Abstract
Background
The COVID-19 pandemic required mental health services around the world to adapt quickly to the new restrictions and regulations put in place to reduce the risk of transmission. As face-to-face contact became difficult, virtual methods were implemented to continue to safely provide mental health care. However, it is unclear to what extent service provision transitioned to telemental health worldwide.
Objective
We aimed to systematically review the global research literature on how mental health service provision adapted during the first year of the pandemic.
Methods
We searched systematically for quantitative papers focusing on the impact of the COVID-19 pandemic on mental health services published until April 13, 2021, in the PubMed, Embase, medRxiv, and bioXriv electronic bibliographic databases, using the COVID-19 Open Access Project online platform. The screening process and data extraction were independently completed by at least two authors, and any disagreement was resolved by discussion with a senior member of the team. The findings were summarized narratively in the context of each country’s COVID-19 Stringency Index, which reflects the stringency of a government’s response to COVID-19 restrictions at a specific time.
Results
Of the identified 24,339 records, 101 papers were included after the screening process. Reports on general services (n=72) showed that several countries’ face-to-face services reduced their activities at the start of the pandemic, with reductions in the total number of delivered visits and with some services forced to close. In contrast, telemental health use rapidly increased in many countries across the world at the beginning of the pandemic (n=55), with almost complete virtualization of general and specialistic care services by the end of the first year. Considering the reported COVID-19 Stringency Index values, the increased use of virtual means seems to correspond to periods when the Stringency Index values were at their highest in several countries. However, due to specific care requirements, telemental health could not be used in certain subgroups of patients, such as those on clozapine or depot treatments and those who continued to need face-to-face visits.
Conclusions
During the pandemic, mental health services had to adapt quickly in the short term, implementing or increasing the use of telemental health services across the globe. Limited access to digital means, poor digital skills, and patients’ preferences and individual needs may have contributed to differences in implementing and accessing telemental health services during the pandemic. In the long term, a blended approach, combining in-person and virtual modalities, that takes into consideration the needs, preferences, and digital skills of patients may better support the future development of mental health services. It will be required to improve confidence with digital device use, training, and experience in all modalities for both clinicians and service users.
Keywords: COVID-19, coronavirus, mental health services, telemental health, telepsychiatry, face-to-face
Introduction
At the start of the COVID-19 pandemic, mental health services around the world, along with health services in general, needed to adapt quickly to reduce the risk of infection and transmission while continuing to support those with mental health problems [1]. However, as identified early in the COVID-19 pandemic by the World Health Organization (WHO), the pandemic went beyond the physical threat to also affect mental health [2].
The link between COVID-19 and mental illness is increasingly supported by robust evidence. The association is bidirectional; mental illness increases the risk of subsequent COVID-19 infection, and the risk of a new mental health diagnosis increases up to 180 days following COVID-19 infection [3,4]. COVID-19 and related coronavirus infections, such as SARS and Middle East respiratory syndrome (MERS), are associated with increased subsequent risk of depression, anxiety, and other neuropsychiatric consequences, such as dysexecutive syndrome [5-7]. This is in addition to any indirect effects on mental health caused by restrictions and lockdowns imposed by the COVID-19 pandemic [8]. Unemployment, financial insecurity, and other socioeconomic effects of the COVID-19 pandemic also adversely impact mental health. Mental health consequences can occur both at the time of a crisis and afterwards [9]. For instance, it has been suggested that suicide rates in some countries may have a delayed increase as a consequence of the social, health, and economic disruption associated with the pandemic [9]. As the pandemic evolved, access to vaccines and their uptake have altered the pattern of infection [10], and therefore, restrictive measures adopted by public health institutions have changed [11]. Taken together, all these factors suggest that there will be a rise in mental health treatment needs, and this is likely to be long-lasting. Consequently, mental health services have also started to plan or implement measures to prepare for an anticipated increase in demand related both directly to COVID-19 infection and indirectly to the sequelae of its associated restrictions.
During the pandemic, the WHO proposed that the goals of mental health care services need to focus not only on responding to the acute mental health emergency, but also on recovery thereafter and preparations for future emergencies [2]. How and to what extent this has happened is yet to be seen.
In contrast to the volume of data on the mental health impact of COVID-19, there have been few systematic considerations of the response of mental health services. Some reports reflect consultation with experts and service users to consider what changes in services might be needed to meet the mental health consequences of COVID-19 [12]. Organizations, such as the WHO, have suggested an integrated approach including mental health and psychosocial support in the COVID-19 response [2], while the United Nations has highlighted the need for changes and investment immediately to reduce mental health effects later [13].
Preliminary data from a WHO survey suggested a considerable detrimental impact on mental health services [14], with telemental health (TMH) considered critical to maintaining delivery of mental health services in response to pandemic-related social distancing measures and confinements [15]. Prompted by this, several countries modified national telemedicine regulations to promote its spread [16]. However, it is unclear whether the apparently rapid transition to TMH observed in many high-income countries [1] has occurred globally, which services have been affected, and whether this change has been sustained through the different phases of the pandemic.
To understand the degree to which service provision has changed during the first year of the pandemic and the extend of the transition to TMH in different countries, we systematically reviewed the available literature on mental health services during the pandemic. We also assessed these changes across the different phases of the COVID-19 pandemic and in the context of the local restrictions imposed.
Methods
Overview
We performed a systematic review of studies describing the impact of the COVID-19 pandemic on mental health services up to 1 year after the pandemic declaration on March 11, 2020 [17]. This is part of a wider assessment of the impact of the COVID-19 pandemic across the mental health field (previously published protocol for the full project is available on PROSPERO, CRD42020178819) [18].
Search Strategy and Screening Process
The search strategy for the full project (see above) included terms relating to mental health and the COVID-19 pandemic, SARS, and MERS, with specific and generic specifiers (eg, Medical Subject Headings [MeSH] terms; for full details, see Multimedia Appendix 1). We searched PubMed, Embase, medRxiv, and bioXriv electronic bibliographic databases using the COAP (COVID-19 Open Access Project) online platform [19] for relevant reports from inception until April 13, 2021. Records on SARS and MERS were independently searched on PubMed and Embase from inception to April 13, 2021.
At least two members of the review team (CZ, EGO, GR, JSWH, KR, KAS, OM, or RS) independently screened the title and abstract of the retrieved records. Full texts of the potentially eligible records were then independently assessed against the eligibility criteria. Any disagreement about eligibility was discussed with a third member of the research team (AC, AP, CV, or KH). The included articles and relevant systematic reviews were also screened for references to identify additional records. References from all sources were cross-checked to ensure that all referenced documents had been searched.
Eligibility Criteria
To examine the consequences of the COVID-19 pandemic on mental health services, we included only reports providing quantitative data on changes in service organization and delivery (eg, how services were delivered: remote versus face to face; the number of patients accessing the service) and the creation of new services (eg, ad hoc created digital technologies and TMH) to overcome the challenges related to the COVID-19 pandemic. Documents solely reporting diagnostic aspects (eg, differential rates of two or more subgroups of mental health diagnoses accessing the service and frequency of mental health symptoms during the pandemic) were excluded, as these data describing part of a service do not provide information about the overall level of activity of a service. We included all types of primary research reports (randomized studies, observational studies, case reports, etc) focusing on mental health services and coronaviruses. No time or language restriction was applied.
Data Extraction
Data extraction was performed independently by at least two reviewers (CZ, EGO, GR, JSWH, KR, KAS, OM, or RS). Relevant data on country of origin, data collection period, service delivery method (ie, face-to-face or TMH), and service provision were extracted from the included papers. We categorized the identified records according to the following categories: randomized controlled trials, cohort studies, before-and-after studies, case-control studies, case reports/case series, and survey/audit. For each paper, we also extracted the key quantitative findings and collected them in a descriptive summary.
COVID-19 Stringency Index
Given that several waves of infections and consequent restrictions related to the COVID-19 pandemic affected different countries at different times, we considered the timing of the study period of the individual studies to be of limited use in contextualizing findings locally. Instead, we reported findings in the context of the country-specific COVID-19 Stringency Index, a composite measure developed within the Our World in Data project by the Global Change Data Lab (a nonprofit organization) and the University of Oxford [20] to reflect the stringency of a government’s response to COVID-19 restrictions at any specific time. The score is based on 9 response indicators, including school closures, workplace closures, and travel bans, rescaled to a value from 0 to 100 (where 100 is the strictest measure of response). This is therefore a dynamic measure, capturing changes in a country’s policies at any point throughout the pandemic. Where policies vary within a particular country, the index reflects the response level of the strictest subregion [11]. For each individual study, we report the minimum and maximum Stringency Index score for the relevant time period. The country-specific graphical representation of the COVID-19 Stringency Index starting from January 2020 can be accessed online [20].
Results
Overview
We identified a total of 24,339 records, and the number reduced by 3699 records after the removal of duplicates. After the abstract and full-text screening, an additional 20,539 records were excluded (Multimedia Appendix 2). A total of 101 papers were therefore included in the review. Of these, 60 were before-and-after studies, 23 were case reports and case series, and 18 were cross-sectional surveys. A summary of the 101 included articles is reported in Multimedia Appendix 3. Overall, the studies were concentrated in high-income countries, with the majority in Europe (39.6%) and North America (29.7%) (Multimedia Appendix 4).
Face-to-Face Mental Health Services
Of the 101 articles, 72 reported data on face-to-face mental health services. A total of 52 of these were before-and-after studies, 7 were case reports and case series, and 14 were cross-sectional surveys. Regionally, 31 studies reported data from Europe, 20 from North America, 1 from South America, 11 from Asia, and 9 from Australia (Multimedia Appendix 5). No studies reported quantitative data from low-income countries, and none were from the African subcontinent. As shown in Multimedia Appendix 3, several studies reported a reduction in face-to-face visits [21,22] and emergency department presentations [23], with a reduction in the activity of specialized settings, such as electroconvulsive therapy clinics [24-27]. Data on hospitalizations were less clear, with some studies reporting evidence of a reduced number of admissions (eg, [28,29]), others reporting evidence of a rapid increase in admissions soon after the pandemic onset (eg, [23,30]), and still others reporting no differences compared to the same period in the previous year (eg, [31,32]).
TMH Services
Table 1 [33-84] summarizes the characteristics of the subgroup of 55 articles reporting data on TMH services, which includes 23 before-after studies, 19 case reports or case series, and 13 cross-sectional surveys. Most of the collected data within these primary sources refer to the timeframe between January and October 2020, with most focusing on the period around March 2020.
Table 1.
