Abstract
Objective
To determine whether COVID-19 has a significant impact on adequacy of household income to meet basic needs (primary outcome) and work absence due to sickness (secondary outcome), both at the onset of illness (short term) and subsequently (long term).
Design
Multilevel mixed regression analysis of self-reported data from monthly online questionnaires, completed 1 May 2020 to 28 October 2021, adjusting for baseline characteristics including age, sex, socioeconomic status and self-rated health.
Setting and participants
Participants (n=16 910) were UK residents aged 16 years or over participating in a national longitudinal study of COVID-19 (COVIDENCE UK).
Results
Incident COVID-19 was independently associated with increased odds of participants reporting household income as being inadequate to meet their basic needs in the short term (adjusted OR (aOR) 1.39, 95% CI 1.12 to 1.73) though this did not persist in the long term (aOR 1.00, 95% CI 0.86 to 1.16). Exploratory analysis revealed a stronger short-term association among those who reported long COVID, defined as the presence of symptoms lasting more than 4 weeks after disease onset, than those reporting COVID-19 without long COVID (p for trend 0.002). Incident COVID-19 associated with increased odds of reporting sickness absence from work in the long term (aOR 4.73, 95% CI 2.47 to 9.06) but not in the short term (aOR 1.34, 95% CI 0.52 to 3.49).
Conclusions
We demonstrate an independent association between COVID-19 and increased risk of economic vulnerability among COVIDENCE participants, measured by both household income sufficiency and sickness absence from work. Taking these findings together with pre-existing research showing that socioeconomic disadvantage increases the risk of developing COVID-19, this may suggest a ‘vicious cycle’ of impaired health and poor economic outcomes.
Trial registration number
Keywords: COVID-19, Economics, Public health
Strengths and limitations of this study.
Prospective longitudinal study design facilitated identification of temporal relationships between exposures and outcomes.
Detailed demographic data allowed adjustment for multiple potential confounding factors in multivariable analyses.
Rich dataset included two indicators of economic vulnerability to corroborate findings.
Reliance on self-reported variables including COVID-19 test results and sufficiency of income for household needs.
Although large (n=16 910), our study sample was imperfectly representative of the overall UK population.
Introduction
The COVID-19 pandemic has caused global health devastation, with huge mortality and morbidity worldwide. Socioeconomic deprivation was recognised as a major risk factor for incidence and severity of disease prior to the development and roll-out of vaccination against SARS-CoV-2, mediated via factors including increased occupational and household SARS-CoV-2 exposure and greater physical vulnerability due to comorbidities.1–3 This association persists in the vaccination era, with lower socioeconomic status associated with increased incidence and severity of breakthrough COVID-19.4 However, the potential for COVID-19 to act as a cause, rather than a consequence, of economic vulnerability has received less research attention, despite the fact that sustained symptoms following an acute episode (long COVID) are common, with potential to impact negatively on people’s daily activities and capacity to work.5
One of the challenges in characterising effects of COVID-19 on economic well-being relates to the fact that societal measures to control the spread of COVID-19 are detrimental to employment and economic participation, and may therefore have negative economic impacts even in those who do not experience disease themselves.1 6 Prepandemic analyses showed a relationship between economic downturns and increased mortality from causes including mental illness, cancer and postulated ‘deaths of despair’ arising from suicide, drug overdose or alcoholism.7–9 This relationship is not straightforward, as parallel evidence found a decline in cardiovascular and traffic accident mortality during recessions.10 Nonetheless, it is likely that pandemic-related economic contractions affect both health and economic well-being. The Brookings Institute draws a direct link from economic vulnerability to the COVID-19 pandemic, with particular harms from COVID-19-related poverty observed among populations who were already poor.11
In order to dissect out impacts of disease from the consequences of the societal response to the pandemic, we conducted a longitudinal cohort study that was initiated at the start of the pandemic, to determine whether incident COVID-19 was associated with key markers of economic vulnerability. We define economic vulnerability as either the existence or threat of poverty, with the former implying current economic hardship and the latter due to a lack of means to cope with negative economic shocks.12 We capture these aspects of economic vulnerability through two distinct outcomes. Our primary outcome was self-report of whether household income was sufficient to meet basic needs; this outcome captures individuals who consider themselves below the poverty line due to an adverse event.13 Our secondary outcome captured participants’ ability to earn income working by asking whether individuals who developed COVID-19 were more likely to report absence from work due to sickness. Associations between incident COVID-19 and both outcomes were explored contemporaneously (henceforth ‘short term’, ie, at the time when a positive SARS-CoV-2 test result was reported) and subsequently (ie, in the long term).
Methods
Study design, setting and participants
COVIDENCE UK is a prospective cohort study (n=16 910) of COVID-19 in the UK population.14 Its aims are to determine risk factors for incident COVID-19 in the UK population; to characterise the natural history of COVID-19 in the UK population; to evaluate the impact of COVID-19 on the physical, mental and economic well-being of the UK population; and to provide a resource from which to identify potential participants for future clinical trials of interventions to prevent or treat acute respiratory infections.
