Abstract
Purpose
To determine whether patients insured through Medicaid exhibit differences in patient-reported outcomes, return to sport rates, and reinjury and reoperation metrics after anterior cruciate ligament (ACL) reconstruction compared with patients insured with private insurance.
Methods
Patients insured through Medicaid who had undergone a primary ACL reconstruction were identified and compared with a matched cohort of patients insured through private insurance with the same age and sex. Patients were contacted via telephone and emailed a questionnaire containing the International Knee Documentation Committee (IKDC) score, return to sport questions, and reinjury and reoperation metrics. Physical therapy (PT) notes were also reviewed to determine number of PT visits attended and distance from patients’ home address to PT facility.
Results
A total of 26 patients insured through Medicaid and 25 insured through private insurance were enrolled in this study. The 2 groups demonstrated no statistically significant differences in age, body mass index, or sex. There were no differences in preoperative meniscus injuries or concomitant meniscus repair or meniscectomy procedures between the 2 groups. There were no differences in preoperative IKDC scores; however, the Medicaid group demonstrated a significantly lower postoperative IKDC score (74.7 vs 90.5; P = .005). Patients insured through Medicaid also demonstrated a significantly lower rate of return to sport and attended significantly fewer PT visits following surgery. There were no significant differences in reinjury or reoperation to the index knee between the 2 groups. The threshold number of PT visits for return to sport was determined to be 31.5 visits. Within the private insurance cohort, 17 of 23 patients (73.9%) exceeded this threshold. However, in the Medicaid cohort, 5 of 18 patients (27.8%) exceeded this threshold.
Conclusions
Patients with Medicaid insurance undergoing ACL reconstruction had lower postoperative IKDC scores and were less likely overall to return to sport than their private insurance counterparts at final follow-up in this study. Preoperative IKDC scores, incidence of preoperative meniscus injury, number of concomitant meniscus procedures, average distance from home to PT facility, return to same level of sport, and reinjury and reoperation rate were similar between groups. However, the number of postoperative PT sessions attended by patients insured through Medicaid was significantly lower than private insurance patients.
Level of Evidence
III, retrospective comparative study.
Anterior cruciate ligament (ACL) injuries have an incidence of 68.6 per 100,000 person-years, leading to a significant increase in the rate of ACL reconstruction over time across all age groups.1 Specifically, Buller et al.2 reported the rate of ACL reconstructions increased 37% from 1994 to 2006. Injury to the ACL often leads to significant functional loss and proprioception of the knee joint.3,4 Consequently, the primary goal of ACL injury treatment is to regain stability and improve range of motion to return to sport (RTS) or a high level of functional activity. Reconstruction of the ACL with a graft has a return to preinjury level of sport rate of approximately 65% among athletes after an ACL injury.5 In a longitudinal study with >10-year follow-up, 90% of patients undergoing ACL reconstruction demonstrated normal International Knee Documentation Committee (IKDC) knee scores regarding range of motion, long-term stability, and strength.6 It is known that mental health may impact the results of patient-reported outcomes (PROs); however, PROs are largely accepted as helpful in assessing clinical outcomes after surgery and aiding in the rehabilitation process.7
In the last decade, disparities in health insurance coverage have been observed to influence outcomes of a variety of different orthopaedic procedures. For instance, patients insured through Medicaid undergoing total joint arthroplasty of the hip or knee have been reported to have greater resource use and greater complications rates.8, 9, 10, 11, 12 For those undergoing shoulder arthroplasty procedures, patients insured through Medicaid demonstrated greater complication rates, lower follow-up rates, and inferior postoperative PROs.13, 14, 15 Similarly, multiple studies reported inferior PROs in patients insured through Medicaid who underwent a variety of foot and ankle procedures.16,17 Medicaid insurance status also was observed to negatively impact pain scores in patients undergoing upper-extremity orthopaedic surgeries, as well as result in more resource consumption and greater complication rates in those undergoing surgery to treat proximal humerus fractures.15,18 However, studies investigating this relationship in patients undergoing ACL reconstruction are limited. As Medicaid coverage has expanded over multiple states in the last decade, these disparities in surgical and functional outcomes are especially significant.
Patients insured through Medicaid, a jointly funded federal and state program for individuals whose financial situations is characterized as low or very low income, may have inferior outcomes after surgical procedures due to a lower socioeconomic status and its associated factors shown to impact patient outcomes. For instance, access to physical therapy (PT) is vital to success of postoperative rehabilitation and recovery. This access is affected by the distance that patients live from PT sites, the distance from the surgical facility, access to transportation, ability to take time off work to attend PT, and the number of PT visits covered by insurance in the perioperative period.19 Curry et al.20 examined national disparities in access to PT services after rotator cuff repair surgery between patients insured through Medicaid compared to private insurance. The authors demonstrated there were significantly fewer PT practices that accepted Medicaid compared with private insurance, even in states participating in Medicaid expansion program as part of the Affordable Care Act. As such, patients’ barrier to accessing PT is a critical factor that must be assessed when evaluating and analyzing postoperative patient outcomes.
