Abstract
Background
Nanosecond electric pulses showed promising results in electrochemotherapy, but the underlying mechanisms of action are still unexplored. The aim of this work was to correlate cellular cisplatin amount with cell survival of cells electroporated with nanosecond or standardly used 8 × 100 μs pulses and to investigate the effects of electric pulses on cisplatin structure.
Materials and methods
Chinese hamster ovary CHO and mouse melanoma B16F1 cells were exposed to 1 × 200 ns pulse at 12.6 kV/cm or 25 × 400 ns pulses at 3.9 kV/cm, 10 Hz repetition rate or 8 × 100 μs pulses at 1.1 (CHO) or 0.9 (B16F1) kV/cm, 1 Hz repetition rate at three cisplatin concentrations. Cell survival was determined by the clonogenic assay, cellular platinum was measured by inductively coupled plasma mass spectrometry. Effects on the structure of cisplatin were investigated by nuclear magnetic resonance spectroscopy and high-resolution mass spectrometry.
Results
Nanosecond pulses equivalent to 8 × 100 μs pulses were established in vitro based on membrane permeabilization and cell survival. Equivalent nanosecond pulses were equally efficient in decreasing the cell survival and accumulating cisplatin intracellularly as 8 × 100 μs pulses after electrochemotherapy. The number of intracellular cisplatin molecules strongly correlates with cell survival for B16F1 cells, but less for CHO cells, implying the possible involvement of other mechanisms in electrochemotherapy. The high-voltage electric pulses did not alter the structure of cisplatin.
Conclusions
Equivalent nanosecond pulses are equally effective in electrochemotherapy as standardly used 8 × 100 μs pulses.
Key words: electroporation, electrochemotherapy, nanosecond pulses, cisplatin
Introduction
Electrochemotherapy (ECT) is a local cancer treatment. The dominant mechanism of ECT is increased cellular uptake of impermeant or low permeant anticancer drugs with high intrinsic cytotoxicity - most commonly bleomycin and cisdiaminedichloroplatinum(II) (cisplatin) - due to transiently increased membrane permeability of cells/tumors after exposure to short high-voltage electric pulses.1
Over the past ten years, the number of ECT treatments performed for superficial tumors has increased dramatically and new indications have been added, such as treatment of skin metastases from visceral or hematological malignancies, vulvar cancer, deep-seated malignancies, and some noncancerous skin lesions.2 ECT has become broadly accepted mainly because of its simplicity (it is easy to master) and versatility (it allows treating a variety of cancers). Its efficacy, tolerability, and high patient satisfaction have been demonstrated in several studies, but also some side effects have been reported. According to the reports, the main side effects are unpleasant sensations, which can be painful, and muscle contractions triggered by applied high voltage electric pulses.3, 4 Most commonly, electric pulses are administrated as trains of eight monophasic pulses with a duration of 100 μs at 1 Hz or 5 kHz pulse repetition rate.
Nanosecond pulses have shown potential advantages over micro- and millisecond pulses in electroporation-based applications. The use of pulses with high electric field strength, but very short duration (i.e., in the nanosecond range) results in low energy transfer by the pulses to the treated volume, resulting in a low heating5, 6 and thereby minimizing the possibility of thermal damage to the tissue, which is very important for sparing delicate structures in and around the treated area.7 In addition, nanosecond pulses limit electrochemical reactions at the electrode-electrolyte interface8 which may affect the treated medium or cells/tissues.9, 10, 11 Although a much higher electric field strength is required to achieve a comparable biological effect, excitation thresholds appear to be higher than the electroporation thresholds with nanosecond pulses12, 13, 14, 15, 16, implying that shortening the pulse duration to nanosecond pulses could also reduce neuromuscular stimulation in electroporation-based applications.
Recently, nanosecond pulses have been explored in ECT and calcium electroporation and have shown promising results – either tumor regression in vivo or a decrease in cell survival in vitro.8,17, 18, 19, 20, 21 We have previously reported that nanosecond pulses of an appropriately chosen amplitude in combination with cisplatin decreased cell survival in in vitro assays to the same extent as standard 8 × 100 μs pulses.8 The aim of our present work was to investigate the underlying mechanisms of ECT with nanosecond pulses and cisplatin in vitro on Chinese hamster ovary CHO and mouse skin melanoma B16F1 cells. Two nanosecond pulse protocols (1 × 200 ns pulse at 12.6 kV/cm and 25 × 400 ns pulses at 3.9 kV/cm, 10 Hz repetition rate) were compared with 8 × 100 μs pulses at 1.1 (CHO) or 0.9 (B16F1) kV/cm, 1 Hz repetition rate standardly used in ECT. Accumulation of cisplatin and cell survival after in vitro ECT were measured and effects of high voltage electric pulses on the cisplatin molecular structure were investigated by nuclear magnetic resonance (NMR) spectroscopy and high-resolution mass spectrometry (HRMS).
Materials and methods
Cell culture of Chinese hamster ovary (CHO) cells and in vitro cell survival after ECT experiment protocols were described previously.8 Mouse skin melanoma cell line B16F1 (European Collection of Authenticated Cell Cultures, cat. no. 92101203, Sigma Aldrich, Germany, mycoplasma free) was cultured in the same way as CHO cells except that Dulbecco’s Modified Eagle Medium (DMEM, cat. no. D5671, Sigma-Aldrich, Missouri, United States) supplemented with 10% FBS (cat. no. F9665, Sigma-Aldrich), 2.0 mM L-glutamine, 1 U/ml penicillin/ streptomycin and 50 μg/ml gentamycin was used instead of Nutrient Mixture F-12 Ham. Briefly, cisplatin (Cisplatin Kabi, 1 mg/mL, Fresenius Kabi, Germany or Cisplatin Accord, 1 mg/ml, Accord, UK) diluted in saline was added to cells suspended in complete growth medium DMEM just before electroporation so that the final concentration was 4 × 106 cell/ml and 0, 10, 30 or 50 μM cisplatin. The cell suspension was exposed to monophasic rectangular pulses (1 × 200 ns pulse at 12.6 kV/cm or 25 × 400 ns at 3.9 kV/cm, 10 Hz repetition rate or 8 × 100 μs at 1.1 (CHO) or 0.9 (B16F1) kV/cm, 1 Hz pulse repetition rate) or no pulses (non-electroporated controls). Cell survival was determined by the clonogenic assay.
