Abstract
Purpose:
Survival of children with rhabdomyosarcoma that suffer from recurrent or progressive disease is poor. Identifying these patients upfront remains challenging, indicating a need for improvement of risk stratification. Detection of tumor-derived mRNA in bone marrow (BM) and peripheral blood (PB) using reverse-transcriptase qPCR (RT-qPCR) is a more sensitive method to detect disseminated disease. We identified a panel of genes to optimize risk stratification by RT-qPCR.
Experimental Design:
Candidate genes were selected using gene expression data from rhabdomyosarcoma and healthy hematologic tissues, and a multiplexed RT-qPCR was developed. Significance of molecular disease was determined in a cohort of 99 Dutch patients with rhabdomyosarcoma (72 localized and 27 metastasized) treated according to the European pediatric Soft tissue sarcoma Study Group (EpSSG) RMS2005 protocol.
Results:
We identified the following 11 rhabdomyosarcoma markers: ZIC1, ACTC1, MEGF10, PDLIM3, SNAI2, CDH11, TMEM47, MYOD1, MYOG, and PAX3/7-FOXO1. RT-qPCR was performed for this 11-marker panel on BM and PB samples from the patient cohort. Five-year event-free survival (EFS) was 35.5% [95% confidence interval (CI), 17.5%–53.5%] for the 33/99 RNA-positive patients, versus 88.0% (95% CI, 78.9%–97.2%) for the 66/99 RNA-negative patients (P < 0.0001). Five-year overall survival (OS) was 54.8% (95% CI, 36.2%–73.4%) and 93.7% (95% CI, 86.6%–100.0%), respectively (P < 0.0001). RNA panel positivity was negatively associated with EFS (Hazard Ratio = 9.52; 95% CI, 3.23–28.02), whereas the RMS2005 risk group stratification was not, in the multivariate Cox regression model.
Conclusions:
This study shows a strong association between PCR-based detection of disseminated disease at diagnosis with clinical outcome in pediatric patients with rhabdomyosarcoma, also compared with conventional risk stratification. This warrants further validation in prospective trials as additional technique for risk stratification.
Translational Relevance.
This study investigated the clinical relevance of molecular detection of disseminated tumor cells in blood and bone marrow at diagnosis and during treatment in 99 children with rhabdomyosarcoma treated according to the European pediatric Soft tissue sarcoma Study Group (EpSSG) RMS2005 protocol. For molecular detection of disseminated tumor cells in blood and bone marrow, we developed a reverse transcriptase (RT)-qPCR–based, 11-marker RNA panel to detect tumor-derived RNA. RNA panel positivity at diagnosis was of significant prognostic value in children with rhabdomyosarcoma, regardless of the risk group. In patients with metastatic as well as localized disease, RNA positivity was associated with an increased risk of an event. These data suggest that molecular detection of disseminated disease at diagnosis could be of additional value to improve risk stratification.
Introduction
Each year, more than 200 children in Europe are diagnosed with rhabdomyosarcoma (1). In the Netherlands, patients are stratified into risk groups and treated according to the European pediatric Soft tissue sarcoma Study Group (EpSSG) RMS2005 protocol with increasing therapy intensities per risk group. Risk stratification depends on several patient- and tumor-dependent factors, such as age, pathology, postsurgical stage (IRS group), nodal stage, tumor size, and location (2). Presence of metastases is a crucial prognostic factor. Patients with localized disease have a 5-year overall survival (OS) of 75%, and below 40% in patients who present with metastatic disease (3–5). At diagnosis, 84% of patients have localized disease (6). Still, 1 in 3 of these patients will suffer relapse (2, 7, 8).
Metastases are detected by imaging and bone marrow (BM) IHC and cytomorphology (9). BM metastases are present in 6% of patients at diagnosis (10), and 3-year event-free survival (EFS) is poorer for these patients than for patients with metastatic disease not involving the BM (3-year EFS 14% vs. 34%, respectively; ref. 5).
Two main histologic subtypes are described in rhabdomyosarcoma: the embryonal (most common) and the alveolar subtype. In 70% to 80% of alveolar rhabdomyosarcoma, a typical fusion gene exists between the PAX3 or PAX7 and FOXO1 locus and its presence is associated with worse prognosis (11–13). Apart from this translocation, the genetic landscape of rhabdomyosarcoma is heterogeneous. There is a scarcity of recurrent mutations, but various copy number variations and epigenetic modifications are prevalent (14–16). It is possible to detect tumor-derived cell-free DNA in plasma using targeted or whole-genome sequencing techniques (17–19). However, these approaches often require knowledge on aberrations present in a specific patient and sophisticated equipment and data analysis pipelines. Consequently, we chose to focus on tumor cell–specific mRNA transcripts to detect circulating tumor cells, aiming to devise a method to cover the entire spectrum of rhabdomyosarcoma. Reverse-transcriptase qPCR (RT-qPCR) represents a cost-efficient and more sensitive approach than IHC, with detection of up to one positive cell in 1,000,000 nontumor cells (20). MYOD1, MYOG, and PAX3/7-FOXO1fusion genes are known rhabdomyosarcoma markers and the feasibility to detect them with RT-qPCR in peripheral blood (PB) and BM has been shown (21–23). Several studies from smaller cohorts report that the presence of these markers in liquid biopsies at diagnosis and during follow-up might correlate with a poor prognosis (22–24). As MYOD1 and MYOG are heterogeneously expressed in rhabdomyosarcoma, with MYOG predominant in the alveolar subtype (25), and the PAX3/7-FOXO1 fusion gene occurring solely in alveolar rhabdomyosarcomas (11, 13, 21), we sought additional rhabdomyosarcoma-specific mRNA markers.
We aimed to design an RNA panel with the potential to detect all pediatric rhabdomyosarcoma subtypes, and to evaluate whether minimal disseminated disease detection in liquid biopsies can improve risk stratification at diagnosis and response evaluation during treatment and follow-up in these pediatric patients with rhabdomyosarcoma.
Materials and Methods
Patients and samples
We included samples from all consecutive Dutch pediatric patients with rhabdomyosarcoma, enrolled in the EpSSG RMS2005 trial (EudraCT number 2005–000217–35) and treated at the Sophia Children's Hospital, Emma Children's Hospital, and the Princess Máxima Center for Pediatric Oncology; samples were collected between 2006 and 2019. Patients included in the trial until 2017 gave informed consent for sample use in the EpSSG RMS2005 add-on study, minimal disseminated disease monitoring in children with rhabdomyosarcoma (MDD study). Samples from patients recruited between 2017 and July 2019 were included if consent was given for biobanking of stored sample residues following routine clinical testing. RNA from 10 primary rhabdomyosarcomas from patients included in this study and from nine established rhabdomyosarcoma cell lines (RH30, RD, RMS-YM, RUCH2, RUCH3, RH18, RH41, TE617T, HS729T) for assay validation was kindly provided by the Human Genetics department at the Amsterdam UMC location AMC and cDNA was generated. As healthy controls, PB from 47 healthy volunteers and 41 BM samples from children in molecular remission for acute lymphoblastic leukemia were used, as described previously (26, 27).