The purpose of this study was to determine whether patients insured through Medicaid exhibit differences in patient-reported outcomes, RTS rates, and reinjury and reoperation metrics after ACL reconstruction compared with patients insured with private insurance. We hypothesized that patients with Medicaid insurance coverage undergoing ACL reconstruction would have poorer PROs, RTS, and complication rates in comparison to a matched cohort of patients with private insurance.
Methods
Institutional review board approval was obtained from Rush University Medical Center before the initiation of this study. Our prospectively collected intradepartmental registry was queried for all patients who underwent primary arthroscopically assisted ACL reconstruction by 8 surgeons in the practice between January 2014 to December 2020. A prospectively collected PRO database was queried, and patients with Medicaid insurance coverage who had completed outcome scores at 6 months and 1 year were identified. This demonstrated a 28.3% (n = 26/92) compliance rate of PRO data within the Medicaid group. A matching cohort model was used to control for confounding variables by identifying an equal number of patients with the same age and sex who had primary private insurance. Blue Cross Blue Shield was the private insurance carrier used in this matched cohort model as it is the most commonly observed insurance carrier in the practice. Patients undergoing revision procedures, any previous history of treatment with septic arthritis, fracture around the knee, varus or valgus malalignment of more than 10° (including previously corrected with osteotomy in affected limb), or concomitant ligamentous procedures were excluded. Eligible patients were contacted via telephone by a trained research coordinator and consented to participate in the study. Patients were then emailed a Health Insurance Portability and Accountability Act of 1996–compliant and secured link via Microsoft Forms (Microsoft, Redmond, WA) to fill out a questionnaire including IKDC scores and a variety of RTS metrics (Appendix Fig 1, available at www.arthroscopyjournal.org). Patients also were queried regarding reinjury rates in the ipsilateral or contralateral knee as well as any additional surgery in the ipsilateral or contralateral knee. A total of 26 patients with Medicaid insurance and 25 patients with private insurance responded to the survey. There was only 1 patient in the Medicaid group who was not matched to a private insurance counterpart.
Among patients who filled out the survey, the electronic medical record was reviewed to collect patient demographics, including age, sex, body mass index, worker’s compensation status, surgical diagnosis, surgical procedure, date of surgery, time from injury to surgery, number of preoperative PT visits, number of postoperative PT visits, distance (in miles) patient lived from surgical facility, distance (in miles) patient lived from PT facility, and preoperative IKDC scores, when available. The number of PT visits was obtained by PT notes from each individual PT clinic when the surgeon’s clinic notes in the electronic medical record were not clear regarding number of sessions attended. The distance from the surgical facility and PT facility was calculated using Google Maps by inputting the patients’ home address to the respective facility. If the patient went to more than 1 PT facility, the distance of the facility closest to their home address was used.
Patients were grouped according to their insurance payor status at the time of surgery: Medicaid or private insurance (Blue Cross Blue Shield). The primary outcome was postoperative IKDC scores at a minimum of 1-year postoperatively. Secondary outcomes were RTS, duration of RTS, return to same level of sport, reinjury to ipsilateral knee, injury to contralateral knee, additional surgery to ipsilateral or contralateral knee.
