Abstract
Background
GLP-1 receptor agonists (GLP-1 RA) and SGLT-2 inhibitors (SGLT-2i) have shown to reduce the risk of major adverse cardiovascular events (MACE), death and worsening nephropathy when added to standard of care. However, these two dug classes differ in efficacy and safety. We compared the effectiveness and safety profile of GLP-1 RA and SGLT-2i in a large and unselected cohort of patients with type 2 diabetes resident in Lombardy from 2015 to 2020.
Methods
Using linkable administrative health databases, we included patients aged 50 years and older initiating GLP-1 RA or SGLT-2i. Clinical events were: death, hospital admission for myocardial infarction (MI), stroke, heart failure (HF), and renal disease as individual and composite outcomes (MACE-3: all cause-death, non-fatal MI, non-fatal stroke; MACE-4: MACE-3 plus unstable angina). Outcomes were evaluated separately in subjects with and without previous cardiovascular (CV) diseases. Treatments were compared using Cox proportional hazards regression model after Propensity Score Matching (PSM) in both intention-to-treat (ITT) and per protocol (PP) analyses. Serious adverse events were also evaluated.
Results
The analysis comprised 20,762 patients per cohort. The ITT analysis showed a significant risk reduction for non-fatal MI (HR 0.77; CI 95% 0.66–0.90), MACE-3 (HR 0.91; CI 95% 0.84–0.98), and MACE-4 (HR 0.92; CI 95% 0.86–0.99) in GLP-1RA compared with SGLT-2i users, while no difference was reported in the incidence of HF hospitalization and stroke between the two cohorts. Similar benefits were found in the subgroup of patients without previous CV diseases only. PP analysis largely confirmed the main results. The incidence of serious adverse events was low in both cohorts (< 1%).
Conclusions
GLP-1RA showed to be equally safe and more effective than SGLT-2i in reducing the risk of MACE-3, MACE-4 and MI. This study adds to the growing body of real-world evidence addressing the specific clinical properties of GLP-1RA and SGLT-2i in everyday practice to tailor treatment to the individual patient.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12933-022-01572-y.
Keywords: Glucagon-like peptide-1 receptor agonists, Sodium-glucose cotransporter-2 inhibitors, Cardiovascular outcomes, Renal disease, Death
Introduction
Cardiovascular outcome trials (CVOT) conducted over the past few years in patients with type 2 diabetes (T2D) have shown that GLP-1 receptor agonists (GLP-1 RA) and SGLT-2 inhibitors (SGLT-2i) reduced the risk of major adverse cardiovascular events (MACE), all-cause mortality and worsening nephropathy [1, 2]. However, GLP-1RA and SGLT-2i displayed several differences in terms of efficacy and safety. Specifically, in these placebo-controlled trials, GLP-1 RA were associated with a remarkable stroke risk reduction as opposed to the neutral effect of SGLT-2i, whereas SGLT-2i exerted a more prominent benefit on hospitalization for heart failure and adverse kidney outcomes [3–5]. With respect to safety and tolerability, gastrointestinal adverse events represent the most frequently reported side effects of GLP-1 RA [5], while genital infections, volume depletion and increased risk of ketoacidosis occur more frequently with SGLT-2i, sometimes leading to drug discontinuation [5, 6]. The subsequent evidence from real-world studies is in line with the results from CVOT, confirming the efficacy and safety profile of GLP-1 RA and SGLT-2i [7–10].
Recent guidelines recommend the initiation of GLP-1 RA or SGLT-2i in patients with high CV risk or in those with established atherosclerotic CV disease, regardless of baseline HbA1c levels [11]. Instead, SGLT-2i should be preferred in patients with heart failure or CKD and albuminuria [11]. Currently, there are no available head-to-head randomized trials comparing the effects of GLP-1RA and SGLT-2i on CV or renal outcomes; hence, despite their recognized limitations—such as the lack of randomization, low quality control surrounding data collection, and susceptibility to multiple sources of bias for comparing outcomes [12]—real-world data may provide guidance in understanding and exploiting the specific clinical properties of these two drug classes. Indeed, several real-world studies (RWS) have been recently carried out in different countries and populations mostly focusing on CV rather than kidney outcomes [13–19]; these studies have suggested an overall similar benefit of GLP-1 RA and SGLT-2i on CV composite endpoints [20].
In this study, we have analyzed the effectiveness and safety profile of first time-users of GLP-1 RA in comparison with first time-users of SGLT-2i from 2015 to 2020 in a routine clinical setting in Lombardy, the most populated Italian region.
Methods
This analysis used linkable administrative health databases of the Lombardy region, which include demographic data of all residents and information on hospital records and drug prescriptions reimbursed by National health System. Data are available for about 10 million inhabitants of Lombardy from 2000 to 2020. Access to data is allowed within the agreement between the Istituto di Ricerche Farmacologiche Mario Negri (IRFMN) and Regional Health Ministry of Lombardy.
Subjects with T2D aged 50 years and older were included if they had at least two prescriptions of a GLP-1RA or a SGLT-2i (ATC code A10*) from January 1, 2015, to December 31, 2019 (from 2015 onward, a relevant number of SGLT-2i prescriptions was observed in the Italian market), and no prior exposure to any medications belonging to the same drug classes in the previous five years before entering study cohorts.
Subjects were split into two study cohorts according to the first exposure (index date) to GLP-1RA or SGLT-2i, respectively. A propensity score matching (PSM) in a 1:1 ratio of GLP-1 RA with SGLT-2i users was applied to reduce confounding due to imbalance in study covariates, considering all the variables reported in Table 1.
Table 1.
