Abstract
Background
Hip osteoarthritis (HOA) is a disabling disease affecting around 33 million people worldwide. People of working age and the elderly are at increased risk of developing HOA and the disease is associated with high costs at individual and societal levels due to sick leaves, job loss, total hip replacements and disability pension. This systematic review evaluated the influence of physically demanding occupations on the development of HOA in men.
Methods
Cohort studies, case–control studies and cross-sectional studies with publications in English or German, which assessed the association between exposure to physically demanding occupations and development of HOA, were searched in electronic databases (Medline, Embase, HSE-Line, Cochrane Library) and conference abstracts from 1990 until May 2020. We assessed the methodological quality of selected studies, interpreted all relative effect estimators as relative risks (RRs) and meta-analytically reviewed the effects of occupations with high physical workloads. All steps are based on a study protocol published in PROSPERO (CRD42015016894).
Results
Seven cohort studies and six case–control studies were included. An elevated risk to develop HOA was shown for six physically demanding occupational groups. Working in agriculture including fishery and forestry and food production doubles the risk of HOA. Construction, metal working and sales as well as exposure to whole body vibration while driving vehicles increases the risk by roughly 50 to 60%. Unskilled or basic level workers, who were frequently exposed to repetitive heavy manual work, had nearly a doubled risk (RR 1.89 95%CI: 1.29 to 2.77) compared to workers with lower exposure.
Conclusions
Existing studies state an association between various occupations with high physical workload and an increased risk of developing HOA. High Physical workloads include including lifting and carrying heavy loads, demanding postures, repetitive activities, long standing and running, as well as exposure to body vibrations. Occupational prevention and early detection as well as individual health promotion strategies should place their focus on reducing the impact of high physical strain at work sites.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12995-022-00358-y.
Keywords: Occupational, Hip, Osteoarthritis, Workplaces, Musculoskeletal
Background
Hip osteoarthritis (HOA) is a disabling disease characterized by pathologic changes of the whole hip joint including the articular cartilage, subchondral bone, and the synovial joint lining [1, 2]. In European studies, HOA prevalence estimates range from 2 to 9% for people under 75 years of age depending on the region and diagnostic criteria [3–5]. The Global Burden of Disease Study 2019 reported lower prevalence estimates for people over the age of 25 with 1.95% (95%-CI 1.48 to 2.49) in Western Europe and 1.01% (95%-CI 0.77 to 1.27) in Eastern Europe [3]. HOA incidence increases at the age of 40–50, which indicates an increased risk of developing HOA for people of working age and the elderly. This is associated with high costs due to necessary medical treatments, sick leaves, job loss or disability pensions [6]. This substantial health burden might be further increased by factors such as willingness of patients to seek care, awareness of primary care physicians, aging, increasing obesity and more frequently occurring joint injuries [1, 2, 7]. On the other hand, changes in occupational exposures, the development of special preventive strategies and technical equipment may reduce this burden [8 9]. Other confirmed risk factors for developing HOA are genetic pathologies and congenital deformit [1–13].
The American College of Rheumatology has established diagnostic criteria for HOA, which are the most frequently used internationally [14]. These include hip pain, restricted internal hip rotation and radiographic changes such as joint space narrowing and marginal femoral or acetabular osteophytes. The Kellgren and Lawrence score and other joint functioning scores are also considered for diagnosis of HOA [15, 16].
Various reviews demonstrate a positive association between long-term lifting and carrying of heavy loads, or physically demanding work in general, and the risk of developing of HOA [17–20]. Thus, in Germany, HOA has been defined in 2020 as an occupational disease for workers lifting heavy loads [21] with a cumulative load of at least 9.500 tons in their working life or ≥ 20 kg handled > 10 times per day. However, HOA is not listed in the European schedule of occupational diseases [22, 23].
We wanted to check whether only occupations associated with lifting and carrying heavy loads have an increased risk of developing HOA, or whether other physically demanding occupations with demanding postures, repetitive activities, long standing and running or body vibrations may also increase the risk of HOA. The aim of this systematic review was to identify studies and appraise and synthesize their results on developing HOA due to specific occupations. The hypothesis was that an increased risk of developing HOA would be observed in occupational sectors with high physical workloads compared to other occupational sectors. This systematic literature review was based on a sensitive search string and concentrated on the exposure of men in physically demanding occupations. Due to the high number of occupations, substantial differences in work exposures for men and women and job sector segregation between the sexes [24], we decided to summarize and discuss the results for women, including gender-specific differences and consequences, in a separate manuscript.
Methods
This systematic review was registered a priori in PROSPERO (CRD42015016894) and follows the PRISMA regulations [25].
Systematic search
We systematically searched cohort studies, case–control studies and cross-sectional studies that assessed the association between exposure to occupational workload or occupations with known high physical workload and development of HOA in February 2015 and published the results on the association between lifting and carrying heavy loads or other demanding work on the risk of HOA [17] and added searches in 2018 and 2020 on the topic of this review. We searched Medline (Ovid) (Supplementary Table S1), Embase (Supplementary Table S2), Cochrane Library (Supplementary Table S3), CINAHL (Supplementary Table S4) and the Health and Safety Executive (HSE)-Line (Supplementary Table S5) with a last update of the search conducted in May 2020. We manually checked the tables of contents of occupational medicine journals (Supplementary Table S6) and checked the abstracts of annual meetings of international orthopaedic conferences (International Epidemiology in Occupational Health (EPICOH), American Occupational Health Conference (AOHC) and the American Orthopaedic Association (AOA)) for additional studies until 2020. Embase was searched in February 2015. The search strategy was based on a combination of controlled vocabulary and key words to describe the association between occupational exposure and the development of HOA. All references were imported to a bibliographic reference management program (Endnote).
Inclusion and exclusion criteria
Criteria summarized in Table 1 were applied to each identified reference to determine eligibility for this systematic review.
Table 1.
Inclusion criteria for studies
| Population | Adult men (≥ 18 years at diagnosis) |
|---|---|
| Exposure | Former or current employment in occupational groups with known heavy physically demanding strain where results on the association between occupational strain and development of HOA were reported in at least three studies |
| Comparison | Occupational groups without heavy occupational workload |
| Endpoints |
Diagnosis of HOA due to occupational strain based on •clinical and radiological criteria (American College of Rheumatology criteria [14] or radiological scoring systems according to Kellgren and Lawrence [16]) •total hip replacement subscales measuring hip pain, stiffness or reduced physical function •hip pain •reported cases with the diagnosis HOA in register data without further information including resulting disability, pension or sick leave Exclusion of studies with HOA due to non-occupational strains (e.g., due to sport, hip dysplasia or other hip deformities) |
| Study design |
Full-text publications in German or English language from 1990 until today of •cohort studies •case–control studies or analysis of data from registry data •cross-sectional studies with relevant data of an exposure to occupations for ≥ 10 years to assure a causal relationship |
Study selection
Two independent reviewers checked titles and abstracts of all references identified from different sources of our systematic search, read full text publications of potentially eligible studies, extracted data and assessed the quality of included studies. In case of disagreement, a third reviewer was consulted to achieve consensus.
