Abstract
Introduction
Cervical disc replacement (CDR) surgery is well established for the treatment of disc degeneration from C3-C7, but there is little data regarding the safety and efficacy of CDR at the cervicothoracic junction, C7-T1. CDR is an appealing option, in terms of range of motion preservation, symptom relief, and absence of risk for nonunion. Currently, C7-T1 CDR is not approved by the Food and Drug Administration, and the existing literature is limited to two case reports that describe the results of a combined two patients. This series explores whether C7-T1 CDR is a reasonable treatment and alternative to fusion.
Methods
We present a case series of seven consecutive patients who underwent CDR at C7-T1 by a single surgeon from January to December of 2019. There were five females and two males with an average age of 61.3 ± 6.4 years.
Results
Average follow up was 18.9 ± 2.5 months. The average postoperative NDI score was 22.6 % ± 14.0. We also recorded qualitative data regarding patient satisfaction and revision surgery status. There was one complication of disc subsidence following three months of complete pain resolution. The six other patients reported being very satisfied with their surgical outcome.
Conclusion
These seven cases dramatically increase the volume of data in the literature on clinical outcomes and patient satisfaction following CDR at the cervicothoracic junction. Additionally, the heterogeneity of cases shows the effectiveness of this treatment in many real-world cases. A greater volume of cases with longer follow up will be necessary to better establish long-term clinical success.
Keywords: Cervical disc replacement, Spine surgery
Highlights
-
•
Cervical disc replacement as an emerging treatment option for preserving motion
-
•
Seven patients with pathology at C7-T1 successfully received disc replacement.
-
•
All resolved symptoms, measured by NDI and survey of patient satisfaction
-
•
CDR as viable treatment option at the cervicothoracic junction
1. Introduction
C7-T1 pathology often presents as neck pain, radiating arm pain to digits 4 and 5, along with numbness, tingling, and weakness [1]. These symptoms arise from the compression of the C8 nerve root, which exits the foramen at the cervicothoracic junction [2]. Spinal cord compression at C7-T1 causing myleopathic symptoms can also occur, but is less common. Sources of spinal cord and nerve root compression at C7-T1 include disc degeneration, bulging discs, spinal stenosis, osteophyte formation, and disc herniation [3].
Anterior cervical decompression and fusion (ACDF) is an effective treatment for many patients with pathology at C7-T1 [1], [2], [4], [5], [6]. There is little data regarding the results of cervical disc replacement (CDR) at the cervicothoracic junction.
Multiple studies on the subaxial cervical spine have shown CDR to have similar or superior outcomes in comparison to ACDF, in terms of preserved range of motion, recovery time, adjacent segment degeneration, and need for future surgery [7], [8], [9]. An extensive literature search yielded only two case reports describing C7-T1 disc replacement in one patient each [11], [12].
The purpose of this study is to present a consecutive case series of patients with a spectrum of pathology that underwent C7-T1 CDR by a single surgeon. This series has been reported in line with the PROCESS 2020 guideline [13].
2. Methods
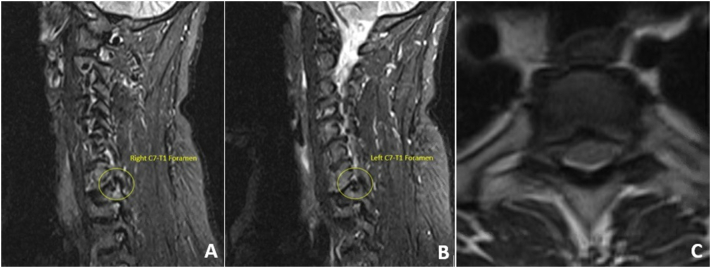
This case series includes seven consecutive patients who underwent cervical disc replacement at C7-T1 by the senior author between January and December of 2019. The group consists of five females and two males with an average age of 61.3 ± 6.4 years at the time of surgery. Of the seven patients, five had a previous ACDF, four of which involved the C6–7 level, and two had no prior neck surgery. All of the patients presented in clinic with radicular symptoms consistent with C8 nerve root compression due to degenerative changes. No patients had signs or symptoms of myelopathy. Three of the seven patients experienced concurrent significant symptoms arising from stenosis at the C5–6(1) and C6–7(3) levels. Diagnosis of the symptomatic level was established by clinical symptoms with concordant examination findings and radiographic evidence of stenosis on MRI. Fig. 1 contains sagittal and axial views of one patient's preoperative MRI, showing severe foraminal stenosis at C7-T1. After conservative treatment options, including injections, medication, and physical therapy failed to resolve their symptoms, a C7-T1 decompression and disc replacement was recommended. All patients received the Prestige LP implant (Medtronic, Dublin). Two patients also received a C6–7 CDR and one patient received concurrent CDRs at C6–7 and C5–6. One of the patients with prior C6–7 ACDF had a nonunion that was treated with a conversion to a CDR under the same anesthetic.