Characteristics of the included studies on telemental health (N=55).
| Study ID (authors, year) | Study design | Study setting | Country | Study period | Stringency Index, value or range | |||
|
|
|
|
|
Start date | End date |
|
|
|
| Arendt et al, 2020 [33] | Before-after study | Crisis hotline services for the general population | Germany and Austria | January 1, 2020 | April 20, 2020 | 0.00-81.48 |
|
|
| Beran et al, 2020 [34] | Before-after study | A large, academic, consultation-liaison service | United States | January 2, 2020 | June 6, 2020 | 5.56-72.69 |
|
|
| Berthaut and Chamignon, 2021 [35] | Descriptive study | A health care and education center for adolescents | France | March 17, 2020 | May 18, 2020 | 76.85-87.96 |
|
|
| Cantini et al, 2020 [36] | Descriptive study | A psycho-oncology unit | Italy | March 3, 2020 | June 3, 2020 | 67.59-93.52 |
|
|
| Carpiniello et al, 2020 [37] | Survey | 71 departments of mental health and 107 psychiatric wards in general hospitals | Italy | April 1, 2020 | April 11, 2020 | 85.19-87.96 |
|
|
| Connoly et al, 2020 [38] | Before-after study | The Department of Veterans Affairs | United States | March 11, 2020 | April 22, 2020 | 21.76-72.69 |
|
|
| Datta et al, 2020 [39] | Before-after study | An eating disorder multidisciplinary unit | United States | March 1, 2020 | May 31, 2020 | 8.33-72.69 |
|
|
| Garcia-Huidobro et al, 2020 [40] | Before-after study | A large private academic health network | Chile | March 1, 2020 | April 30, 2020 | 0.00-73.15 |
|
|
| Ghiretti et al, 2020 [41] | Descriptive study | A free telephone-based psychological support service | Italy | March 18, 2020 | June 3, 2020 | 67.59-93.52 |
|
|
| Ghosh et al, 2021 [42] | Before-after study | An outpatient service for substance use disorder | India | May 18, 2020 | August 31, 2020 | 81.94-87.50 |
|
|
| Graell et al, 2020 [43] | Before-after study | A hospital outpatient service | Spain | March 16, 2020 | May 10, 2020 | 68.98-85.19 |
|
|
| Grover et al, 2020 [26] | Survey | 109 private and public mental health services | India | May 1, 2020 | May 18, 2020 | 81.94-96.30 |
|
|
| Grover et al, 2020 [27] | Survey | 396 private mental health services | India | May 1, 2020 | May 15, 2020 | 81.94-96.30 |
|
|
| Guinart et al, 2021 [44] | Survey | 818 mental health care professionals | United States | April 1, 2020 | May 31, 2020 | 72.69 |
|
|
| Hall and Sukhera, 2020 [45] | Descriptive study | A virtual emergency psychiatric consultation service | Canada | Unknown | Unknown | Unknown |
|
|
| Hames et al, 2020 [46] | Survey | 93 clinic directors or designated representatives of the Association of Psychology Training Clinics | United States | March 11, 2020 | March 31, 2020 | 21.76-72.69 |
|
|
| Harrison et al, 2020 [47] | Descriptive study | A telephone-based program to address substance abuse within emergency departments | Canada and United States | Unknown | Unknown | Unknown |
|
|
| Hazarika et al, 2021 [48] | Survey | A psychological helpline for the general population | India | April 7, 2020 | April 24, 2020 | 96.30-100.00 |
|
|
| Hoffnung et al, 2021 [49] | Before-after study | A community behavioral health center | United States | January 1, 2020 | June 30, 2020 | 0.00-72.69 |
|
|
| Humer et al, 2020 [50] | Before-after study | 338 health care professionals | Germany, Czech Republic, and Slovakia | March 24, 2020 | May 20, 2020 | 54.63-87.04 |
|
|
| Johnson et al, 2020 [51] | Survey | 2180 mental health care workers | United Kingdom | January 1, 2020 | May 1, 2020 | 0.00-72.69 |
|
|
| Karim et al, 2020 [52] | Before-after study | Mental health outpatient services in Qatar | Qatar | March 1, 2020 | June 30, 2020 | 13.89-86.11 |
|
|
| Khanra et al, 2021 [53] | Descriptive study | A large psychiatric hospital | India | April 1, 2020 | September 30, 2020 | 81.94-100.00 |
|
|
| Lian et al, 2020 [54] | Before-after study | A hospital-based psychological counseling program | China | January 23, 2020 | June 30, 2020 | 44.91-81.94 |
|
|
| Looi et al, 2020 [55] | Before-after study | Private psychiatric consultation services in Australia | Australia | April 1, 2020 | June 30, 2020 | 62.04-73.15 |
|
|
| Looi et al, 2020 [56] | Before-after study | Psychiatric consultation services in Australian rural settings (Australian Capital Territory, Northern Territory, South Australia, and Tasmania) | Australia | April 1, 2020 | May 31, 2020 | 64.35-73.15 |
|
|
| Looi et al, 2020 [57] | Before-after study | Private psychiatric consultation services in New South Wales, Queensland, Victoria, and Western Australia regions | Australia | April 1, 2020 | May 31, 2020 | 64.35-73.15 |
|
|
| Looi et al, 2021 [58] | Before-after study | Private psychiatric consultation services in Australia | Australia | July 1, 2020 | September 30, 2020 | 68.06-75.46 |
|
|
| Lunsky et al, 2021 [59] | Survey | 942 direct support professionals working with people with intellectual and development disabilities | Canada | July 2, 2020 | August 10, 2020 | 67.13-68.98 |
|
|
| Mehtani et al, 2021 [60] | Descriptive study | A telephone-based program for people with substance use disorders staying at San Francisco’s COVID-19 isolation and quarantine site | United States | April 10, 2020 | May 25, 2020 | 72.69 |
|
|
| Mishkind et al, 2020 [61] | Descriptive study | An outpatient clinic | United States | March 2, 2020 | April 10, 2020 | 11.11-72.69 |
|
|
| Moreland et al, 2021 [62] | Before-after study | An outpatient service for mental health and substance use treatment to pregnant and postpartum women | United States | March 1, 2020 | May 31, 2020 | 8.33-72.69 |
|
|
| Myers Virtue et al, 2021 [63] | Descriptive study | A psychosocial oncology service | United States | March 1, 2020 | September 30, 2020 | 8.33-72.69 |
|
|
| Naik et al, 2021 [64] | Descriptive study | An outpatient service | India | March 25, 2020 | May 31, 2020 | 81.94-100.00 |
|
|
| Peppou et al, 2020 [65] | Descriptive study | A helpline for the general population | Greece | March 22, 2020 | April 13, 2020 | 74.04-84.26 |
|
|
| Peralta et al, 2020 [66] | Descriptive study | A counseling service for the general population | Dominican Republic | March 25, 2020 | May 17, 2020 | 92.59-100.00 |
|
|
| Perricone et al, 2021 [67] | Descriptive study | A national psychological counseling service | Italy | April 1, 2020 | June 30, 2020 | 67.59-93.52 |
|
|
| Pierce et al, 2020 [68] | Survey | 2619 psychologists | United States | May 11, 2020 | May 25, 2020 | 72.69 |
|
|
| Prior, 2020 [69] | Descriptive study | A psycho-oncology unit | Italy | Unknown | Unknown | Unknown |
|
|
| Probst et al, 2020 [70] | Survey | 1547 psychotherapist | Austria | March 24, 2020 | April 1, 2020 | 81.48 |
|
|
| Rainwater et al, 2020 [71] | Before-after study | An outpatient service for consultation and counseling of cancer patients | United States | April 1, 2020 | September 30, 2020 | 62.50-72.69 |
|
|
| Ravindran et al, 2020 [72] | Descriptive study | A national helpline for the general population | India | Unknown | Unknown | Unknown |
|
|
| Rosen et al, 2020 [73] | Before-after study | The Veterans Health Administration – the largest integrated service in the United States | United States | January 1, 2020 | June 30, 2020 | 0.00-72.69 |
|
|
| Salum et al, 2020 [74] | Descriptive study | A community mental health service | Brazil | March 23, 2020 | March 23, 2020 | 71.76 |
|
|
| Sampaio et al, 2021 [75] | Survey | 768 mental health professionals | United States | April 24, 2020 | May 18, 2020 | 72.69 |
|
|
| Sharma et al, 2020 [76] | Descriptive study | A large child psychiatry department | United States | February 28, 2020 | April 3, 2020 | 5.56-72.69 |
|
|
| Singh Bhandari, 2020 [77] | Descriptive study | An outpatient clinic | India | March 25, 2020 | May 26, 2020 | 81.94-100.00 |
|
|
| Staples et al, 2020 [78] | Before-after study | A national digital mental health service for people experiencing anxiety and depression | Australia | March 19, 2020 | June 10, 2020 | 44.44-73.15 |
|
|
| Steeg et al, 2021 [79] | Before-after study | General practice services in England | United Kingdom | March 10, 2020 | June 10, 2020 | 11.11-79.63 |
|
|
| Stewart and Broadbent, 2020 [22] | Before-after study | A large mental health service | United Kingdom | February 16, 2020 | April 16, 2020 | 11.11-79.63 |
|
|
| Stewart et al, 2020 [80] | Before-after study | A large mental health service | United Kingdom | February 1, 2020 | May 15, 2020 | 11.11-79.63 |
|
|
| Vonderlin et al, 2021 [81] | Descriptive study | A hotline for psychological first aid for the general population | Germany | April 22, 2020 | July 24, 2020 | 55.09-76.85 |
|
|
| Yaffa et al, 2021 [82] | Before-after study | An eating disorder treatment center for adolescents | Israel | January 1, 2020 | October 31, 2020 | 0.00-94.4 |
|
|
| Zhong et al, 2020 [83] | Survey | 108 Chinese residents | China | January 27, 2020 | February 2, 2020 | 69.91-77.31 |
|
|
| Zulfic et al, 2020 [84] | Survey | A community outpatient service | Australia | Unknown | Unknown | Unknown |
|
|
The world distribution of the studies on TMH services (Figure 1) showed a higher representation in North America (n=18) and Europe (n=16, including 19 countries), while fewer articles reported data from Central or South America, Asia, and Australia. No studies reported quantitative data from low-income countries, and none were from the African subcontinent.
Figure 1.
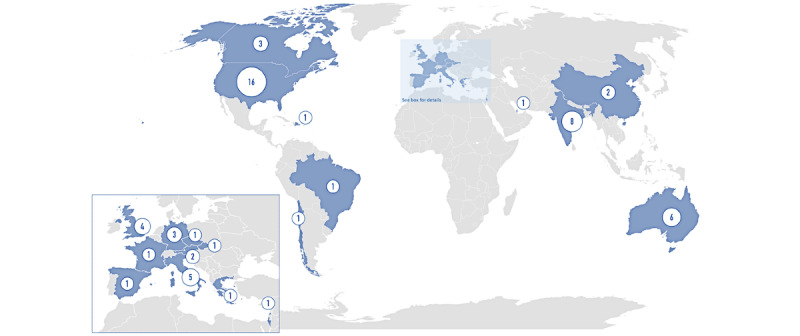
The distribution of articles reporting data on telemental health. Values in the circles indicate the number of articles.
The key findings of included papers involving the impact of COVID-19 on the use of TMH are shown in Textbox 1. Overall, studies set in 19 countries reported the implementation of TMH services locally at the beginning of the pandemic. They include inpatient and outpatient services (eg, [71]), specialized services (eg, [38,82]), adolescent services (eg, [82]), and services in both private and public sectors (eg, [27]). For those services in which TMH was already available, an increase in its use during the pandemic was reported in several countries (eg, [21,50,70]). The specific COVID-19 Stringency Index chart for each country throughout the pandemic can be accessed online [20].
Telemental health services around the world. The specific COVID-19 Stringency Index chart for each country can be accessed online [20].
Asia
China
Before-after study
• A newly created hospital-based psychological counseling program in China served 474 users (7 users per day) during the lockdown, and the number reduced to 162 (2 users per day) after April 2020 [54].
Survey/audit
• 42.6% of 108 survey respondents who received a psychiatric consultation during lockdown attended an internet-based service (n=46), 37.0% attended a face-to-face visit (n=40), and 20.4% attended a telephone-based service (n=22) [83].
India
Before-after study
• In India, a telemedicine-assisted stepped-care outpatient service for substance use disorder was developed and started on the May 18, 2020. By August 31, 2020, 160 new and 219 follow-up patients were registered in the teleaddiction service. Among them, 128 (80%) and 198 (90.2%) patients received teleconsultations, respectively [42].
• Compared to the same period of 2019, the number of patients seen in a psychiatric outpatient service for patients with substance abuse dropped (May: 170 vs 22; June: 351 vs 43; July: 467 vs 44; August: 436 vs 51) [42].
Descriptive study
• A local newly created psychological helpline received 239 calls over the 18 days of lockdown (April 7-24, 2020) [48].
