Abstract
Background
Self-medication has become a serious public health problem posing great risks, especially with the increasing number of cases of COVID-19 disease globally and in Uganda. This may be partly because of the absence of a recognized treatment for the disease, however, the differing prevalence and nature from country to country may influence human behavioral responses.
Purpose
This study aimed to investigate the behavioral response to self-medication practices during the COVID-19 pandemic and lockdown in comparison to the pre-COVID period in Western Uganda.
Methods
A descriptive cross-sectional survey was conducted from June to August 2020 in western Uganda using online Google forms and printed questionnaires to investigate the level of self-medication practice before and during the COVID-19 pandemic. This included 280 participants, aged 18 and above who consented to participate in the study. Participants were selected using a convenience sampling technique, and sampling was done by sending a structured online questionnaire via Google forms and printed questionnaires to participants who did not use the online Google forms.
Results
Respondents that knew about self-medication were 97% of the 272 participants. Those that are aware of self-medication, have heard about it either through different avenues. Respondents who practiced self-medication before the COVID-19 pandemic were 239 (88%); those who practiced self-medication during the COVID-19 pandemic were 156 (57%); those that did not were 115 (43%). There was a statistically significant decrease in the number of respondents who practice self-medication during the COVID-19 pandemic lockdown compared to the practice before the pandemic lockdown. p < 0.05 at 95% confidence interval (OR = 5.39, 95% CI = 3.48, 8.32).
Conclusion
Our investigation showed adequate knowledge of self-medication and a high level of self-medication practice with a decrease in self-medication practices during the COVID-19 pandemic lockdown compared to the practice before the lockdown.
Keywords: before and post COVID-19, self-medication practice, medication, behavioural response, knowledge
Introduction
The outbreak of coronavirus has prompted many countries around the world, including Uganda, to introduce lockdown as advised by WHO because of growing cases. In most countries so far, partial lockdowns as well as social distancing guidelines, frequent washing of hands, and/or sanitizing have been put in place to curb the spread of the virus. Some of these restrictions may remain in place, probably until an appropriate and highly effective vaccine for the virus is developed. In this regard, many human behavioral patterns in life have been seriously affected, ranging from education, economics, health, social, religion, etc.
In Uganda, for example, a total ban on people’s movement from one district to another, border closure, curfew, and others are measures that have been employed to prevent the spread of the virus during the lockdown. Many patients suffering from other diseases have little or no access to health care services as a result of restrictions, especially on movement. Consequently, some studies have revealed significant changes in the way people live their lives during this lockdown, which included avoiding crowded public places, wearing a face mask, avoiding physical contact, improving personal hygiene (eg frequent hand washing and using hand sanitizer), changes in sleep and use of sleep substances, diet and physical activities.1–3 Some of these practices may have certain behavioural and mental health implications.
During the pandemic, the way individuals behave is important to note because a change in public behaviour is an alternative to controlling outbreaks when there are no suitable pharmacological interventions. Furthermore, the behavioral patterns of an individual can influence their family, community, society, and social networks.4 Epidemics have been reported in a study that used mathematical models to affect people’s fears, emotions, and ultimately their behavior.5 With respect to these behavioral changes resulting from the lockdown and restrictions, we envisaged that self-medication practices may be influenced by the way people try to cope with their health management at this crucial time.
Self-medication can be referred to as the intake of drugs, herbs, or home remedies either on one’s initiative or on the advice of another person for physical or psychological ailments.6 Previous prescribed drugs, pharmacists, family, friends, neighbors, the internet, and suggestions from advertisements are all common sources of self-medication. According to Osemene and Lamikanra (2012), self-medication is a serious public health problem globally, posing risks such as drug resistance, organ damage, and deaths (2.9–3.7%) in the world because of drug-drug interactions.7
The probability of drug abuse has been reported to be on the rise as a result of a global increase in self-medication.8,9 Signs and symptoms of underlying disease conditions can be concealed by self-medication, causing drug resistance, delayed diagnoses, and making the problem complex or difficult to deal with.10,11
Although several countries and cultures present the nature and prevalence of self-medication differently globally, the practices are mostly based on certain advantages or disadvantages obtained from past experiences with similar drugs.8 The effects of self-medication can be positive when practiced correctly, such as saving scarce medical resources from being wasted on minor conditions; reducing the pressure on medical services where health care personnel are insufficient; lowering the costs of community-funded health care programs, and reducing absenteeism from work due to minor symptoms.12
However, it also has potential risks at an individual level, such as incorrect self-diagnosis, wrong choice of therapy, incorrect route of administration, and severe adverse effects. Also, failure to recognize that the same active substance is already being taken under a different name and failure to recognize contraindications, interactions, and precautions, incorrect route of administration, inadequate and excessive dosage, and many more could be probable hazards.13 Self-medication could lead to high drug-induced disease and public expenditure wastefulness.