RNA extraction and reverse transcription
Up to 5 mL of PB and BM, collected in EDTA tubes (BD Biosciences), were centrifuged at 1,375 × g for 10 minutes to separate the cellular fraction from the plasma. For PB, cells were isolated by hemolysis (NH4Cl). BM was run through a Ficoll gradient (Ficoll Paque; GE Healthcare) according to manufacturer's protocol. Cells were counted, aliquoted per 5 to 10 million cells in TRizol (Thermo Fisher Scientific) and stored at −80°C. Isolation of total RNA was performed using Direct-Zol DNA/RNA Miniprep (Zymo Research) following the manufacturer's protocol. For cDNA synthesis, High-Capacity RNA-to-cDNA Kit (Thermo Fisher Scientific) was used according to manufacturer's protocol.
Candidate gene selection
The Megasearch software in R2 (28) was used to search for differentially expressed genes. Candidate genes with high expression in rhabdomyosarcomas and low expression in healthy PB and BM were selected, with at least six log difference in gene expression (Supplementary Fig. S1). Affymetrix expression data on RMS tumors from the Human Genome U133A (HG-U133A) microarray chip (n = 162) and the Affymetrix Human Genome U133p2 (HG-U133p2) microarray chip (n = 9) were compared with expression data on normal PB (n = 108) and BM samples (n = 5). The U133A contained data of 66 aRMS, 66 eRMS (xtstriche), and 30 other RMS (xtschafwell). It also contained data of 5 BM (xtnormal353) and 108 PB (perbloodbev). The U133p2 chip contained data of 9 RMS (versteeg), 9 PB controls (per blood), 12 PB from the general population (bloodasd56), and 5 BM (xtnormal353). The initial search was performed in May 2007 and resulted in 250 genes. Expression of these genes was compared with the HaemAtlas (29), and 62 genes were selected as potential markers, which had low expression in healthy hematopoietic tissues. These 62 candidate markers were then tested in SYBRGreen-based RT-qPCR in the RD and RH30 rhabdomyosarcoma cell lines as previously described (27), and healthy PB (n = 3) and BM (n = 3; Supplementary Table S4). Next, 13 candidate markers were selected with low/no expression in control PB and BM samples and high expression in the rhabdomyosarcoma cell lines for further analysis with RT-qPCR with Taqman probes. After extensive testing on control BM (n = 41) and control PB (n = 47), RMS tumors (n = 10), and RMS cell lines (n = 9), seven new genes on top of the established genes (MYOD1, MYOG, PAX3-FOXO1, and PAX7-FOXO1) were selected for testing of clinical samples using multiplex RT-qPCR with Taqman probes; seven for PB and three for BM (Supplementary Fig. S1).
RT-qPCR
Samples were analyzed using multiplexed RT-qPCR with Taqman probes. Primers and Taqman probes were ordered from Eurogentec (Belgium). Probes were designed using Oligo 7 (Molecular Biology Insights) and Primer Express 3.0.1 (Thermo Fisher Scientific). For MYOD1 and MYOG, we initially used the sequences as published previously and listed in the EpSSG RMS2005 MDD study (23, 30). RT-qPCR was performed on a Viia7 Real-time PCR system using TaqMan Multiplex Master Mix (Thermo Fisher Scientific) for 50 cycles at 60°C. Primer concentration in the reaction was 300 nmol/L and probe concentration 200 nmol/L. The gene Glucuronidase-β (GUSB) was used as a reference gene and normalized against GUSB-plasmid DNA (ipsogen; Qiagen) dilutions (31). All RT-qPCR experiments were carried out at least in duplicate and median values were used. An RH30 calibration curve was used as an exogenous positive control to ascertain the efficiency of each PCR reaction, except for the PAX7-FOXO1 assay for which a CW9019 calibration curve was used (CW9019 cell line courtesy of Dr. F. Barr, NCI).
Sanger sequencing
Sanger sequencing was performed on products amplified by PCR. Further processing and analysis as described previously, on BioEdit software version 7.2.5 (32).
Determining a threshold for positivity in patient samples
For genes with expression in normal hematopoietic tissue, we defined thresholds for positivity using the guidelines for minimal residual disease detection in acute lymphatic leukemia, as defined by the European Study Group (33) and as was described previously by our group in neuroblastoma (27). In short, to correct for differences in RNA input, the Ct value of a marker was normalized to reference gene GUSB. Then, the median ΔCt marker expression in healthy tissue (ΔCt = Ct of marker – Ct of GUSB) was calculated and the threshold for positivity was set 3 Ct above the median ΔCt (Supplementary Fig. S2). A patient sample was scored as positive if the ΔCt of at least one marker in the 11-marker panel was above its threshold.
Statistical analysis
EFS and OS from diagnosis were estimated using Kaplan–Meier's methodology; differences in survival outcomes were assessed with the log-rank test. Association between PCR positivity and EFS/OS was estimated using a multivariate Cox regression model with EpSSG risk group stratification as a prognostic factor (34). To estimate the cumulative incidence of relapse or progressive disease from diagnosis for RNA panel positivity/negativity, a competing risks model with death as competing event was employed (35). Gray's test was used to assess statistical significance difference between the cumulative incidence for the RNA panel groups (36). All analyses for the competing risk model were performed by using the mstate library (37) in the R environment version 4.4 (38). The other statistical analyses were performed in SPSS version 23 and figures were generated in Graphpad Prism version 8.
