ABSTRACT
The continuous antigenic variation of influenza A viruses remains a major hurdle for vaccine selection; however, the molecular determinants and mechanisms of antigenic change remain largely unknown. In this study, two escape mutants were generated by serial passages of the Eurasian avian-like H1N1 swine influenza virus (EA H1N1 SIV) A/swine/Henan/11/2005 (HeN11) in the presence of two neutralizing monoclonal antibodies (mAbs) against the hemagglutinin (HA) protein, which were designated HeN11-2B6-P5 and HeN11-4C7-P8, respectively. The HeN11-2B6-P5 mutant simultaneously harbored the N190D and I230M substitutions in HA, whereas HeN11-4C7-P8 harbored the M269R substitution in HA (H3 numbering). The effects of each of these substitutions on viral antigenicity were determined by measuring the neutralization and hemagglutination inhibition (HI) titers with mAbs and polyclonal sera raised against the representative viruses. The results indicate that residues 190 and 269 are key determinants of viral antigenic variation. In particular, the N190D mutation had the greatest antigenic impact, as determined by the HI assay. Further studies showed that both HeN11-2B6-P5 and HeN11-4C7-P8 maintained the receptor-binding specificity of the parent virus, although the single mutation N190D decreased the binding affinity for the human-type receptor. The replicative ability in vitro of HeN11-2B6-P5 was increased, whereas that of HeN11-4C7-P8 was decreased. These findings extend our understanding of the antigenic evolution of influenza viruses under immune pressure and provide insights into the functional effects of amino acid substitutions near the receptor-binding site and the interplay among receptor binding, viral replication, and antigenic drift.
IMPORTANCE The antigenic changes that occur continually in the evolution of influenza A viruses remain a great challenge for the effective control of disease outbreaks. Here, we identified three amino acid substitutions (at positions 190, 230, and 269) in the HA of EA H1N1 SIVs that determine viral antigenicity and result in escape from neutralizing monoclonal antibodies. All three of these substitutions have emerged in nature. Of note, residues 190 and 230 have synergistic effects on receptor binding and antigenicity. Our findings provide a better understanding of the functional effects of amino acid substitutions in HA and their consequences for the antigenic drift of influenza viruses.
KEYWORDS: antigenicity, EA H1N1, escape mutant, HA protein, swine influenza virus
INTRODUCTION
Swine influenza is an acute respiratory disease caused by swine influenza virus (SIV). Pigs have been proposed to be a “mixing vessel” of influenza viruses due to the presence of human- and avian-like sialic acid receptors on their cells, which play important roles in the transmission of viruses and the generation of new strains (1, 2). Multiple lineages of H1N1, H1N2, and H3N2 SIVs cocirculate in swine populations (3, 4). Avian-like H1N1 SIV was first isolated from pigs in 1979 in Belgium (5) and has since spread to many European and Asian countries (6–8); for this reason, it is referred to as Eurasian avian-like H1N1 SIV (EA H1N1 SIV). After the reintroduction of the human pandemic 2009/H1N1 virus to pigs, multiple genotypes of reassortant H1N1 and H1N2 SIVs bearing the hemagglutinin (HA) gene of EA H1N1 SIV have replaced the pure EA H1N1 SIV and are currently prevalent in swine populations in China (9–13). Sporadic infections caused by EA H1N1 or EA H1N1-like viruses and antigenic variation within these viruses pose new potential threats to public health and also present new challenges to the pig industry (10, 12, 14–19).
HA is the key surface glycoprotein of influenza viruses that mediates infection. Antibodies against HA generally neutralize viral infectivity, presumably by interfering with either virus attachment to sialic acid receptors on the host cell surface or the subsequent process of fusion between the virus and endosomal membrane (20–22). Antigenic shift, caused by gene reassortment involving HAs of different subtypes, and antigenic drift, caused mainly by gene mutation in HA, have been widely documented (23–25). Antigenic drift, which plays a pivotal role in the evolution and persistence of influenza viruses in various animal and human populations, leads to the gradual accumulation of point mutations in epitopes or antibody-binding regions. A drifted strain usually carries mutations in several major epitopes of the viral HA surface protein. Several epitopes located around the receptor-binding site of the HA head region (including Sa, Sb, Ca1, Ca2, and Cb) have been proposed as antigenic sites of H1N1 HA based on variants selected by monoclonal antibodies (mAbs) (26, 27).
The targets of antiviral immunity are located mainly on the HA glycoprotein; therefore, it is important to reveal the antigenically relevant parts of the HA molecule that are prone to amino acid substitutions that lead to the acquisition of resistance to neutralizing antibodies. We previously characterized two murine mAbs against the HA of an EA H1N1 SIV (A/swine/Henan/11/2005 [HeN11]) with neutralizing and hemagglutination inhibition (HI) activities that provide complete protection when administered passively to mice prior to challenge with the homologous virus (28). In the present study, escape mutants of HeN11 were generated via virus propagation in the presence of mAbs to identify the key amino acid residues that determine the antigenicity of EA H1N1 SIV. In addition, the impacts of escape mutations on cross-reactive mAb neutralization, antigenicity, receptor-binding specificity or affinity, and viral replication in vitro were also evaluated.
RESULTS
Generation of escape mutants.
To identify the key residues of the epitopes recognized by the two neutralizing mAbs, escape mutants of HeN11 were selected by coculturing the virus with the mAbs. Variants were established when similar levels of growth were obtained in the presence and absence of the mAbs; that is, the virus was no longer neutralized. One variant was generated by the coculturing of HeN11 with mAb 2B6 for five passages and was designated HeN11-2B6-P5. The other variant, designated HeN11-4C7-P8, was generated by the coculturing of HeN11 with mAb 4C7 for eight passages. The complete genomes of the escape mutants were sequenced, and amino acid point mutations were identified by sequence comparisons to the wild-type HeN11 virus. The HeN11-2B6-P5 mutant harbored the N190D and I230M substitutions in HA (H3 numbering), and the HeN11-4C7-P8 harbored the M269R mutation in HA (H3 numbering). Selection for an additional three passages identified no further mutations. No passage-related mutation was detected in the viruses incubated in the absence of the mAbs.
Location of the mutated amino acid residues in the HA structure.
To locate the mutated amino acid residues in the structure of the HA protein, homology models of the HA protein of HeN11 with the three substitutions (N190D, I230M, and M269R) were constructed by using the SWISS-MODEL online server (https://swissmodel.expasy.org). Ramachandran plots revealed that 97.12% of the residues were located in favored regions, indicating that the model was of high quality. The residue at position 190 is located in helix 190 of the receptor-binding site, whereas the residue at position 230 is located at the bottom of the receptor-binding site. Both residues belong to antigenic site Sb of H1 HAs (Fig. 1). The residue at position 269 is located in the head domain of HA and not in any antigenic regions identified previously in the H1 HAs but instead is located in the region corresponding to antigenic site C of H3 HAs (Fig. 1).
FIG 1.
