Abstract
Background:
The COVID-19 pandemic accelerated the development of telehealth services and thus the need for telehealth education and training to support rapid implementation at scale. A national survey evaluating the current state of the telehealth landscape was deployed to organizational representatives, and included questions related to education and training.
Materials and Methods:
In the summer of 2020, 71 survey participants (31.8%) completed an online survey seeking to determine the utilization of telehealth services across institutional types and locations. This included data collected to specifically compare the rates and types of formal telehealth education provided before and during the pandemic.
Results:
Thirty percent of organizations reported no telehealth training before COVID-19, with those in suburban/rural settings significantly less likely to provide any training (55% vs. 82%) compared with urban. Pandemic-related training changes applied to 78% of organizations, with more change happening to those without any training before COVID-19 (95%). Generally, organizations offering training before the pandemic reported deploying COVID-19-related telehealth services, while a higher percentage of those without any training beforehand reported that they either did not plan on providing these services or were in the early planning stages.
Discussion:
Telehealth education is moving from elective to essential based on the need to prepare and certify the workforce to support high-quality telehealth services.
Conclusions:
As telehealth continues to evolve to meet the future health care service needs of patients and providers, education and training will advance to meet the needs of everyday clinical encounters and broader public health initiatives.
Keywords: medical education, telehealth, telemedicine, COVID-19, training, research, online education
Background
Prior to the COVID-19 pandemic, there was limited evidence for standard recommendations and validated best practices for telehealth education for both clinicians and students of health care professions.1,2 Proficiencies, competencies, curricula, and delivery modalities of telehealth education vary across programs, and rigorous research evaluating the effectiveness of telehealth training is minimal but evolving.1,2 Without well-researched and accredited established educational curricula, the COVID-19 pandemic necessitated the rapid scaling of alternative health care delivery models to quickly and effectively train clinicians on telehealth implementation and best practices.
To evaluate the type and maturity of telehealth interventions implemented in response to the novel coronavirus throughout the United States and identify common barriers limiting telehealth utilization during the pandemic, the Supporting Pediatric Research on Outcomes and Utilization of Telehealth (SPROUT)–Clinical and Translational Science Award (CTSA) Collaborative Telehealth Research Network developed the Telehealth Utilization in Response to the COVID-19 Pandemic Survey.
The survey was designed to explore how telehealth was leveraged to support health care delivery during the public health emergency and provide preliminary data to support future research on telehealth efficacy across the health care delivery system not only during a national emergency, but for sustained utilization postpandemic as well. Newly adopted and modified telehealth training modalities were assessed as essential components of effective implementation of telehealth programs.
SPROUT is the research subcommittee of the Section on Telehealth Care (SOTC) at the American Academy of Pediatrics (AAP), which facilitated access to a national collection of pediatric telehealth champions to complete the survey per qualifying organization.3 The SOTC is dedicated to advancing pediatric telehealth education, research, and evidence-based policy development4 nationally, while SPROUT focuses on promoting and supporting interdisciplinary and interprofessional multisite telehealth research and the development of research frameworks, tools, and best practices.5 Each maintains a diverse representation of telehealth professionals, including physicians, advanced practice providers, research professionals, allied health professionals, and telehealth administrators. At the time of survey deployment, the SOTC's membership exceeded 400 members, and SPROUT's membership exceeded 250 members spanning more than 120 medical organizations.
As a result of the pandemic, facility preparedness for rapid rollout of telehealth became mission critical.6,7 To ensure continuity of care, health care organizations and private practices quickly adapted to scaling of telehealth across service lines while simultaneously determining the best methods to efficiently train staff on telehealth utilization and implementation.8,9 Understanding the impact of these rapid changes will benefit researchers, administrators, and educators as they consider the role training played in the success of rapid telehealth implementation. Furthermore, the comparison of telehealth training strategies before the pandemic and changes made in response to rapid rollout provides a unique opportunity to determine needed resources for organizations in the process of developing telehealth programs. Results and analysis of the education and training portions of the Telehealth Utilization in Response to the COVID-19 Pandemic Survey are presented here.
Materials and Methods
The Telehealth Utilization in Response to the COVID-19 Pandemic Survey was deployed to members of the AAP SOTC and SPROUT listservs. The study received IRB exempt status from the AAP.