For determination of cellular cisplatin, 125 μl of the treated cell suspension was diluted 40–100 times in complete growth medium Ham F-12 (CHO) or complete growth medium DMEM (B16F1) 25 min after electroporation (or addition of cisplatin/saline for non-electroporated controls) and centrifuged at 900 g for 5 min at 23°C in 15 ml centrifuge tubes. The supernatant was separated from the cell pellet and the pellet was washed with 2 ml saline and centrifuged again. After centrifugation, saline was discarded, and the cell pellet was kept at −20°C until digestion. For digestion, 0.1 ml H2O2 and 0.1 ml HNO3 (both from Merck, Germany) were added to the cell pellets, and the tubes were closed and sealed with Teflon tape and left overnight at 80°C. After digestion, 1.8 ml of Milli-Q water (18.2 MΩ obtained from a Direct-Q 5 Ultrapure water system, Merck Millipore, Massachusetts, USA) was added and samples were measured by inductively coupled plasma mass spectrometry (7900 ICP-MS Agilent Technologies, Japan) with 193Ir used as an internal standard during the measurement. The experiments were repeated 4–7 times. The number of cisplatin molecules per cell was calculated by first dividing the measured total mass of Pt in the cell pellet by the number of cells in the pellet, then subtracting the average mass of Pt per cell of non-electroporated cell pellets that were not incubated with cisplatin, and finally calculating the number of cisplatin molecules per cell from the difference of the mass of Pt per cell in samples (assuming 1 mol of Pt is equivalent to 1 mol of cisplatin).
Cell survival and amount of Pt data (after outliers, defined using the interquartile range method, were removed) were analyzed using the Kruskal– Wallis test and p-values were adjusted with the post-hoc Holm method test (α = 0.05) because the Shapiro-Wilk normality test failed (α = 0.05). The Spearman correlation coefficient was calculated to test the correlation between the number of cisplatin molecules per cell and cell survival. The data were processed and visualized using Microsoft Excel 2016 and R 3.6.1.22
Potential structural changes of cisplatin in the solution treated with high voltage electric pulses were investigated by NMR spectroscopy and HRMS. For practical reasons, both microsecond and nanosecond pulses were delivered to electroporation cuvettes with 2 mm gap with the laboratory prototype pulse generator based on an H-bridge digital amplifier for this set of experiments. For microsecond pulses, 8 × 100 μs at 1.1 kV/cm at 1 Hz pulse repetition rate were delivered (same pulse protocol as in cellular electrochemotherapy experiments). For nanosecond pulses, 25 × 400 ns at 2.2 kV/cm at 10 Hz repetition rate were delivered – the electric field strength for this pulse protocol was lower than in cellular electrochemotherapy experiments because of the technical limitations of the prototype pulse generator. 1 × 200 ns pulse was not applied because the pulse generator used is not capable of generating such short pulses. 1H NMR spectra were obtained on NMR Bruker AscendTM 600 MHz spectrometer at room temperature at 600 MHz. Chemical shifts, reported in ppm, are referenced to residual peaks of D2O at 4.79 ppm. Spectra were recorded in D2O (with and without NaCl) as well as in 90% H2O/10% D2O (with or without NaCl) using water suppression (WATERGATE) method. NMR data were processed with MestReNova 11.0.4. To approximately 1–2 mg of cisplatin (Sigma Aldrich) 1 mL of a) D2O, b) D2O containing 154 mM NaCl, c) 90% H2O/10% D2O or d) 90% H2O/10% D2O containing 154 mM NaCl was added. The obtained suspension was filtered through Minisart NML Cellulose Acetate Syringe Filter (28 mm, 0.2 μL). 1H NMR spectra were recorded immediately after the filtration when not treated with any pulse protocol or directly after microsecond or nanosecond pulse application. HRMS spectra were recorded on Agilent 6224 Accurate Mass Time of Flight (TOF) Liquid Chromatography-Mass Spectrometry (LC-MS) instrument using water-acetonitrile solution (80:20, v/v) as the mobile phase. Fragmentor voltage was set to 150.0 V. To approximately 1–2 mg of cisplatin (Sigma Aldrich) 1 mL of distilled water or saline was added and obtained suspension was filtered through Minisart NML Cellulose Acetate Syringe Filter (28 mm, 0.2 μL). Filtered solutions underwent a) no pulses, b) microsecond pulses, or c) nanosecond pulses application as mentioned above, followed by immediate injection of such solutions into the LC-MS.
Results
CHO and B16F1 cells were electroporated in presence of 10, 30 and 50 μM cisplatin with: 1 × 200 ns pulse at 12.6 kV/cm; 25 × 400 ns pulses at 3.9 kV/ cm, 10 Hz pulse repetition rate; or 8 × 100 μs pulses at 1.1 (CHO) or 0.9 (B16F1) kV/cm, 1 Hz pulse repetition rate. The electric field strengths for specific pulse parameters were selected based on survivalpermeabilization curves (refer to Vižintin et al.8 for graphs for CHO cells and to Figure S1 in the Supplementary material for graphs for B16F1 cells).
Cell survival results after ECT determined by the clonogenic assay are shown in Figure 1. Survival data of CHO cells were combined from the previous8 (for non-electroporated cells and cells electroporated with 25 × 400 ns and 8 × 100 μs pulses) and the present study (additional non-electroporated cells and cells electroporated with 1 × 200 ns pulse). As intended, electroporation alone (i.e., in the absence of cisplatin) did not decrease cell survival in both cell lines compared with the non-electroporated control for any of the pulse protocols tested. For the non-electroporated cells treated with cisplatin, a statistically significant decrease in cell survival was observed only for CHO cells at the highest (50 μM) cisplatin concentration tested. On the other hand, electroporation in the presence of cisplatin decreased cell survival except for B16F1 cells treated with 1 × 200 ns pulse. For CHO cells, 1 × 200 ns, 25 × 400 ns, and 8 × 100 μs pulse protocols were all equally effective at decreasing cell survival at all the three tested cisplatin concentrations (Figure 1A). In B16F1 cells, 25 × 400 ns and 8 × 100 μs pulses were equally effective, whereas 1 × 200 ns pulse protocol was less effective (Figure 1B).
Figure 1.
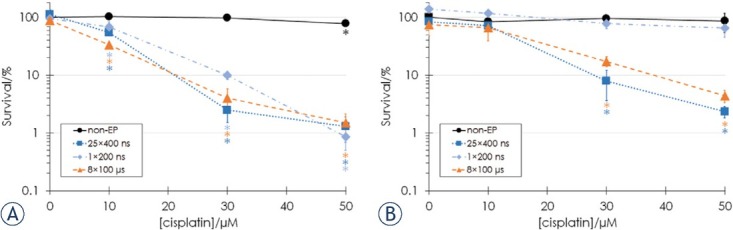
Cell survival of (A) CHO and (B) B16F1 cells at different cisplatin concentrations determined by the clonogenic assay for non-electroporated (non-EP) cells (black circles) and cells electroporated with 25 x 400 ns pulses at 3.9 kV/cm, 10 Hz repetition rate (dark blue squares), 1 × 200 ns pulse at 12.6 kV/cm (light blue diamonds) or 8 × 100 μs pulses at 1.1 (CHO) or 0.9 (B16F1) kV/cm, 1 Hz pulse repetition rate (orange triangles). Bars represent standard deviation, asterisks (*) show statistically significant differences (p < 0.05) to the survival of non-electroporated cells without cisplatin. Survival data were combined from the previous8 (for non-electroporated cells and cells electroporated with 25 × 400 ns and 8 × 100 μs pulses) and the present study (for B16F1 cells, additional non-electroporated CHO cells and CHO cells electroporated with 1 × 200 ns pulse).