Inclusion criteria were age ≥16 years and UK residence at the point of enrolment. Recruitment was via a national media campaign across print newspapers, radio, television and online advertising in order to reach a broad sample of the UK population across ages, ethnicities, socioeconomic groups and other correlates of economic vulnerability. Participants initially completed an online baseline questionnaire capturing COVID-19 status and a wide range of demographic, socioeconomic and clinical characteristics described below. Follow-up questionnaires at monthly intervals captured incidence of RT-PCR- or lateral flow test-confirmed SARS-CoV-2 infection, long-term symptoms of COVID-19 (long COVID) and indicators of economic status. The survey comprised a combination of validated demographic questions based on the 2021 UK census,15 self-reported general health16 and other questions developed to specifically capture data relating to COVID-19. These questions were piloted with members of the patient and public involvement group, across a range of ethnicities and other demographic variables. Specific questions from baseline and monthly questionnaires whose responses contributed data to the current analysis are displayed in online supplemental table 1 and online supplemental table 2. The study launched on 1 May 2020, and this paper reports analyses of data collected up to 28 October 2021. All participants who responded to the baseline questionnaire and provided data on SARS-CoV-2 test status and adequacy of household income to meet basic needs in at least 1 monthly follow-up questionnaire were eligible for inclusion in this analysis. Exclusion criteria for this analysis were self-report of a positive SARS-CoV-2 test, long COVID or hospitalisation for COVID-19 prior to completion of the baseline questionnaire, and self-report of long COVID in the absence of a positive RT-PCR or lateral flow test result for SARS-CoV-2.
bmjopen-2022-065083supp001.pdf (1.3MB, pdf)
Definition of variables
Our primary outcome variable was self-report of a participant’s household income being insufficient to meet their basic needs. This was derived as a binary variable based on responses to the question: ‘Since you last checked in with us, has your household income been sufficient to cover the basic needs of your household, such as food and heating?’. Any answer other than ‘yes’ (namely: ‘no’, ‘sometimes’ or ‘mostly’) was coded as indicating insufficient income, while answering ‘yes’ was coded as indicating sufficient income. We also considered a secondary outcome associated with economic vulnerability, namely the ability to participate in the workforce. This was represented by a binary variable derived from responses to the question: ‘Which of the following best describes your current occupational status?’. Participants selecting ‘not working due to sickness, disability or illness’ from a drop-down menu were coded as being absent from work due to sickness.
The following covariates were selected prior to analysis based on their potential to act as confounders of the relationship between incident COVID-19 and study outcomes17: age (classified as ‘working age’ (16 to 65 years) or ‘not working age’ (>65 years)), sex (male vs female, defined by sex assigned at birth), ethnicity (classified as white or minority ethnic origin), country of residence (England, Scotland, Wales or Northern Ireland), Index of Multiple Deprivation (IMD) quartile of residential area,18 baseline occupational status (employed, self-employed, retired, furloughed, unemployed, student, never employed, not working due to sickness/disability/illness or ‘other’), housing status (owns home outright, mortgage holder, private rental, renting from council or other) and self-reported general health (poor, fair, good, very good or excellent).
The principal independent variable of interest for our analysis main model was SARS-CoV-2 test positivity. This was defined by a binary indicator where ‘yes’ included any self-reported positive lateral flow or RT-PCR SARS-CoV-2 test result, and ‘no’ included either a self-reported negative lateral flow or RT-PCR SARS-CoV-2 test result or no report of any test taken. Associations between this variable and our two outcomes of interest were considered over two time periods. First, we built a short-term model to examine contemporaneous effects of COVID-19 by asking whether SARS-CoV-2 test positivity was associated with increased risk of reporting insufficient income or sickness absence in the same month as the positive result was recorded. Second, we built a ‘long-term’ model to test whether a positive SARS-CoV-2 test result was associated with increased risk of reporting insufficient income or sickness absence in subsequent months, excluding the month of infection.
We also conducted two exploratory analyses to determine whether there was a dose–response relationship for associations between COVID-19 severity and risk of reporting insufficient income. This was implemented by categorising participants reporting a positive SARS-CoV-2 test result according to their response to the question “Would YOU say that you currently have long COVID, that is, ongoing symptoms more than four weeks after the onset of proven or suspected COVID-19?”. We compared those reporting long COVID and those reporting a positive SARS-CoV-2 test result but no long COVID to those without a positive SARS-CoV-2 test result (the referent category). Second, we categorised participants reporting a positive SARS-CoV-2 test result according to whether or not they were hospitalised, comparing those reporting hospitalisation for COVID-19 and those reporting COVID-19 not requiring hospitalisation to those without a positive SARS-CoV-2 test result (the referent category). Both of these exploratory analyses were conducted for the short-term and long-term models as described above.
Statistical analysis
Multilevel mixed effects logistic regression models were applied to assess the relationship between positive SARS-CoV-2 test results (RT-PCR or lateral flow) and reported insufficient income at any point prior to 28 October 2021 in the main analysis. A random effect of unique participant identifier was included in all models to account for repeated measures, allowing assessment of within-participant variability. These analyses were adjusted for baseline socio-demographic characteristics as outlined above.
