Abstract
Background:
Hepatitis B virus infection is a global health priority, and health-care personnel (HCP) have 10 times higher prevalence than the general population. Seromonitoring identifies those with low titers and vaccine nonresponders with increased risk.
Objective:
The objective of the study was to assess hepatitis B surface antibody (anti-HBs) titers and associated factors among HCP vaccinated against hepatitis B in a teaching hospital in Kerala.
Methods:
A cross-sectional study was done among 454 vaccinated HCP, and anti-HBs antibody titers were assessed by enzyme-linked immunosorbent assay method.
Results:
Participants included 162 (35.7%) doctors, 132 (29.3%) nursing and laboratory personnel, and 160 (35.3%) supporting staff. The mean age was 38.06 ± 11.33 years, and 72% were female. Majority (92.5%, 420) were seroprotected and 78.9% (358) with high (>100 mIU) titers. Moderate (10–100 mIU) and low (<10 mIU) level seroprotection was seen in 13.7% (62) and 7.5% (34), respectively. Incomplete vaccination, >10 years since vaccination, and age >40 years were independent predictors for poor seroprotection, while increasing doses and boosters were positively associated.
Conclusions:
Majority of vaccinated HCP were seroprotected. Incomplete schedules, older age, and prolonged time since vaccination can lead to decline in titers, and periodical seromonitoring should guide hepatitis B revaccination strategies.
Keywords: Health-care personnel, hepatitis B surface antibody titer, Kerala
INTRODUCTION
Hepatitis B virus (HBV) infection is a global health priority, with an estimated prevalence of 257 million affected worldwide. In the WHO South-East Asia Region, 2% of the general population is hepatitis B infected.[1] India, falling in the intermediate endemic zone, is the world's second-largest pool of hepatitis B with 2%–8% of hepatitis B surface antigen (HBsAg) carriers and over 50 million cases.[2]
Hepatitis B is an important occupational hazard for health workers. Blood from persons with HBV infection is the most important vehicle of transmission in the health-care setting.[3] HBV is highly infectious and can be transmitted in the absence of visible blood,[3] and remains infectious on environmental surfaces for at least 7 days.[4] Even though infection control protocols are implemented, HBV infection remains a significant occupational risk. In serologic studies from the United States in the 1970s, health-care personnel (HCP) had a prevalence 10 times greater than the general population.[3] The prevalence among Indian HCP has been reported to range from 10% (1992) to 2.21% (1998) and 1% (2008).[5,6,7]
In 2011, the Advisory Committee on Immunization Practices reaffirmed that unvaccinated and incompletely vaccinated HCP are at high risk and should receive hepatitis B vaccination before potential exposure, and should receive postvaccination serologic testing 1–2 months after completion of the vaccine.[8] According to the Centre for Disease Control (CDC), HCP who have received three-dose primary series of hepatitis B vaccine and tested positive for anti-hepatitis B surface (HBs) (≥10 mIU/mL) are considered to be immune to hepatitis B. HCP who do not respond to vaccination (<10 mIU/ml) are thought to remain susceptible. Hence, serological testing for HBs antibody (anti-HBs) identifies those with low titers and nonresponders and guides the need for further counseling and revaccination. The aim of this study was to assess anti-HBs titers among vaccinated HCP in a teaching hospital in Kerala and to find its association with selected factors such as demography, vaccination status, and exposure risks.
METHODS
A cross-sectional study was done at a teaching hospital in Kerala over 1 year from April 2018. Subjects were HCP, including doctors, nursing staff, laboratory technicians, and supporting staff who had received at least one dose of hepatitis B vaccine and consented for the study. We excluded known HBsAg positives and those who reported as having had HBV infection.
A list of 2030 HCP employed in the hospital (800 doctors, 570 nurses, and 660 supporting staff) was obtained. A probability proportionate to size stratified sampling was adopted with doctors, nursing staff/laboratory technicians, and supporting staff as strata.
Seventy percent of the vaccinated HCP showed adequate antibody titers in a Jodhpur study by Batra et al. (2015).[9] A minimum sample size of 321 at 95% confidence level was estimated using Epi Info StatCalc (CDC).