The amount of Pt in the cells was determined by measuring the total mass of Pt in the cell pellets by ICP-MS. Electroporation increased the cellular Pt amount. For both cell lines, there were no statistically significant differences in the measured Pt amount in cells electroporated with 25 × 400 ns or 8 × 100 μs pulses at the same cisplatin concentration. For CHO cells, the amount of Pt in cells electroporated with 1 × 200 ns pulse was statistically significantly lower compared to the amount of Pt in cells electroporated with 25 × 400 ns and 8 × 100 μs pulse incubated only at 50 μM cisplatin (Figure 2A). For B16F1 cells, lower cellular Pt was measured after application of 1 × 200 ns pulse compared to 25 × 400 ns and 8 × 100 μs pulses at all tested cisplatin concentrations (Figure 2B).
Figure 2.
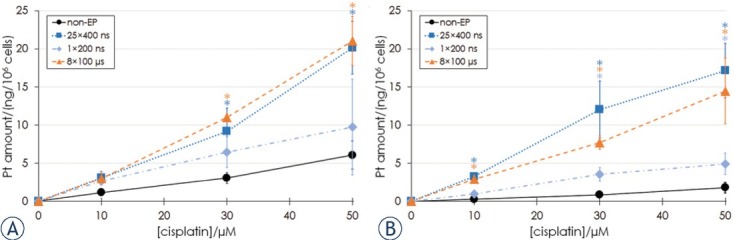
Pt amount in cell pellets of (A) CHO and (B) B16F1 cells after 25 min incubation at different extracellular cisplatin concentrations in non-electroporated (non-EP) cells (black circles) and cells electroporated with 25 x 400 ns pulses at 3.9 kV/ cm, 10 Hz repetition rate (dark blue squares), 1 × 200 ns pulse at 12.6 kV/cm (light blue diamonds) or 8 × 100 μs pulses at 1.1 (CHO) or 0.9 (B16F1) kV/cm, 1 Hz pulse repetition rate (orange triangles). Bars represent standard deviation, asterisks (*) show statistically significant differences (p < 0.05) to the measured number of cisplatin molecules in non-electroporated cells at the same extracellular cisplatin concentration.
From the measured Pt content, the number of cisplatin molecules per cell was calculated and plotted against the cell survival data. The number of cisplatin molecules per cell and cell survival were more strongly correlated for B16F1 cells (Spearman’s correlation coefficient: ρ = −0. 85, p < 0.001 for CHO and ρ = −0. 92, p < 0.01 for B16F1). In the case of CHO cells, at the same number of cisplatin molecules per cell, notably lower cell survival was measured for electroporated cells compared to non-electroporated cells (Figure 3A). For example, cell survival of 98% was achieved for non-electroporated cells with 9.4 × 106 cisplatin molecules per cell, whereas cell survival of 68.5% was measured for cells electroporated with 1 × 200 ns pulse with 8.2 × 106 cisplatin molecules per cell, cell survival of 54.8% was measured for cells electroporated with 25 × 400 ns pulses with 9.5 × 106 cisplatin molecules per cell, and cell survival of 33.7% was measured for cells electroporated with 8 × 100 μs pulses with 9.2 × 106 cisplatin molecules per cell. From the data acquired, it could not be concluded if also in B16F1 cells a lower number of cisplatin molecules per cell causes a larger decrease in cell survival because the range of the number of cisplatin molecules in electroporated and non-electroporated cells did not overlap and thus survival could not be compared at approximately the same number of cisplatin molecules per cells (Figure 3B).
Figure 3.
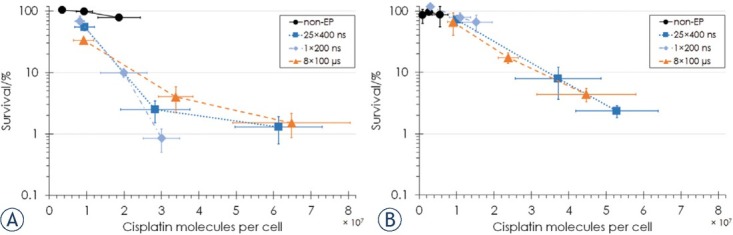
Cell survival as a function of the number of cisplatin molecules per cell for (A) CHO cells and (B) B16F1 cells in non-electroporated (non-EP) cells (black circles) and cells electroporated with 25 x 400 ns pulses at 3.9 kV/cm, 10 Hz repetition rate (dark blue squares), 1 × 200 ns pulse at 12.6 kV/cm (light blue diamonds) or 8 × 100 μs pulses at 1.1 (CHO) or 0.9 (B16F1) kV/cm, 1 Hz pulse repetition rate (orange triangles). Bars represent standard deviation. Survival data were combined from the previous8 (for non-electroporated CHO cells and CHO cells electroporated with 25 × 400 ns and 8 × 100 μs pulses) and the present study (for B16F1 cells, additional non-electroporated CHO cells and CHO cells electroporated with 1 × 200 ns pulse).
Cisplatin has been widely investigated for its biospeciation in aqueous solutions due to its diverse stepwise ligand displacement reactions.23 Therefore, 1H NMR spectroscopy was applied to investigate potential structural changes of cisplatin due to high voltage electric pulses. First, spectra of cisplatin in D2O and D2O with 154 mM NaCl (corresponding to physiological saline 0.9% NaCl) not exposed to electric pulses were recorded (Figure 4A–B). Weak broadened peaks for hydrogen atoms of amino ligands (NH3) were found at approximately 4.08 ppm. Similarly, also representative peaks of cisplatin after treatment with 8 × 100 μs pulses at 1.1 kV/cm at 1 Hz pulse repetition rate or 25 × 400 ns pulses at 2.2 kV/cm at 10 Hz repetition rate remained at the same shift. The only major difference was observed in the spectrum of cisplatin recorded in D2O with 154 mM NaCl after treatment with microsecond pulses (Figure 4B), where the broad peak for hydrogens of cisplatin disappeared. This can be attributed to the fast hydrogen-deuterium (H/D) exchange of deuterium from D2O with hydrogen atoms of NH3 ligands.24 However, when spectra of cisplatin were recorded in 90% H2O/10% D2O solution containing 154 mM NaCl acquiring water suppression (to minimize the intensity of water signal to obtain a stronger signal of the NH3 ligand) no such disappearance of the peak was observed (Figure 4D). Comparable spectra with peaks at 4.08 ppm were obtained also when no electric pulses or nanosecond pulses were applied. Similarly, the hydrogen peak of NH3 was observed in the samples recorded in a 90% H2O/10% D2O solution without NaCl (Figure 4C). It is also important to note that no new peaks appeared in other regions of the NMR spectra.
