To the Editor,
Plastic bronchitis (PB) is a rare presentation wherein thick casts line the airways, leading to respiratory symptoms ranging from cough or wheeze to acute respiratory failure.1 Classification of casts has evolved from inflammatory vs noninflammatory to classification by a combination of etiology and histology.2 Histologic differences are associated with different underlying diseases. Acellular fibrinous or mucinous casts are typically seen in children with congenital heart disease, whereas casts from children with asthma or atopy often contain eosinophils and Charcot-Leyden crystals.1 These patterns suggest differing mechanisms of cast formation.
Many children without significant cardiac history who present acutely with plastic bronchitis do not have recurrence of cast formation. In a retrospective case series that included 9 such children with a follow up period, seven children did not have recurrence.1 Many cases of PB have occurred in influenza2 or adenovirus3 infections, but PB has been reported only twice in patients with human bocavirus (HBoV).2,4 Here we present a severe case of PB secondary to HBoV in a previously healthy child with no asthma history, requiring extracorporeal membrane oxygenation (ECMO) and bronchoscopic cast removal. Per institutional guidelines, it was exempt from Institutional Review Board approval.
CASE:
A 3-year-old previously healthy male presented with respiratory distress following three days of cough and rhinorrhea, and one day of fever. He was hypoxemic with diffuse wheezing and the initial chest radiograph was consistent with a viral process, without focal opacity. Despite treatment with albuterol, methylprednisolone, magnesium, terbutaline, and non-invasive positive pressure ventilation, the patient decompensated, requiring intubation. Following intubation, he had further desaturations with repeat chest radiograph revealing complete opacification of the left lung (Fig. 1A). Despite maximal ventilator support, he had worsening respiratory and metabolic acidosis. He ultimately required veno-venous (VV) ECMO within hours of arrival. A bedside bronchoscopy demonstrated bronchial casts completely obstructing the right upper lobe, and a large obstruction extending from the left main bronchus into the upper and lower bronchi. A combination of suction, saline lavage, and an endovascular snare inserted via the bronchoscope channel achieved cast removal, including one large cast from the left bronchial tree (Fig. 2). Repeat chest radiograph showed improved aeration of the left lung (Fig. 1B). Histopathology revealed a proteinaceous background with extensive inflammatory infiltrate, including numerous eosinophils, without the presence of Charcot-Leyden crystals. Metagenomic next-generation sequencing identified human bocavirus-1 (HBoV1), without the detection of bacteria, fungi, or parasites. Magnetic resonance imaging (MRI) with lymphatic mapping did not demonstrate anatomic abnormalities. The patient was ultimately decannulated from ECMO, extubated and discharged to inpatient rehabilitation after 2 weeks of hospitalization, without recurrence of casts.
Figure 1A and 1B.
