Abstract
Objective:
This integrative review explores the barriers to and facilitators for human papillomavirus (HPV) vaccination among adult transgender and gender diverse (TGD) people in the United States.
Data Source:
A systematic search of electronic databases included PubMed/MEDLINE, CINAHL, and EMBASE from 1985 to 2020.
Inclusion and Exclusion Criteria:
Inclusion criteria included studies from the United States that described HPV vaccination barriers or facilitators and included adult TGD participants, both quantitative and qualitative studies. Exclusion criteria were studies that reported only HPV vaccine prevalence, non-English/non-U.S. studies, and studies limited to pediatric populations.
Data Extraction:
Two investigators used Covidence software to screen studies and manage data extraction. Quality of the quantitative studies was appraised using a checklist proposed by the Joanna Briggs Institute (JBI); qualitative studies were appraised using quality criteria informed by the literature.
Data Synthesis:
The Social Ecological Model guided the review to organize barriers to and facilitators for HPV vaccination at the patient-, provider-, and system-levels.
Results:
Database searches and hand-searching yielded 843 citations. After screening, eight articles were retained in the review. Seven were cross-sectional studies and one was a qualitative focus-group. All retained quantitative studies met six of the eight JBI quality checklist items.
Conclusion:
The low proportion of TGD participants in the retained studies highlights a gap in knowledge about HPV vaccination among this population. Future studies of HPV vaccination should recruit TGD people to better represent their perspectives.
Keywords: gender minorities, HPV, integrative review, papillomavirus, transgender, vaccination
Introduction
Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) in adults in the United States with a prevalence of 79 million existing infections and an incidence rate of 14 million new infections per year.1 High-risk strains of HPV (type 16 and 18) are associated with the majority of oropharyngeal, cervicovaginal, and anorectal cancers.1,2 A preventive vaccine was introduced in 2006, initially only recommended for individuals assigned female at birth, with a two-dose series from age 9 through 14 years, and a three-dose catch-up series from age 15 through 26 years. The recommendation was expanded to individuals assigned male at birth in 2009 and men who have sex with men (MSM) in 2011, but did not further specify any subgroups.3,4 Healthy People 2020 set a national target goal for 80% vaccination completion in adolescents and this was carried forward in Healthy People 2030.3,5 However, the Centers for Disease Control and Prevention (CDC) reported that as of 2019, vaccine completion was ∼54.2% among eligible adolescents in the general population.6 In June 2019, the CDC Advisory Committee on Immunization Practices (ACIP) expanded the recommended age range from 9 through 26 years to 9 through 45 years for everyone.7
Low rates of three-dose vaccine completion (range 13–32%) have been observed in adult sexual minority people defined by their sexual orientation (e.g., gay men, lesbian women, and bisexual men and women).8–10 Studies identified lack of knowledge or trust in vaccines, nondisclosure of sexual identity to providers, and fear of discrimination/stigma as barriers to vaccination among sexual minority people.9,11–14 Less is known about HPV vaccination among transgender and gender diverse (TGD) people who are estimated to number 1.4 million in the United States.15
In contrast to cisgender sexual minority people whose gender identity is consistent with their assigned sex at birth, TGD people have gender identities or gender expressions that may not conform to their assigned sex at birth and may identify as trans men/trans women, transgender men/transgender women, or simply men/women.16,17 Some TGD people identify as nonbinary or genderqueer, terms used to describe people whose gender is not exclusively male or female, including those who identify with a gender other than male or female, as more than one gender, or as no gender.18 It should be pointed out that TGD people may also be sexual minorities in terms of their sexual orientation. The intersection of sexual orientation and gender identity among TGD people is not consistently described in research literature.19
TGD people report a higher prevalence of poor health and experience stigma and discrimination with health care providers based on their gender identity, resulting in poor health outcomes from delaying or deferring necessary care such as vaccination.20–25 For example, TGD people who have a cervix and are sexually active are at risk of HPV, yet have been found to have reduced rates of cervical cancer screening and increased time between recommended screening intervals compared with cisgender women.26,27 Sexual and gender minority people, inclusive of TGD people, were designated a health disparities population for research by the National Institutes of Health in recognition of poor health outcomes among these communities.28
Problem identification
The true proportion of adult sexual minority and TGD people who have not received any doses of HPV vaccine is likely higher than the general population.8,9,29–32 Given the potential for decreased HPV vaccination among TGD people, this integrative review sought to describe barriers to and facilitators for HPV vaccination among adult gender minority people. We used the social ecological model to guide the review. This model has been adopted in numerous settings and is helpful for framing an investigation about vaccination because it considers how an individual's health behavior may be influenced by intrapersonal-, interpersonal-, institutional-, community-, and policy-level factors.33 We adapted this multilevel view of health behavior to three ecological levels: patient-level (intrapersonal); provider-level (interpersonal); and systems-level (institutional/community/policy). We used an integrative review framework proposed by Whittemore and Knafl34 to organize the review that includes the following components: problem identification, literature search strategy, data evaluation, data analysis, and synthesis of findings.
Methods
Data sources
The literature search strategy included a computer search, review of reference lists from retrieved articles, and hand-searching using Google Scholar to identify additional articles. The computer search included three databases: PubMed/MEDLINE, CINAHL, and EMBASE. Searches were performed from February to March 2021. Citations were organized and sorted using EndNote® version X8.2 software (Clarivate Analytics, Inc., Philadelphia, PA). Keywords were explored from the following categories: sexual minority and TGD communities, HPV vaccination, and keywords pertaining to vaccination barriers and facilitators.
We included both sexual minority and TGD keywords to decrease the possibility of omitting a study that included TGD people. Literature searches pertaining to sexual minority and TGD populations are challenging because several terms can be used to describe lesbian, gay, bisexual, and transgender people. Lee et al.35 investigated this issue in a systematic review and identified eight search terms for transgender individuals alone. The query including keywords and Boolean logic suggested by Lee et al.35 informed our search strategy. The final query was formatted for PubMed/MEDLINE using MeSH terms and simplified to comply with the controlled vocabularies for each database. A full description of keywords and query for each database is described in Appendix A1.