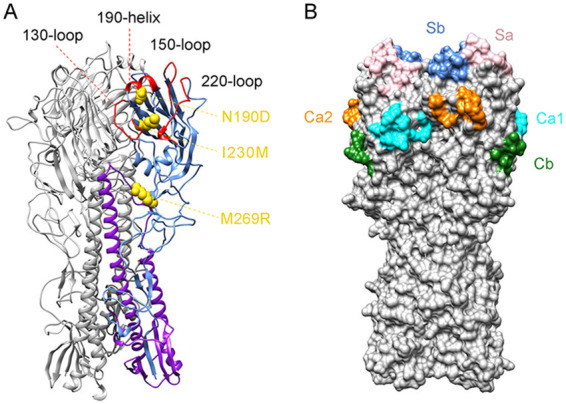
Homology model of HA and location of the mutated amino acid residues in the HA structure. (A) One promoter of the trimeric HA, with HA1 in cornflower blue, HA2 in purple, and the three mutated residues shown as gold spheres. The other two HAs are in gray. The 190 helix, 130 loop, 150 loop, and 220 loop of the receptor-binding site are labeled and shown in red. (B) The surface of the HA trimer. Highlighted sites are Sa (pink), Sb (cornflower blue), Ca1 (cyan), Ca2 (orange), and Cb (forest green).
N190D and M269R are key mediators of antibody binding of the escape mutants.
The HeN11-2B6-P5 mutant carries a double mutation of N190D and I230M in HA. To explore whether both residues acted as functional mediators of antibody binding, we used reverse genetics to rescue the recombinant HeN11 (rHeN11) virus and the recombinant mutants rHeN11/N190D and rHeN11/I230M by introducing the N190D and I230M substitutions, respectively, into the HA of HeN11. We then tested their reactivities with mAb 2B6 in a neutralization assay. As shown in Table 1, the neutralization titer of the mAb against the rHeN11/N190D mutant was 40, which was 16-fold lower than that against the rHeN11 virus. However, there was only a 2-fold reduction in the neutralization titer of the mAb against the rHeN11/I230M mutant, in contrast to the rHeN11 virus (Table 1). In the HeN11-4C7-P8 mutant, the single mutation M269R in HA abolished the ability of mAb 4C7 to bind the virus. These results demonstrate that N190D and M269R are key mediators of the antibody-binding abilities of the escape mutants and that I230M is probably a concomitant compensatory mutation acquired during the generation of the escape mutants.
TABLE 1.
Effects of the amino acid substitution(s) on antigenic variation tested by using a mAb and polyclonal seraa
| Virus | Neutralization antibody titer of mAb 2B6c | HI antibody titer of antisera induced by different virusesb |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| rHeN11 |
rHeN11/N190D |
rHeN11/PR8 |
rHeN11/N190D/PR8 |
||||||
| Chicken sera | Pig sera | Chicken sera | Pig sera | Chicken sera | Pig sera | Chicken sera | Pig sera | ||
| rHeN11 | 640 | 1,024 | 2,560 | 256 | 160 | 512 | 640 | 256 | 160 |
| HeN11-2B6-P5 | <10 | 128 | 160 | 1,024 | 1,280 | 64 | 160 | 512 | 640 |
| HeN11-4C7-P8 | NT | 512 | 1,280 | 128 | 320 | 512 | 1,280 | 128 | 160 |
| rHeN11/N190D | 40 | 64 | 160 | 1,024 | 1,280 | 64 | 320 | 512 | 640 |
| rHeN11/I230M | 320 | 512 | 1,280 | 256 | 160 | 256 | 1,280 | 256 | 320 |
| rHeN11/PR8 | NT | 512 | 1,280 | 256 | 320 | 1,024 | 1,280 | 128 | 320 |
| rHeN11/N190D/PR8 | NT | 64 | 320 | 512 | 1,280 | 64 | 160 | 1,024 | 1,280 |
The antisera were generated by vaccinating specific-pathogen-free chickens or pigs with the indicated oil-emulsified inactivated viruses.
The homologous titers are shown in boldface type.
NT, not tested.
Validation of the antigenic effects of the amino acid substitutions.
First, we tested whether the antibodies induced by the rHeN11 virus still recognized the two escape mutants HeN11-2B6-P5 and HeN11-4C7-P8. Postvaccination sera were generated by inoculating chickens and pigs with the rHeN11 vaccine and tested in an HI assay using the rHeN11 virus and the two escape mutants HeN11-2B6-P5 and HeN11-4C7-P8 as antigens. As shown in Table 1, the HI antibody titers of the HeN11-2B6-P5 mutant with the rHeN11-vaccinated sera from chickens and pigs were 8- and 16-fold lower than the homologous titers. However, the HeN11-4C7-P8 mutant reacted well with the two sera, and the titers were only 2-fold lower than the homologous ones (Table 1). To further determine whether N190D or I230M in the HA of the HeN11-2B6-P5 mutant led to the evasion of recognition by serum antibodies, we performed the HI assay using the rHeN11/N190D and rHeN11/I230M viruses as antigens. The HI titers of the rHeN11/N190D virus with the chicken and pig sera were 16-fold lower than the homologous titers. However, compared to those of the rHeN11 virus, there was a 2-fold reduction in the HI antibody titer of the rHeN11/I230M virus with the two sera (Table 1).
Next, we prepared sera against the rHeN11/N190D virus and performed HI cross-reactions with the test viruses. As shown in Table 1, each serum sample reacted well with the HeN11-2B6-P5 mutant, but the antibody titers against the rHeN11, HeN11-4C7-P8, and rHeN11/I230M viruses were reduced by 4- to 8-fold. Taken together, these results demonstrate that the double mutation of N190D and I230M in HA decreases the reactivity of the HeN11-2C6-P5 mutant with antibodies induced by the rHeN11 virus, whereas the single mutation of M269R is insufficient to reduce the interaction of the HeN11-4C7-P8 mutant with sera against the rHeN11 virus, and the N190D substitution in HA is the key factor influencing viral antigenicity.
To eliminate the impact of other viral proteins on the HI assay, we used the A/Puerto Rico/8/1934 (H1N1) (PR8) virus as a backbone and rescued HeN11/PR8 (1+7) recombinants bearing either the wild-type or mutated HeN11HA gene harboring the single mutation N190D, and the other seven genes of PR8 virus, as described previously (29), which we named rHeN11/PR8 and rHeN11/N190D/PR8, respectively. We then performed HI tests using polyclonal antisera against these two recombinant viruses (Table 1). Compared to those of the rHeN11/PR8 virus, there were 16- and 8-fold reductions in the HI titers of the rHeN11/N190D/PR8 virus with the rHeN11/PR8-vaccinated chicken and pig sera. Conversely, the HI titers of the rHeN11/PR8 virus with the two rHeN11/N190D/PR8-vaccinated sera were 8- and 4-fold lower than the homologous titers (Table 1). These data confirm that the N190D mutation in HA has a high impact on the antigenic variation of the EA H1N1 viruses.
