Abstract
Rising psychiatric emergency department (ED) presentations pose significant financial and administrative burdens to hospitals. Alternative psychiatric emergency services programs have the potential to alleviate this strain by diverting non-emergent mental health issues from EDs. This study explores one such program, the Boston Emergency Services Team (BEST), a multi-channel psychiatric emergency services provider intended for the publicly insured and uninsured population. BEST provides evaluation and treatment for psychiatric crises through specialized psychiatric EDs, a 24/7 hotline, psychiatric urgent care centers, and mobile crisis units. This retrospective review examines the sociodemographic and clinical characteristics of 225,198 BEST encounters (2005–2016). Of note, the proportion of encounters taking place in ED settings decreased significantly from 70 to 58% across the study period. Findings suggest that multi-focal, psychiatric emergency programs like BEST have the potential to reduce the burden of emergency mental health presentations and improve patient diversion to appropriate psychiatric care.
Keywords: Emergency medicine, Psychiatry, Public health, Mental health
Introduction
Psychiatric ED visits have increased dramatically in North America over the past two decades, among both youth and adult populations (Kalb et al., 2019; Larkin et al., 2005; Pittsenbarger & Mannix, 2014; Santillanes et al., 2020; Weiss et al., 2017). Several factors likely contribute to this, including increased incidence of mental illness (Hellebuyck et al., 2019; Twenge et al., 2019; Williams et al., 2017), decreased availability of acute care (Chun et al., 2015; Geller & Biebel, 2006; Sisti et al., 2015), and shortages of trained mental health professionals (Burke et al., 2013; Geller & Biebel, 2006; Thomas et al., 2009). As a result, emergency departments (EDs) often act as ‘default’ or ‘safety-net’ service providers for patients who have difficulty accessing other forms of mental healthcare (Halmer et al., 2015; Larkin et al., 2005; Weber et al., 2005).
Due to their focus on medical stabilization, EDs often lack the resources needed to appropriately identify and respond to psychiatric problems (Baraff et al., 2006; Chun et al., 2015; Newton et al., 2017; Stone et al., 2012). Fewer than one-third of EDs have mental health specialists available to evaluate patients (Middleton & Burt, 2006; Stone et al., 2012), and fewer than one-third of doctors in emergency medicine receive formal training for psychiatric emergencies (Chun et al., 2015; Lelonek et al., 2018; McMillan et al., 2017; Santucci et al., 2003). Of patients who visit the emergency department for suicidal ideation or self-injury, nearly half do not receive any psychiatric evaluation (Baraff et al., 2006; Bridge et al., 2012; Olfson et al., 2012). In addition, psychiatric ED patients experience long wait times, only to receive care that is more costly, less intense, and less focused on long-term rehabilitation than mental healthcare provided in non-emergency settings (Cooper & Masi, 2007; Dolan & Fein, 2011; Slade et al., 2010).
To address the lack of adequate mental health services in EDs and reduce the financial burden that psychiatric ED visits pose to hospitals, some communities are investing in alternative psychiatric emergency services (PES) programs, such as psychiatric urgent care centers (UCCs), mobile crisis units (MCUs), and crisis stabilization centers (Allen et al., 2002; Kowal et al., 2011; McNeil, 2020; Saxon et al., 2018; Shannahan & Fields, 2016; Substance Abuse & Mental Health Services Administration, 2014; Sunderji et al., 2015). Although there is limited research that examines whether these programs effectively reduce psychiatric ED visits, existing studies suggest that alternative PES have positive benefits for both patients and communities (Saxon et al., 2018; Substance Abuse & Mental Health Services Administration, 2014; Sunderji et al., 2015). Some research indicates that mobile crisis units divert patients from unnecessary inpatient hospitalization and are more effective than traditional PES in connecting patients with outpatient services (Currier et al., 2010; Dyches et al., 2002; Guo et al., 2001; Hugo et al., 2002). Research that describes and evaluates alternative models of emergency psychiatric care may inform the development of PES systems that improve care for patients and relieve the strain that psychiatric presentations pose for EDs.
The Boston Emergency Services Team (BEST) is one such alternative PES program, designed to serve the publicly insured and uninsured population in the Boston metropolitan area. BEST began operating in the mid-1990s; since June 2003, BEST has been managed by Boston Medical Center (BMC), the largest safety-net hospital in New England. BEST receives support from the Massachusetts Behavioral Health Partnership, which manages behavioral health services for over half a million Massachusetts residents covered by Medicaid or the Children’s Health Insurance Program (CHIP). In 2003, BEST consisted of two designated, psychiatric EDs, two psychiatric UCCs, and one mobile crisis unit. Over the next decade, BEST expanded to meet rising community need and by 2016, operated a 24/7 triage hotline, three dedicated psychiatric EDs, three psychiatric UCCs, and two MCUs.
Although BEST has been operating as an alternative PES program for approximately 25 years, little published research has examined the program. The current study is a descriptive investigation of the BEST program and its delivery of PES by multiple modalities. First, we describe and map the range of pathways by which people in psychiatric crisis may access BEST services and highlight the sociodemographic and clinical characteristics of encounters from 2005 to 2016. Second, we explore patient volume across the study period to demonstrate the expansion BEST in relation to local policy changes and healthcare reform at the state and federal levels. Finally, we examine the extent to which BEST expansion was accompanied by an increase in the proportion of encounters occurring at non-ED settings. Specifically, we hypothesize that the proportion of encounters occurring in non-ED settings will increase across the study period, as BEST expanded its model and healthcare reform occurred. The policy implications of the findings are discussed with the intent to inform the development and expansion of programs that will help alleviate the burden that psychiatric issues pose for EDs and healthcare systems.
Methods
We performed a retrospective chart review with electronic health records (EHRs) from the BEST program. BEST maintains its own EHR system for quality improvement and billing purposes. Data are recorded at the time of the encounter; in some cases, data are also entered into EHRs at the hospital or healthcare system where BEST services are provided. We analyzed data from 225,198 BEST acute psychiatric encounters between January 1, 2005 and December 31, 2016. Demographic and clinical characteristics for the full sample, youth encounters, and adult encounters are shown in Table 1. All study procedures were approved by the Boston Medical Center Institutional Review Board.