Figure 4.
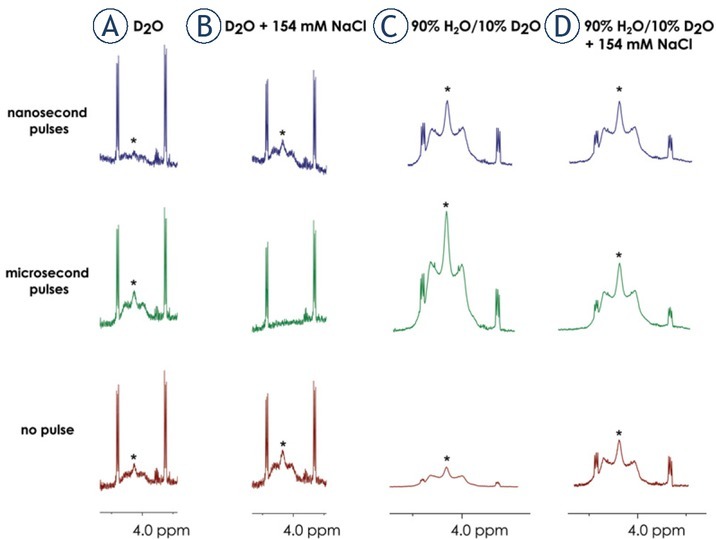
1H NMR spectra of cisplatin, showing the signals for hydrogens of NH3 ligands labeled with asterisks (*). Spectra were recorded in a) D2O, b) D2O containing 154 mM NaCl, c) 90% H2O/10% D2O and d) 90% H2O/10% D2O containing 154 mM NaCl treated with 25 × 400 ns pulses (blue), 8 × 100 μs pulses (green) or no pulses (red).
High-resolution mass spectrometry (HRMS), which can also provide abundant information on molecular structure, was also performed to investigate possible newly formed cisplatin species. In some reports, authors detected hydrolysis products corresponding to mono-, di- and trimeric species, by mass spectrometry.25, 26, 27, 28 Therefore, HRMS was used in our structural investigation of cisplatin in water and saline (0.9% NaCl) exposed to micro-and nanosecond pulses.
First, cisplatin in H2O was investigated and on the full-scan positive-ion mass spectrum (mass range of m/z 100–1100) presented in Figure S2 in Supplementary Material. It can be observed that the most abundant peaks occur in the mass range of m/z 280–330, where the following fragments were observed: [Pt(NH3)2(N2) Cl]+ (m/z 292.9909), [M+NH4]+ (M – indicates molecular formula for cisplatin, i.e. [Pt(NH3)2Cl2]) (m/z 317.9872) (both Figure S3), [M+H]+ (m/z 300.9601) (Figure S4), [Pt(NH3)2(CH3CN)Cl]+ (m/z 306.0101) (Figure S5) and [M+Na]+ (m/z 322.9425) (Figure S6). Additionally, three lower abundant clusters can be found in the mass range of m/z 540–590. Two of them were identified as [Pt(NH3)2Cl2·Pt(NH3)Cl]+ (m/z 547.9121) and [Pt(NH3)2Cl2·Pt(NH3)2Cl]+ (m/z 564.9378) (Figure S7). Additionally, one cluster at m/z 610–630 with the main ion fragment at m/z 617.9408 belongs to [2M+NH4]+ (Figure S8). Similar fragments have been observed when the samples were treated with micro- and nanosecond pulses (Figure S9–10 and Figure S11–S12). The species observed are in agreement with those reported in the literature.26 Figure S19 represents the spectrum of water from the electroporation cuvette without the application of electric pulses. No differences were observed between the solutions treated with either nanosecond or microsecond pulses or untreated control.
HRMS experiments have been further performed in saline, where more extensive fragmentation was observed throughout the mass range of m/z 100–1100 (Figure S13). However, these peaks are comparable to the ones in the spectrum of saline from electroporation cuvette without the application of electric pulses (Figure S20). Similarly to spectra without NaCl, peaks of [Pt(NH3)2(N2)Cl]+ fragment and sodium [M+Na]+ adduct were identified on zoom-scan spectrum (Figure S14). Again, spectra recorded in saline that was not treated with electric pulses are comparable with the spectra where cisplatin in saline solutions were treated with micro- and nanosecond pulses (Figures S15– 16 and Figures S17–18, respectively).
Overall, NMR, as well as HRMS investigations, point to cisplatin remaining structurally comparable after the exposure to high voltage electric pulses similar to those used in in vitro ECT experiments with respect to its aqueous solutions without electric pulses.
Discussion
ECT has been shown to be a safe and effective cancer treatment, requiring much lower doses of the chemotherapeutic agent than conventional chemotherapy. However, pain and muscle contractions were reported as a drawback. Nanosecond pulses and high-frequency biphasic pulses of a few microsecond duration (H-FIRE)29, 30, 31 were suggested to limit neuromuscular stimulation and contractions.15, 16 Additionally, with nanosecond pulses, the possibility of thermal damage to the tissue is minimized5, 6 due to low energy being transferred to the treated area and electrochemical reactions are reduced.8 ECT with nanosecond pulses has shown promising results8,17, 18, 19, but the underlying mechanisms of the observed decrease in cell survival and tumor regression remain to be explained.
In this study, we measured cell survival and cisplatin accumulation after in vitro ECT with 8 × 100 μs pulses, which are standardly used in ECT procedures, and equivalent nanosecond pulses, i.e. pulse protocols that have an equivalent biological effect on cell survival and cell membrane permeabilization. The electric field strength was chosen for each pulse protocol at a value that resulted in the highest permeabilization (determined as the percentage YO-PRO1 fluorescing cells) of the cell membrane without a decrease in cell survival (measured by the metabolic MTS assay). In the case of 8 × 100 μs pulses, 1.1 kV/cm was selected for CHO cells, but the survival for B16F1 cells was around 55% at this electric field strength, thus a lower (i.e. 0.9 kV/cm) electric field strength was used for electroporating B16F1 cells with this pulse protocol. For 25 × 400 ns pulses, the same electric field strength (3.9 kV/cm) was determined to be optimal for both cell lines. For 1 × 200 ns pulse, we used the highest experimentally achievable electric field
strength (i.e. 12.6 kV/cm), which did not decrease the cell survival in either cell line. Electroporating both cell lines with 8 × 100 μs or 25 × 400 ns pulses at the selected electric field strengths resulted in > 95% permeabilization (optimal for ECT), while for the 1 × 200 ns pulse at 12.6 kV/cm the permeabilization was 85% for CHO and only 42% for B16F1 cells (suboptimal for ECT). However, 1 × 200 ns pulse protocol was also included in the study based on results of cell survival of CHO cells after ECT determined by the metabolic MTS assay that showed that this pulse protocol was as effective in decreasing cell survival in ECT with cisplatin as the 25 × 400 ns protocol at all cisplatin concentrations.8
The aim was to test whether the combination of permeabilizing electric pulses (that alone do not cause a decrease in cell survival) and cisplatin results in increased cellular cisplatin accumulation (compared to non-electroporated cells) and whether the amount of cellular cisplatin is correlated to cell survival due to the increase of intracellular accumulation of the chemotherapeutic agent being one of the main mechanisms of action of ECT. To exert its cytotoxic effect, cisplatin must enter the cell. The exact mechanisms of cisplatin uptake have not been fully elucidated. Cisplatin is only slightly permeant; thus, it only partially enters the cell through passive diffusion across the cell membrane. Recent studies pointed out active transport mechanisms such as facilitated diffusion involved in cisplatin uptake - and LRRC8 volume-regulated anion channels (VRAC), copper transporter 1 (CTR1), and organic cation transporters (OCTs) were shown to be involved in cisplatin uptake.32, 33 Electroporation makes the cell membrane non-selectively permeable, allowing a larger quantity of cisplatin to enter the cell (Figure 5).