Data extraction and quality assessment
We extracted information to characterize the researched studies (design, country and time of recruitment), study population (inclusion criteria, number of participants, age and sex), exposure and reference groups (including levels of exposure with their duration and intensity) and outcome (with precise diagnostic criteria). To describe the investigated association, we extracted numbers of participants and events per group and adjusted effect sizes with their 95% confidence intervals (95%-CI) for men and women.
Quality assessment was based on criteria recently used in Bergmann et al. 2017 [17]. These criteria applied the Newcastle–Ottawa Quality Assessment Scale [26] and the Cochrane Handbook [27] to our research question. The assessment criteria were separately developed for case–control and cohort studies. For cohort studies, we judged the representative selection of exposed and non-exposed participants, validity and accuracy of exposure acquisition and assessment of outcomes and the methods to ensure comparability of exposed and non-exposed groups. For case–control studies, we judged the selection, validity and accuracy of exposure and methods to ensure comparability of cases and controls. Best judgement resulted in 19 points for cohort studies and 15 points for case–control studies.
Data synthesis
The association of occupational risks and development of HOA was assessed with all effect measures to compare the risk of occupations with heavy physical strain to non-exposed reference groups. Due to the low prevalence of HOA, different reported effect measures (odds ratios, relative risks, hazard ratios, standardised hospitalisation ratios) do not differ widely and were interpreted as relative risks (RR). If more than one effect estimator was reported in one study, we pooled comparable results from studies, which corresponded best with our research question. This estimator was based on diagnostic criteria with the best validity according to Bergmann et al. 2017 [17] and the highest or longest exposure with a sufficient sample size.
The effect estimators of different studies and their 95%-CI were synthesized with the random effects model using RevMan 5.3 [28] due to differences in measurement of exposure, outcome, study design and effect measures. Reported RRs greater than 1 are considered as a higher risk in occupations with heavy physical strain compared to the reference group. We judged the consistency of results of different studies based on the I2 value and interpreted heterogeneity as small if I2 < 30%, moderate (30 to 60%) or substantial (I2 > 60%). We did not discuss the pooled results in cases of substantial heterogeneity between study results, different conclusions of the studies or clinical heterogeneity in severity of physical demands. To investigate clinical heterogeneity between treatment effects of individual studies, we calculated subgroup analyses for differences in exposure, criteria to diagnose HOA and study design.
Results
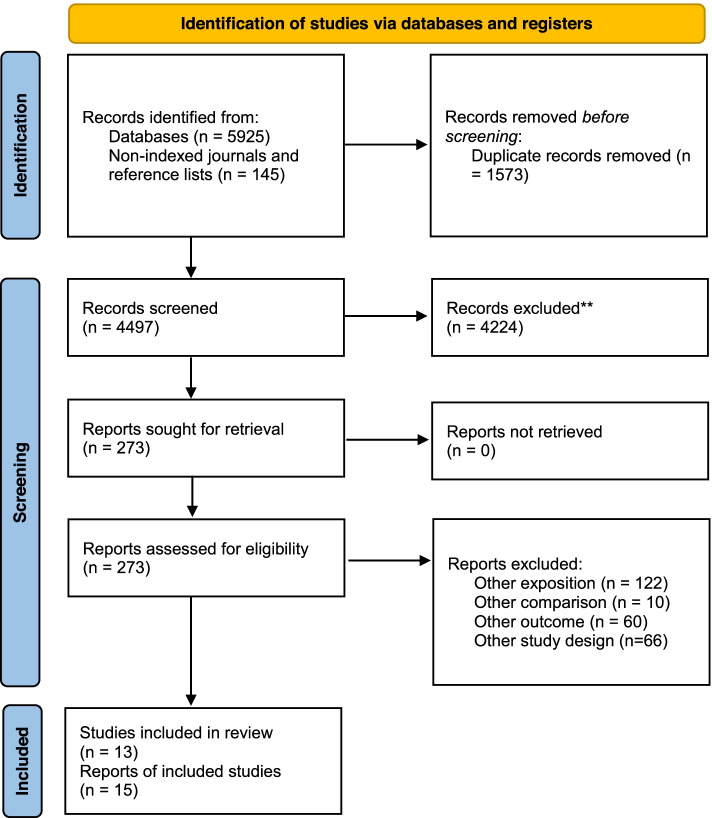
We identified a total of 6070 records and read 273 potentially relevant reports. After exclusion of all reports that did not fulfil our inclusion criteria, we included a total of 13 eligible studies including 7 cohort studies [29–37] and 6 case–control studies [38–43] with a total of 15 publications (Fig. 1). Cross-sectional studies with an exposure to occupations of at least 10 years to ensure the association between occupational exposure and the development of HOA were not identified.
Fig. 1.
Flow chart [44] to describe identification and selection of included studies
Participants
All eligible studies were conducted in Europe, predominantly in Scandinavian countries (Sweden, Denmark, Finland, and Iceland), two studies in the UK and one in Germany. Most studies included working age participants with a mean or median age of over 36 years at time of diagnosis. The proportions of men showed a broad variation across occupational groups. Most studies recruited more men and four studies [38, 39, 42, 43] recruited only men (Supplementary Tables S7 and S8).
Exposure
Information on occupation was based on registry data [29, 31–37] in Scandinavian countries, occupational titles [32] and interviews [38, 39, 43] or questionnaires [40–42] on occupational history. Some studies summarized different occupational groups, others were more specific and differentiated between degrees or periods of exposure. This review focuses on results on the risk to develop HOA in physically demanding occupational groups traditionally dominated by men (farming, construction, driving, metal work, storage and transportation).
We identified nine occupational sectors with physically demanding workloads and resulting high risk to develop HOA. These sectors considered occupations in the following:
•agriculture, fishery or forestry (12 studies): Three of these studies [38, 42, 43] differentiated between exposure lengths. Studies reported results on the exposure of farmers or summarized farmers and forest workers [40, 43] farmers and agricultural workers [38] or agricultural and fishery workers [34] (Supplementary Table S9).
•construction (9 studies): Five studies reported the risk for construction workers [29, 31, 37, 40, 43], three studies summarized exposure of comparably demanding occupations [34, 39, 41] and one study reported more specialized occupations [33] (Supplementary Table S10).