• The Indian Government helpline received 20,475 calls during the first month of activity [72].
• An outpatient service in India created a new telephone outpatient service and delivered 60.1% of the planned follow-up visits using telehealth (1049 of 1748) in the first 2 months of lockdown [64].
• During the first months of the lockdown, a team of psychiatrists of an Indian hospital made 78 teleconsultations with new and followed-up patients. In 6 cases, the patients were referred to their local hospital for further face-to-face assessment [77].
• In a large psychiatric hospital in India, 168 consultations were made using telepsychiatry between April and September 2020. The number of teleconsultations during lockdown was positively correlated with travel cost savings (ρ=0.47, P<.01) and time savings (ρ=0.49, P<.01) [53].
Survey/audit
• A survey comparing the services in both public and private institutes during the lockdown period in India (n=109) showed that telecommunication service use increased from 19.3% to 45.9% comparing the period before and during the pandemic [26].
• A survey evaluating the services in the private sector provided during the lockdown period in India (n=396) showed that telecommunication service use increased from 26.3% to 52.0% comparing the period before and during the pandemic [27].
Israel
Before-after study
• In an eating disorder treatment center for adolescents, telemedicine meetings comprised 37% of all sessions during January to October 2020 (2193 sessions), while they were not used during the respective period between 2015 and 2019 [82].
Qatar
Before-after study
• Analyzing data on the number of visits in the mental health outpatient setting in Qatar in the 4 months following the introduction of telepsychiatry (March-June 2020), the total number of individuals accessing mental health services (both face-to-face and telepsychiatry) increased by approximately 36.5% compared to the same period in 2019 (22,086 and 16,175 cases, respectively) [52].
Australia
Australia
Before-after study
• The use of the MindSpot Clinic, a national digital mental health service (DMHS) providing services to people experiencing anxiety and depression, increased by 16.7% (mean number of assessments per week=455) during the pandemic (March 19 to June 10, 2020) compared to the period between September 1 and September 28, 2019 (390 assessments per week) [78].
• Comparing data on private psychiatrists’ visits held in April-June 2020 and the same period in 2019 in Australia, the number of psychiatry consultations (telehealth and face-to-face) rose during the pandemic by 14%, with telehealth representing nearly half of this total. Face-to-face consultations in 2020 were only 56% of the comparative number of 2019 consultations. Most telehealth involved short telephone consultations of ≤15-30 min. Video consultations comprised 38% of total telehealth provision [55].
• Comparing data on visits held in Australian rural settings (Australian Capital Territory [ACT], Northern Territory [NT], South Australia [SA], and Tasmania [TAS]), the overall rate of consultations (face-to-face and telehealth) increased during March and April 2020, compared to the monthly face-to-face consultation average of July 2018 to June 2019, except TAS (ACT: 1724 in April, increased 114%; 2061 in May, increased 136%; NT: 296 in April, increased 108%; 337 in May, increased 123%; SA: 12,864 in April, increased 116%; 12,876 in May, increased 116%; TAS: 1886 in April, reduced 85%; 2189 in May, reduced 98%). For total video and telephone telehealth consultations combined, video consultations were lower in April 2020 and higher in May 2020 [56].
• The total combined use of telehealth and face-to-face private psychiatric consultation services in New South Wales, Queensland, Victoria, and Western Australia regions (Australia) in April and May 2020 increased by 10%-20% of the average monthly face-to-face consultations in the 2018/19 financial year [57].
• Comparing data on private psychiatrists’ visits held in July-September 2020 and the same period of 2019 in Australia, the number of psychiatry consultations (telehealth and face-to-face) rose during the pandemic by 14%, with telehealth representing 43% of this total. Face-to-face consultations in 2020 were only 64% of the comparative number of 2019 consultations. Most telehealth involved short telephone consultations of ≤15-30 min. Video consultations comprised 42% of total telehealth provision [58].
Survey/audit
• An audit of 314 community patients to examine the potential implications of telephone support found that 21 (7%) did not have access to a phone, and a further 58 (18%) were reported by the original authors as “unreliable in responding to contact over the phone based on past clinician experience.” Moreover, during the first wave, regular face-to-face reviews were necessary for a group of patients, including 91 patients (29%) treated with depot medications, and 71 (23%) taking clozapine [84].
Europe
Austria
Survey/audit
• During the lockdown, the number of patients treated daily via telephone increased from 0.42 ± 3.01 to 4.53 ± 5.77 (+979%, P<.001), and via internet from 0.18 ± 1.35 to 2.99 ± 4.44 (+1561%, P<.001) [70].
Austria and Germany
Before-after study
• The number of crisis hotline calls increased during lockdown in both Austria and Germany [31].
Czech Republic, Germany, and Slovakia
Survey/audit
• A survey on 338 health care professionals showed that the number of patients treated via telephone increased from 0.92 ± 3.16 to 3.28 ± 5.22 per week (+257%, t −8.717, P<.001), and the number of patients treated via the internet increased from 0.59 ± 2.54 to 5.83 ± 6.82 per week (+888%, t −15.346, P<.001) during the 2-month period of confinement [50].
France
Descriptive study
• During lockdown, a health care and education center for adolescents that provides long-term psychiatric care, created a virtual ward using Discord, a platform used to communicate using chat, calls, and video calls, to ensure continuity of care. Of the 38 patients who used this service, only 6 withdrew early [33].
Germany
Descriptive study
• A total of 1292 telephone consultations were made by a telephone hotline for psychological first aid for COVID-19–related burden in 4 months covering a period during and after the German lockdown. In 42% of all consultations, a short therapeutic intervention was performed; in 26%, psychotherapeutic treatment was recommended; and in 11%, referral to other specialized telephone services was made [81].
Greece
Descriptive study
• In a report from a mental health helpline service in Greece during lockdown, most calls pertained to the quarantine (n=482, 83.7%) and more specifically to feelings of “restraint” (56%) and “loneliness” (53%) [65].
Italy
Descriptive study
• In Emilia Romagna region (Italy), a free telephone-based psychological support service was established during lockdown, receiving 312 calls in the first 11 weeks of activity [41].
• A national telephone psychological counseling service established during the COVID-19 pandemic had 193 users between April and June 2020 [67].
• A psycho-oncology unit reported having treated 28 cancer patients, 9 caregivers, and 7 family members during April-September 2020, switching from face-to-face visits to virtual consultations [36].
• In Treviso (Italy), the oncology unit switched their psychological monitoring to a virtual modality during the pandemic. In the first 9 weeks, they conducted 123 online visits (12% were video calls using Google Hangouts, and 88% were telephone calls) [69].
Survey/audit
• Data from 71 departments of mental health and 107 psychiatric wards in general hospitals showed that during the lockdown (April 2020), scheduled psychiatric consultations, both at home and on-site, went ahead for selected cases, being replaced in approximately 75% of cases by scheduled remote contact, mainly telephone calls (100%), video calls (67%), or emails (19%), with 41% of units adopting all these means of contact [37].
Spain
Before-after study
• During the early COVID-19 pandemic (March-May 2020) in a hospital in Madrid, out of 1818 outpatient consultations carried out, 1329 (73.10%) were delivered by telephone or videoconferencing and 489 (26.9%) were face-to-face, corresponding to 365 patients who were receiving treatment at the time in the outpatient clinic or day hospital [43].
United Kingdom
Before-after study
• The likelihood of receiving a remote general practitioner/practice nurse consultation within 3 months of a self-harm episode was higher in the COVID-19 pandemic (67.7%; March-April 2020) than in the prepandemic period (32.3%; ratio 2.10, CI 2.05-2.15; same period of 2010-2019). The overall likelihood of having a general practitioner/practice nurse consultation was slightly lower (80.3% vs 83.2%; ratio 0.97, CI 0.96-0.98) [69].
• Comparing the 31-day periods before and after March 16, 2020 (lockdown announcement), virtual contacts increase by 117% compared to a 3%-22% reduction observed comparing the same periods between 2015 and 2019 [25].
• Comparing the period before March 16 to that between March 16 and May 15, 2020, virtual contacts with community mental health teams increased from 154 ± 17 to 380 ± 97 (+147%). In the same period, mean virtual contacts increased by 102.7% (26.7 ± 7.3 vs 54.2 ± 14.8) and mean total contacts reduced by 24.9% (161.9 ± 30.7 vs 121.5 ± 26.1). Daily caseloads reduced by 2.1% (8729 ± 24 vs 8539 ± 124) and by 26.4% (221.8 ± 8.5 vs 163.3 ± 20.0) [80].
Survey/audit
• During the first COVID-19 wave, 61.1% of 2180 mental health care workers in the United Kingdom rated the adoption of new digital ways of working as “very or extremely important” in the management of the impact of COVID-19 at work [51].
North America
Canada
Descriptive study
• In Ontario, the implementation of a virtual emergency psychiatric consultation service (ie, Emergency Diversion Clinic) during the pandemic allowed provision of consultations for 60% of all youth presenting to the emergency department for a mental health issue. After the assessment, 56% of patients were linked to community mental health support [45].
Survey/audit
• A Canadian survey of direct support professionals (n=942) working during the pandemic with people with intellectual and development disabilities, showed that the majority of them completed telephone-based visits (n=549, 58%), and only 22% (n=204) made at least one videocall. A total of 225 (24%) responders attended at least one face-to-face visit [59].
Canada and United States
Survey/audit
• In March 2020, an online survey involving 93 clinic directors or designated representatives of the Association of Psychology Training Clinics mainly in the United States (n=89) and Canada showed that 23.7% (n=22) were forced to close face-to-face clinics and discontinue services, at least temporarily. Of those that remained open for services, 61 training clinics (65.6% of the total sample, 86% of those that remained open) reported that their sites remained open primarily using telepsychology [46].
United States
Before-after study
• Psychiatric consultations and patient volume in North Carolina decreased with the onset of the pandemic (March 2020) by 66.9% and 25.2%, respectively. After the introduction of video consultations, psychiatric consultations were 39.1% lower compared to prepandemic data [34].
• Daily telemental health visits to the Department of Veterans Affairs rose from 1739 to 11,406 (+556%) in the weeks following the pandemic declaration (March 2020). Daily in-person encounters fell from 57,296 to 10,931 (−81%) [38].
• In an American eating disorder multidisciplinary unit, the yearly average inpatient census by month changed from 31.92 (SD 5.33; before the COVID-19 pandemic) to 19.33 (SD 4.5; March 2020 to May 2020) (59% of the usual census), owing to the implementation of telehealth strategies in most aspects of the services (eg, new admission evaluation, psychotherapy, and group therapy) [39].
• After the onset of COVID-19 (April-May 2020), the average monthly utilization of telehealth services within the Medical University of South Carolina’s Women’s Reproductive Behavioral Health Program (which provides outpatient mental health and substance use treatment to pregnant and postpartum women within obstetric practices) increased by 90% compared to the data prior to the pandemic [62].
• Comparing delivery of telemental health services in New York (USA) before, during, and after the lockdown, there was a tendency for adult patients (n=1115, 21,131 sessions) to prefer telehealth compared to children (n=1374, 22,163 sessions) (P<.001). In this service, telehealth was implemented in March 2020 (onset of lockdown) but patients returned to prefer face-to-face visits when in-person services resumed in May and June 2020 (χ2=21.745, P<.01) [49].
• Data were compared for the number of mental health consultation visits made by cancer patients face-to-face in April-September 2019 and both face-to-face and virtually in April-September 2020. In 2020, the number of inpatient consultations (330 vs 623), referrals (127 vs 175), and outpatient visits (448 vs 550) decreased. Of the outpatient visits, 359 were telephone contacts, 69 were video visits, and only 20 were in person [71].