Inclusion/exclusion criteria
We included studies published from 1985 through 2020, studies that examined factors associated with HPV vaccination in adult TGD communities, both quantitative and qualitative study designs, abstracts, and full-text articles. Studies were included if the sample population included exclusively TGD people, or both sexual minority people and TGD people. We excluded studies that reported only HPV vaccine prevalence without the mention of barriers or facilitators. Non-English language studies and non-U.S.-based studies were excluded as we wished to focus on the experience of TGD people in the United States. We excluded studies that focused exclusively on adolescent/pediatric populations age <18 years because of the difference in health care decision-making agency involving a parent/guardian, compared with an independent adult. We also excluded systematic/clinical review articles with the aim of focusing on original versus secondary sources.
Data extraction
The initial database query results were entered into EndNote and deduplicated using the Bramer dedupe method.36 Two reviewers (A.P. and S.M.) then used Covidence software (Covidence Ltd., Melbourne, Australia) to identify any additional duplicates and proceed with the screening. Reviewers independently screened citations by title and abstract using the inclusion/exclusion criteria. The same criteria were reapplied to the full-text review. Disagreements were discussed and resolved at each phase of screening.
Methodological quality appraisal of studies
There exists no gold standard for quality appraisal in an integrative review and the process of evaluating quality is complex.34 The quantitative studies were evaluated with an eight-item quality checklist published by the Joanna Briggs Institute (JBI).37 Two reviewers, A.P. and S.M., performed quality appraisal for the quantitative studies independently and then met to discuss and resolve any differences. The single qualitative focus group study was evaluated by a single reviewer (A.P.) for qualitative rigor with narrative criteria proposed by Wu et al.38
Data synthesis and analysis
A.P. extracted key results from each study. The data extraction process approach included (1) data reduction, (2) data display, (3) data comparison, and (4) conclusion drawing and verification.34 The data analysis included all studies that met the inclusion criteria regardless of methodological rigor. This enabled the incorporation of as many perspectives as possible for barriers to and facilitators for HPV vaccination. Data analysis included the following steps suggested by Whittemore and Knafl34: first data were reduced according to subcategories and then extracted into a matrix to organize them into a manageable framework; the extracted data were converted into data display in the form of tables; the display data were compared to identify meaningful patterns; and findings synthesized into summary conclusions.
Results
Database search results
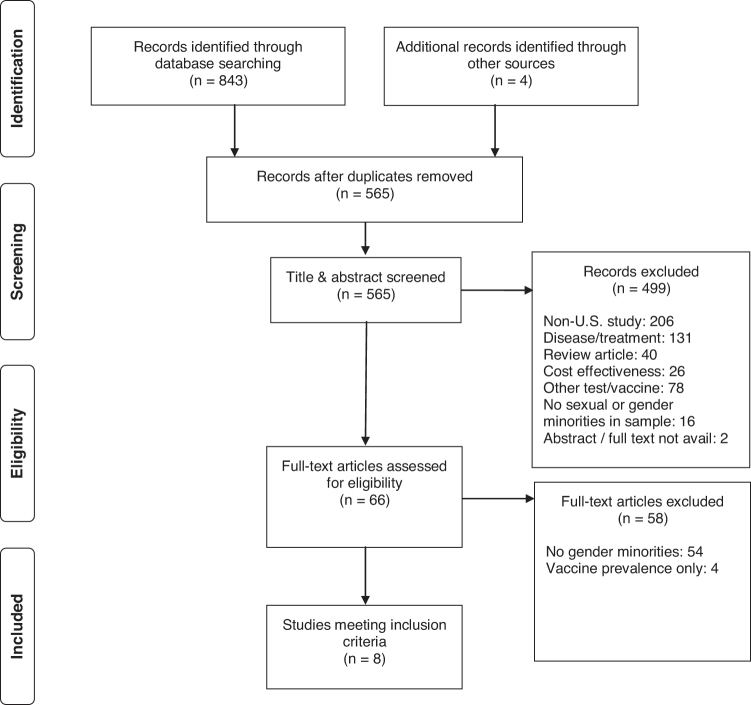
Searches of the 3 databases returned 843 citations and hand-searching for citations using reference lists and Google Scholar yielded 4 citations. After removing duplicates (n=282), the number of studies was reduced to 565. Articles were then screened by title and abstract and after the inclusion/exclusion criteria were applied, 499 articles were excluded for the following reasons: non-U.S. study (n=206), described HPV disease/treatment only (n=131), clinical or systematic review article (n=40), described vaccine cost-effectiveness only (n=26), described other testings and/or vaccines other than HPV (n=78), no sexual minority or TGD people included in the sample (n=16), and conference abstract with full-text unavailable for review (n=2). The remaining 66 studies were screened by full-text review involving line-by-line reading of each study. After inclusion/exclusion criteria were applied again, 58 studies were excluded for the following reasons: no gender minorities included in the study sample (n=54) and study described vaccine prevalence rates only (n=4). We retained eight studies for the integrative review. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines flow diagram documents the article search and selection process (Fig. 1).
FIG. 1.
PRISMA flow diagram for literature search. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Of the retained studies (Table 1), seven were of cross-sectional design,39–44 and one was a qualitative focus group design.45 Two of the cross-sectional studies used electronic health record data,39,41 three studies used in-person computer-assisted interview,42–44 and two studies used an internet-based online survey.40
Table 1.