•driving vehicles with exposure to whole body vibration (8 studies): Two studies reported on the risk of any occupation with exposure to whole body vibration [33, 40], others reported results for professional motorists [31, 34, 39] or differentiated between driving different vehicles [36, 37, 42] (Supplementary Table S11).
•metal work (6 studies): Of these, three studies reported the risk of general occupations in metal work [31, 40, 43], others summarized metal and machinery workers [34] or reported more specific information on sheet-metal workers [33] and furnace men, smiths and workers doing metal processing [37] (Supplementary Table S12).
•sales (5 studies): Of these, four studies reported the risk of working as service or shop worker [34–41], whereas one [37] summarized very heterogeneous demanding occupations for store and warehouse workers (Supplementary Table S13).
•gastronomy (4 studies): All of these studies summarized different occupations with comparable exposure in gastronomy and hotels [34, 36, 37, 40] (Supplementary Table S14).
•food production (4 studies): Three studies summarized comparable demanding occupations [37, 40, 43], whereas one study [36] reported the risk of less demanding occupations as baker, pastry cook or confectionery maker (Supplementary Table S15).
•storage transportation (3 studies): All studies investigated the exposure of postmen [38, 41, 44], one study added results for storage and transport workers (Supplementary Table S16).
•health care (3 studies): Studies reported results for health-care assistants [29], medical doctors [36] and one study reported combined results for nurses and environmental officers [34] (Supplementary Table S17).
Finally, three studies [34, 37, 41] investigated the risk of HOA of men in unskilled or basic level labours in comparison to managers, professionals or low-exposure blue-collar workers (Supplementary Table S18).
Diagnosis
Follow-up periods between exposure and diagnoses are mainly available from cohort studies and ranged from 3 to 28 years.
Various criteria were used for the diagnosis of HOA:
•Clinical or radiological diagnostic criteria [29, 35, 37, 38, 40]
•Disability pension due to low back disorders [43]
A high validity of the diagnosis of HOA was assumed for disability pension due to HOA, THR and radiological imaging compared to a clinical diagnosis and back disorders.
Quality assessment
Cohort studies
The seven cohort studies scored 12 to 15 points on a scale ranging from 0 to 19 points. No study could provide accurate and reliable quantitative data on exposure such as frequency or duration of occupation. All studies adjusted results for age; three used other important confounders (body mass index or education and physical workload factors) [31, 33, 34] (Supplementary Table S7).
Case–control studies
The six case–control studies scored between 5 to 10 points on a scale of 0 to 15. Three studies received less than 3 out of 6 points for the selection of the study population [38–40] due to deficits in the representativeness of the cases and the selection of controls. Two studies [40, 41] had a low response rate. Only one study received full points for an adequate case definition by consideration of people with a THR [41] and one study received no points due to the low validity of diagnostic criteria [43]. Only one studies excluded pre-existing HOA al the baseline [35]. Only two studies received points for including a long enough follow-up of more than 10 years for the endpoint to occur [42, 43]. Four studies were downgraded due to low validity of data acquisition [39–42] and two studies [40, 43] were downgraded because some comparative hypotheses mentioned in the methods section were not reported with quantifiable data. Two studies [38, 41] adjusted their results for age and body weight (Supplementary Table S8).
Study results
Agriculture, fishery or forestry (12 studies)
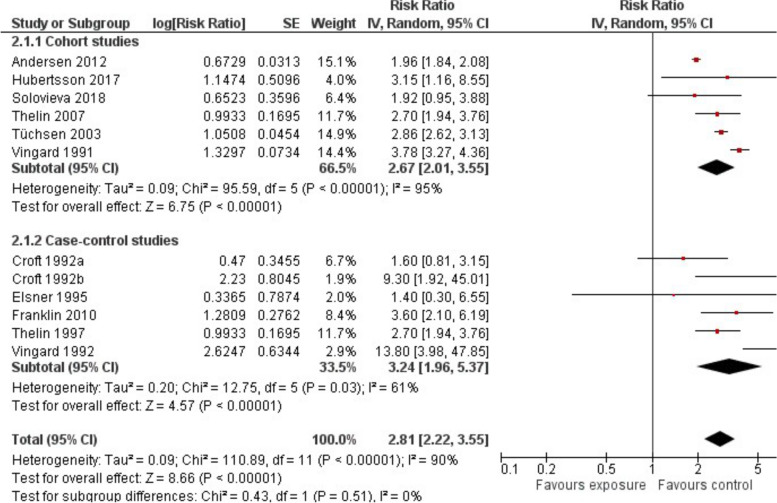
Out of around 273,300 men with occupations in agriculture or forestry, 4,732 were diagnosed with HOA. All studies stated an elevated risk of developing HOA with a pooled RR of 2.81 (95%-CI 2.22 to 3.55) with substantial heterogeneity (I2 = 90%) between results of different studies (Fig. 2). A possible explanation for this heterogeneity might be the increasing relative risk of HOA with increasing numbers of years farming as shown in two studies [38, 42, 45] (Supplemental Table S9).
Fig. 2.
Risk of developing HOA owing to occupations in agriculture, fishery or forestry: Comparison of exposed and non-exposed control groups
Construction worker (9 studies)
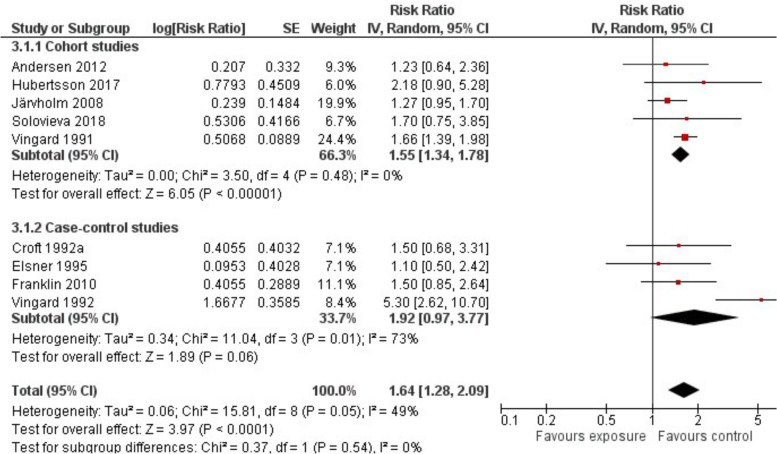
Out of more than 581,000 construction workers, 3,736 were diagnosed with HOA. The results of all studies stated an elevated risk of developing HOA. Summarising the results of all studies, we stated that the risk of construction workers to develop HOA is increased by 64% (RR 1.64; 95%-CI 1.28 to 2.09) compared to non-exposed men with a moderate heterogeneity (I2 = 49%) between studies (Fig. 3).