• Data from the Veterans Health Administration (VHA), the largest integrated health care system in the United States, showed that before the pandemic (October 2019 to February 2020), VHA had 1.5 to 1.8 million visits per month, of which 85% were in-person visits, 11% were by telephone, and 5% were by video. The use of telepsychiatry increased with the pandemic, and in June 2020, there were 1.5 million visits, of which 19% were in person, 59% were by telephone, and 20% were by video [73].
Descriptive study
• During March 2020, a large child psychiatry department registered an overall reduced number of study visits (645 vs 358) over a 1-month period, with a shift toward phone and home-based telemental health (n=171 and n=160, respectively), compared to in-person visits (n=27) [76].
• In the 2 weeks before the implementation of the “Addiction Telehealth Program” (ATP) in April 2020, which is a telephone-based program to reduce treatment access barriers for people with substance use disorders staying at San Francisco’s COVID-19 isolation and quarantine site, the program received 10 calls from other health care providers, whereas in the 6 weeks after the implementation (April 10-May 25, 2020), there were 59 consultations for the isolation and quarantine site [60].
• Data from the Johnson Depression Center and the Steven A. Cohen Military Family Clinic at the University of Colorado Anschutz Medical Campus showed that the change to telemental health helped reduce no-show rates from 11.4% (n=57) in the 2 weeks before the pandemic (March 2-13, 2020) to 7.8% (n=38) after implementation of telehealth (March 30-April 10, 2020). In the following months (April-September 2020), the no-show rate was stable, with a rate between 5.5% and 8.5%, and a 26.2% increase in overall completed visits [61].
• During the first wave (March-September 2020), a psychosocial oncology service in the United States continued to provide visits through telepsychology for 93% of established patients (n=85), while 4 patients left the service and 2 patients preferred to wait for the reintroduction of face-to-face visits. The service also received 263 new referrals and delivered a first visit for 50.6% (n=133), with 82% (n=109) as digital visits and 18% (n=24) as face-to-face visits [63].
• In New York, a telephone-based model was implemented during the pandemic to continue to address substance use within emergency departments (SBIRT program). In 13 weeks, there were 228 incoming calls, 190 outgoing calls, and 4 voicemails processed. Moreover, 108 (26%) calls were with patients, 13 (3%) with family/friends, 224 (53%) with staff members, and 79 (19%) with treatment providers [47].
Survey/audit
• Of the 818 mental health care professionals in the United States who reported using telepsychiatry during the pandemic (April-May 2020), 500 (61%) used both video and telephone, 273 (33%) used only telephone, and 45 (6%) used only video. Among the advantages cited, flexible scheduling or rescheduling, timely appointment starts, and lack or reduction of no-shows were reported. Among the raised concerns, there were technical difficulties and difficult access to video platforms, forcing the provider and patient to conduct visits telephonically despite both parties preferring 2-way video [44].
• A survey of psychologists showed that the use of telepsychology increased with the pandemic, compared to data prior to the pandemic (before January 2020), from 7.07% (SD 14.86) to 85.53% (SD 29.24) of the total activity [68].
• In a survey about the use of telepsychology, data showed that most therapists who already used telepsychology before COVID-19 reported an overall increase in requests for therapy services from current patients (36.5%), whereas 41% of those who had started to use telepsychology during the pandemic reported an overall decrease. Both groups reported a decrease in the number of requests from new clients (45% and 53%, respectively) [75].
Central and South America
Brazil
Descriptive study
• In a community mental health service in Brazil, telephone contact was possible for 61% of 154 treated patients, with 29% being advised face-to-face visits through regular service attendance, and around 7% of service users were unable to be contacted, despite several attempts [74].
Chile
Before-after study
• During the early pandemic, a large private academic health network implemented a new telemental health service. In Santiago, the number of visits delivered during this period via telepsychiatry was comparable to the 24.7% of visits delivered in 2019 by the face-to-face service [40].
Dominican Republic
Descriptive study
• In Santo Domingo, a team of volunteers consisting of 598 psychologists and 70 psychiatrists provided telephone counseling during the pandemic. In the period from March 25 to May 17, 2020, they conducted 6800 phone interventions [66].
Several studies reported the creation of helplines both locally and within national programs in several countries to provide psychiatric and psychological help to the general population (eg, [48,65,67,72]).
Discussion
Principal Findings
Our systematic review found that face-to-face delivery of mental health services was reduced at the start of the pandemic period, with a reduction in the total number of delivered visits and few mental health services forced to close. To meet mental health needs, the use of TMH rapidly increased across high-income countries and low- and middle-income countries at the beginning of the pandemic, with almost complete virtualization of many services by the end of the first year. To the best of our knowledge, this is the first review that, using a preplanned systematic approach, has collected quantitative reports on the extent to which the COVID-19 pandemic impacted mental health services internationally. Moreover, in presenting findings within the context of the relevant COVID-19 Stringency Index, service changes can be understood in the context of how strict national restrictions were throughout the pandemic.
At the beginning of the pandemic, TMH was increasingly adopted by mental health services to overcome the challenges related to COVID-19 restrictions, with a steep rise during the confinement period and, in general, during periods when the COVID-19 Stringency Index was higher. In some settings, this implementation was followed by a greater number of total health care consultations than in previous years, when the only option was face-to-face visits (eg, [34,52,55-58]). Moreover, it also involved specific and specialist (tertiary) mental health service provisions, such as emergency department or services dedicated to postpartum women and patients with cancer. This adaptation was essential to continue following up patients who may have been considered at high risk or as a vulnerable category during the pandemic due to their specific conditions.
The transition to the use of TMH was reported across high- and middle-income countries, but there were no studies from low-income countries. TMH provision has great potential in low-and middle-income countries due to large geographical distances and limited availability of mental health services to cover the population needs [85], combined with reduced health system capacity during the COVID-19 pandemic [86]. However, very few studies quantitively assessed the impact of the COVID-19 pandemic in middle-income countries (Iran, Turkey, Dominican Republic, India, China, and Brazil) and none assessed the impact specifically in low-income or African subcontinent countries. This is despite reports of the rollout of TMH in African nations to provide quicker and more extensive access to mental health services [87]. Additionally, models of service transformation in high-income countries may be difficult to replicate or be less relevant in these settings [88]. Clearly, quantitative data are needed to understand the impact of the COVID-19 pandemic on mental health services and longer-term changes, both positive and negative, in low- and middle-income countries [89].
Although some services provided evidence of a gradual shift back to face-to-face contact with a reduction in the COVID-19 Stringency Index (eg, after the initial lockdown period), virtual delivery methods continued to be used more than in the prepandemic period and, in some cases, remained the method for the majority of patients. This may not have been universal across all services and may have varied with patient preferences and specific characteristics. For example, a US study found that telehealth was less preferred for children after the confinement period compared to adults due to difficulties delivering therapy to them remotely [49]. Moreover, findings indicated that TMH was favored for psychiatric consultations and support services, but less for psychotherapy in both adult and child services [49]. This was despite the findings of a recent systematic review that videoconferencing was an accessible and feasible modality for therapy delivery to adult patients, with comparable levels of therapeutic alliance between virtual and in‐person therapy [90]. This apparent discrepancy might be due to the challenging settings that clinicians and patients faced using the newly created TMH services during the pandemic, but it also suggests that the problems might be remedied by providing training (for both patients and clinicians) in TMH to improve delivery of therapies [15]. Clinicians’ attitudes toward TMH may also have an impact on its implementation in daily practice. As shown in a recent systematic review on barriers to and facilitators of TMH during the pandemic, clinicians reported a reduction in their ability to develop and maintain a therapeutic relationship during televisits [91]. This aligns with prepandemic data that showed that clinicians’ perspectives on TMH can be a major barrier to the uptake of the virtual modality [92]. Other factors influencing clinicians’ adoption of TMH include perceptions of how effectively this can be delivered, fears that aspects of in-person care may be missed in virtual encounters (eg, observation of physical signs such as tremor, fidgeting, and anxiety), and satisfaction with plans for handling clinical emergencies at a distance [92,93]. Moreover, a survey conducted in Hong Kong during the pandemic highlighted the need for mental health staff to receive dedicated training on clinical, technological, and program-specific aspects when providing TMH [94]. There is well-established guidance on virtual consultations to support health care professionals in the pandemic [95-97]. This includes physical examination, risk assessment, and management of emergency situations such as agitation/aggression, suicidality, and domestic violence [98]. During the COVID-19 pandemic, charities and other organizations reported an increase in cases of domestic violence and provided guidance on the safe assessment of domestic abuse during virtual contacts [99]. Although these recommendations may have been helpful to guide staff through the first period of the pandemic, training for clinicians will be crucial to take advantage of TMH in standard clinical care beyond the pandemic [15]. For example, implementing telehealth as part of the formal training for psychiatric residents has been proposed as an effective means of developing these skills [100].
While TMH was implemented for most patients, there were a small number of specific groups where it was not possible to be used alone, and instead, a hybrid model was used, combining face-to-face and digital strategies. This included services providing treatment with clozapine or depot medication, and electroconvulsive therapy. During the pandemic, such services applied several strategies to reduce the risk of exposure for these patients (eg, increasing the timing between blood monitoring for clozapine, new infection control measures, and social distancing) [101], but face-to-face contact could not be avoided completely. This highlighted that while teleassessment may have similar advantages and disadvantages independently to patient diagnoses, implementation of telemedicine in treatment management will face different barriers in different diagnostic groups. For instance, telemedicine has been typically used for the treatment of some diagnoses, such as anxiety and eating disorders [102,103], while programs addressing other diagnostic groups are now emerging [104].
Due to financial barriers, digital literacy, and features of chronic mental illness, a reliance on TMH services is not feasible for a minority of community patients [84]. Studies describing these clinical groups report a higher prevalence of certain diagnoses (eg, schizophrenia or schizoaffective disorder) [84], while others indicated several barriers, such as lack of digital literacy or confidence to make full use of a telephone, and lack of an appropriate device or broadband required to connect with clinicians [105]. In resource-limited settings during the COVID-19 pandemic, mental health staff working for Médecins Sans Frontières used audio-only platforms for 80% of TMH care interventions [106]. Despite this, over half of the patients were unreachable using these interventions, mainly due to poor network coverage, lack of communication devices, or lack of a private space at home [106]. For these patients, specific provision of a device or broadband might be necessary. Investment in providing these resources will have to be balanced at a country level against the costs associated with the anticipated increase in mental health problems. Moreover, appropriate training in TMH as well as the use of digital tools specifically for patients may increase access to and acceptability of virtual means. For instance, the DOORS (Digital Opportunities for Outcomes in Recovery Services) program provides an example of training to increase digital literacy and confidence in patients with first-episode psychosis and serious mental illness [104]. Such models will need to be developed locally to match the needs of local populations and clinical groups.
Limitations
Our study has some limitations. A systematic review relies on the quality of the primary papers, and in this case, although we found 55 articles on TMH, 19 were case reports or case series presenting descriptive data on local services, with limited generalizability. To address this, we grouped our findings according to the country of origin, considering differences in the local service structure, local needs, and stringency of confinement measures during the pandemic. In addition, we found limited reports on middle-income countries, and no reports from the African subcontinent or from low-income countries. Absent data do not represent evidence for the lack of effectiveness or feasibility, as services (such as those in African nations) may have implemented TMH without publishing quantitative data. The lack of representation of low- and middle-income countries in published health research is well documented [107], but without data, it is difficult to assess the impact of the pandemic on mental health services in these areas. Since the literature on COVID-19 is growing at a rapid pace, it is likely that relevant articles have been published after our final search and are therefore not included in our review. Finally, the aim of our project was to collect information about the changes and difficulties that mental health services faced at the start of the pandemic. Therefore, we limited the data collection to the first year of the pandemic. Future studies should evaluate whether these implementations will be confirmed or further refined.