Statistical Analysis
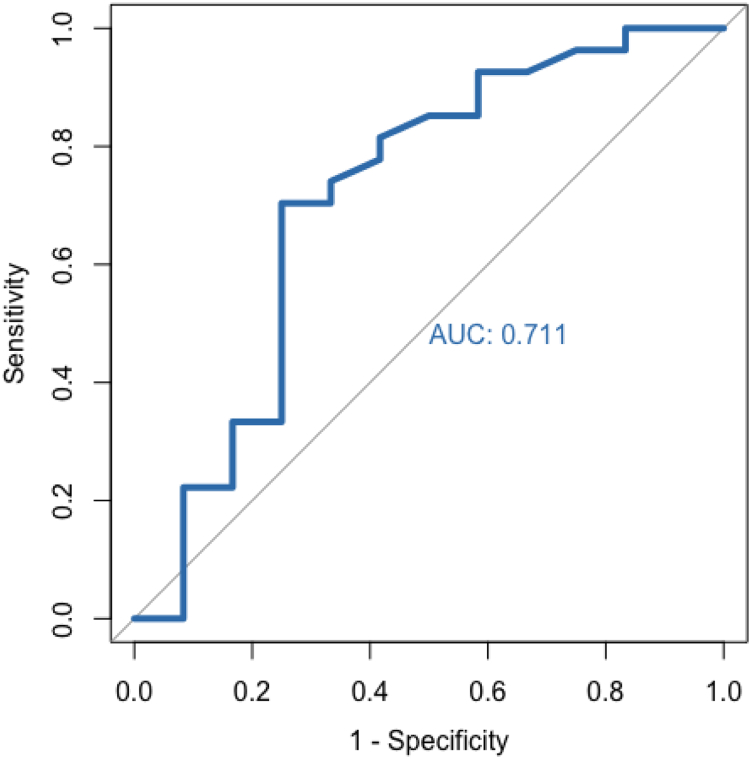
All statistical analysis was performed using RStudio (2021 “Ghost Orchid” Release for macOS). Descriptive statistics are presented as means and standard deviations for continuous variables and counts for categorical variables. Two-tailed paired t-tests were used to determine significant demographic, rehabilitation, and clinical outcome differences between the 2 insurance cohorts. χ2 analysis and the Fisher exact were used to determine baseline differences in meniscus/cartilage injuries between the cohorts, as well as differences in concomitant meniscus repairs or meniscectomies between the cohorts. Linear regression models were used to assess factors predictive of IKDC scores at baseline and follow-up. A generalized logistic regression model was used to determine significant predictors of RTS following surgery for baseline variables such as number of PT visits and distance to PT facility. To quantify a threshold number of PT visits to predict RTS, receiver operating characteristics (ROC) analysis was used based on a generalized logistic regression model. The strength of the model was determined by the area under the curve (AUC) of the ROC curve; an AUC value of ≥0.7 was deemed acceptable, which is consistent with previous studies.21 Optimal cutoffs were determined using the Youden index to maximize sensitivity and specificity of the ROC curve threshold.
Results
A total of 4,263 ACL reconstructions were performed during the study period, 2.2% (n = 92/4,263) of whom were patients insured through Medicaid. Twenty-six patients with Medicaid insurance coverage had completed outcome scores at 6 months and 1 year. This demonstrated a 28.3% (n = 26/92) compliance rate of PRO data within the Medicaid group. A total of 25 patients with private insurance responded to the study survey. There was 1 patient in the Medicaid group who was not matched to a private insurance counterpart.
Medicaid and private cohorts were demographically matched before analysis. Post hoc statistical analysis revealed no differences in age, body mass index, sex distribution, number of meniscus injuries, or number of concomitant meniscus procedures between the 2 cohorts (Table 1). Furthermore, the distance from the patient's home to the surgical site and chronicity of injury at time of surgery were similar between the 2 cohorts.
Table 1.
Demographic and Injury Characteristics of Insurance Cohorts
| Medicaid | Private | P Value | |
|---|---|---|---|
| Age, y | 25.73 ± 10.47 | 27.84 ± 10.97 | .49 |
| BMI | 29.05 ± 6.64 | 26.08 ± 5.32 | .095 |
| Sex, male:female | 12:14 | 11:14 | .88 |
| Meniscus tear, yes:no | 16:10 | 14:11 | .69 |
| Concomitant meniscus procedure, repair:meniscectomy:none | 8:6:12 | 8:6:12 | 1.0 |
| Distance from surgical site, miles | 21.00 ± 28.20 | 29.65 ± 38.82 | .37 |
| Chronicity of injury, acute:chronic∗ | 13:12 | 12:13 | .78 |
NOTE. Continuous variables listed as mean ± standard deviation. Categorical variables listed as counts.
BMI, body mass index.
Chronicity defined as ≥90 days from injury to surgery.
Comparison of the clinical outcomes within the insurance cohorts revealed similar preoperative states on the mean IKDC score; however, at follow-up of at least 1-year postoperatively, the Medicaid cohort demonstrated a significantly lower mean IKDC score (74.68 vs 90.45; P = .005) (Table 2).
Table 2.
Clinical Outcomes Within Insurance Cohorts
| Medicaid | Private | P Value | |
|---|---|---|---|
| Preoperative IKDC | 53.65 ± 21.33 | 53.95 ± 18.35 | .98 |
| Follow-up IKDC | 74.68 ± 24.51 | 90.45 ± 11.18 | .005∗ |
| Average duration of follow-up, mo | 45.23 ± 23.88 | 31.60 ± 13.37 | .016∗ |
NOTE. Continuous variables listed as mean ± standard deviation.
IKDC, International Knee Documentation Committee.
Denotes statistical significance at P < .05.