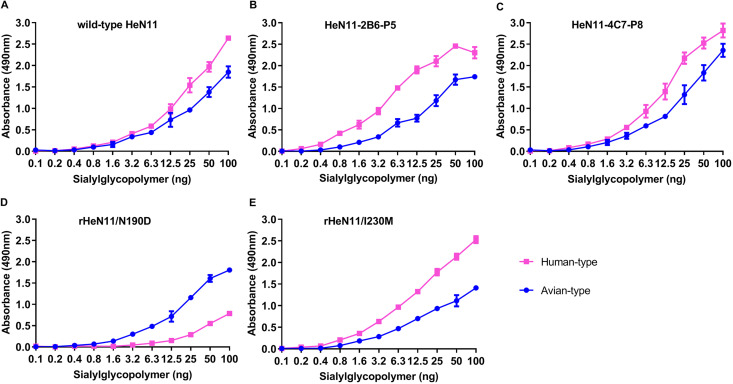
Effects of amino acid changes in the escape mutants on viral receptor-binding preference.
To determine if the amino acid substitutions of the escape mutants altered the viral receptor-binding preference, a solid-phase binding assay was performed to test the receptor-binding properties of the wild-type HeN11 virus and the two escape mutants. The escape mutants HeN11-2B6-P5 and HeN11-4C7-P8 maintained the same receptor-binding properties as those of the wild-type HeN11 virus, binding to both the avian- and human-type receptors with high affinity (Fig. 2A to C). We then tested the receptor-binding preferences of the rHeN11/N190D and rHeN11/I230M mutants. Compared with the wild-type HeN11 virus, the rHeN11/N190D virus showed a decreased binding affinity for the human-type receptor (Fig. 2D), whereas the I230M mutation had no impact on the receptor-binding preference (Fig. 2E). These results indicate that the N190D mutation in HA decreases the affinity of EA H1N1 SIV for the human-type receptor, and while the I230M substitution per se has no effect on receptor-binding properties, in the presence of the N190D mutation, it might synergistically restore the binding affinity of the HeN11-2B6-P5 mutant for the human-type receptor.
FIG 2.
Receptor-binding properties of the indicated viruses. The receptor-binding specificity was tested using two different glycopolymers: an α-2,3-sialylglycopolymer (Neu5Acα2-3Galβ1-4GlcNAcβ1-pAP [para-aminophenyl]-α-PGA [α-polyglutamic acid]) and an α-2,6-sialylglycopolymer (Neu5Acα2-6Galβ1-4GlcNAcβ1-pAP-α-PGA). Chicken antisera against the indicated viruses were used as the primary antibodies, and a horseradish peroxidase-conjugated goat anti-chicken antibody was used as the secondary antibody. The absorbance was measured at a wavelength of 490 nm. The data are presented as the means ± SD from three replicates. (A) Wild-type HeN11 virus. (B) Escape mutant virus HeN11-2B6-P5. (C) Escape mutant virus HeN11-4C7-P8. (D) Rescued virus rHeN11/N190D. (E) Rescued virus rHeN11/I230M.
Replicative abilities of the escape mutants.
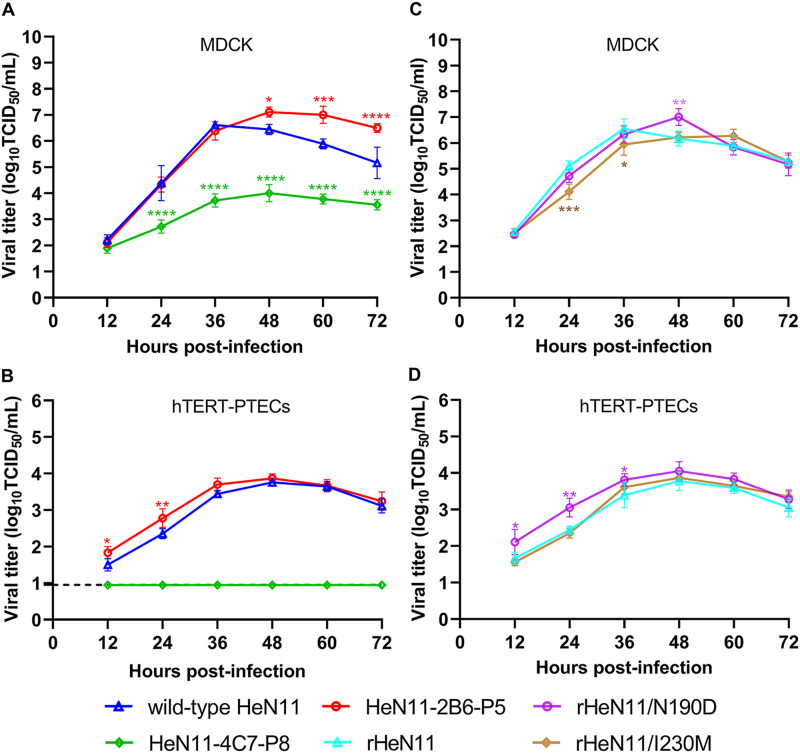
To determine whether both escape mutants maintained a level of replicative ability similar to that of the parent HeN11 virus, we examined virus growth kinetics in Madin-Darby canine kidney (MDCK) cells and human telomerase reverse transcriptase-immortalized porcine tracheal epithelial cells (hTERT-PTECs), which were prepared by transfecting primary PTECs with hTERT (30). Compared with that of the parent HeN11 virus, the replication of the HeN11-2B6-P5 mutant was significantly increased in MDCK cells in the late stage of infection (i.e., 48 to 72 h postinfection [hpi]) (Fig. 3A). In contrast, the replication of the HeN11-4C7-P8 mutant was significantly decreased at all time points tested except 12 hpi (Fig. 3A). Interestingly, the HeN11-2B6-P5 mutant displayed significantly increased replication compared with that of the parent HeN11 virus in hTERT-PTECs at 12 and 24 hpi, whereas the replication of the HeN11-4C7-P8 mutant was completely impaired at all time points tested (Fig. 3B).
FIG 3.
Replication kinetics of wild-type HeN11 and mutant viruses in vitro. MDCK cells and hTERT-PTECs were infected at multiplicities of infection of 0.001 and 0.01. Supernatants were collected at 12, 24, 36, 48, 60, and 72 hpi, and the virus titers were determined by a TCID50 assay in MDCK cells. (A and B) The wild-type HeN11 virus and two escape mutants in MDCK cells and hTERT-PTECs. (C and D) The three rescued viruses in MDCK cells and hTERT-PTECs. Each data point on the curve indicates the mean ± SD from three independent experiments. *, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001. The dashed lines indicate the lower limits of detection.
To determine the effect of each mutated residue on the replicative ability of the escape mutant HeN11-2B6-P5, the replicative capacities of the parent virus and the rescued rHeN11/N190D and rHeN11/I230M viruses were also compared in MDCK cells and hTERT-PTECs. In MDCK cells, both of the rHeN11/N190D and rHeN11/I230M mutants maintained replication characteristics similar to those of the rHeN11 virus at each time point, except at 48 hpi for rHeN11/N190D and 24 and 36 hpi for rHeN11/I230M (Fig. 3C). In hTERT-PTECs, the rHeN11/N190D mutant displayed significantly increased replication in the early stage of infection (i.e., 12 to 36 hpi) compared with the rHeN11 virus. In contrast, no significant difference in replication was observed between the rHeN11/I230M and rHeN11 viruses (Fig. 3D).
