Abstract
Fungal compounds have long been used for centuries as food supplements. β-glucans have been identified as the most interesting molecules with beneficial effects in several chronic diseases. In vitro studies have shown that they are able to elicit the immune cells maturation and activation with the result of an increased release of proinflammatory cytokines and chemokines and a stimulation of anti-bacterial activity of macrophages and neutrophils. As β-glucans enhance pathogen elimination through non-self antigens identification, they can also direct immune response against tumor cells. These compounds also stimulate the activity on adaptive immune cells and they have been regarded as biological response modifiers. In this way, β-glucans can be exploited as adjuvant cancer therapy, in particular by a synergic action with chemotherapy or immunotherapy. In the immuno-oncology era, the need is to identify innovative drugs that can simultaneously target and inhibit different biological processes relevant for cancer cells survivors. Recent clinical studies showed promising results about the combination of β-glucans and immune checkpoint inhibitors for patients affected by different solid tumors. This review aims to investigate molecular mechanisms of action of β-glucans and is focused on their application in clinical practice as immune-adjuvants for treatment of cancer patients.
Keywords: β-glucans, mushrooms, immuno-oncology, immune-modulating, immune checkpoint inhibitors
Introduction
Mushrooms have been utilized as food supplements for several centuries and their therapeutic properties on human health have long been studied.
β-D-glucans are polysaccharides found as cell wall components with structural function and are extracted from different species of yeast, mushroom, bacteria and barley. β-glucans extracted from oat or barley have to be distinguished from ones extracted from fungal cell components, because they have different molecular structure and play distinct roles in regulation of human metabolism [1].
There are numerous pharmaceutical products based on these polysaccharides, such as schizophyllan, lentinan, grifolan, polysaccharide-peptide (PSP) complex and polysaccharide-protein (PSK) complex [2].
These compounds are known to have an immune-modulating action capable of stimulating the immune system’s response by activation of macrophages, phagocytosis of the pathogen and release of proinflammatory cytokines [3]. They positively influence the homeostasis of the organism, particularly modifying the intestinal microbiota [4–7].
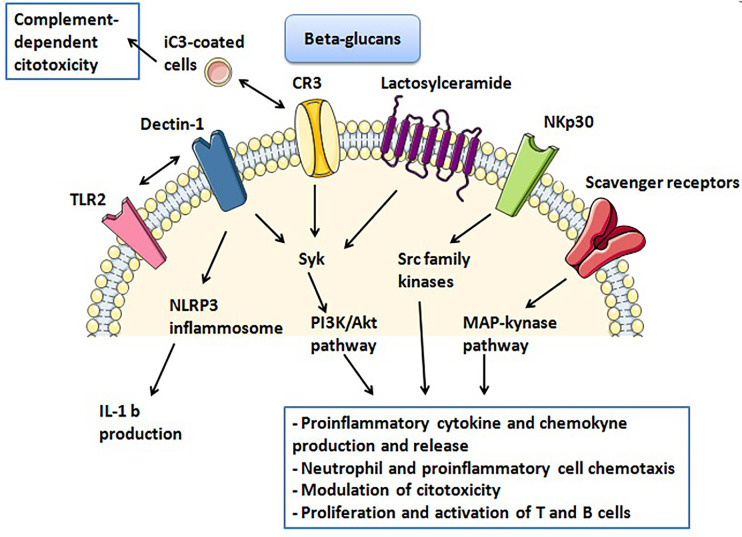
Glucan receptors are expressed on macrophages, natural killer (NK) cells and neutrophils [8]. Among these dectin-1, complement receptor 3 (CR3), lactosylceramide (LacCer), natural cytotoxicity receptor p30 (NKp30) and scavenger receptors are the most studied ones [9]. β-glucans have a distinct affinity with these receptors according to the different chemical structure and are therefore capable of triggering different host responses [10].
This immune-stimulating capacity of β-glucans makes wide and varied medical use. The ability to modulate humoral and cellular immunity can be exploited, for example, in the treatment of various chronic inflammatory diseases.
β-glucans are able to reduce the level of total serum cholesterol and glucose, in addition to acting on the control of body weight [11]. The mechanism that rules the cholesterol-lowering effects of β-glucans takes place through the gut microbiota and the production of short-chain fatty acids (SCFAs, for example propionate). The gut microbiota degrades the fibers from which SCFAs are obtained; the increase of them at the expense of the acetic acid (main substrate for cholesterol biosynthesis) results in decrease in cholesterol biosynthesis [12]. Recent studies suggested that β-glucans control circulating lipid levels by excretion of fecal lipids and by regulation of the activity of hydroxy-3-methyl-glutartyl-coenzyme A reductase [13].
The β-glucans are able to attenuate blood postprandial glycemic and insulin peak forming a barrier in the small intestine which prevents glucose absorption. Moreover, the latest evidence points to a role in activating metabolic pathways through phosphatidylinositol 3-kinase (PI3K)/serine-threonine kinase (Akt), which have a key role in the pathogenesis of diabetes [14]. Furthermore the enrichment of food with β-glucan is required in order to produce low glycemic index meals suitable for diabetic subjects [15, 16].
In this way, β-glucans have a potentially beneficial activity in the prevention and treatment of diabetes mellitus, hypercholesterolemia and associated cardiovascular diseases [14, 17].
β-glucans have been studied as potential adjuvant agents in treatment of gastrointestinal, hepatic and respiratory infections, caused by bacterial, viral and fungal microorganisms.
β-glucans have been also studied as modulators of human immunodeficency virus (HIV)-associated immune dysfunction. In fact, they are involved in regulation of gut barrier permeability [18] and might be responsible for microbial translocation from the gastrointestinal tract into systemic circulation. It has been supposed an interesting role of β-glucans in the pathogenesis of non-acquired immunodeficiency syndrome (non-AIDS) events, but further studies are needed to explore their contribution in HIV infection and course [19–21].
In Eastern world, mushrooms are widely used as medical and nutritional support in cancer patients, in order to improve fatigue and cachexia and to increase tolerability to chemotherapy. In fact, numerous animal and human studies have shown remarkable activity against a wide variety of tumors [22, 23]. In the oncological field, β-glucans can stimulate the innate and adaptive immune response, inhibit the proliferation of cancer cells, promote apoptosis and block the angiogenesis [24–26].
The advantages of β-glucan derive from its non-toxicity and a non-immunogenicity due to its absence of proteins and peptide components; in this way the β-glucans have a specific modulatory activity of the immune system as they bind specific receptors [27].
The purpose of this review is to deepen the molecular mechanism of β-glucan and in particular its role as immune-modulator, the potential association with immunotherapy and future therapeutic applications.
Benefit from β-glucans in cancer patients
As we know, the immune system is classified into adaptive and innate [28]. The first is represented by a rapid line of defense against pathogens while the adaptive system develops a long-lasting response that protects the organism from subsequent encounters with the same pathogen and therefore plays a fundamental role in the protection against infections and in the efficacy of vaccines [29–31]. One of the mechanisms that stimulate the induction of trained immunity is epigenetic reprogramming: after stimulation with certain ligands such as β-glucan or Bacille Calmette-Guerin (BCG), the immune cells undergo a functional reprogramming which involves an increase of their reactivity to the next stimulation [32]. The control and surveillance of tumors involves an intricate dance between the adaptive and innate immune system.
It has been demonstrated that the association of β-glucans with chemotherapy is able to enhance cytotoxicity and can improve patient clinical outcome. The use of medical mushroom extracts has been studied in association with chemotherapy in different kinds of cancers, such as estrogen receptor negative human breast cancer, gastric and colorectal cancer, non-small-cell lung cancer (NSCLC) and hematologic diseases [33–36].
The advent of immunotherapy has dramatically changed cancer treatment. In particular, the use of immune checkpoint inhibitors (ICIs) has had great success in the treatment of numerous types of malignancies and their use in clinical practice is progressively increasing. The response to immunotherapy is variable often due to a different involvement of the tumor microenvironment (TME). To modify TME with increasing the presentation of antigens by the tumor mass and thus stimulating the response of the immune cells towards the tumor cells is, currently, under investigation [27].
In this regard, β-glucan molecules are a potential immune-modulator that acts on the innate and adaptive immune response within TME. B-glucan could have an adjuvant role in stimulating and improve clinical response to ICIs [37].
Molecular composition and modulation of immune cells
β-glucans are polysaccharides composed of D-glucose monomers linked together by 1→3 linear β-glycosidic bonds. The glycosidic chain core has 1→6 side branches that are specific of fungi-derived glucans [38]. In some subgroups of fungi, the polysaccharide chain may also be bound with protein or peptides, by forming PSK or PCP complexes [39].