For analyses exploring potential impacts of long COVID and disease precipitating hospitalisation, a random effect for a unique participant identifier was also included to account for repeated measures, with adjustment for baseline characteristics as before, and substitution of the monthly varying binary principal independent variable indicating SARS-CoV-2 test status with one of the other three-level key independent variables as previously defined above (ie, positive SARS-CoV-2 test result with subsequent long COVID, positive SARS-CoV-2 test result without long COVID vs no positive SARS-CoV-2 test result, OR positive SARS-CoV-2 test result with hospitalisation, positive SARS-CoV-2 test result without hospitalisation vs no positive SARS-CoV-2 test result). The models including these 3-level variables were evaluated twice, first as standard categorical variables and then second exchanging categorical versions for numerical integers, which provided a p value for trend for long COVID and hospitalisation due to COVID-19, respectively, for both short-term and long-term models. Models for each of these monthly varying exploratory analyses were built separately from one another, and from the main model which categorised incident COVID as a binary independent variable.
Mixed effects logistic regression models were also applied to assess the relationship between a positive SARS-CoV-2 test result and reported absence from work due to sickness at any point prior to 28 October 2021. The insufficient income variable was not included in this secondary outcome model, and long COVID and hospitalisation were also not considered. Missing data were assumed to be missing completely at random and were handled with listwise deletion in the generalised linear mixed models so that unbiased estimates were obtained. All statistical analyses were conducted using R V.4.1.1 with the mixed effects models conducted using R-package lmer4.
Subgroup analyses
We tested for effect modification by including interaction terms for SARS-CoV-2 test positivity and age (categorised as ≤65 or >65 years) and sex (categorised as male or female at birth) in multivariable models investigating determinants of our primary outcome.
Patient and public involvement
Three patient and public involvement representatives were involved in development of the research questions and the choice of outcome measures specified in the study protocol. One of them also led on development and implementation of strategies to maximise participant recruitment. Results of work will be disseminated to individual participants via a webinar.
Results
A total of 19 980 participants completed the COVIDENCE UK baseline questionnaire between 1 May 2020 and 29 October 2021, of whom 1412 did not complete any subsequent monthly questionnaire. Of the remaining 18 568 participants, 16 910 (91.2%) contributed data to the current analysis. Reasons for exclusion of the 1658 participants who did not contribute data to this analysis are detailed in the participant flow diagram (online supplemental figure S1). Table 1 presents baseline characteristics of participants contributing data to this analysis: their median age was 63 years, 69.8% were female, 94.7% were of White ethnic origin, 2.7% were receiving universal credit payments, 6.9% reported their household income as being ‘sometimes’, ‘mostly’ or ‘not’ sufficient to meet their basic needs in the month prior to enrolment, and 1.7% reported not working due to sickness. Figure 1 illustrates response flows in sufficiency of income to meet basic household needs over time.
Table 1.
Participant characteristics at baseline
| No participants (%) | ||
| Sex | Male | 5106 (30.2) |
| Female | 11 804 (69.8) | |
| Working age | Yes (16 to 65) | 10 338 (61.1) |
| No | 6570 (38.9) | |
| Ethnicity | Minority ethnic | 894 (5.3) |
| White | 16 015 (94.7) | |
| Country | Scotland | 1029 (6.1) |
| Wales | 604 (3.6) | |
| Northern Ireland | 314 (1.9) | |
| England | 14 956 (88.4) | |
| IMD quartile | 1 (most deprived) | 3990 (23.6) |
| 2 | 4191 (24.8) | |
| 3 | 4299 (25.4) | |
| 4 (least deprived) | 4410 (26.1) | |
| Claiming universal credit | Yes | 464 (2.7) |
| No | 16 390 (96.9) | |
| Occupation | Self-employed | 1554 (9.2) |
| Retired | 7547 (44.6) | |
| Furloughed | 386 (2.3) | |
| Unemployed | 296 (1.8) | |
| Student | 345 (2.0) | |
| Other | 394 (2.3) | |
| Never employed | 10 (0.01) | |
| Not working due to sickness | 281 (1.7) | |
| Employed | 6097 (36.1) | |
| Housing | Mortgage | 4250 (25.1) |
| Private renting | 1227 (7.3) | |
| Renting council | 531 (3.1) | |
| Other | 724 (4.3) | |
| Owns home | 10 174 (60.2) | |
| Self-reported general health | Poor | 480 (2.8) |
| Fair | 1808 (10.7) | |
| Good | 4537 (26.8) | |
| Very good | 6691 (39.6) | |
| Excellent | 3394 (20.1) | |
| Income sufficient to cover basic needs | Yes | 15 749 (93.1) |
| Mostly | 617 (3.6) | |
| Sometimes | 147 (0.9) | |
| No | 396 (2.3) | |
1 Missing data: working age (N=2, 0.01%), ethnicity (N=1, <0.01%), country (N=7, 0.04%), IMD quartile (N=20, 0.12%), housing (N=4, 0.02%), universal credit (N=56, 0.3%), income sufficient (N=1, <0.01%).