Self-medication causes adverse reactions and prolonged suffering as well as other related problems such as wastage of resources and high resistance to pathogens. It is important to note that a current worldwide problem, especially in developing countries where antibiotics are available without a prescription, is antimicrobial resistance.13 The overall self-medication rate in sub-Saharan Africa varies from 11.9% to 75.7%. In Uganda, a high prevalence of self-medication has been previously reported in the northern and southwestern regions before COVID-19.14–16 During the COVID-19 pandemic, many medications have been proposed as potential candidates for the treatment of the disease, and so much misleading information has compelled many people to self-medicate due to the fear of contracting the virus and poor access to health services.17,18
According to Patricia Akankwatsa, COVID-19 has resulted in a high increase in self-medication, leading to many Ugandans engaging in self-treatment without first consulting health officers as the COVID-19 pandemic worsens.19 However, the Pharmaceutical Society of Uganda Council has warned the public to cease managing COVID-19 by using medications such as azithromycin and dexamethasone without seeking the advice of a health professional.20 Therefore, this research sought to investigate the behavioural response of the community in western Uganda towards self-medication practices during the COVID-19 pandemic and lockdown since there is no information in this regard.
Materials and Methods
Study Design, Site, and Population
A descriptive cross-sectional survey was conducted from June to August 2020 in western Uganda using online Google forms and printed questionnaires to investigate the level of self-medication practice before and during the COVID-19 pandemic. The contents of the questionnaire and the purpose of the study were explained at the beginning of the study, along with the informed consent. The study was conducted among adults from age 18 and above and in communities of western Uganda, and to maintain reliability and confidentiality, responses were made anonymous.
Sample Size Determination
The population of the western region, one of the four regions of Uganda, was 8,874,862 according to the 2014 census.21,22 With a population growth rate of 3.32%, the sample size of the study was calculated using the OpenEpi sample size calculator.23,24 The estimated sample size was 280, with a confidence level of 90% using an anticipated frequency (p) of 50%. Since it was risky and not possible to carry out a community-based sampling survey due to the pandemic, study participants were selected using a convenience sampling technique, and sampling was done by sending a structured online questionnaire through Google forms to some participants. Also, a printed hard copied self-administered questionnaire was made available to some participants, mainly the uneducated, who did not use the online questionnaire.
The questionnaire consisted of twenty (20) questions developed in the English language and covered two parts. The first part of the questionnaire included demographic data of the participants (eg, gender, education, occupation, age, religion). The second part of the questionnaire focused on awareness and attitude towards self-medication as well as the practice before and during the COVID-19 pandemic. For the uneducated participants, the questions were read and interpreted to the respondents to get an accurate response. The respondents were asked if they had ever heard of self-medication, if they had ever practiced self-medication before and/or during the COVID-19 pandemic, what medicine they self-medicated with, and where they obtained the medicine, the frequency of illnesses, the reason for self-medication, and their perception of self-medication. To ensure anonymity and confidentiality, no names or email addresses were asked. Those who participated willingly agreed to take part in the study, and for quality control, strict parameters were set to ensure participants answered the questionnaire once. The validity and reliability of the questionnaires were ensured by pre-testing it first with a few respondents among the target population and with some scholars to ascertain its appropriateness.
Data Management
The researcher checked all filled data collection tools for validity and completeness. Any discrepancies in the entries were corrected by referring to the source documents (questionnaires).
Statistical Analysis
The data were entered into and analyzed with MS-Excel and OpenEpi version 3.01. The odd ratio and 95% confidence interval were calculated using MS-Excel. Two-sample independent t-test and Chi-square were the tools used for data analysis with a statistical significance level of 0.05.
Results
Sociodemographic Characteristics of Participants
Our study showed the sociodemographic features of the respondents where most of them were males 149 (54.8%) and females 124 (45.2%) between the ages of 25–34 years (43.8%), Christian (85.7.8%), and others as shown in Table 1. The percentage of respondents that know about self-medication is 97% and those that practice self-medication is approximately 88%.
Table 1.