Fig. 3.
Risk of developing HOA as a construction worker: Comparison of exposed and non-exposed control groups
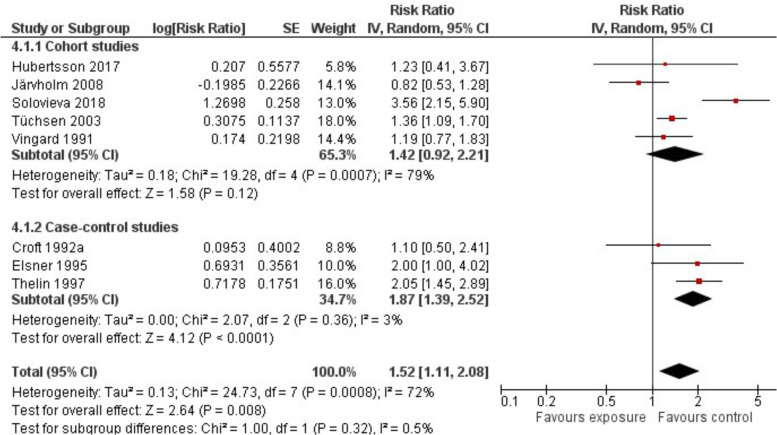
Driving vehicles with whole body vibration (8 studies)
Out of more than 93,418 drivers, 410 (most of them driving different vehicles with whole body vibration) were diagnosed with HOA. The results of 7 out of 8 studies stated an elevated risk with a pooled RR of 1.52 (95%-CI 1.11 to 2.08) and a substantial heterogeneity (I2 = 72%) between results of different studies (Fig. 4). The heterogeneity might be explained by the exposure to very different vehicles and resulting vibrations (Supplementary Table S11).
Fig. 4.
Risk of developing HOA in occupations with whole body vibrations due to driving vehicles: Comparison of exposed and non-exposed control groups
Metal work (6 studies)
Out of more than 77,000 metal workers, 299 were diagnosed with HOA. The results of all studies stated an elevated risk to develop HOA. Summarising the results of all studies, we stated an increased risk of 54% (RR 1.54; 95%-CI 1.21 to 1.97) for metal workers compared to non-exposed men with moderate heterogeneity between results (I2 = 37%) (Table 2).
Table 2.
Effect sizes of occupational exposure to develop HOA among different subgroups
| Occupation | Subgroup | Number of studies | RR (95%-CI) | Hetero- geneity (I2) |
Subgroup differences |
|---|---|---|---|---|---|
| Agriculture and forestry | All studies | 12 | 2.81 (2.22–3.55)a | 90% | |
| Disability pension due to HOA | 3 | 3.96 (1.36–11.51)a | 73% | p = 0.72 | |
| THR, no information on disability pension reported | 3 | 2.41 (1.45–4.00)a | 91% | ||
| Diagnosis, but no THR | 6 | 2.60 (1.81–3.72)a | 92% | ||
| Cohort studies | 6 | 2.67 (2.01–3.55)a | 95% | p = 0.51 | |
| Case–control studies | 6 | 3.24 (1.96–5.37)a | 61% | ||
| Construction worker | All studies | 9 | 1.64 (1.28–2.09) | 49% | |
| Disability pension due to HOA | 3 | 2.79 (1.36–5.72) | 59% | p = 0.12 | |
| THR, no information on disability pension reported | 2 | 1.31 (1.02–1.70) | 38% | ||
| Diagnosis, but no THR | 4 | 1.60 (1.36–1.87) | 0% | ||
| Cohort studies | 5 | 1.55 (1.34–1.78) | 0% | p = 0.54 | |
| Case–control studies | 4 | 1.92 (0.97–3.77)a | 73% | ||
| Driving vehicles with whole body vibration | All studies | 8 | 1.52 (1.11–2.08)a | 72% | |
| Disability pension due to HOA | 2 | 2.35 (0.85–6.49)a | 67% | p = 0.18 | |
| THR, no information on disability pension reported | 3 | 1.12 (0.78–1.59) | 51% | ||
| Diagnosis, but no THR | 3 | 1.68 (1.15–2.45) | 50% | ||
| Cohort studies | 5 | 1.42 (0.92–2.21)a | 79% | p = 0.32 | |
| Case–control studies | 3 | 1.87 (1.39–2.52) | 3% | ||
| Metal work | All studies | 6 | 1.54 (1.21–1.97) | 37% | |
| Disability pension due to HOA | 3 | 1.83 (1.15–2.90) | 0% | p = 0.28 | |
| THR, no information on disability pension reported | 1 | 1.10 (0.67–1.80) | - | ||
| Diagnosis, but no THR | 2 | 1.72 (1.10–2.68) | 22% | ||
| Cohort studies | 4 | 1.42 (1.08–1.87) | 0% | p = 0.21 | |
| Case–Control studies | 2 | 2.09 (1.23–3.56) | 0% | ||
| Sales | All studies | 5 | 1.50 (1.01–2.24)b | 38% | |
| Comparable physical demanding occupations | 4 | 1.50 (0.82–2.75) | 51% | p = 0.83 | |
| Heterogeneous physical demanding occupations | 1 | 1.39 (0.95–2.03) | - | ||
| Disability pension due to HOA | 1 | 2.35 (1.19–4.66) | - | p = 0.33 | |
| THR, no information on disability pension reported | 2 | 1.77 (1.00–3.16) | 0% | ||
| Diagnosis, but no THR | 2 | 0.96 (0.37–2.51)c | 65% | ||
| Cohort studies | 2 | 1.67 (1.02–2.72) | 42% | p = 0.51 | |
| Case–Control Studies | 3 | 1.21 (0.54–2.70) | 56% | ||
| Gastronomy | All studies | 4 | 1.44 (0.78–2.66)c | 63% | |
| Cohort studies | 3 | 1.70 (0.92–3.15)a | 63% | p = 0.13 | |
| Case–Control Studies | 1 | 0.60 (0.18–2.02) | - | ||
| Storage and transportation | All studies | 3 | 2.09 (0.88–4.96) | 0% | |
| Cohort study | 1 | 0.92 (0.12–6.99) | - | p = 0.51 | |
| Case–Control-Studies | 2 | 2.50 (0.96–6.52) | 0% | ||
| Food production | All studies | 4 | 2.13 (1.53–2.95)b | 0% | |
| Comparable physical demanding occupations | 3 | 2.22 (1.39–3.54) | 0% | P = 1.00 | |
| Less physical demanding occupations in construction | 1 | 2.04 (1.28–3.24) | - | ||
| Cohort study | 2 | 2.10 (1.48–2.96)b | 0% | p = 0.84 | |
| Case–Control-Studies | 2 | 2.40 (0.64–8.97) | 37% | ||
| Health care | All studies (only cohort studies) | 3 | 1.21 (0.51–2.88)c | 88% | |
| Unskilled or basic level labours | All studies | 3 | 1.89 (1.29–2.77) | 34% | |
| Cohort studies | 2 | 2.15 (1.31–3.54) | 46% | p = 0.28 | |
| Case–Control Studies | 1 | 1.4 (0.77–2.56) | - |
CI confidence interval, HOA hip osteoarthritis, RR relative risk, THR total hip replacement
Pooling not useful due to substantial heterogeneity between results of individual studies (a), clinical heterogeneity in severity of physical demanding occupations (b) or both (c)
Sales (5 studies)
Out of more than 19,500 men working in sales, 93 were diagnosed with HOA. Among these men, the summary of all studies stated an elevated risk by 50% (RR 1.50; 95%-CI 1.01 to 2.24) with moderate heterogeneity between results (I2 = 38%). A subgroup analysis of the results of four of these studies with comparable physically demanding occupations (warehousemen, clerks, service and shop worker) stated this exposure effect, but decreased precision due to decreasing sample size (supplementary table S13, Table 2).