Results
Assay redesign for MYOD1 detection in liquid biopsies
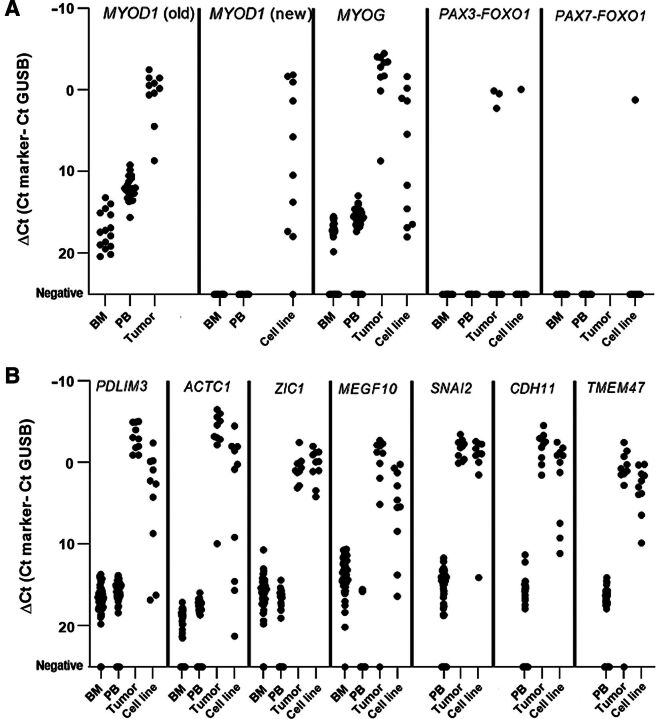
Initial testing detected high background expression using the MYOD1 assay as previously developed by Sartori and colleagues (23) in PB and BM samples from healthy donors (Fig. 1A). Using Sanger sequencing (Supplementary File S1) of the amplicons and RT-qPCR (Supplementary Table S2), we demonstrated that this assay also detected unconverted RNA and genomic DNA. Consequently, we redesigned the forward primer to exclude genomic DNA amplification (Supplementary Table S3; new MYOD1 sequence; Supplementary Table S1). The newly designed MYOD1 assay was shown to be completely tumor specific with no background expression in BM and PB from healthy donors (Fig. 1A) with similar sensitivity (Supplementary Table S3).
Figure 1.
A, Background expression of known markers in control BM and PB, rhabdomyosarcoma (RMS) tumors, and established cell lines. “MYOD1 old design” and MYOG (BM n = 41, PB n = 47, RMS tumors n = 10), “MYOD1 new design” (BM n = 26, PB n = 26, RMS cell lines n = 10), PAX3-FOXO1 fusion gene (BM n = 17, PB n = 10, RMS tumor n = 10, RMS cell lines n = 10), and PAX7-FOXO1 (BM n = 17, PB n = 10, RMS cell lines n = 10). B, Background expression of PDLIM3, ACTC1, and ZIC1 in healthy control BM (n = 41), healthy control PB (n = 47), RMS tumors (n = 10), and RMS cell lines (n = 10). MEGF10, SNAI2, CHD11, and TMEM47 only measured in PB (n = 47), RMS tumors (n = 10), and RMS cell lines (n = 10).
Developing the rhabdomyosarcoma-specific RNA marker panel for testing in liquid biopsies
Candidate markers were selected with high expression in rhabdomyosarcoma and low/no expression in normal PB/BM, as described in the methods (Supplementary Figs. S1 and S3). This selection process identified three new markers for testing in BM and PB (PDLIM3, ACTC1, and ZIC1) in addition to the redesigned MYOD1 and known markers, MYOG and fusions of PAX3 or PAX7 genes with FOXO1 (30). Four new markers were selected for use in blood-based monitoring (SNAI2, CDH11, TMEM47, MEGF10), because background of these markers was high in BM [on SYBR green for SNAI2, CDH11, and TMEM47 and in the Taqman assay for MEGF10 (shown in Supplementary Table S4 and Fig. 1, respectively)].
Thresholds for positivity were set for all markers (Fig. 1), except for MYOD1 and PAX3/7-FOXO1 fusions because these markers were completely tumor specific. Mean Ct values of the 11 markers and the reference gene in 10 primary tumors are shown in Supplementary Table S5. To detect any occult alveolar subtype, because IHC of the primary tumor can be inconclusive and fusion gene status was not available for every patient, we also tested material from patients diagnosed with an embryonal subtype for the PAX3/7-FOXO1 fusion genes. Expression of most selected marker genes in tumor samples was variable, justifying the use of the 11-marker panel to increase sensitivity. We performed a sensitivity assay of RH30 cells (an established rhabdomyosarcoma cell line) in healthy blood cells, which showed a sensitivity of at least one tumor cell in 100,000 healthy blood cells (Supplementary Table S6).
Prospective cohort description
After having established the thresholds for positivity for the marker panel, we tested patient samples. We collected diagnostic BM and PB samples of 99 consecutive patients at diagnosis and follow-up samples from 25 patients (14 BM and 78 PB) treated according to the EpSSG RMS2005 protocol. Median follow-up was 3.5 years (minimum 0.34 – maximum 13.29 years). Patient age and the risk group assigned are shown in Table 1 and Supplementary Table S7. Twenty-seven patients had metastatic disease of which 10 had BM invasion determined by conventional IHC. Twenty-eight patients had the alveolar subtype; PAX3/7-FOXO1 fusion gene status was not recorded in this study. Five-year EFS and OS was 69.7% [95% confidence interval (CI), 59.5–79.9] and 79.9% (95% CI, 70.9–89.9), respectively.
Table 1.
Patient and clinical characteristics with risk group stratification according to the EpSSG RMS2005 trial.
| Number of patients | |
|---|---|
| Age at diagnosis (years) | |
| <1 | 1 |
| 1–10 | 64 |
| >10 | 34 |
| Sex | |
| Female | 38 |
| Male | 61 |
| Histology | |
| Alveolar rhabdomyosarcoma | 28 |
| Botryoid rhabdoyosarcoma | 2 |
| Embryonal rhabdomyosarcoma | 67 |
| Rhabdomyosarcoma not otherwise specified | 1 |
| Spindle cell/leiomyomatous rhabdomyosarcoma | 1 |
| Pathology | |
| Favorable | 71 |
| Unfavorable | 28 |
| Postsurgical tumor staging (IRS grouping) | |
| I | 6 |
| II | 13 |
| III | 53 |
| IV | 27 |
| Tumor size | |
| ≤5 cm | 43 |
| >5 cm | 56 |
| Regional lymph node involvement | |
| No evidence of lymph node involvement | 69 |
| Evidence of regional lymph node involvement | 29 |
| No information about lymph node involvement | 1 |
| Risk group | |
| Low risk | 3 |
| Standard risk | 35 |
| High risk | 29 |
| Very high risk | 5 |
| Metastatic | 27 |
| Site of origin of primary tumor | |
| Orbit | 17 |
| Head/neck | 6 |
| Parameningeal | 21 |
| Bladder prostate | 9 |
| Genitourinary nonbladder prostate | 13 |
| Extremities | 18 |
| Other sites | 15 |
Liquid biopsy–based 11-marker panel detection at diagnosis correlates with clinical outcome
At diagnosis, in 33 of 99 (33.3%) patients molecular disease was detected in PB and/or BM with our 11-marker panel. Primary tumor material was available for 8 patients (Supplementary Table S5). In the samples that tested positive in matched PB and/or BM at diagnosis, most of the markers with a high expression in the primary tumor were also scored as positive in PB and/or BM. Because of low numbers, no statistical analysis was performed. For the 33 RNA-positive patients, paired PB and BM samples were positive in 13 patients, only BM samples were positive in 12 patients, and only PB samples were positive in 8 patients (Supplementary Table S8).