IMD, Index of Multiple Deprivation.
Figure 1.
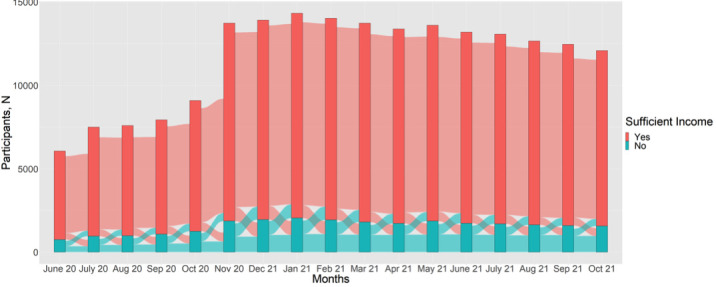
Sankey diagram illustrating response flows in sufficiency of income to meet basic household needs over time.
A total of 1120 participants reported a positive SARS-CoV-2 test result at least once between enrolment and the end of follow-up (28 October 2021). Of these, 39/1120 (3.5%) were hospitalised for COVID-19, and 308/1120 (27.5%) reported long COVID. A total of 7310/16,910 (43.3%) participants reported insufficient income on one or more occasions and 398/16 910 (2.4%) reported absence from work due to sickness on one or more occasions during follow-up (online supplemental table 3).
Incident COVID-19 was independently associated with increased odds of participants reporting household income as being inadequate to meet their basic needs in multivariable analyses in the short term (adjusted OR (aOR) 1.39, 95% CI 1.12 to 1.73) though this did not persist in the long term (aOR 1.00, 95% CI 0.86 to 1.16) (table 2). Of the eight covariates included in each model, independent associations with increased risk of reporting insufficient income were also seen for non-white versus white ethnicity, younger versus older age (≤65 vs >65 years), higher versus lower deprivation quartile, poorer versus better health at baseline, being self-employed, furloughed, other (including sick) or unemployed versus being employed at baseline, and having a mortgage, privately renting, or renting from the council versus owning their home outright. Neither sex nor age modified the association between SARS-CoV-2 test-positivity and reporting insufficient income (for sex, p for interaction=0.23 and 0.51 for short-term and long-term models, respectively; for age, p for interaction=0.48 and 0.14 for short-term and long-term models, respectively).
Table 2.
Determinants of reporting insufficient income during follow-up
| Variable | Response | Short-term responses | Long-term responses | ||
| Adjusted OR (95% CI) | P value | Adjusted OR (95% CI) | P value | ||
| Incident COVID-19 | Yes | 1.39 (1.12 to 1.73) | 0.002 | 1.00 (0.86 to 1.16) | 0.977 |
| No | 1.00 | – | 1.00 | -- | |
| Sex | Male | 1.03 (0.90 to 1.11) | 0.548 | 1.03 (0.93 to 1.15) | 0.564 |
| Female | 1.00 | – | 1.00 | – | |
| Age, years | 16–65 | 1.63 (1.41 to 1.87) | <0.001 | 1.59 (1.39 to 1.83) | <0.001 |
| >65 | 1.00 | – | 1.00 | – | |
| Ethnicity | Minority ethnic | 1.83 (1.49 to 2.27) | <0.001 | 1.85 (1.49 to 2.27) | <0.001 |
| White | 1.00 | – | 1.00 | – | |
| Country | Scotland | 1.01 (0.80 to 1.28) | 0.916 | 1.01 (0.80 to 1.28) | 0.942 |
| Wales | 0.82 (0.61 to 1.09) | 0.164 | 0.82 (0.61 to 1.10) | 0.187 | |
| Northern Ireland | 0.91 (0.62 to 1.31) | 0.588 | 0.91 (0.63 to 1.32) | 0.611 | |
| England (ref) | 1.00 | – | 1.00 | – | |
| IMD quartile | 1 (most deprived) | 1.51 (1.27 to 1.79) | <0.001 | 1.37 (1.17 to 1.60) | <0.001 |
| 2 | 1.26 (1.10 to 1.44) | <0.001 | 1.20 (1.06 to 1.4536) | 0.005 | |
| 3 | 1.04 (0.91 to 1.20) | 0.535 | 1.04 (0.91 to 1.18) | 0.571 | |
| 4 (least deprived, ref) | 1.00 | – | 1.00 | – | |
| Occupation | Self-employed | 1.73 (1.45 to 2.06) | <0.001 | 1.84 (1.54 to 2.19) | <0.001 |
| Retired | 0.63 (0.55 to 0.72) | 0.031 | 0.82 (0.71 to 0.96) | 0.013 | |