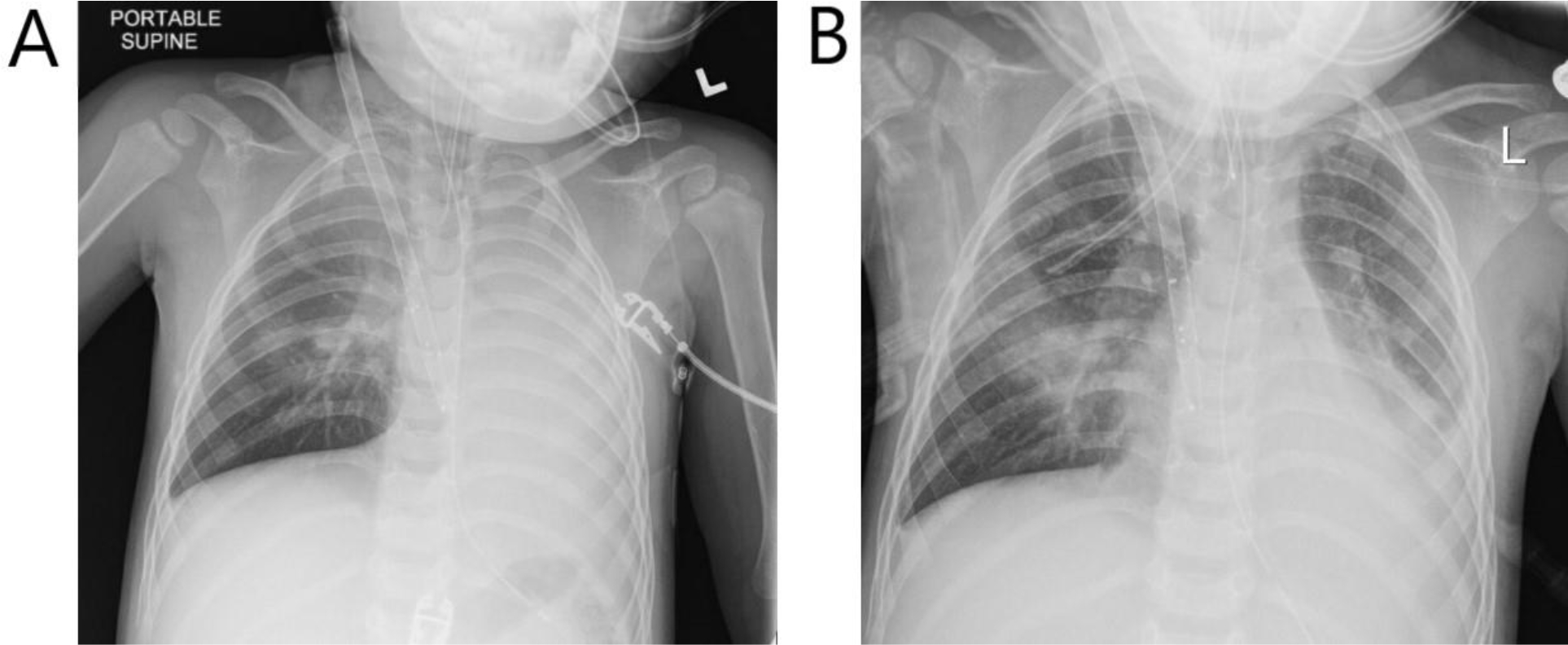
(A) Chest radiograph prior to bronchoscopy, and (B) approximately 1 hour after bronchoscopy.
Figure 2.

Bronchial cast removed from the left mainstem bronchus
DISCUSSION:
Plastic bronchitis is a rare pulmonary condition that has been associated with asthma, atopy, sickle cell anemia, cystic fibrosis and viral respiratory infections.1–4 In rare cases, PB develops in children with no underlying disease.1 Due to the heterogeneity of associated conditions understanding of pathophysiology remains challenging.
Here, we present a case of a child with no significant previous medical history who developed severe acute respiratory failure due to PB, requiring ECMO support within hours of presentation. Classification schemes have attempted to categorize PB as inflammatory or acellular/lymphatic.2 However, in this case, cast histopathology included features of each. Standard viral evaluation was negative, but further viral testing identified HBoV1 as the likely etiologic agent. Of note, the patient’s older brother developed similar viral respiratory symptoms at the same time and required only supportive care at home. Thus, it is likely that predisposing factors existed leading to development of PB in this patient.
With no history of asthma or other chronic illness to suggest the patient was at higher risk for PB, there was question of underlying lymphatic abnormalities or pulmonary lymphatic perfusion syndrome.5 This syndrome, commonly seen in people who have undergone Glenn or Fontan procedures, results in engorgement of the pulmonary lymphatics and subsequent leakage into the airways and formation of casts.5 MRI evaluation of our patient, performed after the acute phase of illness, revealed small bilateral pleural effusions without abnormal lymphatic anatomy or flow.
