Abstract
Study Objective:
We sought to identify longitudinal trends in workforce entry and attrition by rural and urban EM physicians, non-EM physicians, and advanced practice providers (APPs).
Methods:
We performed a repeated cross-sectional analysis from 2013 to 2019 of emergency clinicians receiving reimbursement for at least 50 Evaluation & Management (E/M) services [99281–99285] from Medicare Part B within any study year. We calculated the emergency workforce’s entry and attrition annually. Entry was defined as clinicians entering newly or re-entering the workforce, and attrition was defined as clinicians leaving permanently or temporarily. We stratified analyses by rural designation and assessed proportions and state-level changes in clinician density.
Results:
In total, 82,499 unique clinicians performed at least 50 E/M services within any of the 7 study years examined, including 47,000 EM physicians, 9,029 non-EM physicians, and 26,470 APPs. EM physicians made up a decreasing proportion of the workforce (68.1% in 2013; 65.5% in 2019) and APPs made up an increasing proportion of the workforce (20.9% in 2013; 26.1% in 2019). Annually, 5.9–6.8% (2,186 to 2,407) of EM physicians were newly entering and 0.8–1.4% (264 to 515) were re-entering, while 3.8–4.9% permanently left (1,241 to 1,793) and 0.8–1.6% (276 to 521) temporarily left. Additionally, the total proportion of clinicians practicing in rural designations decreased, and APPs separately made up a substantially increasing proportion of the rural workforce (23.0% in 2013; 32.7% in 2019). Substantial state-level variation existed in the supply and demand of EM clinician densities per 100,000 population.
Conclusion:
Annual EM physician attrition was collectively greater than 5% annually, well above the 3% assumed in a recently publicized projection, suggesting a potential overestimation of the anticipated future clinician surplus. Notably, attrition of EM physicians has disproportionately impacted vulnerable rural areas. This work can inform EM workforce decisions regarding residency training, APP utilization, and clinician employment.
Introduction
Background
The number of Emergency Department (ED) visits and emergency clinicians in the United States have historically increased annually and are projected to continue with similar trends in coming years.1 Over the past two decades, emergency medicine (EM) workforce analyses have demonstrated a changing landscape. Studies from the late-1990s noted an impending clinician shortage, resulting in calls for additional EM residency programs and a need for advanced practice providers (APPs), including nurse practitioners (NPs) and physician assistants (PAs), to meet the increasing clinical demand.2–3 Over time, the rapid expansion of the EM workforce has led to APPs currently constituting over one-quarter of the workforce.4 Furthermore, geographic variation has been noted to exist across the EM workforce, with maldistribution present as rural areas lack comparable access to EM physicians.5–9 In a 2018 analysis, EM physicians constituted 63.9% of the urban workforce as compared to 44.8% of the rural workforce.5 More recent workforce projections have identified concerns for a significant EM physician surplus in coming years.1,10
As a knowledge gap, the majority of workforce analyses have historically focused on new entrants and whether residency training figures support future demand without considering growing concerns regarding non-clinical opportunities, financial-based desires, expanding acute on-demand care practices, and burnout leading to EM clinician attrition.7,8,11 A recent study conducted by Marco et al.1 used Medicare claims data crossmatched with the American Medical Association (AMA) Masterfile and mathematical modeling techniques to forecast an oversupply of 7,845 EM physicians by 2030 with an assumed 3% annual clinician attrition rate. Resultantly, this work has generated substantial concern among emergency physicians, particularly current and graduating EM resident physicians.12,13 Substantial flaws in the accuracy of estimated departure from clinical practice have been noted with conventionally used data sources, including the AMA Masterfile,14 suggesting the critical need to utilize data based on real-world practice and patient data.
Importance
Particular attention paid to attrition from the EM workforce is essential due to resignations having increased recently among health care workers.15–17 The most recent analysis specifically investigating workforce attrition was performed over a decade ago, was limited to EM physicians, and employed a cross-sectional one-year design, perhaps providing false reassurance regarding attrition rates.18 Marco et al.’s recent analysis with an assumed 3% annual clinician attrition rate is critically important,1 with less emphasis being placed on the sensitivity analysis showing that if attrition was just 1% higher than assumed, then the estimated surplus would be a more modest 2,486 EM physicians. This acknowledges that there is uncertainty as to what the magnitude of the anticipated surplus might be, and shows the criticality of attrition in predicting future workforce needs. A contemporary and longitudinal investigation of the dynamic nature of entry and attrition among both physicians and APPs will also provide valuable quantitative and actionable information regarding entry and attrition, as clinicians may leave the workforce temporarily and re-enter in subsequent years for personal or professional reasons. Including the examination of entry and attrition across all clinician types, will be consequential in informing decisions regarding residency training, APP utilization, and clinician employment today and in the short-term future.
Performing continued assessments of the EM workforce is also critical to develop policy initiatives and tailor employment hiring strategies to ensure more equitable access to residency-trained and board-certified EM physicians across geographic distributions. Attention to the rural population’s access to care is timely and critical in the setting of numerous recent rural hospital closures and Medicare’s response through the creation of the Rural Emergency Hospital model to encourage and reimburse facilities at a higher rate for increased outpatient services, including around-the-clock emergency care.19–22
Goals of This Investigation
We sought to describe the longitudinal entry and attrition of EM physicians, non-EM physicians, and APPs working in the ED setting between 2013 and 2019. We hypothesized that the assumed “most likely” 3% attrition rate in the recent forecasting study by Marco et al.1 may be underestimated. As secondary objectives, we compared proportions of EM clinicians by rurality and also identified the longitudinal net change in clinician density at the state level.
Methods
Study Design and Dataset
We performed a repeated cross-sectional analysis of emergency clinicians using the CMS 2013–2019 Provider Utilization and Payment Data from the Physician and Other Supplier Public Use File (PUF).23 The 2013 study year reflected the first year of publicly available data, and 2019 was the most up to date at the time of analysis. Because patient identifiers were not used, this study was deemed exempt by the Institutional Review Board. Our study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.24
Used within several prior EM workforce analyses,4,5,25 the PUF provides information on services provided to Medicare beneficiaries by healthcare professionals and is based on CMS administrative claims data. The data are available from the CMS Chronic Condition Data Warehouse (CCW), a database with 100% of Medicare enrollment and fee-for-service claims data. The PUF provides information on all clinicians with active national practitioner identification (NPI) numbers reimbursed greater than 10 times for a specific Evaluation & Management (E/M) service code by the Medicare fee-for-service Part B program. Clinician demographics (name, credentials, gender, address, rurality, entity type) within the PUF are included from the National Plan and Provider Enumeration System (NPPES). The PUF also includes utilization and payment information, beneficiary characteristics, submitted charges organized by NPI, Healthcare Common Procedure Coding System (HCPCS) codes, and place of service (facility or non-facility).
Data Management
All clinicians in the Medicare PUF with addresses registered to the 50 states and Washington D.C were included. Based on Healthcare Common Procedure Coding System (HCPCS) codes 99281 to 99285, included clinicians were required to cumulatively receive ≥50 reimbursements for ED levels 1 to 5 E/M services in any one of the years between 2013 and 2019, similar to Marco et al.1
Consistent with prior work,4,5,25 clinician type (EM physician, non-EM physician, APP) was determined from the ‘Provider Type’ variable, identified from the clinician specialty code reported on the claim received from participating institutions. EM physicians and APPs were first identified, with the APP category inclusive of certified nurse midwives, certified registered nurse anesthetists, nurse practitioners, and physician assistants, consistent with prior work.4 Non-EM physicians were defined as those with another identified medical specialty. Data management decisions and the number of unique clinicians within each specialty across the study years are presented in Supplemental Table 1.