Socio-Demographic Characteristics of the Study Respondents (n = 272)
| Characteristics | Frequency (n) | Percentage (%) | P value | |
|---|---|---|---|---|
| Gender | Male | 149 | 54.8 | 0.136 |
| Female | 123 | 45.2 | 0.182 | |
| Age | 18–24 | 90 | 33.0 | 0.241 |
| 25–34 | 119 | 43.8 | 0.189 | |
| 35–54 | 51 | 18.8 | 0.315 | |
| 55 and above | 12 | 4.4 | 0.417 | |
| Education status | Uneducated | 10 | 3.7 | 0.425 |
| Primary School | 19 | 7.0 | 0.394 | |
| Secondary school | 11 | 4.0 | 0.421 | |
| Certificate/ Diploma | 137 | 50.4 | 0.158 | |
| Bachelors/ Masters/PhD | 95 | 34.9 | 0.233 | |
| Occupation | Unemployed | 19 | 7.0 | 0.394 |
| Student | 70 | 25.7 | 0.040 | |
| Lecturer/Teacher | 48 | 17.6 | 0.134 | |
| Health worker | 38 | 14.0 | 0.282 | |
| Merchant/Peasant | 80 | 29.4 | 0.260 | |
| Others | 17 | 6.3 | 0.400 | |
| Religion | Christianity | 233 | 85.7 | 0.008 |
| Islam | 36 | 13.2 | 0.349 | |
| Others | 3 | 1.1 | 0.463 |
Knowledge Level of Self-Medication Among the Participants
Our result showed that 97% of respondents had heard about self-medication either through health workers, media, family members, friends, and/or school, while 3% said they had not heard about self-medication. There is a statistically significant difference between those that have heard of self-medication and those that have not. The number of respondents that knew about self-medication was 146 (98%) male and 119 (96%) female, while those that were not aware of self-medication were 3 (2%) male and 5 (4%) female (Table 2).
Table 2.
Showing Odd ratio, confidence interval and p value of the Knowledge and Practice of self-medication before and during COVID-19 pandemic
| Yes | No | Yes (%) | No (%) | Odd Ratio | 95% CI | P value | |
|---|---|---|---|---|---|---|---|
| Knowledge about Self-medication | 264 | 8 | 97 | 3 | 2.00 | 0.49–8.37 | 0.008 |
| Self-medication Practice Before COVID-19 Pandemic | 239 | 33 | 88 | 12 | 5.39 | 3.48–8.32 | < 0.001 |
| Self-medication Practice During COVID-19 Pandemic | 156 | 116 | 57 | 43 | 1.00 | 1.31–5.62 | < 0.001 |
Self-Medication Practices Before and During the COVID-19 Pandemic
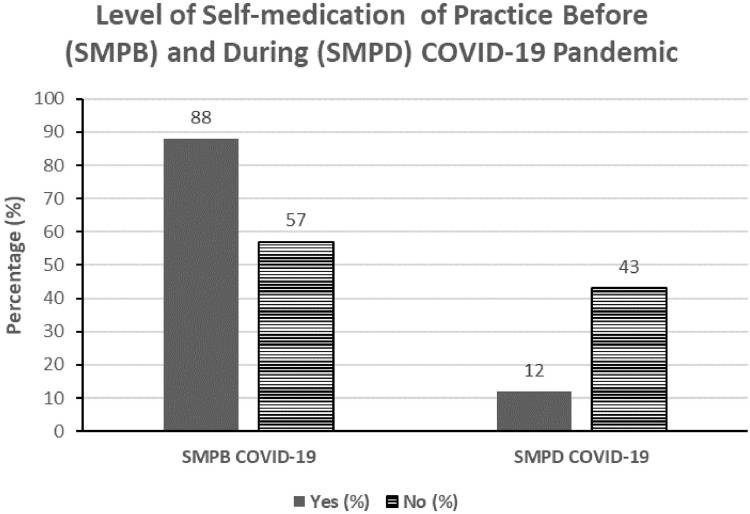
Among the 272 respondents, those who had practiced self-medication before the COVID-19 pandemic were 239 (88%), and those that had not were 33 (12%). Those who used self-medication were statistically significantly more than those who did not (P < 0.001). During the COVID-19 pandemic, the respondents who practiced self-medication were 156 (57%), while those that did not were 116 (43%) (Figure 1).
Figure 1.
Comparison between the level of self-medication before and during the COVID-19 pandemic. A Chi-square test shows a statistically significant difference (P < 0.001) between respondents.
Abbreviations: SMPB COVID-19, Self-medication practice before COVID-19; SMPD COVID-19, Self-medication practice during COVID-19.
There is a statistically significant difference in the number of those who practice self-medication and those that do not; P < 0.001 at a 95% confidence interval. In addition, there was a statistically significant decrease in the number of respondents who used self-medication during the COVID-19 pandemic lockdown compared to before the pandemic lockdown P < 0.001 (Table 2).