Baseline characteristics of matched population by treatments status from 2015 to 2019
| Variables | Cohorts | ||
|---|---|---|---|
| GLP-1 RA (N = 20,762) | SGLT-2i (N = 20,762) | Standardized differences | |
| Mean age (+ SD) | 66.30 ± 8.60 | 66.36 ± 8.25 | − 0.00 |
| Gender (Female) | 8318 (40.1) | 8334 (40.1) | − 0.00 |
| Comorbidities of interest, n (%) (in the previous 5 years) | |||
| Cerebrovascular disease | 795 (3.8) | 785 (3.8) | 0.00 |
| Cardiovascular disease | 2659 (12.8) | 2660 (12.8) | − 0.00 |
| Heart failure | 791 (3.8) | 821 (4.0) | 0.00 |
| Peripheral vascular disease | 655 (3.1) | 655 (3.1) | 0.00 |
| Lower limb complication | 172 (0.8) | 180 (0.9) | − 0.00 |
| Renal disease | 347 (1.7) | 337 (1.6) | 0.00 |
| Neuropathy | 246 (1.2) | 198 (0.9) | 0.02 |
| Diabetic retinopathy | 17 (0.1) | 17 (0.1) | 0.00 |
| Chronic obstructive pulmonary disease | 502 (2.4) | 481 (2.3) | 0.00 |
| Cancer | 1513 (7.3) | 1397 (6.7) | 0.02 |
| Antihyperglycemic drugs, n (%) (in the previous 5 years) | |||
| GLP-1 RA | 0 (0.0) | 1399 (6.7) | − 0.38 |
| SGLT-2i | 0 (0.0) | 0 (0.0) | 0.00 |
| Insulin | 5429 (26.2) | 5414 (26.1) | 0.00 |
| Other AHAs | 19.834 (95.5) | 19.609 (94.4) | 0.04 |
| Metformin | 18,344 (88.3) | 18.323 (88.2) | 0.00 |
| Sulfonylureas | 10.142 (48.8) | 10.167 (49.0) | − 0.00 |
| Glinides | 2128 (10.2) | 2081 (10.0) | 0.00 |
| Glitazones | 4289 (20.7) | 4276 (20.6) | 0.00 |
| Acarbose | 1739 (8.4) | 1707 (8.2) | 0.00 |
| DDP-4i | 7391 (35.6) | 7402 (35.6) | − 0.00 |
| N. of antihyperglycemic drug classes, median [IQR] | 2.0 (1–3) | 2.0 (1–3) | 0.16 |
| Patients with no previous anti-hyperglycemic drug treatment, n (%) | 928 (4.5) | 1148 (5.5) | 0.04 |
| Other medications of interest, n (%) | |||
| Antihypertensive drugs | 16.626 (80.1) | 16.550 (79.7) | 0.00 |
| ACE-I/ARBS | 14.044 (67.6) | 14.002 (67.4) | 0.00 |
| Lipid lowering drugs | 13.548 (65.2) | 13.529 (65.2) | 0.00 |
| Antiplatelet drugs | 6757 (32.5) | 6731 (32.4) | 0.00 |
| Oral anticoagulant drugs | 1426 (6.9) | 1429 (6.9) | 0.00 |
| DDCI Index, median [IQR] | 4 (2.7) | 4 (2.7) | 0.00 |
| Hospital admission, mean (± SD) | 1.2 (± 1.7) | 1.2 (± 1.7) | 0.00 |
| Duration of diabetes, n (%) | |||
| 0–4 | 5106 (24.6) | 5131 (24.7) | 0.00 |
| 5–9 | 5185 (25.0) | 5142 (24.8) | |
| 10–14 | 5265 (25.4) | 5242 (25.3) | |
| 15 + | 5206 (25.1) | 5245 (25.3) | |
| Median [q1-q3] | 10 (5–15) | 10 (5–15) | 0.00 |
GLP-1 RA glucon-like peptide-1 receptor agonists, SGLT-2i sodium glucose cotransporter 2 inhibitors
AHAs antihyperglycemic agents, DPP-4i dipeptidyl peptidase-4 inhibitors, ACE-I angiotensin-converting enzyme inhibitors
ARBs angiotensin II receptor agonist blockers, DCCI Drug Derived Complexity Index, SD standard deviation, IQR interquartile range
The adequacy of PSM was assessed by standardized mean difference (SDM) of post-matching patients’ characteristics. Good balance is conventionally set at SMD < 0.10. Information on history of comorbidities (collected through hospitalization), previous exposure to the medications of interest, any hospital admissions, Drug Derived Complexity Index (DDCI) [21], and duration of diabetes were gathered as reported in Table 1. A sensitivity analysis was performed on subjects treated with insulin in the 12 months before entering study cohort (Additional file 1). Hospitalization and pharmacy prescriptions were collected according to the international classification of diseases, ninth revision, and Anatomic Therapeutic Chemical classification code, respectively (Additional file 2, Appendix).
All subjects were followed-up starting from the first prescription of GLP-1RA or SGLT-2i until the occurrence of one of the following outcomes: death from any cause, hospital admission (as primary diagnosis) for myocardial infarction (MI), stroke (both ischemic or hemorrhagic), heart failure (HF), and renal disease as primary diagnosis (patients with advanced renal disease). Clinical events were also considered as composite outcomes (MACE-3: all cause-death, non-fatal MI, non-fatal stroke; MACE-4: all cause-death, non-fatal MI, non-fatal stroke, unstable angina). Safety was evaluated by retrieving data regarding the occurrence of hospitalization, as primary diagnosis, for hypoglycemia, ketoacidosis, diabetic coma, amputations, acute renal failure, syncope, and fractures.