Outcomes
Entry was defined as clinicians entering newly or re-entering the workforce during the study timeframe. For each study year, newly entering clinicians were those not identified within any preceding year in the combined 2013–2019 dataset (e.g. graduating residents). Re-entering clinicians were those that provided services earlier in the 2013–2019 study timeframe, but who were not identified in the immediate preceding year for the study year being analyzed. Attrition was defined as clinicians leaving permanently or temporarily during the study timeframe. Clinicians exhibiting permanent attrition were those not identified within any subsequent year in the 2013–2019 dataset (e.g. retiring clinicians). Clinicians exhibiting temporary attrition were those who provided services later in the 2013–2019 study timeframe, but were not identified in the immediate following year for the study year being analyzed. For example, consider a non-EM physician who performed moonlighting ED services in 2013 and 2014, then focused on building their outpatient clinic setting for 2015–2017, but who then again performed ED services in 2018 and 2019. This clinician would be characterized as having temporarily left the workforce in 2014 and having re-entered the workforce in 2018.
Data Analyses
Clinician numbers were tabulated longitudinally across the EM workforce, including EM physicians, non-EM physicians, and APPs who provided ≥50 ED E/M services during the 2013–2019 study years. We additionally calculated the EM workforce’s entry and attrition annually for each study year.
As a secondary analysis, we then tabulated clinician numbers to assess entry and attrition stratified by clinician rurality. Rurality was defined using the 2010 primary Rural Urban Commuting Area (RUCA) codes based on the address associated with the clinician’s NPI within the NPPES. RUCA codes classify U.S. census tracts using measures of population density, urbanization, and daily commuting. Guided by the United States Department of Agriculture Economic Research Service and prior literature,25–27 we categorized clinicians in metropolitan areas (RUCA code 1–3) as urban and clinicians in micropolitan and non-metropolitan areas (RUCA code 4–10) as rural.
As an additional secondary analysis, we determined the impact of EM workforce entry and attrition on the geographic distribution and density of emergency clinicians by linking the data to the American Community Survey,28,29 which provided state-level population estimates. We used state-level data here given the presence of data suppression if populations for a geographic region were < 65,000. We also believed this level of analysis to be more interpretable and actionable from policy and employment perspectives. Using the number of clinicians in the EM workforce during 2013 and 2019, we determined ‘EM physician density per 100,000 population’ and ‘APP density per 100,000 population’. Between 2013 and 2019, we then determined the ‘% net change’, defined as the percentage increase or decrease of clinician type density per 100,000 population in 2019 relative to 2013. Calculation of these outcomes was intended to further characterize the geographic distribution of clinician supply and demand and changes over time. For example, a highly positive net change in a state with low EM physician density in 2013 would seemingly be a reassuring finding, as EM physicians migrated to states where there was a perceived need for their services. Conversely, a highly positive net change in a state with an already high EM physician density in 2013 would potentially be a concerning finding, as this would suggest EM physicians migrated to states where there was not as strong of a need for their services. We finally calculated the Pearson correlation between EM physician % net change and APP % net change from 2013 to 2019. A positive value would suggest that both EM physicians and APPs are entering or leaving the same states, while a negative value would suggest that EM physicians are leaving states and APPs are entering those same states (or vice versa). Data preparation and analyses were performed in Stata 16 (StataCorp, College Station, TX). We used GraphPad Prism (San Diego, CA), R software (version 4.0.2; R Foundation), and SankeyMATIC for data visualization.
Results
Study Population Trends
During the 2013 to 2019 timeframe, a total of 82,499 unique clinicians provided ≥50 ED levels 1 to 5 E/M services in at least one of the study years. This included 47,000 EM physicians, 9,029 non-EM physicians, and 26,470 APPs. In 2013, there were 48,483 clinicians in the EM workforce, comprised of 68.1% (33,034) EM physicians, 11.0% (5,321) non-EM physicians, and 20.9% (10,128) APPs. By 2019, there were 57,653 clinicians in the EM workforce, comprised of 65.5% (37,766) EM physicians, 8.4% (4,852) non-EM physicians, and 26.1% (15,035) APPs (Figure 1 and Supplemental Table 2). From 2013 to 2019, the number of clinicians in the EM workforce increased by 18.9% for EM physicians, decreased by 8.8% for non-EM physicians, and increased by 48.4% for APPs.
Figure 1.
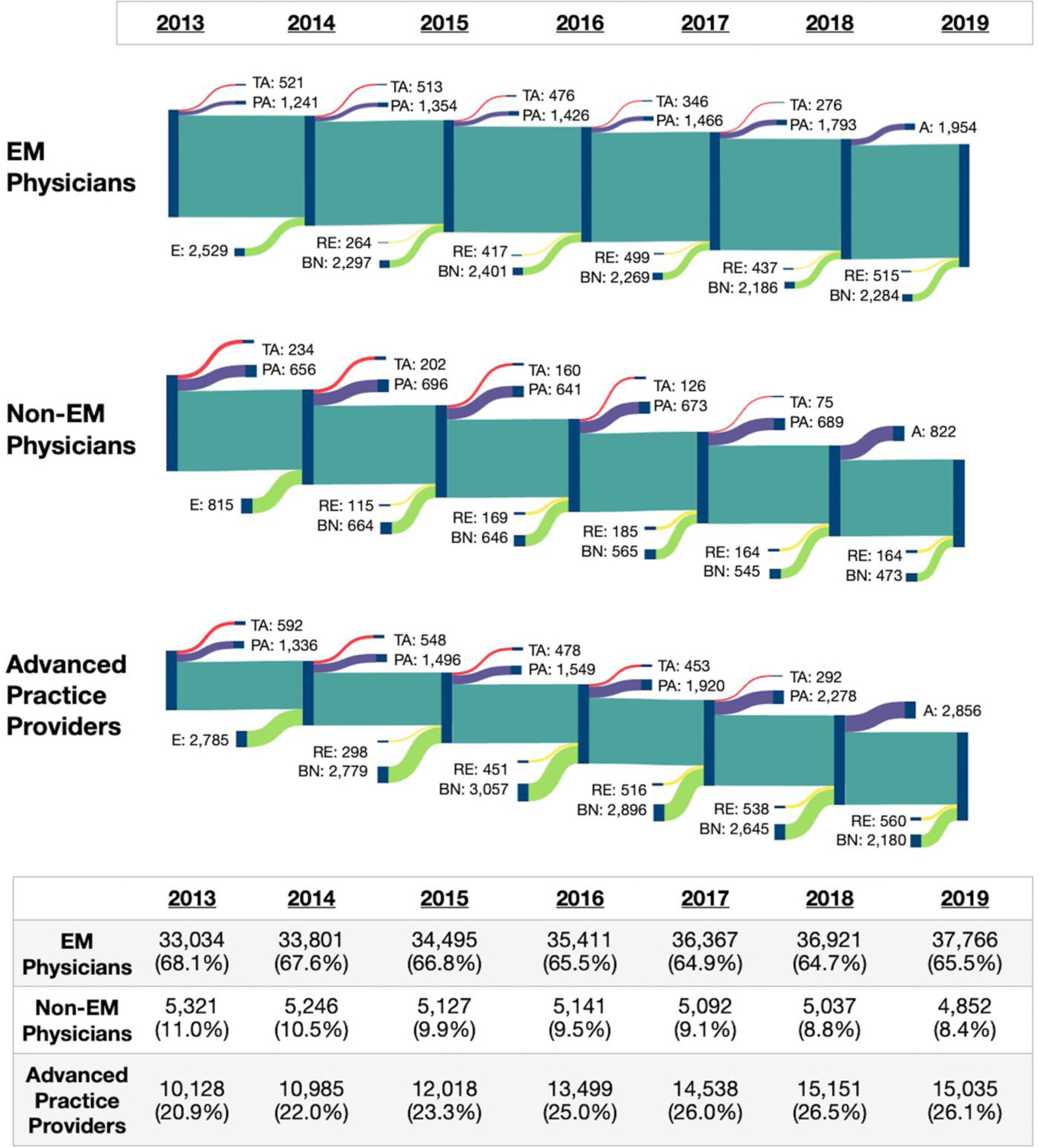
Sankey diagrams of number of clinicians by clinician type entering and leaving the emergency workforce, 2013 to 2019.