Participants
Medical facilities within the United States, delivering direct patient care within academic medical centers, nonacademic medical centers, group practices, and individual practices, were included in the study. Health care organizations with affiliates in different cities or states were counted as independent organizations. We excluded prepandemic telehealth-only practices, telehealth support organizations that do not deliver direct patient care, departments of public health, health insurance companies, and medical facilities without a potential respondent or a respondent whose credentials, facility affiliation, or job title could not be confirmed.
A single telehealth champion from each qualifying medical facility was identified as a unique respondent on behalf of eligible participant organizations. An organizational respondent had to be a clinician or have a clearly defined job title within a telehealth center. Qualifying credentials included MD, DO, DNP, NP, MSN, PA, BSN, MBA, MPH, PhD, or other degrees if the job title was directly related to telehealth and there was no other candidate listed for a particular organization. Selection priority was given to physicians with a telehealth leadership role followed by physicians with a nontelehealth leadership role. Members of both listservs were excluded from participating as a respondent if they were a dentist, had a research-only position, and whose credentials, facility affiliation, or contact information could not be confirmed.
A combined total of 728 members (242 SPROUT members and 474 SOTC members) were vetted for participation. A total of 164 SOTC members and their organizational affiliations were reviewed for participation after excluding 312 members for insufficient information to determine eligibility or redundancy to the SPROUT listserv. All 242 SPROUT members were reviewed for eligibility. The SPROUT listserv resulted in 98 organizations and the SOTC listserv resulted in 125 organizations, for a total of 223 organizations.
Survey Development and Administration
The survey questions were developed de novo by a group of telehealth experts in collaboration with a survey methodologist. One part of the survey was specifically designed to assess whether and how organizations trained their providers on using telehealth before the pandemic, as well as if and what changes were made to the telehealth training due to the COVID-19 pandemic. We classified telehealth training into three categories: (1) no training, (2) real-time training that could either take place in a classroom or individual setting, and in-person as well as online, and (3) synchronous or asynchronous and real-time hybrid training where either all or some portions are completed asynchronously online.
Most of the survey was focused on how organizations were progressing in establishing five common COVID-19-related telehealth services and the barriers they had encountered: (1) virtual COVID-19 screening, (2) scheduled ambulatory visits, (3) inpatient virtual PPE, (4) home-monitoring of COVID-19 patients, and (5) provider-to-provider specialty consults related to confirmed or suspected COVID-19 patients. The survey also included a small number of questions about the respondent, such as specialty and role, and the organization or the practice, such as organization type (academic medical center, nonacademic medical center, private practice), practice setting (urban, suburban/rural), state, and patient population (pediatric patients only, adult, and pediatric patients).
The final survey draft was assessed for understandability and ease of completion through five cognitive interviews, resulting in small changes to the wording of questions and added definitions for several terms. The final survey was programmed in REDCap.10
The selected telehealth champion received an invitation e-mail with a link to the web survey on behalf of the SPROUT-CTSA Network at the beginning of July 2020. Data collection spanned a 2-month period until September 2020 with three reminder e-mails sent during the first 2 weeks, and at least one personal e-mail from one of the study principal investigators during the next 6 weeks. A PDF-version of the survey was made available to participants on request to assist with accurate data collection among their organizational stakeholders.
Data Management and Statistics
All analyses were performed using Stata statistical software version 14.2 (StataCorp., College Station, TX). Descriptive statistics, such as percentages, were primarily used. Bivariate relationships between telehealth training types and organizational characteristics as well as the development status of each COVID-related telehealth services were assessed using Fisher's exact test.
Results
We received 71 eligible responses to our survey, resulting in a response rate of 31.8% (71/223). Respondents represent organizations from 32 states. The majority of respondents work in academic medical centers (55%), are primary care specialists (42%), and located in an urban setting (55%) (Table 1). Nearly half have a role directly related to telehealth as telehealth medical director (31%), telehealth program director (11%), or telehealth manager/coordinator (7%). The patient population served by respondents' organizations is evenly split between pediatric patients only and adults and pediatric patients.
Table 1.