Fig. 1.
Preoperative MRI showing (A) a sagittal view of the right foraminal stenosis at C7-T1, (B) a sagittal view of the left foraminal stenosis at C7-T1, and (C) an axial view of the C7-T1 disc.
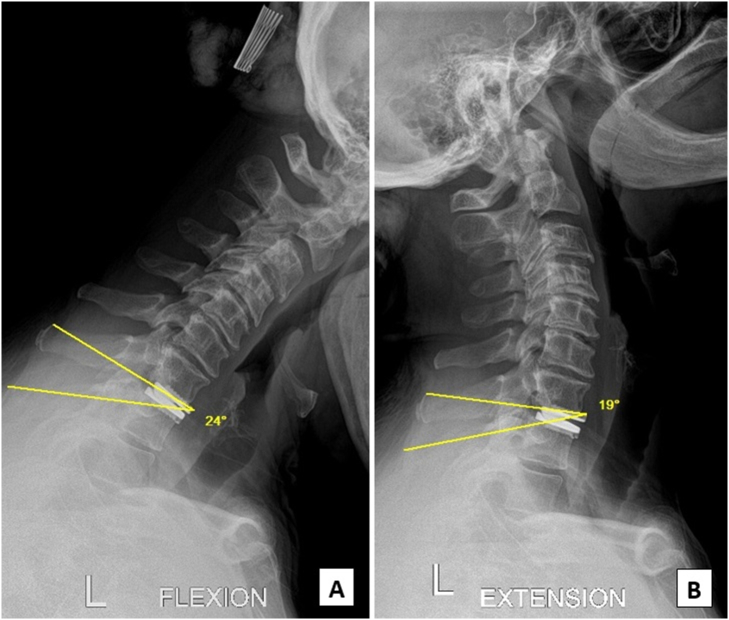
The C7-T1 disc space was approached through a left sided transverse skin incision within a prominent skin crease in the lower neck, as per the surgeon's standard practice. The traditional dissection described by Smith-Robinson provided access to the cervicothoracic junction in all cases [14]. Self-retaining retractors were placed beneath the longus coli muscles bilaterally to protect adjacent structures. A complete discectomy, resection of the PLL and foraminotomy were performed in all cases. The endplates were carefully preserved. The implant size that best approximated the patient's disc space dimensions was selected and inserted. In all cases a Medtronic Prestige LP implant was used, based on surgeon preference. Fig. 2 shows postoperative flexion and extension X-ray images in the same patient from Fig. 1. In no case was there excessive bleeding and in no case was a drain used. Research registry number was obtained for this series [UIN: researchregistry8009].
Fig. 2.
Anteroposterior projection cervical radiograph: Postoperative flexion (A) and extension (B) x-ray images demonstrate a well-placed implant and 5 degrees of motion at the cervicothoracic junction, 2 years out from surgery, in the same patient from Fig. 1.
3. Results
With average follow-up of 18.9 ± 2.5 months, ranging from 17 to 23 months, we obtained new Neck Disability Index (NDI) scores and surveyed the patients regarding satisfaction and revision status. The NDI scores showed one patient with no disability, five with mild disability, and two with moderate disability. The average NDI score was 22.6 % ± 14.0. None of the patients have undergone further neck surgery. Excluding the patient whose implant subsided, the other six patients report being very satisfied with the surgery and say they would highly recommend this operation to someone else with the same issue.
There were no intraoperative or immediate postoperative complications, and all patients reported meaningful improvement following surgery. There was only one postoperative complication three months out from surgery. The patient had been completely pain free for three months when he woke up one morning with recurrent cervical radiculitis causing radiating pain down the left arm. A CT scan was obtained and confirmed that the implant had subsided into the superior endplate of T1. The patient had no history of osteopenia/osteoporosis. The patient was counseled on the options of living with symptoms versus a repeat epidural steroid injection versus an additional surgery involving C7-T1 posterior arthrodesis. The patient chose to live with symptoms for the time being.
4. Discussion
The C7-T1 level has unique anatomic and mechanical factors relative to the subaxial cervical spine. Serving as the transition from the cervical spine to the more rigid thoracic spine, the cervicothoracic junction has less flexibility than the cervical spine. There are no uncovertebral joints present at C7-T1, making lateral disc herniations more likely [2]. C7-T1 disc herniations account for 3.5–8 % of all cervical disc herniations [1]. Due to anatomic constraints, the C7-T1 disc may not be accessible via a traditional anterior approach for a subset of patients with caudally oriented discs, high riding T1 ribs or an especially thick soft tissue envelope. Further, the proximity of thoracic structures such as the thoracic duct, the pleura, the thymus gland, brachiocephalic trunk and the arch of the aorta place these structures at increased risk with a C7-T1 surgical approach [4]. Despite these potential issues, Mostofi et al. conducted a study on the differences between the posterior and anterior fusion approaches in 21 patients with C7-T1 disc herniations and found no significant differences between the outcomes for each group [1].