Studies included in the integrative review with summary features
| Author (year) | Study design | Select sample characteristics | Barriers | Facilitators | Quality criteria |
|---|---|---|---|---|---|
| Apaydin et al. (2018)39 | Cross-sectional EHR data N=301 Clinic, Boston, MA |
Transgender men/women Genderqueer Cisgender male/female Lesbian, gay, bisexual, heterosexual Age (M=26.3, SD=2.48) |
Patient: documented substance use disorder, education attainment lower than some college/postsecondary school | Patient: education attainment college or higher, attended primary care visits, received vaccination for hepatitis A/B, received screening for STIs | 6/8 |
| Apaydin et al. (2018)45 | Qualitative descriptive Focus group N=15 Boston, MA |
Transgender men/women Cisgender male/female Lesbian, gay, bisexual, heterosexual, asexual, pansexual Age (M=25, SD=1) |
Patient: lack of awareness of HPV/vaccine, misconception that vaccine is gender-specific Provider: lack of awareness about HPV and relevance to sexual and gender minority people; lack of sexual and gender minority care competency System: 3-dose vaccine schedule |
Patient: proactive health-seeking behaviors, fear of genital warts, fear of health problems after HIV seroconversion, preexisting health conditions that promote engagement System: access to health care affirming to sexual identity |
No major concerns Not discussed: theoretical model, audit trails, member checks |
| Bednarczyk et al. (2017)40 | Cross-sectional Online survey N=660 Rural ZIP codes |
Transgender men/women Nonbinary Cisgender male/female Age (range 18–34) |
Patient: lack of provider recommendation Provider: bias against vaccinating male sex assigned at birth |
Patient: provider recommendation Provider: bias toward vaccinating female sex assigned at birth |
7/8 |
| Fontenot et al. (2016)41 | Cross-sectional EHR data N=2537 Clinic, Boston, MA |
Transgender men/women Cisgender male/female Lesbian, gay, bisexual, queer, heterosexual Age (M=21–22, SD=3) |
Patient: transgender identity | Patient: having private insurance, annual examination, received another non-HPV vaccine, received cervical Pap test, received STI test, engaged in oral sex | 6/8 |
| Gilbert et al. (2020)46 | Cross-sectional Tablet PC browser in-person initially, then internet-based |
Transgender/genderqueer Cisgender male Cisgender female Sexual orientation: heterosexual, gay, lesbian, bisexual/pansexual, queer/other Age (range 18–60+) |
Provider: Health care provider did not vaccinate after patient or provider brought up topic of vaccination; outright refusal of provider to vaccinate after patient brought it up to health care provider | None identified | 7/8 |
| Gorbach et al. (2017)42 | Cross-sectional In-person computer-assisted interview N=1033 Los Angeles, CA and Chicago, IL |
Transgender women Cisgender male Sexual orientation: gay, bisexual, queer Age (M=23, SD=2) |
Patient: not knowing where to get vaccinated, safety concerns Provider: lack of recommendation System: cost, insurance not covering vaccine |
Patient: appointment in past year, disclosed sexual orientation, screened for HIV/STIs, received other vaccines (hepatitis A/B) Provider: recommendation System: private clinic rather than LGBT or public clinic |
8/8 |
| Halkitis et al. (2019)43 | Cohort N=486 New York, NY |
Transgender men Cisgender male Age (M=23.7, SD=0.7) |
System: no significant difference in HPV vaccination by neighborhood poverty or HIV prevalence, age, education, sexual orientation, gender identity, or income | None identified | 8/8 |
| Singh et al. (2019)44 | Cross-sectional In-person computer-assisted interview N=1033 Los Angeles, CA Chicago, IL |
Gender: Transgender women Cisgender male Sexual orientation: Gay/homosexual Bisexual Heterosexual/straight Other/unknown Age (range 18–26) |
Patient: lack of knowledge of HPV risk, HPV vaccine, unsure whether could obtain HPV vaccine if wanted, lower education attainment | System: CDC ACIP HPV vaccine recommendations include transgender persons as of 2016 | 8/8 |
ACIP, Advisory Committee on Immunization Practices; CDC, Centers for Disease Control and Prevention; EHR, electronic health record; HPV, human papillomavirus; LGBT, lesbian, gay, bisexual, and transgender; SD, standard deviation; STI, sexually transmitted infection.
Inclusion of sexual minority people
None of the studies included gender minorities exclusively and five of the seven studies had samples with <10% TGD people.41–45 The three studies with the highest proportion of gender minorities by Apaydin et al.,39 Gilbert et al.,46 and Bednarczyk et al.40 were the most gender diverse, including participants who identified as gender nonbinary or genderqueer; gender identifications used by TGD people whose gender expression is not exclusively masculine or feminine.16 The cross-sectional study by Apaydin et al.39 included the greatest proportion of TGD participants; total (n=77, 26.9%), trans masculine/transgender man (n=41, 14.9%), trans feminine/transgender woman (n=33, 12%), and of these some also identified as genderqueer (n=17, 6.2%). Bednarczyk et al.40 had more TGD participants but they represented less than 20% of the total sample; total (n=106, 16.1%), transgender woman (n=23, 3.5%), transgender man (n=46, 7.0%), and nonbinary identified (n=37, 5.7%). Gilbert et al.46 aggregated transgender and genderqueer participants, and had the greatest number of TGD participants in any of the studies (n=137, 24.2%). Four studies had both transgender men and women, including the qualitative and cross-sectional studies by Apaydin et al.,39,45 and the studies by Bednarczyk et al.40 and Fontenot et al.41 The studies by Gorbach et al.42 and Singh et al.44 included only transgender women. The study by Halkitis et al.43 included transgender participants (n=33, 6.8%), but did not further specify their gender identity. Likewise, the study by Gilbert et al.46 did not further specify the gender identities of transgender or genderqueer participants although they collected these data. With the exceptions of Bednarczyk et al.,40 the qualitative study by Apaydin et al.,45 and the study by Singh et al.,44 the other studies did not distinguish between TGD and sexual minority participants in their results.
Quality appraisal
To add further rigor to the review, we performed a two-reviewer quality appraisal of the evidence using a standardized instrument.37 The quality of the cross-sectional studies was good with a mean score of 6.3 (maximum possible quality score is 8). All studies met at least six of the eight JBI quality criteria. The most common methodological deficit was lack of consideration for confounders. The quality appraisal for the cross-sectional studies is summarized in Table 2. One reviewer (A.P.) appraised the quality of the single qualitative focus group study by Apaydin et al.,45 using the narrative criteria for qualitative rigor proposed by Wu et al.,38 including credibility, dependability, confirmability, transferability, trustworthiness, and transparency. The study had no major quality concerns, but rigor would have been improved with additional description of the theoretical basis for the thematic content analysis. Trustworthiness and transparency would have been improved with more description of audit trails during and after the focus groups and whether-or-not member checks with participants were performed.