Comparison of the rehabilitation and RTS patterns between the 2 insurance cohorts revealed a significantly reduced mean number of attended postoperative PT visits in the Medicaid group (24.67 vs 44.04; P = .012), despite similar rates of preoperative rehabilitation (P = 0.503) (Table 3). Furthermore, patients with Medicaid insurance coverage were less likely to RTS following surgery than patients with private insurance (P = .035). However, no differences in rates of return to the same level of sport or return to the same position within their sport were observed.
Table 3.
Rehabilitation, Return to Sport, Reinjury and Additional Surgery Within Insurance Cohorts
| Medicaid | Private | P Value | |
|---|---|---|---|
| Distance from PT site, miles | 9.39 ± 9.00 | 6.72 ± 9.42 | .34 |
| Preoperative rehabilitation, yes:no | 9:17 | 11:14 | .50 |
| Postoperative PT visits | 24.67 ± 21.86 | 44.04 ± 25.23 | .012∗ |
| Return to sport, yes:no | 12:12 | 19:5 | .035∗ |
| Duration of RTS, d | 343.97 ± 127.67 | 292.89 ± 110.38 | .27 |
| Return to same level of sport, yes:no | 9:4 | 13:5 | .96 |
| Return to same position, yes:no | 10:4 | 18:1 | .10 |
| Further injury to ipsilateral knee, yes:no | 2:24 | 4:21 | .37 |
| Further injury to contralateral knee, yes:no | 4:22 | 1:24 | .18 |
| Further surgery on ipsilateral knee, yes:no | 0:26 | 3:22 | .083 |
| Further surgery on contralateral knee, yes:no | 1:25 | 0:25 | .33 |
NOTE. Continuous variables listed as mean ± standard deviation. Categorical variables listed as counts (yes:no). Cell counts may not total to cohort sample sizes due to incomplete data.
PT, physical therapy; RTS, return to sport.
Denotes statistical significance at P < .05.
There were no statistically significant differences between the 2 cohorts in rates of injury to the ipsilateral index knee (P = .371) or contralateral knee (P = .176), or additional surgery on either the ipsilateral knee (P = .083) or contralateral knee (P = .327) (Table 3).
Multivariate linear regression analysis for factors predictive of preoperative IKDC score revealed that chronic injury was significantly associated with a greater preoperative score (P = .003) (Table 4). Regression analysis of the postoperative IKDC scores revealed that Medicaid insurance was strongly associated with a lower postoperative IKDC score (P = .044).
Table 4.
Multivariate Regression Analysis for Significant Associations With IKDC Scores and Return to Sport
| Odds Ratio | P Value | |
|---|---|---|
| Preoperative IKDC score | ||
| Age | 0.398 | .16 |
| BMI | 1.573 | .53 |
| Sex (ref = male) | 2.276e–5 | .30 |
| Insurance type (ref = private) | 0.572 | .96 |
| Days from trauma to surgery | 0.979 | .09 |
| Chronicity of injury (ref = acute) | 1.642e16 | .003∗ |
| Preoperative rehabilitation (ref = no) | 4.057e7 | .11 |
| Postoperative IKDC score | ||
| Age | 0.602 | .17 |
| BMI | 0.398 | .15 |
| Sex (ref = male) | 0.810 | .98 |
| Insurance type (ref = private) | 1.304e–8 | .044∗ |
| Days from trauma to surgery | 1.007 | .30 |
| Chronicity of injury (ref = acute) | 77.543 | .55 |
| Preoperative rehabilitation (ref = no) | 0.003 | .64 |
| Postoperative PT visits | 1.051 | .77 |
| Average duration of follow-up, mo | 0.942 | .73 |
| Return to sport | ||
| Age | 0.889 | .029∗ |
| BMI | 0.991 | .92 |
| Sex (ref = male) | 0.783 | .82 |
| Insurance type (ref = private) | 0.199 | .25 |
| Days from trauma to surgery | 1.000 | .74 |
| Chronicity of injury (ref = acute) | 0.840 | .87 |
| Preoperative rehabilitation (ref = no) | 3.446 | .31 |
| Postoperative PT visits | 0.978 | .38 |
| Average duration of follow-up, mo | 0.967 | .16 |
NOTE. Use of standard logistic regression: >1 odds ratio represents the increased likelihood of the outcome within the non-reference group, relative to the reference group. <1 odds ratio represents the decreased likelihood of the outcome within the nonreference group, relative to the reference group.
BMI, body mass index; IKDC, International Knee Documentation Committee; PT, physical therapy; ref, reference.
Denotes statistical significance at P < .05.
Multivariate logistic regression analysis was performed to determine the factors that were predictive of RTS following ACL reconstruction, revealing that greater age was associated with reduced likelihood to RTS (P = .029) (Table 4).