Note – Clinicians were included if they performed ≥50 ED levels 1 to 5 E/M services in a study year.
Note – Summed column percentages may not equal exactly 100% due to rounding.
Note – As an example interpretation, in calendar year 2015 there were 34,495 EM physicians, 5,127 non-EM physicians, and 12,018 Advanced Practice Providers that comprised the EM workforce. There were 264 EM physicians, 115 non-EM physicians, and 298 Advanced Practice Providers that re-entered the workforce in 2015, evidenced by the recognition that they were not in the 2014 EM workforce, but were noted in the 2013 EM workforce. There were 2,297 EM physicians, 664 non-EM physicians, and 2,779 Advanced Practice Providers that entered the workforce brand new (for the first time in the study years) in 2015. Subsequently, there were 476 EM physicians, 160 non-EM physicians, and 478 Advanced Practice Providers considered to exhibit temporary attrition, in that they were within the 2015 EM workforce, absent from the 2016 EM workforce, but then again recognized to perform the required number of services in a later study year. There were also 1,426 EM physicians, 641 non-EM physicians, and 1,549 Advanced Practice Providers that exhibited permanent attrition, in that they were within the 2015 EM workforce, but then not recognized in any of the remaining study years.
Abbreviations: A – attrition: includes attrition for the 2018 study year as permanent attrition (PA) or temporary attrition (TA) was not able to be differentiated given that 2019 was the final study year; BN – brand new: clinicians not identified within any preceding year in the dataset (e.g. graduating residents); E – entry: includes entry for the 2014 study year as brand new (BN) or re-entering (RE) was not able to be differentiated given that 2013 was the first study year; PA – permanent attrition: clinicians not identified within any subsequent year in the dataset (e.g. retiring clinicians); RE – re-entering: clinicians not identified within the immediate preceding year, but did provide services in a year earlier in the dataset (e.g. Non-EM physician foregoing ED moonlighting for 2 years due to other priorities, then re-entered the workforce); TA – temporary attrition: clinicians not identified within the immediate subsequent year, but did provide services in a year later in the dataset (e.g. Advanced Practice Provider leaving primary ED practice for another specialty, then performs per diem ED work 3 years later once established in the new specialty.
Main Results
The annual number of clinicians entering the workforce peaked in 2016, while the annual number of clinicians leaving the workforce was continuing to rise as of 2018. The number and proportion of non-EM physicians entering the workforce has steadily decreased during the 2014 to 2019 timeframe. In 2014, 2,529 (7.5%) of the total 33,801 EM physicians were noted to enter the EM workforce, as they were not noted to provide ED services during the 2013 study year. Additionally, 815 (15.5%) of the total 5,246 non-EM physicians and 2,785 (25.4%) of the total 10,985 APPs were noted to enter the 2014 EM workforce. From 2014 to 2019, 7.1–8.0% of practicing EM physicians entered the workforce annually, including 5.9–6.8% newly entering and 0.8–1.4% re-entering. Among practicing non-EM physicians, a collective 13.1–15.9% entered the workforce annually, including 9.7–13.0% newly entering and 2.2–3.6% re-entering. Among practicing APPs, a collective 18.2–26.0% entered the workforce annually, including 14.5–23.0% newly entering and 2.5–3.7% re-entering.
In 2013, 1,762 (5.3%) of the total 33,034 EM physicians left the EM workforce, as they were not noted to provide ED services during the 2014 study year. Additionally, 890 non-EM physicians (16.7%) of the total 5,321 non-EM physicians and 1,928 APPs (19.0%) of the total 10,128 APPs were noted to leave the 2013 EM workforce. From 2013 to 2019, EM physicians exhibited 5.3–5.7% collective annual attrition, including 3.8–4.9% permanent attrition and 0.8–1.6% temporary attrition. Among practicing non-EM physicians, a collective 15.0–16.7% exited the workforce annually, including 12.3–13.5% permanent attrition and 1.5–4.4% temporary attrition. Among practicing APPs, a collective 16.9–19.0% exited the workforce annually, including 12.9–15.7% permanent attrition and 2.0–5.8% temporary attrition.
Secondary Analyses
In 2013, 7,450 (15.4%) EM clinicians practiced in rural designations and the remaining 41,033 (84.6%) practicing in urban designations. Of the 7,450 rural clinicians, 3,820 (51.3%) were EM physicians, 1,915 (25.7%) were non-EM physicians, and 1,715 (23.0%) were APPs (Figure 2). By clinician type, 11.6% of EM physicians, 36.0% of non-EM physicians, and 16.9% of APPs practiced in rural designations in 2013. By 2019, 7,665 (13.3%) EM clinicians practiced in rural designations and the remaining 49,988 (86.7%) practicing in urban designations. Of the 7,665 rural clinicians, 3,555 (46.4%) were EM physicians, 1,602 (20.9%) were non-EM physicians, and 2,508 (32.7%) were APPs. By clinician type, 9.4% of EM physicians, 33.0% of non-EM physicians, and 16.7% of APPs practiced in rural designations in 2019.
Figure 2.
