Abstract
Purpose:
The randomized phase III coBRIM study (NCT01689519) demonstrated improved progression-free survival (PFS) and overall survival (OS) with addition of cobimetinib to vemurafenib compared with vemurafenib in patients with previously untreated BRAFV600 mutation–positive advanced melanoma. We report long-term follow-up of coBRIM, with at least 5 years since the last patient was randomized.
Patients and Methods:
Eligible patients were randomized 1:1 to receive either oral cobimetinib (60 mg once daily on days 1–21 in each 28-day cycle) or placebo in combination with oral vemurafenib (960 mg twice daily).
Results:
495 patients were randomized to cobimetinib plus vemurafenib (n = 247) or placebo plus vemurafenib (n = 248). Median follow-up was 21.2 months for cobimetinib plus vemurafenib and 16.6 months for placebo plus vemurafenib. Median OS was 22.5 months (95% CI, 20.3–28.8) with cobimetinib plus vemurafenib and 17.4 months (95% CI, 15.0–19.8) with placebo plus vemurafenib; 5-year OS rates were 31% and 26%, respectively. Median PFS was 12.6 months (95% CI, 9.5–14.8) with cobimetinib plus vemurafenib and 7.2 months (95% CI, 5.6–7.5) with placebo plus vemurafenib; 5-year PFS rates were 14% and 10%, respectively. OS and PFS were longest in patients with normal baseline lactate dehydrogenase levels and low tumor burden, and in those achieving complete response. The safety profile remained consistent with previously published reports.
Conclusions:
Extended follow-up of coBRIM confirms the long-term clinical benefit and safety profile of cobimetinib plus vemurafenib compared with vemurafenib monotherapy in patients with BRAFV600 mutation–positive advanced melanoma.
Translational Relevance.
Extended follow-up of the phase III coBRIM study of cobimetinib plus vemurafenib confirms the positive benefit/risk profile of cobimetinib plus vemurafenib in patients with BRAFV600 mutation–positive metastatic melanoma. With at least 5 years of follow-up since the last patient was randomized, results continue to demonstrate substantial progression-free survival and overall survival benefits for cobimetinib plus vemurafenib compared with vemurafenib monotherapy. The long-term safety profile is consistent with previously published reports, with no new safety signals detected. Among patients treated with cobimetinib plus vemurafenib, greatest overall survival benefit is observed in patients who achieve a complete response, and in those with normal lactate dehydrogenase levels and low tumor burden at baseline. Novel treatment strategies are needed to improve long-term outcomes for patients in poor prognosis subgroups, particularly those with elevated lactate dehydrogenase levels at baseline.
Introduction
In the last several years, combination regimens of BRAF- and MEK-targeted agents have improved treatment outcomes in patients with BRAFV600 mutation–positive metastatic melanoma (1–3). Long-term follow-up data from studies of BRAF and/or MEK inhibitors show that about a third of participating patients derive prolonged survival benefit from these regimens (4–7). Long-term follow-up of patients with BRAF inhibitor–naïve BRAFV600 mutation–positive metastatic melanoma in the phase Ib BRIM7 study of the cobimetinib plus vemurafenib combination showed that the overall survival (OS) rate plateaued at 39.2% at years 4 and 5 (4). Similarly, a pooled analysis of patients receiving dabrafenib plus trametinib in the COMBI-d and COMBI-v studies showed OS rates of 37% and 34% at 4 and 5 years, respectively (5). It is of interest to characterize and identify prognostic factors associated with the long-term survival benefits of these treatments, both to inform treatment decisions and to identify new unmet needs for this patient population.
The phase III coBRIM study evaluated the combination of cobimetinib plus vemurafenib compared with placebo plus vemurafenib in previously untreated patients with advanced melanoma harboring BRAFV600 mutations (1). In the primary analysis, with a median follow-up of 7.3 months, median progression-free survival (PFS) was 9.9 versus 6.2 months with cobimetinib plus vemurafenib versus placebo plus vemurafenib [hazard ratio (HR), 0.51; 95% confidence interval (CI), 0.39–0.68; P < 0.001]; OS data were immature (1). With a median follow-up of 14.2 months, updated PFS analysis showed that median PFS had improved to 12.3 months with cobimetinib plus vemurafenib versus 7.2 months with placebo plus vemurafenib (HR, 0.58; 95% CI, 0.46–0.72; P < 0.0001; ref. 8). With a median follow-up of 18.5 months, the final OS analysis showed that cobimetinib plus vemurafenib significantly improved median OS versus placebo plus vemurafenib (22.3 vs. 17.4 months; HR, 0.70; 95% CI, 0.55–0.90; P = 0.005; ref. 8).
Herein, we present the extended follow-up analysis of the coBRIM study, after patients were followed for at least 5 years since the last patient was randomized, evaluating long-term treatment outcomes and prognostic characteristics of patients who derived long-term benefit from this regimen.
Patients and Methods
Study design and patients
The coBRIM study was a multicenter, randomized, double-blind, placebo-controlled, phase III study that evaluated the efficacy and safety of the combination of cobimetinib plus vemurafenib compared with placebo plus vemurafenib. The study was conducted at 135 sites in the United States, Australia, New Zealand, Israel, and Europe. Detailed methods have previously been published, and the protocol is available online (1). Briefly, eligible patients were aged 18 years or older and had histologically confirmed unresectable stage IIIC or stage IV melanoma harboring a BRAFV600 mutation detected using the cobas® 4800 BRAF V600 Mutation Test (Roche Molecular Systems); measurable disease as per Response Evaluation Criteria In Solid Tumors version 1.1 (RECIST v1.1; ref. 9); Eastern Cooperative Oncology Group performance status (ECOG PS) of 0 or 1; and adequate hematologic, hepatic, renal, and cardiac function. Patients with previously treated brain metastases were eligible if they had a history of stable disease for at least 3 weeks.
This study was registered with ClinicalTrials.gov (NCT01689519) and was conducted in accordance with the provisions of the Declaration of Helsinki and Good Clinical Practice guidelines. The protocol and its amendments were approved by the local institutional review board or independent ethics committee at each study site. All patients provided written informed consent.
