Abstract
Background and Aims
The ongoing public health emergency has created incredible fear of getting the infection and a terrible psychological burden among all levels. The pandemic has severely affected private job holders' economic status and lifestyle factors in Bangladesh. Here we aimed to assess fear and depressive symptoms among private job holders in Bangladesh during the Covid‐19 pandemic and associated risk factors.
Methods
We conducted this online cross‐sectional survey between January 15, 2021, and March 15, 2021, among 510 private job holders aged above 18 years. We followed the convenience sampling method for data collection. We assessed sociodemographic factors and two psychometric parameters. We applied the Fear of Covid‐19 Scale and Patient Health Questionnaire‐9 to assess increased fear and depressive symptoms, respectively. Chi‐square test, independent sample t‐test, and binary logistic regression analysis were performed for data analysis.
Results
The prevalence of increased fear and depressive symptoms were 86.27% and 42.16%, respectively. Factors associated with increased fear among private job holders during COVID‐19 were economic class, obesity, on‐time salary, company's downsizing policy, salary reduction, home office, and transportation facilities. However, depressive symptoms were associated with marital status, education level, residence area, the organizational practice of health safety rules, company performance, on‐time salary, health insurance, downsizing, salary reduction policy, organization type, transportation, and mental health support at work. The present study also noticed some interrelations among the above factors with mental health issues.
Conclusion
Based on the present findings, we recommend actionable items to improve the mental health of private job holders in Bangladesh due to the ongoing pandemic. Authorities can develop mental health support programs and efficient Covid‐19 response systems. The policymakers and regulatory bodies might take some initiatives to promote mental health in the private sector in Bangladesh.
Keywords: Covid‐19, depressive symptoms, fear, mental health, private job, public health
1. BACKGROUND
It is now more than one and half years since the world health organization (WHO) declared the Covid‐19 as a global pandemic. 1 The healthcare systems around the globe are fighting critical challenges associated with this disease. 2 , 3 , 4 We have observed the tremendous impact on the mental health of people in Asian countries due to the effects of Covid‐19 that are reflected in different studies. 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 A study measured anxiety and depressive symptoms among healthcare professionals from India, China, Malaysia, and other south Asian countries. 13 The results showed that 36.5% of participants reported anxiety symptoms, 29.5% showed depressive symptoms, and 23.5% had both anxiety and depressive symptoms. 13 According to a study in Iran, 18.5% of people have experienced severe anxiety. 14 Another study from Nepal reported that 38% of the healthcare professionals had at least one psychiatric illness. Among them, 37.3% had an anxiety disorder. 15 Bangladeshi population experiencing social discrimination, suicidal ideation, and social stigma amid the Covid‐19 pandemic. 16 Psychological problems such as fear, anxiety, depressive symptoms, and suicidal ideation have become challenges connected with Covid‐19. 17 We conducted a recent study among the general population of Bangladesh where we observed the prevalence of depressive symptoms, anxiety, loneliness, and sleep problems were 38%, 64%, 71%, and 73%, respectively. 18 People worry about their safety, vaccination, and other consequences such as fear of job security, layoff, and being stuck to the same designation. 19 , 20 , 21 However, Mamun et al. reported a wide range of risk factors for this increased level of depressive symptoms and associated symptoms like suicidal ideation. They mentioned demographic factors, lifestyle‐related factors, and pre‐existing stressors related to personal and job life. 22 Moreover, a recent review identified several economic, psychological, and demographic factors for poor mental health during the ongoing Covid‐19 pandemic. 23 Also, another study revealed that inappropriate use of social media contributes to the poor mental health of the young population in Bangladesh amid the Covid‐19 pandemic. 24
However, the situation is worse in Bangladesh than in developed countries. 25 , 26 , 27 , 28 In a recent nationwide study, a group of researchers found that a large portion of their Bangladeshi respondents reported stress, anxiety, and depressive symptoms with a high prevalence, about 61%, 87%, and 64%, respectively. 29 Fear about careers amid the Covid‐19 pandemic has become a common situation in Bangladesh. Tertiary‐level students who are preparing themselves for jobs are more anxious about the shrinking of the job market. Extended exposure to fear leads to depressive symptoms and anxiety. 30 In addition to the scarcity of new jobs, many private job holders are fighting more with economic shrinking and job insecurity‐related stress than actual Covid‐19 fear. Several studies reported that the prevalence of suicides is more in Bangladesh than the actual deaths due to Covid‐19. Surprisingly, 49% of suicide victims were 20–35 years old. 31 , 32 The new viral strains, subsequent pandemic waves, additional restrictions, and countermeasures might potentially be contributed to the worsening the mental health condition across the world. 33 , 34 , 35 , 36 , 37 , 38 , 39
The private sector of Bangladesh has become quite large, and they are contributing a significant portion of Bangladesh's economy. According to the Bangladesh Bureau of Statistics (BBS), the major establishments in the Bangladesh economy are nongovernment, and a significant number of economic activities are conducted by public–private funded partnerships. 40 , 41 However, the outbreak of Covid‐19 suddenly changed the whole situation. 42 , 43 Approximately, 68% of the people working in the private sector in two major cities (Dhaka and Chittagong) have lost their jobs. In Dhaka city, the rate was 76% whereas, it was 59% in Chittagong city. In both cities, around 80% of earners and 94% of business owners reported a dramatic fall in income due to Covid‐19‐related responses. In poor areas of these cities, about 8 out of 10 adults were suffering from stress and anxiety. 44 , 45 In Bangladesh, many sectors such as manufacturing, agriculture, transport, and construction have been impacted temporarily or permanently due to the ongoing pandemic. 46 The banking sector experienced a very negative impact due to the Covid‐19 pandemic. In six Bangladeshi private banks, more than 3000 employees have resigned. Among them, a significant number of employees reported facing layoffs. 47 Also, the information and communications technology (ICT) sector of Bangladesh is facing significant economic and human resource shrinkage due to the pandemic crisis. Global software orders to Bangladeshi ICT farms has been declined about 70%–80% during the Covid‐19 surge. 48 Companies cannot pay their monthly wages on due time. Therefore, employees had to rely on savings, government, and other external helps for livelihood. People who live on their daily income become one of the worst victims of this loss of income.
However, another group of victims is education employees and students. Many news media have reported a significant dropout of students around the country. At the same time, child labor and child marriage have increased. 49 , 50 However, some experts say it happened due to an elevation of poverty and economic shrinkage related to the job loss of their parents amid a pandemic. 51 , 52 We noticed many schools have permanently closed. And the people working there had lost their jobs. So, many people switched their professions in Bangladesh due to the Covid‐19 pandemic. 53 The ready‐made garment sector in Bangladesh entirely depends on the demand of global fashion companies. The global fashion companies canceled their orders due to the Covid‐19 pandemic. 54 At the same time, the decreased circular of new jobs across the industries depressed the job applicant amid the Covid‐19 pandemic. 55 There might have a set of interconnected factors that would impact the mental health of people working in private sectors in Bangladesh. Therefore, we attempted to assess fear and depressive symptoms levels among private job holders and contributing factors during the Covid‐19 pandemic in Bangladesh.
2. METHODS
2.1. Study participants
We performed this online cross‐sectional survey between January 15, 2021, and March 15, 2021. Our assumed confidence interval (CI), expected response rate, and expected precision were 95%, 25%, and 5%, respectively, to achieve 80% statistical power. Therefore, we required 384 responses from the private job holders. We circulated our study questionnaire to 1600 individuals, and initially, we collected 563 responses. The actual response rate was 35%. After careful evaluation, we left out 53 replies due to incomplete or partial information. Finally, we analyzed 510 complete responses in this study. We followed several exclusion and inclusion criteria to include participants in this study. We collected self‐reporting responses from the invited individuals who have been working in the private sector of Bangladesh, aging above 18 years. The Committee for Advanced Studies at the Department of Pharmacy, University of Asia Pacific approved this study protocol (No. UAP/Pharm/2021/01003). We obtained informed consent from all participants for their participation in this study. We performed this web‐based survey following the checklist for reporting results of internet e‐surveys (CHERRIES) statements.
2.2. Data collection procedure
Face‐to‐face interviews were not feasible during the Covid‐19 pandemic. Therefore, we used Google Forms for data collection. The structured questionnaire link was circulated online through social networking sites such as Facebook, Linked In, Twitter, WhatsApp, Telegram, Messenger, and email. We also tried to obtain a snowball sampling technique to share the link among the potential respondents. There was an option to submit a single response by an account. We conducted a pilot study among a small group of population to confirm a better understanding of the questionnaire. We presented both the original English version and translated the Bengali version for better clarification of the entire questionnaire. Also, we arranged video conferences or phone calls on case to case basis for their clarification about the questionnaire.