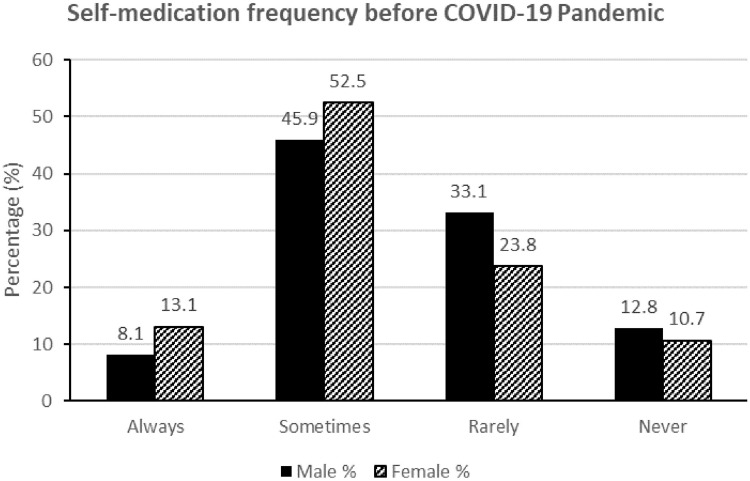
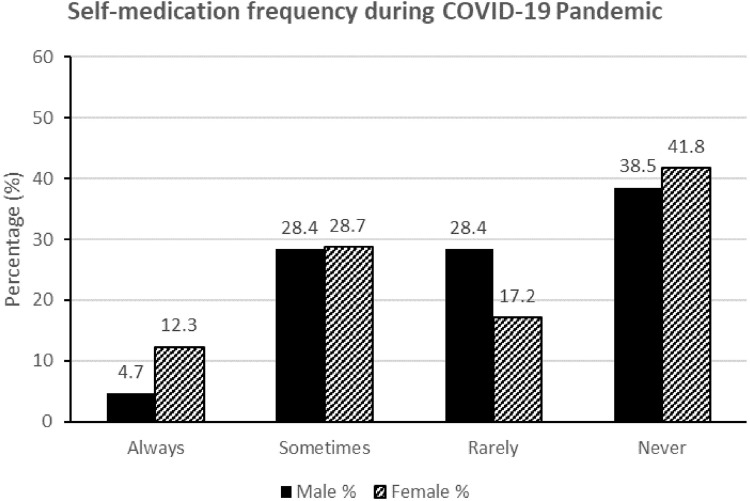
Frequency of Self-Medication Before and During the COVID-19 Pandemic
Considering how often the respondents practice self-medication, our results showed that the majority of the respondents sometimes practice (68, 46% male and 64, 52.5% female) self-medication before the COVID-19 pandemic lockdown while 19 (12.8%) male and 13 (10.7%) female had never used self-medication before the lockdown. The male respondents that always practice self-medication were 12 (8.1%) and female 16 (13.1%), while those that rarely practice self-medication were 49 (33.1%) male and 29 (23.8%) female (OR = 1.0, 95% CI = 1.31, 5.65). A Chi-square test shows a statistically significant difference between males and females, P < 0.05 (Figure 2). During the COVID-19 lockdown, the number of respondents who sometimes practice self-medication was 42 (28.4%) in males and 35 (28.7%) in females. Those respondents who never engage in self-medication at all are 57 (38.5%) males and 51 (41.8%) females. During the pandemic, 42 (28.4%) males and 35 (28.7%) females occasionally practice self-medication, while 42 (28.4%) males and 21 (17.2%) females rarely practice self-medication (OR = 0.96, 95% CI = 1.6, 4.2). A Chi-square test shows a statistically significant difference between males and females, P < 0.05 (Figure 3).
Figure 2.
Frequency of self-medication before the COVID-19 pandemic. A Chi-square test shows a statistically significant difference (P < 0.001) between male and female respondents.
Figure 3.
Frequency of self-medication during the COVID-19 pandemic. Chi-square test shows a statistical significant difference (P < 0.001) between male and female respondents.