β-glucans has been deeply studied as biological response modifiers (BRMs) [40]: they interact directly with receptors located on plasmatic membrane of immune cells and are able to elicit an effective inflammatory and immune response against non-self antigens expressed by pathogens but also on tumor cells [41].
The immune-modulatory properties of β-D-glucans have been widely investigated and it has been supposed that they exert an antitumor activity, by enhancing immune system against tumor cells and by inhibiting tumor invasion and progression through a complex modulation of mechanisms of apoptosis and angiogenesis [42].
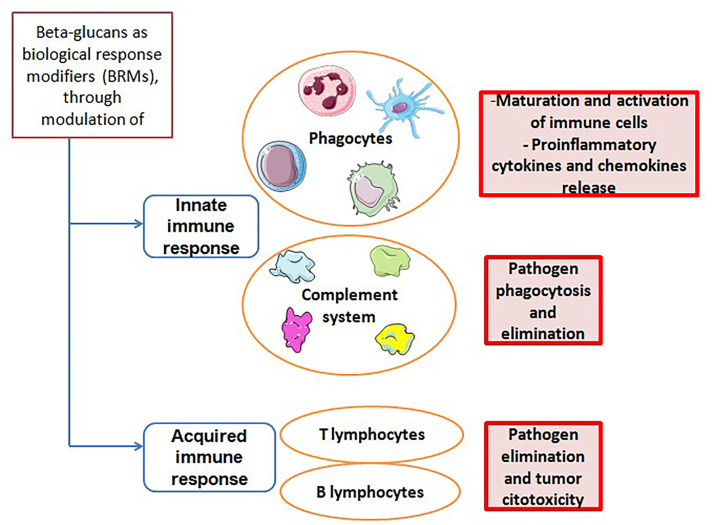
Several preclinical and clinical studies have shown that β-D-glucans are able to modulate the responsiveness and the interaction between innate and adaptive immune systems [43] (Figure 1). They can enhance antimicrobial activity of macrophages, monocytes and neutrophils, leading to maturation of these target cells and to an increased proinflammatory cytokine and chemokine release. This reflects in a stimulation of adaptive immune cells, including CD4+ T cells, CD8+ cytotoxic T lymphocytes (CTL) and B cells. Specifically, the tumoricidal mechanisms carried out by T cells and induced by β-glucans can be summarized in this way. The β-glucan binds specific receptors (for example, Dectin-1 which will be discussed below) expressed on myeloid cells, which are converted into antigen presenting cells (APCs). The binding activates the CD4+ and CD8+ T cells which in turn will produce pro-inflammatory cytokines [respectively tumor necrosis factor (TNF)-α, anti-tumor cytokine interferon-gamma (IFN-γ), Granzyme B, and perforins], leading to the destruction of cancer cells [44]. Similarly β-glucan induces switching of suppressive M2 macrophages into inflammatory M1 macrophages which in turn will activate Th1-type T cells, causing damage to cancer cells through the secretion of pro-inflammatory cytokines by T cells [45]. On the other hand, the link between β-glucan and polymorphonuclear cell will cause cell apoptosis with the release of ROS in the microenvironment leading to the death of tumor cells from oxidative stress [46]. Besides, β-D-glucans are also modulators of NK cells cytotoxicity. These compounds are able to stimulate activation of NK cells against tumor cells, both by production and release of pro-inflammatory cytokines and by complement activation [47]. In this context, it has been shown that β-glucans can induce granulopoietic progenitors and, in general, innate immune cells towards a tumor-suppressive phenotype [48].
Figure 1.
Interaction pathways between β-glucans and the immune system
In this way, it has been hypothesized that β-D-glucans may play an important role as immune-modulator agents and can be used as a synergic treatment in combination with ICIs.
Receptors of β-glucan
The interaction between β-glucans and their receptors on human cells is likely to be very complex and only partially known. The main receptors that are involved in inflammatory and immune-response are Dectin-1, CR3, LacCer, NKp30 and scavenger receptors [9].
Dectin-1
Dectin-1 is a type II transmembrane pattern-recognition receptor with an extracellular C-type lectin-like domain fold and a cytoplasmic domain that contains an immunoreceptor tyrosine-based activation motif (ITAM) [10, 49]. After binding of β-glucans, it can mediate the non-opsonic phagocytosis of opportunistic pathogens and it is responsible of cytokine release [50]. In fact, Dectin-1 induces phosphorylation of its ITAM and spleen tyrosine kinase (Syk) and activates an intracellular PI3K/Akt pathway. Thus, the result is an increased production and release of various inflammatory cytokines, such as TNF, CXC-chemokine ligand 2 (CXCCL2), Interleukin-2 (IL-2), IL-10 and IL-12. Dectin-1 can also collaborates with Toll-like receptors (TLRs) expressed on the same cell, in order to enhance cytokine production, such as TNF-α, IL-6, IL-10 and IL-23, and down-regulate release of IL-12 [51].
Furthermore, Dectin-1 associated intracellular signaling also involves cytoplasmic Nod-like receptor protein 3 (NLRP3) inflammasome, which activation seems to be essential for IL-1b production and secretion [52]. In human cells, Dectin-1 has another binding site that can recognize an endogenous ligand on T cells: in this sense, Dectin-1 has been proposed to act as a T cell co-stimulatory molecule [53].
CR3
CR3, also known as macrophage 1 antigen (Mac-1), belongs to the family of β2 integrins and is an heterodimeric glycoprotein composed of two non-covalently associated chains (CD18 and CD11b), found on immune cells such as neutrophils, macrophages, lymphocytes and NK cells [54]. Its lectin-like domain is responsible for binding to β-glucans and this binding primes leukocytes for cytotoxicity and phagocytosis of target cells, through a Syk-PI3K molecular pathway. In fact, CR3 has a second ligand able to recognize iC3b-coated tumor cells and its activation for complement-dependent cytotoxicity and then tumor cell lysis requires its dual binding to iC3b and β-glucan [55, 56].
LacCer
LacCer is the most abundant neutral glycosphingolipid and it is expressed on various human cells, among these on neutrophils. LacCer forms lipid rafts on plasmatic membrane of neutrophils and, after binding with β-glucans, it activates a signal transduction pathway involving Src family kinase/PI3K. The result is neutrophil chemotaxis [57, 58] and enhanced cytokine release [59, 60]. Furthermore, it has been demonstrated that CR3 and LacCer was partially co-localized on lipid rafts of plasma membrane of neutrophils and some preclinical data suggest that LacCer-mediated phagocytosis may be dependent on CR3, suggesting a co-stimulatory activity of these two β-glucans receptors [61].
NKp30
NKp30 belongs to immunoglobulin-like transmembrane receptor family and it was needed to bind 1-3 β-glucan by NK cells. It has been demonstrated that this receptor can activate Src family kinases and mediate granule polarization and perforin release in NK cells. In this sense, NKp30 has been recognized as a pattern-recognition receptor, whose stimulation enhances NK cell killing of fungi, such as Cryptococcus neoformans and Candida albicans [62].
Scavenger receptors
It has been demonstrated that fungal β-glucans can also bind to other membrane receptors, such as scavenger receptors. β-glucans can interact with the CD5 ectodomain, present on plasmatic membranes of T and B cells and can induce mitogen-activated protein (MAP) kinase activation and cytokine release [63].
Preclinical studies
Several β-glucans extracted from different species of fungi have been investigated as BRMs and the most relevant ones are described in Table 1.
Table 1.