2.3. Demographic and job‐related estimations
We collected necessary sociodemographic information from the study participants. This information includes age, sex, education level, economic impression, marital status, living status, and smoking habit. We collected job‐related information such as organization type, availability of mental healthcare support, transportation, home office facility, salary change, job security, timely salary payment, health insurance, payment during leave (Covid‐19 related), the performance of the organization, and organizational responses against Covid‐19.
2.4. Psychometric estimations
Fear of Covid‐19 Scale (FCV‐19S) was first introduced and validated by Ahorsu and collaborators. It has been widely used to determine fear related to Covid‐19. FCV‐19S consists of seven items. Each question rating from strongly disagree (1), disagree (2), neutral (3), agree (4), and strongly agree (5). The possible minimum total score is seven, and the maximum total score is 35. A validated version of the FCV‐19S is also available in the Bengali language. 56 A higher total score resembles greater fear due to the Covid‐19. 57
The Patient Health Questionnaire‐9 (PHQ‐9) is a checklist consisting of nine questions. The scoring of each question ranges from zero to three based on the responses. Each question has four options ranging from not at all (0), several days (1), more than half the days (2), and nearly every day (3). The highest possible score on the PHQ‐9 scale is 27, and the lowest possible score is 0. We can split the total score into four levels: below 10, no depressive symptoms; 10–15, mild depressive symptoms; 16–21, moderate depressive symptoms; and 22–27, severe depressive symptoms. 58
2.5. Statistical analysis
We applied two tools for data analysis. After data collection, we performed data processing using Microsoft Excel 2016. Then we used IBM SPSS version 25.0 for data analysis. Here, we performed a χ 2 test, independent sample t‐test, and regression analysis. We performed a descriptive statistical analysis to characterize the demographic profiles. We selected independent variables for the adjusted model according to their variability and correlation with the dependent variables. We included confounders to keep the statistical results valid. A p‐value of less than or equal to 0.05 is considered significant.
3. RESULTS
3.1. General description of study population
We presented the sociodemographic profile of the study population in Table 1. A total of 510 participants gave their feedback in this survey. Among the respondents, female and male were 36.47% and 63.53%, respectively. The prevalence of obesity was 38.04%, and only 4.51% were chronic energy deficiency (CED). The majority of the participants were from 18 to 30 years of age (62.75). Among them, 86.08% had a graduate or above education. Among the respondents, 53.33% were married. We observed more than three‐quarters (78.43%) of the respondents living in urban areas. Also, two‐thirds of respondents (61.96%) of the participants were nonsmokers. Moreover, participants with high, middle, and low economic status were 20.00%, 3.35%, and 47.65%, respectively.
Table 1.
Distribution of sociodemographic variables and their association with elevated fear and depressive symptoms among the private job holders during Covid‐19 pandemic
| Sociodemographic parameters | Total (N = 510) | Elevated fear (N = 440) | Depressive symptoms (N = 215) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | χ 2 | df | p Value | n | % | χ 2 | df | p Value | |
| Age in years | ||||||||||||
| 25–35 | 320 | 62.75 | 269 | 84.06 | 4.105 | 3 | 0.250 | 141 | 44.06 | 1.910 | 3 | 0.591 |
| 36–45 | 159 | 31.18 | 142 | 89.31 | 60 | 37.74 | ||||||
| 46–60 | 31 | 6.07 | 29 | 93.55 | 14 | 45.16 | ||||||
| Sex | ||||||||||||
| Female | 186 | 36.47 | 154 | 82.80 | 2.992 | 1 | 0.084 | 85 | 45.70 | 1.506 | 1 | 0.220 |
| Male | 324 | 63.53 | 286 | 88.27 | 130 | 40.12 | ||||||
| BMI (kg/m2) | ||||||||||||
| 18.5–25 (normal) | 293 | 57.45 | 261 | 89.08 | 6.170 | 2 | 0.046 | 128 | 43.69 | 0.781 | 2 | 0.677 |
| Above 25 (obese) | 194 | 38.04 | 162 | 83.51 | 77 | 39.69 | ||||||
| Below 18.5 (CED) | 23 | 4.51 | 17 | 73.91 | 10 | 43.48 | ||||||
| Marital status | ||||||||||||
| Divorced | 28 | 5.49 | 24 | 85.71 | 2.787 | 3 | 0.426 | 16 | 57.14 | 15.617 | 3 | 0.001 |
| Married | 272 | 53.33 | 241 | 88.60 | 93 | 34.19 | ||||||
| Unmarried | 204 | 40.00 | 170 | 83.33 | 103 | 50.49 | ||||||
| Widow | 6 | 1.18 | 5 | 83.33 | 3 | 50.00 | ||||||
| Education level | ||||||||||||
| Graduate and above | 439 | 86.08 | 383 | 87.24 | 4.370 | 2 | 0.112 | 167 | 38.04 | 24.221 | 2 | <0.001 |
| Primary | 5 | 0.98 | 3 | 60.00 | 5 | 100.00 | ||||||
| Secondary | 66 | 12.94 | 54 | 81.82 | 43 | 65.15 | ||||||
| Economic impression | ||||||||||||
| High | 102 | 20.00 | 79 | 77.45 | 8.724 | 2 | 0.013 | 45 | 44.12 | 2.102 | 2 | 0.350 |
| Middle | 165 | 32.35 | 144 | 87.27 | 62 | 37.58 | ||||||
| Low | 243 | 47.65 | 217 | 89.30 | 108 | 44.44 | ||||||
| Residence area | ||||||||||||
| Rural | 110 | 21.57 | 96 | 87.27 | 0.118 | 1 | 0.731 | 62 | 56.36 | 11.608 | 1 | 0.001 |
| Urban | 400 | 78.43 | 344 | 86.00 | 153 | 38.25 | ||||||
| Living status | ||||||||||||
| With family | 372 | 72.94 | 323 | 86.83 | 0.356 | 1 | 0.551 | 158 | 42.47 | 0.056 | 1 | 0.812 |
| Without family | 138 | 27.06 | 117 | 84.78 | 57 | 41.30 | ||||||
| Smoking habit | ||||||||||||
| Nonsmoker | 316 | 61.96 | 269 | 85.13 | 0.924 | 1 | 0.336 | 125 | 39.56 | 2.303 | 1 | 0.129 |
| Smoker | 194 | 38.04 | 171 | 88.14 | 90 | 46.39 | ||||||
Note: p‐values are significant at 95% confidence interval (p < 0.05). Significant p‐values are shown in bold.
Abbreviations: BMI, body mass index; CED, chronic energy deficiency; Covid‐19, coronavirus disease 2019; N, number.
3.2. Description of the job‐related factors
We presented the job‐related factors in Table 2. Among the respondents, participants from healthcare and nonhealthcare were 29.02% and 70.98%, respectively. Only 25.29% of the respondents acknowledged that they worked from home during this Covid‐19 pandemic. According to the present findings, 59.61% of organizations fully maintained health safety rules, 50.20% always used thermal scanning at their entry point, 75.88% always kept hand sanitizer or hand washing facilities, and 66.47% of employees always used facemask at the workplace. Moreover, 74.12% of respondents used public transportation during the COVID‐19 pandemic. About three‐fourths (72.16%) of the respondents reported that their office did not arrange Covid‐19 testing facilities. However, 90.39% of participants acknowledged that quarantine or isolation was mandatory for all when suspected or infected by a coronavirus. In 81.76% of cases, the organizations have granted and paid for their Covid‐19‐related leave. According to the present findings, only 43.14% of private employers provide health insurance in Bangladesh. Among the respondents, 49.22% reported that their organizations reduced employees during the Covid‐19 pandemic. However, 54.12% of respondents got mental healthcare support from the organization. Also, 68.43% of the respondents reported that they got an on‐time salary, and 39.41% of respondents got a reduced payment during the ongoing pandemic.
Table 2.
