Abstract
Differences in patient characteristics between the PTVT and TVT Studies, including the level of preoperative intraocular pressure, contributed to the differences in surgical failure rates in each trial.
The Tube Versus Trabeculectomy (TVT) Study and Primary Tube Versus Trabeculectomy (PTVT) Study are multicenter randomized clinical trials comparing the efficacy and safety of tube shunt surgery and trabeculectomy with mitomycin C (MMC).1,2 The TVT Study enrolled patients with previous cataract and/or glaucoma surgery, and the PTVT Study recruited patients without prior incisional ocular surgery. Both trials randomly assigned patients to placement of a 350-mm2 Baerveldt glaucoma implant or trabeculectomy with MMC, although a lower dosage of MMC was used in the PTVT Study.
The methodology of the TVT and PTVT Studies were previously described in detail.1,2 Both studies defined surgical failure as intraocular pressure (IOP) > 21 mmHg or reduced < 20% below baseline on 2 consecutive follow-up visits after 3 months, IOP ≤ 5 mmHg on 2 consecutive visits after 3 months, reoperation for glaucoma, or loss of light perception vision. In the TVT Study, the cumulative probability of failure using Kaplan-Meier survival analysis was 15% in the tube group and 31% in the trabeculectomy group after 3 years of follow-up (P = 0.010).3 In the PTVT Study, the cumulative probability of failure was 33% in the tube group and 28% in the trabeculectomy group at 3 years (P = 0.17).4
The rate of surgical failure of trabeculectomy with MMC was higher in the TVT Study than the PTVT Study. These results are consistent with a known higher risk of trabeculectomy failure in eyes with prior ocular surgery, likely related to conjunctival scarring and higher concentrations of inflammatory mediators.5–7 In contrast, the failure rate of tube shunt implantation was higher in the PTVT Study compared with the TVT Study. While the success of tube shunt surgery should be less affected by conjunctival scarring, the higher rate of tube shunt failure in previously unoperated eyes relative to those that have undergone previous ocular surgery is counterintuitive. We believe that differences in patient characteristics between the TVT and PTVT Studies likely contributed to the observed differences in treatment outcomes in each trial.
Randomized clinical trials generally produce balanced study groups that differ only by the treatment received, and they are considered the gold standard for comparing therapeutic interventions within a study population. However, caution must be used in making comparisons across different trials. The study populations from the TVT and PTVT Studies differed not only with respect to the presence or absence of prior ocular surgery, but PTVT Study patients were also on average younger (61.4 years vs 71.0 years), had lower preoperative IOP (23.6 mmHg vs 25.3 mmHg), and were more likely to be of Black race (48% vs 39%). A risk factor analysis from pooled data from the Ahmed Baerveldt Comparison Study, Ahmed Versus Baerveldt Study, and the tube group of the TVT Study identified younger age and lower preoperative IOP as significant predictors of tube shunt failure, with Black race also showing borderline significance (E. Bowden, personal communication, February 3, 2020). It seems likely that a greater prevelance of these risk factors for tube shunt failure in the patient population of the PTVT Study compared with the TVT Study influenced the trial results. Some clinical centers participated in both studies, but many centers recruited patients for only one trial. Minimally invasive glaucoma surgery existed as a surgical option during the time of enrollment for the PTVT Study, but not for the TVT Study. These were likely factors that contributed to differences in patient characteristics between the two trials.
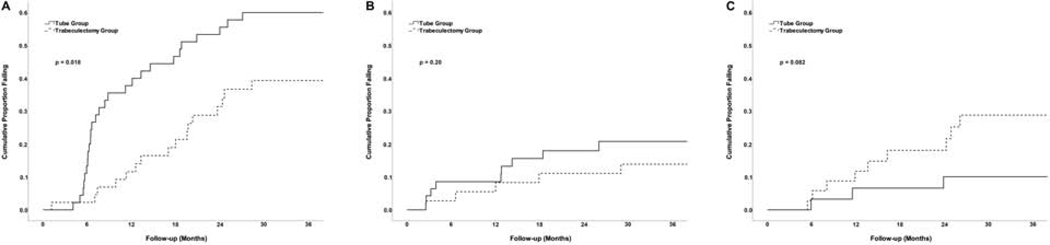
We performed a risk factor analysis in the PTVT Study after 3 years of follow-up to explore baseline demographic and clinical factors as possible predictors for failure. Only lower preoperative IOP was significantly associated with failure in univariable (P < 0.001) and multivariable (P < 0.001) analyses. A significant interaction between treatment and preoperative IOP was associated with surgical failure (P < 0.001). Figure 1 shows Kaplan-Meier survival analysis subdividing patients based on treatment group and preoperative IOP. In the tube group, the cumulative probability of failure was 60% in the 47 patients with preoperative IOP < 21 mmHg, 21% in the 47 patients with IOP 21 to 25 mmHg, and 10% in the 31 patients with IOP > 25 mmHg. In the trabeculectomy group, the cumulative probability of failure was 39% in the 44 patients with preoperative IOP < 21 mmHg, 14% in the 37 patients with IOP 21 to 25 mmHg, and 30% in the 36 patients with IOP > 25 mmHg. The reasons for treatment failure in the PTVT Study are shown in Table 1 (available at www.aaojournal.org).