To further investigate the relationship between number of postoperative PT visits and likelihood to RTS, an ROC model was implemented (Fig 1). The model yielded an AUC value of 0.711, demonstrating acceptable predictivity. The threshold number of PT visits for RTS was determined to be 31.5 visits. Within our private insurance cohort, 17 of 23 patients (73.9%) exceeded this threshold. However, in our Medicaid cohort, 5 of 18 patients (27.8%) exceeded this threshold.
Fig 1.
Receiver operating characteristics analysis for determination of threshold physical therapy visits. (AUC, area under the curve.)
Discussion
The most important findings observed in the current study are as following: (1) patients insured with Medicaid demonstrated lower postoperative IKDC scores at final follow-up than patients with private insurance; (2) the Medicaid group attended fewer postoperative PT visits than the group with private insurance, despite no differences in distance traveled; (3) patients with Medicaid were less likely overall to RTS than those with private insurance; (4) no differences based on insurance status existed for reinjury or additional surgery rates in either ipsilateral or contralateral knee; and (5) a threshold of 31.5 PT visits was determined to predict high likelihood of RTS.
When reporting outcomes of orthopaedic procedures, the socioeconomic status (SES) of patients and type of insurance payer is often disregarded, despite its potential to influence surgical and functional outcomes. It is now widely accepted that disparities in SES and insurance type influence outcomes in a variety of different medical conditions and surgical procedures.22, 23, 24, 25 More specifically, recent investigations have demonstrated that in those undergoing total joint arthroplasty of the hip, knee, or shoulder, patients with Medicaid have greater resource use, greater complication rates, and poorer postoperative outcomes.8,10,13,14,23,26,27 With the expansion of Medicaid through the Affordable Care Act in 2014, the investigation of these disparities in one of the most common orthopaedic sports medicine procedures performed, ACL reconstruction, is critical.23
When assessing our primary outcome, despite similar preoperative IKDC scores (53.65 vs 53.95; P = .978) between the 2 cohorts, we found significantly lower postoperative IKDC scores (P = .005) at final follow-up in patients with Medicaid insurance compared with those with private insurance (74.68 vs 90.45, respectively; P = .005). Additional regression analysis supported our original hypothesis in which Medicaid insurance status was the only statistically significant factor associated with a lower postoperative IKDC score (1.304 × 10-8; P = .044). These results are noteworthy because they differed from previous literature on shoulder arthroplasty. Two different studies evaluating the effects of Medicaid insurance on American Elbow and Shoulder Surgeons (ASES) scores in patients undergoing shoulder arthroplasty found significantly inferior postoperative ASES scores in patients with Medicaid insurance; however, these investigations also reported inferior preoperative ASES scores in patients with Medicaid insurance as compared with controls.13,14 Contrarily, our study demonstrated inferior postoperative PRO scores in patients with Medicaid insurance undergoing ACL reconstruction despite similar baseline scores. As such, the fact that both cohorts exhibited similar baseline IKDC scores, concomitant meniscal procedures, and demographic data leads to more confidence that insurance status, in part, influences postoperative PRO outcomes.
The disparity observed in final PRO follow-up for patients with Medicaid insurance undergoing ACL reconstruction may be due to a variety of factors. We hypothesized that access to PT sessions may be influenced by socioeconomic factors faced by patients with Medicaid insurance. In our study, we found no statistically significant differences in the distance patients with Medicaid insurance lived from their PT facility; however, there was a significant fewer number of PT sessions attended by patients with Medicaid insurance compared with private insurance patients (24.67 vs 44.04; P = .012). This may be due to the greater difficulty patients with Medicaid insurance face when trying to access PT appointments.13 For instance, a cross-sectional study conducted in a large metropolitan area within a Medicaid-expansion state found that 43% fewer PT clinics accept Medicaid and those patients with Medicaid must wait significantly longer for an initial appointment as compared with private insurance patients.28 The PT benefits covered by Medicaid insurance in 2 different states (Illinois and Indiana) is provided in Table 5, suggesting there is no barrier to accessing PT for patients with Medicaid insurance with regards to limitations on number of PT visits or other restrictions. While the medical insurance coverage expansion in the last half decade provides holistically greater coverage to those that have historically had more difficulty accessing care, our finding highlights continued institutional issues that exist for patients navigating the health care system with Medicaid.
Table 5.
Explanation of Benefits and Limits for Medicaid Insurance Coverage in Illinois and Indiana
| Location | Physical Therapy Covered? | Copayment Required? | Limits on Services |
|---|---|---|---|
| Illinois | Yes | No | Previous authorization always required.∗ Coverage is limited to the following CPT codes: 97161-97164 and 97110. Limited to 4 units per day (1 unit = 15-minute increment). |
| Indiana | Yes | No† | Previous authorization required unless ordered by physician before hospital discharge. 12 hours/30 days or 30 therapy session/month in combination with other therapy providers.‡ |
CPT, Current Procedural Terminology; HIP, Healthy Indiana Plan.