Treatment
Patients were randomized in a 1:1 ratio to receive either oral cobimetinib (60 mg once daily for 21 days followed by a 7-day rest period in each 28-day cycle) or placebo in combination with oral vemurafenib (960 mg twice daily), with stratification by disease stage and geographic region. Treatment was continued until disease progression, death, unacceptable toxicity, or withdrawal of consent. Following the primary analysis, the protocol was amended to allow patients in the placebo plus vemurafenib arm to cross over to the cobimetinib plus vemurafenib arm at the discretion of the investigator if they did not have disease progression and had not discontinued vemurafenib. Modification of the cobimetinib or vemurafenib dose was permitted for management of adverse events (AE). Tumor assessments were performed at baseline and every 8 weeks thereafter. Safety was monitored throughout treatment until 28 days after the last dose of study medication; thereafter, safety reporting included deaths, serious AEs (including new primary cancers), and other AEs of concern considered to be related to prior treatment with study medication. Safety data were regularly reviewed by an independent data and safety monitoring committee.
Outcomes
For the long-term follow-up analysis, outcomes of interest were OS (time from randomization until death from any cause), PFS (time from randomization until disease progression per RECIST v1.1 as assessed by the investigator or death from any cause), confirmed objective response rate (proportion of patients with complete response or partial response per RECIST v1.1), response duration (time from first documentation of response until disease progression or death from any cause), and safety.
Statistical analysis
Patients were enrolled between January 8, 2013 and January 31, 2014. The study was terminated by the sponsor because all patients had at least 5 years of follow-up from the time of randomization, with a final data cutoff date of July 21, 2019. All efficacy analyses were conducted in the intent-to-treat (ITT) population according to original randomized treatment assignment. Safety was assessed in patients who received at least one dose of study treatment according to the actual treatment received. PFS and OS were estimated using the Kaplan–Meier method. OS analyses were performed with and without censoring of data for patients in the placebo plus vemurafenib arm who crossed over to cobimetinib plus vemurafenib. HRs and two-sided 95% CIs were estimated using a stratified Cox proportional hazards model.
Exploratory analyses were performed to evaluate PFS and OS outcomes in subgroups defined by baseline lactate dehydrogenase (LDH) level (normal vs. elevated) and confirmed best overall response per RECIST v1.1 (complete response vs. partial response vs. nonresponders). OS outcomes were further analyzed in cobimetinib plus vemurafenib–treated patients according to prognostic subgroups previously identified by Hauschild and colleagues [normal LDH level and sum of the product of longest diameters of target lesions (SLD) ≤45 mm; normal LDH level and SLD >45 mm; elevated LDH level ≤2× upper limit of normal (ULN) and ECOG PS 0; elevated LDH level ≤2× ULN and ECOG PS ≥1; and elevated LDH level >2× ULN; ref. 10] or Long and colleagues (normal LDH level and <3 organ sites; normal LDH level and ≥3 organ sites; elevated LDH level ≤2× ULN and ECOG PS 0; elevated LDH level ≤2× ULN and ECOG PS ≥1; and elevated LDH level >2× ULN; ref. 11).
Data sharing statement
Qualified researchers may request access to individual patient level data through the clinical study data request platform (https://vivli.org/). Further details on Roche's criteria for eligible studies are available here (https://vivli.org/members/ourmembers/). For further details on Roche's Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents, see here (https://www.roche.com/research_and_development/who_we_are_how_we_work/clinical_trials/our_commitment_to_data_sharing.htm).
Results
A total of 495 eligible patients were enrolled and randomized to receive either cobimetinib plus vemurafenib (n = 247) or placebo plus vemurafenib (n = 248). Two patients, one in each arm, were randomized into the study but did not receive any study treatment. Sixteen patients from the placebo plus vemurafenib arm crossed over to the cobimetinib plus vemurafenib arm following the primary analysis. Baseline characteristics were well balanced between treatment arms (Supplementary Table S1).
At data cutoff, median follow-up duration was 21.2 months [interquartile range (IQR), 10.4–59.0] in the cobimetinib plus vemurafenib arm and 16.6 months (IQR, 7.3–42.5) in the placebo plus vemurafenib arm. The most common reasons for discontinuation from the study were death (64% vs. 67%) and withdrawal by patient (8.5% vs. 8.1%) in the cobimetinib plus vemurafenib arm versus the placebo plus vemurafenib arm (Table 1), whereas the most common reasons for discontinuation of study treatment were progressive disease (58% vs. 76%) and AEs (17% vs. 9%).
Table 1.
Patient disposition.
| Patient disposition, n (%) | Placebo + vemurafenib | Cobimetinib + vemurafenib |
|---|---|---|
| Study disposition | n = 248 | n = 247 |
| Discontinued from studya | 248 (100) | 247 (100) |
| Death | 167 (67) | 157 (64) |
| Lost to follow-up | 8 (3) | 4 (2) |
| Withdrawal by patient | 20 (8) | 21 (9) |
| Physician decision | 1 (<1) | 4 (2) |
| Other | 4 (2) | 2 (1) |
| Treatment disposition | n = 245 | n = 248 |
| Discontinued study treatment | 245 (100) | 248 (100) |
| Progressive disease | 185 (76) | 145 (58) |
| Adverse event | 21 (9) | 43 (17) |
| Death | 3 (1) | 4 (2) |
| Other | 19 (8) | 56 (23) |
aForty-eight patients in the placebo + vemurafenib arm and 59 patients in the cobimetinib + vemurafenib arm remained on study at the time of study termination.
Among patients who discontinued study treatment for reasons other than death, 122/240 patients (51%) in the cobimetinib plus vemurafenib arm and 130/227 patients (57%) in the placebo plus vemurafenib arm received subsequent anticancer treatments (Table 2), including immunotherapy (34% vs. 41%), targeted therapy (16% vs. 18%), and chemotherapy (14% vs. 16%).
Table 2.
Subsequent anticancer treatments.a
| Subsequent treatment, n (%) | Placebo + vemurafenib (n = 227) | Cobimetinib + vemurafenib (n = 240) |
|---|---|---|
| ≥1 subsequent treatment | 130 (57) | 122 (51) |
| Chemotherapy | 36 (16) | 33 (14) |
| Targeted therapy | 40 (18) | 38 (16) |
| BRAF inhibitor | 25 (11) | 21 (9) |
| Combined BRAF and MEK inhibitor | 16 (7) | 19 (8) |
| MEK inhibitor | 1 (<1) | 3 (1) |
| Immunotherapy | 94 (41) | 82 (34) |
| Ipilimumab | 83 (37) | 53 (22) |
| Anti–PD-1 agents | 42 (19) | 44 (18) |
| Ipilimumab plus anti–PD-1 | 4 (2) | 6 (3) |
| Other | 1 (<1) | 0 |
aIn patients who discontinued study treatment for reasons other than death.