Background Demographics
| CHARACTERISTIC | N | PERCENTAGE |
|---|---|---|
| Organization type (n = 71) | ||
| Academic medical center | 39 | 55 |
| Nonacademic medical center | 12 | 17 |
| Group practice | 5 | 7 |
| Private practice | 14 | 20 |
| Other | 1 | 1 |
| Specialty (n = 71) | ||
| Not a clinician | 10 | 14 |
| Primary care | 30 | 42 |
| Medical specialty | 13 | 18 |
| Surgical specialty | 1 | 11 |
| Inpatient-only specialty | 11 | 16 |
| Diagnostic specialty | 0 | 0 |
| Emergency medicine | 6 | 9 |
| Setting (n = 71) | ||
| Urban | 39 | 55 |
| Suburban | 27 | 38 |
| Rural | 5 | 7 |
| Role (n = 70) | ||
| Telehealth program director | 8 | 11 |
| Telehealth medical director | 21 | 31 |
| Telehealth manager/coordinator | 5 | 7 |
| Chief medical information officer | 3 | 4 |
| Medical director | 6 | 9 |
| Academic leader | 6 | 9 |
| Clinician/provider | 7 | 10 |
| Owner/partner/C-suite | 8 | 11 |
| Other | 5 | 7 |
| Patient population (n = 70) | ||
| Pediatric patients only | 36 | 51 |
| Adult patients only | 0 | 0 |
| Adult and pediatric patients | 34 | 49 |
Nearly one-third of respondents reported that their organization did not provide any telehealth training before COVID-19 (30%). Those organizations that did provide telehealth training before COVID-19 reported either combined asynchronous and real-time hybrid training (37%) or only real-time training (33%); real-time training in either case could be either in-person or online.
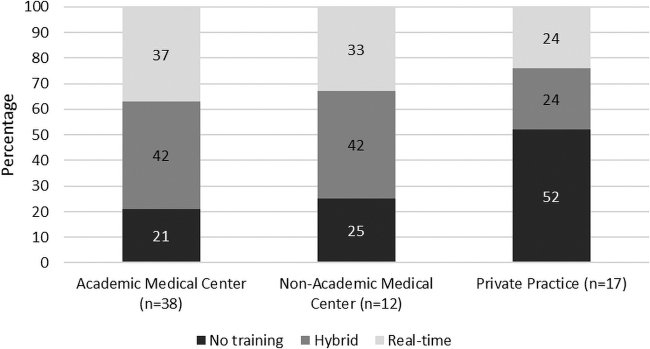
The existence of telehealth training before COVID-19 varied by organization type, although not significantly (Fig. 1). Fifty-two percent of private practices compared with 25% of nonacademic medical centers and 21% of academic medical centers did not report any telehealth training before COVID-19 (p = 0.242).
Fig. 1.
Telehealth training before COVID-19 by organization type (p = 0.242).
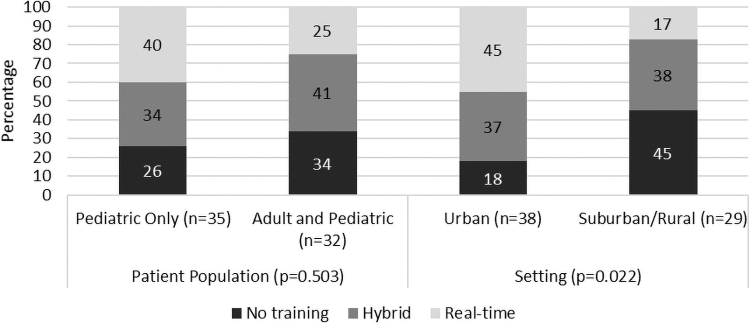
Practices and medical centers in suburban or rural settings were significantly less likely to report having telehealth training (55%) in place before the pandemic compared with those in urban settings (82%) (p = 0.022) (Fig. 2). Of those with existing telehealth training, medical centers and practices in suburban and rural settings were more likely to report the use of hybrid training compared with real-time (38% vs. 17%), while those in an urban setting were slightly more likely to report real-time training compared with hybrid training (45% vs. 37%).
Fig. 2.
Telehealth training before COVID-19 by patient population and setting.