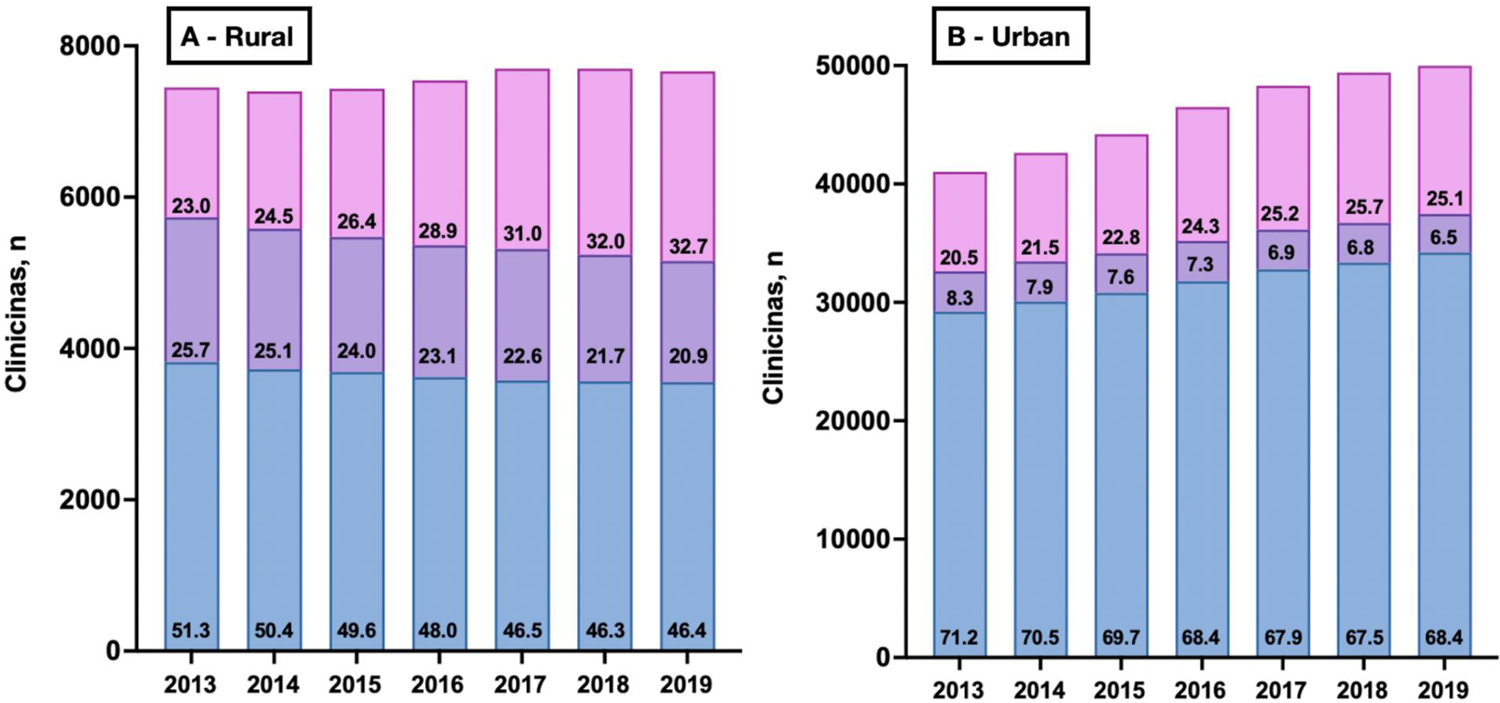
Number of clinicians by clinician type and geographic designation, 2013 to 2019.
Note – Panel A – Rural designation; Panel B – Urban designation. Rurality was determined based on the clinician’s associated Rural Urban Commuting Area (RUCA) codes.
Note – Blue – EM physicians; Purple – non-EM physicians; Pink – Advanced Practice Providers
Note – The numbers listed within the columns represent the proportion (%) that an individual clinician type contributed to all clinicians within that year and rural-urban designation.
In 2014, 922 clinicians were noted to enter the rural EM workforce, including 192 EM physicians. In 2013, 980 clinicians were noted to leave the rural EM workforce, including 294 EM physicians (211 left permanently and 83 left temporarily). For every study year, the number of rural EM physicians leaving the workforce was always greater than the number of rural EM physicians entering the workforce the following year (Supplemental Table 3).
In assessing the geographic distribution of EM clinicians, the three states in 2013 with the highest ‘EM physician density per 100,000 population’ were Washington D.C. (23.0), Michigan (16.5), and Rhode Island (16.4), while the three states with the lowest EM physician density were South Dakota (6.0), Nebraska (6.9), and Montana (7.0). In 2019, the three states with the highest ‘EM physician density per 100,000 population’ were Washington D.C. (24.2), Rhode Island (20.6), and Michigan (19.6), while the three states with the lowest EM physician density were Alabama (7.0), Idaho (7.4), and South Dakota (8.3). From 2013 to 2019, the three states with the highest ‘% net change’ in EM physicians were Montana (+49.8%), South Dakota (+36.7%), and Vermont (+29.6%), while the three states with the lowest ‘% net change’ in EM physicians were Washington (−6.4%), Idaho (−3.2%), and Arkansas (−2.6%) (Figure 3 and Supplemental Table 4).
Figure 3.
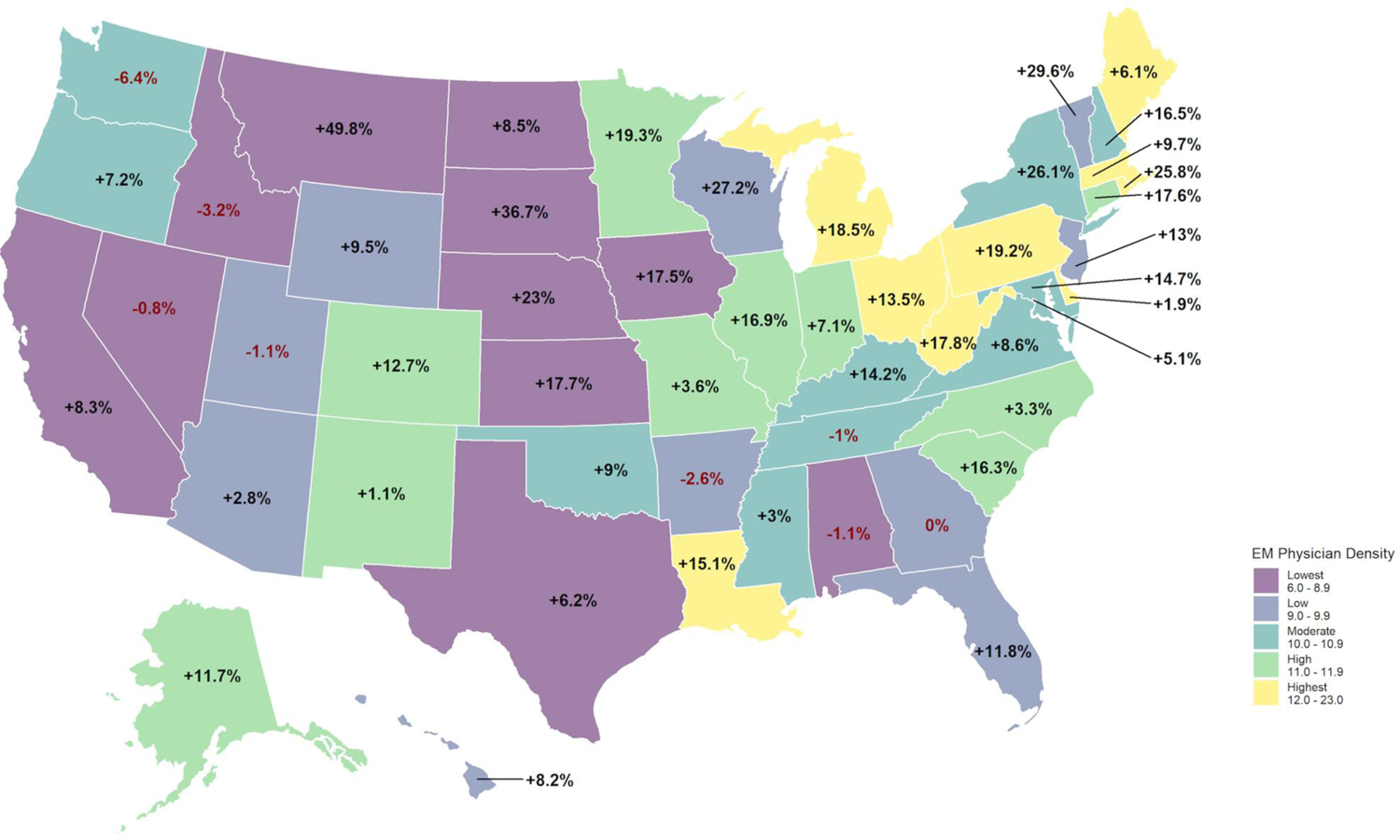
Change in EM physician density per 100,000 population between 2013 and 2019 by state.