Overall survival
At the time of data cutoff, 157/247 patients (64%) in the cobimetinib plus vemurafenib arm and 167/248 patients (67%) in the placebo plus vemurafenib arm had died. Median OS was 22.5 months (95% CI, 20.3–28.8) with cobimetinib plus vemurafenib and 17.4 months (95% CI, 15.0–19.8) with placebo plus vemurafenib (Fig. 1A). Landmark OS rates with cobimetinib plus vemurafenib versus placebo plus vemurafenib were 38% (95% CI, 32–45) versus 31% (95% CI, 25–37) at 3 years, 34% (95% CI, 28–40) versus 29% (95% CI, 23–35) at 4 years, and 31% (95% CI, 25–37) versus 26% (95% CI, 20–32) at 5 years. Results were similar when patients who crossed over to treatment with cobimetinib plus vemurafenib were censored at the date of crossover (Supplementary Table S2).
Figure 1.
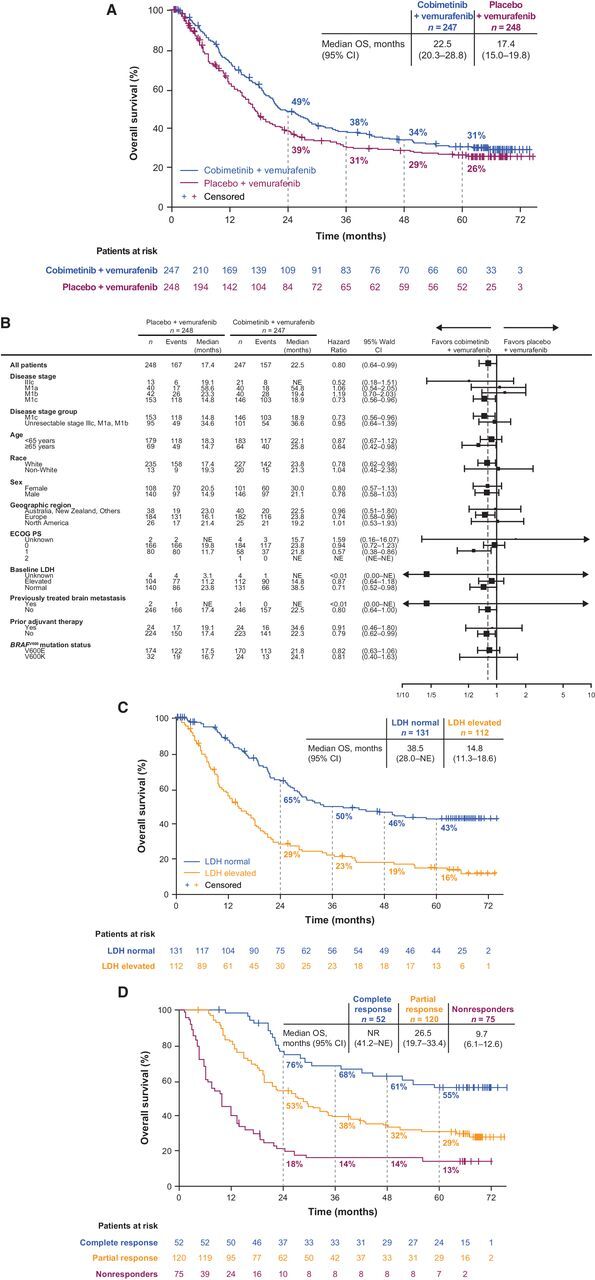
Overall survival. A, Kaplan–Meier curve of overall survival in the ITT population. B, Forest plot of hazard ratios for overall survival across patient subgroups. C, Overall survival in cobimetinib plus vemurafenib–treated patients with normal versus elevated LDH levels at baseline. D, Cobimetinib plus vemurafenib–treated patients who achieved complete response or partial response versus nonresponders.
A trend for OS benefit for cobimetinib plus vemurafenib over placebo plus vemurafenib was observed in most of the prespecified subgroups (Fig. 1B). Among patients treated with cobimetinib plus vemurafenib, median OS was 38.5 months [95% CI, 28.0 months to not estimable (NE)] for patients with normal baseline LDH level versus 14.8 months (95% CI, 11.3–18.6 months) for patients with elevated baseline LDH level; 5-year landmark OS rates were 43% and 16%, respectively (Fig. 1C). Among patients treated with cobimetinib plus vemurafenib, median OS was prolonged in patients who achieved a confirmed best response of complete response (not reached; 95% CI, 41.2–NE) or partial response (26.5 months; 95% CI, 19.7–33.4) compared with nonresponders (9.7 months; 95% CI, 6.1–12.6), with 5-year landmark OS rates of 55%, 29%, and 13%, respectively (Fig. 1D).
In cobimetinib plus vemurafenib–treated patients analyzed according to subgroups identified by Hauschild and colleagues (ref. 10; Fig. 2A), OS was most favorable in patients with normal baseline LDH and SLD ≤45 mm and least favorable in those with elevated baseline LDH >2× ULN (Fig. 2B). Five-year OS rates were 52% in patients with normal LDH and SLD ≤45 mm, 34% in those with normal LDH and SLD >45 mm, 22% in those with elevated LDH ≤2× ULN and ECOG PS 0, 15% in those with elevated LDH ≤2× ULN and ECOG PS ≥1, and could not be evaluated in those with elevated LDH >2× ULN because almost all patients had died by 3 years.
Figure 2.