Figure 1.
Kaplan-Meier plots of the cumulative probability of failure in the PTVT Study among patients with preoperative IOP < 21 mmHg (A), 21 to 25 mmHg (B), and > 25 mmHg (C).
Table 1.
Reasons for Treatment Failure in the PTVT Study Subdividing the Study Population Based on Preoperative Intraocular Pressure
| Tube Group | Trabeculectomy Group | |||||
|---|---|---|---|---|---|---|
| IOP < 21 mmHg (n = 27) | IOP 21–25 mmHg (n = 11) | IOP > 25 mmHg (n = 3) | IOP < 21 mmHg (n = 16) | IOP 21–25 mmHg (n = 5) | IOP > 25 mmHg (n = 9) | |
| Inadequate IOP reduction* | 23 (85) | 2 (18) | 1 (33) | 12 (75) | 3 (60) | 3 (33) |
| Reoperation for glaucoma | 4 (15) | 9 (82) | 2 (67) | 3 (19) | 2 (40) | 3 (33) |
| Persistent hypotony† | 0 | 0 | 0 | 1 (6) | 0 | 3 (33) |
| Loss of light perception vision | 0 | 0 | 0 | 0 | 0 | 0 |
IOP = intraocular pressure
Data are presented as number (percentage)
IOP > 21 mmHg or reduced < 20% below baseline on 2 consecutive follow-up visits after 3 months
IOP ≤ 5 mmHg on 2 consecutive follow-up visits after 3 months
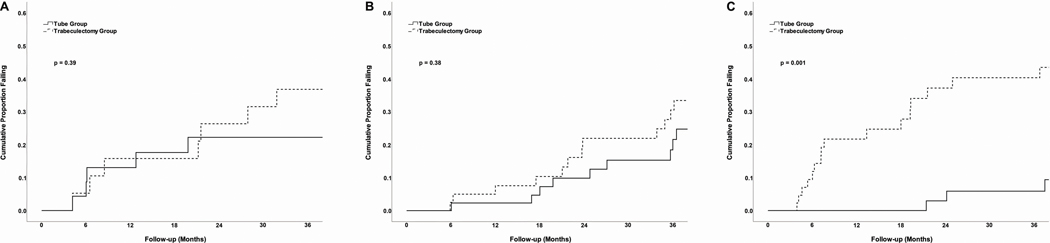
We performed a similar analysis with data from the TVT Study. Identical subgroups of preoperative IOP were used, and Figure 2 (available at www.aaojournal.org) shows the Kaplan-Meier surival plots during the same 3-year follow-up period. In the tube group, the cumulative probability of failure was 22% in the 23 patients with preoperative IOP < 21 mmHg, 22% in the 43 patients with IOP 21 to 25 mmHg, and 6% in the 41 patients with IOP > 25 mmHg. In the trabeculectomy group, the cumulative probability of failure was 37% in the 19 patients with preoperative IOP < 21 mmHg, 31% in the 42 patients with IOP 21 to 25 mmHg, and 40% in the 44 patients with IOP > 25 mmHg. The reasons for treatment failure in the TVT Study are shown in Table 2 (available at www.aaojournal.org).
Figure 2.
Kaplan-Meier plots of the cumulative probability of failure in the TVT Study among patients with preoperative IOP < 21 mmHg (A), 21 to 25 mmHg (B), and > 25 mmHg (C).
Table 2.