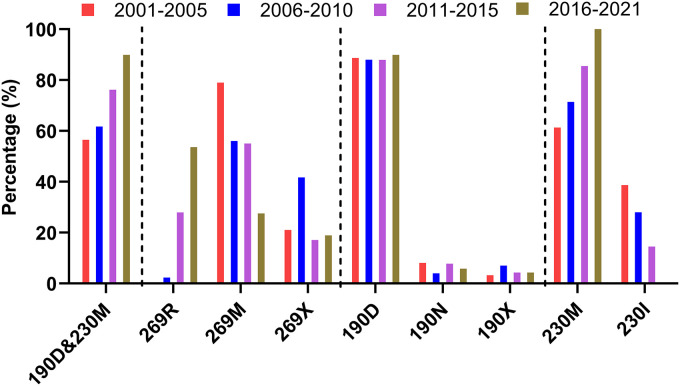
Escape mutants have emerged in nature.
To investigate the polymorphism of each mutated residue detected in the escape mutants, all EA H1 HA sequences of influenza viruses, irrespective of host origin, including branches of 1C1, 1C1-2-like, 1C2, 1C2-like, 1C2.1, 1C2.2, 1C2.2-3-like, and 1C2.3, from 2001 to 2021 at 5-year intervals were downloaded from the Influenza Research Database (https://www.fludb.org/brc/home.spg?decorator=influenza [up to 29 November 2021]). Multiple-sequence alignments of the amino acid sequences of the corresponding regions of the HA proteins were conducted using the MAFFT multiple-sequence alignment program (https://mafft.cbrc.jp/alignment/software/). The two mAb escape mutations, including the double-amino-acid substitution of N190D and I230M and the single mutation of M269R, were found in naturally isolated influenza viruses bearing EA lineage H1 HA (Fig. 4). The percent representation of the HA double mutation of 190D and 230M had gradually increased from 56.5% in 2001 to 89.9% in 2021. The amino acid residue at position 269 of the analyzed sequences varied, with six different amino acid residues besides M and R (designated X in Fig. 4). A virus carrying the HA mutation 269R was first isolated in China in 2010. The prevalence of 269R increased from 2.3% to 53.6% and is now the most common mutation (Fig. 4). Further analysis of the amino acid frequencies at positions 190 and 230 revealed that the most common mutations at position 190 of HA were D, N, V, and S, with 190D accounting for about 88.6%. At position 230, there were two amino acids, 230I and 230M. The percentage of 230M gradually increased from 61.3% in 2001 to 100% in 2021, having completely replaced 230I in 2016 (Fig. 4).
FIG 4.
Polymorphism analysis of the mutated residues in the escape mutants of the HeN11 virus. A total of 768 H1 HA sequences of influenza viruses, including branches of 1C1, 1C1-2-like, 1C2, 1C2-like, 1C2.1, 1C2.2, 1C2.2-3-like, and 1C2.3, isolated from 2001 to 2021 were downloaded from the Influenza Research Database (https://www.fludb.org/brc/home.spg?decorator=influenza [up to 29 November 2021]). These sequences were then subjected to multiple-sequence alignments of the corresponding regions of the HA proteins by using the MAFFT multiple-sequence alignment program (https://mafft.cbrc.jp/alignment/software/). X indicates amino acid residues at the indicated positions other than those found in the HeN11 parent virus and escape mutants.
DISCUSSION
Influenza viruses continually escape antibody-mediated neutralization by changing the amino acid residues in their HA head domain, which induces antigenic drift. Various methods to quantify antigenic drift, as well as site-directed mutagenesis, have revealed that substantial antigenic drift can be caused by one or a few amino acid substitutions adjacent to the functional sites in the head, but not the stalk, of HA (31–33). In the present study, two escape mutants, HeN11-2B6-P5 and HeN11-4B7-P8, were generated by serial passages of the HeN11 virus in MDCK cells in the presence of neutralizing mAbs. The HeN11-2B6-P5 mutant simultaneously carried two mutations, at positions 190 and 230, and the HeN11-4B7-P8 mutant harbored a single mutation, at position 269. Mapping of the HA epitopes revealed that all three mutated residues were located in the head domain of HA. In general, a variant is considered antigenically different when the neutralization titer is reduced by more than 8-fold relative to that of a reference strain (34). In our study, the HeN11-2B6-P5 mutant escaped from mAb 2B6 and the HeN11-4B7-P8 mutant escaped from mAb 4C7 when screened by using a neutralization assay. To further screen the antigenicity-associated amino acid sites, the antigenicities of the two escape mutants were analyzed by neutralization and HI assays using the mAbs 2B6 and 4C7 as well as antisera against the corresponding viruses. The results suggest that the double mutation of N190D and I230M in HA or the single mutation of M269R in HA is sufficient to induce the antigenic drift of EA H1N1 SIV, which is consistent with previous findings that major antigenic changes in seasonal human influenza viruses are due to amino acid substitutions immediately adjacent to the receptor-binding site (32).
Antigenic changes that are sometimes due to a lower affinity for sialic acid and substitutions outside the antigenic motif may be compensatory or simply hitchhiker mutations (35–37). Various amino acid substitutions in the receptor-binding-site regions have been reported to affect the affinity of HA for sialic acid receptors (38–40). In particular, residue 190 plays a prominent role in the receptor-binding preferences of the pandemic 1918/H1N1, avian H1N1, and pandemic 2009/H1N1 viruses (41–44). In the present study, we found that the amino acid substitution N190D reduced the affinity for the human-type sialic acid receptor, which indicates that residue 190 also affects the virus receptor-binding preference of EA H1N1 SIV. In our study, we also found that the rHeN11/I230M mutant harboring a single mutation at position 230 in HA possessed the same reactivity with the mAbs and polyclonal antisera used in the neutralization and HI assays, which demonstrates that a compensatory mutation was induced during the generation of the mAb escape mutant.
The antigenic drift of influenza viruses usually comes with a fitness cost or produces some concomitant effects (45). Therefore, it is important to evaluate the fitness of escape mutants to understand the impact of each mutation in the globular head region of HA. Accordingly, we performed viral growth curve experiments using MDCK cells and hTERT-PTECs and found that the replicative abilities in vitro of the HeN11-2B6-P5 mutant were enhanced at different stages of infection in these two cell types. In contrast, the replicative abilities of the HeN11-4C7-P8 mutant were reduced compared with those of the parent virus. Thus, these two escape mutants showed different fitness changes when their replication kinetics were evaluated, and the underlying mechanism requires further study.