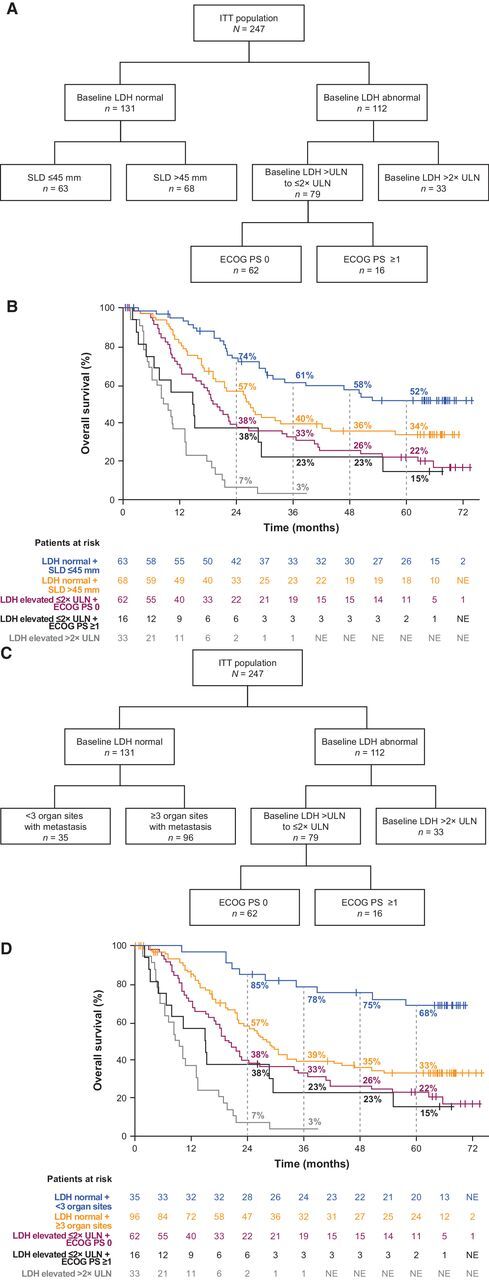
Overall survival outcomes by prognostic subgroups. A, Decision tree for prognostic subgroups identified by Hauschild et al. (10) in cobimetinib plus vemurafenib–treated patients. B, Kaplan–Meier curves of overall survival across prognostic subgroups identified by Hauschild et al. (10) in cobimetinib plus vemurafenib–treated patients. C, Decision tree for prognostic subgroups identified by Long et al. (11) in cobimetinib plus vemurafenib–treated patients. D, Kaplan–Meier curves of overall survival across prognostic subgroups identified by Long et al. (11) in cobimetinib plus vemurafenib–treated patients.
According to subgroups identified by Long and colleagues (ref. 11; Fig. 2C), OS outcomes in the cobimetinib plus vemurafenib arm were most favorable in patients with normal baseline LDH and <3 organ sites with metastases and least favorable in those with elevated baseline LDH >2× ULN (Fig. 2D). Five-year OS rates were 68% in patients with normal LDH and <3 organ sites, 33% in those with normal LDH and ≥3 organ sites, 22% in those with elevated LDH ≤2× ULN and ECOG PS 0, 15% in those with elevated LDH ≤2× ULN and ECOG PS ≥1, and could not be evaluated in those with elevated LDH >2× ULN because almost all patients had died by 3 years.
Progression-free survival
At data cutoff, 195/247 patients (79%) in the cobimetinib plus vemurafenib arm and 207/248 patients (83%) in the placebo plus vemurafenib arm had PFS events (disease progression per investigator assessment or death). Median PFS was 12.6 months (95% CI, 9.5–14.8) with cobimetinib plus vemurafenib and 7.2 months (95% CI, 5.6–7.5) with placebo plus vemurafenib (Fig. 3A). Landmark PFS rates with cobimetinib plus vemurafenib compared with placebo plus vemurafenib were 23% (95% CI, 17–28) versus 13% (95% CI, 9–18) at 3 years, 17% (95% CI, 12–22) versus 12% (95% CI, 8–16) at 4 years, and 14% (95% CI, 9–19) versus 10% (95% CI, 6–14) at 5 years.
Figure 3.
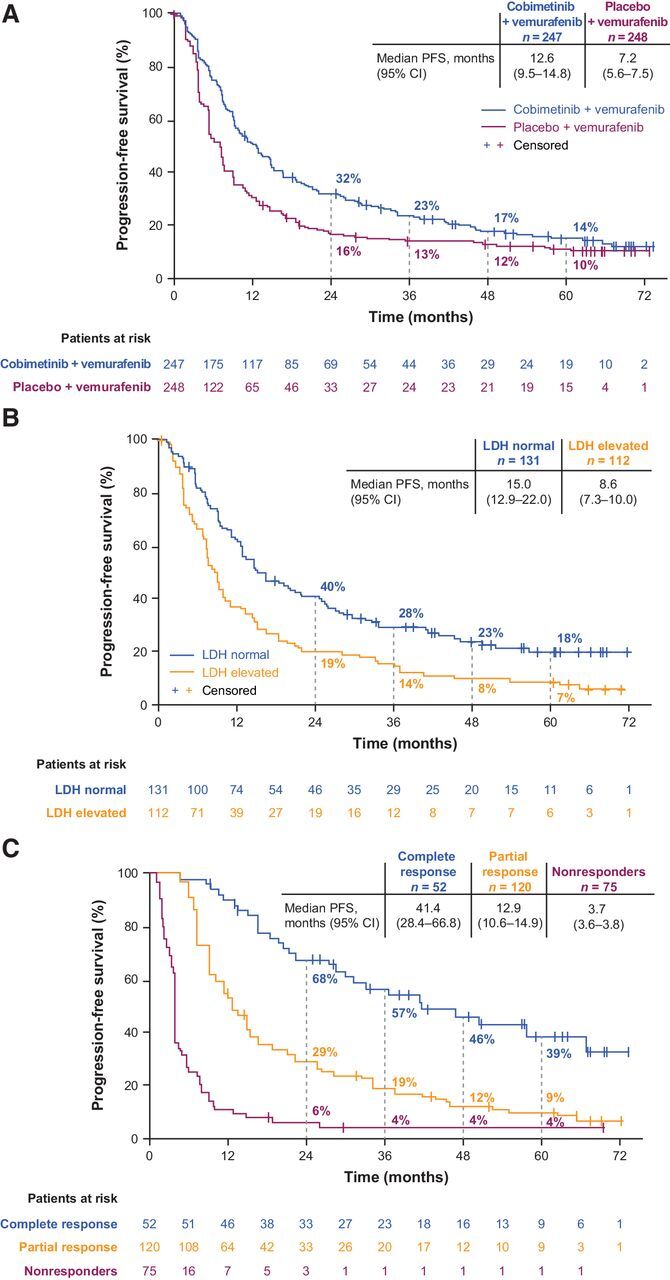
Progression-free survival. A, Kaplan–Meier curves of progression-free survival in the ITT population. B, Cobimetinib plus vemurafenib–treated patients with normal versus elevated LDH levels at baseline. C, Cobimetinib plus vemurafenib–treated patients who achieved complete response or partial response versus nonresponders.
