Abstract
Background
The social consequences of obesity may influence health and mortality rate (MR), given obesity's status as a highly stigmatized condition. Hence, a high absolute body mass index (BMI) in conjunction with the stigmatization of a high BMI may each independently increase the rate of MR.
Objectives
We tested whether relative BMI, defined as ordinal rank within a social reference group jointly defined by age, sex, and race/ethnicity, is associated with MR independent of absolute BMI.
Methods
Data were from three nationally representative datasets: the Health and Retirement Study (n = 31,115), the National Health Interview Survey (NHIS, n = 529,362), and the National Health and Nutrition Examination Survey (n = 31,115). Relative BMI kg/m2 deciles were calculated within twenty-four subgroups jointly defined by age (6 levels), sex (2 levels), and race/ethnicity (4 levels). The association between ordinal rank BMI and MR was assessed using Cox survival generalized additive models in each dataset with adjustments for age, race, sex, smoking, educational attainment, and absolute BMI.
Results
Absolute BMI had a significant non-monotonic association with MR, such that BMI was positively associated with mortality at BMI levels above approximately 25 kg/m2. Contrary to expectations, results from NHIS indicated that individuals in the first decile of relative BMI had the highest MR whereas relative BMI was not associated with MR in the NHANES and HRS.
Conclusion
We hypothesized that the stigmatization of obesity might lead to an increased MR after controlling for absolute BMI. Contrary to expectations, a higher relative BMI was not associated with an increased MR independent of absolute BMI.
Keywords: Mortality rate, Longevity, Lifespan, Stigma, Epidemiology, Relative weight, Deviance, Obesity, BMI
Highlights
-
•
A higher absolute BMI is associated with a higher mortality rate independent of relative BMI within a socially defined reference group.
-
•
A higher BMI relative to a socially defined reference group was not associated with mortality rate independent of absolute BMI.
-
•
After adjusting for absolute and relative BMI, having less than a high school education and being a former or current smoker are significantly associated with a higher mortality rate.
1. Introduction
1.1. The stigmatization of obesity
Discrimination against individuals with obesity is substantial and associated with physical and psychological harm (R. M. Puhl & Heuer, 2010). Weight stigma, sometimes termed “weight bias” or “weight prejudice”, is the discrediting of an individual based on their weight. Drawing on the classic sociological understanding of stigma, weight stigma is the belief that an individual with obesity is “not quite human” and disqualified from full social acceptance (Goffman, 1963). In the US, fatness has long been recognized as a stigmatized condition; indeed, it was one of the first stigmatized conditions to be examined by sociologists (Gutin, 2021), one in which persons who are overweight or obese are perceived as socially deviant and morally responsible for their weight status (Maddox, Back, & Liederman, 1968). Recent surveys of the US population reflect the continued stigmatization of obesity, with substantial negative stereotyping of individuals with obesity observed, including beliefs that individuals who are obese are inactive and lack self-control (T. J. Kim, Makowski, & von dem Kim, Makowski, & vondemKnesebeck, 2019). Consistent with negative stereotyping, individuals with obesity experience discrimination in a variety of settings, including employment, education, and interpersonal relationships (Goffman, 2009; Rebecca M; Puhl & Heuer, 2009). The stigmatization and negative stereotyping of individuals with obesity has spurred the development of destigmatization strategies by groups such as the National Association to Advance Fat Acceptance (NAAFA), founded in 1969 as a fat-rights organization modeling itself after the NAACP (Saguy & Ward, 2011). Given the pervasiveness and consequences of obesity's stigmatization, a 2020 joint international consensus statement by a multidisciplinary group of experts and scientific organizations concluded that "[w]eight stigma can mislead clinical decisions, and public health messages, and could promote unproductive allocation of limited research resources. Weight bias and stigma can result in discrimination, and undermine human rights, social rights, and the health of afflicted individuals” (Rubino et al., 2020).
1.2. The health consequences of stigmatization and discrimination
A growing body of evidence suggests that the experience of discrimination—be it based on race, sex, sexual orientation, weight, or other social identities—is associated with adverse health outcomes, including an increased risk of mortality, higher levels of cardiovascular stress biomarkers, and psychological distress (Alimoradi et al., 2020; Goosby, Malone, Richardson, Cheadle, & Williams, 2015; Major, Eliezer, & Rieck, 2012; Muennig, 2008). Accordingly, weight-based social identity threat occurs when individuals with overweight or obesity are aware of the cultural devaluation of their weight status, an awareness made especially acute by the experience of discrimination (Hunger, Major, Blodorn, & Miller, 2015; Steele, Spencer, & Aronson, 2002). In an analysis using nationally representative US data, discrimination because of one's weight was associated with a 60% increase in the mortality rate (MR)1—a greater increase than that attributed to other forms of perceived discrimination, including race, sex, and age (Sutin, Stephan, & Terracciano, 2015). Finally, greater weight-related self-stigma and perceived stigma are positively associated with depression and anxiety (Alimoradi et al., 2020). These results indicate that the stigmatization of obesity, both internalized and perceived, is associated with, and may drive, significant adverse psychological and physiologic health outcomes (Tomiyama et al., 2018).
In line with the joint consensus statement's recognition of the detrimental health effects of weight bias and discrimination and prior research documenting an association between a threatened social identity and adverse health outcomes, here we test the hypothesis that a high body mass index (BMI; kg/m2) relative to one's sex, race, and birth cohort is associated with an increased MR. We test this hypothesis using a novel operationalization of relative BMI (BMIr) to address a methodologic challenge to analyzing the effects of BMIr on health and MR independent of the effects of absolute BMI (BMIa): i.e., perfect collinearity between BMIa and BMIr.
1.3. Operationalizing relative and absolute BMI
Little research has separately estimated and compared the associations of BMIa and BMIr with health outcomes. Several challenges may underlie this lack of research, including the construction of appropriate reference groups to define relative BMI and jointly fitting BMIa and BMIr given their perfect collinearity within a reference group. An individual's perception of the social appropriateness of their weight and the weight of others depends on social context (Chang & Christakis, 2003), with social norms surrounding eating and body image exerting important influences on body weight (Hammond, 2010). In the United States, as the number of individuals who are overweight or obese increased, the probability that an individual self-classified as being overweight decreased, consistent with the social comparison hypothesis that what is considered a “normal” body size increases as average body size increases (Burke, Heiland, & Nadler, 2010). One's body size relative to a peer group thus shapes perceptions about the appropriateness of one's weight and how others perceive the appropriateness of our weight, with ample evidence that those perceived as having an abnormally high weight experience discrimination.