Figure 5.
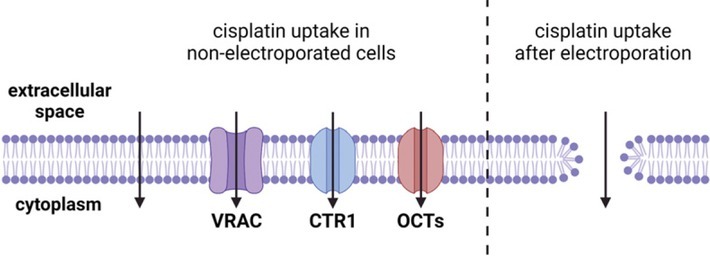
The mechanism of cisplatin uptake into cells is not completely elucidated. In non-electroporated cells, cisplatin enters partially through passive diffusion and facilitated diffusion through ion channels including LRRC8 volume-regulated anion channels (VRAC) and membrane transporters like copper transporter 1 (CTR1) and organic cation transporters (OCTs). In electroporated cells, more cisplatin can enter through the permeabilized cell membrane (pore is a symbolic presentation of increased membrane permeability even though the mechanisms behind electroporation are more complex – refer to34).
As expected, the measured amount of Pt was higher in electroporated cells when compared to non-electroporated cells incubated at the same cisplatin concentration, although the differences were not always statistically significant (Figure 2). These results indicate that the application of electric pulses indeed increases the intracellular accumulation of cisplatin. Overall, the amount of Pt in B16F1 was lower than in CHO cells exposed to the same cisplatin concentration, with or without electroporation, which also correlates with the higher cell survival of B16F1 cells (Figure 1). A comparison of cell survival of CHO and B16F1 cells with a similar number of cisplatin molecules per cell (Figure 3) reveals that a higher number of cisplatin molecules is needed to decrease the cell survival of B16F1 cells compared to CHO.
There were no statistically significant differences in the cell survival and amount of cellular Pt obtained in cells electroporated with 25 × 400 ns and 8 × 100 μs pulses at the same cisplatin concentration when comparing within the same cell line. Thus, it can be assumed that by using equivalent nanosecond pulses, it is possible to achieve the same decrease in cell survival and same cisplatin accumulation in cells and the as with the standard 8 × 100 μs pulses; in other words, equivalent nanosecond pulses are equally effective in ECT as 8 × 100 μs pulses.
The 1 × 200 ns pulse in combination with cisplatin did not decrease cell survival in B16F1 cells. This could be explained by the fact that 1 × 200 ns pulse permeabilizes less than half of the cell population of B16F1 and is also consistent with the measured Pt amount which was not significantly higher as in non-electroporated cells (Figure 2B). Application of 1 × 200 ns pulse alone (i.e., in the absence of cisplatin) seemed to even slightly promote cell growth (although the cell survival was not statistically significantly higher compared to the non-electroporated control). More interestingly, however, is that application of 1 × 200 ns pulse to CHO cells resulted in a lower amount of Pt in cells electroporated with 1 × 200 ns pulse as with 25 × 400 ns or 8 × 100 μs pulses, but the same decrease in cell survival was achieved with the 1 × 200 ns pulse as with 25 × 400 ns or 8 × 100 μs pulses. The lower amount of cisplatin in CHO cells electroporated with 1 × 200 ns could be explained per se by the fact that this pulse protocol achieved suboptimal cell membrane permeabilization compared to the 25 × 400 ns and 8 × 100 μs pulse protocols. Nevertheless, a comparable decrease in cell survival was achieved, suggesting that increased accumulation of cisplatin into cells may not be the only cause of cell death in ECT. Figure 2A indicates that in electroporated CHO cells, a lower number of cisplatin molecules per cell is required to decrease cell survival to the same extent as in non-electroporated cells. Similar results have been reported previously in the literature35, 36, but not discussed. There may be a synergistic effect of cisplatin and electroporation, i.e., the observed decrease in cell survival in ECT is not the sum of the decrease in cell survival caused by electric pulses and cisplatin alone, but electroporation appears to make cells more susceptible to cisplatin.
The results of survival and number of internalized cisplatin molecules for B16F1 cells, however, do not show a similar synergistic effect of cisplatin and electroporation. Contrary to CHO cells, the number of cisplatin molecules per cell seems to linearly correlate with the logarithm of cell survival for B16F1 cells (Figure 3). Nonetheless, as mentioned above, lower cellular cisplatin was consistently measured for the B16F1 cell line and there is only one experimental point from the electroporated cells (cells electroporated with 1 × 200 ns pulse at 10 μM cisplatin) that falls in the range of the number of molecules of the non-electroporated cells. A similar number of internalized cisplatin molecules was measured for non-electroporated cells at 30 μM cisplatin and for cells electroporated with 1 × 200 ns pulse at 10 μM cisplatin, but the cell survival was even slightly higher for the latter. As discussed above, however, the 1 × 200 ns pulse protocol did not effectively permeabilize B16F1 cells. More data (from non-electroporated cells incubated at higher cisplatin concentrations) would thus be needed to determine if also in the case of B16F1 cells a lower number of internalized cisplatin molecules is needed to decrease cell survival in electroporated cells.