After written informed consent, participants were interviewed using a schedule. Blood samples were collected by trained staff and anti-HBs titers were assessed by standardized quantitative enzyme-linked immunosorbent assay method (CMIA) in Abbott ARCHITECT i1000sr immunoassay analyzer at an NABL-accredited laboratory. Seroprotection was defined as anti-HBs >10 mIU/ml.
Ethical clearance was obtained from the Institutional Ethics Committee and data confidentiality was ensured. Test results were communicated and those with low anti-HBs titers (<10 mIU/ml) were referred for booster dose and the incompletely vaccinated counseled for vaccination completion.
Data were entered into Microsoft Excel and analyzed using IBM SPSS Statistics for Windows, version 24.0. (Armonk, NY, USA: IBM Corp). Descriptive tables were generated. The level of anti-HBs titers was categorized as low protection (<10 mIU/ml), moderate protection (10–100 mIU/ml), and adequate protection (>100 mIU/ml). Factors influencing the antibody titers were analyzed using Chi-square test and logistic regression.
RESULTS
Four hundred and fifty-four HCP participated whose mean age was 38.06 ± 11.33 years. Almost 72% (326) were female. 35.7% of HCP were doctors, 29.3% included nursing/laboratory personnel, while 35.3% were supporting staff.
Vaccination schedule was complete for 377 (83.1%). Among 77 (16.9%) with incomplete schedules, 68.8% (53) took two doses and 31.2% (24) took a single dose. 72.7% (330) HCP got vaccinated within the past 10 years. Booster doses were taken by 12.3% (56) subjects, of which 91.1%, 5.4%, and 3.6% took 1, 2, and 3 booster doses, respectively.
About 85.5% (388) were involved with high-risk work and 14.5% (66) had a low risk. Almost 89% of doctors, 93% of nursing staff, and 76% of supporting staff were involved in High-risk work category (76.2%, 346) reported past exposures to blood/body fluids, of which 63.6% (220) were multiple exposures. Needlestick injury (44.8%) was the most common exposure, and only 7.8% (27) reported taking postexposure prophylaxis. The safe injection practices were practiced regularly by only 59% of the study population.
The anti HBs titers revealed that majority (92.5%, 420) of HCP were seroprotected. 78.9% (358) had adequate protection, 13.7% (62) had moderate protection, while 7.5% (34) had low protection. High titers of >1000 mIU/ml were present among 46.7% (212) of participants. The median Serological titers is 814.5(IQR: 132.75 - 1000) [Figure 1].
Figure 1.
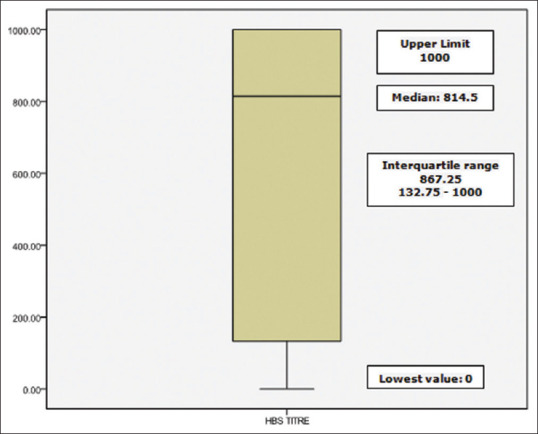
Box plot on serological titers (mIU) of hepatitis B surface antibody among health-care personnel
Age, vaccination status, number of doses, duration since vaccination, and taking boosters were analyzed and found to be influencing the seroprotection status [Table 1].
Table 1.