Reasons for Treatment Failure in the TVT Study Subdividing the Study Population Based on Preoperative Intraocular Pressure
| Tube Group | Trabeculectomy Group | |||||
|---|---|---|---|---|---|---|
| IOP < 21 mmHg (n = 5) | IOP 21–25 mmHg (n = 10) | IOP > 25 mmHg (n = 4) | IOP < 21 mmHg (n = 7) | IOP 21–25 mmHg (n = 13) | IOP > 25 mmHg (n = 17) | |
| Inadequate IOP reduction* | 3 (60) | 6 (60) | 1 (25) | 6 (86) | 7 (54) | 2 (12) |
| Reoperation for glaucoma | 2 (40) | 3 (30) | 2 (50) | 0 | 4 (31) | 6 (35) |
| Persistent hypotony† | 0 | 1 (10) | 1 (25) | 1 (14) | 1 (8) | 9 (53) |
| Loss of light perception vision | 0 | 0 | 0 | 0 | 1 (8) | 0 |
IOP = intraocular pressure
Data are presented as number (percentage)
IOP > 21 mmHg or reduced < 20% below baseline on 2 consecutive follow-up visits after 3 months
IOP ≤ 5 mmHg on 2 consecutive follow-up visits after 3 months
In both the PTVT and TVT Studies, the efficacy of tube shunt surgery relative to trabeculectomy with MMC was greater at higher levels of preoperative IOP. Patients with lower preoperative IOP benefited most from trabeculectomy with MMC over tube shunt implantation in the PTVT Study. Patients with higher preoperative IOP benefited most from tube shunt surgery over trabeculectomy with MMC in the TVT Study. In a pooled analysis of PTVT and TVT Study data, a significant interaction between treatment and preoperative IOP was associated with surgical failure (P < 0.001). Given the relationship between preoperative IOP and tube shunt failure, it is noteworthy that the proportion of patients with IOP < 21 mmHg was 38% in the PTVT Study and 20% in the TVT Study. The greater percentage of patients with low IOP at baseline likely contributed to a higher failure rate of tube shunt surgery in the PTVT Study compared with the TVT Study.
There are several limitations to our study. The TVT and PTVT Studies enrolled patients who met specific inclusion and excusion criteria, and they underwent a trabeculectomy with MMC or placement of a 350-mm2 Baerveldt glaucoma implant. Study results cannot be generalized to different patient groups, implant types, or dosages of MMC. Although aspects of both surgical procedures were standardized, some variation in surgical techniqe occurred because surgeons were provided with sufficient latitude to perform operations in a manner in which they were comfortable. The patients and investigators were not masked to the randomized treatment assignment in either trial, which introduced a potential source of bias.
The TVT and PTVT Studies provide new insights into the association between preoperative IOP and the efficacy of traditional glaucoma surgery. The decision to perform a trabeculectomy with MMC or tube shunt implantation should be influenced by a history of prior ocular surgery, as has been the conventional wisdom.3–7 However, we believe that preoperative IOP should also be considered when selecting a glaucoma procedure.
Acknowledgments
Supported by research grants from Johnson & Johnson Vision, Santa Ana, California, the National Eye Institute (grant EY014801), National Institutes of Health, Bethesda, Maryland, and Research to Prevent Blindness, Inc., New York, New York.
Mr. Feuer has received grant support from Johnson & Johnson Vison. Dr. Singh is a consultant for Johnson & Johnson Vision. The other authors report no proprietary or commercial interest in any materials discussed in this article.
Abbreviations/acronyms:
- IOP
intraocular pressure
- MMC
mitomycin C
- PTVT
Primary Tube Versus Trabeculectomy
- TVT
Tube Versus Trabeculectomy
Footnotes
Human subjects: Human subjects were included in this study. The study was approved by the institutional review board at each clinical center. All research adhered to the tenets of the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. All participants provided informed consent.
No animal subjects were used in this study.
This article contains additional online-only material. The following should appear online-only: Figure 2.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Gedde SJ, Schiffman JC, Feuer WJ, et al. The Tube Versus Trabeculectomy Study: Design and baseline characteristics of study patients. Am J Ophthalmol. 2005;140:275–87. [DOI] [PubMed] [Google Scholar]
- 2.Gedde SJ, Chen PP, Heuer DK, et al. The Primary Tube Versus Trabeculectomy Study: Methodology of a multicenter randomized clinical trial comparing tube shunt surgery and trabeculectomy with mitomycin C. Ophthalmology. 2018;125:774–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gedde SJ, Schiffman JC, Feuer WJ, et al. Three-year follow-up of the Tube Versus Trabeculectomy Study. Am J Ophthalmol. 2009;148:670–684. [DOI] [PubMed] [Google Scholar]
- 4.Gedde SJ, Feuer WJ, Lim KS, et al. Treatment outcomes in the Primary Tube Versus Trabeculectomy (PTVT) Study after 3 years of follow-up. Ophthalmology. 2020;127:333–345. [DOI] [PubMed] [Google Scholar]
- 5.Gross RL, Feldman, RM, Spaeth GL, et al. Surgical therapy of chronic glaucoma in aphakia and pseudophakia. Ophthalmology. 1988;95:119–1201. [DOI] [PubMed] [Google Scholar]
- 6.Broadway DC, Grierson I, Hitchings RA. Local effects of previous conjunctival incisional surgery and the subsequent outcomes of fitration surgery. Am J Ophthalmol. 2001;85:689–695. [DOI] [PubMed] [Google Scholar]
- 7.Inoue T, Kawaji T, Inatani M, et al. Simultanous increase in multiple proinflammatory cytokines in the aqueous humor in pseudophakic glaucomatous eyes. J Catarat Refract Surg. 2012;38:1389–1397. [DOI] [PubMed] [Google Scholar]