Gastronomy (4 studies)
Out of 22,716 men working in gastronomy, 82 were diagnosed with HOA. Different studies summarized different occupational groups, which might explain the substantial heterogeneity of results (I2 = 63%). Due to this, it was not reasonable to pool the results. Two studies stated an increased risk [34, 36] (supplementary table S14, Table 2).
Food production (4 studies)
Out of more than 6,461 workers in food production, 66 were diagnosed with HOA. The results of all studies stated an elevated risk (RR 2.13; 95%-CI 1.53 to 2.95) with small heterogeneity between results (I2 = 0%) (Table 2).
Storage and transportation worker (3 studies)
Out of more than 3,100 men working as postmen, 22 were diagnosed with HOA. Summarising the results of all studies, we stated a non-significantly elevated risk increase (RR 2.09; 95%-CI 0.88 to 4.96) with small heterogeneity between results (I2 = 0%) (Table 2).
Health care (3 studies)
Out of 99,603 men working in health care, 321 were diagnosed with HOA. Exposures and diagnostic criteria were very heterogeneous and explain substantial heterogeneity of results (I2 = 88%) (supplementary table S17, Table 2).
Unskilled or basic level labour (3 studies)
Out of 19,273 men working in unskilled or basic level labour, 383 were diagnosed with HOA. All studies stated an elevated risk with an increase of 89% (RR 1.89; 95%-CI 1.29 to 2.77) compared to jobs requiring higher qualification with moderate heterogeneity between results (I2 = 34%) (Table 2).
In subgroup analyses, we investigated possible sources of heterogeneity and stated no difference of the results depending on different diagnostic criteria and study types (Table 2).
Discussion
This systematic review reveals considerable differences between different physically demanding occupations regarding developing HOA and consequential sick leaves, hospitalisation, THR or disability pensions. We identified six occupational groups with evidence for an increased risk of HOA compared to professionals with no or low physical strain. These groups included workers in agriculture, fishery or forestry, in food production or sales, construction and metal workers and men driving vehicles with whole body vibration.
Our results correspond to the conclusions of recent systematic reviews that heavy physical workload exposure on the job increases the risk of developing HOA [17, 18, 20, 46]. A greater exposure to manual handling of weights at work is associated with a higher risk to develop HOA [47, 48] and can even double this risk [19]. But our results show that occupations demanding various other physical exercises can also increase the risk of HOA. Thus, they are in line with the results from a recent systematic review initiated by the World Health Organisation (WHO) and the International Labour Organisation (ILO) with the aim to develop estimates of work-related burdens to ergonomic risk factors. These factors included force exertion, demanding postures, repetitiveness, vibrations and lifting [49]. Occupations in agriculture, fishery or forestry, construction and metal industry require frequent lifting and carrying of heavy loads and demanding working postures. Food production requires repetitive activities, long standing and running, but workers have to lift and carry of medium loads. Driving vehicles is a predominantly sedentary activity with lack of movement, but with whole body vibrations, which may damage joint cartilage.
For two of these occupational groups with increased risk of HOA, we identified a substantial heterogeneity between results of different studies. These groups will be discussed in detail to explain these different results.
First, we stated the highest risk increase to develop HOA was for men working in agriculture, fishery or forestry with regular long working days, few vacations and different demanding working positions. Due to the large magnitude of the effect and the presence of a dose–response gradient we see evidence of an cause-effect relationship between occupations in agriculture, fishery and forestry and the development of HOA. But despite high prevalence of musculoskeletal disorders [50], the total number of farmers who take time off and seek care [51] is low and it is unclear if farmers, who are very dependent on their mobility, are motivated to accept their situation earlier or to delay THR and continue to work or accept a disability pension. But this evidence is limited by the substantial heterogeneity between the results of different studies. This heterogeneity might be caused by the high variability in the age of farmers, time periods to calculate prevalences, differences in the use of machines to facilitate physically demanding work, daily working time and maximal working time during season [51]. Moreover, some authors propose that work with animal handling might result in an additional immunological stimulation of HOA in contrast to in crop production [52], but other aspects like frequent walking on uneven grounds could also be considered in this context.
Nearly all studies stated an increased risk for HOA by driving vehicles where whole body vibrations may damage cartilage resulting in osteoarthritis. However stated risk increases were heterogeneous. The strength of the vibration transmitted to the skeleton depends on many factors including the vehicle itself, the surface, the sitting posture and whether damping has been built into the seat. In addition, construction machinery and agricultural vehicles cause higher levels of vibration than passenger cars. Our results are in line with the results of a German case–control study [19] which found a relationship between heavily vibrating vehicles and the risk of lumbar disc herniation as well as symptomatic lumbar disc narrowing.
We additionally identified a remarkable risk increase of unskilled and basic level workers compared to workers with higher education (RR 1.89; 95%-CI 1.29 to 2.77). These workers are frequently exposed to lifting heavy loads and carrying out physically demanding repetitive work for long periods due to the specialization of many functions in farming [36] and other jobs. Unskilled workers usually have limited possibilities to adjust their work environment to prevent early sick leave, hospitalization and disability retirement due to HOA. These socioeconomic and resulting health inequality differences have been documented in several studies [53, 54].