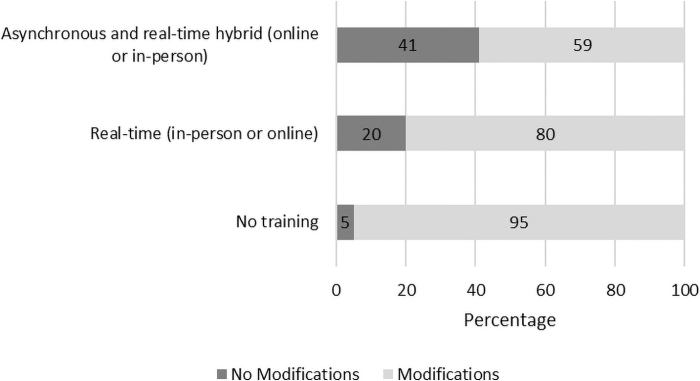
In the face of the COVID-19 pandemic, 78% of organizations made modifications to their telehealth training in response to the pandemic (Fig. 3), including 95% of those without any telehealth training before the pandemic, 80% of those reporting only real-time training before the pandemic, and 59% of those reporting asynchronous and real-time hybrid training before the pandemic.
Fig. 3.
Telehealth training modifications since COVID-19 by training category (p = 0.020).
We asked organizations who reported modifications to describe them in more detail. Several primary care providers who did not provide telehealth training before COVID-19 reported that they used technology, customer service, and vendor-led training or computer-based learning and required it for all users, while others only provided training guides or tip sheets.
One primary care provider commented “[we are a] small practice, had an office meeting, then attended a vendor-led orientation and now keep training info available for practice on google docs,” while another one emphasized that there was “minimal didactic training then [we learned] from providers who started using it in our practice.” Larger medical centers without any training before COVID-19 often organized mandatory mass asynchronous online training of care team members. Because of the rapid evolution of the situation “training was very rushed, very nuts and bolts and not about the experience or best practices of using telehealth.”
The practices and medical centers who had used in-person training reported that the in-person component was either replaced by webinars or asynchronous online training, including video Q&A sessions and recorded teaching videos to supplement existing learning modules. Handouts, tip sheets, and guidelines were used by a vast majority of respondents. Others reported “waiv(ing) the requirements for the computer-based training, which is required of all providers since it is part of their hospital privileges.”
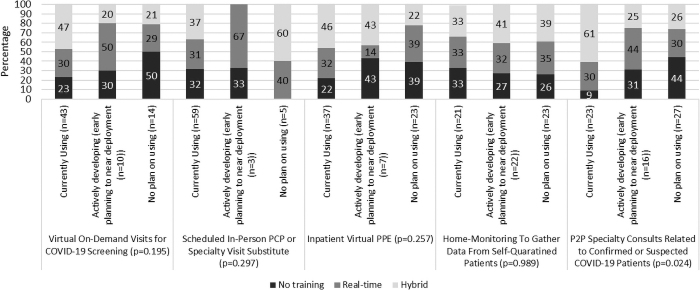
Finally, respondents reported significant variation in service type and the state of development/deployment of that service type correlated to prior telehealth training (Fig. 4). The amount of previous training seems to inform the provision of telehealth services for all service types except the scheduled in-person PCP or specialty visit substitutes. This is due to the nature of virtual visits as continuity of care encounters.
Fig. 4.
Influence of telehealth training before COVID-19 on usage of telehealth by service types.
Added to these telehealth service types are modalities that encompass additional health analytic and artificial intelligence components yet to be defined. Training modalities continue to evolve to meet the needs of new system and technical integrations as telehealth education and training will continue to be a fundamental requirement for program adoption and success.
Discussion
This is the first multicenter national evaluation of telehealth education and training in response to the COVID-19 pandemic. New literature has emerged during the pandemic outlining and evaluating telehealth training modalities across various medical settings and specialties, further highlighting the lack of uniformity of telehealth education.9,11
This survey on telehealth training and educational practices found that telehealth training was not consistently delivered before the pandemic, with 30% of programs reporting no formal training program. The modality of training prepandemic was either exclusively synchronous (33%) or a hybrid of synchronous and asynchronous training (37%). As part of the pandemic response, 78% of organizations modified their prior training plan, with 95% of those who previously did not offer training reporting implementation of telehealth training.