To test whether electric pulses could affect cisplatin by modifying the structure of the molecule as proposed in theoretical studies37, we used NMR spectroscopy and HRMS spectrometry and found that the structure of cisplatin remains comparable after the application of electric pulses to either its saline or water solution (representing a simplified extra- and intracellular environment, respectively). Thus, high voltage electric pulses did not affect the structure of the studied complex under the conditions used in our experiments. Therefore, the reason for the observed increased susceptibility of the electroporated CHO cells to cisplatin is probably a consequence of the effect of electroporation on the cells. The cytotoxicity of cisplatin is thought to be mediated primarily by the formation of DNA adducts and the resulting impairment of transcriptional and/or DNA replication mechanisms. It was shown that electroporation increases the amount of cisplatin bound to the DNA, which could increase cisplatin cytotoxicity in electroporated cells.35, 38 However, additional mechanisms play an important role in exerting the toxic effects of cisplatin, including generation of ROS, mitochondrial dysfunction, increase in intracellular Ca2+ concentration, and activation of signal transduction pathways.39 Electric pulses can also lead to generation of intracellular reactive oxygen species (ROS)40, 41, damage mitochondria42, 43, and disrupt calcium homeostasis through the entry of Ca2+ from the extracellular space or intracellular stores.44, 45 It has been shown that an increase in ROS enhances the efficacy of cisplatin and vice versa.46, 47 Moreover, an increase in intracellular Ca2+ concentration enhances cisplatin-mediated ROS production and increases cisplatin cytotoxicity.48, 49, 50 This type of potentiation of cisplatin cytotoxicity may be responsible for the enhanced cisplatin cytotoxicity in electroporated cells, but it yet needs to be elucidated. Michel et al.51 observed an increased immunoreactivity with SOD-2 (an enzyme that clears mitochondrial ROS) in cells subjected to ECT with cisplatin. To the best of our knowledge, this is the only report that measured ROS after ECT with cisplatin.
Our study also has limitations. Two different pulse generators and electrode geometries (i.e., electroporation cuvettes with 2 or 4 mm gap) were used in the cell experiments because of the technical limitations of the pulse generators used. Also in cell experiments, we did not directly measure the amount of cisplatin in cell pellets, but Pt was measured instead and assumed that cisplatin most likely accounts for the majority of the measured amount of Pt in cells incubated with cisplatin. This assumption is supported by the fact that the amount of Pt in non-electroporated cells that were not incubated with cisplatin was 2–3 orders of magnitude lower than in samples incubated with cisplatin or even below the detection limit. We also do not know whether the measured Pt was located inside the cells or was e.g. bound to the surface of the cell membrane. However, the formation of reactive hydrolyzed cisplatin products that would bind immediately and irreversibly to cell membrane phospholipids is not expected because the electroporation medium used has a high concentration of chloride ions so cisplatin should be stable in it and the measured Pt most probably comes from intracellular cisplatin.52 Additionally, in experiments investigating the effects of electric pulses on cisplatin structure, the conditions before the measurements by NMR spectroscopy and HRMS spectrometry could not be fully matched with the conditions in the cell experiments due to several reasons. First, it was namely not possible to record spectra of cisplatin in growth media due to many species present in the growth medium which interfere with cisplatin signals; thus, pulses were delivered to cisplatin dissolved in water or saline for NMR spectroscopy and HRMS spectrometry. Second, because of the limitations of the pulse generator used for NMR spectroscopy and HRMS spectrometry experiments, 25 × 400 ns pulses were delivered at lower amplitudes than in the cell experiments. Third, because of the difference in conductivity, electric pulses delivered to H2O and D2O had a notably different shape than pulses delivered to saline or cells in growth medium; due to the low conductivity of the load, they resembled an exponentially decaying rather than a rectangular pulse shape.
In conclusion, we have shown that by using equivalent nanosecond pulses in ECT, the same decrease in cell survival is achieved and the same amount of cisplatin accumulates in the cells as with the standard 8 × 100 μs pulses, i.e., that in ECT, equivalent nanosecond pulses are equally efficient as 8 × 100 μs pulses. By investigating the underlying mechanisms in nanosecond pulse ECT, we discovered that electroporated CHO cells are more susceptible to cisplatin than non-electroporated cells (regardless of the pulse protocol). The electric pulses used for electroporation do not appear to alter the structure of the cisplatin molecule, so the observed increased susceptibility is likely a consequence of the effect of electroporation on the cells. The use of nanosecond pulses in ECT is promising as it was demonstrated to be effective with the potential to mitigate muscle contractions. Because extensive preclinical data and solid evidence of mechanisms of action have been the basis for introducing ECT into clinical practice, further studies of nanosecond pulse ECT in vivo are necessary to enable translation into clinical trials.
Acknowledgements
The study was funded by Pulse Biosciences and the Slovenian Research Agency (ARRS) (research core funding No. P2-0249 and P1-0175). The work was partially performed within the network of research and infrastructural centres of University of Ljubljana, which is financially supported by Slovenian Research Agency through infrastructural grant IP-0510. A.V. was granted a scholarship from the University Foundation of ing. Lenarčič Milan. We would like to acknowledge dr. Damijana Urankar for HRMS analyses.
Disclosure
No potential conflicts of interest were disclosed.
Supplementary Material.