Biological activity of most relevant β-glucans investigated in pre-clinical studies
| Pre-clinical study (ref.) | Treatment models | β-glucans/fungus | Biological activity |
|---|---|---|---|
| Sorimachi K, et al., [64] Niu YC, et al., [65] |
Animal model (rat bone marrow) Animal model (mouse S180 cells), IV administration |
Glucan/Agaricus blazei Murill | - ↑ secretion of IL-8 and TNF-α by macrophages - ↑ production of IL-23, IL-12, IL-1 - ↑ cytokine and leukocyte growth factor production |
| Kubala L, et al., [66] Zhong K, et al., [67] |
Human model Mice splenic Lymphocytes |
Schizophyllan/Schizophyllum commune | - ↑ lymphocytes proliferation, through production of IL-2 - ↑ production of pro-inflammatory cytokines IL-6, IL-8, and TNF-alpha |
| Yang A, et al., [68] | Murine macrophages Human hepatoma HepG2 cells |
TPG-1/Trametes robiniophila | - ↑ production of TNF-α and IL-6 through toll-like receptor 4 (TLR4) |
| Wang J, et al., [69] Wang SY, et al., [70] Chien CM, et al., [71] |
Animal model, in vitro, Raw 264.7 cells Human myeloid leukemia cell lines Human umbilical cord blood |
Proteoglycan fraction/Ganoderma lucidum | - ↑ anti-inflammation activity against lipopolysaccharide (LPS) stimulation - ↑ T cells activity - ↑ expression of IL-1, IL-2, IL-6, TNF-α and INF-γ - modulate NK cell cytotoxicity |
| Carmona EM, et al., [72] Ali MF, et al., [73] |
Rat cells Human model |
Glucan/Pneumocystis and Aspergillus | - ↑ TNF-α, IL-6 and IL-8 production by B-lymphocytes - ↑ IL-23 and IL-6 release by dendritic cells - ↑ secretion of IL-17 and IL-22, both Th17-produced cytokines |
| Kankkunen P, et al., [52] Ding J, et al., [74] Vetvicka V, et al., [47] |
Human macrophages Human monocyte-derived DCs Murine melanoma B16 cell line |
Glucan/Saccharomyces cerevisiae | - ↑ Th2 immune response and inhibits Th1 by promoting the release of anti-inflammatory cytokines such as IL-10 and transforming growth factor (TGF-β) - ↑ IL-1β transcription and secretion - ↑ IL12, IL-2, TNF, IFN production - ↑ tumor-specific CTL activity - modulate NK cells activity and killing towards tumor cells |
| Ina K, et al., [75] | Human model (gastric cancer patients), IV administration | Lentinan/Lentinula edodes | - ↑ PD-L1 tumor expression - ↑ release of TNF-α, IL-12 and IFN-γ - ↑ T cells activity, especially CD8+ cells and Th1 polarization |
| Masuda Y, et al., [76] Masuda Y, et al., [77] |
Animal model Animal model |
Maitake α-glucan (YM-2A)/Grifola frondosa | - ↑ activation of dendritic cells and macrophages - ↑ IFN-γ production by CD4+ and CD8+ T cells |
| Bose N, et al., [78] | Human serum | Imprime PGG/Saccharomyces cerevisiae | - ↑ phenotypic and functional activation of monocytes - ↑ activation of neutrophils, through production of IL-8, CCL2, and CD11b |
We focused on BTH-1677 (Imprime-PGG) because it is one of the most studied β-glucans in combination with ICIs.
BTH-1677 is a water-soluble and intravenous formulation of yeast-derived β-glucan purified from the cell wall of Saccharomyces cerevisiae. It is recognized as a fungal pathogen-associated molecular pattern (PAMP) and it is able to trigger a complex and coordinated immune response that involves both innate and adaptive immune cells. Its mechanisms of action as immune-modulator and anti-tumoral agent has been deeply investigated in preclinical and clinical studies.
Bose et al. [78] demonstrated that BTH-1677 interacts with human-isolated neutrophils and monocytes through a CR3 and complement-dependent manner. This result has been also confirmed in a mice model [79].
As shown in preclinical studies [80], when BTH-1677 enters the blood, it is bound by endogenous plasma anti-β-glucan antibodies (ABAs) and it constitutes a tripartite immune complex, by attracting the opsonization by complement protein iC3b. This macro-complex interacts with CR3 and FCγ receptor II (CD32a) located on neutrophils, macrophages and monocytes, and stimulates inflammatory cytokine production and release. It results in activation of innate immune response and enables direct killing of antibody-targeted tumor cells, through a mechanism of antibody-dependent cellular phagocytosis [81, 82]. Dectin-1 binds directly BTH-1677 and other fungal compounds, but it has been suggested that the tripartite immune complex described above could also signal through Dectin-1, by interacting simultaneously with CR3 [81]. These innate immune functions are detected only in the presence of sufficient ABA in serum. It suggests that ABA levels may be a biomarker to select patients who have benefit to administration of β-glucans and that the exogenous supplementation of ABA could apport a rehabilitation of these functions [83, 84].
BTH-1677 can affect macrophage differentiation toward M1 phenotype respect than the suppressive M2 state [85, 86] and inhibits activation of myeloid derived suppressor cells (MDSC) against T cell proliferation [87]. Chan et al. [86] demonstrated that BTH-1677 can modulate in vitro activity of monocyte-derived dendritic cells (MoDCs), by eliciting an increased surface expression of the maturation and co-stimulatory markers, such as CD80, CD83, CD86 as well as HLA-DR. It leads to an increased production of anti-tumor cytokine IFN-γ and surface expression of antigen presentation markers. Furthermore, among biological effects induced by BTH-1677, it seems to be that it up-regulates programmed death-ligand 1 (PD-L1) expression on macrophages surface and also on tumor cells [88].
The activity on innate immunity is also expressed on NK cells: BTH-1677 enhances NK cell functionality and killing, which are dependent on IFN-γ and Dectin-1 and represent the main antibody-dependent cellular cytotoxicity against tumor cells [89].
Besides, BTH-1677 can inhibit the suppressive activity of Tregs on CD4+ T cells and is able, when treated with whole blood, to enhance CD4+ and CD8+ T cell proliferation, also by driving T cell polarization towards anti-tumor Th1 phenotype [90, 91].
In order to exploit the immunomodulating effect of BTH-1677, several preclinical studies investigated the combination of this β-glucan with anti-tumor monoclonal antibodies (mAbs) acting on immune response. The aim was to improve the efficacy of ICIs, in particular anti-programmed death receptor-1 (anti-PD-1)/ PD-L1 mAbs, in combination with β-glucans, by inducing PD-L1 tissutal expression and by enhancing a potent and coordinated immune response against tumor cells.
Fraser et al. [92] demonstrated in two distinct mice models (CT-26 and MC-38 model) that the combination of BTH-1677 with anti-PD-1 or anti-PD-L1 agents is able to repress tumor growth, compared to models treated only with BTH-1677 or anti-PD-1/anti-PD-L1.
In another study, Qiu et al. [93] showed that T cells treated ex vivo with anti-PD-1 antibody and co-cultured with BTH-1677 treated macrophages or dendritic cells have an increased proliferation rate. Then, they observed a significantly reduced median tumor volume in a mice model after administration of both BTH-1677 and anti-PD-1 mAbs.
In summary, what emerged is how the monocyte-macrophages cells activated by BTH-1677 in vitro have an higher expression of membrane PD-L1; simultaneously, an increase in the expression of the co-stimulatory molecule CD86 and other cytokines has been documented, which allow further stimulation on the effector action of T cells. Furthermore, the tumor cells themselves, thanks to the activation of a wider, innate and adaptive immune response induced by BTH-1677 show an increased expression of PD-L1.
Another interesting data reported is that BTH-1677 has the ability to turn off the inhibitory effect of PD-L1 upregulation by enhancing the secretion of immunostimulatory cytokines and the expression of costimulatory proteins. These data confirm the idea that BTH-1677 synergizes with ICIs, particularly with anti-PD1 antibodies, and it may represent an effective adjuvant therapy along with approved and widely used immunotherapy agents [94].
In a similar way, Hong et al. [95] have demonstrated the same effect of a combined therapy of β-glucan and anti-tumor mAbs. In this study developed on mice models, the combining administration of β-glucan and mAbs against naturally occurring antigens GD2 ganglioside or recombinant human Mucin1 (MUC1) elicited a significantly greater tumor regression, respect to the mAbs or β-glucan therapy alone. In this study, the expression of CR3 on leukocytes and the binding of iC3b on tumors seem to be crucial for the β-glucan adjuvant effect and granulocytes showed to be responsible for antitumor activity (Figure 2).
Figure 2.
Activation of β-glucan receptors and intracellular pathways. TLR2: toll-like receptor 2
Clinical studies
Considering the promising results described above in the preclinical models, several trials evaluated the interaction of glucans with mAbs in humans (Table 2).
Table 2.