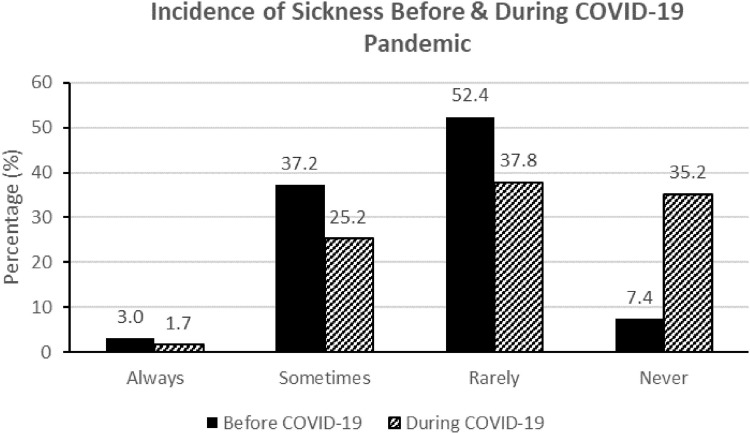
Incidence of Sicknesses Before and During the COVID-19 Pandemic
Among 272 respondents, those that never felt sick before the COVID-19 pandemic lockdown were 17 (7.4%), which increased to 81 (35.2%) during the lockdown while 7 (3%) never, 86 (37.2%) sometimes, 121 (52.4%) rarely practice self-medication before COVID-19 pandemic lockdown. However, 4 (1.7%) never, 58 (25.2%) sometimes, and 87 (37.8%) rarely practice self-medication during the lockdown (Figure 4). Our results revealed a statistically significant decrease (P < 0.05) in the incidence of sickness before and during the COVID-19 pandemic lockdown.
Figure 4.
Incidence of sickness before and during the COVID-19 pandemic.
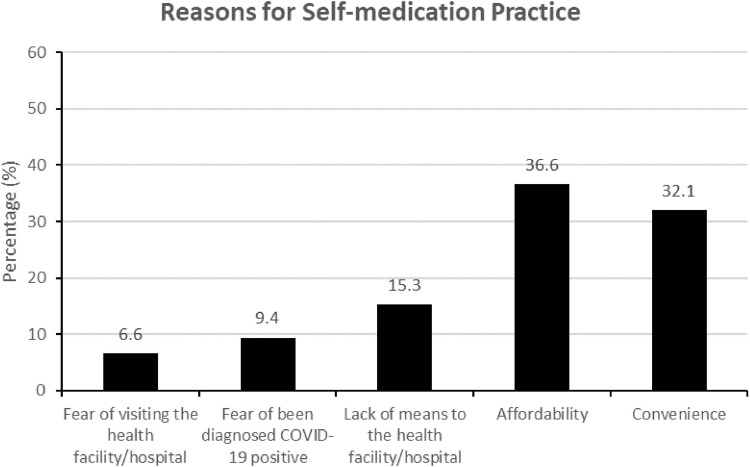
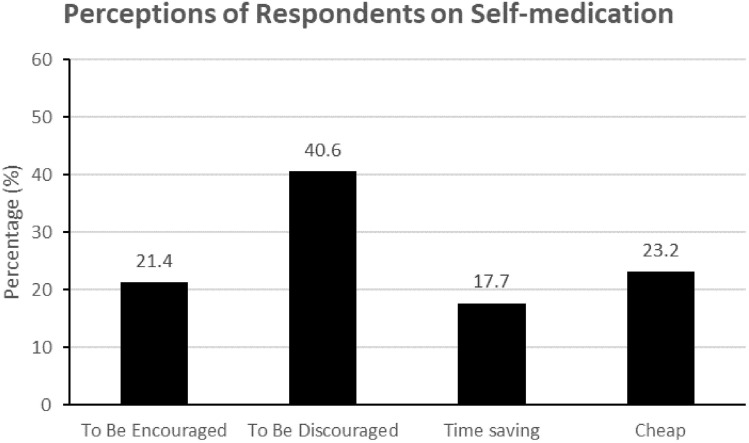
Reason for Self-Medication Practice
The reasons people self-medicate are numerous, some of which were investigated in this study, and from our respondents, 7% fear visiting a health facility or hospital, 9% fear being diagnosed with COVID-19 positive, 15% lack the means to get to the health facility or hospital, 37% consider self-medication affordable, while 32% said it is convenience (Figure 5). Generally, most of the respondents (41%) opined that self-medication should be discouraged, 21% said it should be encouraged, 18% said it is time-saving and 23% said it is cheap (Figure 6).
Figure 5.
Reasons for self-medication practice.
Figure 6.
Perceptions of respondents on self-medication.