In the US, what is perceived as a “normal” body size may change as the number of individuals who are overweight or obese increases. Between 1999/2000 and 2017/2018, the number of US adults aged 20 and over who were obese increased from 30.5% to 42.4%. Further, the percentage of US adults with a BMI of 40 or higher nearly doubled, from 4.7 to 9.2%. Non-Hispanic black adults had the highest prevalence of obesity among women; however, the prevalence of obesity did not vary by race or ethnicity among men. Similarly, the prevalence of obesity did not significantly vary by age, with an estimated prevalence of obesity of 40.0%, 44.8%, and 42.8% among individuals aged 20–39 years, 40–59 years, and aged 60 and over, respectively (Hales, MD, Fryar, & Ogden, 2020). In addition to changing perceptions of normative body size in response to changes in population average body sizes, there is evidence that body size ideals vary by sex and race/ethnicity, with the ideal female figure in Western countries (and increasingly non-Western countries) characterized by thinness (Swami, 2015) and the ideal male figure characterized by leanness, muscularity, and a smaller waist-to-chest ratio (Garza, Heredia, & Cieślicka, 2017; Swami, 2006). Regarding racial and ethnic differences in body shape and weight norms in the US, evidence suggests Asian-American and White females may more strongly adhere to thinness norms, whereas Black females trend to report a stronger preference for a “curvier” body shape with larger buttocks (Overstreet, Quinn, & Agocha, 2010). Previous research has also characterized body size norms among females as existing along a “thinness norm spectrum, with Asian American girls most strongly adhering to thinness norms, followed jointly by non-Hispanic white and Hispanic girls, and lastly Black girls with the weakest adherence to thinness norms” (Martin, Thomas, Adler, & Kreager, 2020). Thus, what is perceived as “normal” body weight may be affected by changing population distributions as well as sex and racial/ethnic specific norms surrounding body weights and shapes and calculating one's BMI relative to mean BMI one's age, sex, and race-group may more precisely capture deviations from these norms.
Regarding the problem of collinearity, if one were to naïvely construct a measure of BMIr as equal to the difference between BMIa and the mean BMI of the sample, and then include measures of both BMIr and BMIa as predictors in a regression model, BMIr and BMIa would be perfectly collinear. The threat of multicollinearity when jointly modeling absolute and relative rank within a distribution is also apparent in research that seeks to estimate the independent contributions of relative and absolute income to personal well-being (Verme, 2013). Of course, research that relies solely on measures of BMIa to draw conclusions about the psychological and physiologic consequences of the stigmatization of larger body sizes due to greater adiposity, or otherwise test social-psychological theories of the consequences of larger body size, is unable to distinguish between BMIa and the associations or effects of BMIr. Similarly, research relying solely on measures of BMIr is unable to control for the associations or effect of BMIa. As noted by Kim, Makowski, and vondemKnesebeck (2019), "controlling for absolute body weight is critical because it allows us to compare those who have the same weight but different ranks due to exposure to the different BMI distributions of each reference group” [13].
Given a general lack of research on the health consequences of BMIr, Kim et al. (2019) operationalized rBMI as ordinal rank within a defined reference group, finding that individuals in a higher BMI decile-defined group (within a demographic reference group defined by 10-year age groups, county of residence, and gender) reported lower life satisfaction scores, on average, than did those in a lower BMI decile-defined group [13]. While a higher BMIr was negatively associated with life satisfaction for both men and women, the results also suggested the importance of considering race in constructing reference groups. Kim et al. (2019) hypothesized that a high BMI relative to one's social reference group might influence life satisfaction through both the comparative and normative functions of reference groups. Individuals who perceive themselves to be comparatively heavier than others might experience more negative emotions about their weight and be subject to social sanctions associated with a high relative BMI, including discrimination. Consistent with discrimination as one mechanism through which individuals with a high relative BMI are subjected to social sanctions, Janssen et al. (Janssen & Fahr, 2014) found that deviations from the median BMI of one's peer group are associated with reduced wages, independent of deviations from “an optimal BMI in a clinical sense,” akin to the concept of absolute BMI we use here.
In sum, a growing body of evidence documents the psychological and physiologic consequences of stigmatization, and recent research has operationalized BMIr as an indicator of the social experience of overweight and obesity. Acknowledging that BMIr may indicate more than social experiences (e.g., variation in lean body mass), we build upon this research by testing the hypothesis that a positive deviation from the reference group mean BMI (i.e., a higher BMIr) will incur the deleterious consequences of obesity's stigmatization and will thus be associated with an increased MR, independent of the association between BMIa and MR. A better understanding of the association between BMIr and MR independent of BMIa will provide insight into the adverse health effects of discrimination against individuals with obesity and the potential health risks associated with other stigmatized conditions.
2. Methods
2.1. Data
Data come from three nationally representative datasets: the 1992–2014 waves of the Health and Retirement Study (HRS, n = 31,115), the 1997–2014 waves National Health Interview Survey (NHIS, n = 529,362), and the 1990–2014 waves of the National Health and Nutrition Examination Survey (NHANES, n = 45,033) (Lynn A. Blewett, Julia A. Rivera Drew, Miriam L. King, & Kari C.W. Williams, 2019). The Health and Retirement assesses the economic, health, marital, and family status of the US population over 50 on a biennial schedule and is sponsored by the National Institute of Aging (grant number NIA U01AG009740). The final year of follow-up for each study (2014) was the last year NHIS and NHANES respondents could be linked to the National Death Index (NDI) at the time of the analysis. Both the NHIS and NHANES are repeated cross-sectional studies of the US population that collect demographics, health information, and numerous other measures from the US population on an annual basis. We used the IPUMS NHIS dataset to download harmonized NHIS data between 1997 and 2014 (Lynn A. Blewett, Rivera Drew, King, & Williams, 2019). These three datasets were selected because of their representativeness of the US population, large sample sizes in anticipation of high multicollinearity between relative BMI and absolute BMI, and availability of information on respondent mortality. We extracted measures of BMI, sex, age, race, educational attainment, smoking status, and MR from each of the three studies, as summarized below.
2.2. Survival time and MR
For participants from the HRS, we calculated the survival times of right-censored observations using the baseline age accompanying the first observation of BMI and attained age, calculated as the age of respondents at the end of their interview in the 2014 wave of the HRS. We calculated the survival times of individuals who died during the study period by using the baseline age accompanying the first observation of BMI and age at death. Respondent MR was ascertained using the variable R12IWSTAT, a derived variable indicating MR status in the RAND HRS Longitudinal File 2014 (RAND, 2013), a cleaned and processed version of the raw data with consistent naming of variables across waves and imputations for key variables often missing in the raw data, and funded by the National Institute on Aging and the Social Security Administration. For participants from the NHIS, we calculated survival times of right-censored observations by using the year of study entry and attained age, calculated as the age of respondents through December 31, 2015. We calculated the survival times of individuals who died during the study period by using the year of study entry and year of death. Respondent MR was ascertained using the NHIS variable MORTDODY, which is available for all persons aged ≥18 years included in the NHIS during survey years 1986–2014 who provided sufficient data for linkage to the National Death Index (NDI). To help account for differences in participants based on the availability of data linkage, we weighted observations from the NHIS using an eligibility-adjusted weight variable (MORTWT) developed by the National Center for Health Statistics. For NHANES participants, we calculated survival times by using the number of person-months of follow-up from the NHANES interview date. Respondent follow-up times and MR were ascertained via the NHANES public use linked MR files via the variable MORTSTAT (National Center for Health Statistics, 2015 2015). All analyses accounted for complex survey design.