Table 1.
Overall, youth, and adult BEST encounter characteristics
| Characteristics | Total encounters | Youth encounters (< 21 years) |
Adult encounters (= > 21 years) |
|||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| N | 225,198 | 49,878 | 22.2 | 175,289 | 77.8 | |
| Sex | ||||||
| Male | 128,067 | 56.9 | 26,625 | 53.4 | 101,426 | 57.9 |
| Female | 94,547 | 42.0 | 22,693 | 45.5 | 71,840 | 41.0 |
| Transgender | 2040 | 0.9 | 480 | 1.0 | 1560 | 0.9 |
| Unknown | 544 | 0.2 | 80 | 0.2 | 463 | 0.3 |
| Race | ||||||
| White | 86,725 | 38.5 | 8839 | 17.7 | 77,884 | 44.4 |
| Black | 67,222 | 29.9 | 18,880 | 37.9 | 48,336 | 27.6 |
| Latino | 38,853 | 17.3 | 13,070 | 26.2 | 25,783 | 14.7 |
| Other | 11,313 | 5.0 | 4251 | 8.5 | 7062 | 4.0 |
| Unknown | 21,805 | 9.4 | 4838 | 9.7 | 16,224 | 9.3 |
| Homelessness | 53,269 | 23.7 | 1802 | 3.6 | 51,464 | 29.4 |
| Insurance Use | ||||||
| Public | 195,327 | 86.7 | 47,661 | 95.6 | 147,638 | 84.2 |
| Uninsured | 23,909 | 10.6 | 164 | 0.3 | 23,745 | 13.6 |
| Commercial | 4830 | 2.1 | 1795 | 3.6 | 3035 | 1.7 |
| Unknown | 1132 | 0.5 | 258 | 0.5 | 871 | 0.5 |
| Existing Patient | 157,022 | 69.7 | 30,017 | 60.2 | 127,003 | 72.5 |
| Psychiatric Diagnosis1 | ||||||
| Mood disorders | 123,627 | 54.9 | 21,106 | 42.3 | 102,511 | 58.5 |
| Substance use disorders | 85,428 | 37.9 | 4359 | 8.7 | 81,062 | 46.2 |
| Stress and adjustment disorders | 50,543 | 22.4 | 19,922 | 39.9 | 30,614 | 17.5 |
| Non-mood psychotic disorders | 46,025 | 20.4 | 3056 | 6.1 | 42,962 | 24.5 |
| Personality disorders | 21,379 | 9.5 | 1666 | 3.3 | 19,711 | 11.2 |
| Anxiety disorders | 20,603 | 9.2 | 4460 | 8.9 | 16,134 | 9.2 |
| Childhood onset disorders | 14,041 | 6.2 | 12,641 | 25.3 | 1400 | 0.8 |
| Other psychiatric disorders | 3334 | 1.5 | 634 | 1.3 | 2700 | 1.5 |
| Evaluation Location | ||||||
| BEST-designated ED | 80,581 | 35.8 | 15,171 | 30.4 | 65,390 | 37.3 |
| Other ED | 61,179 | 27.2 | 10,983 | 22.0 | 50,188 | 28.6 |
| Psychiatric UCC | 42,435 | 18.8 | 5020 | 10.1 | 37,415 | 21.3 |
| Community location (MCU) | 40,683 | 18.1 | 18,654 | 37.4 | 22,027 | 12.6 |
| Unknown | 320 | 0.1 | 50 | 0.1 | 269 | 0.2 |
| Discharge Disposition | ||||||
| Inpatient admission | 87,411 | 38.8 | 17,055 | 34.2 | 70,349 | 40.1 |
| Outpatient care | 67,607 | 30.0 | 17,466 | 35.0 | 50,125 | 28.6 |
| Returned to community | 48,512 | 21.5 | 11,179 | 22.4 | 37,327 | 21.3 |
| Crisis stabilization | 21,339 | 9.5 | 4124 | 8.3 | 17,214 | 9.8 |
| Unknown | 329 | 0.2 | 54 | 0.1 | 274 | 0.2 |
1Diagnoses not mutually exclusive
Measures
Sociodemographic Characteristics
Sociodemographic characteristics pulled from the emergency medical record include date of birth, gender (male, female, transgender), race/ethnicity (non-Latino White, non-Latino Black, Latino, other), whether the patient was homeless at the time of each encounter, and the type of health insurance utilized for each encounter (public, commercial, uninsured). This data is generally reported by the patient, the referral source (e.g. family member or friend), or in the case of youth, by the parent or guardian. For treatment purposes within BEST, anyone below the age of 21 at an encounter is considered youth; for consistency, we used this categorization of youth in the study.
The amount missing data (9.4%) for patient race/ethnicity reflects a common issue with EHR data (Cusick et al., 2020; Polubriaginof et al., 2019). This likely resulted from a combination of factors, including patients declining to or being unable to provide this information and clinicians failing to collect or record this information in the context of emergency encounters; the rate of missing race/ethnicity data in our study is lower than rates of missing data from similar EHR datasets used in scientific research (Polubriaginof et al., 2019).
Clinical Characteristics
Psychiatric Diagnoses
Psychiatric diagnoses were identified in the electronic record with International Classification of Disease (ICD) 9th and 10th version codes.(World Health Organization, 1978, 2004) During evaluations, BEST clinicians are prompted to enter up to 2 psychiatric diagnoses into a patient’s chart during each encounter. Psychiatric diagnoses were classified in the following categories: mood disorders; substance related disorders; stress and adjustment disorders; non-mood psychotic disorders; anxiety disorders; child onset disorders (e.g., ADHD, conduct disorders); personality disorders; or other psychiatric disorders.
Evaluation Location
BEST encounters occur in a variety of locations, including a BEST-designated ED, a non-BEST ED, or a BEST psychiatric UCC. In addition, an MCU may conduct an evaluation at a range of locations in the community, including a patient’s home or another private residence, inpatient medical unit, outpatient office, residential program, school, location associated with law enforcement or the court system, or another community location.