Among patients treated with cobimetinib plus vemurafenib, median PFS was longer for patients with normal LDH level at baseline (15.0 months; 95% CI, 12.9–22.0) compared with those with elevated baseline LDH level (8.6 months; 95% CI, 7.3–10.0; Fig. 3B). Among patients treated with cobimetinib plus vemurafenib, median PFS was longer in patients who achieved a confirmed best response of complete response (41.4 months; 95% CI, 28.4–66.8) or partial response (12.9 months; 95% CI, 10.6–14.9) compared with nonresponders (3.7 months; 95% CI, 3.6–3.8; Fig. 3C).
Best overall response
In the cobimetinib plus vemurafenib arm, a best overall response of confirmed objective response was achieved in 172/247 patients (70%), with complete response in 52 patients (21%) and partial response in 120 patients (49%; Supplementary Table S3). In the placebo plus vemurafenib arm, 123/248 patients (50%) achieved confirmed objective response, with complete response in 32 patients (13%) and partial response in 91 (37%; Supplementary Table S3). In both treatment arms, the complete response rate improved with longer follow-up. In the cobimetinib plus vemurafenib arm, complete response rates improved from 10% at the primary analysis to 16% at the updated PFS analysis and 21% in the current analysis. In the placebo plus vemurafenib arm, the complete response rate improved from 4% at the primary analysis to 11% at the updated PFS analysis and 13% at the current analysis. The median duration of response was 14.7 months (95% CI, 12.9–19.3) in the cobimetinib plus vemurafenib arm and 9.2 months (95% CI, 7.5–12.9) in the placebo plus vemurafenib arm.
Safety
At data cutoff, median duration of cobimetinib treatment was 275 days (range, 4–2,245) and median duration of vemurafenib treatment was 281 days (range, 9–2,246) for patients in the cobimetinib and vemurafenib arm; median duration of vemurafenib treatment for patients in the placebo plus vemurafenib arm was 175 days (range, 5–2,268).
Treatment-emergent AEs of any grade occurred in 246/248 patients (99%) in the cobimetinib plus vemurafenib arm and 240/245 patients (98%) in the placebo plus vemurafenib arm. AEs occurring in ≥20% patients in either arm are shown in Table 3. Grade ≥3 AEs occurred in 194/248 patients (78%) in the cobimetinib plus vemurafenib arm and 155/245 patients (63%) in the placebo plus vemurafenib arm. The difference in grade ≥3 AE rates between arms was largely attributable to laboratory abnormalities of gamma glutamyltransferase (GGT) increased (15% vs. 10%), alanine aminotransferase (ALT) increased (12% vs. 6%), and blood creatine phosphokinase (CPK) increased (12% vs. <1%; Table 3).
Table 3.
Most common AEs,a regardless of attribution to study treatment.
| Placebo + vemurafenib (n = 245) | Cobimetinib + vemurafenib (n = 248) | |||
|---|---|---|---|---|
| AEs, n (%) | Any grade | Grade ≥3 | Any grade | Grade ≥3 |
| Diarrhea | 81 (33) | 3 (1) | 152 (61) | 17 (7) |
| Nausea | 65 (27) | 2 (1) | 108 (44) | 3 (1) |
| Rash | 95 (39) | 14 (6) | 104 (42) | 14 (6) |
| Arthralgia | 103 (42) | 12 (5) | 96 (39) | 7 (3) |
| Fatigue | 83 (34) | 8 (3) | 93 (38) | 11 (4) |
| Blood CPK increased | 7 (3) | 1 (<1) | 91 (37) | 30 (12) |
| Photosensitivity reaction | 47 (19) | 0 | 86 (35) | 8 (3) |
| Pyrexia | 60 (24) | 0 | 79 (32) | 4 (2) |
| Vomiting | 34 (14) | 2 (1) | 69 (28) | 4 (2) |
| ALT increased | 44 (18) | 14 (6) | 68 (27) | 29 (12) |
| AST increased | 30 (12) | 4 (2) | 66 (27) | 23 (9) |
| GGT increased | 43 (18) | 25 (10) | 59 (24) | 38 (15) |
| Decreased appetite | 49 (20) | 1 (<1) | 55 (22) | 0 |
| Asthenia | 43 (18) | 3 (1) | 52 (21) | 5 (2) |
| Anemia | 22 (9) | 8 (3) | 51 (21) | 10 (4) |
| Hypertension | 24 (10) | 7 (3) | 51 (21) | 21 (8) |
| Pruritus | 47 (19) | 1 (<1) | 51 (21) | 3 (1) |
| Headache | 40 (16) | 4 (2) | 50 (20) | 2 (1) |
| Blood alkaline phosphatase increased | 25 (10) | 4 (2) | 47 (19) | 14 (6) |
| Alopecia | 75 (31) | 1 (<1) | 42 (17) | 1 (<1) |
| Myalgia | 31 (13) | 6 (2) | 42 (17) | 1 (<1) |
| Rash maculopapular | 38 (16) | 13 (5) | 39 (16) | 18 (7) |
| Dermatitis acneiform | 22 (9) | 3 (1) | 37 (15) | 6 (2) |
| Ejection fraction decreased | 11 (4) | 3 (1) | 32 (13) | 5 (2) |
| Pain in extremity | 39 (16) | 6 (2) | 32 (13) | 3 (1) |
| Hyperkeratosis | 75 (31) | 6 (2) | 31 (13) | 1 (<1) |
| Basal cell carcinoma | 6 (2) | 6 (2) | 16 (6) | 15 (6) |
| Hyponatremia | 3 (1) | 1 (<1) | 13 (5) | 7 (3) |
| Dehydration | 2 (1) | 0 | 13 (5) | 6 (2) |
| Squamous cell carcinoma of skin | 33 (13) | 33 (13) | 10 (4) | 9 (4) |
| Lipase increased | 4 (2) | 2 (1) | 9 (4) | 8 (3) |
| Pneumonia | 5 (2) | 2 (1) | 7 (3) | 6 (2) |
| Keratoacanthoma | 23 (9) | 23 (9) | 5 (2) | 5 (2) |
aAEs of any grade occurring in ≥20% of patients and AEs of grade ≥3 occurring in ≥2% of patients in either treatment arm.
Protocol-defined AEs of special interest (AESI) were actively monitored during the study. AESIs that were more common in the cobimetinib plus vemurafenib arm compared with the placebo plus vemurafenib arm were retinal detachment or central serous retinopathy (27% vs. 5%), grade ≥3 photosensitivity (4% vs. 0), grade ≥3 liver laboratory abnormalities (25% vs. 15%), grade ≥2 ejection fraction reduction (13% vs. 4%), and grade ≥3 CPK elevation (12% vs. 1%). Fewer patients in the cobimetinib plus vemurafenib arm had any cutaneous primary malignancy compared with the placebo plus vemurafenib arm (13% vs. 23%). Grade ≥3 rash (17% vs. 17%) and grade ≥3 QTc interval prolongation (2% vs. 2%) occurred in similar numbers of patients in each treatment arm.