Telehealth training in response to COVID-19 was primarily online with more organizations commenting on switching to asynchronous online training, presumably due to distancing and infection control precautions aimed at reducing viral spread.
Results of the survey indicate widespread adoption of telehealth training in response to the pandemic across disciplines and practice settings. Previous studies support that telehealth training reduces previously cited barriers to provider adoption and engagement, including ease of use and perceived usefulness of this modality of care delivery.12–15 One qualitative analysis identified training as a key facilitator for delivering telehealth services.16 The vast increase in adoption of telehealth in response to the COVID-19 pandemic magnifies the importance of ensuring that clinicians possess the skills required to deliver care via this modality.
Our findings serve as a foundation for the development of best practices and training resources to support the expansion of telehealth services to meet organizational and health care team needs.17
Before the pandemic, there was a dearth of literature on clinician training for telehealth. A landscape review of telehealth education integrated into health professions training programs revealed no consistency in how telehealth was integrated into various health care curricula1 or the optimal modality for training. We do know that adults learn best through experiential learning18 and that providers familiar with technology are more inclined to use telemedicine,19 a barrier that is overcome with exposure and hands-on training.20,21 Longitudinal interdisciplinary telehealth simulation curriculum of trainees found that it is both feasible and improves confidence in the ability to use telemedicine to provide complex patient care.22
Our results demonstrate that telehealth education is seen as important and was widely integrated into training protocols to facilitate telehealth services at an expanded scale during the pandemic.
Still, higher levels of in-person and experiential training were not possible during the pandemic. In fact, 80% of organizations that had previously provided in-person telehealth training reported pandemic-related modifications. Training modalities varied by population, organization type, service type, and geography. Differences were evident in the training afforded by urban verses suburban and rural populations both before and during the pandemic (Fig. 3).
Based on these data, there are several lessons learned. First, the modality of the training shifted to largely online offerings during the pandemic. A previous study evaluating tele-simulation training for neonatology with both remote participants and facilitators, using telehealth software as an alternative to in-person telehealth training,23 found that larger group trainings were feasible and resulted in increased provider comfort with some telemedicine-specific skills (e.g., sharing pictures), but less so with others (e.g., troubleshooting technical issues). Even with training, 56% of participants expressed continued discomfort with telemedicine applications and technology.
The results support prior assertions that comprehensive telehealth education should include a focus on planning and preparing for telehealth service delivery.8 Hands-on training was not necessary for providers to utilize telehealth, but a minimum amount of process training was required to get providers operational in their institution's platforms.
Our study has limitations, including the distribution of survey invitations to individual contact points representing SPROUT member organizations. While their responses were voluntary, highly informed by those directly responsible for telehealth activities with the organization, and were completed during the pandemic, the results may not tell the whole story of how individual teams implemented training to ensure continuity of care. The survey did not assess training content or length for the training offered pre- or during the pandemic. Most importantly, the survey did not address the effectiveness of training or efficacy related to training as part of the adoption of telehealth services.
Before the pandemic, organizations such as the American Medical Association (AMA) and the Association of American Medical Colleges (AAMC)24 identified gaps in the development of training to support telehealth care delivery. Even with these advances, best practices were not fully defined and training was not uniformly delivered across organizations.1,9 The professional associations along with health care accrediting organizations have since released playbooks and initial competencies to guide training programs and health care providers in how to practice telehealth at the highest levels of professionalism.25–28 Through the continued development and refinement of competencies across discipline and provider roles, structures will be enacted to ensure that telehealth is delivered using standardized procedures.
In addition, educators and researchers are planning for future studies to determine optimal levels of competencies and modalities for initial training as well as subsequent updates, and to ensure provider and patient retention. Information obtained through analysis of survey responses has the potential to inform future research on telehealth efficacy across the health care delivery system not only during a national emergency, but also as an ongoing template to integrate telehealth as a standard method of health care delivery.