The mechanisms of immune escape of influenza viruses are sometimes ascribed to amino acid substitutions that alter the biophysical properties of an epitope and have the potential to cause antigenic change by directly affecting antibody binding. Amino acid substitutions that lead to an additional N-linked glycosylation site in HA have been shown to affect the antigenicity of influenza viruses by masking the antigenic epitopes in the globular region (29, 46, 47). The single-amino-acid substitution G158E in the HA of EA H1N1 SIV was reported previously to alter viral antigenicity, probably due to steric effects (48). In addition, amino acid substitutions that modulate receptor-binding avidity can also contribute to apparent antigenic changes as detected by the HI assay (37, 48). Modulation of avidity has been proposed as a true form of immune escape rather than an artifact of the HI assay (35, 36, 49–51). The results of the present study suggest that residues 190 and 230 play important roles in the antigenicity of EA H1N1 SIV and could be involved in the specificity of host cell recognition. Epitope identification demonstrated that an avian receptor residue at position 190 was essential for antigen recognition. In the present study, the single-amino-acid substitution N190D was found to influence the receptor-binding affinity for the human-type receptor of EA H1N1 SIV, suggesting that the regulation of receptor-binding affinity may be an important mechanism underlying the generation of immune escape variants of EA H1N1 SIV under natural conditions.
Our study found that complete neutralization resistance to two murine mAbs was conferred by the double substitution of N190D and I230M in HA or the single substitution of M269R in HA of EA H1N1 SIV. The decreased affinity for the human-type sialic acid receptor correlated with the antigenicity changes associated with the N190D substitution in the HA of the escape mutant. Given the possibility for antigen drift caused by the widespread presence of EA H1N1 SIV in pigs and the continuing sporadic introductions to humans, intensive monitoring of the effects of mutations in HA is necessary to predict variants with pandemic potential.
MATERIALS AND METHODS
Ethics statement and facility.
The study protocol was approved by the Committee on the Ethics of Animal Experiments of the Harbin Veterinary Research Institute of the Chinese Academy of Agricultural Sciences (Harbin, China) and conducted in strict accordance with the guide for the care and use of laboratory animals of the Ministry of Science and Technology of China (55). All animals were housed in a biosafety level 2 facility.
Cells, viruses, and antibodies.
Human embryonic kidney HEK293T cells were maintained in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum (FBS). MDCK cells were cultured in DMEM containing 5% FBS. hTERT-PTECs were cultured in DMEM/F-12 medium supplemented with 10% FBS and epithelial cell growth factors (Lonza, Basel, Switzerland), as described previously (30). A/swine/Henan/11/2005 (H1N1) (HeN11) (GenBank accession numbers HQ541672 to HQ541679) was isolated from pigs in China. Virus was propagated in MDCK cells and titrated by the Reed-Muench method to determine the 50% tissue culture infectious dose (TCID50) (52).
Two murine mAbs against HA, designated 2B6 and 4C7, were generated by using the purified EA H1N1 SIV HeN11 protein as the immunogen. Both mAbs possessed high virus-neutralizing activities with strong antiviral infection abilities (protective efficacies), as verified in BALB/c mice (28). Chicken antisera against the respective viruses, including the wild-type virus, the escape mutant, and the single-site-directed mutant, were raised by immunization with oil-emulsified inactivated vaccines. Eight-week-old specific-pathogen-free chickens were immunized with 0.2 mL of a whole-virus inactivated oil-emulsified vaccine. Three weeks after vaccination, sera were collected from the chickens, and titers were determined by using the HI assay. Pig antisera against the corresponding viruses were prepared by inoculating 6-week-old pigs that were seronegative for H1 and H3 subtype SIVs. Three weeks after immunization, sera were collected from the pigs and treated with receptor-destroying enzyme prior to use in the HI assay.
Selection of in vitro escape mutants.
The mAb-resistant mutants were selected by propagating the HeN11 virus in the presence of increasing concentrations of mAbs. In brief, mAbs were serially diluted 2-fold and mixed with the HeN11 virus. The virus-mAb mixtures at various mAb dilutions were incubated for 1 h at 37°C and then transferred to MDCK cells. After incubation for 1 h at 37°C under 5% CO2, the medium was replaced with virus growth medium containing 1 μg/mL tosylsulfonyl phenylalanyl chloromethyl ketone (TPCK)-trypsin, and the plates were then incubated at 37°C until HA activities were detected. The culture supernatants that were positive for virus and those with the highest viable concentrations of mAbs were then collected for the next passage. The mAb concentration was increased after each passage, and the initial selection process ended when the passaged virus was no longer neutralized by the respective mAbs. The virus was also propagated in the absence of mAbs in parallel to detect any passage-related mutations.
Viral whole-genome sequencing.
The whole genome of the virus at each passage was sequenced by using an Applied Biosystems (Carlsbad, CA, USA) 3500xL genetic analyzer, as described previously (13). Briefly, viral RNA (vRNA) was extracted using a QIAamp viral RNA minikit (Qiagen, Germantown, MD, USA), and cDNA was synthesized from vRNA, reverse transcribed by using Uni12 primers, and amplified by PCR by using primers specific for each fragment (the primer sequences are available upon request).
Homology modeling.
The SWISS-MODEL online server was used to construct a homology model of HA. Briefly, the amino acid sequence of HA was submitted to the server, and 50 templates were retrieved from the Protein Data Bank (PDB). The base-matched template (PDB accession number 6ONA) showed 76.47% sequence identity to the target HA. Three-dimensional models of the HA trimer were constructed, and the quality of the models was evaluated with Ramachandran plots. The model was visualized and analyzed by using the University of California, San Francisco, Chimera program (https://www.cgl.ucsf.edu/chimera/).
Virus rescue.
A bidirectional eight-plasmid-based reverse genetic system for HeN11 was constructed to insert the corresponding gene into the vector pHW2000 (kindly provided by Richard Webby of St. Jude Children’s Research Hospital, Memphis, TN, USA) and used to rescue the virus as described previously (13). Reassortant viruses were rescued by transfecting cocultured human embryonic kidney HEK293T and MDCK cells with the recombinant plasmids, propagated in MDCK cells or 10-day-old specific-pathogen-free embryonated chicken eggs, followed by whole-genome sequencing to ensure the absence of unwanted mutations. The primer sequences for virus rescue are available upon request.
Serological testing.
HI and neutralization reactivities were tested as previously described (53), and titers were determined as the highest dilution that completely inhibited viral hemagglutination activities.
Receptor-binding assay.
The receptor preference of each tested virus was examined by using a solid-phase binding assay as described previously (54), using two different glycopolymers: an α-2,3-sialylglycopolymer (Neu5Acα2-3Galβ1-4GlcNAcβ1-pAP [para-aminophenyl]-α-PGA [α-polyglutamic acid]) (avian-type receptor) and an α-2,6-sialylglycopolymer (Neu5Acα2-6Galβ1-4GlcNAcβ1-pAP-α-PGA) (human-type receptor). Chicken antisera against the respective viruses were used as the primary antibodies, and a horseradish peroxidase-conjugated goat anti-chicken antibody (Sigma-Aldrich, St. Louis, MO, USA) was used as the secondary antibody. The absorbance was measured at a wavelength of 490 nm. Each experiment included three replicates.