Discharge Disposition
After a BEST evaluation, patients may be discharged to the following treatment settings: inpatient treatment (either psychiatric or medical); a community crisis stabilization program (24-h care in an unlocked unit); or outpatient care. When a patient is discharged to outpatient care, an appointment is set up with a new provider within the BEST system or an existing provider that the patient is already connected with. Patients may also be discharged back into the community. BEST clinicians attempt to connect patients with social services, community supports, or other local resources before discharge to the community; for example, clinicians may connect patients with a homeless shelter or place them on a waitlist for care that is not currently available.
Results
Pathways to BEST Care
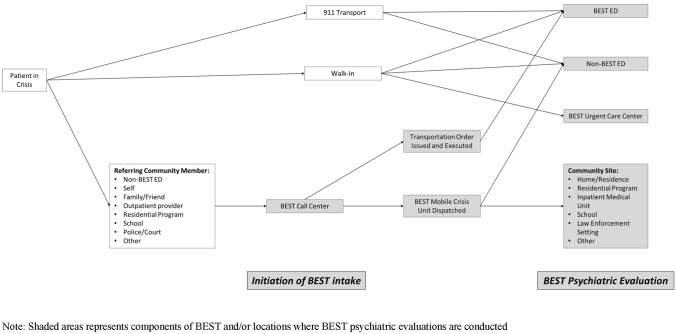
The pathways by which community members receive PES through BEST are illustrated in Fig. 1. Most directly, services are initiated when publicly insured and uninsured patients experiencing psychiatric emergencies walk into a BEST-designated ED or are transported there by emergency medical services. These EDs have staff on-site or on-call 24/7 to perform evaluations. Any member of the community can initiate psychiatric emergency services by contacting BEST through a 24/7 call center which provides initial triage and, if necessary, arranges an evaluation at an appropriate location. A wide range of stakeholders utilize the BEST call center. Healthcare providers at non-designated EDs, inpatient medical units, and outpatient locations refer patients through the call center, which will then dispatch a mobile crisis unit to these locations. Patients or family members also contact the call center, which may dispatch mobile crisis teams, arrange appointments at BEST UCCs, facilitate calls to 911 or emergency medical services, and/or issue involuntary transportations order to BEST-designated EDs. BEST offers the same range of triage and services when law enforcement, schools, homeless shelters, and other community members refer patients through the call center.
Fig. 1.
Pathways to BEST care
After a BEST clinician conducts a psychiatric evaluation, they may initiate one or multiple responses based on their assessments. These responses include: locating an available bed in an inpatient psychiatric unit or crisis stabilization center; facilitating boarding in an appropriate location in a psychiatric bed is needed by not immediately available; referring a patient to outpatient services; connecting a patient with social services or other community resources (e.g. homeless shelters, substance use treatment options. The goal of each BEST encounter is to provide patients treatment for immediate psychiatric needs and connect them with long-term care to support symptom management and recovery.
Sociodemographic and Clinical Characteristics of BEST Encounters
Sociodemographic characteristics for encounters are shown in Table 1. Over three-quarters of BEST encounters were for adults (77.8%). For encounters for which patient race and/or ethnicity was known, over half of encounters were for people of color (80.3% of youth encounters and 51.0% of adult encounters). Almost one-third of adult encounters (29.4%) were for homeless patients. For the overwhelming majority of BEST encounters, patients utilized public insurance (95.6% of youth encounters and 84.2% of adult encounters) or were uninsured (0.3% of youth encounters and 23.6% of adult encounters). Over two-thirds of BEST visits were for patients who had previously received BEST services (60.2% of youth encounters and 72.5% of adult encounters). In fact, the 225,198 encounters included in the study were made by 70,648 unique BEST patients. The mean number of visits per patient across the study period was 3.19 visits (SD = 6.48) and the median number of visits per patient was 1.
The most common psychiatric diagnoses for youth encounters were mood disorders (42.3%), and stress and adjustment disorders (39.9%); For adult encounters, the most common diagnoses were mood disorders (58.5%) and substance use disorders (46.2%). Approximately one-third of encounters took place in a BEST-designated ED (30.4% of youth encounters and 37.3% of adult encounters), and more than one-quarter of encounters took place in a non-BEST ED (27.2% of youth encounters and 28.6% of adult encounters). The remaining visits either took place in psychiatric UCCs (10.1% of youth encounters and 21.3% of adult encounters) or were conducted by an MCU at a community location (37.4% of youth encounters and 12.6% of adult encounters). Over one-third of encounters resulted in admission to inpatient care (34.2% of youth and 40.1% of adults). In addition, almost 10% of patients (8.3% of youth encounters and 9.8% of adult encounters) were admitted to crisis stabilization, which provides 24–7 care in a voluntary, unlocked setting.