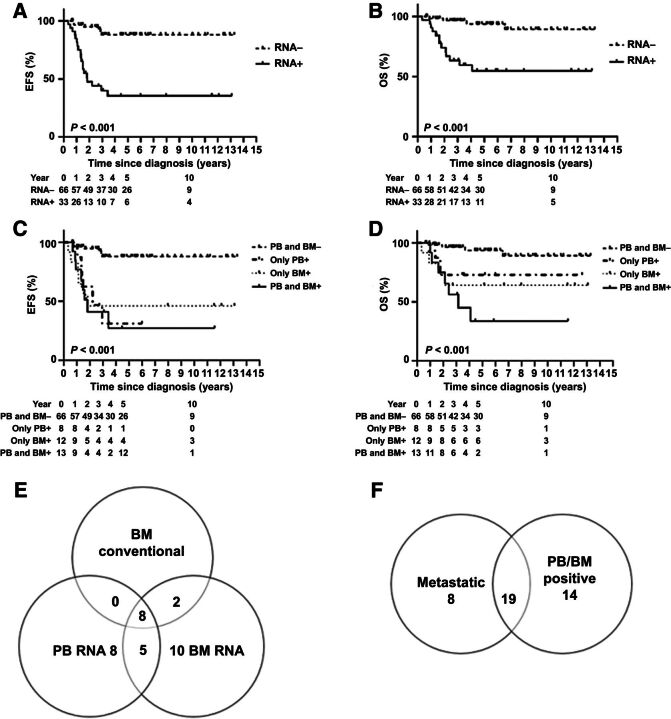
The 5-year EFS was 35.5% (95% CI, 17.5%–53.5%) for the RNA-positive patients, whereas this was 88.0% (95% CI, 78.9%–97.2%) for 66 RNA-negative patients (P < 0.001; Fig. 2A); the 5-year OS was 54.8% (95% CI, 36.2%–73.4%) and 93.7% (95% CI, 86.6%–100.0%), respectively (P < 0.001; Fig. 2B). Patient subgroups defined by molecular detection in BM, PB, and paired BM-PB all show poor EFS and OS (Fig. 2C and D) compared with RNA panel–negative patients. In conclusion, molecular detection of minimal disseminated disease is correlated with outcome.
Figure 2.
RNA positivity (BM and PB) at diagnosis and clinical outcome (A) EFS and (B) OS for SR and RNA panel (C) EFS and (D) OS for patients stratified for PCR testing of BM and PB at diagnosis: negative in PB and BM (PB and BM−), PB positive only (only PB+), BM positive only (only BM+), and positive in PB and BM (PB and BM+). E, Venn diagram depicting number of patients that tested positive with the RNA panel in PB, BM, and by conventional IHC in BM at diagnosis. F, Venn diagram depicting patients that tested positive for PB and/or BM with the RNA panel and patients with metastatic disease, detected by conventional diagnostics at diagnosis.
Liquid biopsy–based molecular detection at diagnosis complements current risk stratification strategies
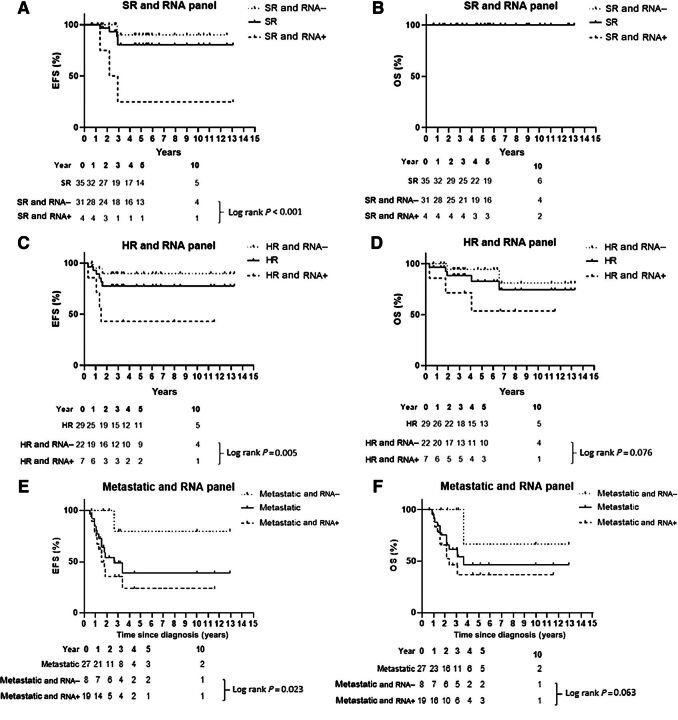
Our patient cohort included 10 patients with BM disease, determined by IHC and cytomorphology. In all 10 BM samples and 8 paired PB samples, tumor-derived mRNA was detected (Fig. 2E). Tumor-derived mRNA in PB/BM was furthermore detected in 23 additional patients (Fig. 2E), among 14 with localized disease and 9 with metastases detected in other sites than the BM (Fig. 2F). Eighteen of the 33 patients testing positive in PB and/or BM had an alveolar subtype. The numbers of patients with low-risk and very high-risk (VHR) disease were too small to allow statistical analyses, so only the larger risk groups [standard risk (SR), high risk (HR), and metastatic disease] according to the risk stratification used in EpSSG RMS2005, were analyzed in relation to RNA panel positivity and survival. There was an association between the risk groups and survival outcomes: within each risk group, RNA panel–negative patients had better outcome than RNA panel–positive patients (Fig. 3A–F).
Figure 3.
RNA positivity at diagnosis and outcome for different risk groups, stratified according RMS2005. Outcome for different risk groups is given as treated (continuous line) and stratified for RNA positivity (RNA+) and RNA negativity (RNA−) at diagnosis. A and B, EFS and OS, respectively, for SR group; please note that no P value is reported since there is no mortality in the SR group. C and D, EFS and OS, respectively, for HR group. E and F, EFS and OS, respectively, for metastatic disease group.