Biological activity of most relevant β-glucans investigated in clinical studies
| Clinical trial (ref.) | Features | Patients | β-glucans/other drugs | Results |
|---|---|---|---|---|
| Halstenson CE, et al., [96] | Phase 1a/b. Single center, randomized, double-bind, placebo-controlled, dose escalation study |
Healthy volunteer subjects | Imprime PGG | Acceptable safety profile, well tolerated |
| NCT03246685 [97] | Phase 2. Multicenter, open-label study |
Advanced Squamous Cell Carcinoma of H&N (SCCHN) patients | Imprime PGG & Pembrolizumab | Terminated for enrollment failure |
| Uhlik M, et al., [98] | Phase 2. Multicenter, open-label study |
44 ABA positive mTNBC patients | Imprime PGG & Pembrolizumab | mTNBC: - Objective response rate (ORR) was 15.9%, with 1 complete response (CR) and 6 partial responses (PR) - 17/44 shown stable diseases (SD) for more than 1 year (best response) and 4/44 for more than 2 years - Overall survival (OS) rate at 1 year was ~ 63%; median OS is 18.1 months by Kaplaian-Meyer estimation (95% CI, 12 months-not reached) |
| Chan A, et al., [99] | Phase 2. Multicenter, open-label study |
40 ABA positive metastatic melanoma patients | Imprime PGG & Pembrolizumab | Melanoma patients: - disease control rate (DCR) was 45% (with 1 CR and 8 SD) - median OS was 8.8 months (with 12 month OS rate equal to 45%) |
| Modak S, et al., [100] | Phase 1. | 24 chemo-resistant NB patients | Oral β-glucan & 3F8 | - Acceptable safety profile, well tolerated - The maximum dose tolerated of β-glucan was not reached - A clinical response was observed in 63% of patients |
| Kushner BH, et al., [101] | Phase 1. | 15 high-risk NB patients in remission | β-glucan & bivalent gangliosides vaccine | Acceptable safety profile, well tolerated |
| NCT03003468 [102] | Phase 1b/2. | mNSCLC patients | Imprime PGG & Pembrolizumab | On going |
| NCT03555149 [103] | Phase 1b/2. Open-label, multicenter, randomized Umbrella study |
mCRC patients (cohort 3) | Imprime PGG & Atezolizumab (cohort 3) | On going |
mCRC: metastatic CRC; mNSCLC: metastatic NSCLC; mTNBC: metastatic triple-negative breast cancer; NB: neuroblastoma
As aforementioned, BTH-1677 is one of most investigated compounds in the field of new frontiers in cancer therapies.
In 2015, Halstenson et al. [96] designed a single center, randomized, double-bind, placebo-controlled, dose escalation study investigating the safety and the tolerability of intravenous injection of BTH-1677 in healthy subjects. In the phase 1a, BTH-1677 was administered to 18 volunteers (≤ 45 years) sequentially randomized to receive the single dose of study drug at 0.5-1-2-4 or 6 mg/kg dose. The control group consisted of 6 people, who received a single dose of placebo. In the phase 1b, 12 subjects were randomized (3:1) to 7 daily i.v. infusion at 1, 2 or 4 mg/kg or placebo respectively. Adverse events (AEs) occurred (headache, dyspnea, paresthesia, nausea, rash and flushing) were mild and moderate, and were described in 67% of the study subjects overall. The appearance of an infusion reaction during the administration of the study product at a dosage of 4 mg/kg resulted in an amendment contemplating a slow administration of the 4 mg/kg and 6 mg/kg doses. In conclusion, the drug was well tolerated after single doses up to 6 mg/kg and after 7 daily doses up to 4 mg/kg.
The benefit of this β-glucan has been evaluated in association with pembrolizumab in various phase II studies in cancer patients. The rationale of the combination with ICIs is based on the hypothesis that glucans may stimulate immune system activation pathways complementary to that triggered by monotherapy with mAbs.
In 2017, a phase II trial aimed to investigate the benefit of this combo in head and neck cancers that failed or experienced stable disease during pembrolizumab monotherapy. Unfortunately, the study has been terminated for enrollment failure [97].
Encouraging data derived from IMPRIME 1, a phase II open-label multicenter trial involving ABA positive mTNBC and metastatic melanoma patients. In the breast cohort, 44 mTNBC pre-treated patients were enrolled to receive Imprime (4 mg/kg i.v. days 1, 8, 15 of each 3-week cycle) plus pembrolizumab 200 mg on day 1 of each cycle [98]. The results presented at San Antonio Breast cancer Symposium in 2019, showed that the primary endpoint, ORR, was 15.9%, with 1 CR and 6 PR. seventeen of 44 patients were stable for more than 1 year (best response) and 4 of 44 for more than 2 years. OS rate detected at 1 year was ~63% and median OS is currently 18.1 months by Kaplaian-Meyer estimation (95% CI, 12 months-not reached) [99]. Moreover, it demonstrates a large activation of both myeloid and T cells with extensive infiltration in tumor tissue samples [98]. These data allow to reacquire a possible role of ICIs in combination with immune-stimulating agents in patients with mTNBC, overcoming the poorer encouraging results of single agent immunotherapy in this setting [104].
In the melanoma subgroup, patients who have failed ICIs therapy undergo the same combined therapeutic regimen. The disease control rate, on 40 patients enrolled, was 45% (with 1 CR and 8 SD) and the median OS was 8.8 months (with 12-month OS rate equal to 45%). As in the breast cancer population, the indirect signs of the improved immune stimulation were observed in tissue samples (biopsy) and in peripheral blood. Therefore, in melanoma patients with disease control this biological finding is linearly correlated with a proportional increase in survival [99].
As previously explained, significant levels of circulating ABA are a sine qua non condition to expect an immune-stimulating β-glucan effect [78, 83].
In this regard, in a case-report it has been supposed that the function of β-glucan can be rehabilitated providing an intravenous supplement of purified ABA or commercial intravenous immunoglobulin G (IVIG) in deficient subjects [105].
This is a case of 84-year-old woman with pre-treated neuroendocrine tumor with baseline ABA levels < 1 μg/mL, who received BTH-1677 (4 mg/kg) in compassionate use, pembrolizumab (200 mg flat dose) and immunoglobulin G (IgG, 500 mg/kg). Immunoglobulins were infused the day before the first cycle of therapy and then on the same day of every subsequent recycle. The treatment was well tolerated, there were no AEs except a worsening of a myalgia in the first cycle. Dose and timing of administration of IVIG (1,000 mg/kg, administered on the same day of treatment, before the infusion of BTH1677 and pembrolizumab) was adapted based on the serum IgG levels detected in the pre-treatment blood samples.
This case-report showed that the minimum amount of IVIG supplement appears to be 1,000 mg/kg, based on the increase in complement activity and cytokine levels. A partial response in radiological evaluation was detected at the second cycle (reduction of 5% of target lesion); at the subsequent control (4th cycle) there was a volume increase of target lesions, no other lesions were detected.
Several phase 1 studies, which aim to investigate the role of β-glucans, have been conducted on young patients with NB, a childhood cancer still orphaned by effective therapeutic strategies. In 2013 twenty-four patients with chemo-resistant NB were enrolled to receive 10 mg/(kg·day) of 3F8 (a mAb directed against the ganglioside GD2, a NB surface antigen) associated in each cycle to an oral β-glucan, dose escalated from 10 to 80 mg/(kg·day). Most patients have a good tolerance of oral β-glucan: there were two cases of severe thrombocytopenia, of which one has not regressed and evolved into chronic. This side effect has never been described in 3F8 and could be linked to glucan mediated CR3 activation. Other AEs reported were fever, pain and urticaria (probably related to 3F8). The maximum dose tolerated of β-glucan was not reached. A clinical response, although not striking and of short duration, was observed in 63% of patients [100].
Kushner et al. [101] conducted a phase 1 study, involving 15 high-risk NB patients in second or later remission who received a combo of an immune-stimulating β-glucan and a vaccine that induced host anti-ganglioside G2/G3 antibodies. The hypothesis is that the stimulation of humoral immunity can maintain the disease remission even among these very high-risk patients. The vaccine/β-glucan treatment was well tolerated with no dose-limiting toxicity; painful local reactions have been reported immediately after the injection but no other early or delayed toxicity has been documented. The serological and minimal residual disease (MRD) responses were encouraging.
Finally, there are two interesting ongoing trials, regarding the association of ICIs and glucan.
(1) The first one (phase Ib-II trial) includes patients with mNSCLC, receiving the combination of pembrolizumab and Imprime PGG in second line. The phase II trial will test whether addition of the glucan to ICIs increases median progression-free survival (PFS) [102].
(2) In Morpheus (phase Ib-II) study, the cohort 3 composed by mCRC patients will be randomized to one of the immunotherapy combination arms, including atezolizumab and Imprime PGG, or the standard-of-care control arm. All patients included in the study are BRAF wild type or without microsatellite instability, in disease progression during or following 2 (but not more) lines of treatment for mCRC, not prior treated with ICIs [103].
Conclusion and future perspective
The new era of drug development has seen integrative therapies as one of the options for numerous diseases. The future of cancer immunotherapy could rely on combination therapies based on ICIs with other adjuvant drugs, such as personalized cancer vaccines and targeted therapies directed to the TME. Bioactive compounds extracted from mushrooms have been shown immuno-modulator activity by stimulating the maturation, differentiation and proliferation of innate and adaptive immune cells. In addition, they are well tolerated and possess a very low risk of significant negative side effects. In this way, β-glucan demonstrate synergic effect with antitumor mAbs agents and they can have an important role to improve the therapeutic effects and the quality of life in cancer patients.
Further studies and clinical investigations are directed to evaluate how mushrooms can be used as complementary/integrative therapy to guide oncology strategies. More research and investigations are necessary to evaluate the route of administration and dosage of β-glucans and their immune effect on bacterial growth and human microbiota.