Distribution of profession‐related variables and their association with elevated fear and depressive symptoms among the private job holders during Covid‐19 pandemic
| Job‐related factors | Total (N = 510) | Elevated fear (N = 440) | Depressive symptoms (N = 215) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | χ 2 | df | p Value | n | % | χ 2 | df | p Value | |
| Organization maintains health safety rules | ||||||||||||
| Fully | 304 | 59.61 | 266 | 87.50 | 2.631 | 2 | 0.268 | 91 | 29.93 | 46.110 | 2 | <0.001 |
| Not at all | 20 | 3.92 | 15 | 75.00 | 12 | 60.00 | ||||||
| Partially | 186 | 36.47 | 159 | 85.48 | 112 | 60.22 | ||||||
| Thermal scanning before entry | ||||||||||||
| Always | 256 | 50.20 | 219 | 85.55 | 0.799 | 2 | 0.671 | 93 | 36.33 | 7.659 | 2 | 0.022 |
| Not at all | 115 | 22.55 | 98 | 85.22 | 58 | 50.43 | ||||||
| Sometimes | 139 | 27.25 | 123 | 88.49 | 64 | 46.04 | ||||||
| Hand sanitizer or hand washing facilities at work | ||||||||||||
| Always | 387 | 75.88 | 338 | 87.34 | 4.656 | 2 | 0.098 | 135 | 34.88 | 35.558 | 2 | <0.001 |
| Not at all | 16 | 3.14 | 11 | 68.75 | 12 | 75.00 | ||||||
| Sometimes | 107 | 20.98 | 91 | 85.05 | 68 | 63.55 | ||||||
| Everyone wears a mask at the workplace | ||||||||||||
| Always | 339 | 66.47 | 295 | 87.02 | 0.663 | 2 | 0.718 | 104 | 30.68 | 58.321 | 2 | <0.001 |
| Not at all | 16 | 3.14 | 13 | 81.25 | 14 | 87.50 | ||||||
| Sometimes | 155 | 30.39 | 132 | 85.16 | 97 | 62.58 | ||||||
| Availability of Covid‐19 testing support from the office | ||||||||||||
| No | 368 | 72.16 | 322 | 87.50 | 1.676 | 1 | 0.195 | 163 | 44.29 | 2.474 | 1 | 0.116 |
| Yes | 142 | 27.84 | 118 | 83.10 | 52 | 36.62 | ||||||
| Quarantine or isolation is mandatory for Covid‐19 positive cases | ||||||||||||
| No | 49 | 9.61 | 40 | 81.63 | 0.986 | 1 | 0.321 | 37 | 75.51 | 24.730 | 1 | <0.001 |
| Yes | 461 | 90.39 | 400 | 86.77 | 178 | 38.61 | ||||||
| Organization is performing like previous | ||||||||||||
| No | 265 | 51.96 | 233 | 87.92 | 1.268 | 1 | 0.260 | 125 | 47.17 | 5.685 | 1 | 0.017 |
| Yes | 245 | 48.04 | 207 | 84.49 | 90 | 36.73 | ||||||
| Organization pays during Covid‐19‐related leave | ||||||||||||
| No | 93 | 18.24 | 78 | 83.87 | 0.555 | 1 | 0.456 | 55 | 59.14 | 13.453 | 1 | <0.001 |
| Yes | 417 | 81.76 | 362 | 86.81 | 160 | 38.37 | ||||||
| Employer provides health insurance | ||||||||||||
| No | 290 | 56.86 | 250 | 86.21 | 0.003 | 1 | 0.959 | 144 | 49.66 | 15.501 | 1 | <0.001 |
| Yes | 220 | 43.14 | 190 | 86.36 | 71 | 32.27 | ||||||
| Getting on‐time salary during Covid‐19 pandemic | ||||||||||||
| No | 161 | 31.57 | 146 | 90.68 | 3.862 | 1 | 0.049 | 92 | 57.14 | 21.668 | 1 | <0.001 |
| Yes | 349 | 68.43 | 294 | 84.24 | 123 | 35.24 | ||||||
| Anybody has lost their job from your organization | ||||||||||||
| No | 259 | 50.78 | 211 | 81.47 | 10.271 | 1 | 0.001 | 85 | 32.82 | 18.820 | 1 | <0.001 |
| Yes | 251 | 49.22 | 229 | 91.24 | 130 | 51.79 | ||||||
| Organization has reduced salary during the pandemic | ||||||||||||
| No | 309 | 60.59 | 259 | 83.82 | 3.993 | 1 | 0.046 | 103 | 33.33 | 25.032 | 1 | <0.001 |
| Yes | 201 | 39.41 | 181 | 90.05 | 112 | 55.72 | ||||||
| Work from home is allowable | ||||||||||||
| Always | 129 | 25.29 | 99 | 76.74 | 13.747 | 2 | 0.001 | 50 | 38.76 | 2.269 | 2 | 0.322 |
| Not at all | 175 | 34.31 | 159 | 90.86 | 70 | 40.00 | ||||||
| Sometimes | 206 | 40.39 | 182 | 88.35 | 95 | 46.12 | ||||||
| Organization type | ||||||||||||
| Healthcare | 148 | 29.02 | 124 | 83.78 | 1.092 | 1 | 0.296 | 44 | 29.73 | 13.205 | 1 | <0.001 |
| Nonhealthcare | 362 | 70.98 | 316 | 87.29 | 171 | 47.24 | ||||||
| Transportation used during Covid‐19 pandemic | ||||||||||||
| Private | 132 | 25.88 | 105 | 79.55 | 8.605 | 2 | 0.014 | 53 | 40.15 | 9.894 | 2 | 0.007 |
| Public | 378 | 74.12 | 335 | 88.62 | 162 | 42.85 | ||||||
| Availability of mental healthcare support at work | ||||||||||||
| No | 234 | 45.88 | 201 | 85.90 | 0.052 | 1 | 0.820 | 135 | 57.69 | 42.796 | 1 | <0.001 |
| Yes | 276 | 54.12 | 239 | 86.59 | 80 | 28.99 | ||||||
Note: p‐values are significant at 95% confidence interval (p < 0.05). Significant p‐values are shown in bold.
Abbreviations: Covid‐19, coronavirus disease 2019; N, number.
3.3. Psychometric evaluation of fear and depressive symptoms
The estimations of elevated fear and depressive symptoms were 86.27% (mild: 31.96%, moderate: 38.04%, severe: 16.27%) and 42.16% (mild: 24.71%, moderate: 12.75%, severe: 4.70%), respectively (Figure 1). Prevalence of elevated fear was associated with (1) sociodemographic factors: (a) economic impression low versus high (89.30% vs. 77.45%, p = 0.013), and less significantly, (b) sex: male versus female (88.27% vs. 82.80%, p = 0.084); at the same time, we found (2) job‐related factors: (a) work from home is not available versus always available (90.86% vs. 76.74%, p = 0.001), (b) anybody has lost their jobs vs. not lost (91.24% vs. 81.47%, p = 0.001), (c) transportation public versus private (91.11% vs. 79.55%, p = 0.014), (d) salary reduction during pandemic versus salary not reduced (90.05% vs. 83.82%, p = 0.046), (e) not getting salary on time versus getting salary on time (90.68% vs. 84.24%, p = 0.049), and less significantly, (f) always having sanitizer or hand washing facility in workplace versus not having that facility (87.34% vs. 68.75%, p = 0.098).
Figure 1.
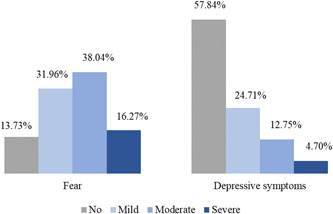
Prevalence and severity of elevated fear and depressive symptoms among private job holders in Bangladesh during the Covid‐19 pandemic.
Prevalence of depressive symptoms was associated with the demographic variables such as (i) marital status divorced versus married (57.14% vs. 34.19%, p = 0.001), (ii) education level primary versus graduate or above (100% vs. 38.04%, p < 0.001), and (iii) residence area rural versus urban (56.36% vs. 38.25%, p = 0.001). Moreover, depressive symptoms was observed against various job‐related factors including (i) organization maintains health safety rules partially versus fully (60.22% vs. 29.93%, p < 0.001), (ii) no thermal scanning before entry versus always (50.43% vs. 36.33%, p = 0.022), (iii) no hand sanitizer or hand washing facilities at workplace versus always (75% vs. 34.88%, p < 0.001), (iv) nobody wears mask versus everybody always wears mask at workplace (87.50% vs. 30.68%, p < 0.001), (v) quarantine or isolation is not mandatory for positive cases versus mandatory (75.51% vs. 38.61%, p < 0.001), (vi) organization is not performing like previous versus yes (47.17% vs. 36.73%, p = 0.017), (vii) organization does not pay during Covid‐19 relative leaves versus pays (59.14% vs. 38.37%, p < 0.001), (viii) the employer does not provide health insurance versus employer provides health insurance (49.66% vs. 32.27%, p < 0.001), (ix) not getting on‐time salary versus getting on‐time salary during Covid‐19 pandemic (57.14% vs. 35.24%, p < 0.001), (x) anybody has lost their job amid pandemic versus not (51.79% vs. 32.82%, p < 0.001), (xi) salary reduction during pandemic versus no reduction of salary (55.72% vs. 33.33%, p < 0.001), (xii) organization type nonhealthcare versus healthcare (47.24% vs. 29.73%, p < 0.001), (xiii) use of public transportation versus private transports (51.11% vs. 40.15%, p = 0.007), (xiv) healthcare support at workplace unavailable versus available (57.69% vs. 28.99%, p < 0.001).