Statistical analysis
Descriptive statistic was reported as mean (± SD), number (%), or median (IQR). Outcomes were calculated as number of events and percentages and, the Cox proportional hazards regression model was used to estimate hazard ratio (HRs) with 95% confidence interval. Outcomes were analyzed by intention-to-treat (ITT) and stratified also according to pre-existing CV diseases (hospitalization for cardio-cerebrovascular disease or peripheral vascular disease in the five years before entering study cohort). Outcomes were adjusted for variables with a SDM ≥ 0.10. A further analysis was performed in a subgroup of subjects who were exposed to insulin in the 12-month period before entering study cohort and were excluded from the main analysis after PSM. In addition, a per protocol (PP) analysis was performed in patients who did not discontinue GLP-1RA or SGLT-2i (discontinuation was defined as no prescription for 7 months after the last refill).
Results
A total of 61,431 first users of GLP-1RA or SGLT-2i were identified between January 1, 2015, and December 31, 2019: 21,960 (35.7%) in the GLP-1RA cohort and 39,471 (64.2%) in the SGLT-2i cohort. After the PSM, 20,762 patients per cohort were included in the analysis. All variables considered in the PSM were well-balanced (all standardized differences were < 0.1) except for higher previous exposure to GLP-1RA in SGLT-2i first-users (Table 1).
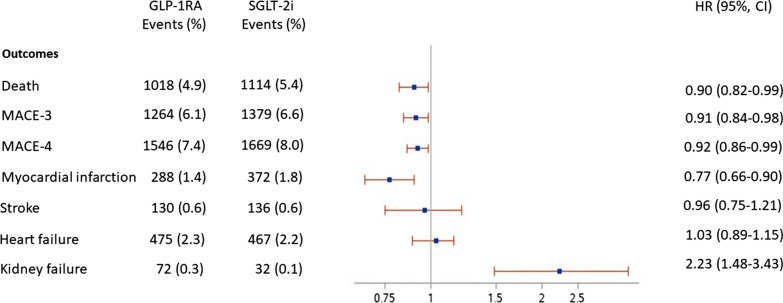
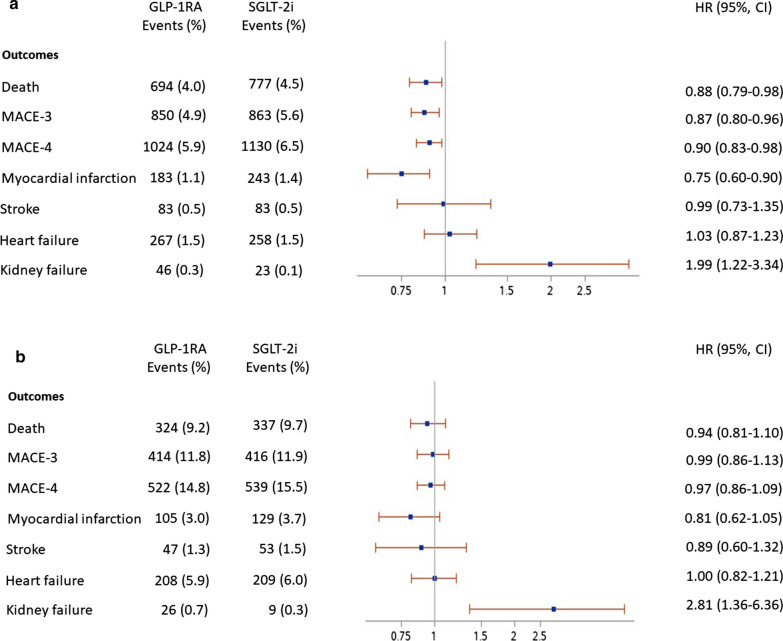
The mean follow-up time was similar for both cohorts (2.78 ± 1.30 years for the GLP-1RA cohort and 2.77 ± 1.37 years for the SGLT-2i cohort). The ITT analysis showed a significant risk reduction for non-fatal MI (HR 0.77; CI 95% 0.66–0.90), MACE-3 (HR 0.91; CI 95% 0.84–0.98), and MACE-4 (HR 0.92; CI 95% 0.86–0.99) in GLP-1RA vs. SGLT-2i first-users (Fig. 1). No difference was observed in the risk of hospitalization for HF and stroke between the two cohorts. A lower prevalence of being hospitalized for renal disease was observed in SGLT-2i first-users as compared to GLP-1RA first-users (0.1% vs. 0.3%). Notably, the risk reduction in death, MACE-3, MACE-4, and MI was evident in the subgroup of subjects without previous CV diseases as opposed to those with a previous hospitalization for CV diseases (Fig. 2A, B).
Fig. 1.
Number of events and hazard ratio (CI 95%), for death and clinical outcomes in matched populations according treatment status (ITT analysis). GLP-1RA Glucagon-like peptide-1 receptor agonists, SGLT-2i Sodium glucose transporter-2 inhibitors, MACE-3 All cause death, non-fatal myocardial infarction, non-fatal stroke, MACE-4 All-cause death, non-fatal myocardial infarction, non-fatal stroke, unstable angina
Fig. 2.