Conclusions
This study provides an assessment of the landscape of the COVID-19 pandemic on telehealth training efforts across the country. These efforts were scaled rapidly across a variety of specialties and practice types, facilitating the nationwide response to the pandemic. Understandably, training also shifted substantially toward online and remote models. The pandemic response increased the allocation of resources for telehealth training programs, reducing the disparity in availability of telehealth training between private practice and larger health care systems (academic and nonacademic), and between rural, suburban, and urban centers. The shift toward remote training, and the development of scalable training models during the pandemic, including asynchronous models, may facilitate the broader and more uniform dissemination of training resources in the future, and thus contribute to a reduction in disparities in access to care across communities and populations.
Telehealth education has entered a period of unprecedented relevance and universal applicability. Just as telehealth services have continued to meet the needs of patients and providers during the second year of the pandemic, additional telehealth education offerings for students, trainees, faculty, and staff are deemed essential to ensure a well-trained health care workforce.
Future research is needed on telehealth efficacy across the health care delivery system not only during a national emergency, but also as an ongoing template to integrate telehealth as a standard method of health care delivery. This research will allow the development of best practices and uniform curricula supporting broader telehealth competencies, which will in turn allow for more rigorous assessment of the clinical and financial/economic impact of telehealth services.
Acknowledgments
We thank John Chuo MD, MSBI, IA, for his significant contributions to project leadership, development of the survey, and access to REDCap through the Children's Hospital of Philadelphia. We also acknowledge the AAP for providing IRB approval and the participant pool through the Section on Telehealth Care and SPROUT listservs.
Authors' Contributions
C.C., MSPA, MPH, contributed to the study design, protocol, and survey development, interpretation of results, article draft, review, and edits.
S.Z. as the coinvestigator contributed to the study design, directed survey development, data acquisition, and data analysis, article draft, review, and edits.
R.D.-M., PhD, contributed to the interpretation of results, expert guidance on telehealth education, article draft, review, and edits.
D.S., MD, contributed to the interpretation of results, expert guidance on telehealth education, article draft, review, and edits.
S.D.M., MD, MPH, was the lead investigator responsible for survey concept, survey development, interpretation of results, and critical review of article.
All authors agreed to the final submission.
Internal Review Board Approval
This study was reviewed and approved for exempt status by the Internal Review Board at the American Academy of Pediatrics on June 3, 2020.
Disclosure Statement
The authors have no competing interests, personal financial interests, employment by an organization that may gain or lose financially from the publication of the article, or personal relationship that may inappropriately affect the integrity of the research reported.
Funding Information
This publication was supported, in part, by the NIH/NCATS SPROUT-CTSA Collaborative Telehealth Network Grant Number U01TR002626. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- 1. Chike-Harris KE, Durham C, Logan A, Smith G, Dubose-Morris R. Integration of telehealth education into the health care provider curriculum: A review. Telemed J E Health 2021;27:137–149. [DOI] [PubMed] [Google Scholar]
- 2. Pourmand A, Ghassemi M, Sumon K, Amini SB, Hood C, Sikka N. Lack of telemedicine training in academic medicine: Are we preparing the next generation? Telemed J E Health 2021;27:62–67. [DOI] [PubMed] [Google Scholar]
- 3. Chuo J, Macy ML, Lorch SA. Strategies for evaluating telehealth. Pediatrics 2020;146:e20201781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. AAP Section on Telehealth Care (SOTC). Available at https://services.aap.org/en/community/aap-sections/telehealth-care (last accessed April 28, 2021).
- 5. Supporting Pediatric Research on Outcomes and Utilization of Telehealth (SPROUT). American Academy of Pediatrics. Available at https://services.aap.org/en/community/aap-sections/telehealth-care/sprout (last accessed June 6, 2021).
- 6. Zheng Wong MY, Visva Gunasekeran D, Nusinovici S, et al. Telehealth demand trends during the COVID-19 pandemic in the top 50 most affected countries: Infodemiological evaluation. JMIR Public Health Surveill 2021;7:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Koonin LM, Hoots B, Tsang CA, et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic—United States, January–March 2020. MMWR Morb Mortal Wkly Rep 2020;69:1595–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rutledge C, Hawkins EJ, Bordelon M, Gustin TS. Telehealth education: An interprofessional online immersion experience in response to COVID-19. J Nurs Educ 2020;59:570–576. [DOI] [PubMed] [Google Scholar]
- 9. Wamsley M, Cornejo L, Kryzhanovskaya I, et al. Best practices for integrating medical students into telehealth visits. JMIR Med Educ 2021;7:e27877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. REDCap. Available at https://www.project-redcap.org (last accessed April 28, 2021).