Note – Overlaid values are the % net change in EM physician density per 100,000 population experienced from 2013 to 2019. States are divided by color into quintiles based on 2013 physician density.
The three states in 2013 with the highest ‘APP density per 100,000 population’ were Maine (6.5), West Virginia (6.1), and Delaware (6.0), while the three states with the lowest APP density were Hawaii (0.6), Utah (1.0), and Nevada (1.1). In 2019, the three states with the highest ‘APP density per 100,000 population’ were West Virginia (7.9), Kansas (7.1), and Kentucky (6.9), while the three states with the lowest APP density were Hawaii (1.6), Utah (1.7), and North Dakota (2.4). From 2013 to 2019, the three states with the highest ‘% net change’ in APPs were Nevada (+343.9%), Hawaii (+142.4%), and Arkansas (+128.1%), while the three states with the lowest ‘% net change’ in APPs were North Dakota (−10.1%), Maine (−8.1%), and Delaware (+12.0%) (Figure 4 and Supplemental Table 4). The state-level Pearson correlation between EM physician % net change and APP % net change was −0.2188, suggesting that EM physician entry/attrition was inversely associated with APP entry/attrition (Figure 5).
Figure 4.
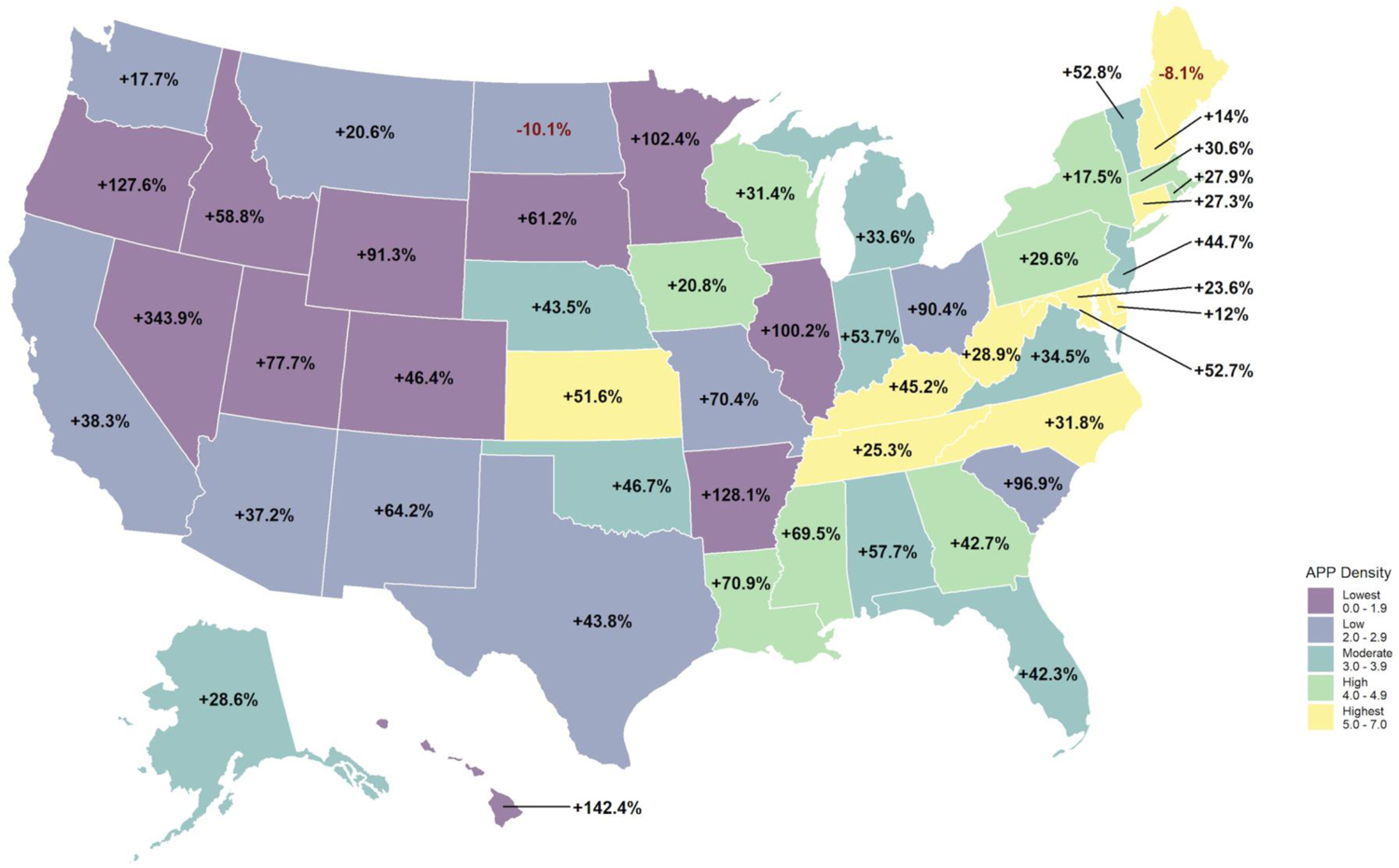
Change in Advanced Practice Provider density per 100,000 population between 2013 and 2019 by state.
Note – Overlaid values are the % net change in Advanced Practice Provider density per 100,000 population experienced from 2013 to 2019. States are divided by color into quintiles based on 2013 Advanced Practice Provider density.
Figure 5.