2.3. BMI
We calculated BMI from self-reported height and weight for HRS and NHIS observations and from objectively measured height and weight for NHANES observations.
2.4. Demographics and smoking
We included age, smoking status, and educational attainment in the analyses. We did not include other variables believed to lie on the causal path between exposure to BMI and MR, such as blood pressure, serum lipids, and glucose tolerance measures. As others have observed (Manson, Stampfer, Hennekens, & Willett, 1987; Sjostrom, 1992), controlling for such variables is inappropriate “over-control” that may remove the effect one is studying. Across all three studies in the pooled dataset, age is measured (in years). Ordinal rank BMI was calculated within one's reference group jointly defined using age (2 levels), race or ethnicity (4 levels), and sex (2 levels).
2.5. Absolute BMI and relative BMI
We refer to observed BMI calculated from height and weight as absolute BMI. We calculated BMIr by first defining social reference groups based on age, sex, and race. To define the social reference groups, the continuous variable, age, was categorized into six groups: (<30), (30, 39), (40, 49), (50, 59), (60, 69), and >70 years old. Because sex is, practically speaking, a two-level factor (i.e., male or female) and race is a four-level factor (i.e., Hispanic, non-Hispanic White, non-Hispanic Black, and other), there were 48 reference groups (= 6*2*4). Similar to Kim's (2021) approach, we defined relative BMI as the respondents' ordinal BMI rank, computed as their percentile in the BMI distribution of the reference group. Thus, relative BMI was defined as a 10-level factor, representing the ten bins created by cutting the distribution at the nine decile points of the local distribution.
2.6. Survey-weighted proportional hazards model
We used survey-weighted proportional hazards models (Lumley, 2010) to jointly analyze the associations between MR, BMIa, and BMIr, adjusting for age, race, sex, smoking, and education. We used natural cubic splines to model possible non-linear relationships between BMI, age, and MR. The proportional hazards model for jointly analyzing absolute BMI and relative BMI can be expressed as:
| h(t | data) = h0(t) exp[ Zα + bmi.r β + s1(bmi) + s2(age)] |
where h0(t) is a common baseline hazard function of arbitrary form; Z consists of two binary covariates, sex and education, and two dummy variables, race and smoking status, and the vector α represents their coefficients; bmi.r is the relative BMI, a 10-level factor as defined above, and β is the vector of coefficients of bmi.r; and s1(bmi) and s2(age) are natural cubic splines for the continuous predictors, bmi and age, respectively. A natural cubic spline is a linear combination of basic functions, i.e., s(x) = b(x) r, where r is a vector of K coefficients with K being the degree of freedom, and b(x) is the design matrix of the basis functions. We used the R package splines to generate the design matrix. The expression, Zα + bmi.r β + s1(bmi) + s2(age), represents the log hazard ratio (log HR).
The complex survey design was incorporated into the model fitting procedure to account for the reduction in variance from stratified sampling and the increase in variance from having only a small number of clusters (Lumley, 2010). We used the package survey to estimate the model described above and to summarize results. The degrees of freedom of the natural cubic splines in the above model were set to be 10, the default value in the commonly used package mgcv (Wood, 2017) for analyzing generalized additive models. As a supplement to our analyses reported herein, we estimated models without race and sex covariates, as their inclusion may induce multicollinearity between absolute BMI and relative BMI, rendering parameter estimates unstable and/or inflating estimated variance given that relative BMI was defined as BMI within age, race, and sex groupings (Verme, 2013). Finally, we compared models with and without BMIr to determine whether the inclusion of BMIr as a covariate improved overall model fit.
3. Results
The demographic characteristics of the sample stratified by dataset are described in Table 1, where the values for the continuous predictors, survival time, BMI, and age, are the mean, 2.5%, and 97.5% quantiles. Across the three studies, the mean BMI was 27.3 kg/m2 (NHIS), 28.5 kg/m2 (NHANES) and 27.4 kg/m2 (HRS). The average sample age ranged from 47.4 years (NHIS) to 60.7 years (HRS), with the majority of respondents in each survey being female, non-Hispanic White, with at least a high school education.
Table 1.
Descriptive statistics.
| NHIS | NHANES | HRS | |
|---|---|---|---|
| Total Sample Size | 529,362 | 45,033 | 31,115 |
| Mean Survival Time (years) | 9.6 (2.0, 18.0) | 8.1 (1.6, 15.8) | 10.6 (0.5, 21.8) |
| Mortality Status (%) | |||
| Alive | 87.6 | 87.6 | 61.0 |
| Dead | 12.4 | 12.4 | 39.0 |
| Sex (%) | |||
| Female | 56.0 | 52.7 | 54.9 |
| Male | 44.0 | 48.3 | 46.1 |
| Age (years) | 47.4 | 47.4 | 60.7 |
| Race/Ethnicity (%) | |||
| Hispanic | 17.0 | 26.3 | 10.4 |
| Non-Hispanic White | 63.4 | 45.3 | 68.6 |
| Non-Hispanic Black | 14.5 | 21.6 | 18.2 |
| Other | 5.1 | 6.7 | 2.7 |
| Education (%) | |||
| Less than High School | 16.3 | 29.9 | 27.3 |
| High School or More | 83.6 | 70.0 | 72.7 |
| Smoking Status (%) | |||
| Never | 56.8 | 53.8 | 41.4 |
| Former | 22.1 | 24.8 | 37.4 |
| Current | 21.1 | 21.4 | 21.2 |
| BMIa | 27.3 (19.7,38.4) | 28.5 (19.8, 40.9) | 27.4 (20.0, 37.6) |
Note. Values for survival time, BMI, and age are the mean(2.5, 97.5 quantiles). HRS, Health and Retirement Study; NHIS, National Health Interview Survey; NHANES, National Health and Nutrition Examination Survey; BMIa, absolute body mass index.