Time Trends
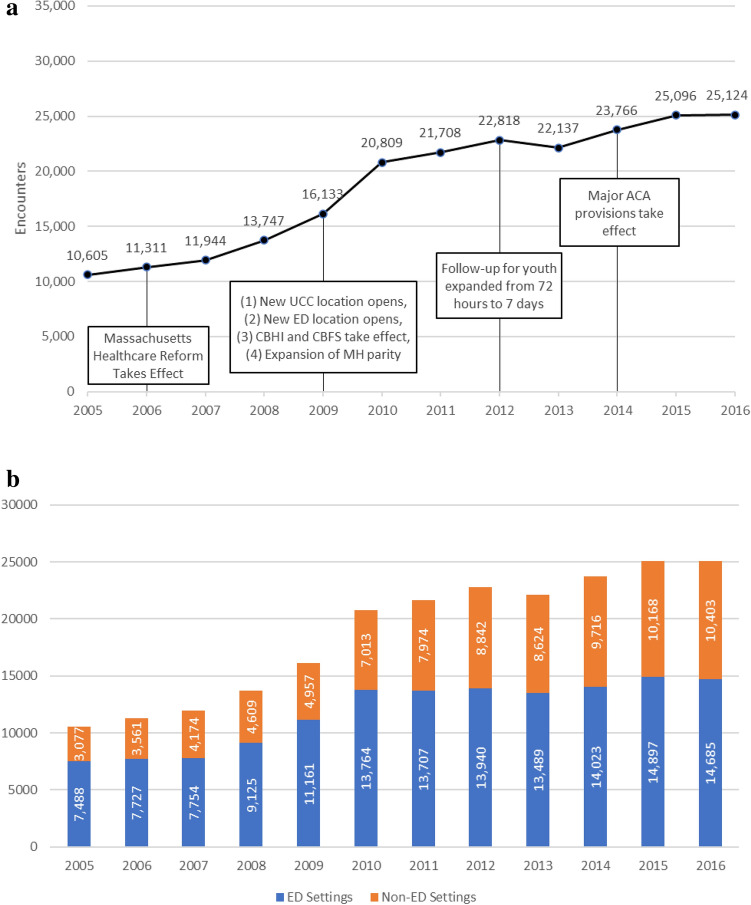
Figure 2a shows BEST encounter volume for each calendar year from 2005 to 2016, along with some of the policy and programmatic changes that may have contributed to changes in volume. BEST encounter volumes grew throughout the study period from 10,605 in 2005 to 25,124 in 2016, an increase of 136.9%. During this time, several health reforms influenced mental health coverage for patients and BEST’s mission. The implementation of Massachusetts healthcare reform in June of 2006 made affordable public health insurance available to uninsured residents (Doonan & Tull, 2010; Massachusetts Legislature, 2006). In 2009, the Children’s Behavioral Health Initiative (CBHI) made behavioral health services such as mobile crisis intervention available to publicly insured patients under the age of 21 (Center for Public Representation, 2008). At the same time, the Massachusetts Department of Mental Health began offering Community Based Flexible Supports (CBFS) to eligible adults, including crisis intervention services (Massachusetts Department of Public Health, 2022). That same year, Massachusetts mental health parity laws expanded to include post-traumatic stress disorder, autism, substance abuse, and eating disorders (Massachusetts Legislature, 2008). All of these changes expanded the ability of BEST to serve the needs of clients with a growing range of behavioral health problems. In 2012, CBHI expanded to cover seven days of follow-up for youth receiving BEST services, an increase from the previous required 72 h. Finally, in 2014, the major provisions of the Affordable Care Act went into effect. Of these changes, the greatest annual increase in BEST volume (29.0%) occurred in 2009–2010, which reflects the opening of new BEST designated EDs and UCCs,
Fig. 2.
a BEST Encounter Volume by Year b BEST Encounter volume by year and evaluation location
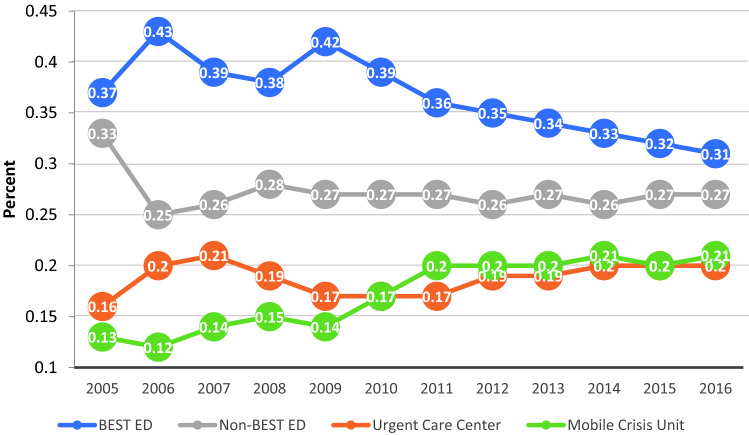
Time Trends and Encounter Location
Figure 2b and Fig. 3 illustrate increases in BEST encounter volume across the study period broken down by encounter location. Although encounter volume rose for both ED locations (BEST-designated and non-BEST EDs) and non-ED locations (psychiatric UCCs and MCU encounters at community locations), there were higher rates of increase at non-ED locations. Specifically, encounters at ED locations rose from 7,488 in 2005 to 14,685 in 2016 (196.2% increase) and encounters at non-ED locations rose from 3,077 in 2005 to 10,402 in 2016.The proportion of encounters occurring at BEST-designated and non-BEST EDs decreased across the study period (70.6% in 2005 to 58.5% in 2016), while the proportion of encounters occurring at psychiatric UCCs and community locations (conducted by MCUs) increased across the study period (29.0% in 2005 to 41.4% in 2016). A two-sample z-test indicated that the proportion of encounters occurring at non-ED locations during the second half of the study (2011–2016; 39.6%) was significantly higher than the proportion of encounters at non-ED locations during the first half of the study (2005–2010; 32.4%), z = − 34.29, p < 0.001.
Fig. 3.
Proportion of BEST encounters by location and year
Discussion
Our data indicates that between 2005 and 2016, BEST served a racially/ethnically diverse population with a wide range of psychiatric disorders who overwhelmingly relied on public insurance or safety-net services to meet their behavioral health needs. Approximately 1 in 5 adults served by BEST were homeless at some point during the study period; this finding is consistent with research documenting the connections between mental health problems, homelessness, and utilization of emergency services (Fazel et al., 2008; Moulin et al., 2018). In response to mental health policy changes, BEST expanded available services offerings beginning in 2009, which was accompanied by a rise in encounter volumes for the remainder of the study period. At the same time, BEST’s efforts to serve patients in non-ED settings paid off, decreasing the proportion of encounters taking place in EDs from 70.6% of encounters in 2005 to 58.5% of encounters in 2016.
Available data on patient race/ethnicity indicates approximately 60% of BEST patients were people of color. This differs from the racial/ ethnic background of the primary communities served by BEST; according to 2010 census information, only 42.5% of the population in the BEST catchment area was non-White (United States Census Bureau, 2021). This difference may reflect a number of issues, including undercounting of people of color in the census (United States Census Bureau, 2012) and racial and ethnic disparities in health insurance coverage (Buchmueller et al., 2016), psychiatric ED utilization (Snowden et al., 2008, 2009), and access to mental health care (Cook et al., 2013, 2016). This suggests that BEST provides critical services for people of color in the Boston metropolitan area.