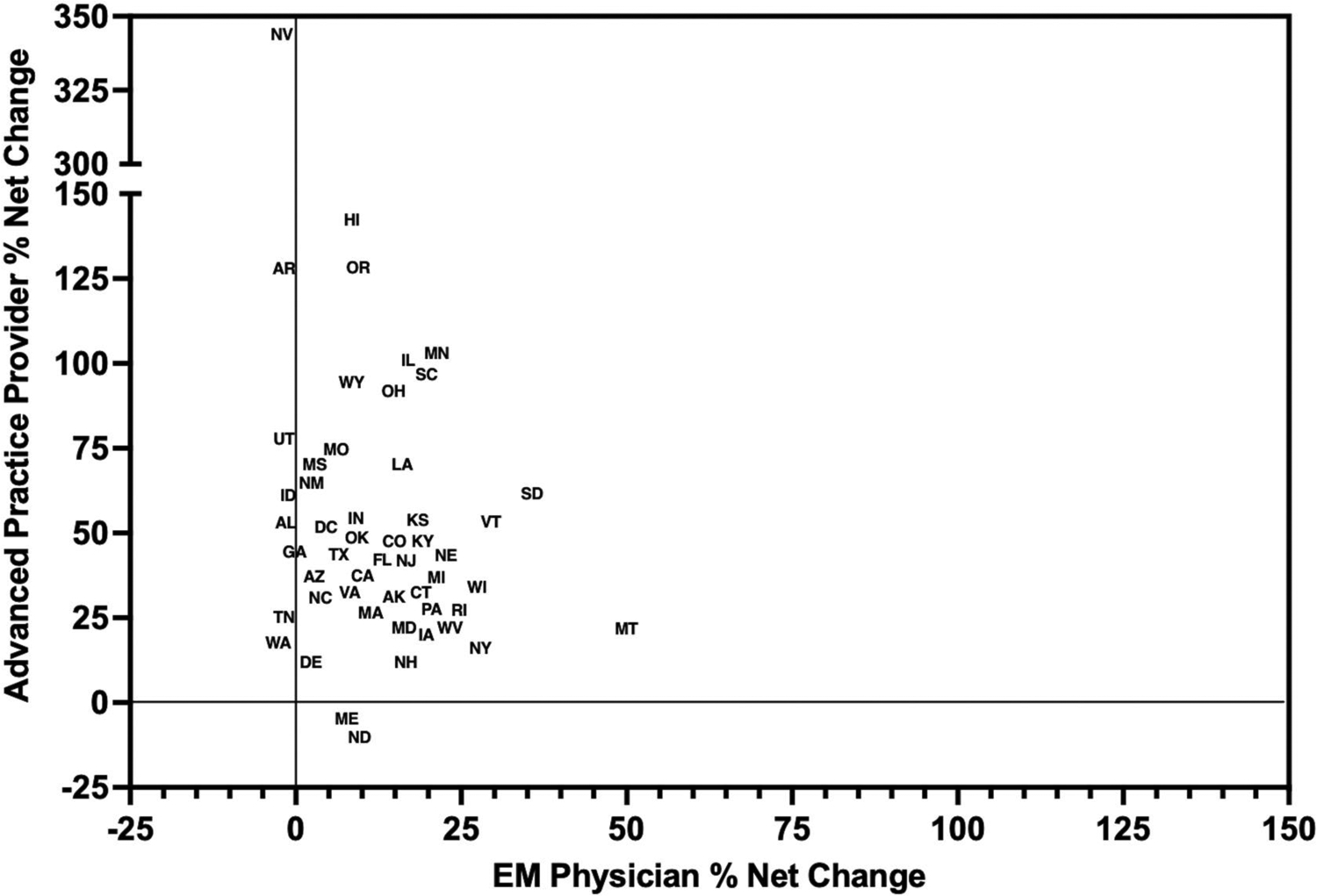
State-level correlation between EM physician and Advanced Practice Provider % net change from 2013 to 2019.
Note – Example: In South Dakota, the EM physician % net change from 2013 to 2019 was 36.7%, while the Advanced Practice Provider % net change was 61.2%.
Note – A small amount of state labels were moved a very limited distance to enhance data visualization and prevent significant overlap. Exact values for each state are present in Supplemental Table 4.
Limitations
As in our previous analyses using the CMS Provider Utilization and Payment Data from the Physician and Other Supplier PUF,4,25 the current study has several potential limitations. First, the PUF data may not be representative of the clinician’s entire practice as it only includes information on Medicare fee-for-service beneficiaries. However, there is unlikely to be a large number of EM clinicians that do not accept Medicare insurance and therefore the risk of systematic bias in our estimates is very low. Second, clinicians were required to perform ≥50 ED levels 1 to 5 E/M services in a study year for inclusion. A lower threshold may include a clinician who performed 40 E/M services in a study year, for example, thereby creating a small risk for misclassification. However, we believe this risk to be very small and impact equally those entering as well as those leaving the workforce. On a related note, critical care E/M services (99291 and 99292) were excluded when defining the clinician population of interest, as the setting associated with these codes may be non-specific and refer to the ED, Intensive Care Unit, or floor level of care. The threshold of ≥50 ED levels 1 to 5 and exclusion of critical care E/M services are consistent with recent and comparable work.1 Third, national practitioner identification (NPI) data have limitations. For example, a clinician working within the Indian Health Service may have a license from any state, and the address associated with the NPI may be inaccurate. This limitation may categorize a very small proportion of rural-practicing physicians as urban physicians. Fourth, in the potential case of physicians identified as belonging to multiple specialties, the PUF reports the specialty for which the clinician billed the largest number of services that year. CMS’s approach to this possibility is not expected to systematically redistribute clinicians in a biased fashion, thereby maintaining our findings. Fifth, as in any repeated cross-sectional analysis, we were limited by the study years included. Therefore, definitions of brand new, re-entering, permanent attrition, and temporary attrition are dependent on the start and stop end dates of the available study time period. To mitigate this risk, we used all available study years publicly available from CMS.23 Finally, care provided and services billed for by APPs may be underreported as these PUFs only capture APP services in which no attending physician supervision was present to sufficiently meet physician billing requirements. Therefore, estimates of APP proportion within the EM workforce are likely conservative.
Discussion
In our analysis of a nationwide 2013 to 2019 Medicare reimbursement dataset, we identified 82,499 unique clinicians who provided ≥50 ED levels 1 to 5 E/M services in a study year. This is the first longitudinal EM analysis assessing workforce entry and exit across all clinician types and geographic designations. There are five key findings from our analysis. First, APPs make up an increasing proportion of the workforce, rising from 20.9% in 2013 to 26.1% in 2019, while the proportion of EM physicians within the workforce more subtly decreased from 68.1% to 65.5% over the same time period. Second, EM clinician entry to the workforce peaked in 2016, while clinician exit from the workforce was still rising as of 2018. Third, approximately, 5.3–5.7% of EM physicians were noted to leave the workforce annually, this included approximately 3.8–4.9% annually exhibiting permanent attrition and an additional 0.8–1.6% exhibiting temporary attrition, collectively greater than the assumed 3% attrition rate deemed most likely by Marco et al.1 Fourth, EM physicians comprise less than half of the rural EM workforce, initially representing 51.3% in 2013 and decreasing to 46.4% of all clinicians serving rural designations in 2019. Conversely, APPs market share has increased from representing 23.0% of rural clinicians in 2013 to 32.7% in 2019. Fifth, substantial state-level variation exists in the supply and demand of EM clinician densities per 100,000 population during the 2013 to 2019 time period. These findings provide critical descriptive data, which can inform decisions regarding residency training, APP utilization, and clinician employment today.
Our work builds upon the literature in a number of ways, primarily by providing a unique longitudinal and individual level analysis of entry and exit from the EM clinician workforce. This work identifies that approximately one-fifth of the annual APP EM workforce is brand new, with a similar portion leaving the workforce annually either permanently or temporarily. Many personal and professional factors, including burnout, high acuity, unpredictable practice environment, and mental stress, may play a role in the attrition rates seen among all clinician types, including EM physicians.18,30–36 Furthermore, while the Marco et al. study did take into account attrition and presented a sensitivity analysis of predictions based on variance in this and other assumptions,1 the inability to account for permanent and temporary attrition of both physicians and APPs may have resulted in error in projections. With EM physician annual attrition estimates identified to be greater than the assumed 3% attrition rate as the most likely scenario in the Marco et al. study,1 we propose that the workforce’s future for current and graduating EM residents may not be as bleak as anticipated if identified contemporary trends continue.