Previous authorization is currently waived for outpatient therapy visits due to the coronavirus disease 2019 pandemic.
HIP Basic (coverage under Indiana’s Section 1115 waiver) has a $4 copay.
HIP Basic (coverage under Indiana's Section 1115 waiver) has a combined visit limit of 60 per year. HIP Plus has a combined visit limit of 75 per year.
Overall, patients with Medicaid insurance were also less likely to RTS than those patients with private insurance (50% vs 79%; P = .035). However, of those that were able to RTS, there was no observed differences in the rate of returning to the same level of sport or same position within a sport between the 2 cohorts. Previous literature on the impact of Medicaid on orthopaedic outcomes focus mainly on total joint arthroplasty procedures and, consequently, do not report RTS metrics. Contrarily, the findings from our study report on the association between Medicaid insurance and inferior RTS rates. This disparity in RTS is most likely influenced, in part, by the challenges in access to postoperative PT sessions for patients with Medicaid insurance. While number of postoperative PT visits was not a significant predictor of RTS (Table 4), our ROC analysis found that a threshold of 31.5 postoperative PT visits was predictive of RTS (Fig 1). Within our study cohorts, 17 of 23 patients with private insurance exceeded this threshold, whereas only 5 of 18 patients with Medicaid insurance coverage exceeded this number. This explanation would explain why there were no differences in returning to the same level of sport, because those patients with Medicaid insurance coverage who had access to PT are likely those who RTS and, thus, would have the same overall opportunity to return to the same level of sports as those with private insurance.
When reporting reinjury rates to either knee or further surgical intervention on either knee, there were no differences between patients with Medicaid insurance and patients with private insurance. These observations are not surprising because factors that lead to reoperation for ACL retears or meniscus injuries in young, active ACL-reconstructed patients are likely multifactorial. Despite 2 previous matched-cohort analyses showing patients with Medicaid insurance undergoing total hip, knee, or shoulder arthroplasty are at a greater risk of certain complications, these studies do not reflect the same complications or demographic of patients undergoing ACL reconstruction in the current study.23,27
We also performed regression analysis to determine which factors were predictive of preoperative IKDC score, postoperative IKDC score, and RTS rate. It was observed that the only significant factor predictive of preoperative increased IKDC score was a chronic ACL injury, defined as ≥90 days from injury to surgery. This finding is supported by the rationale that a patient with a higher IKDC score is more likely to delay surgery, whereas a lower IKDC would most likely result in more urgent surgical intervention. Second, regression analysis determined that having Medicaid insurance was predictive of a lower postoperative IKDC score, which is consistent with previous investigations on the association between PROs and Medicaid insurance. For instance, 2 separate studies found Medicaid insurance to be associated with inferior postoperative ASES scores relative to patients undergoing shoulder arthroplasty with Medicare or private insurance.13,14 Similarly, in patients undergoing primary total hip or knee arthroplasty, Halawi et al.12 found that Medicaid insurance type was associated with inferior Oxford Hip Score. Finally, our regression found that the only significant factor predictive of patients less likely to RTS was increased age at time of surgery. This is consistent with previous well-established literature on ACL reconstruction that younger patients are more likely to RTS.29, 30, 31 Nevertheless, the association between insurance payer type and outcomes following ACL reconstruction is likely multifactorial and should be acknowledged when educating patients, facilitating patient care, assisting patients in navigating the healthcare system, and evaluating outcomes after surgery.
Limitations
This study is not without limitations. First, by using chart review to collect demographic data, we were unable to determine information on education, employment, health literacy, or other important socioeconomic factors that may influence outcomes. Future studies on ACL reconstructions would benefit from a regression analysis that analyzed the association between these SES factors and postoperative outcomes. Second, the average follow-up duration for postoperative IKDC scores is significantly longer in the Medicaid cohort as compared to the private insurance cohort (45.23 vs 31.60 months, P = .016). However, this difference should not confound our findings that the Medicaid group had an inferior average IKDC score because previous literature has demonstrated that IKDC scores following ACL reconstruction are not time sensitive after six months postoperatively.32,33 Next, due to the initial low compliance with PROs, our study design inherently relied on contacting patients via phone call, which resulted in a limited number of patients to include in our analysis (26 patients with Medicaid insurance and 25 patients with private insurance). This also introduces the potential for response bias of those respondents who agreed to fill out the survey. Finally, the method in which we reported distance patient lived from PT facility may also introduce some inaccuracies as we used patients’ home address that was provided in their electronic medical record. However, these inaccuracies are likely limited as our clinic verifies the home address of each patient at every office visit.