Conclusions
During sudden health emergencies or disasters, such as the COVID-19 pandemic, mental health services cannot rely on face-to-face activities to provide care to all patients. The implementation of TMH has been demonstrated as feasible and widespread in different countries, allowing mental health services to continue the provision of essential care for patients, even during times of extreme confinement. Although many high-income countries and some middle-income countries were able to transition mental health services to digital delivery, this brought some challenges. While TMH was predominantly used in the acute pandemic, some findings showed a reduction in its use with time. Further training and support will be needed to maintain the benefits of TMH and to address barriers, such as digital exclusion. The pandemic can be seen as an opportunity to explore the benefits of TMH in enabling broader access to high-quality psychiatric treatment in the longer term [108]. Telehealth delivery methods are not only useful tools for the acute pandemic, but also have a role in addressing the anticipated increase in mental health needs after the immediate disruption and in preparation for future emergencies [15]. However, specific subgroups of patients will likely need or prefer face-to-face care, while others may not have access to virtual means. A blended approach, combining in-person and virtual modalities, that takes into consideration the needs, preferences, and digital skills of patients may suit the future development of mental health services, but this requires further investigation that considers acceptability to patients, carers, and clinicians. Delivering effective and equitable blended approaches will require confidence in using digital technologies, training, and experience in all modalities [108,109] to ensure that the benefits of TMH and associated eHealth technologies spark a transformation that is sustained beyond the immediate crisis.
Acknowledgments
AC and EGO are supported by the National Institute for Health Research (NIHR) Research Professorship to AC (grant RP-2017-08-ST2-006). EGO is also supported by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration Oxford and Thames Valley (ARC OxTV) at Oxford Health NHS Foundation Trust. AC, CZ, EGO, and KAS are supported by the NIHR Oxford Cognitive Health Clinical Research Facility and by the NIHR Oxford Health Biomedical Research Centre (grant BRC-1215-20005). The views expressed are those of the authors and not necessarily those of the UK National Health Service, the NIHR, or the Department of Health and Social Care.
Abbreviations
- MERS
Middle East respiratory syndrome
- TMH
telemental health
- WHO
World Health Organization
Search strategy.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart.
Impact of COVID-19 on mental health services: summary of key findings.
World distribution of 101 included papers.
Characteristics of 72 papers on face-to-face services.
Footnotes
Conflicts of Interest: AC has received research and consultancy fees from the INCiPiT (Italian Network for Paediatric Trials), CARIPLO Foundation, and Angelini Pharma, outside the submitted work. EGO has received research and consultancy fees from Angelini Pharma. All other authors declare no conflicts.
References
- 1.Hong J, Sheriff R, Smith K, Tomlinson A, Saad F, Smith T, Engelthaler T, Phiri P, Henshall C, Ede R, Denis M, Mitter P, D'Agostino A, Cerveri G, Tomassi S, Rathod S, Broughton N, Marlowe K, Geddes J, Cipriani A. Impact of COVID-19 on telepsychiatry at the service and individual patient level across two UK NHS mental health Trusts. Evid Based Ment Health. 2021 Nov;24(4):161–166. doi: 10.1136/ebmental-2021-300287. http://europepmc.org/abstract/MED/34583940 .ebmental-2021-300287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adhanom Ghebreyesus T. Addressing mental health needs: an integral part of COVID-19 response. World Psychiatry. 2020 Jun;19(2):129–130. doi: 10.1002/wps.20768. doi: 10.1002/wps.20768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. The Lancet Psychiatry. 2021 Feb;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. The Lancet Psychiatry. 2021 May;8(5):416–427. doi: 10.1016/S2215-0366(21)00084-5. doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, Collange O, Boulay C, Fafi-Kremer S, Ohana M, Anheim M, Meziani F. Neurologic Features in Severe SARS-CoV-2 Infection. N Engl J Med. 2020 Jun 04;382(23):2268–2270. doi: 10.1056/NEJMc2008597. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, Zandi MS, Lewis G, David AS. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. The Lancet Psychiatry. 2020 Jul;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varatharaj A, Thomas N, Ellul M, Davies NW, Pollak T, Tenorio E, Sultan M, Easton A, Breen G, Zandi M, Coles JP, Manji H, Al-Shahi Salman R, Menon D, Nicholson T, Benjamin L, Carson A, Smith C, Turner MR, Solomon T, Kneen R, Pett S, Galea I, Thomas RH, Michael B, Allen C, Archibald N, Arkell J, Arthur-Farraj P, Baker M, Ball H, Bradley-Barker V, Brown Z, Bruno S, Carey L, Carswell C, Chakrabarti A, Choulerton J, Daher M, Davies R, Di Marco Barros R, Dima S, Dunley R, Dutta D, Ellis R, Everitt A, Fady J, Fearon P, Fisniku L, Gbinigie I, Gemski A, Gillies E, Gkrania-Klotsas E, Grigg J, Hamdalla H, Hubbett J, Hunter N, Huys A, Ihmoda I, Ispoglou S, Jha A, Joussi R, Kalladka D, Khalifeh H, Kooij S, Kumar G, Kyaw S, Li L, Littleton E, Macleod M, Macleod M, Madigan B, Mahadasa V, Manoharan M, Marigold R, Marks I, Matthews P, Mccormick M, Mcinnes C, Metastasio A, Milburn-McNulty P, Mitchell C, Mitchell D, Morgans C, Morris H, Morrow J, Mubarak Mohamed A, Mulvenna P, Murphy L, Namushi R, Newman E, Phillips W, Pinto A, Price D, Proschel H, Quinn T, Ramsey D, Roffe C, Ross Russell A, Samarasekera N, Sawcer S, Sayed W, Sekaran L, Serra-Mestres J, Snowdon V, Strike G, Sun J, Tang C, Vrana M, Wade R, Wharton C, Wiblin L, Boubriak I, Herman K, Plant G. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. The Lancet Psychiatry. 2020 Oct;7(10):875–882. doi: 10.1016/S2215-0366(20)30287-X. doi: 10.1016/S2215-0366(20)30287-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. 2020 Mar;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Botchway S, Fazel S. Remaining vigilant about COVID-19 and suicide. The Lancet Psychiatry. 2021 Jul;8(7):552–553. doi: 10.1016/S2215-0366(21)00117-6. doi: 10.1016/S2215-0366(21)00117-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baraniuk C. How to vaccinate the world against covid-19. BMJ. 2021 Feb 05;372:n211. doi: 10.1136/bmj.n211. doi: 10.1136/bmj.n211. [DOI] [PubMed] [Google Scholar]
- 11.Hale T, Angrist N, Goldszmidt R, Kira B, Petherick A, Phillips T, Webster S, Cameron-Blake E, Hallas L, Majumdar S, Tatlow H. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker) Nat Hum Behav. 2021 Apr;5(4):529–538. doi: 10.1038/s41562-021-01079-8. doi: 10.1038/s41562-021-01079-8.10.1038/s41562-021-01079-8 [DOI] [PubMed] [Google Scholar]
- 12.Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, Cannon M, Correll C, Byrne L, Carr S, Chen E, Gorwood P, Johnson S, Kärkkäinen H, Krystal J, Lee J, Lieberman J, López-Jaramillo C, Männikkö M, Phillips M, Uchida H, Vieta E, Vita A, Arango C. How mental health care should change as a consequence of the COVID-19 pandemic. The Lancet Psychiatry. 2020 Sep;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Policy Brief: COVID-19 and the Need for Action on Mental Health. United Nations. 2020. [2022-07-30]. https://unsdg.un.org/sites/default/files/2020-05/UN-Policy-Brief-COVID-19-and-mental-health.pdf .
- 14.The impact of COVID-19 on mental, neurological and substance use services. World Health Organization. [2022-07-30]. https://www.who.int/publications/i/item/978924012455 .
- 15.Torous J, Wykes T. Opportunities From the Coronavirus Disease 2019 Pandemic for Transforming Psychiatric Care With Telehealth. JAMA Psychiatry. 2020 Dec 01;77(12):1205–1206. doi: 10.1001/jamapsychiatry.2020.1640.2765953 [DOI] [PubMed] [Google Scholar]
- 16.Kinoshita S, Cortright K, Crawford A, Mizuno Y, Yoshida K, Hilty D, Guinart D, Torous J, Correll CU, Castle DJ, Rocha D, Yang Y, Xiang Y, Kølbæk P, Dines D, ElShami M, Jain P, Kallivayalil R, Solmi M, Favaro A, Veronese N, Seedat S, Shin S, Salazar de Pablo G, Chang C, Su K, Karas H, Kane JM, Yellowlees P, Kishimoto T. Changes in telepsychiatry regulations during the COVID-19 pandemic: 17 countries and regions' approaches to an evolving healthcare landscape. Psychol. Med. 2020 Nov 27;:1–8. doi: 10.1017/s0033291720004584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. World Health Organization. 2020. [2022-07-30]. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 .
- 18.Cipriani A, Ostinelli E, Smith K, Macdonald O, Sheriff R, Harrison P, Hawton K. COVID-19 and its impact on mental health patients, staff and services: systematic review with recommendations for clinical practice and research. PROSPERO International prospective register of systematic reviews. [2022-07-30]. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020178819 .
- 19.COAP (COVID-19 Open Access Project) COVID-19 Living Evidence. [2022-07-30]. https://zika.ispm.unibe.ch/assets/data/pub/search_beta/
- 20.COVID-19: Stringency Index. Our World in Data. [2022-07-30]. https://ourworldindata.org/grapher/covid-stringency-index .
- 21.Fredwall M, Terry D, Enciso L, Burch MM, Trott K, Albert DVF. Short-term outcomes in pediatric and adolescent patients with psychogenic nonepileptic events seen by telemedicine during the COVID-19 pandemic. Epilepsy Behav. 2021 Apr;117:107739. doi: 10.1016/j.yebeh.2020.107739. doi: 10.1016/j.yebeh.2020.107739.S1525-5050(20)30919-7 [DOI] [PubMed] [Google Scholar]
- 22.Stewart R, Broadbent M. Using past and current data to estimate potential crisis service use in mental healthcare after the COVID-19 lockdown: South London and Maudsley data. medRxiv. 2020. [2022-07-30]. https://www.medrxiv.org/content/10.1101/2020.06.29.20142448v1 .