A Number of events and hazard ratio (CI 95%), for death and clinical outcomes in matched populations without previous cardiovascular disease according to treatment status. B Number of events and hazard ratio (CI 95%), for death and clinical outcomes in matched populations with previous cardiovascular disease according to treatment status. GLP-1RA glucagon-like peptide-1 receptor agonists, SGLT-2i sodium glucose transporter-2 inhibitors, MACE-3 all cause death, non-fatal myocardial infarction, non-fatal stroke, MACE-4 all-cause death, non-fatal myocardial infarction, non-fatal stroke, unstable angina
We also carried out a PP analysis in 58.1% GLP-1RA and 55.2% SGLT-2i first-users who remained adherent to treatment (Table 2). A similar trend in the risk reduction of MACE-4, as in the ITT analysis, was observed, and a statistically significant risk reduction was seen for MI (HR 0.70, 95% CI 0.57–0.85) and MACE-3 (HR 0.88, 95% CI 0.79–0.98) in the GLP-1RA cohort compared to the SGLT-2i cohort. As in the ITT analysis, GLP-1RA initiators were at higher risk of hospitalization for renal disease compared to SGLT-2i (HR 2.23, CI 95% 1.48–3.43).
Table 2.
Number of events and hazard ratio (CI 95%), for death and clinical outcomes in matched populations according to treatment status (PP analysis)
| Outcomes | Cohort | ||
|---|---|---|---|
| GLP-1 RA N = 12,062 N (%) | SGLT-2i N = 11,470 N (%) | HR (CI95%) | |
| Death | 528 (4.4) | 555 (4.8) | 0.89 (0.79–1.00) |
| Mace3 | 690 (5.7) | 736 (6.4) | 0.88 (0.79–0.98) |
| Mace4 | 881 (7.3) | 917 (8.0) | 0.91 (0.83–1.00) |
| Myocardial infarction | 170 (1.4) | 228 (2.0) | 0.70 (0.57–0.85) |
| Stroke | 71 (0.6) | 82 (0.7) | 0.82 (0.60–1.13) |
| Heart failure | 277 (1.7) | 238 (2.0) | 1.11 (0.93–1.32) |
| Renal disease | 36 (0.3) | 11 (0.1) | 3.04 (1.60–6.20) |
GLP-1RA glucagon-like peptide-1 receptor agonists, SGLT-2i sodium glucose transporter-2 inhibitors;
MACE-3 all cause death, non-fatal myocardial infarction, non-fatal stroke, MACE-4 all-cause death, non-fatal myocardial infarction, non-fatal stroke, unstable angina
A subgroup of subjects treated with insulin in the 12-month period before entering study cohort, likely reflecting individuals with an advanced disease, was also computed after PSM (N = 5,529 in both cohorts; Additional file 1: Table S1). In this subgroup, after adjustment for the variables whose standardized differences were > 10%, including age, duration of diabetes, renal disease, and DDCI-Index, point estimates for the risk of MACE-3, MACE-4, MI and stroke favored new users of GLP-1RA versus SGLT-2i although this difference was not statistically significant (Additional file 1: Table S2).
During follow-up, the incidence of serious adverse events was relatively low in each group (i.e., less than 1%). Fractures (GLP-1 RA 1.16%; SGLT-2i 1.17%) and syncope (GLP-1 RA 0.34%; SGLT-2i 0.35%) were more frequently registered in both cohorts (Table 3).
Table 3.
Frequency of serious adverse events according treatment status from 2015 to 2019
| Events | Cohorts | |
|---|---|---|
| GLP-1RA (N = 20,762) N (%) | SGLT-2i (N = 20,762) N (%) | |
| Hypoglycemia | 11 (0.05) | 1 (0.00) |
| Ketoacidosis | 14 (0.07) | 18 (0.09) |
| Diabetic coma | 5 (0.02) | 7 (0.03) |
| Acute kidney failure | 12 (0.06) | 2 (0.01) |
| Syncope | 70 (0.34) | 72 (0.35) |
| Fractures | 241 (1.16) | 243 (1.17) |
| Amputations | 53 (0.26) | 67 (0.32) |
GLP-1RA glucagon-like peptide-1 receptor agonists, SGLT-2i sodium glucose transporter-2 inhibitors;
MACE-3 all cause death, non-fatal myocardial infarction, non-fatal stroke, MACE-4 all-cause death, non-fatal myocardial infarction, non-fatal stroke, unstable angina
Discussion
In this analysis, new users of GLP-1RA displayed a significantly lower risk of non-fatal MI, MACE-3, and MACE-4 with respect to SGLT-2i initiators. This benefit appeared to be driven by the favorable effect of GLP-1RA versus SGLT-2i in patients without established CV disease. The overall neutral effect of SGLT-2i on MACE reduction in patients in primary prevention had already been suggested by a meta-analysis of SGLT-2i CVOT [1]. On the other hand, while GLP-1RA failed to demonstrate significant CV protection in patients without overt CV disease in another comprehensive systematic review and meta-analysis [2], the REWIND trial, enrolling 68.5% of individuals without established CV disease, proved the CV superiority of dulaglutide compared to placebo in both primary and secondary prevention cohorts with a similar MACE HR (p for interaction = 0.97) [22]. Therefore, GLP-1RA may be more effective than SGLT-2i in reducing MACE over a large spectrum of CV risk.
It should be acknowledged that in the present study the definition of established CV disease differed from that used in CVOT, as only patients with a hospitalization for a CV event within the last 5 years were considered, likely resulting in an apparent increased CV risk of the cohort without overt CV disease. The CV protective effects of GLP-1RA have been extensively investigated in both pre-clinical studies as well as in human RCT and RWS [23], and their ability to ameliorate early phases of the atherosclerotic process, such as inflammation, endothelial dysfunction and intima-media thickening, as well as to improve circulating stem cells functions, has been suggested [24].