The critical need for mental health services within the BEST catchment area was demonstrated by the finding that over two-thirds of BEST encounters involved known patients who had previously used BEST services. This finding echoes prior research showing high rates of repeated use of PES (Chaput & Lebel, 2007; Cloutier et al., 2010; LaCalle & Rabin, 2010; Mapelli et al., 2015) and is consistent with scholars’ suggestions that emergency services have become a primary provider for patients who have difficulty accessing other types of mental healthcare (Halmer et al., 2015; Larkin et al., 2005; Weber et al., 2005). The specialized evaluation and treatment provided by BEST is intended to decrease the likelihood of repeat utilization; however, when there are repeat presentations, BEST remains better suited to manage patient needs than an ED.
BEST provided psychiatric evaluation and care to patients at multiple levels of acuity. Close to one-half of BEST clients required intensive intervention, as reflected by their admission to inpatient treatment or voluntary crisis stabilization. The ability of BEST to discharge patients into inpatient or voluntary care is dependent upon the supply of psychiatric beds, and Massachusetts, like many states, has been experiencing a psychiatric bed shortage for over two decades (Fuller et al., 2016); as a result, there may have been additional cases where patients acuity warranted admission to inpatient care or crisis stabilization and clinicians were unable to secure a placement.
Approximately one-quarter of BEST encounters were conducted by BEST MCUs in non-designated EDs, demonstrating that even hospitals not directly affiliated with BEST rely on the program to evaluate and treat psychiatric emergency patients. As an integral component of psychiatric emergency care in the Boston area, the MCUs provide a supplemental workforce when traditional EDs must manage psychiatric crises, which research shows they are not prepared to address (Baraff et al., 2006; Chun et al., 2015; Newton et al., 2017; Stone et al., 2012). Although BEST is an important provider in ED settings, over a third of BEST evaluations during the study period were conducted in non-emergency settings, including BEST-operated psychiatric UCC, patient homes, schools, and shelters. Without the BEST psychiatric UCCs and MCUs, some of these encounters would likely have occurred in EDs. Furthermore, the proportion of ED encounters was almost 10% lower in the second half of the study period than the first. This increase in the proportion of visits occurring in non-ED settings is promising, as it suggests that ED alternatives are accessible to patients who may be experiencing psychiatric issues that are urgent but are not true emergencies. Although MCUs cannot always respond immediately when care is requested, they offer professional mental health services within a few hours and do not involve long wait-times at the ED.
The overall volume within the BEST program more than doubled during the study period, and these increases are consistent with other studies conducted across the U.S. and Canada (Kalb et al., 2019; Larkin et al., 2005; Pittsenbarger & Mannix, 2014; Santillanes et al., 2020; Weiss et al., 2017). Researchers generally agree that these increases are the combined result of increases in the prevalence of psychiatric illness and shortages in the availability of care (Chun et al., 2015; Fuller et al., 2016; Geller & Biebel, 2006; Hellebuyck et al., 2019; Sisti et al., 2015; Thomas et al., 2009; Williams et al., 2017). In order to better understand increases in BEST volume, we looked at more closely at different encounter locations. Our finding that volume at non-ED locations increased at a greater rate than volume at ED locations may be explained by several factors. First, the expansion of BEST in 2009 to include an additional designated ED and psychiatric UCC represents an increased supply of services. Statewide policy changes, specifically the creation of CBHI and CBFS, expanded the availability of mobile crisis intervention services within BEST, also increasing supply. Second, Massachusetts Health Care Reform drastically decreased the uninsured population in Massachusetts (Long, 2008; Pande et al., 2011). Although BEST has always served patients regardless of insurance status, some individuals may have felt more comfortable seeking care through psychiatric UCCs and MCUs after becoming insured. Regardless of the cause, the growth in utilization of non-ED services highlights the potential for alternative PES programs to divert non-emergent cases away from hospital settings.
The current study details the central components of BEST that have established it as an important provider of PES in the metropolitan Boston area. However, our study does have some limitations. First, this study is descriptive and does not evaluate the efficacy of the program. Because this program has been operating in the Boston area for over 2 decades, it may be difficult to isolate and measure its impact. There are also limitations related to the use of EHRs in research. The administrators and providers who collect and record the data in EHRs vary in how they obtain sociodemographic information, their comprehensiveness in documenting clinical information, and their accuracy in medical coding (Spiranovic et al., 2016; Weiskopf & Weng, 2013). Third, our data do not allow us to evaluate the quality of the treatment provided, or to account for other behavioral healthcare that may be accessed by the patient over time (e.g., inpatient or outpatient services or emergency services outside the Boston metropolitan area). Fourth, findings from BEST may not generalize to all populations. Finally, we only examined encounters from 2005 to 2016. Future research should examine more recent patterns in the provision of PES, and particularly how the COVID-19 pandemic was associated with changes utilization of PES. Despite these limitations, this study provides valuable insight into how one local PES program operates in concert with area hospitals to meet the needs of a population that may otherwise be underserved.
Our study bolsters calls from leaders in the fields of psychiatry and public health for communities to develop comprehensive crisis response systems with a continuum of services, including call centers, psychiatric UCCs, and MCUs (Committee on Psychiatry & the Community for the Group for the Advancement of Psychiatry, 2021; National Association of State Mental Health Program Directors, 2018; Substance Abuse & Mental Health Services Administration, 2020). Additionally, it provides initial support for the hypothesis that alternative PES programs have the potential to address several issues associated with rising rates of psychiatric ED utilization. First, these programs may divert non-emergent patients from EDs to more appropriate evaluation and care setting, reducing the burdens that psychiatric ED visits pose for the entire healthcare system. This can be achieved through 24/7 call centers or collaboration with emergency dispatch infrastructure, allowing operators to conduct triage, facilitate care for true psychiatric emergencies, and redirect non-emergent cases to mobile crisis units and psychiatric urgent care centers. Second, alternative PES programs like BEST can ensure all patients, regardless of urgence, receive evaluation and treatment from a licensed mental health care professional. For example, BEST-designated EDs have staff available around the clock to respond to psychiatric emergencies; the program will also send MCUs to non-designated EDs that do not have mental health specialists available. Outside the ED, psychiatric UCCs and MCUs can offer patients more privacy during assessment and may have shorter wait times than EDs, where non-emergent psychiatric issues are a low priority. Regardless of referral source or evaluation location, BEST clinicians are well-positioned to connect patients with both immediate and long-term behavioral health services that may increase the likelihood of symptom reduction and recovery.