The future perspective should be also oriented to discovering molecular mechanisms of different fungal compounds, interactions with cancer immunotherapy and future applications in clinical practice.
Abbreviations
- ABAs:
anti-β-glucan antibodies
- AEs:
adverse events
- CR:
complete response
- CR3:
complement receptor 3
- ICIs:
immune checkpoint inhibitors
- IFN-γ:
interferon-gamma
- IgG:
immunoglobulin G
- IVIG:
intravenous immunoglobulin G
- LacCer:
Lactosylceramide
- mAbs:
monoclonal antibodies
- mTNBC:
metastatic triple-negative breast cancer
- NB:
neuroblastoma
- NK:
natural killer
- NKp30:
natural cytotoxicity receptor p30
- NSCLC:
non-small-cell lung cancer
- OS:
overall survival
- PD-L1:
programmed death-ligand 1
- PI3K:
phosphatidylinositol 3-kinase
- PR:
partial responses
- SD:
stable diseases
- TME:
tumor microenvironment
- TNF:
tumor necrosis factor
Declarations
Author contributions
VC, NR and FT contributed to literature research and article’s selection. VC, NR, FT and FM wrote the manuscript and generated the figures and tables. FM and RB contributed to the revisions of the manuscript. All authors approved the published version of the manuscript.
Conflict of interest
All authors declare that there are no conflicts of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent to publication
Not applicable.
Availability of data and materials
Not applicable.
Funding
Not applicable.
Copyright
© The Author(s) 2021.
References
- 1.Hoenigl M, Lin J, Finkelman M, Zhang Y, Karris MY, Letendre SL, et al. Glucan rich nutrition does not increase gut translocation of β-glucan. Mycoses. 2021;64:24–9. 10.1111/myc.13161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ooi VE, Liu F. Immunomodulation and anti-cancer activity of polysaccharide-protein complexes. Curr Med Chem. 2000;7:715–29. 10.2174/0929867003374705 [DOI] [PubMed] [Google Scholar]
- 3.Ren L, Perera C, Hemar Y. Antitumor activity of mushroom polysaccharides: a review. Food Funct. 2012;3:1118–30. 10.1039/c2fo10279j [DOI] [PubMed] [Google Scholar]
- 4.Jaskari J, Kontula P, Siitonen A, Jousimies-Somer H, Mattila-Sandholm T, Poutanen K. Oat β-glucan and xylan hydrolysates as selective substrates for Bifidobacterium and Lactobacillus strains. Appl Environ Microbiol. 1998;49:175–81. 10.1007/s002530051155 [DOI] [PubMed] [Google Scholar]
- 5.Drzikova B, Dongowski G, Gebhardt E. Dietary fibre-rich oat-based products affect serum lipids, microbiota, formation of short-chain fatty acids and steroids in rats. Br J Nutr. 2005;94:1012–25. 10.1079/bjn20051577 [DOI] [PubMed] [Google Scholar]
- 6.Snart J, Bibiloni R, Grayson T, Lay C, Zhang H, Allison GE, et al. Supplementation of the diet with high-viscosity β-glucan results in enrichment for lactobacilli in the rat cecum. Appl Environ Microbiol. 2006;72:1925–31. 10.1128/AEM.72.3.1925-1931.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitsou EK, Turunen K, Anapliotis P, Zisi D, Spiliotis V, Kyriacou A. Impact of a jelly containing short-chain fructo-oligosaccharides and Sideritis euboea extract on human faecal microbiota. Int J Food Microbiol 2009;135:112–7. 10.1016/j.ijfoodmicro.2009.08.004 [DOI] [PubMed] [Google Scholar]
- 8.Akramiene D, Kondrotas A, Didziapetriene J, Kevelaitis E. Effects of β-glucans on the immune system. Medicina (Kaunas). 2007;43:597–606. [PubMed] [Google Scholar]
- 9.Legentil L, Paris F, Ballet C, Trouvelot S, Daire X, Vetvicka V, et al. Molecular interactions of β-(1→3)-glucans with their receptors. Molecules. 2015;20:9745–66. 10.3390/molecules20069745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown GD, Gordon S. Immune recognition. A new receptor for β-glucans. Nature. 2001;413:36–7. 10.1038/35092620 [DOI] [PubMed] [Google Scholar]
- 11.Behall KM, Scholfield DJ, Hallfrisch J. Lipids significantly reduced by diets containing barley in moderately hypercholesterolemic men. J Am Coll Nutr. 2004;23:55–62. 10.1080/07315724.2004.10719343 [DOI] [PubMed] [Google Scholar]
- 12.De Angelis M, Montemurno E, Vannini L, Cosola C, Cavallo N, Gozzi G, et al. Effect of whole-grain barley on the human fecal microbiota and metabolome. Appl Environ Microbiol. 2015;81:7945–56. 10.1128/AEM.02507-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tong LT, Zhong K, Liu L, Zhou X, Qiu J, Zhou S. Effects of dietary hull-less barley β-glucan on the cholesterol metabolism of hypercholesterolemic hamsters. Food Chem. 2015;169:344–9. 10.1016/j.foodchem.2014.07.157 [DOI] [PubMed] [Google Scholar]
- 14.Chen J, Raymond K. β-glucans in the treatment of diabetes and associated cardiovascular risks. Vasc Health Risk Manag. 2008;4:1265–72. 10.2147/vhrm.s3803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tappy L, Gugolz E, Würsch P. Effects of breakfast cereals containing various amounts of β-glucan fibers on plasma glucose and insulin responses in NIDDM subjects. Diabetes Care. 1996;19:831–4. 10.2337/diacare.19.8.831 [DOI] [PubMed] [Google Scholar]
- 16.Pick ME, Hawrish ZJ, Gee MI, Toth E, Garg ML, Hardin RT. Oat bran concentrate bread products improve long-term control of diabetes: a pilot study. J Am Diet Assoc. 1996;96:1254–61. 10.1016/S0002-8223(96)00329-X [DOI] [PubMed] [Google Scholar]
- 17.Theuwissen E, Mensink RP. Water-soluble dietary fibers and cardiovascular disease. Physiol Behav. 2008;94:285–92. 10.1016/j.physbeh.2008.01.001 [DOI] [PubMed] [Google Scholar]
- 18.Ouyang J, Isnard S, Lin J, Fombuena B, Chatterjee D, Wiche Salinas TR, et al. Daily variations of gut microbial translocation markers in ART-treated HIV-infected people. AIDS Res Ther. 2020;17:15. 10.1186/s12981-020-00273-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramendra R, Isnard S, Mehraj V, Chen J, Zhang Y, Finkelman M, et al. Circulating LPS and (1→3)-β-D-glucan: a folie à deux contributing to HIV-associated immune activation. Front Immunol. 2019;10:465. 10.3389/fimmu.2019.00465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mehraj V, Ramendra R, Isnard S, Dupuy FP, Ponte R, Chen J, et al. Circulating (1→3)-β-D-glucan is associated with immune activation during human immunodeficiency virus infection. Clin Infect Dis. 2020;70:232–41. 10.1093/cid/ciz212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoenigl M. Fungal translocation: a driving force behind the occurrence of non-AIDS events? Clin Infect Dis. 2020;70:242–4. 10.1093/cid/ciz215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malyarenko OS, Usoltseva RV, Zvyagintseva TN, Ermakova SP. Laminaran from brown alga Dictyota dichotoma and its sulfated derivative as radioprotectors and radiosensitizers in melanoma therapy. Carbohydre Polym. 2019;206:539–47. 10.1016/j.carbpol.2018.11.008 [DOI] [PubMed] [Google Scholar]
- 23.Geraldelli D, Ribeiro MC, Medeiros TC, Comiran PK, Martins KO, Oliveira MF, et al. Botryosphaeran, a (1→3) (1→6)-β-D-glucan, reduces tumor development and cachexia syndrome in obese male rats by increasing insulin sensitivity and FOXO3a activity. Int J Biol Macromol. 2020;165:985–94. 10.1016/j.ijbiomac.2020.09.168 [DOI] [PubMed] [Google Scholar]
- 24.Vetvicka V, Vashishta A, Saraswat-Ohri S, Vetvickova J. Immunological effects of yeast- and mushroom-derived β-glucans. J Med Food. 2008;11:615–22. 10.1089/jmf.2007.0588 [DOI] [PubMed] [Google Scholar]