References
- 1.Miklavčič D, Mali B, Kos B, Heller R, Serša G. Electrochemotherapy: from the drawing board into medical practice. BioMed Eng Online. 2014;13:1–20. doi: 10.1186/1475-925X-13-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campana LG, Miklavčič D, Bertino G, Marconato R, Valpione S, Imarisio I. Electrochemotherapy of superficial tumors – Current status: basic principles, operating procedures, shared indications, and emerging applications. Semin Oncol. 2019;46:173–91. doi: 10.1053/j.seminoncol.2019.04.002. M, et al. [DOI] [PubMed] [Google Scholar]
- 3.Gehl J, Sersa G, Matthiessen LW, Muir T, Soden D, Occhini A, Quaglino P. Updated standard operating procedures for electrochemotherapy of cutaneous tumours and skin metastases. Acta Oncol. 2018;57:874–82. doi: 10.1080/0284186X.2018.1454602. et al. [DOI] [PubMed] [Google Scholar]
- 4.Kendler M, Micheluzzi M, Wetzig T, Simon JC. Electrochemotherapy under tumescent local anesthesia for the treatment of cutaneous metastases. Dermatologic Surg. 2013;39:1023–32. doi: 10.1111/dsu.12190. [DOI] [PubMed] [Google Scholar]
- 5.Schoenbach KH, Beebe SJ, Buescher ES. Intracellular effect of ultrashort electrical pulses. Bioelectromagnetics. 2001;22:440–8. doi: 10.1002/bem.71. [DOI] [PubMed] [Google Scholar]
- 6.Pliquett U, Nuccitelli R. Measurement and simulation of Joule heating during treatment of B-16 melanoma tumors in mice with nanosecond pulsed electric fields. Bioelectrochemistry. 2014;100:62–8. doi: 10.1016/j.bioelechem.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Cornelis FH, Cindrič H, Kos B, Fujimori M, Petre EN, Miklavčič D. Peritumoral metallic implants reduce the efficacy of irreversible electroporation for the ablation of colorectal liver metastases. Cardiovas Intervent Radiol. 2020;43:84–93. doi: 10.1007/s00270-019-02300-y. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vižintin A, Marković S, Ščančar J, Miklavčič D. Electroporation with nanosecond pulses and bleomycin or cisplatin results in efficient cell kill and low metal release from electrodes. Bioelectrochemistry. 2021;140:107898. doi: 10.1016/j.bioelechem.2021.107798. [DOI] [PubMed] [Google Scholar]
- 9.Saulis G, Rodaite R, Rodaitė-Riševičienė R, Dainauskaitė VS, Saulė R. Rai VR. Advances in food biotechnology. First Edition. Wiley Online Books, John Wiley & Sons Ltd; 2016. Electrochemical processes during high-voltage electric pulses and their importance in food processing technology; pp. 575–92. editor. p. –. [Google Scholar]
- 10.Kotnik T, Miklavčič D, Mir LM. Cell membrane electropermeabilization by symmetrical bipolar rectangular pulses: Part II. Reduced electrolytic contamination. Bioelectrochemistry. 2001;54:91–5. doi: 10.1016/S1567-5394(01)00115-3. [DOI] [PubMed] [Google Scholar]
- 11.Loomis-Husselbee JW, Cullen PJ, Irvine RF, Dawson AP. Electroporation can cause artefacts due to solubilization of cations from the electrode plates. Aluminum ions enhance conversion of inositol 1,3,4,5-tetrakisphosphate into inositol 1,4,5-trisphosphate in electroporated L1210 cells. Biochem J. 1991;277(Pt 3):883–5. doi: 10.1042/bj2770883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Long G, Shires PK, Plescia D, Beebe SJ, Kolb JF, Schoenbach KH. Targeted tissue ablation with nanosecond pulses. IEEE Trans Biomed Eng. 2011;58:2161–7. doi: 10.1109/TBME.2011.2113183. [DOI] [PubMed] [Google Scholar]
- 13.Rogers WR, Merritt JH, Comeaux JA, Kuhnel CT, Moreland DF, Teltschik DG. Strength-duration curve an electrically excitable tissue extended down to near 1 nanosecond. IEEE Trans on Plasma Sci. 2004;32:1587–99. doi: 10.1109/TPS.2004.831758. et al. [DOI] [Google Scholar]
- 14.Pakhomov AG, Pakhomova ON. The interplay of excitation and electroporation in nanosecond pulse stimulation. Bioelectrochemistry. 2020;136:107598. doi: 10.1016/j.bioelechem.2020.107598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gudvangen EK, Kondratiev O, Redondo L, Xiao S, Pakhomov AG. Peculiarities of neurostimulation by intense nanosecond pulsed electric fields: how to avoid firing in peripheral nerve fibers. Int J Mol Sci. 2021;22:1763. doi: 10.3390/ijms22137051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gudvangen EK, Novickij V, Battista F, Pakhomov AG. Electroporation and cell killing by milli-to nanosecond pulses and avoiding neuromuscular stimulation in cancer ablation. Sci Rep. 2022;12:1–15. doi: 10.1038/s41598-022-04868-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silve A, Leray I, Mir LM. Demonstration of cell membrane permeabilization to medium-sized molecules caused by a single 10 ns electric pulse. Bioelectrochemistry. 2012;87:260–4. doi: 10.1016/j.bioelechem.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Tunikowska J, Antończyk A, Rembiałkowska N, Jóźwiak Ł Novickij V, Kulbacka J. The first application of nanoelectrochemotherapy in feline oral malignant melanoma treatment – case study. Animals. 2020;10:556. doi: 10.3390/ani10040556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Novickij V, Malyško V, Želvys A, Balevičiūte A, Zinkevičiene A, Novickij J. Electrochemotherapy using doxorubicin and nanosecond electric field pulses: a pilot in vivo study. Molecules. 2020;25:4601. doi: 10.3390/molecules25204601. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kiełbik A, Szlasa W, Novickij V, Szewczyk A, Maciejewska M, Saczko J. Effects of high-frequency nanosecond pulses on prostate cancer cells. Sci Rep. 2021;11:1–10. doi: 10.1038/s41598-021-95180-7. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kulbacka J, Rembiałkowska N, Szewczyk A, Moreira H, Szyjka A, Girkontaitė I. The impact of extracellular Ca2+ and nanosecond electric pulses on sensitive and drug-resistant human breast and colon cancer cells. Cancers. 2021;13:3216. doi: 10.3390/cancers13133216. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.A language and environment for statistical computing. [internet] 2018. https://www.r-project.org/ R Core Team R. Available at.
- 23.Berners-Price SJ, Appleton TG. Kelland LR, Farrell NP. Platinum-based drugs in cancer therapy. Cancer drug discovery and development. Totowa, NJ: Humana Press; 2000. The chemistry of cisplatin in aqueous solution; pp. 3–35. p. –. [DOI] [Google Scholar]
- 24.Chen Y, Guo Z, Sadler PJ. Lippert B. Cisplatin. Chemistry and biochemistry of a leading anticancer drug. Wiley Online Library; 195Pt- and 15N-NMR spectroscopic studies of cisplatin reactions with biomolecules; pp. 293–318. editor. p. –. [DOI] [Google Scholar]
- 25.Cui M, Mester Z. Electrospray ionization mass spectrometry coupled to liquid chromatography for detection of cisplatin and its hydrated complexes. Rapid Commun Mass Spectrom. 2003;17:1517–27. doi: 10.1002/rcm.1030. [DOI] [PubMed] [Google Scholar]
- 26.Feifan X, Pieter C, Jan VB. Electrospray ionization mass spectrometry for the hydrolysis complexes of cisplatin: implications for the hydrolysis process of platinum complexes. J Mass Spectrom. 2017;52:434–41. doi: 10.1002/jms.3940. [DOI] [PubMed] [Google Scholar]