- 23.Baugh JJ, White BA, McEvoy D, Yun BJ, Brown DF, Raja AS, Dutta S. The cases not seen: Patterns of emergency department visits and procedures in the era of COVID-19. Am J Emerg Med. 2021 Aug;46:476–481. doi: 10.1016/j.ajem.2020.10.081. http://europepmc.org/abstract/MED/33189517 .S0735-6757(20)30964-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amad A, Magnat M, Quilès C, Yrondi A, Sauvaget A, Bulteau S, Plaze M, Rotharmel M, Polosan M, Lévy-Chavagnat D, Jaafari N, Vaiva G, Thomas P. [Evolution of electro-convulsive therapy activity in France since the beginning of the COVID-19 pandemic] Encephale. 2020 Jun;46(3S):S40–S42. doi: 10.1016/j.encep.2020.04.004. http://europepmc.org/abstract/MED/32370981 .S0013-7006(20)30072-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Casano K, Capone E. Unexpected cancellation on a catatonic patient's electroconvulsive therapy due to the coronavirus pandemic. Gen Psychiatr. 2020 Sep 24;33(6):e100271. doi: 10.1136/gpsych-2020-100271. http://europepmc.org/abstract/MED/33083693 .gpsych-2020-100271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grover S, Mehra A, Sahoo S, Avasthi A, Tripathi A, D'Souza A, Saha G, Jagadhisha A, Gowda M, Vaishnav M, Singh O, Dalal P, Kumar P. State of mental health services in various training centers in India during the lockdown and COVID-19 pandemic. Indian J Psychiatry. 2020;62(4):363. doi: 10.4103/psychiatry.indianjpsychiatry_567_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grover S, Mehra A, Sahoo S, Avasthi A, Tripathi A, D'Souza A, Saha G, Jagadhisha A, Gowda M, Vaishnav M, Singh O, Dalal P, Kumar P. Impact of COVID-19 pandemic and lockdown on the state of mental health services in the private sector in India. Indian J Psychiatry. 2020;62(5):488. doi: 10.4103/psychiatry.indianjpsychiatry_568_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bollmann A, Hohenstein S, Pellissier V, Stengler K, Reichardt P, Ritz JP, Thiele H, Borger MA, Hindricks G, Meier-Hellmann A, Kuhlen R. Utilization of in- and outpatient hospital care in Germany during the Covid-19 pandemic insights from the German-wide Helios hospital network. PLoS One. 2021;16(3):e0249251. doi: 10.1371/journal.pone.0249251. https://dx.plos.org/10.1371/journal.pone.0249251 .PONE-D-20-31366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clerici M, Durbano F, Spinogatti F, Vita A, de Girolamo G, Micciolo R. Psychiatric hospitalization rates in Italy before and during COVID-19: did they change? An analysis of register data. Ir J Psychol Med. 2020 Dec 05;37(4):283–290. doi: 10.1017/ipm.2020.29. http://europepmc.org/abstract/MED/32368994 .S0790966720000294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee A, Mo FYM, Lam LCW. Higher psychogeriatric admissions in COVID-19 than in severe acute respiratory syndrome. Int J Geriatr Psychiatry. 2020 Dec;35(12):1449–1457. doi: 10.1002/gps.5422. doi: 10.1002/gps.5422. [DOI] [PubMed] [Google Scholar]
- 31.Itrat A, Jagadheesan K, Danivas V, Lakra V. A comparative study of access to inpatient psychiatric treatment in a public mental health service in Melbourne during COVID-19. Indian J Psychiatry. 2020;62(9):454. doi: 10.4103/psychiatry.IndianJPsychiatry_852_20. doi: 10.4103/psychiatry.IndianJPsychiatry_852_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jagadheesan K, Danivas V, Itrat Q, Sekharan L, Lakra APV. COVID-19 and psychiatric admissions: An observational study of the first six months of lockdown in Melbourne. Psychiatry Res. 2021 Jun;300:113902. doi: 10.1016/j.psychres.2021.113902. http://europepmc.org/abstract/MED/33799197 .S0165-1781(21)00199-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arendt F, Markiewitz A, Mestas M, Scherr S. COVID-19 pandemic, government responses, and public mental health: Investigating consequences through crisis hotline calls in two countries. Soc Sci Med. 2020 Nov;265:113532. doi: 10.1016/j.socscimed.2020.113532. https://linkinghub.elsevier.com/retrieve/pii/S0277-9536(20)30751-6 .S0277-9536(20)30751-6 [DOI] [PubMed] [Google Scholar]
- 34.Beran C, Sowa NA. Adaptation of an Academic Inpatient Consultation-Liaison Psychiatry Service During the SARS-CoV-2 Pandemic: Effects on Clinical Practice and Trainee Supervision. J Acad Consult Liaison Psychiatry. 2021;62(2):186–192. doi: 10.1016/j.psym.2020.11.002. http://europepmc.org/abstract/MED/33288272 .S0033-3182(20)30285-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berthaut E, Chamignon T. Le fil institutionnel en période Covid : utilisation de la plateforme Discord au CMPA. Neuropsychiatrie de l'Enfance et de l'Adolescence. 2021 May;69(3):142–144. doi: 10.1016/j.neurenf.2021.01.002. doi: 10.1016/j.neurenf.2021.01.002. [DOI] [Google Scholar]
- 36.Cantini S, Caponigro G, Fusco O, Deligiannis P, Pastorini A, Cubeddu A, Maiolani M, Menatti E, Bazza T, Bertolini A. Psychoncology in front of Covid-19. Tumori. 2020 Oct 20;106(2_suppl):95–96. doi: 10.1177/0300891620953388. doi: 10.1177/0300891620953388. [DOI] [Google Scholar]
- 37.Carpiniello B, Tusconi M, Zanalda E, Di Sciascio G, Di Giannantonio M, Executive Committee of The Italian Society of Psychiatry Psychiatry during the Covid-19 pandemic: a survey on mental health departments in Italy. BMC Psychiatry. 2020 Dec 16;20(1):593. doi: 10.1186/s12888-020-02997-z. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-020-02997-z .10.1186/s12888-020-02997-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Connolly SL, Stolzmann KL, Heyworth L, Weaver KR, Bauer MS, Miller CJ. Rapid Increase in Telemental Health Within the Department of Veterans Affairs During the COVID-19 Pandemic. Telemed J E Health. 2021 Apr 01;27(4):454–458. doi: 10.1089/tmj.2020.0233. doi: 10.1089/tmj.2020.0233. [DOI] [PubMed] [Google Scholar]
- 39.Datta N, Derenne J, Sanders M, Lock JD. Telehealth transition in a comprehensive care unit for eating disorders: Challenges and long-term benefits. Int J Eat Disord. 2020 Nov 27;53(11):1774–1779. doi: 10.1002/eat.23348. doi: 10.1002/eat.23348. [DOI] [PubMed] [Google Scholar]
- 40.Garcia-Huidobro D, Rivera S, Valderrama Chang S, Bravo P, Capurro D. System-Wide Accelerated Implementation of Telemedicine in Response to COVID-19: Mixed Methods Evaluation. J Med Internet Res. 2020 Oct 06;22(10):e22146. doi: 10.2196/22146. https://www.jmir.org/2020/10/e22146/ v22i10e22146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ghiretti F, Gildoni G, Grassi GM, Torricelli L, Benassi E, Bonaretti E, Bonazzi F, Borelli S, Cagnolati F, Covati K, Errera F, Finardi V, Grisendi R, Libanti J, Lumia R, Montanari A, Morini G, Pettinari S, Peverini A, Ragone C, Santachiara M, Valentini V, Zanchetta A, Zapponi S, Pensieri L, Poletti M. Psychological Support to the Community During the COVID-19 Pandemic: Field Experience in Reggio Emilia, Northern Italy. Front Psychol. 2020 Nov 17;11:561742. doi: 10.3389/fpsyg.2020.561742. doi: 10.3389/fpsyg.2020.561742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ghosh A, Mahintamani T, Pillai RR, Mattoo SK, Basu D. Telemedicine-assisted stepwise approach of service delivery for substance use disorders in India. Asian J Psychiatr. 2021 Apr;58:102582. doi: 10.1016/j.ajp.2021.102582. doi: 10.1016/j.ajp.2021.102582.S1876-2018(21)00038-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Graell M, Morón-Nozaleda MG, Camarneiro R, Villaseñor Á, Yáñez S, Muñoz R, Martínez-Núñez B, Miguélez-Fernández C, Muñoz M, Faya M. Children and adolescents with eating disorders during COVID-19 confinement: Difficulties and future challenges. Eur Eat Disord Rev. 2020 Nov 29;28(6):864–870. doi: 10.1002/erv.2763. doi: 10.1002/erv.2763. [DOI] [PubMed] [Google Scholar]
- 44.Guinart D, Marcy P, Hauser M, Dwyer M, Kane JM. Mental Health Care Providers' Attitudes Toward Telepsychiatry: A Systemwide, Multisite Survey During the COVID-19 Pandemic. Psychiatr Serv. 2021 Jun;72(6):704–707. doi: 10.1176/appi.ps.202000441. doi: 10.1176/appi.ps.202000441. [DOI] [PubMed] [Google Scholar]
- 45.Hall P, Sukhera J. Emergency Diversion Clinic: Lessons from Southwestern Ontario's Pandemic Response. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2020;29(4):271. https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-1106994 . [Google Scholar]
- 46.Hames JL, Bell DJ, Perez-Lima LM, Holm-Denoma JM, Rooney T, Charles NE, Thompson SM, Mehlenbeck RS, Tawfik SH, Fondacaro KM, Simmons KT, Hoersting RC. Navigating uncharted waters: Considerations for training clinics in the rapid transition to telepsychology and telesupervision during COVID-19. Journal of Psychotherapy Integration. 2020 Jun;30(2):348–365. doi: 10.1037/int0000224. doi: 10.1037/int0000224. [DOI] [Google Scholar]
- 47.Harrison L, DeMasi L, Butkus S, O'Neill K, Kwon N, D'Angelo J, Morgenstern J, Kapoor S. 163 Implementation of a Telephonic-Based Model to Continue to Address Substance Use as Part of Usual Care in Emergency Departments during COVID-19. Annals of Emergency Medicine. 2020 Oct;76(4):S64. doi: 10.1016/j.annemergmed.2020.09.175. doi: 10.1016/j.annemergmed.2020.09.175. [DOI] [Google Scholar]
- 48.Hazarika M, Das B, Das S, Baruah A, Sharma N, Barua C, Das J, Choudhury S, Hazarika D, Sarma P, Bhandari SS. Profile of distress callers and service utilisation of tele-counselling among the population of Assam, India: an exploratory study during COVID-19. Open J Psychiatry Allied Sci. 2021;12(1):7–12. doi: 10.5958/2394-2061.2021.00001.x. http://europepmc.org/abstract/MED/33163629 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hoffnung G, Feigenbaum E, Schechter A, Guttman D, Zemon V, Schechter I. Children and Telehealth in Mental Healthcare: What We Have Learned From COVID-19 and 40,000+ Sessions. Psychiatr Res Clin Pract. 2021 Sep;3(3):106–114. doi: 10.1176/appi.prcp.20200035. http://europepmc.org/abstract/MED/33821240 .RCP21022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Humer E, Pieh C, Kuska M, Barke A, Doering BK, Gossmann K, Trnka R, Meier Z, Kascakova N, Tavel P, Probst T. Provision of Psychotherapy during the COVID-19 Pandemic among Czech, German and Slovak Psychotherapists. Int J Environ Res Public Health. 2020 Jul 04;17(13):4811. doi: 10.3390/ijerph17134811. https://www.mdpi.com/resolver?pii=ijerph17134811 .ijerph17134811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnson S, Dalton-Locke C, Vera San Juan N, Foye U, Oram S, Papamichail A, Landau S, Rowan Olive R, Jeynes T, Shah P, Sheridan Rains L, Lloyd-Evans B, Carr S, Killaspy H, Gillard S, Simpson A, COVID-19 Mental Health Policy Research Unit Group Impact on mental health care and on mental health service users of the COVID-19 pandemic: a mixed methods survey of UK mental health care staff. Soc Psychiatry Psychiatr Epidemiol. 