Association of antibody-hepatitis B surface seroprotection status and with selected factors in health-care personnel
| Variables | Anti HBs titer levels (mIU) | Chi-sqaure value; degree of freedom P value | ||
|---|---|---|---|---|
|
| ||||
| <10, n (%) | 10-100, n (%) | >100, n (%) | ||
| Age (years) | ||||
| <40 (n=239) | 12 (5) | 28 (11.7) | 199 (83.3) | χ2=6.71; df=2; P=0.034 |
| ≥40 (n=215) | 22 (10.2) | 34 (15.8) | 159 (74) | |
| Hepatitis B vaccination status | ||||
| Complete (n=377) | 22 (5.8) | 53 (14.1) | 302 (80.1) | χ2=8.82; df=2; P=0.012 |
| Incomplete (n=77) | 12 (15.6) | 9 (11.7) | 56 (72.7) | |
| Hepatitis B vaccination doses | ||||
| 1 (n=24) | 7 (29.2) | 3 (12.5) | 14 (58.3) | χ2=18.34; df=4; P=0.001 |
| 2 (n=53) | 5 (9.4) | 6 (11.3) | 42 (79.2) | |
| 3 (n=377) | 22 (5.8) | 53 (14.1) | 302 (80.1) | |
| Hepatitis B booster status | ||||
| Taken (n=56) | 0 | 6 (10.7) | 50 (89.3) | χ2=6.07; df=2; P=0.048 |
| Not taken (n=398) | 34 (8.5) | 56 (14.1) | 308 (77.4) | |
| Duration since vaccination (years) | ||||
| ≤10 (n=330) | 20 (6.1) | 35 (10.6) | 275 (83.3) | χ2=14.60; df=2; P=0.001 |
| >10 (n=124) | 14 (11.3) | 27 (21.8) | 83 (66.9) | |
| Duration of work (years) | ||||
| ≤5 (n=276) | 16 (5.8) | 24 (8.7) | 236 (85.5) | χ2=19.33; df=2; P<0.001 |
| >5 (n=178) | 18 (10.1) | 38 (21.3) | 122 (68.5) | |
Anti-HBs: Hepatitis B surface antibody
HCP <40 years had better seroprotection versus those >40 years old (P = 0.034).
Being completely vaccinated was associated with seroprotection. 15.6% of health workers who were incompletely vaccinated had low anti-HBs levels compared to only 5.8% among completely vaccinated (P = 0.012).
An association was evident with increasing number of doses. Good seroprotection (>100) was found among 58.3%, 79.2%, and 80.1% of workers who took 1 dose, 2 doses, and 3 doses of vaccine, respectively (P = 0.001).
Booster status was associated with anti-HBs levels (P < 0.05). All the workers who had taken boosters had seroprotection against hepatitis B.
Duration since hepatitis B vaccination was a significant factor (P = 0.001). 83.3% of workers vaccinated within the past 10 years had good titers compared to 66.9% among those vaccinated beyond 10 years and 6.1% had low titers compared to 11.3%, respectively, in the two groups showing waning immunity with time.
Duration of work was a significant factor for seroprotection (P < 0.001). Health workers who had lesser duration (<5 years) of work were found to have good seroprotection compared to those working for more than 5 years which may be related to a younger age and recent vaccination history.
Multivariate analysis was done to find the independent predictors of poor seroprotection [Table 2]. Incomplete hepatitis B vaccination, duration since vaccination of more than 10 years, and older age >40 years were predictors for poor seroprotection. HCP who were >40 years, who took <3 doses of hepatitis B vaccine, and whose duration since immunization was >10 years were found to be having 2.18, 2.56, and 2.41 times higher odds, respectively, for poor seroprotection compared to their counterparts.
Table 2.