Viral growth kinetics.
MDCK cells and hTERT-PTECs were infected with the test viruses at multiplicities of infection of 0.001 and 0.01 in the presence of 1 μg/mL and 0.1 μg/mL TPCK-trypsin, respectively, at 37°C. Supernatants were collected at 12, 24, 36, 48, 60, and 72 hpi and stored at −80°C. The viral titers were determined by endpoint titration and expressed as the mean log10 TCID50 per milliliter ± the standard deviation (SD) from three independent experiments.
Statistical analysis.
Data were analyzed by using two-way analysis of variance followed by Tukey’s multiple-comparison test in GraphPad Prism software (version 8.0; GraphPad Software, Inc., San Diego, CA, USA). A P value of <0.05 was considered statistically significant.
Data availability.
The HA genes of the escape mutants were sequenced and have been deposited in GenBank under the accession numbers ON479265 and ON479266.
ACKNOWLEDGMENTS
This study was supported by the National Key Research and Development Program of China (grant number 2021YFD1800200) and the National Natural Science Foundation of China (grant number 31872472).
We thank Xing Xie (Jiangsu Academy of Agricultural Sciences) for providing hTERT-PTECs and for helpful discussions.
Contributor Information
Chuanling Qiao, Email: qiaochuanling@caas.cn.
Hualan Chen, Email: chenhualan@caas.cn.
Stacey Schultz-Cherry, St. Jude Children’s Research Hospital.
REFERENCES
- 1.Ito T, Couceiro JN, Kelm S, Baum LG, Krauss S, Castrucci MR, Donatelli I, Kida H, Paulson JC, Webster RG, Kawaoka Y. 1998. Molecular basis for the generation in pigs of influenza A viruses with pandemic potential. J Virol 72:7367–7373. 10.1128/JVI.72.9.7367-7373.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ma W, Kahn RE, Richt JA. 2008. The pig as a mixing vessel for influenza viruses: human and veterinary implications. J Mol Genet Med 3:158–166. [PMC free article] [PubMed] [Google Scholar]
- 3.Qiao C, Liu L, Yang H, Chen Y, Xu H, Chen H. 2014. Novel triple reassortant H1N2 influenza viruses bearing six internal genes of the pandemic 2009/H1N1 influenza virus were detected in pigs in China. J Clin Virol 61:529–534. 10.1016/j.jcv.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Anderson TK, Chang J, Arendsee ZW, Venkatesh D, Souza CK, Kimble JB, Lewis NS, Davis CT, Vincent AL. 2021. Swine influenza A viruses and the tangled relationship with humans. Cold Spring Harb Perspect Med 11:a038737. 10.1101/cshperspect.a038737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pensaert M, Ottis K, Vandeputte J, Kaplan MM, Bachmann PA. 1981. Evidence for the natural transmission of influenza A virus from wild ducts [sic] to swine and its potential importance for man. Bull World Health Organ 59:75–78. [PMC free article] [PubMed] [Google Scholar]
- 6.Guan Y, Shortridge KF, Krauss S, Li PH, Kawaoka Y, Webster RG. 1996. Emergence of avian H1N1 influenza viruses in pigs in China. J Virol 70:8041–8046. 10.1128/JVI.70.11.8041-8046.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown I. 2000. The epidemiology and evolution of influenza viruses in pigs. Vet Microbiol 74:29–46. 10.1016/s0378-1135(00)00164-4. [DOI] [PubMed] [Google Scholar]
- 8.Liu J, Bi Y, Qin K, Fu G, Yang J, Peng J, Ma G, Liu Q, Pu J, Tian F. 2009. Emergence of European avian influenza virus-like H1N1 swine influenza A viruses in China. J Clin Microbiol 47:2643–2646. 10.1128/JCM.00262-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang H, Lam TTY, Fan X, Chen X, Zeng Y, Zhou J, Duan L, Tse M, Chan CH, Li L, Leung TY, Yip CH, Cheung CL, Zhou B, Smith DK, Poon LLM, Peiris M, Guan Y, Zhu H. 2014. Expansion of genotypic diversity and establishment of 2009 H1N1 pandemic-origin internal genes in pigs in China. J Virol 88:10864–10874. 10.1128/JVI.01327-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang H, Chen Y, Qiao C, He X, Zhou H, Sun Y, Yin H, Meng S, Liu L, Zhang Q, Kong H, Gu C, Li C, Bu Z, Kawaoka Y, Chen H. 2016. Prevalence, genetics, and transmissibility in ferrets of Eurasian avian-like H1N1 swine influenza viruses. Proc Natl Acad Sci USA 113:392–397. 10.1073/pnas.1522643113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He P, Wang G, Mo Y, Yu Q, Xiao X, Yang W, Zhao W, Guo X, Chen Q, He J, Liang M, Zhu J, Ding Y, Wei Z, Ouyang K, Liu F, Jian H, Huang W, García-Sastre A, Chen Y. 2018. Novel triple-reassortant influenza viruses in pigs, Guangxi, China. Emerg Microbes Infect 7:85. 10.1038/s41426-018-0088-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun H, Xiao Y, Liu J, Wang D, Li F, Wang C, Li C, Zhu J, Song J, Sun H, Jiang Z, Liu L, Zhang X, Wei K, Hou D, Pu J, Sun Y, Tong Q, Bi Y, Chang K, Liu S, Gao GF, Liu J. 2020. Prevalent Eurasian avian-like H1N1 swine influenza virus with 2009 pandemic viral genes facilitating human infection. Proc Natl Acad Sci USA 117:17204–17210. 10.1073/pnas.1921186117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu C, Xu B, Wu Y, Yang S, Jia Y, Liang W, Yang D, He L, Zhu W, Chen Y, Yang H, Yu B, Wang D, Qiao C. 2020. A single amino acid at position 431 of the PB2 protein determines the virulence of H1N1 swine influenza viruses in mice. J Virol 94:e1930-19. 10.1128/JVI.01930-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Jong JC, Paccaud MF, de Ronde-Verloop FM, Huffels NH, Verwei C, Weijers TF, Bangma PJ, van Kregten E, Kerckhaert JAM, Wicki F, Wunderli W. 1988. Isolation of swine-like influenza A(H1N1) viruses from man in Switzerland and the Netherlands. Ann Inst Pasteur Virol 139:429–437. 10.1016/s0769-2617(88)80078-9. [DOI] [PubMed] [Google Scholar]