2021 Jan;56(1):25–37. doi: 10.1007/s00127-020-01927-4. http://europepmc.org/abstract/MED/32857218 .10.1007/s00127-020-01927-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Karim M, Wadoo O, Reagu SM, Amro R, Abdulla MA. Telepsychiatry in the Arabian Gulf region - Implications beyond the Covid-19 pandemic. Asian J Psychiatr. 2020 Dec;54:102397. doi: 10.1016/j.ajp.2020.102397. http://europepmc.org/abstract/MED/33271697 .S1876-2018(20)30510-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Khanra S, Mukherjee A, Goyal N, Das B, Munda SK. Service utilization and saved travel cost in telepsychiatry consultation by outpatients at a psychiatric hospital in India during COVID-19 pandemic. Asian J Psychiatr. 2021 Mar;57:102568. doi: 10.1016/j.ajp.2021.102568. http://europepmc.org/abstract/MED/33535135 .S1876-2018(21)00024-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lian W, Wen L, Zhou Q, Zhu W, Duan W, Xiao X, Mhungu F, Huang W, Li C, Cheng W, Tian J. Digital Health Technologies Respond to the COVID-19 Pandemic In a Tertiary Hospital in China: Development and Usability Study. J Med Internet Res. 2020 Nov 24;22(11):e24505. doi: 10.2196/24505. https://www.jmir.org/2020/11/e24505/ v22i11e24505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Looi JC, Allison S, Bastiampillai T, Pring W, Reay R. Australian private practice metropolitan telepsychiatry during the COVID-19 pandemic: analysis of Quarter-2, 2020 usage of new MBS-telehealth item psychiatrist services. Australas Psychiatry. 2021 Apr 06;29(2):183–188. doi: 10.1177/1039856220975294. https://journals.sagepub.com/doi/10.1177/1039856220975294?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Looi JC, Allison S, Bastiampillai T, Pring W. Private practice metropolitan telepsychiatry in smaller Australian jurisdictions during the COVID-19 pandemic: preliminary analysis of the introduction of new Medicare Benefits Schedule items. Australas Psychiatry. 2020 Dec 05;28(6):639–643. doi: 10.1177/1039856220960381. doi: 10.1177/1039856220960381. [DOI] [PubMed] [Google Scholar]
- 57.Looi JC, Allison S, Bastiampillai T, Pring W. Private practice metropolitan telepsychiatry in larger Australian states during the COVID-19 pandemic: an analysis of the first 2 months of new MBS telehealth item psychiatrist services. Australas Psychiatry. 2020 Dec 30;28(6):644–648. doi: 10.1177/1039856220961906. doi: 10.1177/1039856220961906. [DOI] [PubMed] [Google Scholar]
- 58.Looi JC, Allison S, Bastiampillai T, Pring W, Reay R, Kisely SR. Increased Australian outpatient private practice psychiatric care during the COVID-19 pandemic: usage of new MBS-telehealth item and face-to-face psychiatrist office-based services in Quarter 3, 2020. Australas Psychiatry. 2021 Apr 24;29(2):194–199. doi: 10.1177/1039856221992634. https://journals.sagepub.com/doi/10.1177/1039856221992634?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lunsky Y, Bobbette N, Selick A, Jiwa M. "The doctor will see you now": Direct support professionals' perspectives on supporting adults with intellectual and developmental disabilities accessing health care during COVID-19. Disabil Health J. 2021 Jul;14(3):101066. doi: 10.1016/j.dhjo.2021.101066. doi: 10.1016/j.dhjo.2021.101066.S1936-6574(21)00007-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mehtani NJ, Ristau JT, Snyder H, Surlyn C, Eveland J, Smith-Bernardin S, Knight KR. COVID-19: A catalyst for change in telehealth service delivery for opioid use disorder management. Subst Abus. 2021 Mar 08;42(2):205–212. doi: 10.1080/08897077.2021.1890676. doi: 10.1080/08897077.2021.1890676. [DOI] [PubMed] [Google Scholar]
- 61.Mishkind MC, Shore JH, Bishop K, D'Amato K, Brame A, Thomas M, Schneck CD. Rapid Conversion to Telemental Health Services in Response to COVID-19: Experiences of Two Outpatient Mental Health Clinics. Telemed J E Health. 2021 Jul 01;27(7):778–784. doi: 10.1089/tmj.2020.0304. doi: 10.1089/tmj.2020.0304. [DOI] [PubMed] [Google Scholar]
- 62.Moreland A, Guille C, McCauley JL. Increased availability of telehealth mental health and substance abuse treatment for peripartum and postpartum women: A unique opportunity to increase telehealth treatment. J Subst Abuse Treat. 2021 Apr;123:108268. doi: 10.1016/j.jsat.2020.108268. doi: 10.1016/j.jsat.2020.108268.S0740-5472(20)30525-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Myers Virtue S, Howrey HL, Duffy NM, Wallace M. Shifting psychosocial oncology care to telepsychology during the COVID-19 pandemic. J Psychosoc Oncol. 2021;39(3):416–427. doi: 10.1080/07347332.2021.1894526. doi: 10.1080/07347332.2021.1894526. [DOI] [PubMed] [Google Scholar]
- 64.Naik S, Rahul P, Harihara S, Pahuja E, Chithra NK, Ramachandraiah S, Kumar V, Mehta UM, Manjunatha N, Channaveerachari NK, Math SB, Thirthalli J. Telephonic follow-up during COVID-19 to maintain continuity of care for persons with psychiatric disorders. Asian J Psychiatr. 2021 Mar;57:102564. doi: 10.1016/j.ajp.2021.102564. http://europepmc.org/abstract/MED/33516153 .S1876-2018(21)00020-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Peppou L, Economou M, Skali T, Papageorgiou C. From economic crisis to the COVID-19 pandemic crisis: evidence from a mental health helpline in Greece. Eur Arch Psychiatry Clin Neurosci. 2021 Mar;271(2):407–409. doi: 10.1007/s00406-020-01165-4. http://europepmc.org/abstract/MED/32666279 .10.1007/s00406-020-01165-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Peralta E, Taveras M. Effectiveness of teleconsultation use in access to mental health services during the coronavirus disease 2019 pandemic in the Dominican Republic. Indian J Psychiatry. 2020;62(9):492. doi: 10.4103/psychiatry.IndianJPsychiatry_1047_20. doi: 10.4103/psychiatry.IndianJPsychiatry_1047_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Perricone G, Rotolo I, Beninati V, Billeci N, Ilarda V, Polizzi C. The Lègami/Legàmi Service-An Experience of Psychological Intervention in Maternal and Child Care during COVID-19. Pediatr Rep. 2021 Mar 22;13(1):142–161. doi: 10.3390/pediatric13010021. https://www.mdpi.com/resolver?pii=pediatric13010021 .pediatric13010021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pierce BS, Perrin PB, Tyler CM, McKee GB, Watson JD. The COVID-19 telepsychology revolution: A national study of pandemic-based changes in U.S. mental health care delivery. Am Psychol. 2021 Jan;76(1):14–25. doi: 10.1037/amp0000722. doi: 10.1037/amp0000722.2020-61592-001 [DOI] [PubMed] [Google Scholar]
- 69.Prior M, Bellè M, Burelli M, Favaretto A. On-line psychological treatment with oncology patients during COVID-19 emergency. Tumori. 2020 Oct 20;106(2_suppl):81. doi: 10.1177/0300891620953388. doi: 10.1177/0300891620953388. [DOI] [Google Scholar]
- 70.Probst T, Stippl P, Pieh C. Changes in Provision of Psychotherapy in the Early Weeks of the COVID-19 Lockdown in Austria. Int J Environ Res Public Health. 2020 May 27;17(11):3815. doi: 10.3390/ijerph17113815. https://www.mdpi.com/resolver?pii=ijerph17113815 .ijerph17113815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rainwater L, Lichiello S, Duckworth K, Tolbert A, Moskop R, McQuellon R. Psychosocial oncology care during a pandemic: Effect of offering telemental health in an academic medical center. Psychooncology. 2021 Mar;30(S1):18.1. doi: 10.1002/pon.5637. http://doi:10.1002/pon.5637 . [DOI] [Google Scholar]
- 72.Ravindran S, Channaveerachari NK, Seshadri SP, Kasi S, Manikappa SK, Cherian AV, Palanimuthu TS, Sudhir P, Govindan R, Christopher AD, George S. Crossing barriers: Role of a tele-outreach program addressing psychosocial needs in the midst of COVID-19 pandemic. Asian J Psychiatr. 2020 Oct;53:102351. doi: 10.1016/j.ajp.2020.102351. http://europepmc.org/abstract/MED/32871399 .S1876-2018(20)30463-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rosen C, Morland LA, Glassman LH, Marx BP, Weaver K, Smith CA, Pollack S, Schnurr PP. Virtual mental health care in the Veterans Health Administration's immediate response to coronavirus disease-19. Am Psychol. 2021 Jan;76(1):26–38. doi: 10.1037/amp0000751. doi: 10.1037/amp0000751.2020-81589-001 [DOI] [PubMed] [Google Scholar]
- 74.Salum GA, Rehmenklau JF, Csordas MC, Pereira FP, Castan JU, Ferreira AB, Delgado VB, Bolzan LDM, de Lima MA, Blauth JH, Dos Reis JR, Rocha PB, Guerra TA, Saraiva IM, Gramz BDC, Ronchi BR, Ribeiro BL, Konig DF, Grevet EH. Supporting people with severe mental health conditions during the COVID-19 pandemic: considerations for low- and middle-income countries using telehealth case management. Braz J Psychiatry. 2020 Aug;42(4):451–452. doi: 10.1590/1516-4446-2020-1078. http://europepmc.org/abstract/MED/32578690 .S1516-44462020005019203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sampaio M, Haro MVN, De Sousa B, Melo WV, Hoffman HG. Therapists Make the Switch to Telepsychology to Safely Continue Treating Their Patients During the COVID-19 Pandemic. Virtual Reality Telepsychology May Be Next. Front Virtual Real. 2021 Jan;1:576421. doi: 10.3389/frvir.2020.576421. http://europepmc.org/abstract/MED/33585834 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sharma A, Sasser T, Schoenfelder Gonzalez E, Vander Stoep A, Myers K. Implementation of Home-Based Telemental Health in a Large Child Psychiatry Department During the COVID-19 Crisis. J Child Adolesc Psychopharmacol. 2020 Sep;30(7):404–413. doi: 10.1089/cap.2020.0062. doi: 10.1089/cap.2020.0062. [DOI] [PubMed] [Google Scholar]
- 77.Singh Bhandari S, Joseph SJ, Udayasankaran JG, Konthoujam B, Shoib S, Dutta S. Telepsychiatry: A Feasible Means to Bridge the Demand-Supply Gaps in Mental Health Services During and After the COVID-19 Pandemic: Preliminary Experiences from Sikkim State of India. Indian J Psychol Med. 2020 Oct 27;42(5):500–502. doi: 10.1177/0253717620951282. https://journals.sagepub.com/doi/10.1177/0253717620951282?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .10.1177_0253717620951282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Staples L, Nielssen O, Kayrouz R, Cross S, Karin E, Ryan K, Dear B, Titov N. Rapid report 2: Symptoms of anxiety and depression during the first 12 weeks of the Coronavirus (COVID-19) pandemic in Australia. Internet Interv. 2020 Dec;22:100351. doi: 10.1016/j.invent.2020.100351. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(20)30117-2 .S2214-7829(20)30117-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Steeg S, Carr MJ, Trefan L, Ashcroft DM, Kapur N, Nielsen E, McMillan B, Webb RT. Primary care clinical management following self-harm during the first wave of COVID-19 in the UK. medRxiv. [2022-07-30]. https://www.medrxiv.org/content/10.1101/2021.03.19.21253969v1 . [DOI] [PMC free article] [PubMed]
- 80.Stewart R, Martin E, Broadbent M. Mental health service activity during COVID-19 lockdown: South London and Maudsley data on working age community and home treatment team services and mortality from February to mid-May 2020. medRxiv. [2022-07-30]. https://www.medrxiv.org/content/10.1101/2020.06.13.20130419v1 .