Discussion
Many factors have been reported to affect self-medication practice, which includes the availability of drugs, education, society, and many more.25–27 Our investigation revealed that most of the respondents know about self-medication and practice it (Table 1). The rate of self-medication was 88% before the COVID-19 lockdown, with females practicing more, but dropped to 57% during the lockdown (Table 2). This high incidence is consistent with a similar report of 88% among Gujarat students and was as high as 92% among Indian students,28–30 while prevalence among students in countries such as Palestine and Brazil was found to be 98% and 86.4% respectively31,32 In Sub-Saharan Africa, the prevalence of self-medication in a study among undergraduate students has been reported to be 81.8% in Nigeria, 64.98% in Northeast Ethiopia and 63.5% in Western Uganda.16,33,34 However, a previous study carried out among adult household members in communities in Northern Uganda reported 75.7% self-medication.15 This study shows a higher self-medication prevalence before the COVID-19 pandemic compared to the reports of previous studies conducted among students in Uganda and Ethiopia as well as in the communities in Northern Uganda. The higher rate of self-medication found among females compared to males in this study is consistent with previous studies.35,36
The World Health Organization (WHO) has continued to promote self-medication as a means to treat common diseases in the community, considering it beneficial and helping to decrease the burden on health care services, especially in developing countries.37 In this respect, self-medication when practiced correctly could be a great benefit to the community during the COVID-19 lockdown as it allows patients to become responsible and build confidence to manage their health. Nevertheless, previous studies have shown quite many negative effects of substance use resulting from social isolation, such as COVID-19 lockdown and restrictions, with probable drug abuse associated more with socially isolated people and most likely diagnosed with substance use disorder.38–41
Our results show a significant decrease in the percentage of people that practiced self-medication before the COVID-19 pandemic compared to the percentage of people that practiced self-medication during the COVID-19 pandemic lockdown (Figure 1). Furthermore, our study revealed gender differences in the behavioural responses to self-medication before and during the COVID-19 pandemic, where there were more female than male participants who were always engaged or never engaged in self-medication practice during the pandemic but fewer females than males who had never engaged in self-medication before COVID-19 pandemic. (Figures 2 and 3). Also, there was a decrease in the incidence of sickness during the COVID-19 lockdown as many of the respondents never felt sick during lockdown (Figure 4).
The decrease in the incidence of sickness may be due to the change in the behavior of people as a result of the measures put in place to combat the spread of the disease. During the lockdown, there is a high propensity for people to pay more attention to their health as people were encouraged to practice more personal hygiene such as washing their hands regularly and/or using sanitizers, wearing face masks, and maintaining social distance, which may have resulted in the improvement of people’s health status in the community. This is consistent with the report that maintaining good personal hygiene can reduce the incidence of diseases such as infections, trachoma, diarrhea-related diseases, pneumonia, and many others.3 The decrease in the incidence of illnesses may have resulted in the decrease in self-medication practices since people no longer fell as ill as they were before the COVID-19 pandemic, hence there was no need to take medications.
The most common reasons for self-medication were affordability, convenience, a lack of transportation to the health facility/hospital, fear of being diagnosed COVIC-19 positive, and fear of visiting the health facility/hospital (Figure 5). Concerning the perception of respondents to self-medication, most of them (40.6%) opined that self-medication should be discouraged (Figure 6), but the percentage of respondents practicing self-medication is still high. This may have emanated from the fact that self-medication practice reduces the time spent waiting for a doctor, can save a life in emergencies, and lowers the cost of health care.42
Also, the World Health Organization recommended that self-medication can assist in the prevention and treatment of illnesses, where consulting a doctor is not necessary, therefore making treatment of common illnesses cheaper. Nevertheless, inappropriate use of medication could lead to a rise in diseases triggered by abuse and cause waste of public funds.12
Conclusion
Our investigation showed that the majority of the populace has adequate knowledge of self-medication as evidenced by the higher percentage of respondents in this category and there was a high level of self-medication practice before the COVID-19 pandemic lockdown. However, there was a decrease in self-medication practices during the COVID-19 pandemic lockdown compared to the practices before the lockdown. This decrease correlates with a reduction in the incidence of sickness during the lockdown, which could have resulted from the practice of good personal hygiene as recommended and campaigned by WHO to prevent the spread of COVID-19. A decrease in the incidence of illnesses may have resulted in the decrease in self-medication practices since people no longer fell as ill as they were before the COVID-19 pandemic, hence there was no need to take medications. The recommendation of WHO to teach self-medication with the right approach and proper regulation to prevent drug resistance problems associated with the wrong use of drugs globally should be given serious attention. More teaching and regulation of self-medication should be done particularly in developing countries where there is no control over the use of antibiotics.
Acknowledgment
The authors wish to acknowledge the efforts of research assistants who helped in the data collection process, Kampala International University Ethical Review Committee, and the Department of Human Anatomy, Kabale University for support.