| Furloughed | 2.18 (1.60 to 2.97) | <0.001 | 2.17 (1.59 to 2.96) | <0.001 | |
| Unemployed | 7.76 (5.50 to 11.0) | <0.001 | 7.66 (5.43 to 10.83) | <0.001 | |
| Student | 1.15 (0.81 to 1.64) | 0.558 | 1.12 (0.78 to 1.59) | 0.549 | |
| Other/never employed/sick | 2.08 (1.59 to 2.62) | <0.001 | 2.07 (1.61 to 2.66) | <0.001 | |
| Employed (ref) | 1.00 | – | 1.00 | – | |
| Housing | Mortgage | 1.66 (1.45 to 1.89) | <0.001 | 1.53 (1.34 to 1.74) | <0.001 |
| Private renting | 4.55 (3.75 to 5.53) | <0.001 | 4.35 (3.58 to 5.28) | <0.001 | |
| Renting council | 11.6 (8.81 to 15.30) | <0.001 | 11.5 (8.72 to 15.10) | <0.001 | |
| Other | 2.94 (2.28 to 3.79) | <0.001 | 2.77 (2.15 to 3.57) | <0.001 | |
| Owns home (ref) | 1.00 | – | 1.00 | – | |
| Self-reported general health | Poor | 5.32 (3.94 to 7.18) | <0.001 | 5.38 (3.98 to 7.26) | <0.001 |
| Fair | 3.41 (2.84 to 4.09) | <0.001 | 3.47 (2.88 to 4.14) | <0.001 | |
| Good | 1.98 (1.72 to 2.29) | <0.001 | 2.01 (1.74 to 2.33) | <0.001 | |
| Very good | 1.21 (1.06 to 1.39) | 0.003 | 1.23 (1.07 to 1.40) | 0.003 | |
| Excellent (ref) | 1.00 | – | 1.00 | – | |
IMD, Index of Multiple Deprivation.
To explore these findings further, we investigated whether associations between incident COVID-19 and income insufficiency were stronger for the subset of participants who either reported long COVID or who were hospitalised for COVID-19 treatment. Results are shown in table 3: point estimates for aORs in the short-term model were higher for those who reported long COVID or hospitalisation than for those who did not (p values for trend 0.002 for both long COVID and hospitalisation). We also note clinical interest in the direction of association shown in the long term long COVID model (aOR 1.26, 95% CI 0.98 to 1.61) with a CI crossing 1 but leaning in positive direction.
Table 3.
Impact of self-reported long COVID and hospitalisation for COVID-19 on reporting insufficient income during follow-up
| Variable | Response | Short-term responses | Long-term responses | ||
| Adjusted OR (95% CI) | P value | Adjusted OR (95% CI) | P value | ||
| Self-report of long COVID | No COVID-19 (ref) | 1.00 | – | 1.00 | – |
| COVID-19, no long COVID | 1.44 (1.15 to 1.80) | 0.003 | 0.90 (0.75 to 1.08) | 0.263 | |
| Long COVID | 1.50 (1.14 to 1.95) | 0.002 | 1.26 (0.98 to 1.61) | 0.067 | |
| P for trend | – | 0.002 | – | 0.477 | |
| Hospitalisation due to COVID-19 | No COVID-19 (ref) | 1.00 | – | 1.00 | – |
| COVID-19, not hospitalised | 1.37 (1.10 to 1.71) | 0.002 | 0.99 (0.85 to 1.16) | 0.942 | |
| COVID-19, hospitalised | 1.91 (0.694 to 5.25) | 0.220 | 1.38 (0.69 to 2.78) | 0.365 | |
| P for trend | – | 0.002 | – | 0.902 | |
Multivariable regression models fully adjusted for the following baseline variables: sex, age, ethnicity, country, IMD quartile, occupation, housing and self-reported general health.
IMD, Index of Multiple Deprivation.
Finally, we examined whether incident COVID-19 was associated with our secondary outcome of absence from work due to sickness. Results are presented in table 4: incident COVID-19 was associated with increased odds of reporting sickness absence from work in the long term (aOR 4.73, 95% CI 2.47 to 9.06) but not in the short term (aOR 1.34, 95% CI 0.52 to 3.49).
Table 4.