- 27.Du Y, Zhang N, Cui M, Liu Z, Liu S. Investigation on the hydrolysis of the anticancer drug cisplatin by Fourier transform ion cyclotron resonance mass spectrometry. Rapid Commun Mass Spectrom. 2012;26:2832–6. doi: 10.1002/rcm.6408. [DOI] [PubMed] [Google Scholar]
- 28.Cui M, Ding L, Mester Z. Separation of cisplatin and its hydrolysis products using electrospray ionization high-field asymmetric waveform ion mobility spectrometry coupled with ion trap mass spectrometry. Anal Chem. 2003;75:5847–53. doi: 10.1021/ac0344182. [DOI] [PubMed] [Google Scholar]
- 29.Arena CB, Sano MB, Rossmeisl Jr JH, Caldwell JL, Garcia PA, Rylander MN. High-frequency irreversible electroporation (H-FIRE) for non-thermal ablation without muscle contraction. BioMed Eng Online e. 2011;10:102. doi: 10.1186/1475-925X-10-102. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scuderi M, Reberšek M, Miklavčič D, Dermol-Černe J. The use of high-frequency short bipolar pulses in cisplatin electrochemotherapy in vitro. Radiol Oncol. 2019;53:194–205. doi: 10.2478/raon-2019-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pirc E, Miklavčič D, Uršič K, Serša G, Reberšek M. High-frequency and high-voltage asymmetric bipolar pulse generator for electroporation based technologies and therapies. Electronics. 2021. p. 10. [DOI]
- 32.Makovec T. Cisplatin and beyond: molecular mechanisms of action and drug resistance development in cancer chemotherapy. Radiol Oncol. 2019;53:148–58. doi: 10.2478/raon-2019-0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hucke A, Ciarimboli G. The role of transporters in the toxicity of chemotherapeutic drugs: focus on transporters for organic cations. J Clin Pharmacol. 2016;56(Suppl 7):S157–72. doi: 10.1002/jcph.706. [DOI] [PubMed] [Google Scholar]
- 34.Kotnik T, Rems L, Tarek M, Miklavčič D. Membrane electroporation and electropermeabilization: mechanisms and models. Annu Rev Biophys. 2019;48:63–91. doi: 10.1146/annurev-biophys-052118-115451. [DOI] [PubMed] [Google Scholar]
- 35.Ursic K, Kos S, Kamensek U, Cemazar M, Scancar J, Bucek S, Kranjc S, Staresinic B, Sersa G. Comparable effectiveness and immunomodulatory actions of oxaliplatin and cisplatin in electrochemotherapy of murine melanoma. Bioelectrochemistry. 2018;119:161–71. doi: 10.1016/j.bioelechem.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 36.Zakelj MN, Prevc A, Kranjc S, Cemazar M, Todorovic V, Savarin M. Electrochemotherapy of radioresistant head and neck squamous cell carcinoma cells and tumor xenografts. Oncol Rep. 2019;41:1658–68. doi: 10.3892/or.2019.6960. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang L, Ye Y, Zhang X, Li X, Chen Q, Sun JCW. Cisplatin under oriented external electric fields: a deeper insight into electrochemotherapy at the molecular level. Int J Quantum Chem. 2020;121:e26578. doi: 10.1002/qua.26578. [DOI] [Google Scholar]
- 38.Cemază r M, Miklavcĭc ˘ D, Šc̆ăncă r J, Dolză n V, Golouh R, Sersă G. Increased platinum accumulation in SA-1 tumour cells after in vivo electrochemotherapy with cisplatin. Br J Cancer. 1999;79:1386–91. doi: 10.1038/sj.bjc.6690222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Florea AM, Büsselberg D. Cisplatin as an anti-tumor drug: cellular mechanisms of activity, drug resistance and induced side effects. Cancers. 2011;3:1351–71. doi: 10.3390/cancers3011351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pakhomova ON, Khorokhorina VA, Bowman AM, Rodaite-Riševičiene R, Saulis G, Xiao S. Oxidative effects of nanosecond pulsed electric field exposure in cells and cell-free media. Arch Biochem Biophys. 2012;527:55–64. doi: 10.1016/j.abb.2012.08.004. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Szlasa W, Kiełbik A, Szewczyk A, Rembiałkowska N, Novickij V, Tarek M. Oxidative effects during irreversible electroporation of melanoma cells – in vitro study. Molecules. 2021;26 doi: 10.3390/molecules26010154. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Batista Napotnik T, Wu Y-H, Gundersen MA, Miklavčič D, Vernier PT. Nanosecond electric pulses cause mitochondrial membrane permeabilization in Jurkat cells. Bioelectromagnetics. 2012;33:257–64. doi: 10.1002/bem.20707. [DOI] [PubMed] [Google Scholar]
- 43.Nuccitelli R, McDaniel A, Connolly R, Zelickson B, Hartman H. Nano-pulse stimulation induces changes in the intracellular organelles in rat liver tumors treated in situ. Lasers Surg Med. 2020;52:882–9. doi: 10.1002/lsm.23239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Semenov I, Xiao S, Pakhomov AG. Primary pathways of intracellular Ca2 + mobilization by nanosecond pulsed electric field. Biochim Biophys Acta - Biomembr. 2013;1828:981–9. doi: 10.1016/j.bbamem.2012.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Frandsen SK, Gissel H, Hojman P, Tramm T, Eriksen J, Gehl J. Direct therapeutic applications of calcium electroporation to effectively induce tumor necrosis. Cancer Res. 2012;72:1336–41. doi: 10.1158/0008-5472.CAN-11-3782. [DOI] [PubMed] [Google Scholar]
- 46.Marullo R, Werner E, Degtyareva N, Moore B, Altavilla G, Ramalingam SS. Cisplatin induces a mitochondrial-ros response that contributes to cytotoxicity depending on mitochondrial redox status and bioenergetic functions. PLoS ONE. 2013;8:1–15. doi: 10.1371/journal.pone.0081162. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kleih M, Böpple K, Dong M, Gaißler A, Heine S, Olayioye MA. Direct impact of cisplatin on mitochondria induces ROS production that dictates cell fate of ovarian cancer cells. Cell Death Dis. 2019;10:31–59. doi: 10.1038/s41419-019-2081-4. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kawai Y, Nakao T, Kunimura N, Kohda Y, Gemba M. Relationship of intracellular calcium and oxygen radicals to cisplatin-related renal cell injury. J Pharmacol Sci. 2006;100:65–72. doi: 10.1254/jphs.FP0050661. [DOI] [PubMed] [Google Scholar]
- 49.Al-Taweel N, Varghese E, Florea A-M, Büsselberg D. Cisplatin (CDDP) triggers cell death of MCF-7 cells following disruption of intracellular calcium ([Ca2+] i) homeostasis. J Toxicol Sci. 2014;39:765–74. doi: 10.2131/jts.39.765. [DOI] [PubMed] [Google Scholar]
- 50.Gualdani R, de Clippele M, Ratbi I, Gailly P, Tajeddine N. Store-operated calcium entry contributes to cisplatin-induced cell death in non-small cell lung carcinoma. Cancers. 2019;11:2023. doi: 10.3390/cancers11030430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Michel O, Kulbacka J, Saczko J, Mączyńska J, Błasiak P, Rossowska J. Electroporation with cisplatin against metastatic pancreatic cancer: in vitro study on human primary cell culture. Biomed Res Int. 2018;2018:7364539. doi: 10.1155/2018/7364539. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Speelmans G, Sips WHHM, Grisel RJH, Staffhorst RWHM, Fichtinger-Schepman AMJ, Reedijk J. The interaction of the anti-cancer drug cisplatin with phospholipids is specific for negatively charged phospholipids and takes place at low chloride ion concentration. Biochim Biophys Acta - Biomembr. 1996;1283:60–6. doi: 10.1016/0005-2736(96)00080-6. et al. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