Ethical Consideration
Expedited ethical clearance and approval were sought from the Kampala International University Ethical Review Committee and registered as Nr.UG-REC-023/201914. All participants were informed about the purpose of this study and informed consent to participate was acquired, which included the publication of anonymized responses and the right to withdraw from the study at any time during the study, which was conducted in accordance with the Declaration of Helsinki.
Consent for Publication
All the authors have consented that the contents of this article be published accordingly.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest regarding the publication of this article.
References
- 1.de Bruin WB, Bennett D. Relationships between initial covid-19 risk perceptions and protective health behaviors: a national survey. Am J Prev Med. 2020;59:157–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arora T, Grey I. Health behaviour changes during COVID-19 and the potential consequences: a mini-review. J Health Psychol. 2020;25(9):1155–1163. doi: 10.1177/1359105320937053 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization: Hygiene. Available from: http://www.who.int/topics/hygiene. Accessed January 2 2018.
- 4.Chen J, Lewis B, Marathe A, Marathe M, Swarup S, Vullikanti AKS. Chapter 12 - individual and collective behavior in public health epidemiology. In: Srinivasa Rao ASR, Pyne S, Rao CR, editors. Handbook of Statistics. Netherlands: Elsevier; 2017:329–365. [Google Scholar]
- 5.Bi K, Chen Y, Zhao S, Ben-Arieh D, Wu CH. Modeling learning and forgetting processes with the corresponding impacts on human behaviors in infectious disease epidemics. Comput Ind Eng. 2019;129(5):1297. doi: 10.1016/j.cie.2018.04.035 [DOI] [Google Scholar]
- 6.Hernandez-Juyol M, Job-Quesada JR. Dentistry and self-medication: a current challenge. Med Oral. 2002;7:344–347. [PubMed] [Google Scholar]
- 7.Osemene K, Lamikanra A. A study of the prevalence of self-medication practice among university students in south-western Nigeria. Trop J Pharm Res. 2012;11. doi: 10.4314/tjpr.v11i4.21 [DOI] [Google Scholar]
- 8.McCabe SE, Teter CJ, Boyd CJ. Illicit use of prescription pain medication among college students. Drug Alcohol Depend. 2005;77(1):37–47. doi: 10.1016/j.drugalcdep.2004.07.005 [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. “(e role of the pharmacist in self-care and self-medication,” Report of the 4th WHO consultative group on the role of the pharmacist. Hague, Netherlands: World Health Organization; 1998. Available from: http://www.who.int/medicines/library/dap/whodap-98-13/who-dap-98-13.pdf. Accessed August 12, 2022. [Google Scholar]
- 10.Bauchner H, Wise PH. Antibiotics without prescription: “bacterial or medical resistance”? E Lancet. 2000;355(9214):1480–1484. doi: 10.1016/S0140-6736(00)02160-7 [DOI] [PubMed] [Google Scholar]
- 11.Calabresi P, Cupini LM. Medication-overuse headache: similarities with drug addiction. Trends Pharmacol Sci. 2005;26(2):62–68. doi: 10.1016/j.tips.2004.12.008 [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-medication. Geneva: World Health Organization; 2000. [Google Scholar]
- 13.Bennadi D. Self-medication: a current challenge. J Basic Clin Physiol Pha. 2013;5(1):19–23. doi: 10.4103/0976-0105.128253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mouankié JB, Mazonga B, Abena AA. L’automédication chez l’adulte à Brazzaville. Sci Med Afr. 2011;3:459–463. [Google Scholar]
- 15.Ocan M, Bwanga F, Bbosa GS, et al. Patterns and predictors of self-medication in Northern Uganda. PLoS One. 2014;9(3):e92323. doi: 10.1371/journal.pone.0092323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Niwandinda F, Lukyamuzi EJ, Ainebyona C, Ssebunya VN, Murungi G, Atukunda EC. Patterns and practices of self-medication among students enrolled at mbarara university of science and technology in Uganda. Integr Pharm Res Pract. 2020;9:41. doi: 10.2147/IPRP.S237940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;323(18):1824–1836. [DOI] [PubMed] [Google Scholar]
- 18.Quincho-Lopez A, Benites-Ibarra CA, Hilario-Gomez MM, Quijano-Escate R, Taype-Rondan A. Self-medication practices to prevent or manage COVID-19: a systematic review. PLoS One. 2021;16(11):e0259317. doi: 10.1371/journal.pone.0259317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Independent T. COVID-19 pushes self-medication up. The Independent Uganda; 2021. Available from: https://www.independent.co.ug/covid-19-pushes-self-medication-up/. Accessed August 12, 2022. [Google Scholar]
- 20.Uganda warns against self-medication as COVID-19 cases surge—Xinhua. English.news.cn. (n.d.); 2022. Available from http://www.xinhuanet.com/english/africa/2021-06/15/c_1310009282.htm. Accessed August 12, 2022.