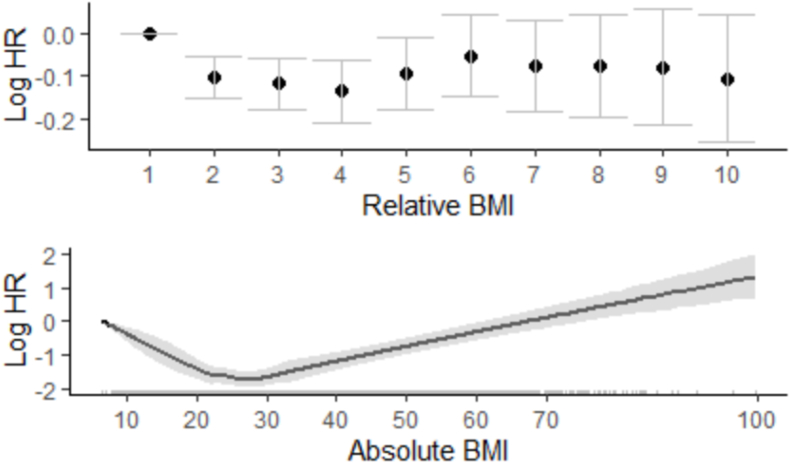
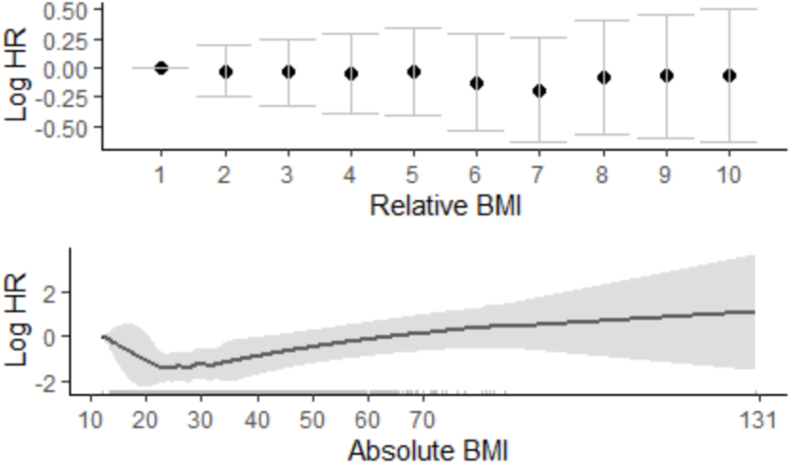
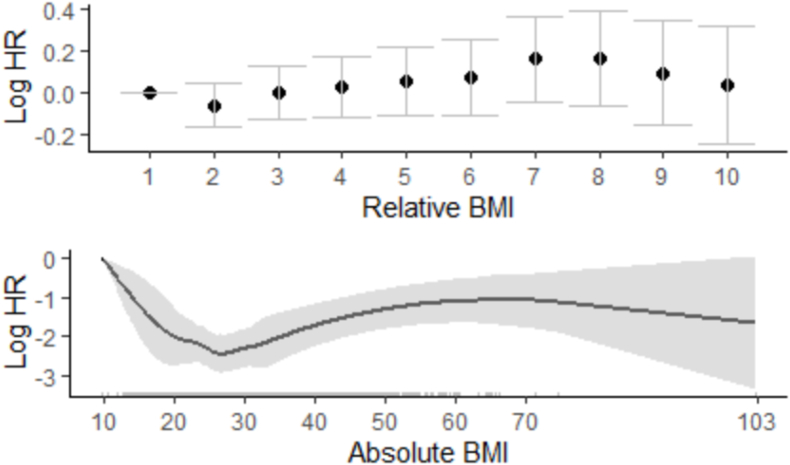
Table 2 summarizes the parametric components of the fitted models for each of the three datasets (i.e., Zα and bmi.r β), including the estimates of the parametric linear effects, their standard error, and p-values for testing the hypotheses αj = 0 and βj = 0. Although the individual coefficients in the natural cubic splines s1(bmi) and s2(age) were estimated, Table 2 does not present these estimates because they are not interpretable separately; instead, Fig. 1, Fig. 2, Fig. 3 visually display the marginal estimates of MR by absolute and relative BMI, demonstrating the non-monotonic relationship between BMI and MR.
Table 2.
Estimates of parametric effects in the survey-weighted Cox proportional hazards models.
| Variable | NHIS |
NHANES |
HRS |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | se | p-value | Estimate | se | p-value | Estimate | se | p-value | |
| Male | 0.37 | 0.01 | <0.0001 | 0.43 | 0.04 | <0.0001 | 0.35 | 0.02 | <0.0001 |
| Race/Ethnicity | |||||||||
| Non-Hispanic White (ref) | – | – | – | – | – | – | – | – | – |
| Hispanic | 0.01 | 0.02 | 0.6233 | 0.19 | 0.12 | 0.1727 | −0.15 | 0.05 | 0.0024 |
| Non-Hispanic Black | 0.17 | 0.02 | <0.0001 | 0.10 | 0.11 | 0.4870 | 0.17 | 0.03 | <0.0001 |
| Other | −0.06 | 0.03 | 0.0911 | 0.24 | 0.12 | 0.1143 | −0.03 | 0.07 | 0.0656 |
| Education | |||||||||
| High School or Higher (ref) | – | – | – | – | – | – | – | – | – |
| Less than High School | 0.32 | 0.01 | <0.0001 | 0.33 | 0.04 | <0.0001 | 0.25 | 0.02 | <0.0001 |
| Smoking Status | |||||||||
| Never (ref) | – | – | – | – | – | – | – | – | – |
| Former | 0.28 | 0.01 | <0.0001 | 0.23 | 0.04 | <0.0001 | 0.24 | 0.02 | <0.0001 |
| Current | 0.84 | 0.01 | <0.0001 | 0.87 | 0.05 | <0.0001 | 0.85 | 0.03 | <0.0001 |
| BMIr Decile-defined group | |||||||||
| 1 | – | – | – | – | – | – | – | – | – |
| 2 | −0.10 | 0.02 | 0.0002 | −0.03 | 0.11 | 0.8088 | −0.06 | 0.05 | 0.3293 |
| 3 | −0.12 | 0.03 | 0.0006 | −0.04 | 0.14 | 0.8079 | −0.00 | 0.06 | 0.9849 |
| 4 | −0.14 | 0.04 | 0.0012 | −0.05 | 0.17 | 0.7925 | 0.03 | 0.07 | 0.7288 |
| 5 | −0.09 | 0.04 | 0.0512 | −0.04 | 0.19 | 0.8640 | 0.05 | 0.08 | 0.5579 |
| 6 | −0.05 | 0.05 | 0.3177 | −0.12 | 0.21 | 0.5552 | 0.07 | 0.09 | 0.4940 |
| 7 | −0.08 | 0.05 | 0.1990 | 0.19 | 0.23 | 0.4075 | 0.16 | 0.10 | 0.1603 |
| 8 | −0.08 | 0.06 | 0.2516 | −0.09 | 0.24 | 0.7435 | 0.16 | 0.11 | 0.1406 |
| 9 | −0.08 | 0.07 | 0.2877 | −0.07 | 0.26 | 0.7960 | 0.09 | 0.12 | 0.4724 |
| 10 | −0.11 | 0.07 | 0.2055 | −0.07 | 0.28 | 0.8181 | 0.03 | 0.14 | 0.8367 |
| N | 529,362 | 45,033 | 31,115 | ||||||
Note. HRS, Health and Retirement Study; NHIS, National Health Interview Survey; NHANES, National Health and Nutrition Examination Survey; BMIa, absolute body mass index.
Fig. 1.