Table 2.
Methodological appraisal of cross-sectional studies
| Cross-sectional studies JBI quality criteria | Apaydin et al. (2018)39 | Bednarczyk et al. (2017)40 | Fontenot et al. (2016)41 | Gilbert et al. (2020)46 | Gorbach et al. (2017)42 | Halkitis et al. (2019)43 | Singh et al. (2019)44 |
|---|---|---|---|---|---|---|---|
| 1. Criteria for inclusion in the sample clearly defined? | Y | Y | Y | Y | Y | Y | Y |
| 2. Study subjects and the setting described in detail? | Y | Y | Y | Y | Y | Y | Y |
| 3. Exposure measured in a valid and reliable way? | Y | Y | Y | Y | Y | Y | Y |
| 4. Objective/standard criteria used for measurement? | Y | Y | Y | Y | Y | Y | Y |
| 5. Confounding factors identified? | N | Y | N | N | Y | Y | Y |
| 6. Strategies to deal with confounding factors stated? | N | N | N | N | Y | Y | Y |
| 7. Outcomes measured in a valid and reliable way? | Y | Y | Y | Y | Y | Y | Y |
| 8. Appropriate statistical analysis used? | Y | Y | Y | Y | Y | Y | Y |
| Score | 6 | 7 | 6 | 7 | 8 | 8 | 8 |
JBI, Joanna Briggs Institute; N, no; Y, yes.
Vaccination barriers
Patient level
The most frequently cited patient-level barrier to vaccination was lack of knowledge of HPV, HPV risk, and the HPV vaccine. Apaydin et al. explored this in a focus group of sexual minority and TGD people.45 Transgender women were unaware of the risks associated with HPV infection in the context of trans feminine bodies and some had the misconception that sexual activity before or after gender affirmation surgery affected relevance of the need for the HPV vaccine. Singh et al.44 also found that less than half (n=23, 46.9%) of the transgender women in their study were aware that there is a vaccine that can protect against certain types of HPV and only one in four (n=12, 24.5%) transgender women was aware that HPV can cause throat and oral cancer. Gorbach et al.42 found that lack of knowledge extended to not knowing where to get the vaccine and concerns over safety of vaccines, but these patient-level barriers were not specific to transgender participants. Apaydin et al.45 noted a unique personal-level barrier expressed by a transgender woman who had to weigh anxiety about being in public as a transgender person with the need for multiple visits for the shots. All sexual minority and TGD participants viewed long time intervals between doses, multiple doses, and inconvenience of work conflicting with appointment hours as additional barriers to vaccination.45 Fontenot et al.41 found that transgender men had 62% lower odds of HPV vaccination compared with cisgender females, however, specific barriers related to transgender men in the study were not identified. Additional patient-level barriers to vaccination included lower education attainment and the presence of substance use disorders in a mixed sexual minority and TGD participant sample.45
Provider level
Bednarczyk et al.,40 examined the association between provider recommendation and vaccination and found that providers recommended HPV vaccination less to individuals with male sex assigned at birth (n=53, 17%), regardless of their gender identity and these individuals received at least one dose of the vaccine (n=40, 13.7%), less frequently than individuals with female sex assigned at birth who were recommended to get the HPV vaccine more frequently (n=146, 47.2%), and subsequently initiated at least one dose more frequently (n=130, 43.9%). Gorbach et al.42 also noted that more than one-fourth (n=217, 26.9%) of their study participants cited lack of provider recommendation as a barrier to vaccination, however, the sample was predominantly cisgender male with only (n=39, 4.8%) identifying as transgender women. Apaydin et al.39 also found that sexual minority and TGD people cited negative interactions with primary care providers when discussing their care, especially sexual behavior, as a provider-level barrier to vaccination. Similarly, Gilbert et al.46 found in a survey of sexual and gender minority (SGM) adults in Iowa that of respondents eligible for HPV vaccine but reported no HPV vaccination (n=151), a minority of respondents (20.5%) reported they or their health care provider had brought vaccination up, but they had not received it. A small proportion (3.3%) had been outright refused vaccination by a health care provider when they brought it up. However, the study did not distinguish the experience of sexual minority from gender minority people in these responses.
System level
Singh et al.44 identified that a lag in HPV vaccination among cisgender women may be associated with the fact that their study was conducted within a few years of the CDC ACIP change in recommendation to include men, women, and transgender persons. Apaydin et al.39 cited a system-level bias in historical trends in HPV vaccine marketing that targets cisgender straight women, whereas transgender women expressed such marketing made them question whether they needed the vaccine or if it would be effective on them. Gorbach et al.42 noted the system-level barriers of cost of vaccine and whether insurance would cover the vaccine. Although Halkitis et al.43 explored system-level constructs such as residential neighborhood poverty and HIV prevalence, they did not find any association between these system-level factors as HPV vaccination in the cisgender sexual minority males as transgender individuals in their sample. Singh et al.44 highlighted that the latest CDC ACIP recommended groups for HPV vaccination do include transgender people and MSM, which would in theory be a policy system-level facilitator. However, the authors point out that the HPV vaccination recommendations have not led to significant vaccine uptake in MSM.
Vaccination facilitators
Patient level
Fear of disease, specifically genital warts and HIV coinfection, and health concerns related to being HIV positive, were a motivator for cisgender gay men to receive HPV vaccination in the qualitative study by Apaydin et al.45 In their related study, they also observed that participants had more than two and half times the odds (OR=2.59, 95% CI 95% 1.2–5.59) of having received HPV vaccination if they had received hepatitis A/B vaccination and had 1.2 times the odds (OR=1.22, 95% CI 1.03–1.43) of receiving HPV vaccination if they had received STI screening, however, transgender/gender diverse identity or experience was not significantly associated with the three-dose vaccine completion.
