)-based Prospective Study. Sci Rep 2017;7:12964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kennedy B, Fang F, Valdimarsdóttir U, Udumyan R, Montgomery S, Fall K. Stress resilience and cancer risk: a nationwide cohort study. J Epidemiol Community Health 2017;71:947–53. [DOI] [PubMed] [Google Scholar]
- 11. Gradus JL, Farkas DK, Svensson E, Ehrenstein V, Lash TL, Milstein A, et al. Posttraumatic stress disorder and cancer risk: a nationwide cohort study. Eur J Epidemiol 2015;30:563–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Le Grand C, Szulkin R, Tåhlin M. The governments official investigations. SOU 2001;53:79–119. [Google Scholar]
- 13. Cohen S, McKay G. Social support, stress and the buffering hypothesis: a theoretical analysis. Handbook of psychology and health 1984;4:253–67. [Google Scholar]
- 14. Hallmans G, Ågren Å, Johansson G, Johansson A, Stegmayr B, Jansson JH, et al. Cardiovascular disease and diabetes in the Northern Sweden Health and Disease Study Cohort - evaluation of risk factors and their interactions. Scand J Public Health 2003;61:18–24. [DOI] [PubMed] [Google Scholar]
- 15. Norberg M, Wall S, Boman K, Weinehall L. The västerbotten intervention programme: background, design and implications. Global Health Action 2010;3:4643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q 1979;24:285–308. [Google Scholar]
- 17. Theorell T, Perski A, Akerstedt T, Sigala F, Ahlberg-Hultén G, Svensson J. Changes in job strain in relation to changes in physiological state. A longitudinal study. Scand J Work Environ Health 1988;14:189–96. [DOI] [PubMed] [Google Scholar]
- 18. Henderson S, Duncan-Jones P, Byrne DG, Scott R. Measuring social relationships. The interview schedule for social interaction. Psychol Med 1980;10:723–34. [DOI] [PubMed] [Google Scholar]
- 19. Unden AL, Orth-Gomer K. Development of a social support instrument for use in population surveys. Soc Sci Med 1989;29:1387–92. [DOI] [PubMed] [Google Scholar]
- 20. Klitzman S, House JS, Israel BA, Mero RP. Work stress, nonwork stress, and health. J Behav Med 1990;13:221–43. [DOI] [PubMed] [Google Scholar]
- 21. Kruk J. Self-reported psychological stress and the risk of breast cancer: a case-control study. Stress 2012;15:162–71. [DOI] [PubMed] [Google Scholar]
- 22. Kvikstad A, Vatten LJ, Tretli S, Kvinnsland S. Death of a husband or marital divorce related to risk of breast cancer in middle-aged women. A nested case-control study among Norwegian women born 1935–1954. Eur J Cancer 1994;30:473–7. [DOI] [PubMed] [Google Scholar]
- 23. Rosander M, Blomberg S. Workplace bullying of immigrants working in Sweden. Int J Hum Res Man 2021Mar 8 [Epub ahead of print]. [Google Scholar]
- 24. Cole SW, Sood AK. Molecular pathways: beta-adrenergic signaling in cancer. Clin Cancer Res 2012;18:1201–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Thaker PH, Lutgendorf SK, Sood AK. The neuroendocrine impact of chronic stress on cancer. Cell Cycle 2007;6:430–3. [DOI] [PubMed] [Google Scholar]
- 26. Volden PA, Conzen SD. The influence of glucocorticoid signaling on tumor progression. Brain Behav Immun 2013;30:S26–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Powell ND, Tarr AJ, Sheridan JF. Psychosocial stress and inflammation in cancer. Brain Behav Immun 2013;30:S41–7. [DOI] [PubMed] [Google Scholar]
- 28. WHO. Cardiovascular diseases; data and statistics. Copenhagen (Denmark): WHO Regional Office for Europe; 2021. Available from: https://www.euro.who.int/en/health-topics/noncommunicable-diseases/cardiovascular-diseases/data-and-statistics. [Google Scholar]
- 29. WHO. Cardiovascular diseases. Available from: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). 2021.
- 30. WHO. Cancer. Available from: https://www.who.int/health-topics/cancer#tab=tab_2. 2021.
- 31. Weinehall L, Hallgren CG, Westman G, Janlert U, Wall S. Reduction of selection bias in primary prevention of cardiovascular disease through involvement of primary health care. Scand J Prim Health Care 1998;16:171–6. [DOI] [PubMed] [Google Scholar]
- 32. Statistics Sweden 2018. Women and men in Sweden 2018; facts and figures. Örebro (Sweden): Population and Economic Welfare; 2018. [Google Scholar]
- 33. Statistics Sweden. Labour force surveys. Available from: https://www.scb.se/en/finding-statistics/statistics-by-subject-area/labour-market/labour-force-surveys/labour-force-surveys-lfs/.