The anti-atherosclerotic effect might at least partially explain why GLP-1RA could reduce CV outcomes vs. SGLT-2i in people without overt CV disease. A study recently published by Wright et al. [25] showed that in comparison with other combination regimens, the use of GLP-1RA was associated with a 7% risk reduction of major adverse cardiac and cerebrovascular events in people with T2D without CV disease. However, an increasing body of evidence, coming mostly from preclinical studies, highlighted that also SGLT-2i might exert beneficial effects on inflammation, macrophage polarization and arterial-flow mediated dilation [26].
In a recent systematic review and meta-analysis of RWS, no differences in the occurrence of composite CV outcomes and MACE were found between new users of SGLT-2i and GLP-1RA [20]. Indeed, the studies by Patorno et al. [27], enrolling the largest population to date, and Longato et al. [13] were the only ones to detect a significantly lower risk of composite CV outcome occurrence (hospitalization for MI or stroke and all-cause death or myocardial infarction or stroke, respectively) in SGLT-2i compared to GLP-1RA new users. However, Patorno et al. and Longato et al. found a significant CV benefit in SGLT-2i initiators in comparison with GLP-1 RA initiators in the cohort of patients in secondary prevention. It should be noted that RWS, such as the retrospective observational study of Longato et al., differ in the definition of the investigated composite CV outcomes as well as the criteria according to which patients are defined as affected from established CV disease, making direct study comparisons difficult. For instance, in the study by Patorno et al., patients were considered as in secondary prevention if diagnosed with chronic ischemic heart disease or peripheral artery disease or related procedures, heart failure, ischemic stroke, or lower extremity amputation in the 12 months before inclusion [27].
In our analysis, in the subgroup of new users of GLP-1RA and SGLT-2i treated with insulin in the previous 12 months, likely at a more advanced stage of diabetes, both cohorts displayed a similar risk of CV events occurrence. In a meta-analysis of CVOT with SGLT-2i and GLP-1RA, patients on background insulin therapy had a higher CV event rate than those not on insulin [28], reinforcing the notion that GLP-1RA may be more effective than SGLT-2i only in patients without overt CV disease.
No significant difference in hospitalization for HF was found between the two cohorts, whereas in previous in RWS SGLT-2i seem to be associated with lower risk of heart failure and total mortality comparing new users of SGLT-2i and GLP-1RA [17–19]. SGLT-2i displayed an unparalleled benefit on HF-related outcomes in randomized controlled trials regardless of the baseline cardio-renal risk of the enrolled population [29]; accordingly, a meta-analysis of RWS showed that SGLT-2i were more effective than GLP-1RA on prevention of HF worsening [30]. On the other hand, albeit to a lesser extent, GLP-1RA have also been proven beneficial, significantly reducing HF hospitalization by 11% compared to placebo in CVOT [2] and by 12% compared to other glucose-lowering drugs except for SGLT-2i in RWS [20]. Interestingly, in three nested case–control studies involving 336,334 T2D patients without previous CV disease and HF, Wright et al. have recently shown that GLP-1RA were associated with a 18% risk reduction of HF compared to other glucose-lowering drugs [25]. However, Natali et al. recently reviewed the available clinical studies on GLP-1R agonism and left ventricular function, concluding that its role is still unclear in patients with both preserved or reduced left ventricle ejection fraction [30], despite the encouraging results of preclinical studies [31]. Further evidence is warranted to better understand the potential benefit of GLP-1RA in patients with HF; relevant to this question, the STEP-HFpEF trial is currently assessing the effect of semaglutide 2.4 mg once weekly in patients affected by HF with preserved ejection fraction (NCT04788511).
In our study, GLP-1RA initiators had a twofold risk to be hospitalized for renal disease compared to SGLT-2i. This result could be due to a higher prevalence of patients with a reduced renal function in GLP-1 RA group related to the different indications of these two drug classes. Indeed up to 2019 SGLT-2i could be prescribed only in patients with eGFR > 60 ml/min/1.73m2 while GLP-1 RA in those with eGFR up to 30 and more recently up to 15 ml/min/1.73m2. To date, only Lugner et al. investigated the renal composite outcome occurrence in GLP-1RA and SGLT-2i initiators, finding no significant differences between groups, even though point estimates for most kidney outcomes favoured SGLT-2i initiators [16]. Lugner et al. enrolled a population with preserved renal function (eGFR > 90 ml/min/1.73m2) [16], while the baseline eGFR of the patients included in the present study is unknown due to the use of claims data. Even though the proportion of patients with advanced and or acute renal disease at baseline was similar in the two cohorts according to the well-balanced PSM, we cannot exclude that SGLT-2i initiators could have had a better baseline renal function. The CVOT have been instructive on the SGLT-2i-mediated remarkable 38% reduction of hard kidney outcomes [1], hence SGLT-2i are currently preferred in patients with CKD and albuminuria [32, 33]. Nonetheless, GLP-1RA were also able to reduce the risk of broad kidney endpoints including new-onset macroalbuminuria by 21% [2]; in addition, dulaglutide exhibited a significant reduction in the risk of eGFR decline in exploratory analyses of the REWIND and AWARD-7 trials [22, 34]. Specifically, in AWARD-7, dulaglutide was associated with a risk reduced the of 40% eGFR decline or end stage kidney disease. This was most evident among participants with macroalbuminuria, who had a 75% risk reduction, suggesting a potentially pronounced effect of dulaglutide to delay progression in participants with advanced CKD [34]. Finally, during follow-up, the incidence of serious adverse events (hypoglycemia, ketoacidosis, diabetic coma, amputations, acute kidney failure, syncope, and fractures) was relatively low in each group (less than 1%).