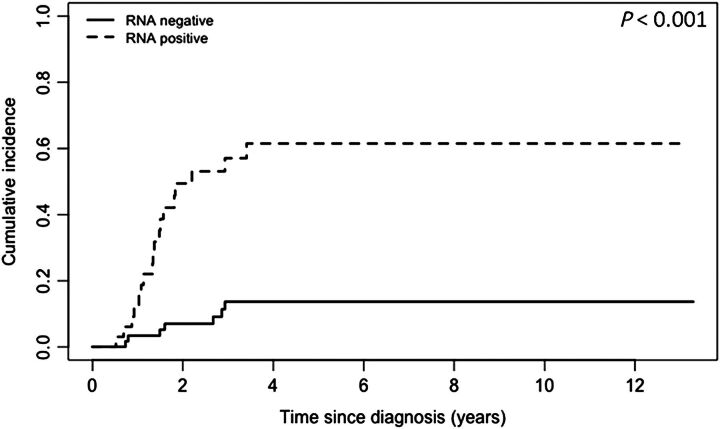
Considering the entire cohort of 99 patients, 6 of 14 (42.9%) patients with localized disease and RNA positivity suffered from relapse (3 localized relapses, 3 metastatic relapses) and 3 eventually died (2 after relapse, 1 due to sepsis during primary treatment), compared with five events in the 58 (8.6%) patients with localized disease without RNA-panel positivity (Supplementary Fig. S4). Molecular disseminated disease was detected in 19/27 (70.3%) patients diagnosed with metastatic disease in bone, BM, lung, and/or distant lymph nodes. Seven of these 19 patients experienced relapse, 5 progressive disease, and 10 eventually died of disease. In contrast, 1 of 8 patients with metastatic disease (6/8 pulmonary lesions and 8/8 distant lymph nodes) and negative for our 11-marker panel, suffered from recurrent disease and later died (Supplementary Fig. S4). The cumulative incidence of the event of interest (relapse/progressive disease) for RNA panel positivity is significantly different (P < 0.001; Fig. 4).
Figure 4.
Cumulative incidence for relapse for RNA-negative/positive patients, as defined at diagnosis. Gray's test was used to compute the P value.
We evaluated the prognostic impact of liquid biopsy–based molecular minimal disease detection at diagnosis on EFS and OS in univariate and multivariate Cox regression models (respectively, Supplementary Table S9 and Table 2) for the largest groups in this cohort (SR, HR, and metastatic disease). Risk factors included in the analysis, that all have prognostic value in univariate analysis, were metastatic disease, positive BM IHC, age above 10 years, alveolar subtype, tumor size, and regional lymph node involvement (Supplementary Table S9). Other clinical characteristics like tumor site and IRS group were not included in this analysis due to low number of patients and/or no events in the subgroups. RNA panel positivity was a prognostic factor for EFS (Hazard Ratio = 9.52; 95% CI, 3.23–28.02), whereas RMS2005 risk group stratification was not, in the multivariate model (Table 2). RNA positivity was also associated with EFS for the other risk factors in multivariate analyses. The low number of events in the SR group in the 5-year follow-up prevented estimation of the effect on OS in multivariate analysis. However in multivariate analyses, the RNA panel was significantly associated with OS, where conventional BM IHC and alveolar subtype was not (Table 2).
Table 2.
Hazard Ratios with 95% CI based on the Cox proportional hazard regression model for EFS and OS.
| EFS | OS | |||
|---|---|---|---|---|
| Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | |
| RNA panel: PB and/or BM positive | 9.52 | 3.23–28.02 | Not possible due to low number of events in Standard Risk group | |
| Standard Risk | 1 | |||
| High Risk | 1.15 | 0.35–3.83 | ||
| Metastatic disease | 1.52 | 0.50–4.66 | ||
| RNA panel: PB and/or BM positive | 8.83 | 3.38–23.10 | 7.13 | 2.19–23.18 |
| Positive BM immunohistochemistry | 0.91 | 0.33–2.54 | 1.22 | 0.37–3.98 |
| RNA panel: PB and/or BM positive | 6.98 | 2.58–18.85 | 4.48 | 1.32–15.15 |
| Metastatic disease | 1.69 | 0.72–3.98 | 3.70 | 1.23–11.16 |
| RNA panel: PB and/or BM positive | 7.71 | 2.85–20.89 | 5.91 | 1.71–20.45 |
| Alveolar rhabdomyosarcoma | 1.29 | 0.55–3.02 | 1.66 | 0.57–4.85 |
| RNA panel: PB and/or BM positive | 8.22 | 3.25–20.78 | 6.21 | 2.00–19.28 |
| Age > 10 years | 2.07 | 0.93–4.61 | 5.65 | 1.92–16.59 |
| RNA panel: PB and/or BM positive | 7.80 | 2.89–21.01 | 4.27 | 1.23–14.87 |
| Regional lymph node involvement | 1.17 | 0.50–2.78 | 3.29 | 1.06–10.18 |
| RNA panel: PB and/or BM positive | 6.63 | 2.53–17.38 | 4.20 | 1.33–13.24 |
| Tumor size >5 cm | 2.33 | 0.83–6.54 | 9.57 | 1.21–75.84 |
CDH11 is an important novel marker
Molecular testing in liquid biopsies revealed differential impact for certain markers, although the number of markers contributing to the positive score in paired BM and PB samples did not correlate with outcome (Supplementary Table S10). MYOD1, PAX3/7-FOXO1, and MYOG were the markers most often contributing to assay positivity in both PB and BM samples (Supplementary Figs. S5 and S6). Interestingly, MYOG was also positive in 3 out of the 15 patients with nonalveolar subtype testing positive at diagnosis; all 3 suffered from an event. CDH11 contributed as single marker to positive scoring in diagnostic blood samples from 6/21 patients (Supplementary Fig. S5); 5 of 6 were histologically diagnosed with an embryonal rhabdomyosarcoma subtype. One of these 6 CHD11-positive patients died of disease and 2 suffered relapses.
The 11-marker panel does not adequately detect minimal residual disease following treatment
We evaluated the potential of the 11-marker panel to detect minimal residual disease in BM and PB samples collected during primary therapy and 5-year follow-up. We tested 42 PB and 4 BM samples from 20 patients during primary treatment (the first 24 weeks after primary diagnosis within the EpSSG RMS2005 trial) and 9 BM and 35 PB samples collected for 20 patients during follow-up after treatment (Supplementary Table S11). For the 19 patients who suffered from an event (15 relapse, 4 progressive disease), blood samples were available at first clinical relapse diagnosis from 10, and tested positive in only 3 patients. BM was available for 5 patients and tested positive in 1 patient (Supplementary Table S11). Although longitudinal blood sampling was not complete for any of these patients, at least two samples were collected for 16 patients during treatment and for 9 patients during follow-up. However, blood samples from only 1 (RMS007) of these 25 patients tested positive for the 11-marker panel during therapy and follow-up. This patient had a complex course with the blood samples at diagnosis, after three chemotherapy cycles, and shortly before death testing positive (Supplementary Table S11). The blood sample following primary treatment was negative; three blood samples during follow-up remained negative even after diagnosis of progressive disease. When tested in a small patient cohort during therapy and follow-up, our 11-marker panel only detected minimal residual disease in a small proportion of patients who experienced an event, even though it clearly identified patients with risk of an event when tested at diagnosis.