Conclusions
Patients with Medicaid insurance undergoing ACL reconstruction had lower postoperative IKDC scores and were less likely overall to RTS than their private insurance counterparts at final follow-up in this study. Preoperative IKDC scores, incidence of preoperative meniscus injury, number of concomitant meniscus procedures, average distance from home to PT facility, return to same level of sport, and reinjury and reoperation rate were similar between groups. However, the number of postoperative PT sessions attended by patients with Medicaid insurance were significantly lower than patients with private insurance.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Sanders T.L., Maradit Kremers H., Bryan A.J., et al. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am J Sports Med. 2016;44:1502–1507. doi: 10.1177/0363546516629944. [DOI] [PubMed] [Google Scholar]
- 2.Buller L.T., Best M.J., Baraga M.G., Kaplan L.D. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967114563664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fridén T., Roberts D., Ageberg E., Waldén M., Zätterström R. Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture. J Orthop Sports Phys Ther. 2001;31:567–576. doi: 10.2519/jospt.2001.31.10.567. [DOI] [PubMed] [Google Scholar]
- 4.Zätterström R., Fridén T., Lindstrand A., Moritz U. The effect of physiotherapy on standing balance in chronic anterior cruciate ligament insufficiency. Am J Sports Med. 1994;22:531–536. doi: 10.1177/036354659402200416. [DOI] [PubMed] [Google Scholar]
- 5.Burland J.P., Toonstra J.L., Howard J.S. Psychosocial barriers after anterior cruciate ligament reconstruction: A clinical review of factors influencing postoperative success. Sports Health. 2019;11:528–534. doi: 10.1177/1941738119869333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shelbourne K.D., Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: How the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2008;37:471–480. doi: 10.1177/0363546508326709. [DOI] [PubMed] [Google Scholar]
- 7.Baumhauer J.F., Bozic K.J. Value-based healthcare: Patient-reported outcomes in clinical decision making. Clin Orthop Relat Res. 2016;474:1375–1378. doi: 10.1007/s11999-016-4813-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lakomkin N., Hutzler L., Bosco J.A., 3rd The relationship between medicaid coverage and outcomes following total knee arthroplasty: A systematic review. JBJS Rev. 2020;8 doi: 10.2106/JBJS.RVW.19.00085. [DOI] [PubMed] [Google Scholar]
- 9.Feng J.E., Roof M.A., Adnan M., et al. Do patient point of entry and medicaid status affect quality outcomes following total knee arthroplasty? J Arthroplasty. 2020;35:1761–1765. doi: 10.1016/j.arth.2020.02.023. [DOI] [PubMed] [Google Scholar]
- 10.Roof M.A., Feng J.E., Anoushiravani A.A., et al. The effect of patient point of entry and Medicaid status on quality outcomes following total hip arthroplasty. Bone Joint J. 2020;102-b:78–84. doi: 10.1302/0301-620X.102B7.BJJ-2019-1424.R2. [DOI] [PubMed] [Google Scholar]
- 11.Shau D., Shenvi N., Easley K., Smith M., Bradbury T., Guild G., 3rd Medicaid payer status is associated with increased 90-day morbidity and resource utilization following primary total hip arthroplasty: A propensity-score-matched analysis. J Bone Joint Surg Am. 2018;100:2041–2049. doi: 10.2106/JBJS.17.00834. [DOI] [PubMed] [Google Scholar]
- 12.Halawi M.J., Cote M.P., Savoy L., Williams V.J., Lieberman J.R. The effect of payer type on patient-reported outcomes in total joint arthroplasty is modulated by baseline patient characteristics. J Arthroplasty. 2019;34:1072–1075. doi: 10.1016/j.arth.2019.01.069. [DOI] [PubMed] [Google Scholar]
- 13.Lansdown D.A., Ma G.C., Aung M.S., et al. Do patient outcomes and follow-up completion rates after shoulder arthroplasty differ based on insurance payor? J Shoulder Elbow Surg. 2021;30:65–71. doi: 10.1016/j.jse.2020.04.028. [DOI] [PubMed] [Google Scholar]
- 14.Strotman P., Perry M., LeDuc R., Joyce C., Garbis N. Effect of insurance status on clinical outcomes after shoulder arthroplasty. Orthopedics. 2020;43:e523–e528. doi: 10.3928/01477447-20200827-02. [DOI] [PubMed] [Google Scholar]
- 15.Sabesan V.J., Petersen-Fitts G., Lombardo D., Briggs D., Whaley J. Medicaid payer status is linked to increased rates of complications after treatment of proximal humerus fractures. J Shoulder Elbow Surg. 2017;26:948–953. doi: 10.1016/j.jse.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Abdurrob A., Smith J.T. The effect of health insurance coverage on orthopaedic patient-reported outcome measures. J Am Acad Orthop Surg. 2020;28:e729–e734. doi: 10.5435/JAAOS-D-19-00487. [DOI] [PubMed] [Google Scholar]