Predictors of poor seroprotection of antibody hepatitis B surface titer <10 mIU*
| Variables (reference category) | OR (95% CI) | Adjusted OR (95% CI) | P |
|---|---|---|---|
| Vaccination status (incomplete versus complete) | 2.98 (1.41-6.32) | 2.56 (1.18-5.55) | 0.017 |
| Duration since vaccination (>10 years versus <10 years) | 1.973 (0.963-4.040) | 2.41 (1.14-5.13) | 0.022 |
| Booster doses (taken) | 0 | 0 | 0.997 |
| Age (>40 versus <40 years) | 0.464 (0.224-0.961) | 2.18 (1.02-4.64) | 0.044 |
*Multivariate analysis. OR: Odds ratio, CI: Confidence interval
DISCUSSION
We evaluated the immune response among 454 HCP vaccinated for hepatitis B and found that majority (92.5%) were seroprotected. Published literature[10,11] on HCP regarding the occupational risk, vaccination status, and immune response against hepatitis B reports similar results. Dini et al. in Italy (2017) measured the persistence of protective anti-HBs antibody levels in immunized students and found that 70.7% showed seroprotection.[10] Researchers from developing countries such as Pakistan,[12] Sri Lanka,[13] and India[9,14,15,16] have also published articles in this domain. Zeeshan et al. (Pakistan) evaluated newly HBV vaccinated HCP for immune response, 6 weeks postvaccination, and reported that 14% remained seronegative after vaccination.[12] Chathuranga et al. in a retrospective study in Sri Lanka noted that among vaccinated HCP, there were 9.9% of nonresponders.[13] In our study, low anti-HBs titer was present among 7.5% of health-care workers. In a tertiary care hospital in Hyderabad (2017), 62.5% showed protective levels.[14] The previous studies from Kerala on serology of vaccinated HCP also noted a lower proportion of HCP with low seroprotection. A study at Thrissur by Rao et al. (2008) among 65 vaccinated health workers revealed that low, moderate, and adequate protection was present among 10.5%, 10.5%, and 79% of vaccinated HCP, respectively.[16] Kollathodi et al. among medical students and health-care workers also report that 97.8% showed adequate anti-HBs titers.[17] Another study from Kerala also showed that 93.34% of vaccines had high antibody titers, but 6.6% were nonresponders.[18]
Studies have reported factors such as age, gender, body mass index, smoking, duration since vaccination, booster doses, and exposure risk affecting seroprotection. In our study, age, vaccination status, number of doses, duration since vaccination, and taking boosters were found to predict the seroprotection among vaccinated HCP. Younger individuals were found to have a better seroprotection compared to older HCP. Kollathodi et al. in Kerala also reported 98.2% immune response in participants <30 years of age.[17] Chaudhari et al. in their study among HCP in armed forces showed a 93.8% response in participants <30 years compared to only 77.5% response in those who were >30 years of age.[19] Gara et al. (2014) tested anti-HBs levels at a clinical center in Bethesda and concluded that anti-HBs levels decrease after 10–31 years and fall below a level considered protective in approximately 25% of HCWs.[11]
Time since vaccination beyond 10 years was found to be an independent predictor for poor seroprotection in our study. Similar results were noted in a published research by Batra et al. who noted a significant difference in mean titer among HCWs vaccinated within and beyond 5 years.[9] Recent literature also suggests that even if anti-HBs titers decline over time, an exposure augments the immune response and immune memory remains, which protects the HCP avoiding the need for booster vaccination.[20] In our study, all the health workers who had taken hepatitis B booster had adequate seroprotection.
CONCLUSIONS
Hepatitis B vaccines confer long-term protection from hepatitis B infections, but anti-HBs levels can wane over time, and health-care workers need to be monitored periodically as part of a preventive occupational surveillance program. Where schedules are incomplete and testing after the primary vaccine series is uncommon, anti-HBs titer assessment in HCP vaccinated more than 10 years back is advisable as they are a high-risk group, especially in endemic developing countries, and booster doses can be recommended if anti-HBs titers are low.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organisation. Hepatitis B Fact Sheet. Geneva: World Health Organisation; 2017. [Last accessed on 2018 Apr 23]. Available from: http://www.who.int/mediacentre/factsheets/fs204/en/ [Google Scholar]