Discussion
We present results of the largest prospective study to date detecting minimal disseminated disease in liquid biopsies from pediatric patients with rhabdomyosarcoma, treated according to uniform guidelines. We identified and optimized new mRNA markers for the sensitive detection of tumor-derived mRNA in PB and BM samples and designed an 11-marker RT-qPCR panel assay. The presence of minimal disseminated disease in liquid biopsies at diagnosis correlates with poor outcome in our patient cohort, supporting inclusion of this assay in future studies to further improve risk stratification for children and adolescents diagnosed with rhabdomyosarcoma.
Our 11-marker panel detected BM disease in all BM samples with positive histology, and in addition in 15 BM IHC-negative samples (from 8 patients with localized disease and 7 with metastatic disease without known BM metastasis). Our data concur with findings from Gallego and colleagues (22), who conducted a study in 16 patients (14 localized, 2 metastatic) with the PAX-FOXO1 fusion gene, MYOD1, and acetylcholine receptor as targets for RT-qPCR in PB and BM samples. In their study, all BM samples with positive histology were positive with PCR as well, and six additional BM were only positive with PCR. This points out that PCR-based detection of minimal disseminated disease can help improve the diagnosis of BM metastasis because conventional diagnostics of BM metastasis can be inconclusive. In our cohort, 2 of 8 patients diagnosed with localized disease and molecular disease detected in BM suffered relapse (1 metastatic, 1 localized). An important question for a future validation study of the RNA panel is whether patients diagnosed with occult BM disease detected by PCR alone should be considered for upstaging of their treatment protocol at initial diagnosis. This might spare them additional morbidity due to further treatment for relapse and more importantly increase survival chance, because relapse is associated with lower survival (7, 39, 40).
PCR-based detection of minimal disseminated disease in PB and/or BM has been associated with poor outcome in several smaller studies (22–24), consistent with the very poor patient outcome previously correlated with documented BM metastases (5, 10). We observed a striking decline in OS for patients diagnosed with metastatic disease by both conventional diagnostics and RNA positivity in liquid biopsies. These suggest the existence of an RNA-positive subgroup within the metastatic risk group with an ultrahigh-risk profile, including patients with histologically documented BM metastases and/or alveolar subtype, who could be considered for further therapy intensification. RT-qPCR–based detection alone was not associated with the type of relapse (localized vs. metastatic) in our study. Because metastatic relapse is associated with worse survival (7), this is an interesting question for a follow-up study. Overall, we observe that patients for whom liquid biopsies test positive for the 11-marker panel at diagnosis have a higher risk of suffering an event. This suggests that the use of the RNA panel in addition to conventional strategies at initial diagnosis could improve risk stratification, however this needs to be further investigated in a larger cohort. We made an effort to avoid selection bias, as we included all consecutive patients treated in the participating centers, regardless of risk groups. However, this also resulted in underrepresented subgroups (LR and VHR). A future study in an independent cohort to evaluate whether the use of the RNA panel improves current risk stratification for these risk groups and for patients that would potentially benefit most from improving risk stratification (patients with metastatic disease testing positive for the 11-marker panel) is crucial.
The 11-marker assay was positive in samples collected after start of treatment for only a small number of patients in our cohort. This is in contrast to data from earlier publications (22–24). Sartori and colleagues reported MYOD1 expression in BM samples collected after the first therapy cycle in 5/10 patients (23). Gallego and colleagues and Krskova and colleagues detected MYOD1 and PAX3/7-FOXO1 in proportionately more blood and BM samples collected during treatment and follow-up (22, 24). The use of the MYOD1 assay that also detected genomic DNA complicates the comparison. Gallego and colleagues confirmed the potential for false-positive results by describing discrete but positive expression of MYOD1 in healthy PB (22). Our redesigned MYOD1 assay eliminates false-positive detection from DNA binding. Furthermore, in our study BM samples were important for RNA positivity at diagnosis, but unfortunately only a low number of BM samples after diagnosis was available. Comparison of our cohort, consisting of patients treated completely according to the EpSSG RMS2005 protocol, to these three older studies is further complicated by the distinct treatment protocols patients were subjected to more than a decade ago. The absence of circulating tumor cells in patients from our cohort during treatment or even a change in gene expression due to treatment-driven clonal evolution of the disease (41–43) can be another explanation. Although we already applied a panel of multiple markers, we cannot exclude that during relapse our panel of markers is less sensitive in relapse samples than at diagnosis. Analysis of RNA sequencing data from pretreated tumors might offer further insight into gene expression during treatment. Also, further investigation into the potential of DNA-based techniques to detect minimal residual disease, which have shown great promise in other solid tumors as well as rhabdomyosarcoma, should be pursued (17–19, 44).
Most positively scored samples in our cohort detected the known markers, MYOD1, PAX3/7-FOXO1 fusion, and MYOG. Because of absence of background expression in healthy PB and BM, our redesigned MYOD1 is completely tumor specific, which presents a major advantage compared with other markers. CDH11 was the only marker in our panel that detected additional patients who suffered events later, especially in embryonal rhabdomyosarcoma which is in agreement with a report from 1999, which reports CDH11 as being specific for fusion gene–negative rhabdomyosarcoma cells (45). The majority of the patients with diagnostic liquid biopsies expressing CDH11 test negative for all the other markers. This makes CDH11 an interesting novel marker for detection of minimal disseminated disease in fusion gene–negative tumors and further research should address its potential as a prognostic marker.
Conclusion
Here we demonstrate that RT-qPCR–based detection of minimal disseminated disease in blood and BM samples collected at diagnosis in pediatric patients with rhabdomyosarcoma is associated with survival. We identify CDH11 as an important novel blood-based marker for detection of minimal disseminated disease. The redesigned MYOD1 assay supports highly sensitive rhabdomyosarcoma detection in liquid biopsies. The association between molecularly detected minimal disseminated disease at diagnosis and outcome warrants further investigations into the added value of this 11-marker panel at initial diagnosis on conventional diagnostic strategies to improve risk stratification for treatment of pediatric patients with rhabdomyosarcoma.
Authors' Disclosures
N.S.M. Lak reports grants from Children Cancer Free (KiKa) during the conduct of the study. J.H.M. Merks reports personal fees from Bayer advisory board and GSK advisory board outside the submitted work. No disclosures were reported by the other authors.