Cervical disc replacement at C7-T1 has theoretic appeal due to its preservation of motion, avoidance of nonunion risk, reduction of stress on adjacent levels and the prospect for improved patient outcomes relative to arthrodesis [7], [8], [9]. Contraindications for cervical disc replacement include underlying instability, spondyloarthropathies, poor bone quality, and infection [3].
In 2005, Sekhon detailed the case of a 25-year-old woman with a history of C5–6 and C6–7 ACDF who presented with degeneration of C4–5 and C7-T1 [11]. In order to preserve range of motion in the young patient, they proceeded with C4–5 and C7-T1 CDR. There were no complications, and at the 10-month follow-up there was maintained range of motion and no reoccurrence of pain. A report from Australia in 2016 presented the case of a 43-year-old man who underwent a hybrid surgery consisting of ACDF at C5–6 and CDR at C7-T1 [12]. All of his preoperative symptoms were resolved by the 3 month follow up. At the 2 year follow up, there was no reoccurrence of symptoms. Outside of these reports, a few C7-T1 disc replacements have been included in larger studies on cervical disc replacement devices [10]. However, they do not include level specific data or discussion to add to the literature on C7-T1 disc replacements.
This case series adds greatly to the current literature on C7-T1 CDR by expanding the number and diversity of cases. All seven patients reported meaningful improvement in their symptoms following surgery. There were no intraoperative complications, and only one patient experienced a postoperative complication of subsidence three months after surgery. There is no established rate of subsidence at C7-T1, but subsidence is not unique to the cervicothoracic junction. The rate of clinically significant subsidence is disputed; however large studies report it as less than 3 % [15]. Despite this unfortunate complication, the patient's NDI score 18 months out from surgery was 38 %, significantly improved from the preoperative score of 72 %. Fig. 1, Fig. 2 demonstrate pre- and post-operative images of one of the seven patients two years after a primary C7-T1 CDR.
Our average NDI of 22.6 % approximately 1.5 years out from surgery is similar to the average NDI following 2-level CDR and ACDF at other levels of the cervical spine, as reported in a 10-year IDE follow-up study of the Prestige LP implant [16]. For the CDR group, Gornet et. Al reported an average NDI score of 15.7 % at year 1 and 15.0 % at year 2. The average NDI for the ACDF group at these time points was 20.6 % and 20.0 %. The IDE study included 148 CDR patients and 118 ACDF patients, who did not differ significantly in terms of preoperative condition, previous surgery, medication usage, and symptom duration. This series of seven patients represents an especially challenging cohort due to many requiring multi-level procedures and or revision surgery. It is expected, therefore, that this cohort might have a higher mean postoperative NDI than a less complex collection of patients. Our group of seven patients includes one primary single level CDR, one primary 3 level CDR, three single level CDRs adjacent to a previous fusion, and two 2 level CDRs adjacent to a previous fusion.
As four of the seven patients had previous C6-C7 fusions, we thought this unique solution of a CDR rather than an extension of fusion to the level below would significantly help preserve the range of motion at the cervicothoracic junction, as well as prevent further degeneration at the adjacent levels.
The similar results of this series of seven patients to that of other published ACDF series provide evidence that C7-T1 CDR is an effective treatment for a variety of real-world cases involving symptomatic degenerative C7-T1 pathology.
5. Conclusion
The current series provide promising results for the viability of cervical disc replacement as a treatment for various pathologies at the cervicothoracic junction. To the authors' knowledge, this case series is the largest reported collection of data regarding C7-T1 cervical disc replacements. The preliminary results of this study warrants further research with longer follow up and more patients to show the long-term clinical outcomes.
Funding
The authors received no funding in the creation of this manuscript.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Sarah Leonard: Data Collection, Investigation, Formal analysis, Writing-Original Draft Hyun Song: Data Collection, Investigation, Writing – Review & Editing, Formal analysis Charles Edwards II: Conceptualization, Methodology, Supervision, Project administration, Writing – Reviewing & Editing.
Ethical approval
This case report is exempt from ethical approval by the Mercy Medical Center IRB.
Consent
Each patient consented to the use of their data and treatment course for publication.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Sarah E. Leonard, B.S.
-Data Collection
-Writing the manuscript
-Critical revision of the manuscript
Hyun Song, B.A.
-Analysis and interpretation of data
-Data Analysis
-Writing the manuscript
-Critical revision of the manuscript
Charles C. Edwards II, M.D.
-Study concept and design
-Data collection
-Critical revision of the manuscript
-Supervision and expertise
Registration of research studies
-
1.
Name of the registry: Research Registry
-
2.