While we identified that an increasing annual number of EM physicians are leaving the workforce, we conversely did not identify the same for EM physicians entering the workforce. In our analysis, EM physicians entering the workforce peaked in 2016, which is consistent with the previously identified dramatic increase in new EM residency programs and trainee positions during the early-mid 2010s, many offered by for-profit hospitals and large, corporate, medical groups.37–39 However, despite the increase in residency positions, the number of medical school graduates matching into EM has plateaued. The most recent 2022 cycle data from the Electronic Residency Application Service even suggests that the entering pipeline may be diminishing, as the number of EM residency applicants decreased 17% (the largest decrease among all specialties) and the number of unfilled residency positions rose from 14 to 219 compared to the 2021 application season.40,41 Therefore, we anticipate that the combination of increased attrition and decreased entry will reduce the magnitude of the expected 2030 surplus. However, immediate attention must be paid to mitigate the underlying stressors that may prompt premature clinician attrition or prevent medical school students pursuing the specialty of EM. Our study includes data from 2013 to 2019, which is prior to the COVID-19 pandemic. Given reports of clinicians increasingly leaving the workforce during the COVID-19 pandemic,16,17 repeat analyses should be performed to support workforce surveillance efforts and optimize the dynamically changing workforce needs.
Our findings also have substantial implications for the practice of EM in rural designations. APPs have had a significant proportional increase as a component within the EM workforce, but rural clinicians providing emergency care in 2019 are now more likely to be a non-EM physician or an APP rather than an EM physician. Our work uniquely identifies a concerning trend regarding the recruitment of rural EM physicians. From 2013 to 2019, the number of EM physicians entering the rural workforce never offset the number leaving from the prior year, suggesting that shortages and inequities in access will persist unless substantial efforts are made to address EM physician recruitment and retention issues. Priority areas outlined to date have included increasing rural EM residency programs, enhancing opportunities and partnerships with urban academic medical centers, addressing prohibitive guidelines and requirements from the Residency Review Committee for EM (RRC-EM), expanding dual EM/family medicine programs, and creating financial or loan repayment incentives for clinicians to practice rural EM.42–47 One potential contributing factor to the finding of increased APP presence in rural designations may be the increased use of telemedicine within critical access hospitals and rural EDs. A 2013 memorandum from CMS clarified that a telemedicine physician could fulfill the regulatory requirements for physician backup when APPs staff critical access hospital EDs primarily, resulting in several EDs implementing this practice in subsequent years.48,49
Our work identified that largely rural states such as Montana and South Dakota were in the lowest quartile for 2013 EM physician density, and reassuringly had substantial increases in EM physician density by the 2019 study year. However, this work also uncovered persistent maldistribution as several other rural states (e.g. North Dakota) in the lowest quartile for EM physician density did not see a substantial increase by 2019, while several states such as Rhode Island saw a 25.8% increase in % net change despite already being in the highest quartile in 2013. We believe these state-level findings can be informative for policy implementation and targeting hiring strategies to incentivize EM physicians to practice in rural areas with lower access to care.
In summary, APPs have made up an increasing proportion of the EM workforce from 2013 to 2019, particularly within rural designations. Approximately 5.3–5.7% of EM physicians were noted to leave the workforce annually, including those with permanent and temporary attrition, collectively greater than assumptions used within recent projection studies. Substantial state-level variation exists in the supply and demand of EM and APP clinician density during the 2013 to 2019 time period. These findings can help inform EM workforce decisions regarding residency training, APP utilization, and clinician employment.
Supplementary Material
Grant/Financial Support:
Dr. Gettel is a Pepper Scholar with support from the Claude D. Pepper Older Americans Independence Center at Yale School of Medicine (P30AG021342), the National Institute on Aging (NIA) of the National Institutes of Health (NIH; R03AG073988), the Society for Academic Emergency Medicine Foundation, and the Emergency Medicine Foundation. Dr. Venkatesh is supported in part by the American Board of Emergency Medicine National Academy of Medicine Anniversary fellowship and the Yale Center for Clinical Investigation grant KL2 TR000140 from the National Center for Advancing Translational Science (NCATS/NIH). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meetings:
This work has been accepted for presentation at the 2022 Society for Academic Emergency Medicine (SAEM) national meeting, as well as the 2022 SAEM New England regional meeting.
Declaration of Conflicting Interests: The authors declare that there are no conflicts of interest.
References
- 1.Marco CA, Courtney DM, Ling LJ, et al. The emergency medicine physician workforce: projections for 2030. Ann Emerg Med. 2021;78(6):726–737. [DOI] [PubMed] [Google Scholar]
- 2.Macy J Jr. The role of emergency medicine in the future of American medical care. Ann Emerg Med. 1995;25(2):230–233. [DOI] [PubMed] [Google Scholar]
- 3.Holliman CJ, Wuerz RC, Chapaman DM, et al. Workforce projections for emergency medicine: how many emergency physicians does the United States need? Acad Emerg Med. 1997;4(7):725–730. [DOI] [PubMed] [Google Scholar]
- 4.Gettel CJ, Canavan ME, D’Onofrio G, et al. Who provides what care? An analysis of clinical focus among the national emergency care workforce. Am J Emerg Med. 2021;42:228–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall MK, Burns K, Carius M, et al. State of the national emergency department workforce: who provides care where? Ann Emerg Med. 2018;72(3):302–307. [DOI] [PubMed] [Google Scholar]
- 6.Barreto T, Jetty A, Eden AR, et al. Distribution of physician specialties by rurality. J Rural Health. 2021;37(4):714–722. [DOI] [PubMed] [Google Scholar]
- 7.Clay CE, Sullivan AF, Bennett CL, et al. Supply and demand of emergency medicine board-certified emergency physicians by U.S. state, 2017. Acad Emerg Med. 2021;28(1):98–106. [DOI] [PubMed] [Google Scholar]
- 8.Bennett CL, Sullivan AF, Ginde AA, et al. National study of the emergency physician workforce, 2020. Ann Emerg Med. 2020;76(6):695–708. [DOI] [PubMed] [Google Scholar]
- 9.Ginde AA, Rao M, Simon EL, et al. Regionalization of emergency care future directions and research: workforce issues. Acad Emerg Med. 2010;17(12):1286–1296. [DOI] [PubMed] [Google Scholar]
- 10.Reiter M, Allen BW. The emergency medicine workforce: shortage resolving, future surplus expected. J Emerg Med. 2020;58(2):198–202. [DOI] [PubMed] [Google Scholar]
- 11.Ginde AA, Sullivan AF, Camargo CA. National study of the emergency physician workforce, 2008. Ann Emerg Med. 2009;54(3):349–359. [DOI] [PubMed] [Google Scholar]
- 12.ACEPNow. Emergency physicians explore the future of the emergency medicine workforce. Available at: https://www.acepnow.com/article/emergency-physiciansexplore-the-future-of-the-emergency-medicine-workforce/. Accessed February 14, 2022.
- 13.AAEM Resident & Student Association. An Open Letter to the Specialty of Emergency Medicine. Available at: https://www.aaemrsa.org/UserFiles/file/FINAL_Official_AnOpenLettertotheSpecialtyofEmergencyMedicine.pdf. Accessed February 14, 2022.
- 14.Rittenhouse DR, Mertz E, Keane D, et al. No exit: an evaluation of measures of physician attrition. Health Serv Res. 2004;39(5):1571–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harvard Business Review. Who is driving the Great Resignation? Available at: https://hbr.org/2021/09/who-is-driving-the-great-resignation. Accessed February 16, 2022.