Determinants of reporting 'not working due to sickness’ during follow-up
| Variable | Response | Short-term response | Long-term response | ||
| Adjusted OR (95% CI) | P value | Adjusted OR (95% CI) | P value | ||
| Incident COVID-19 | Yes | 1.34 (0.52 to 3.49) | 0.54 | 4.73 (2.47 to 9.06) | <0.001 |
| No | 1.00 | – | 1.00 | ||
| Sex | Male | 0.58 (0.52 to 2.24) | 0.433 | 0.58 (0.15 to 2.24) | 0.427 |
| Female (ref) | 1.00 | – | 1.00 | – | |
| Working age | Yes (16 to 65) | 14.5 (1.57 to 134.0) | 0.018 | 13.82 (1.48 to 129.30) | 0.021 |
| No (ref) | 1.00 | – | 1.00 | – | |
| Ethnicity | Minority ethnic | 0.76 (0.08 to 6.75) | 0.814 | 0.75 (0.15 to 11.53) | 0.805 |
| White (ref) | 1.00 | – | 1.00 | – | |
| Country | Scotland | 0.44 (0.04 to 5.03) | 0.508 | 0.47 (0.04 to 5.51) | 0.550 |
| Wales | 0.98 (0.07 to 14.80) | 0.992 | 0.95 (0.06 to 14.64) | 0.972 | |
| Northern Ireland | 0.59 (0.03 to 12.11) | 0.731 | 0.57 (0.03 to 12.25) | 0.717 | |
| England (ref) | 1.00 | – | 1.00 | – | |
| IMD quartile | 1 (most deprived) | 1.59 (0.31 to 8.24) | 0.587 | 1.57 (0.30 to 8.28) | 0.594 |
| 2 | 1.06 (0.21 to 5.29) | 0.948 | 1.08 (0.21 to 5.46) | 0.923 | |
| 3 | 1.03 (0.19 to 5.49) | 0.970 | 1.02 (0.19 to 5.47) | 0.986 | |
| 4 (least deprived, ref) | 1.00 | – | 1.00 | – | |
| Housing | Mortgage | 0.76 (0.19 to 3.07) | 0.702 | 0.74 (0.18 to 3.00) | 0.671 |
| Private renting | 1.60 (0.30 to 8.64) | 0.587 | 1.58 (0.29 to 8.58) | 0.595 | |
| Renting council | 8.62 (1.96 to 37.8) | 0.004 | 8.56 (1.92 to 38.19) | 0.005 | |
| Other | 1.56 (0.22 to 11.1) | 0.042 | 1.53 (0.21 to 10.98) | 0.673 | |
| Owns home (ref) | 1.00 | – | 1.00 | – | |
| Self-reported general health | Poor | 94.6 (5.82 to 1540.0) | 0.001 | 101.80 (6.13 to 1689.72) | 0.001 |
| Fair | 17.6 (1.12 to 276.0) | 0.042 | 17.93 (1.12 to 287.80) | 0.042 | |
| Good | 3.86 (0.23 to 66.0) | 0.352 | 3.94 (0.23 to 68.90) | 0.348 | |
| Very good | 2.24 (0.12 to 40.8) | 0.587 | 2.28 (0.12 to 42.57) | 0.580 | |
| Excellent (ref) | 1.00 | – | – | ||
IMD, Index of Multiple Deprivation.
Discussion
To our knowledge, this study is the first to investigate the impact of COVID-19 on subsequent risk of becoming economically vulnerable. We report that incident COVID-19 was independently associated with increased risk of participants reporting insufficient household income in the short term, though not in the long term. This increased odds in the short-term model equates to a 32% increase in risk when the aOR is converted to an adjusted risk ratio (1.32, 95% CI 1.10 to 1.58). The short-term association was stronger where COVID-19 precipitated long COVID or hospitalisation, supporting causal interpretation. Incident COVID-19 was also associated with increased risk of participants reporting absence from work due to sickness in the long term.
Our findings accord with those of studies that have investigated the impact of other infectious diseases on economic outcomes. People living with HIV have been reported to experience higher rates of severe poverty, employment loss and impaired physical and mental functioning.19–21 Similar analyses revealed a link between tuberculosis and increased poverty in both the UK and India.22 23 However, these studies were all cross-sectional in design, leaving uncertainty as to whether the diseases in question were a cause or consequence of the observed poverty.
Our analysis aimed to identify whether there is evidence of an association between these outcomes in a specific direction of causality, that is, from disease to economic vulnerability. The prospective design employed in the current study was valuable to this end, as it allowed us to focus on the timing of onset of the relationship between incident COVID-19 and subsequent economic vulnerability. Demonstration of a dose–response relationship between severity of COVID-19 and the primary outcome, along with consistency of association for two different measures of economic vulnerability (inadequate income and sickness absence) both strengthen the case for causal interpretation.24
Taking these findings together with other research showing that socioeconomic disadvantage increases the risk of developing COVID-19,1–4 our current study represents an important advance by indicating that the relationship between COVID-19 and socioeconomic deprivation may be bidirectional. This suggests a ‘vicious cycle’ of poor health and economic vulnerability which individuals could be pushed into, or accelerated along, by COVID-19. The poorer someone was, is the more likely they were to fall sick. If they did fall sick, they were more likely to experience poverty during the pandemic, with further health risks.
It is notable that incident COVID-19 had a significant negative impact on self-assessed adequacy of household income in the short term, whereas the impact on work absence due to sickness was only evident in the long term. One potential reason for this is that those ill with COVID-19 would still self-classify as ‘employed’ but on temporary leave in the short term, while persistent COVID-19 symptoms might lead to a change in status to official sickness absence. This raises the possibility that COVID-19 may impact economic vulnerability through multiple mechanisms including non-employment-based mechanisms in the short term, such as increased health-related costs and employment-based mechanisms in the longer term. Early, decisive policy interventions could help prevent this potential vicious cycle, with employment advice and other economic support offered alongside healthcare follow-up at hospital discharge.
Our study has several strengths. Its large size afforded ample power to detect potential impacts of COVID-19 on our primary and secondary outcomes, while its population-based recruitment and prospective design maximises generalisability of our findings while allowing us to characterise temporal relationships between exposures and outcomes. Detailed characterisation of participants allowed us to adjust for multiple potential confounding factors in multivariable analyses, and to explore two different indicators of economic vulnerability.