3.4. Associated risk factors for elevated fear and depressive symptoms
We measured correlations of sociodemographic profile (Table 3) and job‐related factors (Table 4) with psychometric parameters using binary logistic regression analysis. The probability of elevated fear in respondents with CED was 4.063 times more likely than in obese respondents (95% CI: 1.217–13.571, significance p = 0.023). Participants having a primary degree were more likely than participants with at least graduation or above (odds ratio [OR] = 2.651, 95% CI: 1.048–6.709, p = 0.040). Also, interconnections of job‐related factors were contributing to the increased fear. Precaution‐related variables have played a vital role in fear elevation. The unavailability of Covid‐19 testing support from the office was associated with elevated fear among the respondents at 1.523 folds (95% CI: 0.780–2.975, p = 0.218). We noticed the employees whose organization pays them during Covid‐19‐related leave are less likely than others (OR = 0.602, 95% CI: 0.255–1.423, p = 0.248). An interesting fact we have found in employees is that if anybody lost their job from an organization during the pandemic and increased fear associated to Covid‐19 of existing employees reduced to half (OR = 0.513, 95% CI: 0.240–1.556, p = 0.085). Respondents from healthcare organizations were less likely to have increased fear than nonhealthcare organizations (OR = 0.507, 95% CI: 0.227–1.132, p = 0.097). Employees who can work from home are less likely than those who cannot (OR = 0.254, 95% CI: 0.123–0.527, p < 0.001).
Table 3.
Regression analysis of sociodemographic variables by elevated fear and depressive symptoms among the private job holders
| Sociodemographic parameters | Elevated fear (N = 440) | Depressive symptoms (N = 215) | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | df | 95% CI | p Value | OR | df | 95% CI | p Value | |
| Age in years | ||||||||
| 25–35 | 0.725 | 1 | 0.073–1.273 | 0.999 | 1.115 | 1 | 0.125–9.951 | 0.922 |
| 36–45 | 0.982 | 1 | 0.063–11.052 | 0.999 | 0.876 | 1 | 0.100–7.698 | 0.905 |
| 46–60 | 1 | 1 | ||||||
| Sex | ||||||||
| Male | 0.871 | 1 | 0.457–1.659 | 0.674 | 1.287 | 1 | 0.774–2.139 | 0.331 |
| Female | 1 | |||||||
| BMI (kg/m2) | ||||||||
| Below 18.5 (CED) | 4.063 | 1 | 1.217– 13.571 | 0.023 | 1.556 | 1 | 0.526–4.603 | 0.425 |
| 18.5–25 (normal) | 2.255 | 1 | 0.680–7.476 | 0.184 | 1.007 | 1 | 0.333–3.041 | 0.991 |
| Above 25 (obese) | 1 | 1 | ||||||
| Marital status | ||||||||
| Married | 0.871 | 1 | 0.046–16.451 | 0.926 | 0.347 | 1 | 0.045–2.689 | 0.311 |
| Unmarried | 0.746 | 1 | 0.052–10.700 | 0.830 | 0.586 | 1 | 0.091–3.766 | 0.573 |
| Divorced | 0.577 | 1 | 0.040–8.271 | 0.685 | 0.919 | 1 | 0.140–6.021 | 0.929 |
| Widow | 1 | 1 | ||||||
| Education level | ||||||||
| Primary | 2.651 | 1 | 1.048–6.709 | 0.040 | 0.510 | 1 | 0.258–1.009 | 0.050 |
| Secondary | 0.881 | 1 | 0.093–8.330 | 0.912 | 0.530 | 1 | 0.372–1.526 | 0.999 |
| Graduate and above | 1 | 1 | ||||||
| Economic impression | ||||||||
| Low | 0.757 | 1 | 0.348–1.648 | 0.483 | 1.622 | 1 | 0.864–3.046 | 0.132 |
| Medium | 0.977 | 1 | 0.470–2.029 | 0.950 | 1.091 | 1 | 0.651–1.829 | 0.741 |
| High | 1 | 1 | 1 | 1 | ||||
| Residence area | ||||||||
| Urban | 0.854 | 1 | 0.380–1.921 | 0.703 | 1.414 | 1 | 0.822–2.431 | 0.211 |
| Rural | 1 | 1 | 1 | 1 | ||||
| Living status | ||||||||
| With family | 1.252 | 1 | 0.629–2.492 | 0.522 | 1.472 | 1 | 0.877–2.471 | 0.143 |
| Without family | 1 | 1 | 1 | 1 | ||||
| Smoking habit | ||||||||
| Smoker | 0.848 | 1 | 0.422–1.707 | 0.645 | 0.668 | 1 | 0.409–1.093 | 0.108 |
| Nonsmoker | 1 | 1 | 1 | 1 | ||||
Note: p‐values are significant at 95% confidence interval (p < 0.05). Significant p‐values are shown in bold.
Abbreviations: BMI, body mass index; CED, chronic energy deficiency; Covid‐19, coronavirus disease 2019; CI, confidence interval; df, degree of freedom; N, number; OR, odds ratio.
Table 4.
Regression analysis of variables by elevated fear and depressive symptoms among the private job holders
| Job‐related factors | Elevated fear (N = 440) | Depressive symptoms (N = 215) | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | df | 95% CI | p Value | OR | df | 95% CI | p Value | |
| Organization maintains health safety rules | ||||||||
| Fully | 1.176 | 1 | 0.545–2.535 | 0.680 | 0.497 | 1 | 0.291–0.849 | 0.010 |
| Partially | 0.572 | 1 | 0.138–2.367 | 0.440 | 0.521 | 1 | 0.154–1.762 | 0.294 |
| Not at all | 1 | 1 | ||||||
| Thermal scanning before entry | ||||||||
| Always | 1.096 | 1 | 0.475–2.53 | 0.830 | 1.786 | 1 | 0.987–3.23 | 0.055 |
| Sometimes | 0.687 | 1 | 0.268–1.76 | 0.434 | 1.027 | 1 | 0.529–1.991 | 0.938 |
| Not at all | 1 | |||||||
| Hand sanitizer or hand washing facilities at work | ||||||||
| Always | 1.415 | 1 | 0.582–3.437 | 0.444 | 0.954 | 1 | 0.506–1.8 | 0.885 |
| Sometimes | 0.288 | 1 | 0.063–1.313 | 0.108 | 1.54 | 1 | 0.372–6.379 | 0.551 |
| Not at all | 1 | 1 | ||||||
| Everyone wears a mask at the workplace | ||||||||
| Always | 0.796 | 1 | 0.357–1.779 | 0.579 | 0.567 | 1 | 0.321–1.001 | 0.051 |
| Sometimes | 0.751 | 1 | 0.141–4.011 | 0.738 | 2.814 | 1 | 0.522–15.171 | 0.229 |
| Not at all | 1 | 1 | ||||||
| Availability of mental healthcare support at work | ||||||||
| Yes | 0.822 | 1 | 0.404–1.67 | 0.587 | 2.068 | 1 | 1.267–3.376 | 0.004 |
| No | 1 | 1 | ||||||
| Availability of Covid‐19 testing support from office | ||||||||
| Yes | 1.523 | 1 | 0.78–2.975 | 0.218 | 1.062 | 1 | 0.626–1.803 | 0.822 |
| No | 1 | 1 | ||||||
| Quarantine or isolation is mandatory for Covid‐19 positive cases | ||||||||
| Yes | 0.933 | 1 | 0.321–2.711 | 0.898 | 3.263 | 1 | 1.372–7.759 | 0.007 |
| No | 1 | 1 | ||||||
| Organization pays during Covid‐19‐related leave | ||||||||
| Yes | 0.602 | 1 | 0.255–1.423 | 0.248 | 0.83 | 1 | 0.447–1.544 | 0.557 |
| No | 1 | 1 | ||||||
| Organization is performing like previous | ||||||||
| Yes | 0.827 | 1 | 0.44–1.556 | 0.557 | 0.989 | 1 | 0.618–1.581 | 0.962 |
| No | 1 | 1 | ||||||
| Employer provides health insurance | ||||||||
| Yes | 0.762 | 1 | 0.385–1.505 | 0.433 | 1.016 | 1 | 0.612–1.687 | 0.95 |
| No | 1 | 1 | ||||||
| Getting on‐time salary during Covid‐19 pandemic | ||||||||
| Yes | 1.999 | 1 | 0.812–4.92 | 0.132 | 1.114 | 1 | 0.642–1.935 | 0.701 |
| No | 1 | 1 | ||||||
| Anybody has lost their job from your organization | ||||||||
| Yes | 0.513 | 1 | 0.24–1.097 | 0.085 | 0.671 | 1 | 0.394–1.144 | 0.143 |
| No | 1 | 1 | ||||||
| Organization has reduced salary during the pandemic | ||||||||
| Yes | 0.792 | 1 | 0.346–1.811 | 0.580 | 0.513 | 1 | 0.287–0.915 | 0.024 |
| No | 1 | 1 | ||||||
| Work from home is allowable | ||||||||
| Always | 0.254 | 1 | 0.123–0.527 | <0.001 | 0.724 | 1 | 0.414–1.268 | 0.258 |
| Sometimes | 1.667 | 1 | 0.754–3.681 | 0.207 | 0.873 | 1 | 0.517–1.474 | 0.611 |
| Not at all | 1 | 1 | ||||||
| Organization type | ||||||||
| Healthcare | 0.507 | 1 | 0.227–1.132 | 0.097 | 0.806 | 1 | 0.443–1.466 | 0.480 |
| Nonhealthcare | 1 | 1 | ||||||
Note: p‐values are significant at 95% confidence interval (p < 0.05). Significant p‐values are shown in bold.