- 2.Gupta S, Gupta R, Joshi YK, Singh S. Role of horizontal transmission in hepatitis B virus spread among household contacts in north India. Intervirology. 2008;51:7–13. doi: 10.1159/000118790. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Public Health Service. Updated US public health service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for post exposure prophylaxis. MMWR Recomm Rep. 2001;50:1. [PubMed] [Google Scholar]
- 4.Bond WW, Favero MS, Petersen NJ, Gravelle CR, Ebert JW, Maynard JE. Survival of hepatitis B virus after drying and storage for one week. Lancet. 1981;1:550–1. doi: 10.1016/s0140-6736(81)92877-4. [DOI] [PubMed] [Google Scholar]
- 5.Elavia AJ, Banker DD. Hepatitis B virus infection in hospital personnel. Natl Med J India. 1992;5:265–8. [PubMed] [Google Scholar]
- 6.Kumar KA, Baghal PK, Shukla CB, Jain MK. Prevalence of hepatitis B surface antigen (HBsAg) among health care personnelss. Indian J Community Med. 2000;25:93–6. [Google Scholar]
- 7.Sukriti, Pati NT, Sethi A, Agrawal K, Agrawal K, Kumar GT, et al. Low levels of awareness, vaccine coverage, and the need for boosters among health care workers in tertiary care hospitals in India. J Gastroenterol Hepatol. 2008;23:1710–5. doi: 10.1111/j.1440-1746.2008.05483.x. [DOI] [PubMed] [Google Scholar]
- 8.CDC. Immunization of health care personnel: Recommendations of the advisory committee on immunization practices (ACIP) MMWR. 2011:603–8. [PubMed] [Google Scholar]
- 9.Batra V, Goswami A, Dadhich S, Kothari D, Bhargava N. Hepatitis B immunization in healthcare workers. Ann Gastroenterol. 2015;28:276–80. [PMC free article] [PubMed] [Google Scholar]
- 10.Dini G, Toletone A, Barberis I, Debarbieri N, Massa E, Paganino C, et al. Persistence of protective anti-HBs antibody levels and anamnestic response to HBV booster vaccination: A cross-sectional study among healthcare students 20 years following the universal immunization campaign in Italy. Hum Vaccin Immunother. 2017;13:440–4. doi: 10.1080/21645515.2017.1264788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gara N, Abdalla A, Rivera E, Zhao X, Werner JM, Liang TJ, et al. Durability of antibody response against hepatitis B virus in healthcare workers vaccinated as adults. Clin Infect Dis. 2014;60:505–13. doi: 10.1093/cid/ciu867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zeeshan M, Jabeen K, Ali AN, Ali AW, Farooqui SZ, Mehraj V, et al. Evaluation of immune response to hepatitis B vaccine in health care workers at a tertiary care hospital in Pakistan: An observational prospective study. BMC Infect Dis. 2007;7:120. doi: 10.1186/1471-2334-7-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chathuranga LS, Noordeen F, Abeykoon AM. Immune response to hepatitis B vaccine in a group of health care workers in Sri Lanka. Int J Infect Dis. 2013;17:e1078–9. doi: 10.1016/j.ijid.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 14.Sahana HV, Sarala N, Prasad SR. Decrease in anti-HBs antibodies over time in medical students and healthcare workers after hepatitis B vaccination. Biomed Res Int. 2017;2017:1327492. doi: 10.1155/2017/1327492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaya Lakshmi L, Alekhya P, Sasikala G. Anti HBs titers in health care persons of clinical laboratory. IOSR J Dent Med Sci. 2017;16:54–7. [Google Scholar]
- 16.Rao TV, Suseela IJ, Sathiavathy KA. Estimation of antibodies to HBsAg in vaccinated health care workers. Indian J Med Microbiol. 2008;26:93–4. doi: 10.4103/0255-0857.38876. [DOI] [PubMed] [Google Scholar]
- 17.Kollathodi N, Moorkoth AP, George K, Narayanan MP, Balakrishnan SM, LelithaBai SD. Hepatitis B vaccination - immune response and persistence of protection in susceptible population. J Acad Clin Microbiol. 2017;19:42–6. [Google Scholar]
- 18.Oomen S, Jagan AO. Anti HBs antibody status of HCW. Pushpagiri Med J. 2014;5:111–3. [Google Scholar]
- 19.Chaudhari CN, Bhagat MR, Shah T, Misra RN. Antibody to hepatitis B surface antigen in vaccinated health care workers. Med J Armed Forces India. 2008;64:329–32. doi: 10.1016/S0377-1237(08)80013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leuridan E, Van Damme P. Hepatitis B and the need for a booster dose. Clin Infect Dis. 2011;53:68–75. doi: 10.1093/cid/cir270. [DOI] [PubMed] [Google Scholar]