This work also has limitations. First, the variables of interest are all self-reported, including both SARS-CoV-2 test results and indicators of economic vulnerability. Participants were unaware of the hypotheses tested in this work, however, reducing potential for reporter bias to operate. We also relied on reports of voluntary tests, which allows the possibility that some COVID-positive individuals did not receive a test and thus were treated as negative. However, testing was readily available and mandatory for many workplaces and all individuals with symptoms throughout the study period. Participant exclusion criteria also included self-report of long COVID in the absence of a positive RT-PCR or lateral flow test result for ‘SARS-CoV-2’. This minimises the likelihood of a symptomatic individual classified as test-negative. Nonetheless, some with asymptomatic infection may still have been misclassified.
Second, the study population was not perfectly representative of the adult UK population as a whole: males, younger people, people of minority ethnic origin and those with lower educational attainment were all under-represented. Limitations of non-random sampling include potential undetected sampling error, selection bias or motivation bias of participants to engage with the study. Caution is therefore required when extrapolating conclusions beyond the sample population. Further, internet access was a prerequisite to take part, which could limit generalisability of results particularly among the most economically deprived. While this may have limited our power to detect associations within subgroups, we highlight that representativeness is not necessarily a barrier to identification of causal associations in observational epidemiology.25
Fourth, we acknowledge that the precise order of COVID-19 and economic events cannot be guaranteed by our short-term model. We cannot rule out the theoretical possibility that a negative economic shock in the same month preceded COVID-19 infection for some individuals. Nonetheless, this is unlikely to drive the majority of the effect identified, as we do not see a plausible mechanism for an economic shock to precipitate COVID-19 infection in a matter of days. The reverse relationship, where infection precedes economic vulnerability, remains more plausible. We also note that the findings of this short-term model are consistent with both the long COVID and long-term sickness absence models, which increases confidence that COVID-19 infection preceded economic vulnerability for the vast majority of participants considered.
Finally, as with any observational study, residual or unmeasured confounding cannot be ruled out as an explanation for the associations we observe. We handled missing data under the assumption that survey data were missing at random, but it is possible that data were more likely to be missing if someone had COVID-19 or became economically vulnerable. In the most extreme case, fatal or very severe COVID-19 would prevent questionnaire completion; alternatively, someone may have become ill or lost their job then no longer have the cognitive or physical capacity to complete the questionnaires. Conversely, it is possible that SARS-CoV-2 test positivity may have increased the likelihood of participants completing their monthly follow-up questionnaires.
Our findings highlight the need for further research in three areas. First, analogous studies should be done in other populations to determine whether our findings can be replicated; ideally such studies should capture details of longitudinal earnings to introduce greater objectivity and quantification of impacts while reducing reporting bias. Second, further work is needed to understand the specific mechanisms by which COVID-19 may lead to economic vulnerability, investigating the relative importance of factors including lost employment, long COVID symptoms and stigmatisation. Third, our findings suggest the need for further work to explore bidirectional relationships between illness and deprivation more generally.
In conclusion, we report independent associations between incident COVID-19 and subsequent development of economic vulnerability, exposing a previously hidden human cost of the pandemic. Our findings have potentially significant policy implications, given the economic imperative to plan COVID-19-related spending in the most efficient way possible. While a ‘vicious cycle’ of sickness and poverty presents a major threat to well-being, its recognition could also offer an opportunity for effective, early-stage circuit-breaker interventions with potential to avert greater costs in the future.
Supplementary Material
Footnotes
Twitter: @a_williamson1
Contributors: The corresponding author attests that all listed authors meet all four ICMJE authorship criteria and that no others meeting the criteria have been omitted. ARM planned and conducted the COVIDENCE UK study. AEW, FT and ARM wrote the original draft, and KP and AM contributed key intellectual content and critical revisions. FT and KP carried out the statistical analyses. The corresponding author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned (and, if relevant, registered) have been explained. ARM is the study guarantor.
Funding: This study was funded by Barts Charity, ref MGU0466.
Disclaimer: The funder had no role in any aspect of the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/disclosure-of-interest/ and declare: this study was supported by a grant from Barts Charity to ARM (MGU0466). We confirm the independence of researchers from funders and that all authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Deidentified participant data will be made available on reasonable request to ARM (a.martineau@qmul.ac.uk), subject to terms of Research Ethics Committee approval and sponsor requirements.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Leicester South Research Ethics CommitteeEthics approval ID 20/EM/0117. Participants gave informed consent to participate in the study before taking part.