Supplementary Material
Supplementary tables and figures
Sanger Sequencing
Acknowledgments
N.S.M. Lak, L. Zappeij-Kannegieter, and J. Stutterheim were supported by the Children Cancer-Free Foundation (KiKa), project number 312. The cell line CW9019 was kindly provided by Dr. F. Barr, NCI, Bethesda, USA. The authors would like to thank Marcel Kool for his contributions in the early phase of this project and Kathy Astrahantseff for her contribution in the editing of this manuscript.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
Footnotes
Note: Supplementary data for this article are available at Clinical Cancer Research Online (http://clincancerres.aacrjournals.org/).
Authors' Contributions
N.S.M. Lak: Data curation, formal analysis, investigation, writing–original draft. T.L. Voormanns: Investigation. L. Zappeij-Kannegieter: Investigation, methodology. L.M.J. van Zogchel: Writing–review and editing. M. Fiocco: Formal analysis, methodology, writing–review and editing. M.M. van Noesel: Writing–review and editing. J.H.M. Merks: Conceptualization, resources, writing–review and editing. C.E. van der Schoot: Conceptualization, supervision, writing–review and editing. G.A.M. Tytgat: Conceptualization, supervision, funding acquisition, methodology, writing–review and editing. J. Stutterheim: Conceptualization, supervision, funding acquisition, investigation, methodology, writing–review and editing.
References
- 1. Gatta G, Botta L, Rossi S, Aareleid T, Bielska-Lasota M, Clavel J, et al. Childhood cancer survival in Europe 1999–2007: results of EUROCARE-5—a population-based study. Lancet Oncol 2014;15:35–47. [DOI] [PubMed] [Google Scholar]
- 2. Bisogno G, Jenney M, Bergeron C, Gallego Melcon S, Ferrari A, Oberlin O, et al. Addition of dose-intensified doxorubicin to standard chemotherapy for rhabdomyosarcoma (EpSSG RMS 2005): a multicentre, open-label, randomised controlled, phase 3 trial. Lancet Oncol 2018;19:1061–71. [DOI] [PubMed] [Google Scholar]
- 3. Oberlin O, Rey A, Sanchez de Toledo J, Martelli H, Jenney ME, Scopinaro M, et al. Randomized comparison of intensified six-drug versus standard three-drug chemotherapy for high-risk nonmetastatic rhabdomyosarcoma and other chemotherapy-sensitive childhood soft tissue sarcomas: long-term results from the International Society of Pediatric Oncology MMT95 study. J Clin Oncol 2012;30:2457–65. [DOI] [PubMed] [Google Scholar]
- 4. Arndt CAS, Bisogno G, Koscielniak E. Fifty years of rhabdomyosarcoma studies on both sides of the pond and lessons learned. Cancer Treat Rev 2018;68:94–101. [DOI] [PubMed] [Google Scholar]
- 5. Oberlin O, Rey A, Lyden E, Bisogno G, Stevens MC, Meyer WH, et al. Prognostic factors in metastatic rhabdomyosarcomas: results of a pooled analysis from United States and European cooperative groups. J Clin Oncol 2008;26:2384–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Weiss AR, Lyden ER, Anderson JR, Hawkins DS, Spunt SL, Walterhouse DO, et al. Histologic and clinical characteristics can guide staging evaluations for children and adolescents with rhabdomyosarcoma: a report from the Children's Oncology Group Soft Tissue Sarcoma Committee. J Clin Oncol 2013;31:3226–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chisholm JC, Marandet J, Rey A, Scopinaro M, de Toledo JS, Merks JH, et al. Prognostic factors after relapse in nonmetastatic rhabdomyosarcoma: a nomogram to better define patients who can be salvaged with further therapy. J Clin Oncol 2011;29:1319–25. [DOI] [PubMed] [Google Scholar]
- 8. Oberlin O, Rey A, Brown KL, Bisogno G, Koscielniak E, Stevens MC, et al. Prognostic factors for outcome in localized extremity rhabdomyosarcoma. Pooled analysis from four international cooperative groups. Pediatr Blood Cancer 2015;62:2125–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dasgupta R, Fuchs J, Rodeberg D. Rhabdomyosarcoma. Semin Pediatr Surg 2016;25:276–83. [DOI] [PubMed] [Google Scholar]
- 10. Bailey KA, Wexler LH. Pediatric rhabdomyosarcoma with bone marrow metastasis. Pediatr Blood Cancer 2020;67:e28219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Barr FG. Gene fusions involving PAX and FOX family members in alveolar rhabdomyosarcoma. Oncogene 2001;20:5736–46. [DOI] [PubMed] [Google Scholar]
- 12. Selfe J, Olmos D, Al-Saadi R, Thway K, Chisholm J, Kelsey A, et al. Impact of fusion gene status versus histology on risk-stratification for rhabdomyosarcoma: Retrospective analyses of patients on UK trials. Pediatr Blood Cancer 2017;64. [DOI] [PubMed] [Google Scholar]
- 13. Anderson J, Gordon T, McManus A, Mapp T, Gould S, Kelsey A, et al. Detection of the PAX3-FKHR fusion gene in paediatric rhabdomyosarcoma: a reproducible predictor of outcome? Br J Cancer 2001;85:831–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Seki M, Nishimura R, Yoshida K, Shimamura T, Shiraishi Y, Sato Y, et al. Integrated genetic and epigenetic analysis defines novel molecular subgroups in rhabdomyosarcoma. Nat Commun 2015;6:7557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Parham DM, Barr FG. Classification of rhabdomyosarcoma and its molecular basis. Adv Anat Pathol 2013;20:387–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Anderson J, Gordon A, Pritchard-Jones K, Shipley J. Genes, chromosomes, and rhabdomyosarcoma. Genes Chromosomes Cancer 1999;26:275–85. [PubMed] [Google Scholar]
- 17. Klega K, Imamovic-Tuco A, Ha G, Clapp AN, Meyer S, Ward A, et al. Detection of somatic structural variants enables quantification and characterization of circulating tumor DNA in children with solid tumors. JCO Precis Oncol 2018;2018:PO.17.00285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Eguchi-Ishimae M, Tezuka M, Kokeguchi T, Nagai K, Moritani K, Yonezawa S, et al. Early detection of the PAX3-FOXO1 fusion gene in circulating tumor-derived DNA in a case of alveolar rhabdomyosarcoma. Genes Chromosomes Cancer 2019;58:521–9. [DOI] [PubMed] [Google Scholar]