- 15.Yang H, Qiao C, Tang X, Chen Y, Xin X, Chen H. 2012. Human infection from avian-like influenza A (H1N1) viruses in pigs, China. Emerg Infect Dis 18:1144–1146. 10.3201/eid1807.120009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang DY, Qi SX, Li XY, Guo JF, Tan MJ, Han GY, Liu YF, Lan Y, Yang L, Huang WJ, Cheng YH, Zhao X, Bai T, Wang Z, Wei HJ, Xiao N, Shu YL. 2013. Human infection with Eurasian avian-like influenza A(H1N1) virus, China. Emerg Infect Dis 19:1709–1711. 10.3201/eid1910.130420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhu W, Zhang H, Xiang X, Zhong L, Yang L, Guo J, Xie Y, Li F, Deng Z, Feng H, Huang Y, Hu S, Xu X, Zou X, Li X, Bai T, Chen Y, Li Z, Li J, Shu Y. 2016. Reassortant Eurasian avian-like influenza A(H1N1) virus from a severely ill child, Hunan Province, China, 2015. Emerg Infect Dis 22:1930–1936. 10.3201/eid2211.160181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li X, Guo L, Liu C, Cheng Y, Kong M, Yang L, Zhuang Z, Liu J, Zou M, Dong X, Su X, Gu Q. 2019. Human infection with a novel reassortant Eurasian-avian lineage swine H1N1 virus in northern China. Emerg Microbes Infect 8:1535–1545. 10.1080/22221751.2019.1679611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parys A, Vandoorn E, King J, Graaf A, Pohlmann A, Beer M, Harder T, Van Reeth K. 2021. Human infection with Eurasian avian-like swine influenza A(H1N1) virus, the Netherlands, September 2019. Emerg Infect Dis 27:939–943. 10.3201/eid2703.201863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johansson BE, Bucher DJ, Kilbourne ED. 1989. Purified influenza virus hemagglutinin and neuraminidase are equivalent in stimulation of antibody response but induce contrasting types of immunity to infection. J Virol 63:1239–1246. 10.1128/JVI.63.3.1239-1246.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Couceiro JN, Paulson JC, Baum LG. 1993. Influenza virus strains selectively recognize sialyloligosaccharides on human respiratory epithelium; the role of the host cell in selection of hemagglutinin receptor specificity. Virus Res 29:155–165. 10.1016/0168-1702(93)90056-s. [DOI] [PubMed] [Google Scholar]
- 22.Johansson BE, Kilbourne ED. 1993. Dissociation of influenza virus hemagglutinin and neuraminidase eliminates their intravirionic antigenic competition. J Virol 67:5721–5723. 10.1128/JVI.67.10.5721-5723.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Webster RG, Laver WG, Air GM, Schild GC. 1982. Molecular mechanisms of variation in influenza viruses. Nature 296:115–121. 10.1038/296115a0. [DOI] [PubMed] [Google Scholar]
- 24.Wilson IA, Cox NJ. 1990. Structural basis of immune recognition of influenza virus hemagglutinin. Annu Rev Immunol 8:737–771. 10.1146/annurev.iy.08.040190.003513. [DOI] [PubMed] [Google Scholar]
- 25.Nelson MI, Holmes EC. 2007. The evolution of epidemic influenza. Nat Rev Genet 8:196–205. 10.1038/nrg2053. [DOI] [PubMed] [Google Scholar]
- 26.Caton AJ, Brownlee GG, Yewdell JW, Gerhard W. 1982. The antigenic structure of the influenza virus A/PR/8/34 hemagglutinin (H1 subtype). Cell 31:417–427. 10.1016/0092-8674(82)90135-0. [DOI] [PubMed] [Google Scholar]
- 27.Matsuzaki Y, Sugawara K, Nakauchi M, Takahashi Y, Onodera T, Tsunetsugu-Yokota Y, Matsumura T, Ato M, Kobayashi K, Shimotai Y, Mizuta K, Hongo S, Tashiro M, Nobusawa E. 2014. Epitope mapping of the hemagglutinin molecule of A/(H1N1)pdm09 influenza virus by using monoclonal antibody escape mutants. J Virol 88:12364–12373. 10.1128/JVI.01381-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liang W-H, Jia Y-H, Zhi X-C, Wu Y-P, Chen Y, Yang H-L, Qiao C-L, Chen H-L. 2018. Preparation and antiviral activity of two neutralizing monoclonal antibodies against HA protein of H1N1 swine influenza virus. Acta Vet Zootech Sin 49:1460–1466. [Google Scholar]
- 29.Gu C, Zeng X, Song Y, Li Y, Liu L, Kawaoka Y, Zhao D, Chen H. 2019. Glycosylation and an amino acid insertion in the head of hemagglutinin independently affect the antigenic properties of H5N1 avian influenza viruses. Sci China Life Sci 62:76–83. 10.1007/s11427-018-9439-0. [DOI] [PubMed] [Google Scholar]
- 30.Xie X, Hao F, Wang H, Pang M, Gan Y, Liu B, Zhang L, Wei Y, Chen R, Zhang Z, Bao W, Bai Y, Shao G, Xiong Q, Feng Z. 2022. Construction of a telomerase-immortalized porcine tracheal epithelial cell model for swine-origin mycoplasma infection. J Integr Agric 21:504–520. 10.1016/S2095-3119(21)63644-4. [DOI] [Google Scholar]
- 31.Lewis NS, Daly JM, Russell CA, Horton DL, Skepner E, Bryant NA, Burke DF, Rash AS, Wood JLN, Chambers TM, Fouchier RAM, Mumford JA, Elton DM, Smith DJ. 2011. Antigenic and genetic evolution of equine influenza A (H3N8) virus from 1968 to 2007. J Virol 85:12742–12749. 10.1128/JVI.05319-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koel BF, Burke DF, Bestebroer TM, van der Vliet S, Zondag GCM, Vervaet G, Skepner E, Lewis NS, Spronken MIJ, Russell CA, Eropkin MY, Hurt AC, Barr IG, de Jong JC, Rimmelzwaan GF, Osterhaus ADME, Fouchier RAM, Smith DJ. 2013. Substitutions near the receptor binding site determine major antigenic change during influenza virus evolution. Science 342:976–979. 10.1126/science.1244730. [DOI] [PubMed] [Google Scholar]
- 33.Koel BF, van der Vliet S, Burke DF, Bestebroer TM, Bharoto EE, Yasa IWW, Herliana I, Laksono BM, Xu K, Skepner E, Russell CA, Rimmelzwaan GF, Perez DR, Osterhaus ADME, Smith DJ, Prajitno TY, Fouchier RAM. 2014. Antigenic variation of clade 2.1 H5N1 virus is determined by a few amino acid substitutions immediately adjacent to the receptor binding site. mBio 5:e01070-14. 10.1128/mBio.01070-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li C, Hatta M, Burke DF, Ping J, Zhang Y, Ozawa M, Taft AS, Das SC, Hanson AP, Song J, Imai M, Wilker PR, Watanabe T, Watanabe S, Ito M, Iwatsuki-Horimoto K, Russell CA, James SL, Skepner E, Maher EA, Neumann G, Klimov AI, Kelso A, McCauley J, Wang D, Shu Y, Odagiri T, Tashiro M, Xu X, Wentworth DE, Katz JM, Cox NJ, Smith DJ, Kawaoka Y. 2016. Selection of antigenically advanced variants of seasonal influenza viruses. Nat Microbiol 1:16058. 10.1038/nmicrobiol.2016.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hensley SE, Das SR, Bailey AL, Schmidt LM, Hickman HD, Jayaraman A, Viswanathan K, Raman R, Sasisekharan R, Bennink JR, Yewdell JW. 2009. Hemagglutinin receptor binding avidity drives influenza A virus antigenic drift. Science 326:734–736. 10.1126/science.1178258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Y, Bostick DL, Sullivan CB, Myers JL, Griesemer SB, Stgeorge K, Plotkin JB, Hensley SE. 2013. Single hemagglutinin mutations that alter both antigenicity and receptor binding avidity influence influenza virus antigenic clustering. J Virol 87:9904–9910. 