Provider level
The single most important provider-level facilitator for HPV vaccination was health care provider recommendation. Gorbach et al.42 found that in a predominantly cisgender male sample, individuals who received a provider recommendation for HPV vaccination had nearly 12 times increased odds (aOR=11.85, 95% CI 6.70–20.98) of vaccinating. Bednarczyk et al.40 also noted a potentially profound effect of provider recommendation on vaccination among TGD participants (n=106); nearly half of transgender men received an HPV vaccination recommendation (n=17, 47.2%) but less transgender men received at least one dose of HPV vaccine (n=14, 41.2%), a small proportion of transgender women received a vaccination recommendation (n=1, 6.7%) and at least one dose of HPV vaccine (n=1, 6.7%), less than half of nonbinary participants received a vaccination recommendation (n=6, 42.9%) but slightly more nonbinary participants received at least one dose of HPV vaccine (n=7, 50%). The authors did not specify how many individuals who did not receive a vaccination recommendation did receive a vaccine. Apaydin et al.45 found that transgender men expressed that the gender-affirming care they received resulted in comfort levels and trust in their primary care provider, which facilitated their receiving a full three-dose adult vaccine series.
System level
The most prominent system-level facilitator of vaccination was access to sexual minority and TGD-affirming care and engagement with primary care. Apaydin et al.39 found that the percentage of completed primary care appointments among sexual minority and TGD participants was associated with increased odds (OR=1.03, 95% CI 1.01–1.05, p=0.018) of three-dose HPV vaccination completion. This study also noted that for all sexual minority and TGD focus group participants regardless of HIV status, gender identity, and/or sexual orientation, having access to a gender affirming health care system was a major facilitator for vaccination.
Discussion
Synthesis of findings
This integrative review summarizes existing evidence that explores barriers to and facilitators for HPV vaccination among TGD people. We identified eight studies that included TGD people. However, studies rarely treated TGD participants separately from sexual minority participants when reporting results. This limited our ability to distinguish barriers and facilitators that could be considered specific to TGD people. Vaccination barriers and facilitators according to the levels of the social ecological model were also explored variably. The studies in our review focused primarily on patient-level and provider-level factors with less attention to system-level factors. The small number of studies that included TGD people and relatively small proportions of TGD participants recruited for each study suggests a gap in the literature regarding HPV vaccination among TGD people. This dearth of knowledge is concerning as evidence suggests that TGD people have increased risk for HPV infection and HPV-associated cancer than cisgender people.26,44,47,48
Many of the findings for vaccination barriers and facilitators in this review are not unique to TGD people. For example, facilitators such as vaccine knowledge and perceived threat of disease are all also known to be key facilitators for preventive vaccination in the general population.49 However, some facilitators and barriers may be more relevant and impactful in the context of U.S.-based TGD experience. We offer discussion of some of these results through this lens.
The patient-level finding that lack of HPV knowledge is a profound barrier to vaccination, especially for TGD people who are not aware of their risk for HPV disease and may have additional misconceptions about HPV vaccination appropriateness related to gender affirmation surgery. These findings support the notion that TGD people may have complex health information needs related to their gender identity.50,51 Moreover, anxiety expressed by a transgender participant regarding the need to attend multiple visits for HPV shots may suggest a proxy for anxiety related to engaging with the health care system. This would be consistent with studies that show that TGD people are more likely to delay care or not receive care due to fear of discrimination and stigma.21,24
The provider-level finding that provider recommendation is a key facilitator of vaccination is consistent with studies that examined provider recommendation in preventive vaccination in sexual minority communities that is likely also applicable to TGD communities. A study of MSM found that participants who had received a provider recommendation had over 42 times the odds (OR=42.23, 95% CI 14.90–19.68) of HPV vaccination initiation than those who did not receive a recommendation.11 The findings from our review reinforce the profound ability of providers to increase HPV vaccination. However, providers who are not culturally competent with respect to TGD people and their bodies may not recommend HPV vaccination appropriately. This may explain cases where patients did not receive vaccination despite bringing it up with their health care providers.46 Studies have shown that a significant barrier to vaccination is posed when health care providers lack competence in the care of sexual minority and TGD people.52,53
Of the system-level findings, access to care is a well understood facilitator of health care, and in the case of TGD communities, access to care from gender affirming providers is a potential facilitator for preventive care such as HPV vaccination.45 Research has shown that TGD people and cisgender sexual minority people who are less “out” to their medical providers and others in general (e.g., not disclosing their sexual orientation or gender identity) are also less likely to engage in primary care services such as preventive vaccination.54
From a policy perspective, a lack of national recommendations is a potential system-level barrier to vaccination for TGD people. Before 2016, MSM were the only sexual minority group that was mentioned in adult vaccination recommendations, yet TGD people share risk factors for HPV infection with MSM, especially those relating to sexual health.55 The CDC ACIP recommendation for HPV vaccination added “transgender persons” in December 2016 without further elaboration.56 Even after the addition of MSM to the vaccine guidelines for HPV, the rates of vaccination in this group continue to lag behind the general population and there is emerging evidence that TGD people may also lag behind the general population despite being added to the national recommendation.57 This suggests that merely adding TGD and sexual minority people to national recommendations may not facilitate vaccine uptake among these populations; moreover, given the strong association between provider recommendation and vaccine receipt, the lag in vaccine uptake may also highlight a gap in knowledge about the national vaccine recommendations and lack of competence among health care providers for caring for TGD people.40,42
When considered in gestalt, the findings of this review begin to outline an integrated perspective of HPV vaccination among TGD people that emphasizes a set of key facilitators including patient knowledge of HPV risk, compelling recommendations from health care providers who are attuned to their needs, and national vaccination recommendations that establish TGD people as a priority at-risk population to offer HPV vaccination.