Strengths and limitations
The large and unselected population, representing the real clinical setting, and the longer follow-up duration compared to similar studies [20] represent the main strengths of this study.
Also, besides the study specifically conducted in elderly patients by Patorno et al. [14], the population enrolled in this study was averagely older (mean age 66.3 years) than that of previous RWS (mean age ranging from 50 years in [15] to 63 years in [13], adding valuable insight on a subgroup of patients widely represented in everyday clinical practice.
A relevant limitation is represented by the possibility of residual confounding since clinical variables, such as HbA1c, eGFR, NYHA classification, body weight, and blood pressure, and the results of outpatient visits, were unavailable with claims analysis. Moreover, concomitant antihyperglycemic drugs may have changed during follow-up, potentially affecting patients’ CV and renal risk. In addition, analyzing data from a single Region cannot be generalized to the overall Italian population.
In conclusion, in the present study, GLP-1RA showed to be equally safe and more effective in reducing the risk of MACE-3, MACE-4 and MI when compared to SGLT-2i. On the other hand, GLP-1RA initiation was associated with a similar risk of hospitalization for HF and an increased risk of hospitalization for renal disease compared to SGLT-2i. This study adds to the growing body of real-world evidence, addressing the need to better understand the specific abilities of GLP-1RA and SGLT-2i in everyday clinical practice to tailor treatment to the individual patient.
Supplementary Information
Additional file 1: Table S1. Baseline characteristics of matched population by treatment status from 2015 to 2019. Table S2. Events, incidence rate, hazard ratio (CI 95%) for death and clinical outcomes in matched populations previously treated with insulin, according to treatment status.
Acknowledgements
We thank Giuseppe Preziosi, Monica Arivetti and Giovanna Rigotti from ARIA S.p.A, Alfredo Bevilacqua from Laife Reply S.p.A., Marco D. Forlani from T Bridge—BV Tech S.p.A and Igor Monti from Istituto di Ricerche Farmacologiche Mario Negri IRCCS who kindly assisted us with data collection.
Author contributions
Study concept and design: MB, AF, MCR, SG, FG; Acquisition of data: IF; Analysis of data: PC, GM; Interpretation of data: MB, AF, MCR, MT, IC, SG, FG; Drafting the manuscript: MB, AF, IC, FG; Critical revision of the manuscript for important intellectual content: MCR, MT, PC, SG, IF. All authors read and approved the final manuscript.
Funding
This study was supported by grants from the Health Ministry of the Lombardy region as part of the EPIFARM-Pharmaco-epidemiology Agreement between the Istituto di Ricerche Farmacologiche Mario Negri IRCCS and the Lombardy region.
Availability of data and materials
The data that support the findings of this study are available from Lombardy Region, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the Lombardy Region upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Marta Baviera, Andreana Foresta, Pierluca Colacioppo, Giulia Macaluso, Maria Carla Roncaglioni, Mauro Tettamanti, Ida Fortino, Irene Caruso declare no conflict of interest. Francesco Giorgino receives research support from Eli Lilly, Lifescan, and Roche Diabetes Care; is a consultant for Boehringer Ingelheim, Lifescan, Merck Sharp & Dohme, Sanofi, AstraZeneca, and Roche Diabetes Care; and is on the advisory boards for AstraZeneca, Eli Lilly, Novo Nordisk, Roche Diabetes Care, and Sanofi. Stefano Genovese received research funding from Novartis and has been a consultant for, or received honoraria from Abbott Diabetes Care, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Hikma Pharmaceuticals, Janssen, Menarini, Merck Sharp & Dohme, Molteni Farmaceutici, Mundipharma, Novartis, Novo Nordisk, Sanofi, Takeda, Teva and Zentiva.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Marta Baviera and Andreana Foresta contributed equally to this work
References
- 1.McGuire DK, Shih WJ, Cosentino F, Charbonnel B, Cherney DZI, Dagogo-Jack S, Pratley R, Greenberg M, Wang S, Huyck S, Gantz I, Terra SG, Masiukiewicz U, Cannon CP. Association of SGLT2 inhibitors with cardiovascular and kidney outcomes in patients with type 2 diabetes: a meta-analysis. JAMA Cardiol. 2021;6(2):148–158. doi: 10.1001/jamacardio.2020.4511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sattar N, Lee MMY, Kristensen SL, Branch KRH, Del Prato S, Khurmi NS, Lam CSP, Lopes RD, McMurray JJV, Pratley RE, Rosenstock J, Gerstein HC. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol. 2021;9(10):653–662. doi: 10.1016/S2213-8587(21)00203-5. [DOI] [PubMed] [Google Scholar]
- 3.Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Furtado RH, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Bhatt DL. Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus. Circulation. 2019;139(17):2022–2031. doi: 10.1161/CIRCULATIONAHA.118.038868. [DOI] [PubMed] [Google Scholar]
- 4.Li S, Vandvik PO, Lytvyn L, Guyatt GH, Palmer SC, Rodriguez-Gutierrez R, et al. SGLT-2 inhibitors or GLP-1 receptor agonists for adults with type 2 diabetes: a clinical practice guideline. BMJ. 2021;11(373):n1091. doi: 10.1136/bmj.n1091. [DOI] [PubMed] [Google Scholar]