Unique identifying number or registration ID: researchregistry8009
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-the-registry#user-researchregistry/registerresearchdetails/62a954e967b709001e669505/
Guarantor
Hyun Song, B.A.
Charles C. Edwards II, M.D.
Declaration of competing interest
There are no conflicts of interest.
The authors do not have any proprietary interests in the materials described in this article.
References
- 1.Mostofi K., Peyravi M., Moghadam B.G. Cervicothoracic junction disc herniation: our experience, technical remarks, and outcome. J. Craniovertebral Junct. Spine. 2020;11(1):22–25. doi: 10.4103/jcvjs.JCVJS_102_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Post N., Cooper P., Frempong-Boadu A., Costa M.E. Unique features of herniated discs at the cervicothoracic junction: clinical presentation, imaging, operative management, and outcome after anterior decompressive operation in 10 patients. Neurosurgery. 2006;58(3) doi: 10.1227/01.NEU.0000197118.86658.A6. 497-50. [DOI] [PubMed] [Google Scholar]
- 3.Leven D., Meaike J., Radcliff K., Qureshi S. Cervical disc replacement surgery: indications, technique, and technical pearls. Curr. Rev. Musculoskelet. Med. 2017;10(2):160–169. doi: 10.1007/s12178-017-9398-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Donnarumma P., Nigro L., Tarantino R., De Giacomo T., Delfini R. The manubriotomy is a safe option for the anterior approach to the cervico-thoracic junction. J. Spine Surg. 2017;3(3):426–428. doi: 10.21037/jss.2017.06.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee J.G., Kim H.S., Ju C.I., Kim S.W. Clinical features of herniated disc at cervicothoracic junction level treated by anterior approach. Kor. J. Spine. 2016;13(2):53–56. doi: 10.14245/kjs.2016.13.2.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Falavigna A., Righesso O., Betemps A., de los Rios PF Vela, Guimarães R., Ziegler M. Surgical planning and neurological outcome after anterior approach to remove a disc herniation at the C7–T1 level in 19 patients. Spine. 2014;39(3) doi: 10.1097/BRS.0000000000000109. E219-E225. [DOI] [PubMed] [Google Scholar]
- 7.Safili C., et al. Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine J. 2018;18(6):1022–1029. doi: 10.1016/j.spinee.2017.10.072. [DOI] [PubMed] [Google Scholar]
- 8.Laratta J.L., Shillingford J.N., Saifi C., Riew K.D. Cervical disc arthroplasty: a comprehensive review of single-level, multilevel, and hybrid procedures. Glob. Spine J. 2018;8(1):78–83. doi: 10.1177/2192568217701095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Badhiwala J.H., Platt A., Witiw C.D., Traynelis V.C. Cervical disc arthroplasty versus anterior cervical discectomy and fusion: a meta-analysis of rates of adjacent-level surgery to 7-year follow-up. J. Spine Surg. 2020;6(1):217–232. doi: 10.21037/jss.2019.12.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pimenta L., McAfee P.C., Cappuccino A., Bellera F.P., Link H.D. Clinical experience with the new artificial cervical PCM (Cervitech) disc. Spine J. 2004;4(6):315S–321S. doi: 10.1016/j.spinee.2004.07.024. [DOI] [PubMed] [Google Scholar]
- 11.Sekhon L. Cervicothoracic junction arthroplasty after previous fusion surgery for adjacent segment degeneration: case report. Neurosurgery. 2005;56(1) doi: 10.1227/01.neu.0000144173.35366.55. [DOI] [PubMed] [Google Scholar]
- 12.Yang Y., Litai M., Shan W., Ying H., Hao L. Two-year follow-up results of artificial disc replacement C7–T1. Int. J. Clin. Exp. Med. 2016;9(4) 4748-4653. [Google Scholar]
- 13.Agha R.A., Sohrabi C., Mathew G., Franchi T., Kerwan A., O'Neill N., PROCESS Group The PROCESS 2020 guideline: updating consensus Preferred Reporting Of Case Series in Surgery (PROCESS) guidelines. Int. J. Surg. 2020 Dec;84:231–235. doi: 10.1016/j.ijsu.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Smith G.W., Robinson R.A. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J. Bone Joint Surg. Am. 1958;40-A(3):607–624. [PubMed] [Google Scholar]
- 15.Parish J.M., Asher A.M., Coric D. Complications and complication avoidance with cervical total disc replacement. Int. J. Spine Surg. 2020;14(s2):S50–S56. doi: 10.14444/7091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gornet M.F., Lanman T.H., Burkus J.K., et al. Two-level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10-year outcomes of a prospective, randomized investigational device exemption clinical trial. J. Neurosurg. Spine. 2019;31(4):508–518. doi: 10.3171/2019.4.SPINE19157. [DOI] [PubMed] [Google Scholar]