Limitations
This review addresses a gap in the literature regarding barriers to and facilitators for HPV vaccination among TGD people but is not without several limitations. First, although we conducted a thorough search of the literature from three major databases, it is possible that we missed studies that were indexed in other databases. We did not include gray literature in our search, which may have further excluded relevant citations, especially nonquantitative studies. We restricted our inclusion criteria to U.S.-based studies only, which may have excluded studies that had larger proportions of TGD people or studies focused solely on this group. Because of the limited number of studies that included TGD people in the sample, this necessitated considering study results that mixed sexual minority and TGD participants together. Although sexual minority and TGD people may experience similar challenges relating to fear of discrimination and stigma in health care, there is growing evidence that TGD people have unique health care needs and may engage in preventive care differently than cisgender sexual minority people.58
Conclusion
This study identifies the current evidence that describes barriers to and facilitators for HPV vaccination among TGD people in the United States. Few studies were identified that included TGD people and the low proportion of TGD participants in each study sample points to a significant gap in knowledge about this population that warrants further research. Our review highlights some of the factors that may contribute to disparities in HPV vaccination among sexual minority and TGD people overall, and that TGD people have additional patient-level, provider-level, and system-level factors that may influence HPV vaccine uptake. Future avenues for research should focus on recruiting TGD people to better explore HPV vaccination from their perspectives.
Abbreviations Used
- ACIP
Advisory Committee on Immunization Practices
- aOR
adjusted odds ratio
- CDC
Centers for Disease Control and Prevention
- CI
confidence interval
- CINAHL
Cumulative Index of Nursing and Allied Health Literature
- EHR
electronic health record
- HPV
human papillomavirus
- JBI
Joanna Briggs Institute
- MeSH
medical subject headings
- MSM
men who have sex with men
- OR
odds ratio
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SD
standard deviation
- STI
sexually transmitted infection
- TGD
transgender and gender diverse
Appendix A1. Database Search Queries
PubMed/MEDLINE
bisexual[tiab] OR bisexuality[MeSH Terms] OR bisexuality[tiab] OR bisexuals[tiab] OR gay[tiab] OR gays[tiab] OR GLB[tiab] OR GLBT[tiab] OR homosexual[tiab] OR homosexualities[tiab] OR homosexuality[MeSH Terms] OR homosexuality[tiab] OR homosexuals[tiab] OR intersex[tiab] OR lesbian[tiab] OR lesbianism[tiab] OR lesbians[tiab] OR LGB[tiab] OR LGBT[tiab] OR “men who have sex with men”[tiab] OR msm[tiab] OR queer [tiab] OR “sexual minorities”[tiab] OR “sexual minority”[tiab] OR “sexual orientation”[tiab] OR transgender[tiab] OR transgendered[tiab] OR transgenders[tiab] OR transsexual[tiab] OR transsexualism[MeSH Terms] OR transsexualism[tiab] OR transsexuality[tiab] OR transsexuals[tiab] OR “women loving women”[tiab] OR “women who have sex with women”[tiab] OR WSW[tiab] NOT gay[au] OR “laparoscopic gastric bypass”[tiab] OR “markov state model” OR “multiple source method”[tiab]
AND
HPV[tiab] OR human papillomavirus[tiab] OR “papillomavirus vaccines”[MeSH] OR human papilloma virus* OR HPV*[tiab] OR papillomavirus*[tiab] OR immunis*[tiab] OR immuniz*[tiab] OR vaccin*[MeSH] OR vaccine*[tiab] OR vaccination*[tiab]
AND
accept*[tiab] OR attitud*[tiab] OR attitud*[tiab] OR aware*[tiab] OR barrier*[tiab] OR behavior*[tiab] OR choice*[tiab] OR cognitive*[tiab] OR decision*[tiab] OR educat*[tiab] OR “eHealth literacy”[tiab] OR “electronic health literacy”[tiab] OR facilitat*[tiab] OR health information[tiab] OR “health literacy”[tiab] OR information*[tiab] OR intent*[tiab] OR knowledg*[tiab] OR knowledg*[tiab] OR literacy[tiab] OR literate[tiab] OR motivat*[tiab] OR participat*[tiab] OR percept*[tiab] OR predict*[tiab] OR primary prevention[tiab] OR refus*[tiab] OR seek*[tiab] OR social norm*[tiab] OR uncertain*[tiab] OR uptak*[tiab] OR value*[tiab]
CINAHL
bisexual OR bisexuality OR bisexuality OR bisexuals OR gay OR gays OR GLB OR GLBT OR homosexual OR homosexualities OR homosexuality OR homosexuality OR homosexuals OR intersex OR lesbian OR lesbianism OR lesbians OR LGB OR LGBT OR “men who have sex with men” OR msm OR queer OR “sexual minorities” OR “sexual minority” OR “sexual orientation” OR transgender OR transgendered OR transgenders OR transsexual OR transsexualism OR transsexualism OR transsexuality OR transsexuals OR “women loving women” OR “women who have sex with women” OR WSW NOT gay OR “laparoscopic gastric bypass” OR “markov state model” OR “multiple source method”
AND
HPV OR human papillomavirus OR “papillomavirus vaccines” OR human papilloma virus* OR HPV* OR papillomavirus* OR immunis* OR immuniz* OR vaccin* OR vaccine* OR vaccination*
AND
accept* OR attitud* OR attitud* OR aware* OR barrier* OR behavior* OR choice* OR cognitive* OR decision* OR educat* OR “eHealth literacy” OR “electronic health literacy” OR facilitat* OR health information OR “health literacy” OR information* OR intent* OR knowledg* OR knowledg* OR literacy OR literate OR motivat* OR participat* OR percept* OR predict* OR primary prevention OR refus* OR seek* OR social norm* OR uncertain* OR uptak* OR value*
EMBASE
bisexuality OR “LGBT people” OR homosexuality OR intersex OR “homosexual female” OR “men who have sex with men” OR “homosexual male” OR “sexual and gender minority” OR “sexual orientation” OR transgender OR transgenderism OR transsexualism OR transsexuality OR “women who have sex with women” OR “women who have sex with women and men” OR “men who have sex with men and women”
AND
“Wart virus vaccine” OR immunization OR vaccination
AND
acceptance OR “attitude to health” OR attitude OR awareness OR barriers OR behavior OR “decision making” OR cognition OR education OR “medical information” OR “health literacy” OR behavior OR literacy OR motivation OR participation OR perception OR prediction OR “primary prevention” OR prevention OR knowledge OR refuse OR “social norm” OR uncertainty OR uptake OR value
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Anthony T. Pho received predoctoral funding from The Robert Wood Johnson Future of Nursing Scholars Program. Sabrina Mangal received predoctoral funding from Reducing Health Disparities Through Informatics (RHeaDI), T32NR007969.