10.1128/JVI.01023-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Myers JL, Wetzel KS, Linderman SL, Li Y, Sullivan CB, Hensley SE. 2013. Compensatory hemagglutinin mutations alter antigenic properties of influenza viruses. J Virol 87:11168–11172. 10.1128/JVI.01414-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Daniels PS, Jeffries S, Yates P, Schild GC, Rogers GN, Paulson JC, Wharton SA, Douglas AR, Skehel JJ, Wiley DC. 1987. The receptor-binding and membrane-fusion properties of influenza virus variants selected using anti-haemagglutinin monoclonal antibodies. EMBO J 6:1459–1465. 10.1002/j.1460-2075.1987.tb02387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fleury D, Wharton SA, Skehel JJ, Knossow M, Bizebard T. 1998. Antigen distortion allows influenza virus to escape neutralization. Nat Struct Biol 5:119–123. 10.1038/nsb0298-119. [DOI] [PubMed] [Google Scholar]
- 40.Vachieri SG, Xiong X, Collins PJ, Walker PA, Martin SR, Haire LF, Zhang Y, McCauley JW, Gamblin SJ, Skehel JJ. 2014. Receptor binding by H10 influenza viruses. Nature 511:475–477. 10.1038/nature13443. [DOI] [PubMed] [Google Scholar]
- 41.Glaser L, Stevens J, Zamarin D, Wilson IA, Garcia-Sastre A, Tumpey TM, Basler CF, Taubenberger JK, Palese P. 2005. A single amino acid substitution in 1918 influenza virus hemagglutinin changes receptor binding specificity. J Virol 79:11533–11536. 10.1128/JVI.79.17.11533-11536.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solorzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, Garcia-Sastre A. 2007. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science 315:655–659. 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 43.Ayora-Talavera G, Cetina-Montejo L, Matos-Patrón A, Romero-Beltrán L. 2014. Hemagglutinin variants of influenza A(H1N1)pdm09 virus with reduced affinity for sialic acid receptors. Arch Virol 159:1207–1211. 10.1007/s00705-013-1934-x. [DOI] [PubMed] [Google Scholar]
- 44.Teng Q, Xu D, Shen W, Liu Q, Rong G, Li X, Yan L, Yang J, Chen H, Yu H, Ma W, Li Z. 2016. A single mutation at position 190 in hemagglutinin enhances binding affinity for human type sialic acid receptor and replication of H9N2 avian influenza virus in mice. J Virol 90:9806–9825. 10.1128/JVI.01141-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rudneva I, Ignatieva A, Timofeeva T, Shilov A, Kushch A, Masalova O, Klimova R, Bovin N, Mochalova L, Kaverin N. 2012. Escape mutants of pandemic influenza A/H1N1 2009 virus: variations in antigenic specificity and receptor affinity of the hemagglutinin. Virus Res 166:61–67. 10.1016/j.virusres.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 46.Wang W, Lu B, Zhou H, Suguitan JAL, Cheng X, Subbarao K, Kemble G, Jin H. 2010. Glycosylation at 158N of the hemagglutinin protein and receptor binding specificity synergistically affect the antigenicity and immunogenicity of a live attenuated H5N1 A/Vietnam/1203/2004 vaccine virus in ferrets. J Virol 84:6570–6577. 10.1128/JVI.00221-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yin X, Deng G, Zeng X, Cui P, Hou Y, Liu Y, Fang J, Pan S, Wang D, Chen X, Zhang Y, Wang X, Tian G, Li Y, Chen Y, Liu L, Suzuki Y, Guan Y, Li C, Shi J, Chen H. 2021. Genetic and biological properties of H7N9 avian influenza viruses detected after application of the H7N9 poultry vaccine in China. PLoS Pathog 17:e1009561. 10.1371/journal.ppat.1009561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang Z, Chen Y, Chen H, Meng F, Tao S, Ma S, Qiao C, Chen H, Yang H. 2021. A single amino acid at position 158 in haemagglutinin affects the antigenic property of Eurasian avian-like H1N1 swine influenza viruses. Transbound Emerg Dis 69:e236–e243. 10.1111/tbed.14288. [DOI] [PubMed] [Google Scholar]
- 49.Peacock TP, Harvey WT, Sadeyen J-R, Reeve R, Iqbal M. 2018. The molecular basis of antigenic variation among A(H9N2) avian influenza viruses. Emerg Microbes Infect 7:176. 10.1038/s41426-018-0178-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu Y, Childs RA, Matrosovich T, Wharton S, Palma AS, Chai W, Daniels R, Gregory V, Uhlendorff J, Kiso M, Klenk H, Hay A, Feizi T, Matrosovich M. 2010. Altered receptor specificity and cell tropism of D222G hemagglutinin mutants isolated from fatal cases of pandemic A(H1N1) 2009 influenza virus. J Virol 84:12069–12074. 10.1128/JVI.01639-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Koel BF, Mögling R, Chutinimitkul S, Fraaij PL, Burke DF, van der Vliet S, de Wit E, Bestebroer TM, Rimmelzwaan GF, Osterhaus ADME, Smith DJ, Fouchier RAM, de Graaf M. 2015. Identification of amino acid substitutions supporting antigenic change of influenza A(H1N1)pdm09 viruses. J Virol 89:3763–3775. 10.1128/JVI.02962-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reed L, Muench H. 1938. A simple method of estimating fifty per cent endpoints. Am J Hyg 27:493–497. 10.1093/oxfordjournals.aje.a118408. [DOI] [Google Scholar]
- 53.WHO Global Influenza Surveillance Network. 2011. Manual for the laboratory diagnosis and virological surveillance of influenza. World Health Organization, Geneva, Switzerland. http://apps.who.int/iris/bitstream/handle/10665/44518/9789241548090_eng.pdf. [Google Scholar]
- 54.Liang L, Deng G, Shi J, Wang S, Zhang Q, Kong H, Gu C, Guan Y, Suzuki Y, Li Y, Jiang Y, Tian G, Liu L, Li C, Chen H. 2016. Genetics, receptor binding, replication, and mammalian transmission of H4 avian influenza viruses isolated from live poultry markets in China. J Virol 90:1455–1469. 10.1128/JVI.02692-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ministry of Science and Technology of China . 2021. Guide for the care and use of laboratory animals of the Ministry of Science and Technology of China, 4th ed. Central People’s Government of the People’s Republic of China, Beijing. http://www.gov.cn/zhengce/2020-12/25/content_5574003.html. Accessed May 20, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The HA genes of the escape mutants were sequenced and have been deposited in GenBank under the accession numbers ON479265 and ON479266.