Abbreviations: BMI, body mass index; CED, chronic energy deficiency; COVID‐19, coronavirus disease 2019; CI, confidence interval; df, degree of freedom; N, number; OR, odds ratio.
Participants from primary education levels were more likely to have depressive symptoms than the graduate or above‐level education group (OR = 0.510, 95% CI: 0.258–1.009, p = 0.050). However, healthcare‐related factors are significantly associated with the possibility of depressive symptoms among private job holders. The probability of having depressive symptoms in the employees of organizations that fully maintained health safety rules was less than which did not (OR = 0.497, 95% CI: 0.291–0.849, p = 0.010). Participants from the workplaces, where everyone wears a mask have 0.567 folds less chance to get depressive symptoms than those where everyone does not wear a mask (OR = 0.567, 95% CI: 0.321–1.001, p = 0.051), and availability of thermal scanning was less likely than others (OR = 1.786, 95% CI: 0.987–3.23, p = 0.055). However, the availability of mental healthcare support at the workplace increased the likelihood of having depressive symptoms (OR = 2.068, 95% CI: 1.267–3.376, p = 0.004). In organizations where quarantine or isolation is mandatory in confirmed or suspected cases, their employees are 3.263 times more prone to depressive symptoms than others (OR = 3.263, 95% CI: 1.372–7.759, p = 0.007). However, we observed in the case of salary reduction, the chances of depressive symptoms were dropped to half when in reduced salary (OR = 0.513, 95% CI: 0.287–0.915, p = 0.024).
3.5. Reliability
We measured the internal consistency of FCV‐19 and PHQ‐9 scales used in the present study by Cronbach's α. Values of the reliability coefficient Cronbach's α for FCV‐19 and PHQ‐9 scales were 0.87 and 0.84, respectively. The reliability values of both scares are higher than the recommended value of 0.80.
4. DISCUSSION
This is the first‐ever study addressing the mental health of private job holders in Bangladesh due to the Covid‐19 pandemic. The private sector contributes a significant share to the economy of any country, and Bangladesh is not an exception. The private sector of Bangladesh has grown significantly over the last few decades. According to CEIC data, among the 169.3 million population, 60.80 million people are employed privately in Bangladesh. 59 , 60 Individual proprietorship engages the greatest proportion of the workforce, followed by households and private sectors. Government/autonomous/local government organizations employed a small percentage of the population in Bangladesh. 61 Therefore, the present study was necessary to explore the fear and depressive symptoms among private service holders due to the Covid‐19 pandemic in Bangladesh.
In this study, we observed the prevalence of increased fear and depressive symptoms was high among Bangladeshi private service holders working in either healthcare or nonhealthcare organizations. In another study, we noticed that the ongoing Covid‐19 pandemic, its responses, and other global health emergencies have created psychological problems among the general population across the world. 62 , 63 , 64 , 65 Moreover, we have seen the prevalence of depressive symptoms, anxiety, loneliness, and sleep problems were 44%, 78%, 89%, and 87% among the healthcare professionals in Bangladesh. 18 A study among the Saudi population also observed that the mental health of one‐fourth of the study population was affected during the Covid‐19 outbreak. 66 However, according to the current study, the prevalence of Covid‐19‐related fear and depressive symptoms among private service holders from nonhealthcare organizations was higher than healthcare organizations. But another similar study conducted among nurses in Qatar reported that nurses working in non‐Covid and Covid facilities had mental stress, depressive symptoms, and anxiety at normal to mild levels, which made no significant differences. 67 A group of German scientists suggested a high prevalence of depressive symptoms, generalized anxiety, and fear symptoms associated with Covid‐19 factors among German people amid the pandemic. 68 So, findings and discussion of the above studies support the present study results.
We observed the prevalence of depressive symptoms among private service holders in rural areas was higher than in urban areas. Job security and health precaution‐related variables have a vital role in maintaining the mental health of private service holders. 69 , 70 , 71 The current study identified several precaution‐related factors for Covid‐19 in the alteration of mental health among private job holders. The employees were less likely to have mental health problems whose organization adequately maintained health safety rules at the workplace. According to current findings, isolation or quarantine were mandatory for confirmed or suspected cases in most organizations. But, employees of these organizations are more vulnerable to depressive symptoms than where it is not applicable. Therefore, we can assume that those Covid‐19 responses created psychological consequences among their employees. Also, a bunch of evidence reported the risks of getting depressive symptoms and anxiety increased as an outcome of isolation or quarantine. 72 , 73 , 74 The current study observed a high prevalence of depressive symptoms among the employees where a health insurance scheme does not exist, the organization does not perform like previous, does not pay during Covid‐19‐associated leave, and employees do not get an on‐time salary. However, this circumstance is quite common in private sectors in healthcare and several categories of nonhealthcare organizations across the globe. 75 , 76 , 77 , 78 Also, in organizations where anybody has lost their job or experienced a salary reduction, depressive symptoms, and fear among existing employees decreased significantly. It might be occurred due to any form of schadenfreude in workplaces. 79 , 80 Previous studies also reported similar crises in interpersonal relationships and behavior among co‐workers. 81 , 82 , 83 , 84 , 85
Before the Covid‐19 pandemic, the prevalence of mental health problems among the adult population ranged from 6.5% to 31.0% in Bangladesh. 86 The significant increase in fear and depressive symptoms among private service holders during the Covid‐19 pandemic (86.27% and 42.16%, respectively) is a concern for Bangladesh. Therefore, the healthcare authorities should take necessary initiatives to promote good mental health during this global health emergency. The National Institute of Mental Health (NIMH) of Bangladesh has declared some actionable items to deal with these additional psychological burdens. This government authority recommended using psychotropics, avoiding repeated scrolling of Covid‐19 news, accepting Covid‐19‐related information after verification, and reducing the frequent use of social media. Also, they advised to adopt some simple relaxation techniques and breathing exercises to be mentally strong during this global health crisis. 87 Inconsistent with them, some earlier research suggested social support, online responses, counseling, and some techniques for promoting good mental health. 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 Authorities of private establishments may enhance their plans and policy for employees using the findings of this study. Academics and researchers may get access to secondary data for further studies. Moreover, the authorities can apply terror management theory (TMT) to cope up with the elevated fear among private service holders with respect to the COVID‐19 pandemic. According to the TMT theory, awareness of death plays an important role to manage potential anxiety by maintaining faith in self‐esteem, close relationships, and cultural worldviews. The anxiety‐buffering systems might mitigate elevated fear and anxiety due to Covid‐19 imposing a sense that the life of every person is meaningful in this nice world. 99
4.1. Study strengths and limitations
The present study has several strengths. We used web‐based platforms to reach a bulk of individuals, and rapid data collection was possible during public health emergencies. We translated our data collection tools from English into Bengali and provided both versions for better understanding and clarity. This is the first study to evaluate the mental health of private job holders in Bangladesh. Also, this study has a few limitations. A web‐based survey may not reach the day‐labor class. The self‐responding online study might have some respondent‐associated biases. A cross‐sectional study itself is a limitation to assess the impact of these mental health issues over time. Follow‐up studies are appreciated to assess the gravity of the highlighted mental health problems among the private job holders in Bangladesh. Future research can discover their actual mental condition after the pandemic crisis. Findings from the present and follow‐up studies would help to develop context‐specific mental health interventions in private organizations.