- 19. Tombolan L, Zin A, Bisogno G. Cell-free DNA in pediatric rhabdomyosarcoma: potential and challenges. Methods Mol Biol 2019;1909:165–75. [DOI] [PubMed] [Google Scholar]
- 20. Hoon DS, Kuo CT, Wen S, Wang H, Metelitsa L, Reynolds CP, et al. Ganglioside GM2/GD2 synthetase mRNA is a marker for detection of infrequent neuroblastoma cells in bone marrow. Am J Pathol 2001;159:493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Michelagnoli MP, Burchill SA, Cullinane C, Selby PJ, Lewis IJ. Myogenin–a more specific target for RT-PCR detection of rhabdomyosarcoma than MyoD1. Med Pediatr Oncol 2003;40:1–8. [DOI] [PubMed] [Google Scholar]
- 22. Gallego S, Llort A, Roma J, Sabado C, Gros L, de Toledo JS. Detection of bone marrow micrometastasis and microcirculating disease in rhabdomyosarcoma by a real-time RT-PCR assay. J Cancer Res Clin Oncol 2006;132:356–62. [DOI] [PubMed] [Google Scholar]
- 23. Sartori F, Alaggio R, Zanazzo G, Garaventa A, Di Cataldo A, Carli M, et al. Results of a prospective minimal disseminated disease study in human rhabdomyosarcoma using three different molecular markers. Cancer 2006;106:1766–75. [DOI] [PubMed] [Google Scholar]
- 24. Krskova L, Mrhalova M, Hilska I, Sumerauer D, Drahokoupilova E, Mudry P, et al. Detection and clinical significance of bone marrow involvement in patients with rhabdomyosarcoma. Virchows Arch 2010;456:463–72. [DOI] [PubMed] [Google Scholar]
- 25. Dias P, Chen B, Dilday B, Palmer H, Hosoi H, Singh S, et al. Strong immunostaining for myogenin in rhabdomyosarcoma is significantly associated with tumors of the alveolar subclass. Am J Pathol 2000;156:399–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stutterheim J, Gerritsen A, Zappeij-Kannegieter L, Kleijn I, Dee R, Hooft L, et al. PHOX2B is a novel and specific marker for minimal residual disease testing in neuroblastoma. J Clin Oncol 2008;26:5443–9. [DOI] [PubMed] [Google Scholar]
- 27. Stutterheim J, Gerritsen A, Zappeij-Kannegieter L, Yalcin B, Dee R, van Noesel MM, et al. Detecting minimal residual disease in neuroblastoma: the superiority of a panel of real-time quantitative PCR markers. Clin Chem 2009;55:1316–26. [DOI] [PubMed] [Google Scholar]
- 28. R2: Genomics Analysis and Visualization Platform. Available from: http://r2.amc.nl. [Google Scholar]
- 29. Watkins NA, Gusnanto A, de Bono B, De S, Miranda-Saavedra D, Hardie DL, et al. A HaemAtlas: characterizing gene expression in differentiated human blood cells. Blood 2009;113:e1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Carli M, Outcome of consortium meeting within EpSSG. Protocol for detection of minimal disease by quantitative real-time PCR in blood and bone marrow of children with RMS. Final version of the protocol with changes as agreed on Sept 1 (2009) conference call. [Google Scholar]
- 31. Beillard E, Pallisgaard N, van der Velden VH, Bi W, Dee R, van der Schoot E, et al. Evaluation of candidate control genes for diagnosis and residual disease detection in leukemic patients using ‘real-time’ quantitative reverse-transcriptase polymerase chain reaction (RQ-PCR) - a Europe Against Cancer program. Leukemia 2003;17:2474–86. [DOI] [PubMed] [Google Scholar]
- 32. van Wezel EM, Zwijnenburg D, Zappeij-Kannegieter L, Bus E, van Noesel MM, Molenaar JJ, et al. Whole-genome sequencing identifies patient-specific DNA minimal residual disease markers in neuroblastoma. J Mol Diagn 2015;17:43–52. [DOI] [PubMed] [Google Scholar]
- 33. van der Velden VH, Cazzaniga G, Schrauder A, Hancock J, Bader P, Panzer-Grumayer ER, et al. Analysis of minimal residual disease by Ig/TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia 2007;21:604–11. [DOI] [PubMed] [Google Scholar]
- 34. Group EpStsS. Combination chemotherapy in treating young patients with nonmetastatic rhabdomyosarcoma. 2006. Available from: https://clinicaltrials.gov/ct2/show/NCT00379457. [Google Scholar]
- 35. Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Stat Med 2007;26:2389–430. [DOI] [PubMed] [Google Scholar]
- 36. Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. The Annals of Statistics 1988;16:1141–54. [Google Scholar]
- 37. de Wreede LC, Fiocco M, Putter H. An R package for the analysis of competing risks and multi-state models. Journal of Statistical Software 2011;38. [Google Scholar]
- 38. Team RC. R: A language and environment for statistical computing. 2017. [Google Scholar]
- 39. Winter S, Fasola S, Brisse H, Mosseri V, Orbach D. Relapse after localized rhabdomyosarcoma: evaluation of the efficacy of second-line chemotherapy. Pediatr Blood Cancer 2015;62:1935–41. [DOI] [PubMed] [Google Scholar]
- 40. Mascarenhas L, Lyden ER, Breitfeld PP, Walterhouse DO, Donaldson SS, Rodeberg DA, et al. Risk-based treatment for patients with first relapse or progression of rhabdomyosarcoma: a report from the Children's Oncology Group. Cancer 2019;125:2602–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Meacham CE, Morrison SJ. Tumour heterogeneity and cancer cell plasticity. Nature 2013;501:328–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Roerink SF, Sasaki N, Lee-Six H, Young MD, Alexandrov LB, Behjati S, et al. Intra-tumour diversification in colorectal cancer at the single-cell level. Nature 2018;556:457–62. [DOI] [PubMed] [Google Scholar]
- 43. Schulte M, Koster J, Rahmann S, Schramm A. Cancer evolution, mutations, and clonal selection in relapse neuroblastoma. Cell Tissue Res 2018;372:263–8. [DOI] [PubMed] [Google Scholar]
- 44. Chicard M, Colmet-Daage L, Clement N, Danzon A, Bohec M, Bernard V, et al. Whole-exome sequencing of cell-free DNA reveals temporo-spatial heterogeneity and identifies treatment-resistant clones in neuroblastoma. Clin Cancer Res 2018;24:939–49. [DOI] [PubMed] [Google Scholar]
- 45. Markus MA, Reichmuth C, Atkinson MJ, Reich U, Hoffmann I, Balling R, et al. Cadherin-11 is highly expressed in rhabdomyosarcomas and during differentiation of myoblasts in vitro. J Pathol 1999;187:164–72. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary tables and figures
Sanger Sequencing