Serious AEs occurred in 105/248 patients (42%) with cobimetinib plus vemurafenib and 71/245 patients (29%) with placebo plus vemurafenib. Serious AEs occurring in ≥2% of patients in either arm were pyrexia (3% vs. 1%), pneumonia (2% vs. 1%), and dehydration (2% vs. 0). Grade 5 AEs occurred in 6/248 patients (2%) in the cobimetinib plus vemurafenib arm [cardiac arrest, pneumonia, death (unknown), coma, Clostridium difficile colitis, and myocardial infarction] and 5/245 patients (2%) in the placebo plus vemurafenib arm [cardiac failure, pulmonary embolism, atelectasis, death (unknown), and hemorrhagic stroke].
AEs leading to discontinuation of any study drug occurred in 67/248 patients (27%) in the cobimetinib plus vemurafenib arm and 30/245 patients (12%) in the placebo plus vemurafenib arm. AEs leading to discontinuation of cobimetinib or placebo in ≥2% of patients were aspartate aminotransferase (AST) increased (2% vs. <1%), ejection fraction decreased (2% vs. 1%), and rash (2% vs. <1%) in the cobimetinib plus vemurafenib arm versus the placebo plus vemurafenib arm. AEs leading to discontinuation of vemurafenib in ≥2% of patients were AST increased (2% vs. 1%), ALT increased (2% vs. 1%), GGT increased (2% vs. 2%), and rash (2% vs. <1%).
Discussion
This extended follow-up of the phase III coBRIM study confirms both the long-term clinical benefit and the safety profile of cobimetinib plus vemurafenib in patients with BRAFV600 mutation–positive metastatic melanoma. With at least 5 years of follow-up since the last patient was randomized, results continue to demonstrate substantial PFS and OS benefits for cobimetinib plus vemurafenib compared with vemurafenib monotherapy. The safety profile was consistent with previously published reports (1, 8), with no new safety signals detected over extended follow-up.
The 5-year OS rate of 31% for cobimetinib plus vemurafenib is consistent with that reported with the combination of dabrafenib plus trametinib (34%) in a pooled analysis of the COMBI-d and COMBI-v studies (5). Similar to the COMBI-d and COMBI-v pooled analysis, we observed a plateauing of both PFS and OS curves from approximately 3 years, suggesting favorable survival outcomes for a substantial proportion of patients treated with the combination. Moreover, the 5-year OS rates for cobimetinib plus vemurafenib in patients with normal and elevated LDH (43% and 16%, respectively) were identical to those achieved with dabrafenib plus trametinib in the pooled analysis of the COMBI-d and COMBI-v studies (5). Similar proportions of patients across these studies received subsequent anticancer treatment with immunotherapy or further targeted therapy. Although the extent to which long-term OS is influenced by subsequent treatment is unclear, recent analyses suggest that patients who progress following treatment with BRAF and/or MEK inhibitors derive an OS benefit from subsequent treatment with immunotherapy or additional targeted therapy (12).
Identification of subgroups of patients likely to achieve long-term treatment benefit is important to inform treatment decisions in the management of patients with metastatic melanoma. Conventional prognostic factors for survival in patients with metastatic melanoma include disease stage, baseline LDH levels, and baseline ECOG PS (13, 14). Recent analyses suggest that LDH level at baseline remains the most important prognostic factor for survival in patients treated with targeted therapy or immunotherapy (10, 11, 15, 16). Consistent with these findings, we observed longer PFS and OS for cobimetinib plus vemurafenib–treated patients with normal LDH levels (below ULN) at baseline compared with those who had elevated LDH levels at baseline. In accordance with previous prognostic models in patients with metastatic melanoma treated with BRAF and MEK inhibitor combination therapy, long-term OS was most favorable in patients with normal LDH levels and low tumor burden (defined as either SLD ≤45 mm or <3 organ sites with metastasis; refs. 10, 11). The majority of these patients had long-term survival with cobimetinib plus vemurafenib therapy, with 5-year OS rates of 52% in the subgroup defined by normal baseline LDH and SLD ≤45 mm, and 68% in the subgroup defined by normal baseline LDH and <3 organ sites. The 5-year OS rate of 68% in patients with normal baseline LDH and <3 organ sites treated with cobimetinib plus vemurafenib in the current study compares favorably with the 5-year OS rate of 55% for this subgroup of patients treated with dabrafenib plus trametinib (5). Conversely, patients with elevated baseline LDH >2× ULN had the least favorable long-term OS outcomes, with less than 3% of patients surviving beyond 3 years.
A previous pooled analysis of four studies in patients with BRAFV600-mutated metastatic melanoma treated with vemurafenib or cobimetinib plus vemurafenib (BRIM-2, BRIM-3, BRIM-7, and coBRIM) demonstrated that greater depth of response was associated with improved survival (17). Among patients treated with cobimetinib plus vemurafenib in the coBRIM study, those who achieved complete response had the best long-term survival outcomes, with 5-year PFS and OS rates of 39% and 55%, respectively, compared with 14% and 31%, respectively, in the overall population. PFS and OS outcomes remained unfavorable in patients who did not achieve objective response, with 5-year PFS and OS rates of only 4% and 13%, respectively, representing an area of unmet need. It was also demonstrated that with at least 5 years of follow-up, complete response rates had increased compared with rates in the primary analysis (1) in both the cobimetinib plus vemurafenib arm (21% vs. 10%) and the placebo plus vemurafenib arm (13% vs. 4%), indicating a beneficial long-term effect with BRAF and MEK inhibitor therapy.
Novel treatment strategies are needed to improve long-term outcomes for patients in poor prognosis subgroups, particularly those with elevated LDH levels at baseline. One strategy that has been investigated is the addition of immune-checkpoint inhibitors to BRAF inhibitor plus MEK inhibitor combination therapy. Recently, the phase III IMspire150 study demonstrated that the combination of atezolizumab plus vemurafenib plus cobimetinib improved investigator-assessed PFS compared with placebo plus vemurafenib plus cobimetinib (median, 15.1 vs. 10.6 months; HR, 0.78; 95% CI, 0.63–0.97; log-rank P = 0.025) in patients with BRAFV600 mutation–positive advanced melanoma (18). Interestingly, exploratory analyses suggested that the treatment benefit observed with atezolizumab plus vemurafenib plus cobimetinib was more pronounced among patients with elevated LDH levels at baseline in the subgroup of patients whose tumors did not express PD-L1 (19). However, long-term outcomes are not yet available and further analyses are needed to evaluate subgroups of patients who may benefit from triplet combination therapy.