- 16.Sinsky CA, Brown RL, Stillman MJ, et al. COVID-related stress and work intentions in a sample of US health care workers. Mayo Clin Proc Innov Qual Outcomes. 2021;5(6):1165–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Atlantic. Why health-care workers are quitting in droves. Available at: https://www.theatlantic.com/health/archive/2021/11/the-mass-exodus-ofamericas-health-care-workers/620713/. Accessed February 2, 2022.
- 18.Ginde AA, Sullivan AF, Camargo CA. Attrition from emergency medicine clinical practice in the United States. Ann Emerg Med. 2010;56(2):66–71. [DOI] [PubMed] [Google Scholar]
- 19.Venkatesh AK, Janke A, Rothenberg C, et al. National trends in emergency department closures, mergers, and utilization, 2005–2015. PLoS One. 2021;16(5):e0251729. Doi: 10.1371/journal.pone.0251729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.University of North Carolina – The Cecil G. Sheps Center for Health Services Research. Rural Hospital Closures. Available at: https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/closures/. Accessed February 16, 2022.
- 21.Nikpay S, Tschautscher C, Scott NL, et al. Association of hospital closures with changes in Medicare-covered ambulance trips among rural emergency medical services agencies. Acad Emerg Med. 2021;28(9):1070–1072. [DOI] [PubMed] [Google Scholar]
- 22.National Advisory Committee on Rural Health and Human Services. Rural Emergency Hospital – Policy Brief and Recommendations to the Secretary. Available at: https://www.hrsa.gov/sites/default/files/hrsa/advisorycommittees/rural/publications/2021-rural-emergency-hospital-policy-brief.pdf. Accessed February 16, 2022.
- 23.Centers for Medicare & Medicaid Services. Medicare Physician & Other Practitioners – by Provider and Service. Available at: https://data.cms.gov/provider-summary-by-type-of-service/medicare-physicianother-practitioners/medicare-physician-other-practitioners-by-provider-andservice. Accessed January 3, 2022.
- 24.Von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–577. [DOI] [PubMed] [Google Scholar]
- 25.Gettel CJ, Canavan ME, Greenwood-Ericksen MB, et al. A cross-sectional analysis of high-acuity professional services performed by urban and rural emergency care physicians across the United States. Ann Emerg Med. 2021;78(1):140–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.United States Department of Agriculture – Economic Research Service. Rural-Urban Commuting Area Codes. Available at: https://www.ers.usda.gov/dataproducts/rural-urban-commuting-area-codes/. Accessed January 27, 2022.
- 27.WWAMI RUCA Rural Health Research Center. RUCA Data. Available at: https://depts.washington.edu/uwruca/ruca-uses.php. Accessed January 27, 2022.
- 28.United States Census Bureau. 2019 American Community Survey Single-Year Estimates. Available at: https://www.census.gov/newsroom/press-kits/2020/acs-1year.html. Accessed January 28, 2022.
- 29.United States Census Bureau. 2013 American Community Survey Single-Year Estimates. Available at: https://www.census.gov/newsroom/presskits/2014/20140918_acs1yr2013.html. Accessed January 28, 2022.
- 30.Seitz R, Robertson J, Moran TP, et al. Emergency medicine nurse practitioner and physician assistant burnout, perceived stress, and utilization of wellness resources during 2020 in a large urban medical center. Adv Emerg Nurs J. 2022;44(1):63–73. [DOI] [PubMed] [Google Scholar]
- 31.Lall MD, Chang BP, Park J, et al. Are emergency physicians satisfied? An analysis of operational/organization factors. J Am Coll Emerg Physicians Open. 2021;2(6):e12546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lall MD, Perman SM, Garg N, et al. Intention to leave emergency medicine: mid-career women are at increased risk. West J Emerg Med. 2020;21(5):1131–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holmes JL. Sustaining a long career in emergency medicine: issues for emergency physicians of all ages. Emerg Med Australas. 2019;31(6):1112–1114. [DOI] [PubMed] [Google Scholar]
- 34.Wu YF, Wang PC, Chen YC. Gender differences and work-family conflicts among emergency physicians with intention to leave. Emerg Med Int. 2018:3919147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuhn G, Goldberg R, Compton S. Tolerance for uncertainty, burnout, and satisfaction with the career of emergency medicine. Ann Emerg Med. 2009;54(1):106–113. [DOI] [PubMed] [Google Scholar]
- 36.Cydulka R, Korte R. Career satisfaction in emergency medicine: the ABEM Longitudinal Study of Emergency Physicians. Ann Emerg Med. 2008;51(6):714–722. [DOI] [PubMed] [Google Scholar]
- 37.Haas MRC, Hopson LR, Zink BJ. Too big too fast? Potential implications of the rapid increase in emergency medicine residency positions. AEM Educ Train. 2019;4(Suppl 1):S13–S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.National Resident Matching Program. Advance Data Tables – 2021 Main Residency Match. Available at: https://www.nrmp.org/wpcontent/uploads/2021/08/Advance-Data-Tables-2021_Final.pdf. Accessed February 17, 2022.
- 39.Emergency Medicine News. After the Match: Corporations rush in to fill MD shortage. Available at: https://journals.lww.com/emnews/Fulltext/2017/01000/After_the_Match__Corporations_Rush_In_to_Fill_MD.3.aspx. Accessed February 17, 2022.
- 40.Association of American Medical Colleges. ERAS Statistics. Available at: https://www.aamc.org/data-reports/interactive-data/eras-statistics-data. Accessed February 17, 2022.
- 41.American College of Emergency Physicians. Joint statement on the 2022 Emergency Medicine residency match. Available at: https://www.acep.org/news/acep-newsroom-articles/joint-statement-match-2022/. Accessed April 11, 2022.
- 42.Handel DA, Hedges JR, SAEM IOM Task Force. Improving rural access to emergency physicians. Acad Emerg Med. 2007;14(6):562–565. [DOI] [PubMed] [Google Scholar]
- 43.Patterson DG, Preparing physicians for rural practice: availability of rural-training in rural-centric residency programs. J Grad Med Educ. 2019;11(5):550–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Peterson LE, Dodoo M, Bennett KJ, et al. Nonemergency medicine-trained physician coverage in rural emergency departments. J Rural Health. 2008;24(2):183–188. [DOI] [PubMed] [Google Scholar]
- 45.Talley BE, Moore SA, Camargo CA, et al. Availability and potential effect of rural rotations in emergency medicine residency programs. Acad Emerg Med. 2011;18(3):297–300. [DOI] [PubMed] [Google Scholar]
- 46.Wadman MC, Clark TR, Kupas DF, et al. Rural clinical experiences for emergency medicine residents: a curriculum template. Acad Emerg Med. 2012;19(11):1287–1293. [DOI] [PubMed] [Google Scholar]
- 47.Casaletto JJ, Wadman MC, Ankel FK, et al. Emergency medicine rural rotations: a program director’s guide. Ann Emerg Med. 2013;61(5):578–583. [DOI] [PubMed] [Google Scholar]
- 48.Ward MM, Merchant KAS, Carter KD, et al. Use of telemedicine for ED physician coverage in critical access hospitals increased after CMS policy clarification. Health Aff (Millwood). 2018;37(12):2037–2044. [DOI] [PubMed] [Google Scholar]
- 49.Center for Clinical Standards and Quality/Survey & Certification Group. Critical Access Hospital (CAH) emergency services and telemedicine: implications for emergency services Condition of Participation (CoPs) and Emergency Medical Treatment and Labor Act (EMTALA) on-call compliance. Available at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-13-38.pdf. Accessed April 11, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