5. CONCLUSIONS
The present study findings suggest that high proportions of private job holders in Bangladesh have experienced increased fear and depressive symptoms during the early stage of the Covid‐19 pandemic. Several Covid‐19‐related and sociodemographic factors are responsible for the poor mental health of private service holders in Bangladesh. Therefore, we recommend actionable measures for private establishments to improve the affected mental health of their employees due to the Covid‐19 pandemic. Authorities can develop efficient mental health and Covid‐19 support systems. The findings of our present study have diverse implications. The policymakers and regulatory bodies might take some initiatives to promote mental health in the private sector in Bangladesh.
AUTHOR CONTRIBUTIONS
Md. Rabiul Islam: Conceptualization; supervision; writing—review & editing. Zabun Nahar: Data curation; writing—original draft. Md. Sakhawat Hossain: Data curation; writing—original draft. Md. Jamal Hossain: Data curation; formal analysis; writing—review & editing. Mohammad Shahriar: Data curation; formal analysis; writing—review & editing. Sardar Mohammad Ashraful Islam: Data curation; formal analysis; writing—review & editing. Mohiuddin Ahmed Bhuiyan: Supervision; writing—review & editing.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
Md. Rabiul Islam affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
ACKNOWLEDGMENTS
All the authors are thankful to the participants for their cooperation to conduct this study.
Islam MR, Nahar Z, Hossain MS, et al. Prevalence and associated factors for elevated fear and depressive symptoms among the private service holders in Bangladesh during the Covid‐19 pandemic: a cross‐sectional study. Health Sci Rep. 2022;5:e795. 10.1002/hsr2.795
Md. Rabiul Islam and Zabun Nahar contributed equally to this study.
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article or its supplementary materials.
REFERENCES
- 1.WHO. WHO Director‐General's Opening Remarks at the Media Briefing on COVID‐19—11 March 2020. WHO Director General's Speeches. 2020. Accessed 29 Sep 2021. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 2. Daria S, Asaduzzaman M, Shahriar M, Islam MR. The massive attack of COVID‐19 in India is a big concern for Bangladesh: the key focus should be given on the interconnection between the countries. Int J Health Plann Manage. 2021;36(5):1947‐1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Daria S, Islam MR. The use of cow dung and urine to cure COVID‐19 in India: a public health concern. Int J Health Plann Manage. 2021;36(5):1950‐1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Islam MR, Qusar MMAS, Islam MS. Mental health of children amid COVID‐19 pandemic in Bangladesh: an exploratory observation. Asia Pac J Public Health. 2021;33(4):469‐470. [DOI] [PubMed] [Google Scholar]
- 5. Rahman FI, Islam MR. Sexual violence against woman at quarantine center during coronavirus disease 2019 in Bangladesh: risk factors and recommendations. Womens Health (Lond). 2021;17:17455065211043851. 10.1177/17455065211043851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rahman FI, Ether SA, Islam MR. Upsurge of dengue prevalence during the third wave of COVID‐19 pandemic in Bangladesh: pouring gasoline to fire. Clin Pathol. 2022;15:2632010X221076068. 10.1177/2632010X221076068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Islam MR, Rahman MS, Qusar MS. Community‐based decentralized mental health services are essential to prevent the epidemic turn of post‐covid mental disorders in Bangladesh: a call to action. Health Sci Rep. 2022;5(4):e734. 10.1002/hsr2.734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rahman S, Hossain MJ, Islam MR. The upsurge of diarrhea amid COVID‐19 pandemic makes matter worse in Bangladesh: a call to action. Gerontol Geriatr Med. 2022;8:1‐5. 10.1177/23337214221117419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hossain MS, Islam MR, Islam MT, et al. Knowledge, acceptance and perception about COVID‐19 vaccines in Bangladesh: findings from a web‐based cross‐sectional study. Open Health. 2022;3:73‐86. 10.1515/openhe-2022-0010 [DOI] [Google Scholar]
- 10. Bari MS, Hossain MJ, Ahmmed F, et al. Knowledge, perception, and willingness towards immunization among Bangladeshi population during COVID‐19 vaccine rolling period. Vaccines (Basel). 2021;9(12):1449. 10.3390/vaccines9121449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Islam MR. Urgent call for mass immunization against coronavirus in Bangladesh. Sci Prog. 2021;104(4):368504211058562. 10.1177/00368504211058562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Islam MR, Hasan M, Nasreen W, Tushar MI, Bhuiyan MA. The COVID‐19 vaccination experience in Bangladesh: findings from a cross‐sectional study. Int J Immunopathol Pharmacol. 2021;35:20587384211065628. 10.1177/20587384211065628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chow SK, Francis B, Ng YH, et al. Religious coping, depression and anxiety among healthcare workers during the COVID‐19 pandemic: a Malaysian perspective. Healthcare (Basel, Switzerland). 2021;9(1):79. 10.3390/healthcare9010079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mirhosseini S, Dadgari A, Basirinezhad MH, Mohammadpourhodki R, Ebrahimi H. The role of hope to alleviate anxiety in COVID‐19 outbreak among community dwellers: an online cross‐sectional survey. Ann Acad Med Singap. 2020;49(10):723‐730. [PubMed] [Google Scholar]
- 15. Gupta AK, Mehra A, Niraula A, et al. Prevalence of anxiety and depression among the healthcare workers in Nepal during the COVID‐19 pandemic. Asian J Psychiatr. 2020;54:102260. 10.1016/j.ajp.2020.102260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Islam MR, Hossain MJ. Social stigma and suicide in Bangladesh: the Covid‐19 has worsened the situation. Chronic Stress (Thousand Oaks). 2021;5:24705470211035602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mamun MA, Sakib N, Gozal D, et al. The COVID‐19 pandemic and serious psychological consequences in Bangladesh: a population‐based nationwide study. J Affect Disord. 2021;279:462‐472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Das R, Hasan MR, Daria S, Islam MR. Impact of COVID‐19 pandemic on mental health among general Bangladeshi population: a cross‐sectional study. BMJ Open. 2021;11(4):e045727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rahman FI, Ether SA, Islam MR. The “Delta Plus” COVID‐19 variant has evolved to become the next potential variant of concern: mutation history and measures of prevention. J Basic Clin Physiol Pharmacol. 2021;33:109‐112. 10.1515/jbcpp-2021-0251 [DOI] [PubMed] [Google Scholar]
- 20. Rahman FI, Islam MR, Bhuiyan MA. Mucormycosis or black fungus infection is a new scare in south asian countries during the COVID‐19 pandemic: associated risk factors and preventive measures. J Med Virol. 2021;93(12):6447‐6448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moona AA, Islam MR. Mucormycosis or black fungus is a new fright in India during covid‐19 pandemic: associated risk factors and actionable items. Public Health Pract (Oxf). 2021;2:2100153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mamun MA. Suicide and suicidal behaviors in the context of COVID‐19 pandemic in Bangladesh: a systematic review. Psychol Res Behav Manag. 2021;14:695‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hossain MM, Tasnim S, Sultana A, et al. Epidemiology of mental health problems in COVID‐19: a review. F1000Res. 2020;9:636. 10.12688/f1000research.24457.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Islam MR, Jannath S, Moona AA, Akter S, Hossain MJ, Islam SMA. Association between the use of social networking sites and mental health of young generation in Bangladesh: a cross‐sectional study. J Community Psychol. 2021;49(7):2276‐2297. [DOI] [PubMed] [Google Scholar]
- 25. Daria S, Islam MR. The second wave of COVID‐19 pandemic in Bangladesh: an urgent call to save lives. Asia Pac J Public Health. 2021;33(5):665‐666. [DOI] [PubMed] [Google Scholar]