Cite this article as: Pho AT, Mangal S, Bakken S (2022) Human papillomavirus vaccination among transgender and gender diverse people in the United States: an integrative review, Transgender Health 7:4, 303–313, DOI: 10.1089/trgh.2020.0174.
References
- 1. Dunne EF, Markowitz LE, Saraiya M, et al. CDC grand rounds: reducing the burden of HPV-associated cancer and disease. MMWR Morb Mortal Wkly Rep. 2014;63:69–72. [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention. Incidence, Prevalence, and Cost of Sexually Transmitted Infections in the United States. Atlanta, GA: National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, 2013. [Google Scholar]
- 3. Markowitz LE, Dunne EF, Saraiya M, et al. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2014;63:1–30. [PubMed] [Google Scholar]
- 4. Petrosky E, Bocchini JA Jr., Hariri S, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2015;64:300–304. [PMC free article] [PubMed] [Google Scholar]
- 5. Office of Disease Prevention and Health Promotion—U. S. Department of Health and Human Services. Healthy People 2030. Available at https://health.gov/healthypeople/objectives-and-data/social-determinants-health%E2%80%8B Accessed March 15, 2020.
- 6. Elam-Evans LD, Yankey D, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69:1109–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Meites E, Szilagyi PG, Chesson HW, et al. Human papillomavirus vaccination for adults: updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2019;68:698–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reiter PL, McRee AL, Katz ML, Paskett ED. Human papillomavirus vaccination among young adult gay and bisexual men in the United States. Am J Public Health. 2015;105:96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McRee AL, Katz ML, Paskett ED, Reiter PL. HPV vaccination among lesbian and bisexual women: findings from a national survey of young adults. Vaccine. 2014;32:4736–4742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Williams WW, Lu PJ, O'Halloran A, et al. Surveillance of vaccination coverage among adult populations—United States, 2015. MMWR Surveill Summ. 2017;66:1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gerend MA, Madkins K, Phillips G, et al. Predictors of human papillomavirus vaccination among young men who have sex with men. Sex Transm Dis. 2016;43:185–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barefoot KN, Warren JC, Smalley KB. Women's health care: the experiences and behaviors of rural and urban lesbians in the USA. Rural Remote Health. 2017;17:3875. [DOI] [PubMed] [Google Scholar]
- 13. Cummings T, Kasting ML, Rosenberger JG, et al. Catching up or missing out? human papillomavirus vaccine acceptability among 18- to 26-year-old men who have sex with men in a US National Sample. Sex Transm Dis. 2015;42:601–606. [DOI] [PubMed] [Google Scholar]
- 14. Youatt EJ, Harris LH, Harper GW, et al. Sexual health care services among young adult sexual minority women. Sex Res Social Policy. 2017;14:345–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Flores ARB, Taylor NT, Herman JL. Race and Ethnicity of Adults Who Identify as Transgender in the United States. Los Angeles, CA: The Williams Institute, 2016. [Google Scholar]
- 16. Institute of Medicine (US) Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. The Health of Lesbian, Gay, Bisexual and Transgender People: Building a Foundation for Better Understanding. Washington DC: The National Academies Press, 2011. [PubMed] [Google Scholar]
- 17. American Psychological Association. Guidelines for psychological practice with transgender and gender nonconforming people. Am Psychol. 2015;70:832–864. [DOI] [PubMed] [Google Scholar]
- 18. James S, Herman J, Rankin S, et al. The report of the 2015 US transgender survey. 2016. Available at https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf Accessed August 1, 2020.
- 19. Bosse JD, Chiodo L. It is complicated: gender and sexual orientation identity in LGBTQ youth. J Clin Nurs. 2016;25:3665–3675. [DOI] [PubMed] [Google Scholar]
- 20. Safer JD, Coleman E, Feldman J, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016;23:168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jaffee KD, Shires DA, Stroumsa D. Discrimination and delayed health care among transgender women and men: implications for improving medical education and health care delivery. Med Care. 2016;54:1010–1016. [DOI] [PubMed] [Google Scholar]
- 22. Winter S, Diamond M, Green J, et al. Transgender people: health at the margins of society. Lancet. 2016;388:390–400. [DOI] [PubMed] [Google Scholar]
- 23. Macapagal K, Bhatia R, Greene GJ. Differences in healthcare access, use, and experiences within a community sample of racially diverse lesbian, gay, bisexual, transgender, and questioning emerging adults. LGBT Health. 2016;3:434–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bradford J, Reisner SL, Honnold JA, Xavier J. Experiences of transgender-related discrimination and implications for health: results from the Virginia Transgender Health Initiative Study. Am J Public Health. 2013;103:1820–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Meyer IH, Brown TN, Herman JL, et al. Demographic characteristics and health status of transgender adults in select US regions: behavioral risk factor surveillance system, 2014. Am J Public Health. 2017;107:582–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Peitzmeier SM, Khullar K, Reisner SL, Potter J. Pap test use is lower among female-to-male patients than non-transgender women. Am J Prev Med. 2014;47:808–812. [DOI] [PubMed] [Google Scholar]
- 27. Peitzmeier SM, Reisner SL, Harigopal P, Potter J. Female-to-male patients have high prevalence of unsatisfactory Paps compared to non-transgender females: implications for cervical cancer screening. J Gen Intern Med. 2014;29:778–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. National Institutes of Health. Sexual & Gender Minority Research Office. 2019. Available at https://dpcpsi.nih.gov/sgmro Accessed March 3, 2020.