- 17.Bakhsh W., Childs S., Oh I., Flemister S., Baumhauer J., Ketz J. Evaluating patients for elective outpatient foot and ankle surgery: Insurance as a predictor of patient outcomes. Foot Ankle Spec. 2019;12:522–529. doi: 10.1177/1938640018823070. [DOI] [PubMed] [Google Scholar]
- 18.Scott M.T., Boden A.L., Boden S.A., Boden L.M., Farley K.X., Gottschalk M.B. Medicaid payer status is a predictor of early postoperative pain following upper extremity procedures. Hand (N Y) 2022;17:162–169. doi: 10.1177/1558944720912565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ziedas A., Abed V., Swantek A., et al. Social determinants of health influence access to care and outcomes in patients undergoing anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2022;38:583–594.e584. doi: 10.1016/j.arthro.2021.06.031. [DOI] [PubMed] [Google Scholar]
- 20.Curry E.J., Penvose I.R., Knapp B., Parisien R.L., Li X. National disparities in access to physical therapy after rotator cuff repair between patients with Medicaid vs. private health insurance. JSES Int. 2021;5:507–511. doi: 10.1016/j.jseint.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chahla J., Kunze K.N., Tauro T., et al. Defining the minimal clinically important difference and patient acceptable symptom state for microfracture of the knee: A psychometric analysis at short-term follow-up. Am J Sports Med. 2020;48:876–883. doi: 10.1177/0363546520903279. [DOI] [PubMed] [Google Scholar]
- 22.Ackerman I.N., Graves S.E., Wicks I.P., Bennell K.L., Osborne R.H. Severely compromised quality of life in women and those of lower socioeconomic status waiting for joint replacement surgery. Arthritis Rheum. 2005;53:653–658. doi: 10.1002/art.21439. [DOI] [PubMed] [Google Scholar]
- 23.Browne J.A., Novicoff W.M., D'Apuzzo M.R. Medicaid payer status is associated with in-hospital morbidity and resource utilization following primary total joint arthroplasty. J Bone Joint Surg Am. 2014;96:e180. doi: 10.2106/JBJS.N.00133. [DOI] [PubMed] [Google Scholar]
- 24.Trupin L., Tonner M.C., Yazdany J., et al. The role of neighborhood and individual socioeconomic status in outcomes of systemic lupus erythematosus. J Rheumatol. 2008;35:1782–1788. [PMC free article] [PubMed] [Google Scholar]
- 25.Ward E., Jemal A., Cokkinides V., et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54:78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 26.Like B.J., White R.S., Tangel V., et al. Medicaid payer status is associated with increased mortality and morbidity after inpatient shoulder arthroplasty: A multistate analysis, 2007-2014. Reg Anesth Pain Med. 2019;44:182–190. doi: 10.1136/rapm-2018-000020. [DOI] [PubMed] [Google Scholar]
- 27.Li X., Veltre D.R., Cusano A., et al. Insurance status affects postoperative morbidity and complication rate after shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26 8:1423–1431. doi: 10.1016/j.jse.2016.12.071. [DOI] [PubMed] [Google Scholar]
- 28.Rogers M.J., Penvose I., Curry E.J., DeGiacomo A., Li X. Medicaid health insurance status limits patient accessibility to rehabilitation services following ACL reconstruction surgery. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118763353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Webster K.E., Feller J.A. Who passes return-to-sport tests, and which tests are most strongly associated with return to play after anterior cruciate ligament reconstruction? Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120969425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ardern C.L., Taylor N.F., Feller J.A., Webster K.E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543–1552. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 31.Mardani-Kivi M., Azari Z., Hasannejad F. Return to sport activity after anterior cruciate ligament reconstruction: A 6-10 years follow-up. J Clin Orthop Trauma. 2020;11:S319–s325. doi: 10.1016/j.jcot.2019.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agarwalla A., Puzzitiello R.N., Liu J.N., et al. Timeline for maximal subjective outcome improvement after anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47:2501–2509. doi: 10.1177/0363546518803365. [DOI] [PubMed] [Google Scholar]
- 33.Risberg M.A., Holm I., Steen H., Beynnon B.D. Sensitivity to changes over time for the IKDC form, the Lysholm score, and the Cincinnati knee score. A prospective study of 120 ACL reconstructed patients with a 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1999;7:152–159. doi: 10.1007/s001670050140. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.