- 25.Sarangi I, Ghosh D, Bhutia SK, Mallick SK, Maiti TK. Anti-tumor and immunomodulating effects of Pleurotus ostreatus mycelia-derived proteoglycans. Int Immunopharmacol. 2006;6:1287–97. 10.1016/j.intimp.2006.04.002 [DOI] [PubMed] [Google Scholar]
- 26.Matsui K, Kodama N, Nanba H. Effects of maitake (Grifola frondosa) D-Fraction on the carcinoma angiogenesis. Cancer Lett. 2001;172:193–8. 10.1016/s0304-3835(01)00652-8 [DOI] [PubMed] [Google Scholar]
- 27.Zhang M, Kim JA, Huang AY. Optimizing tumor microenvironment for cancer immunotherapy: β-glucan-based nanoparticles. Front Immunol. 2018;9:341. 10.3389/fimmu.2018.00341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Medzhitov R, Janeway C., Jr. Innate immune recognition: mechanisms and pathways. Immunol Rev. 2000;173:89–97. 10.1034/j.1600-065x.2000.917309.x [DOI] [PubMed] [Google Scholar]
- 29.Bonilla FA, Oettgen HC. Adaptive immunity. J Allergy Clin Immunol. 2010;125:S33–40. 10.1016/j.jaci.2009.09.017 [DOI] [PubMed] [Google Scholar]
- 30.Dominguez-Andres J, Netea MG. Long-term reprogramming of the innate immune system. J Leukoc Biol. 2019;105:329–38. 10.1002/JLB.MR0318-104R [DOI] [PubMed] [Google Scholar]
- 31.Netea MG, Giamarellos-Bourboulis EJ, Domínguez-Andrés J, Curtis N, van Crevel R, van de Veerdonk FL, et al. Trained Immunity: a tool for reducing susceptibility to and the severity of SARS-CoV-2 infection. Cell. 2020;181:969–77. 10.1016/j.cell.2020.04.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arts RJW, Moorlag SJCFM, Novakovic B, Li Y, Wang SY, Oosting M, et al. BCG vaccination protects against experimental viral infection in humans through the induction of cytokines associated with trained immunity. Cell Host Microbe. 2018;23:89–100.e5. 10.1016/j.chom.2017.12.010 [DOI] [PubMed] [Google Scholar]
- 33.Oba K, Kobayashi M, Matsui T, Kodera Y, Sakamoto J. Individual patient based meta-analysis of lentinan for unresectable/recurrent gastric cancer. Anticancer Res. 2009;29:2739–45. [PubMed] [Google Scholar]
- 34.Nakano H, Namatame K, Nemoto H, Motohashi H, Nishiyama K, Kumada K. A multi-institutional prospective study of lentinan in advanced gastric cancer patients with unresectable and recurrent diseases: effect on prolongation of survival and improvement of quality of life. Kanagawa Lentinan Research Group. Hepatogastroenterology. 1999;46:2662–8. [PubMed] [Google Scholar]
- 35.Cheung NK, Modak S, Vickers A, Knuckles B. Orally administered β-glucans enhance anti-tumor effects of monoclonal antibodies. Cancer Immunol Immunother. 2002;51:557–64. 10.1007/s00262-002-0321-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yin X, Ying J, Li L, Zhang H, Wang H. A meta-analysis of lentinan injection combined with chemotherapy in the treatment of non small cell lung cancer. Indian J Cancer. 2015;52 Suppl 1:e29–31. 10.4103/0019-509X.168953 [DOI] [PubMed] [Google Scholar]
- 37.Liu J, Gunn L, Hansen R, Yan J. Combined yeast-derived β-glucan with anti-tumor monoclonal antibody for cancer immunotherapy. Exp Mol Pathol. 2009;86:208–14. 10.1016/j.yexmp.2009.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen J, Seviour R. Medicinal importance of fungal β-(1→3), (1→6)-glucans. Mycol Res. 2007;111:635–52. 10.1016/j.mycres.2007.02.011 [DOI] [PubMed] [Google Scholar]
- 39.Kidd PM. The use of mushroom glucans and proteoglycans in cancer treatment. Altern Med Rev. 2000;5:4–27. [PubMed] [Google Scholar]
- 40.Chan GC, Chan WK, Sze DM. The effects of β-glucan on human immune and cancer cells. J Hematol Oncol. 2009;2:25. 10.1186/1756-8722-2-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vos AP, M’Rabet L, Stahl B, Boehm G, Garssen J. Immune-modulatory effects and potential working mechanisms of orally applied nondigestible carbohydrates. Crit Rev Immunol. 2007;27:97–140. 10.1615/critrevimmunol.v27.i2.10 [DOI] [PubMed] [Google Scholar]
- 42.Wang N, Liu H, Liu G, Li M, He X, Yin C, et al. Yeast β-D-glucan exerts antitumour activity in liver cancer through impairing autophagy and lysosomal function, promoting reactive oxygen species production and apoptosis. Redox Biol. 2020;32:101495. 10.1016/j.redox.2020.101495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vetvicka V, Vetvickova J. Natural immunomodulators and their stimulation of immune reaction: true or false? Anticancer Res. 2014;34:2275–82. [PubMed] [Google Scholar]
- 44.Li B, Cai Y, Qi C, Hansen R, Ding C, Mitchell TC, et al. Orally administered particulate β-glucan modulates tumor-capturing dendritic cells and improves antitumor T-cell responses in cancer. Clin Cancer Res. 2010;16:5153–64. 10.1158/1078-0432.CCR-10-0820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu M, Luo F, Ding C, Albeituni S, Hu X, Ma Y, et al. Dectin-1 activation by a natural product β-glucan converts immunosuppressive macrophages into an M1-like phenotype. J Immunol. 2015;195:5055–65. 10.4049/jimmunol.1501158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Albeituni SH, Ding C, Liu M, Hu X, Luo F, Kloecker G, et al. Yeast-derived particulate β-glucan treatment subverts the suppression of myeloid-derived suppressor cells (MDSC) by inducing polymorphonuclear MDSC apoptosis and monocytic MDSC differentiation to APC in cancer. J Immunol. 2016;196:2167–80. 10.4049/jimmunol.1501853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vetvicka V, Vetvickova J. Glucan supplementation has strong anti-melanoma effects: role of NK cells. Anticancer Res. 2015;35:5287–92. [PubMed] [Google Scholar]
- 48.Kalafati L, Kourtzelis I, Schulte-Schrepping J, Li X, Hatzioannou A, Grinenko T, et al. Innate immune training of granulopoiesis promotes anti-tumor activity. Cell. 2020;183:771–85.e12 10.1016/j.cell.2020.09.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Herre J, Gordon S, Brown GD. Dectin-1 and its role in the recognition of β-glucans by macrophages. Mol Immunol. 2004;40:869–76. 10.1016/j.molimm.2003.10.007 [DOI] [PubMed] [Google Scholar]
- 50.Brown GD. Dectin-1: a signalling non-TLR pattern-recognition receptor. Nat Rev Immunol. 2006;6:33–43. 10.1038/nri1745 [DOI] [PubMed] [Google Scholar]
- 51.Reid DM, Gow NA, Brown GD. Pattern recognition: recent insights from Dectin-1. Curr Opin Immunol. 2009;21:30–7. 10.1016/j.coi.2009.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kankkunen P, Teirilä L, Rintahaka J, Alenius H, Wolff H, Matikainen S. (1,3)-β-glucans activate both dectin-1 and NLRP3 inflammasome in human macrophages. J Immunol. 2010;184:6335–42. 10.4049/jimmunol.0903019 [DOI] [PubMed] [Google Scholar]
- 53.Ariizumi K, Shen GL, Shikano S, Kumamoto T, Edelbaum D, Morita A, et al. Identification of a novel, dendritic cell-associated molecule, dectin-1, by subtractive cDNA cloning. J Biol Chem. 2000;275:20157–67. 10.1074/jbc.M909512199 [DOI] [PubMed] [Google Scholar]
- 54.Thornton BP, Vĕtvicka V, Pitman M, Goldman RC, Ross GD. Analysis of the sugar specificity and molecular location of the β-glucan-binding lectin site of complement receptor type 3 (CD11b/CD18). J Immunol. 1996;156:1235–46. [PubMed] [Google Scholar]
- 55.Hong F, Yan J, Baran JT, Allendorf DJ, Hansen RD, Ostroff GR, et al. Mechanism by which orally administered β-1,3-glucans enhance the tumoricidal activity of antitumor monoclonal antibodies in murine tumor models. J Immunol. 2004;173:797–806. 10.4049/jimmunol.173.2.797 [DOI] [PubMed] [Google Scholar]