References
- 1.Blundell R, Costa Dias M, Joyce R, et al. COVID-19 and inequalities. Fisc Stud 2020;41:291–319. 10.1111/1475-5890.12232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holt H, Talaei M, Greenig M. Risk factors for developing COVID-19: a population-based longitudinal study (COVIDENCE UK). Thorax. 10.1136/thoraxjnl-2021-217487 [DOI] [PubMed] [Google Scholar]
- 3.Ahmed F, Ahmed Na'eem, Pissarides C, et al. Why inequality could spread COVID-19. Lancet Public Health 2020;5:e240. 10.1016/S2468-2667(20)30085-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Antonelli M, Penfold RS, Merino J, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID symptom study APP: a prospective, community-based, nested, case-control study. Lancet Infect Dis 2022;22:43–55. 10.1016/S1473-3099(21)00460-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Employers NHS. Supporting recovery after long COVID, 2021. Available: https://www.nhsemployers.org/articles/supporting-recovery-after-long-covid
- 6.De Vos J. The effect of COVID-19 and subsequent social distancing on travel behavior. Transp Res Interdiscip Perspect 2020;5:100121. 10.1016/j.trip.2020.100121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burgard SA, Kalousova L. Effects of the great recession: health and well-being. Annu Rev Sociol 2015;41:181–201. 10.1146/annurev-soc-073014-112204 [DOI] [Google Scholar]
- 8.Deaton A, Case A. Deaths of Despair and the Future of Capitalism. Princeton University Press: Princeton, 2020. [Google Scholar]
- 9.Friebel R, Yoo KJ, Maynou L. Opioid abuse and austerity: evidence on health service use and mortality in England. Soc Sci Med 2022;298:114511. 10.1016/j.socscimed.2021.114511 [DOI] [PubMed] [Google Scholar]
- 10.Strumpf EC, Charters TJ, Harper S, et al. Did the great recession affect mortality rates in the metropolitan United States? effects on mortality by age, gender and cause of death. Soc Sci Med 2017;189:11–16. 10.1016/j.socscimed.2017.07.016 [DOI] [PubMed] [Google Scholar]
- 11.Graham C. The human costs of the pandemic: Is it time to prioritize well-being? Brookings Institute, 2020. Available: https://www.brookings.edu/research/the-human-costs-of-the-pandemic-is-it-time-to-prioritize-well-being [Accessed 14 Dec 2021].
- 12.Dercon S. Vulnerability: a micro perspective. Securing development in an unstable world: Annual World Bank Conference on Development Economics, 2006: 117–46. [Google Scholar]
- 13.Chaudhuri S. Assessing vulnerability to poverty: concepts, empirical methods and illustrative examples. New York: Department of Economics, Columbia University, 2003. http://econdse.org/wp-content/uploads/2012/02/vulnerability-assessment.pdf [Google Scholar]
- 14.Talaei M, Faustini S, Holt H, et al. Determinants of pre-vaccination antibody responses to SARS-CoV-2: a population-based longitudinal study (COVIDENCE UK). BMC Med 2022;20:87. 10.1186/s12916-022-02286-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Office for National Statistics . Approach and processes for assuring the quality of the 2021 census data. Available: https://www.ons.gov.uk/census/censustransformationprogramme/approachandprocessesforassuringthequalityofthe2021censusdata
- 16.Ganna A, Ingelsson E. 5 year mortality predictors in 498 103 UK Biobank participants: a prospective population-based study. The Lancet 2015;383:533–40. 10.1016/S0140-6736(15)60175-1 [DOI] [PubMed] [Google Scholar]
- 17.VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol 2019;34:211–9. 10.1007/s10654-019-00494-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ministry of Housing, Communities and Local Government . The English indices of deprivation 2019, 2019. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/853811/IoD2019_FAQ_v4.pdf
- 19.National AIDS Trust . Extreme poverty among people with HIV in the UK increasing, 2010. Available: https://www.nat.org.uk/press-release/extreme-poverty-among-people-hiv-uk-increasing
- 20.Dray-Spira R, Gueguen A, Lert F, et al. Disease severity, self-reported experience of workplace discrimination and employment loss during the course of chronic HIV disease: differences according to gender and education. Occup Environ Med 2008;65:112–9. 10.1136/oem.2007.034363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.APA, HIV/AIDS and Socioeconomic Status . American psychological association, 2010. Available: https://www.apa.org/pi/ses/resources/publications/hiv-aids
- 22.Spence DP, Hotchkiss J, Williams CS, et al. Tuberculosis and poverty. BMJ 1993;307:759–61. 10.1136/bmj.307.6907.759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rajeswari R, Balasubramanian R, Muniyandi M, et al. Socio-Economic impact of tuberculosis on patients and family in India. Int J Tuberc Lung Dis 1999;3:869–77. [PubMed] [Google Scholar]
- 24.Hill AB. The environment and disease: association or causation? Proc R Soc Med 1965;58:295–300. 10.1177/003591576505800503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rothman KJ, Gallacher JEJ, Hatch EE. Why representativeness should be avoided. Int J Epidemiol 2013;42:1012–4. 10.1093/ije/dys223 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-065083supp001.pdf (1.3MB, pdf)
Data Availability Statement
Data are available on reasonable request. Deidentified participant data will be made available on reasonable request to ARM (a.martineau@qmul.ac.uk), subject to terms of Research Ethics Committee approval and sponsor requirements.