Funding
This work was funded by the Department of Psychiatry at Boston Medical Center and a philanthropic donation. Dr. Were's contribution to this paper was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Boston University's Clinical and Translational Science Institute Grant Number 1ULT1R00430. Dr. Kalesan is employed by Regeneron Pharmaceuticals.
Data Availability
Dr. Henderson participates in a Data Safety Monitoring Board for Sunovion Pharmaceuticals.
Declarations
Conflict of interest
Dr. Oblath, Ms. Herrera, Dr. Were, Ms. Syeda, Dr. Duncan, Ms. Ferguson, Ms. Perez, Ms. Taglieri and Dr. Borba have reported no biomedical financial interests or potential conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Christina P. C. Borba and David C. Henderson are co-senior authors.
References
- Allen, M. H., Forster, P., Zealberg, J., & Currier, G. (2002). Report and recommendations regarding psychiatric emergency and crisis services: A review and model program descriptions. APA Task Force on Psychiatric Emergency Services. https://www.psychiatry.org/psychiatrists/search-directories-databases/library-and-archive/task-force-reports
- Baraff LJ, Janowicz N, Asarnow JR. Survey of California emergency departments about practices for management of suicidal patients and resources available for their care. Annals of Emergency Medicine. 2006;48(4):452–458.e2. doi: 10.1016/j.annemergmed.2006.06.026. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Marcus SC, Olfson M. Outpatient care of young people after emergency treatment of deliberate self-harm. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(2):213–222.e1. doi: 10.1016/j.jaac.2011.11.002. [DOI] [PubMed] [Google Scholar]
- Buchmueller TC, Levinson ZM, Levy HG, Wolfe BL. Effect of the affordable care act on racial and ethnic disparities in health insurance coverage. American Journal of Public Health. 2016;106(8):1416–1421. doi: 10.2105/AJPH.2016.303155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke BT, Miller BF, Proser M, Petterson SM, Bazemore AW, Goplerud E, Phillips RL. A needs-based method for estimating the behavioral health staff needs of community health centers. BMC Health Services Research. 2013 doi: 10.1186/1472-6963-13-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Public Representation. (2008). Rosie D.: Reforming the mental health system in Massachusetts. http://www.rosied.org/
- Chaput YJA, Lebel M-J. Demographic and clinical profiles of patients who make multiple visits to psychiatric emergency services. Psychiatric Services. 2007;58(3):335–341. doi: 10.1176/ps.2007.58.3.335. [DOI] [PubMed] [Google Scholar]
- Chun TH, Katz ER, Duffy SJ, Gerson RS. Challenges of managing pediatric mental health crises in the emergency department. Child and Adolescent Psychiatric Clinics of North America. 2015;24(1):21–40. doi: 10.1016/j.chc.2014.09.003. [DOI] [PubMed] [Google Scholar]
- Cloutier P, Martin J, Kennedy A, Nixon MK, Muehlenkamp JJ. Characteristics and co-occurrence of adolescent non-suicidal self-injury and suicidal behaviours in pediatric emergency crisis services. Journal of Youth and Adolescence. 2010;39(3):259–269. doi: 10.1007/s10964-009-9465-1. [DOI] [PubMed] [Google Scholar]
- Committee on Psychiatry and the Community for the Group for the Advancement of Psychiatry . Roadmap to the ideal crisis system: Essential elements, measurable standards and best practices for behavioral health crisis response. National Council for Mental Wellbeing; 2021. [Google Scholar]
- Cook BL, Barry CL, Busch SH. Racial/Ethnic disparity trends in children’s mental health care access and expenditures from 2002 to 2007. Health Services Research. 2013;48(1):129–149. doi: 10.1111/j.1475-6773.2012.01439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, Trinh N-H, Li Z, Hou SS-Y, Progovac AM. Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatric Services. 2016;68(1):9–16. doi: 10.1176/appi.ps.201500453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper JL, Masi R. Child and youth emergency mental health care: A national problem. National Center for Children in Poverty; 2007. p. 15. [Google Scholar]
- Currier GW, Fisher SG, Caine ED. Mobile crisis team intervention to enhance linkage of discharged suicidal emergency department patients to outpatient psychiatric services: A randomized controlled trial. Academic Emergency Medicine. 2010;17(1):36–43. doi: 10.1111/j.1553-2712.2009.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cusick MM, Sholle ET, Davila MA, Kabariti J, Cole CL, Campion TR. A method to improve availability and quality of patient race data in an electronic health record system. Applied Clinical Informatics. 2020;11(5):785–791. doi: 10.1055/s-0040-1718756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan C, Fein J. Pediatric and adolescent mental health emergencies in the emergency medical services system. Pediatrics. 2011;127(5):e1356–e1366. doi: 10.1542/peds.2011-0522. [DOI] [PubMed] [Google Scholar]
- Doonan MT, Tull KR. Health care reform in Massachusetts: Implementation of coverage expansions and a health insurance mandate. The Milbank Quarterly. 2010;88(1):54–80. doi: 10.1111/j.1468-0009.2010.00589.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyches H, Biegel DE, Johnsen JA, Guo S, Min MO. The impact of mobile crisis services on the use of community-based mental health services. Research on Social Work Practice. 2002;12(6):731–751. doi: 10.1177/104973102237470. [DOI] [Google Scholar]
- Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: Systematic review and meta-regression analysis. PLOS Medicine. 2008;5(12):e225. doi: 10.1371/journal.pmed.0050225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller, D. A., Sinclair, Elizabeth, Geller, Jeffrey, Quanbeck, Cameron, & Snook, John. (2016). Going, going, gone: Trends and consequences of eliminating state psychiatric beds. Treatment Advocacy Center. https://www.treatmentadvocacycenter.org/going-going-gone
- Geller JL, Biebel K. The premature demise of public child and adolescent inpatient psychiatric beds: Part I: Overview and current conditions. Psychiatric Quarterly. 2006;77(3):251–271. doi: 10.1007/s11126-006-9012-0. [DOI] [PubMed] [Google Scholar]
- Guo S, Biegel DE, Johnsen JA, Dyches H. Assessing the impact of community-based mobile crisis services on preventing hospitalization. Psychiatric Services. 2001;52(2):223–228. doi: 10.1176/appi.ps.52.2.223. [DOI] [PubMed] [Google Scholar]
- Halmer TC, Beall RC, Shah AA, Dark C. Health policy considerations in treating mental and behavioral health emergencies in the United States. Emergency Medicine Clinics of North America. 2015;33(4):875–891. doi: 10.1016/j.emc.2015.07.013. [DOI] [PubMed] [Google Scholar]
- Hellebuyck, M., Halpern, M., Nguyen, N., & Fritze, D. (2019). State of mental health in America. Mental Health America. https://mhanational.org/research-reports/2019-state-mental-health-america-report
- Hugo M, Smout M, Bannister J. A comparison in hospitalization rates between a community-based mobile emergency service and a hospital-based emergency service. Australian & New Zealand Journal of Psychiatry. 2002;36(4):504–508. doi: 10.1046/j.1440-1614.2002.01042.x. [DOI] [PubMed] [Google Scholar]
- Kalb LG, Stapp EK, Ballard ED, Holingue C, Keefer A, Riley A. Trends in psychiatric emergency department visits among youth and young adults in the US. Pediatrics. 2019;143(4):e20182192. doi: 10.1542/peds.2018-2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowal J, Swenson JR, Aubry TD, Marchand HD, MacPhee C. Improving access to acute mental health services in a general hospital. Journal of Mental Health. 2011;20(1):5–14. doi: 10.3109/09638237.2010.492415. [DOI] [PubMed] [Google Scholar]
- LaCalle E, Rabin E. Frequent users of emergency departments: The myths, the data, and the policy implications. Annals of Emergency Medicine. 2010;56(1):42–48. doi: 10.1016/j.annemergmed.2010.01.032. [DOI] [PubMed] [Google Scholar]
- Larkin GL, Claassen CA, Emond JA, Pelletier AJ, Camargo CA. Trends in US emergency department visits for mental health conditions, 1992 to 2001. Psychiatric Services. 2005;56(6):671–677. doi: 10.1176/appi.ps.56.6.671. [DOI] [PubMed] [Google Scholar]
- Massachusetts Legislature. (2006). Chapter 58: An act providing access to affordable, quality, accountable health care. 192nd General Court of the Commonwealth of Massachusetts. https://malegislature.gov/Laws/SessionLaws/Acts/2006/Chapter58
- Massachusetts Legislature. (2008). Chapter 256: An act relative to mental health parity. 192nd General Court of the Commonwealth of Massachusetts. https://malegislature.gov/Laws/SessionLaws/Acts/2008/Chapter256
- Lelonek G, Crook D, Tully M, Trufelli K, Blitz L, Rogers SC. Multidisciplinary approach to enhancing safety and care for pediatric behavioral health patients in acute medical settings. Child and Adolescent Psychiatric Clinics of North America. 2018;27(3):491–500. doi: 10.1016/j.chc.2018.03.004. [DOI] [PubMed] [Google Scholar]
- Long SK. On the road to universal coverage: Impacts of reform in Massachusetts at one year. Health Affairs. 2008;27(Supplement 1):w270–w284. doi: 10.1377/hlthaff.27.4.w270. [DOI] [PubMed] [Google Scholar]
- Mapelli E, Black T, Doan Q. Trends in pediatric emergency department utilization for mental health-related visits. The Journal of Pediatrics. 2015;167(4):905–910. doi: 10.1016/j.jpeds.2015.07.004. [DOI] [PubMed] [Google Scholar]
- Massachusetts Department of Public Health. (2022). CBFS FAQ’s/Information Sheets. https://www.mass.gov/service-details/cbfs-faqsinformation-sheets
- McMillan JA, Land M, Leslie LK. Pediatric residency education and the behavioral and mental health crisis: A call to action. Pediatrics. 2017 doi: 10.1542/peds.2016-2141. [DOI] [PubMed] [Google Scholar]
- McNeil, S. E. (2020). Alternative models of emergency psychiatric care: Regional emergency psychiatric facilities, freestanding emergency departments, and urgent care centers. In M. J. Fitz-Gerald & J. Takeshita (Eds.), Models of emergency psychiatric services that work (pp. 73–83). Springer. 10.1007/978-3-030-50808-1_7
- Middleton KR, Burt CW. Availability of pediatric services and equipment in emergency departments: United States, 2002–03. Advance Data. 2006;367:1–16. [PubMed] [Google Scholar]
- Moulin A, Evans EJ, Xing G, Melnikow J. Substance use, homelessness, mental illness and Medicaid coverage: A set-up for high emergency department utilization. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health. 2018;19:6. doi: 10.5811/westjem.2018.9.38954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of State Mental Health Program Directors. (2018). A comprehensive crisis system: Ending unnecessary emergency room admissions and jail bookings associated with mental illness.