This extended analysis of the randomized phase III coBRIM study, with at least 5 years since the last patient was randomized and a relatively low dropout rate, allows robust estimation of long-term OS outcomes. Limitations include the potential confounding effect of postprogression treatments on OS outcomes, the retrospective exploratory nature of analyses according to prognostic subgroups, and the potential influence of immortal time bias on analysis of survival outcomes according to best overall response.
Long-term follow-up efficacy and safety data continue to support a positive benefit/risk balance for cobimetinib plus vemurafenib compared with placebo plus vemurafenib. The OS results confirmed the long-term OS benefit in patients treated with cobimetinib plus vemurafenib compared with placebo plus vemurafenib in patients with previously untreated, BRAFV600 mutation–positive advanced melanoma. The greatest benefit was observed in patients who achieved a complete response and in those with normal LDH levels and low tumor burden at baseline.
Authors' Disclosures
P.A. Ascierto reports grants from Roche-Genentech during the conduct of the study. P.A. Ascierto also reports grants and personal fees from Bristol Myers Squibb, Roche-Genentech, Array BioPharma, and Sanofi; personal fees and other support from Merck Sharp & Dohme; and personal fees from Novartis, Merck Serono, Pierre Fabre, Incyte, MedImmune, AstraZeneca, Syndax, Sun Pharma, Idera, Ultimovacs, Sandoz, Immunocore, 4SC, Alkermes, Italfarmaco, Nektar, Boehringer Ingelheim, Eisai, Regeneron, Daiichi Sankyo, Pfizer, OncoSec, Nouscom, Takis, Lunaphore, and Seagen outside the submitted work. B. Dréno reports grants from Roche during the conduct of the study. J. Larkin reports personal fees and other support from Roche, Novartis, Bristol Myers Squibb, Pfizer, Immunocore, and Merck Sharpe & Dohme; personal fees from iOnctura, Incyte, Dynavax, CRUK, GSK, Eisai, Merck, touchIME, touchExperts, Iovance, Boston Biomedical, YKT Global, Apple Tree, Pierre Fabre, AstraZeneca, EUSA Pharma, Ipsen, Aptitude, Calithera, Ultimovacs, and Seagen; grants and other support from Achilles, Nektar, Pharmacyclics, and Aveo; and other support from Covance outside the submitted work. A. Ribas reports personal fees from Genentech-Roche during the conduct of the study. A. Ribas also reports personal fees from Amgen, Chugai, Genentech, Merck, Novartis, Roche, Sanofi, Vedanta, 4C Biomed, Apricity, Arcus, Highlight, Compugen, ImaginAb, MapKure, Merus, Rgenix, Lutris, PACT Pharma, Tango, Advaxis, CytomX, Five Prime, RAPT, Isoplexis, and Kite-Gilead, as well as grants from Agilent and Bristol Myers Squibb outside the submitted work. G. Liszkay reports personal fees from Pfizer, Bristol Myers Squibb, Roche, Merck Sharpe & Dohme, and Novartis during the conduct of the study, as well as personal fees from Pfizer, Bristol Myers Squibb, Roche, Merck Sharpe & Dohme, and Novartis outside the submitted work. M. Maio reports other support from University Hospital of Siena–Italy during the conduct of the study, as well as personal fees from Roche, Bristol Myers Squibb, Merck, Incyte, AstraZeneca, Amgen, Pierre Fabre, Eli Lilly, GSK, Sanofi, Alfasigma, and Merck Serono outside the submitted work. M. Mandalà reports personal fees from Novartis, Pierre Fabre, Merck Sharpe & Dohme, Bristol Myers Squibb, and Sanofi outside the submitted work. L. Demidov reports grants from Novartis, as well as personal fees from Novartis, Roche, Bristol Myers Squibb, Merck Sharpe & Dohme, and BIOCAD outside the submitted work. L. Thomas reports other support from Roche during the conduct of the study. L. de la Cruz-Merino reports grants and personal fees from Roche, Merck Sharpe & Dohme, Bristol Myers Squibb, and Novartis, as well as grants from Celgene outside the submitted work. V. Atkinson reports personal fees and non-financial support from Bristol Myers Squibb, as well as personal fees from Merck Sharpe & Dohme, Novartis, Nektar, Roche, QBiotics, and Pierre Fabre outside the submitted work. C. Garbe reports grants and personal fees from Roche during the conduct of the study. C. Garbe also reports personal fees from Amgen, Merck Sharpe & Dohme, and Philogen, as well as grants and personal fees from Bristol Myers Squibb, NeraCare, Novartis, and Sanofi outside the submitted work. H. Li reports other support from Roche Canada during the conduct of the study, as well as other support from Roche Canada outside the submitted work. E. McKenna reports other support from Roche-Genentech outside the submitted work. A. Voulgari reports other support from Roche during the conduct of the study. G.A. McArthur reports other support from Genentech-Roche and Array BioPharma/Pfizer during the conduct of the study. No disclosures were reported by the other authors.
Supplementary Material
Tables S1-S3
Acknowledgments
The study was funded by F. Hoffmann-La Roche Ltd. The authors thank all the patients and their families, and the investigators and research teams who participated in this study. Medical writing and editorial support for this manuscript were provided by Melanie Sweetlove, MSc (ApotheCom, San Francisco, CA, USA), and were funded by F. Hoffmann-La Roche Ltd.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
This article is featured in Highlights of This Issue, p. 5151
Footnotes
Note: Supplementary data for this article are available at Clinical Cancer Research Online (http://clincancerres.aacrjournals.org/).