NHIS data. The top plot shows the estimates (points) and 95% intervals (bars) of the effects of relative BMI. The numbers (1–10) on the x-axis represent the levels of BMI, with lower (higher) levels representing lower (higher) BMI. The bottom plot shows the estimated splines (black curve) and 95% pointwise confidence intervals (shaded region) of absolute BMI. The tick marks on the x-axis indicate the observed values of BMI.
Fig. 2.
NHANES data. The top plot shows the estimates (points) and 95% intervals (bars) of the effects of relative BMI. The numbers (1–10) on the x-axis represent relative BMI deciles, with lower (higher) levels representing lower (higher) BMI. The bottom plot shows the estimated splines (black curve) and 95% pointwise confidence intervals (shaded region) of absolute BMI. The tick marks on the x-axis indicate the observed values of BMI.
Fig. 3.
HRS data. The top plot shows the estimates (points) and 95% intervals (bars) of the effects of relative BMI. The numbers (1–10) on the x-axis represent relative BMI deciles, with lower (higher) levels representing lower (higher) BMI. The bottom plot shows the estimated splines (black curve) and 95% pointwise confidence intervals (shaded region) of absolute BMI. The tick marks on the x-axis indicate the observed values of BMI.
Results from the NHANES and HRS indicated that relative BMI decile was not associated with MR; however, results NHIS indicated that individuals in the second through fourth deciles of BMI had a significantly lower MR compared to individuals in the lowest relative BMI decile, whereas individuals in the fifth through tenth deciles did not have a statistically significant higher MR. Thus, only in the NHIS was there an association between relative BMI decile and mortality, and in a direction opposite of what was hypothesized. Results also indicated that those with less than a high school education, and current or former smokers, had a higher hazard of MR than those with a high school education or more and never smokers, respectively. Most of the coefficients in the splines s1(bmi) and s2(age) were estimated to be significantly nonzero, indicating that BMIa had a significant non-linear association with MR. Fig. 1, Fig. 2, Fig. 3 display the estimated effects of relative and absolute BMI using the NHIS, NHANES, and HRS datasets, respectively. The top panel of Fig. 1 plots the marginal effects of BMI ordinal rank as estimated by using NHIS data and indicates that the lowest decile-defined group of the percentile BMI rank had the highest hazard ratio. The bottom panel of Fig. 1 plots the marginal effects of absolute BMI, indicating that individuals with a BMI of approximately 27 kg/m2 had the lowest hazard of MR. As expected, owing to sparse data, the confidence interval for the estimated marginal effect with high BMI was wider. The top panel of Fig. 2 plots the marginal effects of BMI ordinal rank as estimated using NHANES, indicating a similar MR across all deciles of relative BMI. As in the NHANES data, the bottom panel of Fig. 2 suggests that individuals with a BMI of approximately 25 kg/m2 had the lowest hazard of MR. Finally, Fig. 3 plots the marginal effects of BMI ordinal rank as estimated using the HRS, suggesting a similar MR across deciles of relative BMI, consistent with findings from NHANES. The bottom panel of Fig. 3 suggests that individuals with a BMI of approximately 26 kg/m2 had the lowest hazard of MR. Finally, we assessed whether the inclusion of BMIr as a covariate improved model fit using AIC. The AIC for the models with or without the relative BMI were 261400.2 and 264291.4 for HRS, 100451.7 and 100665.9 for NHANES, 1262544 and 1263551 for NHIS, respectively, providing evidence that including BMIr as a covariate improved model fit. Finally, Supplemental Table 1 and Supplemental Figs. 1–3 present results from models that do not include race and sex as covariates. Including race and sex in models estimating the association between relative BMI (defined as ranking within one's age, race, and sex group) increases multicollinearity between absolute and relative BMI; nonetheless, not including them as covariates would likely lead to omitted variable bias. We thus present results from models without their inclusion in supplemental materials.
4. Discussion
Scientific analyses of the relationship between obesity and MR extend back more than a century (Dublin & Marks, 1951; Rogers, 1901), and debate about the strength and nature of the relationship continues to the present (Hughes, 2013; Stefan, Schick, & Häring, 2017). Notably, much of this research has focused on the physiologic consequences of obesity per se on the health and MR of individuals. Yet, given growing evidence that the experience of discrimination can harm the health of individuals, and the status of obesity as a highly stigmatized condition, this research tested whether a high BMI relative to one's age, sex, and racial/ethnic group was associated with an increased rate of MR, independent of one's absolute BMI. Contrary to our hypotheses that a higher relative BMI would be associated with an increased rate of MR, a higher relative BMI was not associated with an increased MR. Our findings contrast with recent research using an ordinal rank approach to operationalize BMIr. In an analysis of the relationship between BMIr and life satisfaction, Kim et al. (J. Kim, 2021) found evidence that individuals with a higher decile-defined BMIr reported lower life satisfaction relative to individuals in the fifth decile-defined group, although the magnitude of the association and statistical significance of different BMIr decile-defined groups was sensitive to the specification of reference groups. In particular, Kim et al. found race/ethnicity to be a “crucial element in defining a reference group for weight comparison” for women, but not for men (J. Kim, 2021). These findings underscore the importance of how social reference groups are constructed and that conclusions about the effects of BMIr on health outcomes may be sensitive to the construction of reference groups.
One notable difference between the research presented herein and that of Kim et al. in the construction of social reference groups for calculating BMIr is Kim et al.'s use of county of residence to define reference groups; that is, BMI deciles were calculated for individuals within age group–sex–race/ethnicity and county. The present analysis did not account for county of residence when defining social reference groups owing to a lack of data; this may be an important limitation given evidence that county-level BMI distributions influence individual-level weight perceptions. For example, Wedow et al. (Wedow, Masters, Mollborn, Schnabel, & Boardman, 2018) found that county-level weight norms influence adolescents' perceptions of their own weight status, with those residing in counties with a heavier weight norm being less likely to perceive themselves as being overweight relative to those residing in counties with a lighter weight norm, independent of actual BMI. Wedow et al.'s use of perceived (self-reported) weight status relative to one's peers, rather than a more objective indicator of relative BMI (e.g., BMI decile), has the benefit of avoiding the problem of perfect collinearity between BMIa and BMIr. Finally, Wedow at al. [26] found that the influence of county-level weight norms appeared to be stronger for women than men, again indicating the importance of adequately defining social reference groups. Given the potential influence of county-level weight norms on self-perception of weight status, and that both internalized and perceived stigmatization of obesity are associated with significant adverse psychological and physiologic health outcomes (Alimoradi et al., 2020; Panza et al., 2019), the present analysis may underestimate the potential influence of BMIr on the rate of MR. Nonetheless, recent research that examined deviations from community mean BMI indicated absolute (i.e., personal) BMI was a stronger predictor of weight-related perceptions and satisfaction (Feng & Wilson, 2022). Research that seeks to understand the potential health consequences of weight discrimination per se may be better suited by using more direct measures of discrimination (e.g., self-reported measures of discrimination) rather than a measure of relative BMI, which only indirectly captures possible weight discrimination while introducing the added complexity of jointly modeling both relative and absolute BMI in statistical models. Nonetheless, there are advantages to using relative BMI as an indicator of potential weight-based discrimination. First, the threat of instrument reactivity is reduced, as it does not require investigators to directly query respondents about past weight-based discrimination, which may lead respondents to the conclusion that previous experiences of discrimination were due to weight. Similarly, directly querying respondents about improvements in their quality of life as a result of weight change might create the impression that weight loss should, in fact, lead to a better quality of life and thereby altering respondent perceptions (e.g., The Impact of Weight on Quality of Life Scale (Kolotkin & Crosby, 2002)). Second, asking individuals about past instances of weight-based discrimination may ask “more than we can know”, drawing from Nisbett and Wilson's (1977) critique on verbal reports of mental processes, as individuals may be unaware that they were discriminated against, or mistakenly believe that they were discriminated against because of their weight (Nisbett & Wilson, 1977). Another strength of this research relative to previous literature examining the influence of relative BMI on health is the use of longitudinal data. The average survival time from observed BMI was 10.60 years (ranging from 1.83 to 22.99 years); thus, while factors that confound the relationship between BMIr and MR cannot be ruled out owing to the observational design, our findings are less susceptible to the risk of immediate reverse causality, as might be the case in research investigating self-reported outcomes (e.g., life satisfaction) contemporaneous with measures of BMI. Still, illness-related weight loss may confound the estimated relationship between BMI and rate of MR in longitudinal studies, although this bias appears to be small and methods used to account for illness-related weight loss may themselves introduce bias (Flegal, Graubard, Williamson, & Cooper, 2011).