- Newton AS, Hartling L, Soleimani A, Kirkland S, Dyson MP, Cappelli M. A systematic review of management strategies for children’s mental health care in the emergency department: Update on evidence and recommendations for clinical practice and research. Emergency Medicine Journal. 2017;34(6):376–384. doi: 10.1136/emermed-2016-205939. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus SC, Bridge JA. Emergency treatment of deliberate self-harm. Archives of General Psychiatry. 2012;69(1):80–88. doi: 10.1001/archgenpsychiatry.2011.108. [DOI] [PubMed] [Google Scholar]
- Pande AH, Ross-Degnan D, Zaslavsky AM, Salomon JA. Effects of healthcare reforms on coverage, access, and disparities: Quasi-experimental analysis of evidence from Massachusetts. American Journal of Preventive Medicine. 2011;41(1):1–8. doi: 10.1016/j.amepre.2011.03.010. [DOI] [PubMed] [Google Scholar]
- Pittsenbarger ZE, Mannix R. Trends in pediatric visits to the emergency department for psychiatric illnesses. Academic Emergency Medicine. 2014;21(1):25–30. doi: 10.1111/acem.12282. [DOI] [PubMed] [Google Scholar]
- Polubriaginof FCG, Ryan P, Salmasian H, Shapiro AW, Perotte A, Safford MM, Hripcsak G, Smith S, Tatonetti NP, Vawdrey DK. Challenges with quality of race and ethnicity data in observational databases. Journal of the American Medical Informatics Association : JAMIA. 2019;26(8–9):730–736. doi: 10.1093/jamia/ocz113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santillanes G, Axeen S, Lam CN, Menchine M. National trends in mental health-related emergency department visits by children and adults, 2009–2015. The American Journal of Emergency Medicine. 2020;38(12):2536–2544. doi: 10.1016/j.ajem.2019.12.035. [DOI] [PubMed] [Google Scholar]
- Santucci KA, Sather J, Baker DM. Emergency medicine training programsʼ educational requirements in the management of psychiatric emergencies: Current perspective. Pediatric Emergency Care. 2003;19(3):154–156. doi: 10.1097/01.pec.0000081235.20228.7a. [DOI] [PubMed] [Google Scholar]
- Saxon, V., Mukherjee, D., & Thomas, D. (2018). Behavioral health crisis stabilization centers: A new normal. Journal of Mental Health & Clinical Psychology, 2(3). https://www.mentalhealthjournal.org/articles/behavioral-health-crisis-stabilization-centers-a-new-normal.html
- Shannahan, R., & Fields, S. (2016). Services in support of community living for youth with serious behavioral health challenges: Mobile crisis response and stabilization services. Substance Abuse and Mental Health Services Administration.
- Sisti DA, Segal AG, Emanuel EJ. Improving long-term psychiatric care: Bring back the asylum. JAMA. 2015;313(3):243. doi: 10.1001/jama.2014.16088. [DOI] [PubMed] [Google Scholar]
- Slade EP, Dixon LB, Semmel S. Trends in the duration of emergency department visits, 2001–2006. Psychiatric Services. 2010;61(9):878–884. doi: 10.1176/ps.2010.61.9.878. [DOI] [PubMed] [Google Scholar]
- Snowden LR, Catalano R, Shumway M. Disproportionate use of psychiatric emergency services by African Americans. Psychiatric Services. 2009;60(12):1664–1671. doi: 10.1176/ps.2009.60.12.1664. [DOI] [PubMed] [Google Scholar]
- Snowden LR, Masland MC, Libby AM, Wallace N, Fawley K. Racial/Ethnic minority children’s use of psychiatric emergency care in California’s public mental health system. American Journal of Public Health. 2008;98(1):118–124. doi: 10.2105/AJPH.2006.105361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiranovic C, Matthews A, Scanlan J, Kirkby KC. Increasing knowledge of mental illness through secondary research of electronic health records: Opportunities and challenges. Advances in Mental Health. 2016;14(1):14–25. doi: 10.1080/18387357.2015.1063635. [DOI] [Google Scholar]
- Stone A, Rogers D, Kruckenberg S, Lieser A. Impact of the mental healthcare delivery system on California emergency departments. Western Journal of Emergency Medicine. 2012;13(1):51–56. doi: 10.5811/westjem.2011.6.6732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2014). Crisis services: Effectiveness, cost-effectiveness, and funding strategies. https://www.nasmhpd.org/content/new-samhsa-publication-crisis-services-effectiveness-cost-effectiveness-and-funding
- Substance Abuse and Mental Health Services Administration. (2020). National guidelines for behavioral health crisis care: Best practice toolkit. https://nicic.gov/national-guidelines-behavioral-health-crisis-care-best-practice-toolkit-2020
- Sunderji N, de Bibiana JT, Stergiopoulos V. Urgent psychiatric services: A scoping review. The Canadian Journal of Psychiatry. 2015;60(9):393–402. doi: 10.1177/070674371506000904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psychiatric Services. 2009;60(10):1323–1328. doi: 10.1176/ps.2009.60.10.1323. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. Journal of Abnormal Psychology. 2019;128(3):185–199. doi: 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. (2012). Census Bureau releases estimates of undercount and overcount in the 2010 Census (News Release No. CB12–95). https://www.census.gov/newsroom/releases/archives/2010_census/cb12-95.html
- United States Census Bureau. (2021). Explore Census Data. https://data.census.gov/cedsci/
- Weber EJ, Showstack JA, Hunt KA, Colby DC, Callaham ML. Does lack of a usual source of care or health insurance increase the likelihood of an emergency department visit? Results of a national population-based study. Annals of Emergency Medicine. 2005;45(1):4–12. doi: 10.1016/j.annemergmed.2004.06.023. [DOI] [PubMed] [Google Scholar]
- Weiskopf NG, Weng C. Methods and dimensions of electronic health record data quality assessment: Enabling reuse for clinical research. Journal of the American Medical Informatics Association. 2013;20(1):144–151. doi: 10.1136/amiajnl-2011-000681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss, A. J., Barrett, M. L., Heslin, K. C., & Stocks, C. (2017). Trends in emergency department visits involving mental and substance use disorders, 2006–2013: Statistical brief #216. Agency for Healthcare Research and Quality. https://europepmc.org/article/NBK/nbk409512 [PubMed]
- Williams NJ, Scott L, Aarons GA. Prevalence of serious emotional disturbance among US children: A meta-analysis. Psychiatric Services. 2017;69(1):32–40. doi: 10.1176/appi.ps.201700145. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (1978). International classification of diseases: Ninth revision. World Health Organization. https://apps.who.int/iris/handle/10665/39473
- World Health Organization. (2004). International statistical classification of diseases and related health problems: Tenth revision (2nd ed.). World Health Organization. https://apps.who.int/iris/handle/10665/42980 [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Dr. Henderson participates in a Data Safety Monitoring Board for Sunovion Pharmaceuticals.