Authors' Contributions
P.A. Ascierto: Conceptualization, data curation, supervision, investigation, writing–original draft, writing–review and editing. B. Dréno: Conceptualization, resources, data curation, supervision, validation, investigation, visualization, writing–review and editing. J. Larkin: Investigation, writing–review and editing. A. Ribas: Conceptualization, data curation, supervision, investigation, writing–review and editing. G. Liszkay: Resources, validation, investigation, writing–review and editing. M. Maio: Data curation, supervision, investigation, writing–review and editing. M. Mandalà: Resources, data curation, writing–review and editing. L. Demidov: Data curation, writing–review and editing. D. Stroyakovskiy: Investigation, writing–review and editing. L. Thomas: Data acquisition, investigation, writing–review and editing. L. de la Cruz-Merino: Validation, visualization, writing–review and editing. V. Atkinson: Formal analysis, supervision, writing–review and editing. C. Dutriaux: Resources, investigation, writing–review and editing. C. Garbe: Data curation, formal analysis, supervision, writing–review and editing. J. Hsu: Formal analysis, methodology, writing–review and editing. S. Jones: Formal analysis, validation, writing–review and editing. H. Li: Formal analysis, methodology, writing–review and editing. E. McKenna: Formal analysis, methodology, writing–original draft, writing–review and editing. A. Voulgari: Conceptualization, resources, data curation, formal analysis, supervision, writing–original draft, writing–review and editing. G.A. McArthur: Conceptualization, supervision, investigation, methodology, writing–review and editing.
References
- 1. Larkin J, Ascierto PA, Dreno B, Atkinson V, Liszkay G, Maio M, et al. Combined vemurafenib and cobimetinib in BRAF-mutated melanoma. N Engl J Med 2014;371:1867–76. [DOI] [PubMed] [Google Scholar]
- 2. Long GV, Stroyakovskiy D, Gogas H, Levchenko E, de Braud F, Larkin J, et al. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N Engl J Med 2014;371:1877–88. [DOI] [PubMed] [Google Scholar]
- 3. Robert C, Karaszewska B, Schachter J, Rutkowski P, Mackiewicz A, Stroiakovski D, et al. Improved overall survival in melanoma with combined dabrafenib and trametinib. N Engl J Med 2015;372:30–9. [DOI] [PubMed] [Google Scholar]
- 4. Ribas A, Daud A, Pavlick AC, Gonzalez R, Lewis KD, Hamid O, et al. Extended 5-year follow-up results of a phase Ib study (BRIM7) of vemurafenib and cobimetinib in BRAF-mutant melanoma. Clin Cancer Res 2020;26:46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Robert C, Grob JJ, Stroyakovskiy D, Karaszewska B, Hauschild A, Levchenko E, et al. Five-year outcomes with dabrafenib plus trametinib in metastatic melanoma. N Engl J Med 2019;381:626–36. [DOI] [PubMed] [Google Scholar]
- 6. Hauschild A, Ascierto PA, Schadendorf D, Grob JJ, Ribas A, Kiecker F, et al. Long-term outcomes in patients with BRAF V600-mutant metastatic melanoma receiving dabrafenib monotherapy: analysis from phase 2 and 3 clinical trials. Eur J Cancer 2020;125:114–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Robert C, Flaherty K, Nathan P, Hersey P, Garbe C, Milhem M, et al. Five-year outcomes from a phase 3 METRIC study in patients with BRAF V600 E/K-mutant advanced or metastatic melanoma. Eur J Cancer 2019;109:61–9. [DOI] [PubMed] [Google Scholar]
- 8. Ascierto PA, McArthur GA, Dréno B, Atkinson V, Liszkay G, Di Giacomo AM, et al. Cobimetinib combined with vemurafenib in advanced BRAFV600-mutant melanoma (coBRIM): updated efficacy results from a randomised, double-blind, phase 3 trial. Lancet Oncol 2016;17:1248–60. [DOI] [PubMed] [Google Scholar]
- 9. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. [DOI] [PubMed] [Google Scholar]
- 10. Hauschild A, Larkin J, Ribas A, Dréno B, Flaherty KT, Ascierto PA, et al. Modeled prognostic subgroups for survival and treatment outcomes in BRAF V600–mutated metastatic melanoma: pooled analysis of 4 randomized clinical trials. JAMA Oncol 2018;4:1382–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Long GV, Grob JJ, Nathan P, Ribas A, Robert C, Schadendorf D, et al. Factors predictive of response, disease progression, and overall survival after dabrafenib and trametinib combination treatment: a pooled analysis of individual patient data from randomised trials. Lancet Oncol 2016;17:1743–54. [DOI] [PubMed] [Google Scholar]
- 12. Ascierto PA, Ribas A, Larkin J, McArthur GA, Lewis KD, Hauschild A, et al. Impact of initial treatment and prognostic factors on postprogression survival in BRAF-mutated metastatic melanoma treated with dacarbazine or vemurafenib ± cobimetinib: a pooled analysis of four clinical trials. J Transl Med 2020;18:294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dickson PV, Gershenwald JE. Staging and prognosis of cutaneous melanoma. Surg Oncol Clin 2011;20:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Balch CM, Gershenwald JE, Soong S-j, Thompson JF, Atkins MB, Byrd DR, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol 2009;27:6199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Long G, Blank C, Ribas A, Mortier L, Carlino M, Lotem M, et al. Impact of baseline serum lactate dehydrogenase concentration on the efficacy of pembrolizumab and ipilimumab in patients with advanced melanoma: data from KEYNOTE-006. Eur J Cancer 2017;72:S122–S3. [Google Scholar]
- 16. Schadendorf D, Long GV, Stroiakovski D, Karaszewska B, Hauschild A, Levchenko E, et al. Three-year pooled analysis of factors associated with clinical outcomes across dabrafenib and trametinib combination therapy phase 3 randomised trials. Eur J Cancer 2017;82:45–55. [DOI] [PubMed] [Google Scholar]
- 17. Lewis KD, Larkin J, Ribas A, Flaherty KT, McArthur GA, Ascierto PA, et al. Impact of depth of response on survival in patients treated with cobimetinib ± vemurafenib: pooled analysis of BRIM-2, BRIM-3, BRIM-7 and coBRIM. Br J Cancer 2019;121:522–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gutzmer R, Stroyakovskiy D, Gogas H, Robert C, Lewis K, Protsenko S, et al. Atezolizumab, vemurafenib, and cobimetinib as first-line treatment for unresectable advanced BRAFV600 mutation-positive melanoma (IMspire150): primary analysis of the randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2020;395:1835–44. [DOI] [PubMed] [Google Scholar]
- 19. Ascierto PA, Robert C, Lewis K, Gutzmer R, Stroyakovskiy D, Gogas HJ, et al. 1102P clinical benefit in BRAFV600 mutation-positive melanoma defined by programmed death ligand 1 (PD-L1) and/or lactate dehydrogenase (LDH) status: exploratory analyses from the IMspire150 study. Ann Oncol 2020;31:S745. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1-S3