- 5.Seferović PM, Coats AJS, Ponikowski P, Filippatos G, Huelsmann M, Jhund PS, et al. European Society of Cardiology/Heart Failure Association position paper on the role and safety of new glucose-lowering drugs in patients with heart failure. Eur J Heart Fail. 2020;22(2):196–213. doi: 10.1002/ejhf.1673. [DOI] [PubMed] [Google Scholar]
- 6.Toyama T, Neuen BL, Jun M, Ohkuma T, Neal B, Jardine MJ, Heerspink HL, Wong MG, Ninomiya T, Wada T, Perkovic V. Effect of SGLT2 inhibitors on cardiovascular, renal and safety outcomes in patients with type 2 diabetes mellitus and chronic kidney disease: a systematic review and meta-analysis. Diabetes Obes Metab. 2019;21(5):1237–1250. doi: 10.1111/dom.13648. [DOI] [PubMed] [Google Scholar]
- 7.Kosiborod M, Cavender MA, Fu AZ, et al. Investigators and Study Group. Lower risk of heart failure and death in patients initiated on sodium-glucose cotransporter-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL study (Comparative Effectiveness of Cardiovascular Outcomes in New Users of Sodium-Glucose Cotransporter-2 Inhibitors) Circulation. 2017;136(3):249–259. doi: 10.1161/CIRCULATIONAHA.117.029190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kosiborod M, Lam CSP, Kohsaka S, et al. CVD-REAL Investigators and Study Group. Cardiovascular events associated with SGLT-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL 2 study. J Am Coll Cardiol. 2018;71(23):2628–2639. doi: 10.1016/j.jacc.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 9.Birkeland KI, Jørgensen ME, Carstensen B, et al. Cardiovascular mortality and morbidity in patients with type 2 diabetes following initiation of sodium-glucose co-transporter-2 inhibitors versus other glucose-lowering drugs (CVD-REAL Nordic): a multinational observational analysis. Lancet Diabetes Endocrinol. 2017;5(9):709–717. doi: 10.1016/S2213-8587(17)30258. [DOI] [PubMed] [Google Scholar]
- 10.Baviera M, Genovese S, Lepore V, Colacioppo P, Robusto F, Tettamanti M, D'Ettorre A, Avanzini F, Fortino I, Nicolucci A, Roncaglioni MC. Lower risk of death and cardiovascular events in patients with diabetes initiating glucagon-like peptide-1 receptor agonists or sodium-glucose cotransporter-2 inhibitors: A real-world study in two Italian cohorts. Diabetes Obes Metab. 2021;23:1484–1495. doi: 10.1111/dom.14361. [DOI] [PubMed] [Google Scholar]
- 11.Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C, D’Alessio DA, Davies MJ. 2019 update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the american diabetes association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes. 2020;43(2):487–493. doi: 10.2337/dci19-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen AT, et al. Why do we need observational studies of everyday patients in the real-life setting? Eur Heart J Suppl. 2015 doi: 10.1093/eurheartj/suv035. [DOI] [Google Scholar]
- 13.Longato E, Di Camillo B, Sparacino G, Gubian L, Avogaro A, Fadini GP. Cardiovascular outcomes of type 2 diabetic patients treated with SGLT-2 inhibitors versus GLP-1 receptor agonists in real-life. BMJ Open Diabetes Res Care. 2020;8(1):e001451. doi: 10.1136/bmjdrc-2020-001451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patorno E, Pawar A, Bessette LG, Kim DH, Dave C, Glynn RJ, Munshi MN, Schneeweiss S, Wexler DJ, Kim SC. Comparative effectiveness and safety of sodium-glucose cotransporter 2 inhibitors versus glucagon-like peptide 1 receptor agonists in older adults. Diabetes Care. 2021;44(3):826–835. doi: 10.2337/dc20-1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeRemer CE, Vouri SM, Guo J, Donahoo WT, Winterstein AG, Shao H. Comparing cardiovascular benefits between GLP-1 receptor agonists and SGLT2 inhibitors as an add-on to metformin among patients with type 2 diabetes: a retrospective cohort study. J Diabetes Complications. 2021;35(9):107972. doi: 10.1016/j.jdiacomp.2021.107972. [DOI] [PubMed] [Google Scholar]
- 16.Nørgaard CH, Starkopf L, Gerds TA, Vestergaard P, Bonde AN, Fosbøl E, Køber L, Wong ND, Torp-Pedersen C, Lee C-J-Y. Cardiovascular outcomes with GLP-1 receptor agonists vs SGLT-2 inhibitors in patients with type 2 diabetes. Eur Heart J Cardiovasc Pharmacother. 2021 doi: 10.1093/ehjcvp/pvab053. [DOI] [PubMed] [Google Scholar]
- 17.Lugner M, Sattar N, Miftaraj M, Ekelund J, Franzén S, Svensson AM, Eliasson B. Cardiorenal and other diabetes related outcomes with SGLT-2 inhibitors compared to GLP-1 receptor agonists in type 2 diabetes: nationwide observational study. Cardiovasc Diabetol. 2021;20(1):67. doi: 10.1186/s12933-021-01258-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pineda ED, Liao IC, Godley PJ, Michel JB, Rascati KL. Cardiovascular outcomes among patients with type 2 diabetes newly initiated on sodium-glucose cotransporter-2 inhibitors, glucagon-like peptide-1 receptor agonists, and other antidiabetic medications. J Manag Care Spec Pharm. 2020;26(5):610–618. doi: 10.18553/jmcp.2020.26.5.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomsen RW, Knudsen JS, Kahlert J, Baggesen LM, Lajer M, Holmgaard PH, Vedin O, Ustyugova A, Sørensen HT. Cardiovascular events, acute hospitalizations, and mortality in patients with type 2 diabetes mellitus who initiate empagliflozin versus liraglutide: a comparative effectiveness study. J Am Heart Assoc. 