- 26. Islam MR, Hossain MJ. Increments of gender‐based violence amid COVID‐19 in Bangladesh: a threat to global public health and women's health. Int J Health Plann Manage. 2021;36:2436‐2440. 10.1002/hpm.3284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nahar Z, Sohan M, Hossain MJ, Islam MR. Unnecessary cesarean section delivery causes risk to both mother and baby: a commentary on pregnancy complications and women's health. Inquiry. 2022;59:469580221116004. 10.1177/00469580221116004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rahman FI, Ether SA, Islam MR. The growing rape incidences seems an epidemic turn of sexual violence in Bangladesh: a letter to the editor. Womens Health (Lond). 2021;17:1717455065211063285. 10.1177/17455065211063285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Abir T, Kalimullah NA, Osuagwu UL, et al. Prevalence and factors associated with mental health impact of COVID‐19 pandemic in Bangladesh: a survey‐based cross‐sectional study. Ann Glob Health. 2021;87(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mohapatra RK, Tiwari R, Sarangi AK, Islam MR, Chakraborty C, Dhama K. Omicron (B.1.1.529) variant of SARS‐CoV‐2: concerns, challenges, and recent updates. J Med Virol. 2022;94(6):2336‐2342. 10.1002/jmv.27633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Daria S, Islam MR. The SARS‐CoV‐2 omicron wave is indicating the end of the pandemic phase but the COVID‐19 will continue. J Med Virol. 2022;94(6):2343‐2345. 10.1002/jmv.27635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hossain MJ, Ahmmed F, Khan MR, et al. Impact of prolonged COVID‐19 lockdown on body mass index, eating habits, and physical activity of university students in Bangladesh: a web‐based cross‐sectional study. Front Nutr. 2022;9:873105. 10.3389/fnut.2022.873105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Islam MR, Hossain MJ. Detection of SARS‐CoV‐2 Omicron (B.1.1.529) variant has created panic among the people across the world: what should we do right now? J Med Virol. 2022;94(5):1768‐1769. 10.1002/jmv.27546 [DOI] [PubMed] [Google Scholar]
- 34. Daria S, Bhuiyan MA, Islam MR. Detection of highly muted coronavirus variant Omicron (B.1.1.529) is triggering the alarm for South Asian countries: associated risk factors and preventive actions. J Med Virol. 2022;94(4):1267‐1268. 10.1002/jmv.27503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Islam T, Hasan M, Rahman MS, Islam MR. Comparative evaluation of authorized drugs for treating Covid‐19 patients. Health Sci Rep. 2022;5(4):e671. 10.1002/hsr2.671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Daria S, Islam MR. Indiscriminate use of antibiotics for COVID‐19 treatment in south asian countries is a threat for future pandemics due to antibiotic resistance. Clin Pathol. 2022;15:2632010X221099889. 10.1177/2632010X221099889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mahmud MS, Talukder MU, Rahman SM. Does ‘Fear of COVID‐19’ trigger future career anxiety? An empirical investigation considering depression from COVID‐19 as a mediator. Int J Soc Psychiatry. 2021;67(1):35‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sakib SN. Bangladesh: Suicide Claims More Lives Than Coronavirus. Anadolu Agency. 2021. Accessed September 29, 2021. https://www.aa.com.tr/en/asia-pacific/bangladesh-suicide-claims-more-lives-than-coronavirus/2175200
- 39.Tribune Report. 70% More Suicides Than Covid‐19 Deaths in the Last Year. Dhaka Tribune. 2021. Accessed September 29, 2021. https://www.dhakatribune.com/bangladesh/2021/03/13/70-more-suicides-than-covid-19-deaths-in-the-last-year
- 40.Bangladesh Bureau of Statistics (BBS). Report on Economic Census 2013. 2015. Accessed October 01, 2021. www.bbs.gov.bd
- 41.MOF. Bangladesh‐Economic‐Review‐2020—Finance Division, Ministry of Finance‐Government of the People\'s Republic of Bangladesh. 2021. Accessed October 02, 2021. https://mof.portal.gov.bd/site/page/28ba57f5-59ff-4426-970a-bf014242179e/Bangladesh-Economic-Review-2020
- 42. Rahman FI, Islam MR. Sexual violence against woman at quarantine center during coronavirus disease 2019 in Bangladesh: risk factors and recommendations. Womens Health (Lond). 2021;17:17455065211043851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Islam MR, Daria S, Das R, Hasan MR. A nationwide dataset on the mental health of the Bangladeshi population due to the COVID‐19 pandemic. Data Brief. 2021;38:107347. 10.1016/j.dib.2021.107347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Byron RK, Habib A. Covid‐19 Fallout: 68% Lost Jobs in Dhaka and Ctg. The Daily Star. 2020. Accessed September 28, 2021. https://www.thedailystar.net/frontpage/news/68pc-lost-jobs-dhaka-and-ctg-1968641
- 45.IANS. Bangladesh update: 68% Lost Jobs in Dhaka, Chittagong due to Covid‐19. Business Standard. 2020. Accessed September 28, 2021. https://www.business-standard.com/article/international/bangladesh-update-68-lost-jobs-in-dhaka-chittagong-due-to-covid-19-120092800283_1.html
- 46. Amit S. Coronavirus and impact on the Bangladesh economy: assessing the damage of the black swan of 2020. Asia‐Pacific J: Jpn Focus. 2020;18(15):5441. [Google Scholar]
- 47. Mavis M. 3,313 Bankers Quit in 19 Months. Dhaka Tribune. 2021. Accessed September 29, 2021. https://www.dhakatribune.com/business/banks/2021/09/15/3-313-bankers-quit-in-19-months
- 48.The Financial Express. Bangladeshi Software Firms Take a Hit From Covid. 2021. Accessed October 02, 2021. https://thefinancialexpress.com.bd/sci-tech/bangladeshi-software-firms-take-a-hit-from-covid-1632024155
- 49. Alam A. Addressing School Dropout in Texas. The Independent. 2021. Accessed October 02, 2021. https://m.theindependentbd.com/post/268549
- 50. Hossain MJ, Soma MA, Bari MS, Emran TB, Islam MR. COVID‐19 and child marriage in Bangladesh: emergency call to action. BMJ Paediatr Open. 2021;5(1):e001328. 10.1136/bmjpo-2021-001328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Akhter S. Countless Students Drop Out, Schools Close. New Age. 2021. Accessed October 02, 2021. https://www.newagebd.net/article/150657/countless-students-drop-out-schools-close
- 52. Mamun S. Covid‐19: Over 45% Secondary School Students May Drop Out. Dhaka Tribune. 2020. Accessed October 02, 2021. https://www.dhakatribune.com/bangladesh/2020/08/07/covid-19-over-45-secondary-school-students-may-drop-out
- 53. Alamgir M. World Teachers' Day 2021: Jobs Gone, Hopes Too. The Daily Star. 2021. Accessed October 03, 2021. https://www.thedailystar.net/news/bangladesh/news/world-teachers-day-today-jobs-gone-hopes-too-2190731
- 54. Hossain M. COVID‐19 impacts on employment and livelihood of marginal people in Bangladesh: lessons learned and way forward. South Asian Survey. 2021;28(1):57‐71. [Google Scholar]
- 55. Shovon FR. Covid‐19: Employment Takes a Serious Hit in Bangladesh. Dhaka Tribune. 2020. Accessed October 03, 2021. https://www.dhakatribune.com/health/coronavirus/2020/09/23/employment-during-an-economy-ravaged-by-covid-19
- 56. Sakib N, Bhuiyan AKMI, Hossain S, et al. Psychometric validation of the Bangla Fear of COVID‐19 Scale: confirmatory factor analysis and rasch analysis. Int J Ment Health Addict . 2020;1‐12. [DOI] [PMC free article] [PubMed]
- 57. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID‐19 Scale: development and initial validation. Int J Ment Health Addict. 2022;20(3):1537‐1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kroenke K, Spitzer RL, Williams JB. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606‐613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.CEIC Data. Bangladesh Employed Persons [1996–2017] [Data & Charts]. 2019. Accessed October 04, 2021. https://www.ceicdata.com/en/indicator/bangladesh/employed-persons
- 60.CEIC Data. Bangladesh Population, 1990–2021. 2021. Accessed October 04, 2021. https://www.ceicdata.com/en/indicator/bangladesh/population
- 61.Bangladesh Bureau of Statistics (BBS). Labour Force Survey Bangladesh 2016–17. 2018. Accessed October 04, 2021. http://203.112.218.65:8008/WebTestApplication/userfiles/Image/LatestReports/LFS_2016-17.pdf
- 62. Islam MR, Hasan M, Rahman MS, Rahman MA. Monkeypox outbreak—no panic and stigma; only awareness and preventive measures can halt the pandemic turn of this epidemic infection. Int J Health Plann Manage . 2022. 10.1002/hpm.3539 [DOI] [PubMed]
- 63. Islam MR, Asaduzzaman M, Shahriar M, Bhuiyan MA. The spreading of monkeypox in nonendemic countries has created panic across the world: could it be another threat? J Med Virol . 2022. 10.1002/jmv.27919 [DOI] [PubMed]