To our knowledge, there have been only 2 prior case reports of plastic bronchitis in the setting of HBoV1.2,4 HBoV1, a member of the family Parvoviridae, is one of the most common viruses associated with upper and lower respiratory tract infection in children less than 5 years of age in Europe.2 The exact prevalence in the US is not clear, and in the authors’ experience it is not a virus that is routinely tested. Not all cases in the literature report an identified etiologic agent, thus it is possible HBoV1 is underappreciated as a causative agent.
Treatment for plastic bronchitis varies depending on the etiology and cellular component of casts. Treatment strategies may include bronchoscopy for cast removal, chest physiotherapy, albuterol, inhaled or systemic corticosteroids, inhaled tissue plasminogen activator (tPA), inhaled heparin, hypertonic saline, and dornase alpha.1 During bronchoscopic intervention, our institution has found the endovascular snare to be helpful in large cast removal.
CONCLUSION:
This case of a child presenting with severe acute respiratory failure requiring ECMO due to plastic bronchitis demonstrates the possibility of developing this rare condition despite having no known underlying inflammatory or lymphatic issues. The normal lymphatic anatomy and flow in our patient several weeks after the acute illness suggests a transient lymphatic flow abnormality possibly driven by the acute lower respiratory tract infection with HBoV1. As there are now 4 patients in the literature identified with PB in the setting of HBoV1, it may be beneficial to include HBoV1 in the initial workup of patients with unknown etiology of PB. While routine use of MR lymphangiography is not warranted, we wonder if the procedure might help realize lymphatic flow abnormalities crucial to the pathophysiology if it can be performed safely in the acute setting. The heterogeneous population presents a challenge when studying PB, thus future studies are needed to elucidate the complex pathophysiology, guide management, and better understand prognosis.
FUNDING:
KT is supported by the National Institutes of Health T32 HG009495.
Footnotes
CONFLICTS OF INTERESTS:
The authors have declared no conflicts of interest.
Contributor Information
Cynara Leon, Division of Pulmonary and Sleep Medicine, The Children’s Hospital of Philadelphia, Philadelphia, PA.
Katharine Tsukahara, Division of Pulmonary and Sleep Medicine, The Children’s Hospital of Philadelphia, Philadelphia, PA.
Kaitlyn Boggs, Department of Anesthesiology and Critical Care Medicine, The Children’s Hospital of Philadelphia, Philadelphia, PA.
Pelton Phinizy, Division of Pulmonary and Sleep Medicine, The Children’s Hospital of Philadelphia, Philadelphia, PA.
References
- 1.Li Y, Williams RJ, Dombrowski ND, et al. Current evaluation and management of plastic bronchitis in the pediatric population. Int J Pediatr Otorhinolaryngol 2020;130:109799. DOI: 10.1016/j.ijporl.2019.109799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruegger CM, Bar W, Iseli P. Simultaneous atelectasis in human bocavirus infected monozygotic twins: was it plastic bronchitis? BMC Pediatr 2013;13:209. DOI: 10.1186/1471-2431-13-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeng L, Wei J, Tang Y, Liu E, Li Q, Zang N. Clinical Characteristics of Human Adenovirus Plastic Bronchitis in 10 Pediatric Cases: A Retrospective Study of Seven Years. Virol Sin 2021;36(3):550–554. DOI: 10.1007/s12250-021-00394-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oikawa J, Ogita J, Ishiwada N, et al. Human bocavirus DNA detected in a boy with plastic bronchitis. Pediatr Infect Dis J 2009;28(11):1035–6. DOI: 10.1097/INF.0b013e3181ac4d0d. [DOI] [PubMed] [Google Scholar]
- 5.Ramirez-Suarez KI, Tierradentro-Garcia LO, Smith CL, et al. Dynamic contrast-enhanced magnetic resonance lymphangiography. Pediatr Radiol 2022;52(2):285–294. DOI: 10.1007/s00247-021-05051-6. [DOI] [PubMed] [Google Scholar]