The results of this review support the need for advanced preventive measures especially in the affected occupational groups in agriculture, construction and food production. Workplace risk assessments regarding manual handling of (heavy) loads, the job-related need of repetitive body movements and intensive-load working postures like forward trunk inclination and torsion, kneeling, squatting, other manual demanding tasks like pushing and pulling of loads and exposure to vibrations should consider HOA as an adverse health effect. Long lasting, highly intensive, biomechanical or physical workload is associated with a wide range of clinical outcomes, mostly degenerative changes [55]. Therefore, preventive measures are mostly not specific to reducing a single adverse health effect like HOA. Evidence from this review may provide support to offer special preventive strategies and tools to reduce workload, to improve technical equipment and organizational aspects and workers’ knowledge to tackle the demands in these occupations with a high risk to develop HOA. Preventive occupational medicine should include examination of the hip after no more than 15 to 20 years in the identified physically demanding occupations. Early detection and management of HOA might prevent or delay hospital admissions, support return to work and rehabilitation efforts [9], and avoid severe consequences like total hip replacement, disability retirement or occupational disease claims due to HOA.
Limitations
The precision of our results is reduced by heterogeneity of exposed occupational groups with intensive physical strain and non-exposed reference groups. Development of HOA was measured with very different diagnoses including clinical and radiological criteria, THR and disability pension. Some of these endpoints do not include all cases of HOA. This substantial heterogeneity of exposures and diagnosis of HOA resulted in a low precision with a broad range of results. Finally, BMI as important confounder was not.
Our systematic review is restricted to studies with publications in English and German language. Thus, we might have missed studies published in other languages including Chinese and Russian. Despite these limitations, we were able to identify a number of occupations with an increased risk to develop HOA.
Conclusion
Occupations with high physical workload to manually handle heavy loads, with intensive-load working demanding postures, repetitive activities or exposures to vibrations increase the risk of HOA with resulting pain, sick leave, hospital admissions, THR and disability retirement. Evidence from this review may support the discussion to define HOA as an occupational disease and to develop special preventive strategies and technical equipment to reduce the impact of mechanical occupational exposure at work sites with high physical strain .
Supplementary Information
Additional file 1: Table S1. Search strategy in Medline (Ovid). Table S2. Search strategy in Embase. Table S3. Search strategy in the Cochrane Library. Table S4. Search strategy in CINAHL. Table S5. Search strategy in HSE-Line. Table S6. Search in Occupational medicine journals
Additional file 2: Table S7. Characteristics of eligible cohort studies. Table S8. Characteristics of eligible case-control studies. Table S9. Summary of reported results on the association of occupations in agriculture, fishery or forestry and the risk to develop hip osteoarthritis (HOA). Table S10. Summary of reported results on the association of occupations in construction and the risk to develop hip osteoarthritis (HOA). Table S11. Summary of reported results on the association of occupations with whole body vibrations and the risk to develop hip osteoarthritis (HOA). Table S12. Summary of reported results on the association of occupations in metal work and the risk to develop hip osteoarthritis (HOA). Table S13. Summary of reported results on the association of occupations in sales and the risk to develop hip osteoarthritis (HOA). Table S14. Summary of reported results on the association of occupations in gastronomy and the risk to develop hip osteoarthritis (HOA). Table S15. Summary of reported results on the association of occupations in food production and the risk to develop hip osteoarthritis (HOA). Table S16. Summary of reported results on the association of occupations in storage and transportation and the risk to develop hip osteoarthritis (HOA). Table S17. Summary of reported results on the association of occupations in health care and the risk to develop hip osteoarthritis (HOA). Table S18. Summary of reported results on the association of unskilled and basic level labour and the risk to develop hip osteoarthritis (HOA).
Acknowledgements
Not applicable.
Abbreviations
- CI
Confidence Interval
- HOA
Hip osteoarthitis
- RR
Relative risk
- THR
Total hip replacement
Authors' contributions
AB, U B-A, AS and SU developed the methodological concept. AB, U B-A, AS, JH, JW and SU screened study titles and abstracts and examined the full texts for inclusion. AB, JW and SU performed the data analysis from the included articles and evaluated the study quality. All authors participated in interpretation of the study results and in reading and approving the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have confirmed that we have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hunter D, Bierma-Zeinstra S. Osteoarthritis Lancet. 2019;393:1745–1759. doi: 10.1016/S0140-6736(19)30417-9. [DOI] [PubMed] [Google Scholar]
- 2.Katz JN, Arant KR, Loeser RF. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA. 2021;325(6):568–578. doi: 10.1001/jama.2020.22171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tepper S, Hochberg MC. Factors associated with hip osteoarthritis: data from the first National Health and Nutrition Examination Survey (NHANES-1) Am J Epidemiol. 1993;137(10):1081–1088. doi: 10.1093/oxfordjournals.aje.a116611. [DOI] [PubMed] [Google Scholar]
- 4.Van Saase J, Van Romunde L, Cats A, Vandenbroucke J, Valkenburg H. Epidemiology of osteoarthritis: Zoetermeer survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populations. Ann Rheum dis. 1989;48(4):271–80. 10.1136/ard.48.4.271. [DOI] [PMC free article] [PubMed]
- 5.Grubber JM, Callahan LF, Helmick CG, Zack MM, Pollard RA. Prevalence of radiographic hip and knee osteoarthritis by place of residence. J Rheumatol. 1998;25(5):959–63. https://www.ncbi.nlm.nih.gov/pubmed/9598898. [PubMed]
- 6.Muchmore L, Lynch WD, Gardner HH, Williamson T, Burke T. Prevalence of arthritis and associated joint disorders in an employed population and the associated healthcare, sick leave, disability, and workers' compensation benefits cost and productivity loss of employers. J Occup Environ Med. 2003;45(4):369–378. doi: 10.1097/01.jom.0000063621.37065.26. [DOI] [PubMed] [Google Scholar]
- 7.Turkiewicz A, Petersson IF, Bjork J, Hawker G, Dahlberg LE, Lohmander LS, et al. Current and future impact of osteoarthritis on health care: a population-based study with projections to year 2032. Osteoarthr Cartil. 2014;22(11):1826–32. 10.1016/j.joca.2014.07.015. [DOI] [PubMed]
- 8.Bouziri H, Descatha A, Roquelaure Y, Dab W, Jean K. Disentangling the roles of demographic and temporal changes in the incidence and prevalence of musculoskeletal disorders: a systematic review. medRxiv. 2021. 10.1101/2021.09.20.21263840. [DOI] [PMC free article] [PubMed]