- 81.Vonderlin R, Biermann M, Konrad M, Klett M, Kleindienst N, Bailer J, Lis S, Bohus M. [Implementation and evaluation of a telephone hotline for professional mental health first aid during the COVID-19 pandemic in Germany] Nervenarzt. 2022 Jan;93(1):24–33. doi: 10.1007/s00115-021-01089-x. http://europepmc.org/abstract/MED/33725184 .10.1007/s00115-021-01089-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yaffa S, Adi E, Itai P, Marit J, Doron G, Daniel S. Treatment of eating disorders in adolescents during the COVID-19 pandemic: a case series. J Eat Disord. 2021 Mar 10;9(1):17. doi: 10.1186/s40337-021-00374-z. https://jeatdisord.biomedcentral.com/articles/10.1186/s40337-021-00374-z .10.1186/s40337-021-00374-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhong B, Zhou DY, He MF, Li Y, Li WT, Ng CH, Xiang YT, Chiu HFK. Mental health problems, needs, and service use among people living within and outside Wuhan during the COVID-19 epidemic in China. Ann Transl Med. 2020 Dec;8(21):1392. doi: 10.21037/atm-20-4145. doi: 10.21037/atm-20-4145.atm-08-21-1392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zulfic Z, Liu D, Lloyd C, Rowan J, Schubert KO. Is telepsychiatry care a realistic option for community mental health services during the COVID-19 pandemic? Aust N Z J Psychiatry. 2020 Dec;54(12):1228. doi: 10.1177/0004867420937788. http://europepmc.org/abstract/MED/32571079 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Merchant R, Torous J, Rodriguez-Villa E, Naslund JA. Digital technology for management of severe mental disorders in low-income and middle-income countries. Curr Opin Psychiatry. 2020 Sep;33(5):501–507. doi: 10.1097/YCO.0000000000000626. http://europepmc.org/abstract/MED/32520747 .00001504-202009000-00011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Walker P, Whittaker C, Watson OJ, Baguelin M, Winskill P, Hamlet A, Djafaara BA, Cucunubá Z, Olivera Mesa D, Green W, Thompson H, Nayagam S, Ainslie KEC, Bhatia S, Bhatt S, Boonyasiri A, Boyd O, Brazeau NF, Cattarino L, Cuomo-Dannenburg G, Dighe A, Donnelly CA, Dorigatti I, van Elsland SL, FitzJohn R, Fu H, Gaythorpe KAM, Geidelberg L, Grassly N, Haw D, Hayes S, Hinsley W, Imai N, Jorgensen D, Knock E, Laydon D, Mishra S, Nedjati-Gilani G, Okell LC, Unwin HJ, Verity R, Vollmer M, Walters CE, Wang H, Wang Y, Xi X, Lalloo DG, Ferguson NM, Ghani AC. The impact of COVID-19 and strategies for mitigation and suppression in low- and middle-income countries. Science. 2020 Jul 24;369(6502):413–422. doi: 10.1126/science.abc0035. http://europepmc.org/abstract/MED/32532802 .science.abc0035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Adepoju P. Africa turns to telemedicine to close mental health gap. The Lancet Digital Health. 2020 Nov;2(11):e571–e572. doi: 10.1016/S2589-7500(20)30252-1. doi: 10.1016/S2589-7500(20)30252-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Arango C, Wykes T, Moreno C. Mental health care and COVID-19. The Lancet Psychiatry. 2020 Dec;7(12):1013. doi: 10.1016/S2215-0366(20)30480-6. doi: 10.1016/S2215-0366(20)30480-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kola L, Kohrt BA, Hanlon C, Naslund JA, Sikander S, Balaji M, Benjet C, Cheung EYL, Eaton J, Gonsalves P, Hailemariam M, Luitel NP, Machado DB, Misganaw E, Omigbodun O, Roberts T, Salisbury TT, Shidhaye R, Sunkel C, Ugo V, van Rensburg AJ, Gureje O, Pathare S, Saxena S, Thornicroft G, Patel V. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. The Lancet Psychiatry. 2021 Jun;8(6):535–550. doi: 10.1016/S2215-0366(21)00025-0. doi: 10.1016/S2215-0366(21)00025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Thomas N, McDonald C, de Boer K, Brand RM, Nedeljkovic M, Seabrook L. Review of the current empirical literature on using videoconferencing to deliver individual psychotherapies to adults with mental health problems. Psychol Psychother. 2021 Sep 23;94(3):854–883. doi: 10.1111/papt.12332. http://europepmc.org/abstract/MED/33620133 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Appleton R, Williams J, Vera San Juan N, Needle JJ, Schlief M, Jordan H, Sheridan Rains L, Goulding L, Badhan M, Roxburgh E, Barnett P, Spyridonidis S, Tomaskova M, Mo J, Harju-Seppänen J, Haime Z, Casetta C, Papamichail A, Lloyd-Evans B, Simpson A, Sevdalis N, Gaughran F, Johnson S. Implementation, Adoption, and Perceptions of Telemental Health During the COVID-19 Pandemic: Systematic Review. J Med Internet Res. 2021 Dec 09;23(12):e31746. doi: 10.2196/31746. https://www.jmir.org/2021/12/e31746/ v23i12e31746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cowan K, McKean AJ, Gentry MT, Hilty DM. Barriers to Use of Telepsychiatry: Clinicians as Gatekeepers. Mayo Clin Proc. 2019 Dec;94(12):2510–2523. doi: 10.1016/j.mayocp.2019.04.018. doi: 10.1016/j.mayocp.2019.04.018.S0025-6196(19)30400-8 [DOI] [PubMed] [Google Scholar]
- 93.Yellowlees P. Impact of COVID-19 on Mental Health Care Practitioners. Psychiatr Clin North Am. 2022 Mar;45(1):109–121. doi: 10.1016/j.psc.2021.11.007. http://europepmc.org/abstract/MED/35219432 .S0193-953X(21)00085-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fong R, Tsai CF, Yiu OY. The Implementation of Telepractice in Speech Language Pathology in Hong Kong During the COVID-19 Pandemic. Telemed J E Health. 2021 Jan 01;27(1):30–38. doi: 10.1089/tmj.2020.0223. doi: 10.1089/tmj.2020.0223. [DOI] [PubMed] [Google Scholar]
- 95.Wahezi SE, Duarte RA, Yerra S, Thomas MA, Pujar B, Sehgal N, Argoff C. Telemedicine During COVID-19 and Beyond: A Practical Guide and Best Practices Multidisciplinary Approach for the Orthopedic and Neurologic Pain Physical Examination. Pain Phys. 2020;23:S205–S237. doi: 10.36076/ppj.2020/23/s205. [DOI] [PubMed] [Google Scholar]
- 96.Waller G, Pugh M, Mulkens S, Moore E, Mountford VA, Carter J, Wicksteed A, Maharaj A, Wade TD, Wisniewski L, Farrell NR, Raykos B, Jorgensen S, Evans J, Thomas JJ, Osenk I, Paddock C, Bohrer B, Anderson K, Turner H, Hildebrandt T, Xanidis N, Smit V. Cognitive-behavioral therapy in the time of coronavirus: Clinician tips for working with eating disorders via telehealth when face-to-face meetings are not possible. Int J Eat Disord. 2020 Jul 08;53(7):1132–1141. doi: 10.1002/eat.23289. http://europepmc.org/abstract/MED/32383530 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Smith K, Ostinelli E, Macdonald O, Cipriani A. COVID-19 and Telepsychiatry: Development of Evidence-Based Guidance for Clinicians. JMIR Ment Health. 2020 Aug 28;7(8):e21108. doi: 10.2196/21108. https://mental.jmir.org/2020/8/e21108/ v7i8e21108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Digital technologies and telepsychiatry. Oxford Health Biomedical Research Centre. [2022-07-30]. https://oxfordhealthbrc.nihr.ac.uk/our-work/oxppl/table-5-digital-technologies-and-telepsychiatry/
- 99.Domestic violence and abuse. Oxford Health Biomedical Research Centre. [2022-07-30]. https://oxfordhealthbrc.nihr.ac.uk/our-work/oxppl/domestic-violence-and-abuse/
- 100.Torous J, Jän Myrick K, Rauseo-Ricupero N, Firth J. Digital Mental Health and COVID-19: Using Technology Today to Accelerate the Curve on Access and Quality Tomorrow. JMIR Ment Health. 2020 Mar 26;7(3):e18848. doi: 10.2196/18848. https://mental.jmir.org/2020/3/e18848/ v7i3e18848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Clozapine treatment. Oxford Health Biomedical Research Centre. [2022-07-30]. https://oxfordhealthbrc.nihr.ac.uk/our-work/oxppl/table-1-clozapine-treatment/
- 102.Krzyzaniak N, Greenwood H, Scott AM, Peiris R, Cardona M, Clark J, Glasziou P. The effectiveness of telehealth versus face-to face interventions for anxiety disorders: A systematic review and meta-analysis. J Telemed Telecare. 2021 Dec 03;:1357633X2110537. doi: 10.1177/1357633X211053738. doi: 10.1177/1357633X211053738. [DOI] [PubMed] [Google Scholar]
- 103.Loucas C, Fairburn CG, Whittington C, Pennant ME, Stockton S, Kendall T. E-therapy in the treatment and prevention of eating disorders: A systematic review and meta-analysis. Behav Res Ther. 2014 Dec;63:122–31. doi: 10.1016/j.brat.2014.09.011. https://linkinghub.elsevier.com/retrieve/pii/S0005-7967(14)00162-4 .S0005-7967(14)00162-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hoffman L, Wisniewski H, Hays R, Henson P, Vaidyam A, Hendel V, Keshavan M, Torous J. Digital Opportunities for Outcomes in Recovery Services (DOORS): A Pragmatic Hands-On Group Approach Toward Increasing Digital Health and Smartphone Competencies, Autonomy, Relatedness, and Alliance for Those With Serious Mental Illness. J Psychiatr Pract. 2020 Mar;26(2):80–88. doi: 10.1097/PRA.0000000000000450. http://europepmc.org/abstract/MED/32134881 .00131746-202003000-00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Triana AJ, Gusdorf RE, Shah KP, Horst SN. Technology Literacy as a Barrier to Telehealth During COVID-19. Telemed J E Health. 2020 Sep 01;26(9):1118–1119. doi: 10.1089/tmj.2020.0155. doi: 10.1089/tmj.2020.0155. [DOI] [PubMed] [Google Scholar]
- 106.Ibragimov K, Palma M, Keane G, Ousley J, Crowe M, Carreño C, Casas G, Mills C, Llosa A, M. S. F. Mental Health Working Group Shifting to Tele-Mental Health in humanitarian and crisis settings: an evaluation of Médecins Sans Frontières experience during the COVID-19 pandemic. Confl Health. 2022 Mar 14;16(1):6. doi: 10.1186/s13031-022-00437-1. https://conflictandhealth.biomedcentral.com/articles/10.1186/s13031-022-00437-1 .10.1186/s13031-022-00437-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Dimitris MC, Gittings M, King NB. How global is global health research? A large-scale analysis of trends in authorship. BMJ Glob Health. 2021 Jan 26;6(1):e003758. doi: 10.1136/bmjgh-2020-003758. https://gh.bmj.com/lookup/pmidlookup?view=long&pmid=33500263 .bmjgh-2020-003758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Shore J. Managing Virtual Hybrid Psychiatrist-Patient Relationships in a Digital World. JAMA Psychiatry. 2020 May 01;77(5):541–542. doi: 10.1001/jamapsychiatry.2020.0139. doi: 10.1001/jamapsychiatry.2020.0139.2762527 [DOI] [PubMed] [Google Scholar]
- 109.Shore J, Schneck CD, Mishkind MC. Telepsychiatry and the Coronavirus Disease 2019 Pandemic-Current and Future Outcomes of the Rapid Virtualization of Psychiatric Care. JAMA Psychiatry. 2020 Dec 01;77(12):1211–1212. doi: 10.1001/jamapsychiatry.2020.1643. doi: 10.1001/jamapsychiatry.2020.1643.2765954 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart.
Impact of COVID-19 on mental health services: summary of key findings.
World distribution of 101 included papers.
Characteristics of 72 papers on face-to-face services.