- 11. Hah H, Goldin D. Exploring care providers' perceptions and current use of telehealth technology at work, in daily life, and in education: Qualitative and quantitative study. J Med Internet Res 2019;21:e13350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hopp F, Whitten P, Subramanian U, Woodbridge P, Mackert M, Lowery J. Perspectives from the Veterans Health Administration about opportunities and barriers in telemedicine. J Telemed Telecare 2006;12:404–409. [DOI] [PubMed] [Google Scholar]
- 13. Sisk B, Alexander J, Bodnar C, et al. Pediatrician attitudes toward and experiences with telehealth use: Results from a national survey. Acad Pediatr 2020;20:628–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rogove HJ, McArthur D, Demaerschalk BM, Vespa PM. Barriers to telemedicine: Survey of current users in acute care units. Telemed J E Health 2012;18:48–53. [DOI] [PubMed] [Google Scholar]
- 15. Moore MA, Coffman M, Jetty A, Petterson S, Bazemore A. Only 15% of FPs report using telehealth; training and lack of reimbursement are top barriers. Am Fam Physician 2016;93:101. [PubMed] [Google Scholar]
- 16. Traube DE, Cederbaum JA, Taylor A, Naish L, Rau A. Telehealth training and provider experience of delivering behavioral health services. J Behav Health Serv Res 2021;48:93–102. [DOI] [PubMed] [Google Scholar]
- 17. Johnson KF, Rehfuss M. Telehealth interprofessional education: Benefits, desires, and concerns of counselor trainees. J Creat Ment Health 2020;16:15–30. [Google Scholar]
- 18. Yardley S, Teunissen PW, Dornan T. Experiential learning: Transforming theory into practice. Med Teach 2012;34:161–164. [DOI] [PubMed] [Google Scholar]
- 19. Holden RJ, Karsh B-T. The technology acceptance model: Its past and its future in health care. J Biomed Inform 2010;43:159–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cappi V, Artioli G, Ninfa E, et al. The use of blended learning to improve health professionals' communication skills: A literature review. Acta Biomed 2019;90(Suppl 4):17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wang JJ, Lavigueur O, Sheridan M, Stern E. Implementation of a simulation-based telemedicine curriculum. Med Educ 2017;51:1178–1179. [DOI] [PubMed] [Google Scholar]
- 22. Wong R, Ng P, Spinnato T, et al. Expanding telehealth competencies in primary care: A longitudinal interdisciplinary simulation to train internal medicine residents in complex patient care. J Grad Med Educ 2020;12:745–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Brei BK, Neches S, Gray MM, et al. Telehealth training during the COVID-19 pandemic: A feasibility study of large group multiplatform telesimulation training. Telemed J E Health 2021;27:1166–1173. [DOI] [PubMed] [Google Scholar]
- 24. Galpin K, Sikka N, King SL, Horvath KA, Shipman SA. Expert consensus: Telehealth skills for health care professionals. Telemed J E Health 2021;27:820–824. [DOI] [PubMed] [Google Scholar]
- 25. Coenen C, Dijkstra A, Fautz C, et al. New and Emerging Areas in Medicine Series: Telehealth Competencies. 2020;5. Available at https://www.aamc.org/system/files/2020-09/hca-telehealthcollection-telehealth-competencies.pdf (last accessed May 14, 2021).
- 26. American Medical Association. Telehealth Implementation Playbook. 2020. Available at https://www.ama-assn.org/terms-use
- 27. Quick Safety Issue 55: The optimal use of telehealth to deliver safe patient care | The Joint Commission. 2020. Available at https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/quick-safety/quick-safety-issue-55 (last accessed May 14, 2021).
- 28. AAMC. Telehealth Competencies Across the Learning Continuum. AAMC New and Emerging Areas in Medicine Series. Washington, DC: AAMC, 2021. [Google Scholar]