- 9.Sundstrup E, Seeberg KGV, Bengtsen E, Andersen LL. A Systematic Review of Workplace Interventions to Rehabilitate Musculoskeletal Disorders Among Employees with Physical Demanding Work. J Occup Rehabil. 2020;30(4):588–612. doi: 10.1007/s10926-020-09879-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aresti N, Kassam J, Nicholas N, Achan P. Hip osteoarthritis. BMj. 2016;354. 10.1136/bmj.i3405 . [DOI] [PubMed]
- 11.Jiang L, Rong J, Wang Y, Hu F, Bao C, Li X, et al. The relationship between body mass index and hip osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2011;78(2):150–155. doi: 10.1016/j.jbspin.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthr Cartil. 2011;19(11):1270–85. 10.1016/j.joca.2011.08.009. [DOI] [PubMed]
- 13.Sandhar S, Smith TO, Toor K, Howe F, Sofat N. Risk factors for pain and functional impairment in people with knee and hip osteoarthritis: a systematic review and meta-analysis. BMJ Open. 2020;10(8):e038720. doi: 10.1136/bmjopen-2020-038720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Altman R, Alarcon G, Appelrouth D, Bloch D, Borenstein D, Brandt K, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505–14. 10.1002/art.1780340502. [DOI] [PubMed]
- 15.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988. https://pubmed.ncbi.nlm.nih.gov/3068365/. [PubMed]
- 16.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergmann A, Bolm-Audorff U, Krone D, Seidler A, Liebers F, Haerting J, et al. Occupational Strain as a Risk for Hip Osteoarthritis. Deutsches Arzteblatt Int. 2017;114(35–36):581–8. 10.3238/arztebl.2017.0581. [DOI] [PMC free article] [PubMed]
- 18.Jensen LK. Hip osteoarthritis: influence of work with heavy lifting, climbing stairs or ladders, or combining kneeling/squatting with heavy lifting. Occup Environ Med. 2008;65(1):6–19. doi: 10.1136/oem.2006.032409. [DOI] [PubMed] [Google Scholar]
- 19.Seidler A, Bergmann A, Jager M, Ellegast R, Ditchen D, Elsner G, et al. Cumulative occupational lumbar load and lumbar disc disease–results of a German multi-center case-control study (EPILIFT) BMC Musculoskelet Disord. 2009;10(1):48. doi: 10.1186/1471-2474-10-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sulsky SI, Carlton L, Bochmann F, Ellegast R, Glitsch U, Hartmann B, et al. Epidemiological evidence for work load as a risk factor for osteoarthritis of the hip: a systematic review. PLoS ONE. 2012;7(2):e31521. doi: 10.1371/journal.pone.0031521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bundeskanzleramt, BMAS. Fifth Ordinance amending the Ordinance on Occupational Diseases [Fünfte Verordnung zur Änderung der Berufskrankheiten-Verordnung]. https://www.bundesrat.de/SharedDocs/drucksachen/2021/0301-0400/388-21.html. Accessed 2 Jul 2021.
- 22.European Commission. Commission Recommendation of 19 September 2003 concerning the European schedule of occupational diseases (notified under document number C(2003) 3297) (Text with EEA relevance) (2003/670/EC). 2003. https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32003H0670&from=EN. Accessed 17 Aug 2021.
- 23.European Commission. Report on the current situation in relation to occupational diseases' systems in EU Member States and EFTA/EEA countries, in particular relative to Commission Recommendation 2003/670/EC concerning the European Schedule of Occupational Diseases and gathering of data on relevant related aspects Luxemburg: European Commission. 2013. https://osha.europa.eu/de/legislation/guidelines/commission-recommendation-concerning-the-european-schedule-of-occupational-diseases. Accessed 17 Aug 2021.
- 24.Messing K, Punnett L, Bond M, Alexanderson K, Pyle J, Zahm S, et al. Be the fairest of them all: challenges and recommendations for the treatment of gender in occupational health research. Am J Ind Med. 2003;43(6):618–629. doi: 10.1002/ajim.10225. [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1371/journal.pmed.1000097. [DOI] [PubMed] [Google Scholar]
- 26.Wells GA, Shea B, O’Connell Da, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford. 2000. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 17 Aug 2021.
- 27.Higgins JPT, Green Se. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] 2011 [Available from: https://handbook-5-1.cochrane.org/.
- 28.Review Manager (RevMan) [Computer program]. Version 5.4, The Cochrane Collaboration, 2020.
- 29.Andersen S, Thygesen LC, Davidsen M, Helweg-Larsen K. Cumulative years in occupation and the risk of hip or knee osteoarthritis in men and women: a register-based follow-up study. Occup Environ Med. 2012;69(5):325–330. doi: 10.1136/oemed-2011-100033. [DOI] [PubMed] [Google Scholar]
- 30.Holmberg S, Thelin A, Stiernström E-L, Svärdsudd K. The impact of physical work exposure on musculoskeletal symptoms among farmers and rural non-farmers. A population-based study. Ann Agric Environ Med. 2003;10(2):179–84. https://pubmed.ncbi.nlm.nih.gov/14677909/. [PubMed]
- 31.Hubertsson J, Turkiewicz A, Petersson IF, Englund M. Understanding Occupation, Sick Leave, and Disability Pension Due to Knee and Hip Osteoarthritis From a Sex Perspective. Arthritis Care Res (Hoboken) 2017;69(2):226–233. doi: 10.1002/acr.22909. [DOI] [PubMed] [Google Scholar]
- 32.Jarvholm B, From C, Lewold S, Malchau H, Vingård E. Incidence of surgically treated osteoarthritis in the hip and knee in male construction workers. Occup Environ Med. 2008;65(4):275–278. doi: 10.1136/oem.2007.033365. [DOI] [PubMed] [Google Scholar]
- 33.Jarvholm B, Lundstrom R, Malchau H, Rehn B, Vingård E. Osteoarthritis in the hip and whole-body vibration in heavy vehicles. Int Arch Occup Environ Health. 2004;77(6):424–426. doi: 10.1007/s00420-004-0528-z. [DOI] [PubMed] [Google Scholar]
- 34.Solovieva S, Kontio T, Viikari-Juntura E. Occupation, Physical Workload Factors, and Disability Retirement as a Result of Hip Osteoarthritis in Finland, 2005–2013. J Rheumatol. 2018;45(4):555–562. doi: 10.3899/jrheum.170748. [DOI] [PubMed] [Google Scholar]
- 35.Thelin A, Holmberg S. Hip osteoarthritis in a rural male population: A prospective population-based register study. Am J Ind Med. 2007;50(8):604–607. doi: 10.1002/ajim.20484. [DOI] [PubMed] [Google Scholar]
- 36.Tüchsen F, Hannerz H, Jensen M, Krause N. Socioeconomic status, occupation, and risk of hospitalisation due to coxarthrosis in Denmark 1981–99. Ann Rheum Dis. 2003;62:1100–5. 10.1136/ard.62.11.1100. [DOI] [PMC free article] [PubMed]
- 37.Vingård E, Alfredsson L, Goldie I, Hogstedt C. Occupation and osteoarthrosis of the hip and knee: a register-based cohort study. Int J Epidemiol. 1991;20(4):1025–1031. doi: 10.1093/ije/20.4.1025. [DOI] [PubMed] [Google Scholar]
- 38.Croft P, Cooper C, Wickham C, Coggon D. Osteoarthritis of the hip and occupational activity. Scand J Work Environ Health. 1992:59–63. https://www.jstor.org/stable/40965967. [DOI] [PubMed]
- 39.Croft P, Coggon D, Cruddas M, Cooper C. Osteoarthritis of the hip: an occupational disease in farmers. BMJ. 1992;304(6837):1269–1272. doi: 10.1136/bmj.304.6837.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elsner G, Nienhaus A, Beck W. Coxarthrosis and occupational work load. Z.f. Gesundheitswiss. 1995;3(2):131–44. 10.1007/BF02959989.