- 56.O’Brien XM, Heflin KE, Lavigne LM, Yu K, Kim M, Salomon AR, et al. Lectin site ligation of CR3 induces conformational changes and signaling. J Biol Chem. 2012;287:3337–48. 10.1074/jbc.M111.298307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sato T, Iwabuchi K, Nagaoka I, Adachi Y, Ohno N, Tamura H, et al. Induction of human neutrophil chemotaxis by Candida albicans-derived β-1,6-long glycoside side-chain-branched β-glucan. J Leukoc Biol. 2006;80:204–11. 10.1189/jlb.0106069 [DOI] [PubMed] [Google Scholar]
- 58.Tsikitis VL, Martin A, Albina J, Reichner J. Ligation of the lactosylceramide receptor (CDw17) promotes neutrophil migration. J Am Coll Surg. 2004;199:44. 10.1016/j.jamcollsurg.2004.05.079 [DOI] [Google Scholar]
- 59.Hahn PY, Evans SE, Kottom TJ, Standing JE, Pagano RE, Limper AH. Pneumocystis carinii cell wall β-glucan induces release of macrophage inflammatory protein-2 from alveolar epithelial cells via a lactosylceramide-mediated mechanism. J Biol Chem. 2003;278:2043–50. 10.1074/jbc.M209715200 [DOI] [PubMed] [Google Scholar]
- 60.Evans SE, Hahn PY, McCann F, Kottom TJ, Pavlovic’ ZV, Limper AH. Pneumocystis cell wall β-glucans stimulate alveolar epithelial cell chemokine generation through nuclear factor-kappaB-dependent mechanisms. Am J Respir Cell Mol Biol. 2005;32:490–7. 10.1165/rcmb.2004-0300OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nakayama H, Yoshizaki F, Prinetti A, Sonnino S, Mauri L, Takamori K, et al. Lyn-coupled LacCer-enriched lipid rafts are required for CD11b/CD18-mediated neutrophil phagocytosis of nonopsonized microorganisms. J Leukoc Biol. 2008;83:728–41. 10.1189/jlb.0707478 [DOI] [PubMed] [Google Scholar]
- 62.Li SS, Ogbomo H, Mansour MK, Xiang RF, Szabo L, Munro F, et al. Identification of the fungal ligand triggering cytotoxic PRR-mediated NK cell killing of Cryptococcus and Candida. Nat Commun. 2018;9:751. 10.1038/s41467-018-03014-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vera J, Fenutría R, Cañadas O, Figueras M, Mota R, Sarrias M, et al. The CD5 ectodomain interacts with conserved fungal cell wall components and protects from zymosan-induced septic shock-like syndrome. Proc Natl Acad Sci U S A. 2009;106:1506–11. 10.1073/pnas.0805846106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sorimachi K, Akimoto K, Ikehara Y, Inafuku K, Okubo A, Yamazaki S. Secretion of TNF-α, IL-8 and nitric oxide by macrophages activated with Agaricus blazei Murill fractions in vitro. Cell Struct Func. 2001;26:103–8. [DOI] [PubMed] [Google Scholar]
- 65.Niu YC, Liu JC, Zhao XM, Wu XX. A low molecular weight polysaccharide isolated from Agaricus blazei suppresses tumor growth and angiogenesis in vivo. Oncol Rep. 2009;21:145–52. [PubMed] [Google Scholar]
- 66.Kubala L, Frankova J, Nickova K, Sandula J, Ciz M, Lojek A. The effect of (1→3)-β-D-glucans, carboxymethylglucan and schizophyllan on human leukocytes in vitro. Carbohydr Res, 2003;338: 2835–40. 10.1016/j.carres.2003.09.007 [DOI] [PubMed] [Google Scholar]
- 67.Zhong K, Tong L, Liu L, Zhou X, Liu X, Zhang Q, et al. Immunoregulatory and antitumor activity of schizophyllan under ultrasonic treatment. Int J Biol Macromol, 2015;80:302–8. 10.1016/j.ijbiomac.2015.06.052 [DOI] [PubMed] [Google Scholar]
- 68.Yang A, Fan H, Zhao Y, Chen X, Zhu Z, Zha X, et al. An immune-stimulating proteoglycan from the medicinal mushroom Huaier up-regulates NF-κB and MAPK signaling via Toll-like receptor 4. J Biol Chem. 2019;294:2628–41. 10.1074/jbc.RA118.005477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang J, Yuan Y, Yue T. Immunostimulatory activities of β-D-glucan from Ganoderma lucidum. Carbohydr Polym. 2014;102:47–54. 10.1016/j.carbpol.2013.10.087 [DOI] [PubMed] [Google Scholar]
- 70.Wang SY, Hsu ML, Hsu HC, Tzeng CH, Lee SS, Shiao MS, et al. The anti-tumor effect of Ganoderma lucidum is mediated by cytokines released from activated macrophages and T lymphocytes. Int J Cancer. 1997;70:699–705. [DOI] [PubMed] [Google Scholar]
- 71.Chien CM, Cheng JL, Chang WT, Tien MH, Tsao CM, Chang YH, et al. Polysaccharides of Ganoderma lucidum alter cell immunophenotypic expression and enhance CD56+ NK-cell cytotoxicity in cord blood. Bioorg Med Chem. 2004;12:5603–9. 10.1016/j.bmc.2004.08.004 [DOI] [PubMed] [Google Scholar]
- 72.Carmona EM, Kottom TJ, Hebrink DM, Moua T, Singh R, Pagano RE, et al. Glycosphingolipids mediate pneumocystis cell wall β-glucan activation of the IL-23/IL-17 axis in human dendritic cells. Am J Respir Cell Mol Biol. 2012;47:50–9. 10.1165/rcmb.2011-0159OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ali MF, Driscoll CB, Walters PR, Limper AH, Carmona EM. β-Glucan-Activated human B lymphocytes participate in innate immune responses by releasing proinflammatory cytokines and stimulating neutrophil chemotaxis. J Immunol. 2015;195:5318–26. 10.4049/jimmunol.1500559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ding J, Feng T, Ning Y, Li W, Wu Q, Qian K, et al. β-Glucan enhances cytotoxic T lymphocyte responses by activation of human monocyte-derived dendritic cells via the PI3K/AKT pathway. Hum Immunol. 2015;76:146–54. 10.1016/j.humimm.2015.01.009 [DOI] [PubMed] [Google Scholar]
- 75.Ina K, Kanda M, Yoneda M, Kodera Y, Kabeya M, Yuasa S, et al. A shiitake mushroom β-Glucan, stimulates tumor-specific adaptive immunity through PD-L1 down-regulation in gastric cancer cells. Med Chem. 2016;6:710–4. [Google Scholar]
- 76.Masuda Y, Nakayama Y, Tanaka A, Naito K, Konishi M. Antitumor activity of orally administered maitake α-glucan by stimulating antitumor immune response in murine tumor. PLoS One. 2017;12:e0173621. 10.1371/journal.pone.0173621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Masuda Y, Nakayama Y, Mukae T, Tanaka A, Naito K, Konishi M. Maturation of dendritic cells by maitake α-glucan enhances anti-cancer effect of dendritic cell vaccination. Intl Immunopharmacol. 2019;67: 408–16. 10.1016/j.intimp.2018.12.039 [DOI] [PubMed] [Google Scholar]
- 78.Bose N, Chan AS, Guerrero F, Maristany CM, Qiu X, Walsh RM, et al. Binding of soluble yeast β-Glucan to human neutrophils and monocytes is complement-dependent. Front Immunol. 2013;4:230. 10.3389/fimmu.2013.00230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Qi C, Cai Y, Gunn L, Ding C, Li B, Kloecker G, et al. Differential pathways regulating innate and adaptive antitumor immune responses by particulate and soluble yeast-derived β-glucans. Blood. 2011;117:6825–36. 10.1182/blood-2011-02-339812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jonas A, Qiu X, Chan A, McMurray D, Bose N. Imprime PGG, a yeast β-glucan immunomodulator, can engage Fc gamma receptor (FcγR) in addition to complement receptor 3 (CR3) on human neutrophils and monocytes (abstract). In: Keystone Symposium on Tumor Immunology, Multidisciplinary Science Driving Combination Therapy; USA. Eagan, MN: Biothera; 2015. [Google Scholar]
- 81.Leonardo SM, Fulton RB, Wurst LR, Gorden KB, Bykowski Jonas A, Qui X, et al. Imprime PGG binds to neutrophils through complement, Fc, and dectin-1 receptors, priming these cells for enhanced ROS production and tumor cell cytotoxicity. Cancer Immunol Res. 2016;4 Suppl 1:Abstract nr A160. 10.1158/2326-6074.CRICIMTEATIAACR15-A160 [DOI] [Google Scholar]
- 82.Li B, Allendorf DJ, Hansen R, Marroquin J, Ding C, Cramer DE, et al. Yeast β-glucan amplifies phagocyte killing of iC3b-opsonized tumor cells via complement receptor 3-Syk-phosphatidylinositol 3-kinase pathway. J Immunol. 2006;177:1661–9. 10.4049/jimmunol.177.3.1661 [DOI] [PubMed] [Google Scholar]