Regarding the findings for absolute BMI, BMI is a strong predictor of overall MR both above and below the apparent optimum of about 22.5–25 kg/m2 (Prospective Studies Collaboration et al., 2009). BMI has a J-shaped curve relationship (for both males and females) such that among those with a BMI>25, the higher the BMI, the higher the yearly deaths per 1000 cases of all-cause MR. Also, median survival time may be reduced by about 8–10 years in those categorized as having Class III obesity (BMI ≥40). While the “J-shaped” or “U-shaped” association between BMI and MR is well-known, such that individuals who are underweight have an increased rate of MR (Cao, Moineddin, Urquia, Razak, & Ray, 2014), the present analyses included statistical adjustment for BMIa, accounting for underlying health conditions (and other factors) associated with being underweight that might increase the mortality hazard. Regarding the unexpected finding that in the NHIS, ordinal rank BMI in the second, third, or fourth deciles was associated with a reduced MR relative to the lowest decile, it may be that adjusting for BMIa in our analyses did not fully account for the health risks associated with being underweight, nor the selection of unhealthy individuals into the underweight BMI category. Another possibility discussed below is the problem of multicollinearity. Finally, another limitation of this research, though perhaps a necessary one to address collinearity between BMIr and BMIa, is the coarse categorization of individuals into decile-defined groups based on their exact value of BMIr. While coarse categorization appears to sufficiently address collinearity such that joint estimation of BMIa and BMIr is possible, it may merely disguise the collinearity.
4.1. Intertwined statistical and conceptual issues
Testing the conceptual hypothesis that relative BMI (that is, the degree to which one's, individual BMI deviates from the norm of one's reference group) is a contributor to the hypothesized negative health effects of stigma, in addition to, or more strongly than the association or effects of absolute BMI on MR presents several challenges. The first is conceptual. Because the concept of relative BMI is subjective, there is no intrinsic a priori scaling that is definitively correct. Apart from the perhaps reasonable presumption that above and below the mean or median BMI, the relationship between perceived deviation and stigma will be monotonic with actual BMI, the shape of those monotonic relations on either side of an absolute BMI reference point are unknown. Therefore, any monotonic transformation of relative BMI might be reasonable, yet the choice of transformation is open to question. The second challenge is distinguishing the introduction of measurement error from a transformation that preserves monotonicity, reduces collinearity, and is conceptually sound. For example, in the present research, we used a rank transformation in this paper, following the work of Kim (J. Kim, 2021). This reduces the collinearity (although only very modestly) but whether it does so by introducing additional measurement error into the variable via coarse categorization or whether it more accurately captures the underlying construct of interest is unknown, and these two possibilities are not mutually exclusive.
In terms of how the hypothesis test is statistically established, one can ask whether relative BMI is associated with MR after controlling for absolute BMI; whether the strength of the association between relative BMI and MR is greater than the strength of the association between absolute BMI and MR when strength of association is quantified in terms of slopes; whether the strength of the relation between absolute BMI and MR is reduced when controlling for relative BMI (i.e, Clogg's test of collapsibility); or whether the strength of the association between relative BMI and MR is greater than the strength of the association between absolute BMI and MR when strength of association is quantified in terms of predictive ability or “variance explained."
Such questions can be addressed by modeling both relative BMI and absolute BMI together in a single model, by testing for interaction effects between absolute BMI and the reference norms which define relative BMI, by testing for differences in coefficients when both relative BMI and absolute BMI are included in the same model (In a generalized variant of the method described by Neter in Section 7.3), and by comparing the predictive ability of non-nested models as, for example, described here (Neter, Wasserman, & Kutner, 1989). All of this is made more complicated by the extraordinary degree of collinearity between relative BMI and absolute BMI, which, though we were able to reduce by using subgroup-defined relative BMI, multiple cohorts, and non-linear estimates of the association between absolute BMI and MR, remains high.
A second challenge is the marked nonlinearity in the association between BMI, and likely relative BMI as well, with MR necessitating models that do not readily permit characterization of that relationship by a single coefficient that can be compared to a single coefficient for a different variable or a different model. We have tested and utilized one set of approaches herein, but we believe that other approaches merit use in future research and that methodologic research on how to best address these questions is also warranted.
5. Conclusion
Finally, it is important to reiterate that explicit discrimination is not the sole means by which social identity threat occurs. Steele et al. (Steele et al., 2002) propose that social identity threat is “aroused by any cue relevant to the evaluative jeopardy of people with a given social identity”, including minority status in a given setting, the cultural centeredness of an identity other than one's own, and ambiguous criteria for evaluation and upward progression in a given setting.” Thus, threat to the social identity of individuals with a high BMIr may be frequently aroused if they often find themselves in settings in which they appear to have a higher BMI than others, are consistently exposed to cues that smaller body sizes are normative or are employed in settings where the evaluative criteria of one's performance are sufficiently vague as to arouse concern that one's body size is a barrier to advancement. Given that the dominant ideal body type in Western countries remains a “slim and toned physique” (Aniulis, Sharp, & Thomas, 2021), US adults with a high BMIr likely find themselves in settings that frequently arouse social identity threat, though we did not find evidence that a high BMIr ultimately leads to an increased MR.