- 64. Sohan M, Hossain MJ, Islam MR. The SARS‐CoV‐2 Omicron (B.1.1.529) variant and effectiveness of existing vaccines: what we know so far. J Med Virol. 2022;94(5):1796‐1798. 10.1002/jmv.27574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Jannath S, Sohan M, Rahman MA, Islam MR. Suicides among university students during the COVID‐19 pandemic: Bangladeshi press reports. Open Health. 2022;3:13‐19. 10.1515/openhe-2022-0002 [DOI] [Google Scholar]
- 66. Repon MAU, Pakhe SA, Quaiyum S, Das R, Daria S, Islam MR. Effect of COVID‐19 pandemic on mental health among Bangladeshi healthcare professionals: a cross‐sectional study. Sci Prog. 2021;104(2):368504211026409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. The psychological impact of COVID‐19 pandemic on the general population of Saudi Arabia. Compr Psychiatry. 2020;102:152192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Nashwan AJ, Villar RC, Al‐Qudimat AR, et al. Quality of life, sleep quality, depression, anxiety, stress, eating habits, and social bounds in nurses during the coronavirus disease 2019 pandemic in Qatar (The PROTECTOR Study): a cross‐sectional, comparative study. J Pers Med. 2021;11(9):918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Bäuerle A, Teufel M, Musche V, et al. Increased generalized anxiety, depression and distress during the COVID‐19 pandemic: a cross‐sectional study in Germany. J Public Health (Oxf). 2020;42(4):672‐678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Araç S, Dönmezdil S. Investigation of mental health among hospital workers in the COVID‐19 pandemic: a cross‐sectional study. Sao Paulo Med J. 2020;138(5):433‐440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Deora H, Mishra S, Tripathi M, et al. Adapting neurosurgery practice during the COVID‐19 pandemic in the Indian subcontinent. World Neurosurg. 2020;142:e396‐e406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Obrenovic B, Du J, Godinic D, Baslom MMM, Tsoy D. The threat of COVID‐19 and job insecurity impact on depression and anxiety: an empirical study in the USA. Front Psychol. 2021;12:648572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Abad C, Fearday A, Safdar N. Adverse effects of isolation in hospitalised patients: a systematic review. J Hosp Infect. 2010;76(2):97‐102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Henssler J, Stock F, van Bohemen J, Walter H, Heinz A, Brandt L. Mental health effects of infection containment strategies: quarantine and isolation‐a systematic review and meta‐analysis. Eur Arch Psychiatry Clin Neurosci. 2021;271(2):223‐234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Purssell E, Gould D, Chudleigh J. Impact of isolation on hospitalised patients who are infectious: systematic review with meta‐analysis. BMJ Open. 2020;10(2):e030371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Buchanan M, McClenaghan M. Covid Debt: A Baby, Job Loss—and Now Eviction. BBC News. 2021. Accessed October 04, 2021. https://www.bbc.com/news/uk-58643437
- 77. Karp P. ‘Highly Disproportionate’: Australia's Casual Workers Bear Brunt of Job Losses Amid Lockdowns. The Guardian. 2021. Accessed October 04, 2021. https://www.theguardian.com/australia-news/2021/oct/04/highly-disproportionate-australias-casual-workers-bear-brunt-of-job-losses-amid-lockdowns
- 78. Omjasvin M. Delayed Payments, Job Loss Hit Covid Doctors in TN. The New Indian Express. 2021. Accessed October 04, 2021. https://www.newindianexpress.com/states/tamil-nadu/2021/sep/18/delayed-payments-job-loss-hit-covid-doctors-in-tn-2360329.html
- 79. Phadnis A. Covid impact: SpiceJet Defers up to 50% Salary of Most Employees in April. Business Standard. 2021. Accessed October 04, 2021. https://www.business-standard.com/article/companies/covid-impact-spicejet-defers-up-to-50-salary-of-most-employees-in-april-121050100377_1.html
- 80. Kalra A, Narang A. Schadenfreude. Eur Heart J. 2019;40(48):3885‐3886. [DOI] [PubMed] [Google Scholar]
- 81. Pietraszkiewicz A, Chambliss C. The link between depression and schadenfreude: further evidence. Psychol Rep. 2015;117(1):181‐187. [DOI] [PubMed] [Google Scholar]
- 82. Cleary M, Hunt GE, Horsfall J. Identifying and addressing bullying in nursing. Issues Ment Health Nurs. 2010;31(5):331‐335. [DOI] [PubMed] [Google Scholar]
- 83. da Silva João AL, Saldanha Portelada AF. Mobbing and its impact on interpersonal relationships at the workplace. J Interpers Violence. 2019;34(13):2797‐2812. [DOI] [PubMed] [Google Scholar]
- 84. Horita Y, Otsuka Y. Relationships between workers' interpersonal helping behavior, social supports, job stressors, psychological stress responses, and vigour in manufacturing industry. Sangyo Eiseigaku Zasshi/J Occup Health. 2014;56(6):259‐267. [DOI] [PubMed] [Google Scholar]
- 85. Kostev K, Rex J, Waehlert L, Hog D, Heilmaier C. Risk of psychiatric and neurological diseases in patients with workplace mobbing experience in Germany: a retrospective database analysis. Ger Med Sci. 2014;12:Doc10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Whitaker T. Social workers and workplace bullying: perceptions, responses and implications. Work. 2012;42(1):115‐123. [DOI] [PubMed] [Google Scholar]
- 87. Hossain MD, Ahmed HU, Chowdhury WA, Niessen LW, Alam DS. Mental disorders in Bangladesh: a systematic review. BMC Psychiatry. 2014;14:216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.National Institute of Mental Health (NIMH). Recommendations From Sub Committee For Mental Health. 2020. Accessed October 1, 2021. https://mofa.portal.gov.bd/sites/default/files/files/mofa.portal.gov.bd/page/ad1f289c_47cf_4f6c_8dee_887957be3176/Guideline%20for%20Mental%20Health%20Issue-COVID-19-%20DGHS.pdf
- 89. Armitage R, Nellums LB. The COVID‐19 response must be disability inclusive. Lancet Public Health. 2020;5(5):e257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Daria S, Islam MR. Increased suicidal behaviors among students during COVID‐19 lockdowns: a concern of student's mental health in Bangladesh. J Affect Disord Rep. 2022;8:100320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Shalahuddin Qusar MMA, Hossain R, Sohan M, Nazir S, Hossain MJ, Islam MR. Attitudes of mental healthcare professionals and media professionals towards each other in reducing social stigma due to mental illness in Bangladesh. J Community Psychol. 2022;50:3181‐3195. 10.1002/jcop.22823 [DOI] [PubMed] [Google Scholar]
- 93. Hossain MJ, Ahmmed F, Sarker MMR, et al. Factors associated with underprivileged E‐learning, session jam phobia, and the subsequent mental distress among students following the extended university closure in Bangladesh. Front Public Health. 2022;9:807474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Islam S, Islam T, Islam MR. New coronavirus variants are creating more challenges to global healthcare system: a brief report on the current knowledge. Clin Pathol. 2022;15:2632010X221075584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Ether SA, Emon FA, Roknuzzaman A, Rakibuzzaman M, Rahman FI, Islam MR. A cross‐sectional study of COVID‐19‐related knowledge, risk perceptions, and preventive practices among pharmacy students in Bangladesh. SAGE Open Med. 2022;10:20503121211073014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Islam MR, Quaiyum S, Pakhe SA, Repon MAU, Bhuiyan MA. Dataset concerning the mental health of healthcare professionals during COVID‐19 pandemic in Bangladesh. Data Brief. 2021;39:107506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Islam MR, Tushar MI, Jannath S, Moona AA, Akter S, Islam SMA. Data set concerning the use of social networking sites and mental health problems among the young generation in Bangladesh. Data Brief. 2021;39:107593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Islam MR. The SARS‐CoV‐2 Omicron (B.1.1.529) variant and the re‐emergence of COVID‐19 in Europe: an alarm for Bangladesh. Health Sci Rep. 2022;5(2):e545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Pyszczynski T, Lockett M, Greenberg J, Solomon S. Terror management theory and the COVID‐19 pandemic. J Humanist Psychol. 2021;61(2):173‐189. 10.1177/00221678209594 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article or its supplementary materials.