- 29. Agenor M, Peitzmeier S, Gordon AR, et al. Sexual orientation identity disparities in awareness and initiation of the human papillomavirus vaccine among U.S. women and girls: a national survey. Ann Intern Med. 2015;163:99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Agenor M, McCauley HL, Peitzmeier SM, et al. Sex of sexual partners and human papillomavirus vaccination among U.S. girls and women. Am J Prev Med. 2016;50:318–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Agenor M, Peitzmeier SM, Gordon AR, et al. Sexual orientation identity disparities in human papillomavirus vaccination initiation and completion among young adult US women and men. Cancer Causes Control. 2016;27:1187–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Charlton BM, Reisner SL, Agenor M, et al. Sexual orientation disparities in human papillomavirus vaccination in a longitudinal cohort of U.S. males and females. LGBT Health. 2017;4:202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. [DOI] [PubMed] [Google Scholar]
- 34. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52:546–553. [DOI] [PubMed] [Google Scholar]
- 35. Lee JGL, Ylioja T, Lackey M. Identifying lesbian, gay, bisexual, and transgender search terminology: a systematic review of health systematic reviews. PLoS One. 2016;11:e0156210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bramer WM, Giustini D, de Jonge GB, et al. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016;104:240–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Johanna Briggs Institute. EBP Resources and Publications—Critical Appraisal Tools. 2018. Available at http://joannabriggs.org/research/critical-appraisal-tools.html Accessed December 25, 2018.
- 38. Wu YP, Thompson D, Aroian KJ, et al. Commentary: writing and evaluating qualitative research reports. J Pediatr Psychol. 2016;41:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Apaydin KZ, Fontenot HB, Borba CPC, et al. Three-dose HPV vaccine completion among sexual and gender minority young adults at a Boston community health center. Vaccine. 2018;36:4897–4903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bednarczyk RA, Whitehead JL, Stephenson R. Moving beyond sex: assessing the impact of gender identity on human papillomavirus vaccine recommendations and uptake among a national sample of rural-residing LGBT young adults. Papillomavirus Res. 2017;3:121–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fontenot HB, Lee-St John T, Vetters R, et al. The association of health seeking behaviors with human papillomavirus vaccination status among high-risk urban youth. Sex Transm Dis. 2016;43:771–777. [DOI] [PubMed] [Google Scholar]
- 42. Gorbach PM, Cook R, Gratzer B, et al. Human papillomavirus vaccination among young men who have sex with men and transgender women in 2 US cities, 2012–2014. Sex Transm Dis. 2017;44:436–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Halkitis PN, Valera P, LoSchiavo CE, et al. Human papillomavirus vaccination and infection in young sexual minority men: the P18 cohort study. AIDS Patient Care STDS. 2019;33:149–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Singh V, Gratzer B, Gorbach PM, et al. Transgender women have higher human papillomavirus prevalence than men who have sex with men-two U.S. cities, 2012–2014. Sex Transm Dis. 2019;46:657–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Apaydin KZ, Fontenot HB, Shtasel D, et al. Facilitators of and barriers to HPV vaccination among sexual and gender minority patients at a Boston community health center. Vaccine. 2018;36:3868–3875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Gilbert PA, Lee AA, Pass L, et al. Queer in the heartland: cancer risks, screenings, and diagnoses among sexual and gender minorities in Iowa. J Homosex. 2020. [Epub ahead of print]; DOI: 10.1080/00918369.2020.1826832. [DOI] [PubMed] [Google Scholar]
- 47. Kobayashi T, Sigel K, Gaisa M. Prevalence of anal dysplasia in human immunodeficiency virus-infected transgender women. Sex Transm Dis. 2017;44:714–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Gatos KC. A literature review of cervical cancer screening in transgender men. Nurs Womens Health. 2018;22:52–62. [DOI] [PubMed] [Google Scholar]
- 49. Nowak GJ, Sheedy K, Bursey K, et al. Promoting influenza vaccination: insights from a qualitative meta-analysis of 14 years of influenza-related communications research by U.S. Centers for Disease Control and Prevention (CDC). Vaccine. 2015;33:2741–2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Horvath KJ, Iantaffi A, Grey JA, Bockting W. A review of the content and format of transgender-related webpages. Health Commun. 2012;27:457–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. MacCarthy S, Reisner SL, Nunn A, et al. The time is now: attention increases to transgender health in the United States but scientific knowledge gaps remain. LGBT Health. 2015;2:287–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wheldon CW, Sutton SK, Fontenot HB, et al. Physician communication practices as a barrier to risk-based HPV vaccine uptake among men who have sex with men. J Cancer Educ. 2018;33:1126–1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Blackwell CW. Knowledge of vaccination needs of HIV-infected men who have sex with men in a national sample of ‘Gay Friendly’ health care providers. Public Health Nursing. 2016;33:403–411. [DOI] [PubMed] [Google Scholar]
- 54. Whitehead J, Shaver J, Stephenson R. Outness, stigma, and primary health care utilization among rural LGBT populations. PLoS One. 2016;11:e0146139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Castillo R, Konda KA, Leon SR, et al. HIV and sexually transmitted infection incidence and associated risk factors among high-risk MSM and male-to-female transgender women in Lima, Peru. J Acquir Immune Defic Syndr. 2015;69:567–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Meites E, Kempe A, Markowitz LE. Use of a 2-Dose Schedule for Human Papillomavirus Vaccination—Updated Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2016;65:1405–1408. [DOI] [PubMed] [Google Scholar]
- 57. Oliver SE, Hoots BE, Paz-Bailey G, et al. Increasing human papillomavirus vaccine coverage among men who have sex with men-national HIV behavioral surveillance, United States, 2014. J Acquir Immune Defic Syndr. 2017;75(Suppl 3):S370–S374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Edmiston EK, Donald CA, Sattler AR, et al. Opportunities and gaps in primary care preventative health services for transgender patients: a systemic review. Transgend Health. 2016;1:216–230. [DOI] [PMC free article] [PubMed] [Google Scholar]