Funding
Supported in part by NIH grants R01AG057703. The opinions expressed are those of the authors and do not necessarily represent those of the NIH or any other organization.
Ethics statement
This research uses publicly available data derived from the Health and Retirement Study, the National Health and Nutrition Examination Survey, and the National Health Interview Survey. This research did not involve merging any of the data sets in such a way that individuals might be identified nor did the research enhance the public data set with identifiable, or potentially identifiable data. Accordingly, the University of Alabama at Birmingham ORIB has determined that research involving these datasets does not meet the regulatory criteria for human subjects research.
Author statement
Gregory Pavela: Writing-Original Draft, Funding Acquisition, Data curation, Project administration, Nengjun Yi: Formal analysis, Writing- Review and Editing, Visualization. Luis Mestre: Writing- Review and Editing, Validation. Stella Lartey: Writing- Review and Editing: Pengcheng Xun: Data curation, Writing- Review and Editing. David B. Allison: Writing- Reviewing and Editing, Supervision, Conceptualization, Funding Acquisition.
Declaration of competing interest
Greg Pavela Declarations of interest: none; Nengjun Yi Declarations of interest: none; Luis Mestre Declarations of interest: none; Stella Lartey Declarations of interest: none; Pengcheng Xun Declarations of interest: Dr. Xun was an employee and shareholder of Atara Biotherapeutics Inc. at submission. David B. Allison Declarations of interest: In the last thirty-six months, Dr. Allison has received personal payments or promises for same from: Alkermes, Inc.; Amin, Talati, Wasserman for KSF Acquisition Corporation (Glanbia); Big Sky Health, Inc.; Biofortis Innovation Services (Merieux NutriSciences); California Walnut Commission; Clark Hill PLC; Kaleido Biosciences; Law Offices of Ronald Marron; Medpace/Gelesis; Nestec/Nestle; Novo Nordisk Foundation; Schiff Hardin LLP; Sports Research Corp.; and Tomasik, Kotin& Kasserman, LLC. Donations to a foundation have been made on his behalf by the Northarvest Bean Growers Association/Communique. Dr. Allison's institution, Indiana University, and the Indiana University Foundation have received funds or donations to support his research or educational activities from: Alliance for Potato Research and Education; American Egg Board; California Walnut Commission; Dairy Management Inc.; Eli Lilly and Co.; Herbalife International; National Cattlemen's Beef Association; Reckitt Bencksier Group, PLC (a division of Mead Johnson Nutrition); Soleno Therapeutics; and numerous other for-profit and non-profit organizations to support the work of the School of Public Health and the university more broadly.
Footnotes
The words risk and rate are sometimes used interchangeably and inconsistently but herein we use risk to refer to the probability of an event in a defined and finite period or interval of time and rate to be the tangent to the survival distribution (Centers for Disease Control and Prevention, 2012).
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2022.101200.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
The authors do not have permission to share data.
References
- Alimoradi Z., Golboni F., Griffiths M.D., Broström A., Lin C.Y., Pakpour A.H. Weight-related stigma and psychological distress: A systematic review and meta-analysis. Clinical Nutrition. 2020;39(7):2001–2013. doi: 10.1016/j.clnu.2019.10.016. [DOI] [PubMed] [Google Scholar]
- Aniulis E., Sharp G., Thomas N.A. The ever-changing ideal: The body you want depends on who else you’re looking at. Body Image. 2021;36:218–229. doi: 10.1016/j.bodyim.2020.12.003. [DOI] [PubMed] [Google Scholar]
- Blewett L.A., Rivera Drew J.A., King M.L., Williams K.C.W. 2019. IPUMS health surveys: National health interview survey.https://nhis.ipums.org/ Version 6.4. Retrieved from. [Google Scholar]
- Burke M.A., Heiland F.W., Nadler C.M. From “overweight” to “about right”: Evidence of a generational shift in body weight norms. Obesity. 2010;18(6):1226–1234. doi: 10.1038/oby.2009.369. [DOI] [PubMed] [Google Scholar]
- Cao S., Moineddin R., Urquia M.L., Razak F., Ray J.G. J-Shapedness: An often missed, often miscalculated relation: The example of weight and mortality. Journal of Epidemiology & Community Health. 2014;68(7):683. doi: 10.1136/jech-2013-203439. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2012. Lesson 3: Measures of risk. Principles of epidemiology in public health practice, third edition an Introduction to applied Epidemiology and biostatistics.https://www.cdc.gov/csels/dsepd/ss1978/lesson3/section2.html 2021. Retrieved from. [Google Scholar]
- Chang V.W., Christakis N.A. Self-perception of weight appropriateness in the United States. American Journal of Preventive Medicine. 2003;24(4):332–339. doi: 10.1016/s0749-3797(03)00020-5. [DOI] [PubMed] [Google Scholar]
- Dublin L.I., Marks H.H. Mortality among insured overweights in recent years. Transactions of the Association of Life Insurance Medical Directors of America. 1951;35:235–266. https://www.ncbi.nlm.nih.gov/pubmed/14922474 Retrieved from. [PubMed] [Google Scholar]
- Feng X., Wilson A. Association between community average body mass index and perception of overweight. Social Science & Medicine. 2022 doi: 10.1016/j.socscimed.2021.114694. [DOI] [PubMed] [Google Scholar]
- Flegal K.M., Graubard B.I., Williamson D.F., Cooper R.S. Reverse causation and illness-related weight loss in observational studies of body weight and mortality. American Journal of Epidemiology. 2011;173(1):1–9. doi: 10.1093/aje/kwq341. [DOI] [PubMed] [Google Scholar]
- Garza R., Heredia R.R., Cieślicka A.B. An eye tracking examination of men's attractiveness by conceptive risk women. Evolutionary Psychology. 2017;15(1) doi: 10.1177/1474704917690741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E. 1963. Stigma: Notes on the management of a spoiled identity. null. [Google Scholar]
- Goffman E. Simon and Schuster; 2009. Stigma: Notes on the management of spoiled identity. [Google Scholar]
- Goosby B.J., Malone S., Richardson E.A., Cheadle J.E., Williams D.T. Perceived discrimination and markers of cardiovascular risk among low-income African American youth. American Journal of Human Biology. 2015;27(4):546–552. doi: 10.1002/ajhb.22683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutin I. Body mass index is just a number: Conflating riskiness and unhealthiness in discourse on body size. Sociology of Health & Illness. 2021;43(6):1437–1453. doi: 10.1111/1467-9566.13309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales C., Md C., Fryar C., Ogden C. 2020. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. . NCHS data brief, no 360.https://www.cdc.gov/nchs/products/databriefs/db360.htm Retrieved from. [PubMed] [Google Scholar]
- Hammond R.A. Social influence and obesity. Current Opinion in Endocrinology Diabetes and Obesity. 2010;17(5):467–471. doi: 10.1097/MED.0b013e32833d4687. [DOI] [PubMed] [Google Scholar]