- 41.Franklin J, Ingvarsson T, Englund M, Lohmander S. Association between occupation and knee and hip replacement due to osteoarthritis: a case-control study. Arthritis Res Ther. 2010;12(3):R102. doi: 10.1186/ar3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thelin A, Jansson B, Jacobsson B, Strom H. Coxarthrosis and farm work: a case-referent study. Am J Ind Med. 1997;32(5):497–501. doi: 10.1002/(SICI)1097-0274(199711)32:5<497::AID-AJIM9>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 43.Vingård E, Alfredsson L, Fellenius E, Hogstedt C. Disability Pensions Due to Musculo-Skeletal Disorders among Men in Heavy Occupations A Case-Control Study. Scand J Soc Med. 1992;20(1):31–36. doi: 10.1177/140349489202000107. [DOI] [PubMed] [Google Scholar]
- 44.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harris EC, Coggon D. HIP osteoarthritis and work. Best Pract Res Clin Rheumatol. 2015;29(3):462–482. doi: 10.1016/j.berh.2015.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lievense A, Bierma-Zeinstra S, Verhagen A, Verhaar J, Koes B. Influence of work on the development of osteoarthritis of the hip: a systematic review. J Rheumatol. 2001;28(11):2520–8. https://pubmed.ncbi.nlm.nih.gov/11708427/. [PubMed]
- 47.Seidler A, Lüben L, Hegewald J, Bolm-Audorff U, Bergmann A, Liebers F, et al. Dose-response relationship between cumulative physical workload and osteoarthritis of the hip–a meta-analysis applying an external reference population for exposure assignment. BMC Musculoskelet Disord. 2018;19(1):1–12. doi: 10.1186/s12891-018-2085-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaila-Kangas L, Arokoski J, Impivaara O, Viikari-Juntura E, Leino-Arjas P, Luukkonen R, et al. Associations of hip osteoarthritis with history of recurrent exposure to manual handling of loads over 20 kg and work participation: a population-based study of men and women. Occup Environ Med. 2011;68(10):734–738. doi: 10.1136/oem.2010.061390. [DOI] [PubMed] [Google Scholar]
- 49.Hulshof CT, Pega F, Neupane S, Colosio C, Daams JG, Kc P, et al. The effect of occupational exposure to ergonomic risk factors on osteoarthritis of hip or knee and selected other musculoskeletal diseases: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ Int. 2021;150:106349. doi: 10.1016/j.envint.2020.106349. [DOI] [PubMed] [Google Scholar]
- 50.McMillan M, Trask C, Dosman J, Hagel L, Pickett W, Team SFICS. Prevalence of musculoskeletal disorders among Saskatchewan farmers. J Agromed. 2015;20(3):292–301. 10.1080/1059924x.2015.1042611. [DOI] [PubMed]
- 51.Tonelli S, Culp K, Donham KJ. Prevalence of Musculoskeletal Symptoms and Predictors of Seeking Healthcare among Iowa Farmers. J Agric Saf Health. 2015;21(4):229–39. 10.13031/JASH.21.10825. [DOI] [PubMed]
- 52.Thelin A, Vingard E, Holmberg S. Osteoarthritis of the hip joint and farm work. Am J Ind Med. 2004;45(2):202–209. doi: 10.1002/ajim.10330. [DOI] [PubMed] [Google Scholar]
- 53.Krokstad S, Westin S. Disability in society-medical and non-medical determinants for disability pension in a Norwegian total county population study. Soc Sci Med. 2004;58(10):1837–1848. doi: 10.1016/S0277-9536(03)00409-X. [DOI] [PubMed] [Google Scholar]
- 54.Lampert T, Kroll LE, von der Lippe E, Muters S, Stolzenberg H. Socioeconomic status and health: results of the German Health Interview and Examination Survey for Adults (DEGS1) Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56(5–6):814–821. doi: 10.1007/s00103-013-1695-4. [DOI] [PubMed] [Google Scholar]
- 55.Camp CL, Spiker AM, Zajac JM, Pearson D, Sinatro AM, Dines JS, et al. Decreased Hip Internal Rotation Increases the Risk of Back and Abdominal Muscle Injuries in Professional Baseball Players: Analysis of 258 Player-seasons. J Am Acad Orthop Surg. 2018;26(9):e198–e206. doi: 10.5435/JAAOS-D-17-00223. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Search strategy in Medline (Ovid). Table S2. Search strategy in Embase. Table S3. Search strategy in the Cochrane Library. Table S4. Search strategy in CINAHL. Table S5. Search strategy in HSE-Line. Table S6. Search in Occupational medicine journals
Additional file 2: Table S7. Characteristics of eligible cohort studies. Table S8. Characteristics of eligible case-control studies. Table S9. Summary of reported results on the association of occupations in agriculture, fishery or forestry and the risk to develop hip osteoarthritis (HOA). Table S10. Summary of reported results on the association of occupations in construction and the risk to develop hip osteoarthritis (HOA). Table S11. Summary of reported results on the association of occupations with whole body vibrations and the risk to develop hip osteoarthritis (HOA). Table S12. Summary of reported results on the association of occupations in metal work and the risk to develop hip osteoarthritis (HOA). Table S13. Summary of reported results on the association of occupations in sales and the risk to develop hip osteoarthritis (HOA). Table S14. Summary of reported results on the association of occupations in gastronomy and the risk to develop hip osteoarthritis (HOA). Table S15. Summary of reported results on the association of occupations in food production and the risk to develop hip osteoarthritis (HOA). Table S16. Summary of reported results on the association of occupations in storage and transportation and the risk to develop hip osteoarthritis (HOA). Table S17. Summary of reported results on the association of occupations in health care and the risk to develop hip osteoarthritis (HOA). Table S18. Summary of reported results on the association of unskilled and basic level labour and the risk to develop hip osteoarthritis (HOA).
Data Availability Statement
All data generated or analysed during this study are included in this published article.