2021;10:e019356. doi: 10.1161/JAHA.120.019356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caruso I, Cignarelli A, Sorice GP, Natalicchio A, Perrini S, Laviola L, Giorgino F. Cardiovascular and renal effectiveness of GLP-1 receptor agonists vs other glucose-lowering drugs in type 2 diabetes: a systematic review and meta-analysis of real-world studies. Metabolites. 2022;12(2):183. doi: 10.3390/metabo12020183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robusto F, Lepore V, D'Ettorre A, Lucisano G, De Berardis G, Bisceglia L, Tognoni G, Nicolucci A. The drug derived complexity index (DDCI) predicts mortality, unplanned hospitalization and hospital readmissions at the population level. PLoS ONE. 2016;11(2):e0149203. doi: 10.1371/journal.pone.0149203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, Probstfield J, Riesmeyer JS, Riddle MC, Rydén L, Xavier D, Atisso CM, Dyal L, Hall S, Rao-Melacini P, Wong G, Avezum A, Basile J, Chung N, Conget I, Cushman WC, Franek E, Hancu N, Hanefeld M, Holt S, Jansky P, Keltai M, Lanas F, Leiter LA, Lopez-Jaramillo P, Cardona Munoz EG, Pirags V, Pogosova N, Raubenheimer PJ, Shaw JE, Sheu WH, Temelkova-Kurktschiev T, REWIND Investigators Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394(10193):121–130. doi: 10.1016/S0140-6736(19)31149-3. [DOI] [PubMed] [Google Scholar]
- 23.Giorgino F, Caruso I, Moellmann J, Lehrke M. Differential indication for SGLT-2 inhibitors versus GLP-1 receptor agonists in patients with established atherosclerotic heart disease or at risk for congestive heart failure. Metabolism. 2020;104:154045. doi: 10.1016/j.metabol.2019.154045. [DOI] [PubMed] [Google Scholar]
- 24.Sforza A, Vigorelli V, Rurali E, Perrucci GL, Gambini E, Arici M, Metallo A, Rinaldi R, Fiorina P, Barbuti A, Raucci A, Sacco E, Rocchetti M, Pompilio G, Genovese S, Vinci MC. Liraglutide preserves CD34+ stem cells from dysfunction Induced by high glucose exposure. Cardiovasc Diabetol. 2022;21(1):51. doi: 10.1186/s12933-022-01486-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wright AK, Carr MJ, Kontopantelis E, Leelarathna L, Thabit H, Emsley R, Buchan I, Mamas MA, van Staa TP, Sattar N, Ashcroft DM, Rutter MK. Primary prevention of cardiovascular and heart failure events with SGLT2 Inhibitors, GLP-1 receptor agonists, and their combination in type 2 diabetes. Diabetes Care. 2022;45(4):909–918. doi: 10.2337/dc21-1113. [DOI] [PubMed] [Google Scholar]
- 26.Barraclough JY, Patel S, Yu J, Neal B, Arnott C. The role of sodium glucose cotransporter-2 inhibitors in atherosclerotic cardiovascular disease: a narrative review of potential mechanisms. Cells. 2021;10(10):2699. doi: 10.3390/cells10102699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patorno E, Htoo PT, Glynn RJ, Schneeweiss S, Wexler DJ, Pawar A, Bessette LG, Chin K, Everett BM, Kim SC. Sodium-glucose cotransporter-2 inhibitors versus glucagon-like peptide-1 receptor agonists and the risk for cardiovascular outcomes in routine care patients with diabetes across categories of cardiovascular disease. Ann Intern Med. 2021;174(11):1528–1541. doi: 10.7326/M21-0893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khatib JE, Shao Y, Shi L, Fonseca VA. The association between baseline insulin treatment and cardiovascular events: a meta-analysis. J Endocr Soc. 2020 doi: 10.1210/jendso/bvaa193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caruso I, Giorgino F. SGLT-2 inhibitors as cardio-renal protective agents. Metabolism. 2022;127:154937. doi: 10.1016/j.metabol.2021.154937. [DOI] [PubMed] [Google Scholar]
- 30.Natali A, Nesti L, Tricò D, Ferrannini E. Effects of GLP-1 receptor agonists and SGLT-2 inhibitors on cardiac structure and function: a narrative review of clinical evidence. Cardiovasc Diabetol. 2021;20(1):196. doi: 10.1186/s12933-021-01385-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu Q, Anderson C, Broyde A, Polizzi C, Fernandez R, Baron A, Parkes DG. Glucagon-like peptide-1 and the exenatide analogue AC3174 improve cardiac function, cardiac remodeling, and survival in rats with chronic heart failure. Cardiovasc Diabetol. 2010;16(9):76. doi: 10.1186/1475-2840-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Diabetes Association Professional Practice Committee 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2022. Diabetes Care. 2022;45(Suppl. 1):S125–S143. doi: 10.2337/dc22-S009. [DOI] [PubMed] [Google Scholar]
- 33.Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group Clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2022 doi: 10.1016/j.kint.2020.06.019. [DOI] [Google Scholar]
- 34.Tuttle KR, Rayner B, Lakshmanan MC, Kwan AY, Konig M, Shurzinske L, Botros FT. Clinical outcomes by albuminuria status with dulaglutide versus insulin glargine in participants with diabetes and CKD: AWARD-7 exploratory analysis. Kidney360. 2020;2(2):254–262. doi: 10.34067/KID.0005852020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Baseline characteristics of matched population by treatment status from 2015 to 2019. Table S2. Events, incidence rate, hazard ratio (CI 95%) for death and clinical outcomes in matched populations previously treated with insulin, according to treatment status.
Data Availability Statement
The data that support the findings of this study are available from Lombardy Region, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the Lombardy Region upon reasonable request.