- 83.Chan AS, Jonas AB, Qiu X, Ottoson NR, Walsh RM, Gorden KB, et al. Imprime PGG-mediated anti-cancer immune activation requires immune complex formation. PLoS ONE. 2016;11:e0165909. 10.1371/journal.pone.0165909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bose N, Ottoson NR, Qiu X, Harrison B, Lowe JR, Uhlik MT, et al. Immune pharmacodynamic responses of the novel cancer immunotherapeutic Imprime PGG in healthy volunteers. J Immunol. 2019;202:2945–56. 10.4049/jimmunol.1801533 [DOI] [PubMed] [Google Scholar]
- 85.Chan A, Qiu X, Jonas AB, Patchen ML, Bose N. Imprime PGG, a yeast β-glucan immunomodulator, has the potential to repolarize human monocyte-derived M2 macrophages to M1 phenotype. J Immunother Cancer. 2014;2 Suppl 3:P191. 10.1186/2051-1426-2-S3-P191 [DOI] [Google Scholar]
- 86.Chan A, Qiu X, Jonas A, Kangas T, Ottoson N, Bose N. Imprime PGG modulates the function of monocyte-derived M2 macrophages and dendritic cells to drive T cell expansion (abstract). Cancer Res. 2015;75 Suppl 15:LB225. 10.1158/1538-7445.AM2015-LB-225 [DOI] [Google Scholar]
- 87.Fraser K, Ottoson N, Qiu X, Chan A, Jonas A, Kangas T, et al. Imprime PGG modulates the myeloid component of the tumor microenvironment to coordinate an anti-tumor immune response (abstract). 2016;76 Suppl 3:A02. 10.1158/1538-7445.FBCR15-A02 [DOI] [Google Scholar]
- 88.Bose N, Chan A, Jonas A, Qiu X, Ottoson N, Kangas T, et al. Imprime PGG treatment elicits a coordinated antitumor immune response that triggers enhanced expression of PD-L1 on tumor cells as well as monocyte-derived macrophages and dendritic cells (abstract). Cancer Res. 2015;75 Suppl 15:LB-228. 10.1158/1538-7445.AM2015-LB-228 [DOI] [Google Scholar]
- 89.Fraser KA, Kangas T, Fulton RB. Imprime PGG, a soluble yeast β-glucan PAMP, enhancement of anti-tumor responses in combination with tumor targeting antibody is highly dependent on NK cell killing (abstract). Cancer Res. 2018;78 Suppl 13:3767. 10.1158/1538-7445.AM2018-3767 [DOI] [Google Scholar]
- 90.Leonardo S, Gorden K, Fulton R, Wurst L. Imprime PGG decreases regulatory T cell suppression and enhances T cell proliferation and differentiation revealing additional mechanisms for its anti-tumor activity (abstract). Cancer Res. 2015;78 Suppl 15:5034. 10.1158/1538-7445.AM2015-5034 [DOI] [Google Scholar]
- 91.Fulton R, Leonardo S, Michel K, Danielson M, Gorden K, Graff J. Imprime PGG, a soluble β-glucan, binds to and activate dendritic cells resulting in enhanced T cell priming, expansion, and cytokine production (abstract). Cancer Res. 2016;4 Suppl 1:B019. 10.1158/2326-6074.CRICIMTEATIAACR15-B019 [DOI] [Google Scholar]
- 92.Fraser K, Chan A, Fulton R, Leonardo S, Jonas A, Qiu X, et al. Imprime PGG triggers PD-L1 expression on tumor and myeloid cells and prevents tumor establishment in combination with αPD-L1 treatment in vivo (abstract). Cancer Res. 2016;76 Suppl 14:2335. 10.1158/1538-7445.AM2016-2335 [DOI] [Google Scholar]
- 93.Qiu X, Chan A, Jonas A, Kangas T, Ottoson N, Graff J, et al. Imprime PGG, a yeast β-glucan PAMP elicits a coordinated immune response in combination with anti-PD1 antibody. J Immunol. 2016;196 Suppl 1:214–6. [Google Scholar]
- 94.Fulton R, Leonardo S, Jonas A, Fraser K, Chan A, Ottoson N, et al. Imprime PGG, a β-glucan PAMP (pathogen-associated molecular pattern), effectively elicits in vivo maturation of antigen-presenting cells in mice and humans, suggesting potential synergy with checkpoint inhibitor therapy (abstract). Cancer Res. 2016;76 Suppl 14:LB-089, 10.1158/1538-7445.AM2016-LB-089 [DOI] [Google Scholar]
- 95.Hong F, Hansen RD, Yan J, Allendorf DJ, Baran JT, Ostroff GR, et al. B-glucan functions as an adjuvant for monoclonal antibody immunotherapy by recruiting tumoricidal granulocytes as killer cells. Cancer Res. 2003;63:9023–31. [PubMed] [Google Scholar]
- 96.Halstenson CE, Shamp T, Gargano MA, Walsh RM, Patchen ML. Two randomized, double-blind, placebo-controlled, dose-escalation phase 1 studies evaluating BTH1677, a 1, 3-1,6 β glucan pathogen associated molecular pattern, in healthy volunteer subjects. Invest New Drugs. 2016;34:202–15. 10.1007/s10637-016-0325-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Iglesias JL, Prathikanti R, Ma B, Mattson P, Kedrowski D, Lowe J, et al. A multicenter, open-label, phase 2 study of imprime PGG & pembrolizumab in subjects with adv squamous cell carcinoma of H&N (SCCHN) who failed pembro monotherapy or experiencing SD following completion of 4 to 8 cycles of pembro monotherapy. J Clin Oncol. 2017;35:TPS3105. [Google Scholar]
- 98.Uhlik M, Bose N, Cox J, Mattson P, Gargano M, O’Day S, et al. Response and clinical benefit assessment of the combination of the dectin-1 agonist imprime PGG and anti-PD-1 pembrolizumab in chemotherapy-resistant metastatic triple negative breast cancer (TNBC) (abstract). Cancer Res. 2020;80 Suppl 4:PD1-02. [Google Scholar]
- 99.Chan A, Bose N, Ottoson N, Qiu X, Harrison B, Walsh R. Clinical benefit potentially evident with immunopharmacodynamic responses in prior-checkpoint failed metastatic melanoma patients treated with imprime PGG and pembrolizumab (abstract). JITC. 2020;8:P862. 10.1136/LBA2019.15 [DOI] [Google Scholar]
- 100.Modak S, Kushner BH, Kramer K, Vickers A, Cheung IY, Cheung NK. Anti-GD2 antibody 3F8 and barley-derived (1→3), (1→4)-β-D-glucan: a phase I study in patients with chemoresistant neuroblastoma. Oncoimmunology. 2013;2:e23402. 10.4161/onci.23402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kushner BH, Cheung IY, Modak S, Kramer K, Ragupathi G, Cheung NK. Phase I trial of a bivalent gangliosides vaccine in combination with β-glucan for high-risk neuroblastoma in second or later remission. Clin Cancer Res. 2014;20:1375–82. 10.1158/1078-0432.CCR-13-1012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.A phase Ib/II study of anti-PD-1 antibody pembrolizumab and imprime PGG for patients with metastatic non-small cell lung cancer after progression on first-line therapy: big ten cancer research consortium BTCRC-LUN15-017. [Internet]. Bethesda (MD): National Library of Medicine (US); c2016 [updated 2021 Jan 27; cited 2020 Apr 20]. ClinicalTrials.gov Identifier: NCT03003468. Available from: https://www.clinicaltrials.gov/ct2/show/NCT03003468
- 103.A phase Ib/II, open-label, multicenter, randomized umbrella study evaluating the efficacy and safety of multiple immunotherapy-based treatment combinations in patients with metastatic colorectal cancer (morpheus-CRC). [Internet]. Bethesda (MD): National Library of Medicine (US); c2018 [updated 2021 Jan 27; cited 2020 Apr 20]. ClinicalTrials.gov Identifier: NCT03555149. Available from: https://www.clinicaltrials.gov/ct2/show/NCT03555149
- 104.Winer E, Dang T, Karantza V, Su SC. KEYNOTE-119: a randomized phase III study of single-agent pembrolizumab (MK-3475) vs. single-agent chemotherapy per physician’s choice for metastatic triple-negative breast cancer (mTNBC). J Clin Oncol. 2016;34:TPS1102. 10.1200/JCO.2016.34.15_suppl.TPS1102 [DOI] [Google Scholar]
- 105.Hurley PJ, Bose N, Jha G, Gargano M, Ottoson N, Gorden K, et al. Immunoglobulin restores immune responses to BTH1677 in patients with low levels of antibodies to β-glucan. Anticancer Res. 2020;40:1467–73. 10.21873/anticanres.14090 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.