- 21.Uganda Bureau of Statistics. GeoHive; 2013.
- 22.City Population. Population of Cities and Towns. Available from:; 2016. Accessed August 15, 2022.
- 23.World Population Review. Uganda Population 2022. Available from: https://worldpopulationreview.com/countries/uganda-population. Accessed August 12, 2022.
- 24.Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version 3.01. Available from: http://openepi.com/SampleSize/SSPropor.htm. Accessed March 9, 2020.
- 25.Vizhi SK, Senapathi R. Evaluation of the perception, attitude and practice of self-medication among business students in 3 select Cities, South India. Int J Entrep Innov Manag Stud. 2010;1(3):40. [Google Scholar]
- 26.Montastruc JL, Bagheri H, Geraud T, Lapeyre-Mestre M. Pharmacovigilance of self-medication. Therapie. 1997;52:105–110. [PubMed] [Google Scholar]
- 27.Habeeb GE Jr, Gearhart JG. Common patient symptoms: patterns of self-treatment and prevention. J Miss State Med Assoc. 1993;34:179–181. [PubMed] [Google Scholar]
- 28.Pateh MM, Singh U, Sapre C, Salvi K, Shah A, Vasoya B. Self-medication practices among college students: a cross sectional study in Gujarat. National J Med Res. 2013;3(3):257–260. [Google Scholar]
- 29.Verma RK, Mohan L, Pandey M. Evaluation of self-medication among professional students in North India: proper statutory drug control must be implemented. Asian J Pharm Clin Res. 2010;3(1):60–64. [Google Scholar]
- 30.Goel DD. Self-medication patterns among nursing students in North India. IOSR J Dent Med Sci. 2013;11(4):14–17. doi: 10.9790/0853-1141417 [DOI] [Google Scholar]
- 31.Sawalha AF. Assessment of self-medication practice among university students in Palestine: therapeutic and toxicity implications. IUG J Nat Stud. 2007;15(2):67–82. [Google Scholar]
- 32.Corrˆ Ea da Silva G, Soares MCF, Muccillo-Baisch AL. Self-medication in university students from the city of Rio Grande, Brazil. BMC Public Health. 2012;12(1):339. doi: 10.1186/1471-2458-12-339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Esan DT, Fasoro AA, Odesanya OE, Esan TO, Ojo EF, Faeji CO. Assessment of self-medication practices and its associated factors among undergraduates of a Private University in Nigeria. J Environ Public Health. 2018;2018:e5439079. doi: 10.1155/2018/5439079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zewdie S, Andargie A, Kassahun H. Self-medication practices among Undergraduate University students in Northeast Ethiopia. Risk Manag Healthc Policy. 2020;13:1375–1381. doi: 10.2147/RMHP.S266329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Figueiras A, Caamano F, Gestal OJJ. Socio-demographic factors related to self-medication in Spain. Eur J Epidemiol. 2000;16(1):19–26. doi: 10.1023/A:1007608702063 [DOI] [PubMed] [Google Scholar]
- 36.Awad A, Eltayeb I, Matowe L, Thalib L. Self-medication with antibiotics and antimalarials in the community of Khartoum state, Sudan. J Pharm Pharmaceut Sci. 2005;8(2):326–331. [PubMed] [Google Scholar]
- 37.World Health Organization. Guidelines for Assessment of Drugs for Use in Self-Medication. World Health Organization (Regional office) Copenhagen; 1986. [Google Scholar]
- 38.Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218–227. doi: 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dyal SR, Valente TW. A Systematic review of loneliness and smoking: small effects, big implications. Subst Use Misuse. 2015;50(13):1697–1716. doi: 10.3109/10826084.2015.1027933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Niño MD, Cai T, Ignatow G. Social isolation, drunkenness, and cigarette use among adolescents. Addict Behav. 2016;53:94–100. doi: 10.1016/j.addbeh.2015.10.005 [DOI] [PubMed] [Google Scholar]
- 41.Chou KL, Liang K, Sareen J. The association between social isolation and DSM-IVmood, anxiety, and substance use disorders: wave 2 of the National epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2011;72(11):1468–1476. doi: 10.4088/JCP.10m06019gry [DOI] [PubMed] [Google Scholar]
- 42.Almasdy D, Sherrif A. Self-medication practice with nonprescription medication among University students: a review of the literature. Arch Pharma Pract. 2011;2(3):95–100. [Google Scholar]