- Hughes V. The big fat truth. Nature. 2013;497(7450):428–430. doi: 10.1038/497428a. [DOI] [PubMed] [Google Scholar]
- Hunger J.M., Major B., Blodorn A., Miller C.T. Weighed down by stigma: How weight-based social identity threat contributes to weight gain and poor health. Soc Personal Psychol Compass. 2015;9(6):255–268. doi: 10.1111/spc3.12172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen E.A., Fahr R. 2014. The wage effects of social norms-evidence of deviations from peers' body mass in europe. Retrieved from. [Google Scholar]
- Kim J. Assessing the importance of relative body weight in shaping life satisfaction: Evidence from 1 million Americans. Current Psychology. 2021 doi: 10.1007/s12144-021-01360-z. [DOI] [Google Scholar]
- Kim T.J., Makowski A.C., von dem Knesebeck O. Obesity stigma in Germany and the United States – results of population surveys. PLoS One. 2019;14(8) doi: 10.1371/journal.pone.0221214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolotkin R.L., Crosby R.D. Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (IWQOL-Lite) in a community sample. Quality of Life Research. 2002;11(2):157–171. doi: 10.1023/A:1015081805439. [DOI] [PubMed] [Google Scholar]
- Lumley T. John Wiley & Sons; New Jersey: 2010. Complex survey - a guide to analysis using R. [Google Scholar]
- Maddox G.L., Back K.W., Liederman V.R. Overweight as social deviance and disability. Journal of Health and Social Behavior. 1968;9(4):287–298. doi: 10.2307/2948537. [DOI] [PubMed] [Google Scholar]
- Major B., Eliezer D., Rieck H. The psychological weight of weight stigma. Social Psychological and Personality Science. 2012;3(6):651–658. doi: 10.1177/1948550611434400. [DOI] [Google Scholar]
- Manson J.E., Stampfer M.J., Hennekens C.H., Willett W.C. Body weight and longevity. A reassessment. JAMA. 1987;257(3):353–358. https://www.ncbi.nlm.nih.gov/pubmed/3795418 Retrieved from. [PubMed] [Google Scholar]
- Martin M.A., Thomas T., Adler G.J., Kreager D.A. Are feminine body weight norms different for black students or in black schools? Girls' weight-related peer acceptance across racialized school contexts. Journal of Health and Social Behavior. 2020;61(2):239–258. doi: 10.1177/0022146520920599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muennig P. The body politic: The relationship between stigma and obesity-associated disease. BMC Public Health. 2008;8 doi: 10.1186/1471-2458-8-128. 128-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics . 2015. Office of analysis and epidemiology, public-use linked mortality file.https://www.cdc.gov/nchs/data-linkage/mortality-public.htm Retrieved from, 2015. [Google Scholar]
- Neter J., Wasserman W., Kutner M.H. 1989. Applied linear regression models. [Google Scholar]
- Nisbett R.E., Wilson T.D. Telling more than we can know: Verbal reports on mental processes. Psychological Review. 1977;84(3):231–259. doi: 10.1037/0033-295X.84.3.231. [DOI] [Google Scholar]
- Overstreet N.M., Quinn D.M., Agocha V.B. Beyond thinness: The influence of a curvaceous body ideal on body dissatisfaction in black and white women. Sex Roles. 2010;63(1):91–103. doi: 10.1007/s11199-010-9792-4. [DOI] [Google Scholar]
- Panza G.A., Puhl R.M., Taylor B.A., Zaleski A.L., Livingston J., Pescatello L.S. Links between discrimination and cardiovascular health among socially stigmatized groups: A systematic review. PLoS One. 2019;14(6) doi: 10.1371/journal.pone.0217623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl R.M., Heuer C.A. The stigma of obesity: A review and update. Obesity. 2009;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Puhl R.M., Heuer C.A. Obesity stigma: Important considerations for public health. American Journal of Public Health. 2010;100(6):1019–1028. doi: 10.2105/ajph.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rand . RAND center for the study of aging, with funding from the national Institute on aging and the social security administration. 2013. RAND HRS data, version M. Santa Monica, CA. [Google Scholar]
- Rogers O. Build as a factor influencing longevity. Proceedings of the Association of Life Insurance Medical Directors of America (PALIMDA) 12th Annual Meeting. 1901:280–288. [Google Scholar]
- Rubino F., Puhl R.M., Cummings D.E., Eckel R.H., Ryan D.H., Mechanick J.I.…Dixon J.B. Joint international consensus statement for ending stigma of obesity. Nature Medicine. 2020 doi: 10.1038/s41591-020-0803-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saguy A.C., Ward A. Coming out as fat: Rethinking stigma. Social Psychology Quarterly. 2011;74(1):53–75. doi: 10.1177/0190272511398190. [DOI] [Google Scholar]
- Sjostrom L.V. Mortality of severely obese subjects. American Journal of Clinical Nutrition. 1992;55(2 Suppl):516S–523S. doi: 10.1093/ajcn/55.2.516s. https://www.ncbi.nlm.nih.gov/pubmed/1531097 Retrieved from. [DOI] [PubMed] [Google Scholar]
- Steele C.M., Spencer S.J., Aronson J. Contending with group image: The psychology of stereotype and social identity threat. Advances in Experimental Social Psychology. 2002;34:379–440. [Google Scholar]
- Stefan N., Schick F., Häring H.-U. Causes, characteristics, and consequences of metabolically unhealthy normal weight in humans. Cell Metabolism. 2017;26(2):292–300. doi: 10.1016/j.cmet.2017.07.008. [DOI] [PubMed] [Google Scholar]
- Sutin A.R., Stephan Y., Terracciano A. Weight discrimination and risk of mortality. Psychological Science. 2015;26(11):1803–1811. doi: 10.1177/0956797615601103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swami V. 2006. The influence of body weight and shape in determining female and male physical attractiveness. [Google Scholar]
- Swami V. Cultural influences on body size ideals. European Psychologist. 2015;20(1):44–51. doi: 10.1027/1016-9040/a000150. [DOI] [Google Scholar]
- Tomiyama A.J., Carr D., Granberg E.M., Major B., Robinson E., Sutin A.R., et al. How and why weight stigma drives the obesity 'epidemic' and harms health. BMC Medicine. 2018;16(1):123. doi: 10.1186/s12916-018-1116-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verme P. World Bank Policy Research Working Paper(6606); 2013. The relative income and relative deprivation hypotheses: A review of the empirical literature. [Google Scholar]
- Wedow R., Masters R.K., Mollborn S., Schnabel L., Boardman J.D. Body size reference norms and subjective weight status: A gender and life course approach. Social forces; a scientific medium of social study and interpretation. 2018;96(3):1377–1409. doi: 10.1093/sf/sox073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prospective Studies Collaboration. Whitlock G., Lewington S., Sherliker P., Clarke R., Emberson J., al e. Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood S. 2nd ed. CRC Press; 2017. Generalized additive models: An introduction with R. Taylor & Francis Group. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors do not have permission to share data.