Abstract
Background
Modern transportation plays a key role in the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and new variants. However, little is known about the exact transmission risk of the virus on airplanes.
Methods
Using the itinerary and epidemiological data of coronavirus disease 2019 (COVID-19) cases and close contacts on domestic airplanes departing from Wuhan city in China before the lockdown on 23 January 2020, we estimated the upper and lower bounds of overall transmission risk of COVID-19 among travelers.
Results
In total, 175 index cases were identified among 5797 passengers on 177 airplanes. The upper and lower attack rates (ARs) of a seat were 0.60% (34/5622, 95% confidence interval [CI] .43–.84%) and 0.33% (18/5400, 95% CI .21–.53%), respectively. In the upper- and lower-bound risk estimates, each index case infected 0.19 (SD 0.45) and 0.10 (SD 0.32) cases, respectively. The seats immediately adjacent to the index cases had an AR of 9.2% (95% CI 5.7–14.4%), with a relative risk 27.8 (95% CI 14.4–53.7) compared to other seats in the upper limit estimation. The middle seat had the highest AR (0.7%, 95% CI .4%–1.2%). The upper-bound AR increased from 0.7% (95% CI 0.5%–1.0%) to 1.2% (95% CI .4–3.3%) when the co-travel time increased from 2.0 hours to 3.3 hours.
Conclusions
The ARs among travelers varied by seat distance from the index case and joint travel time, but the variation was not significant between the types of aircraft. The overall risk of SARS-CoV-2 transmission during domestic travel on planes was relatively low. These findings can improve our understanding of COVID-19 spread during travel and inform response efforts in the pandemic.
Keywords: airplane, attack rate, COVID-19, SARS-CoV-2, transmission
Theattack rate of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission of a seat on airplane varies from 0.33% to 0.60%. The overall risk is relatively low, although it varies by seat distance from the index case and joint travel time.
Large-scale population movements through long-distance travel are one of the most important reasons for the rapid spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and new variants as well many other emerging infectious diseases across the planet [1–7]. Studies have shown that the number of imported coronavirus disease 2019 (COVID-19) cases by country in the early stage of the pandemic has a significant correlation with the volume of travelers from other epidemic areas [8–12]. Toward this, many domestic and international travel routes have been restricted or suspended to contain the further spread of SARS-CoV-2 [13, 14].
Airplanes have become some of the most important modes of transportation for long-distance travel within and across many countries. According to the World Bank statistics, the number of global air passengers reached 4.2 billion in 2018 [15]. Due to travel restrictions during the pandemic, the transport industry has been hit hard. Countries have been trying to resume socioeconomic activities and transportation after the rollout of COVID-19 vaccines. However, there is still a long way to achieve herd immunity, considering the shortage of vaccines and the inequalities in the dissemination as well as their efficacy that might be undermined by new variants [16, 17]. Moreover, the spread of new variants through travelers may lead to another resurgence and lockdown if the risk is not fully recognized and addressed [18].
Airlines preparing to resume timetables have been also struggling to implement social distancing guidelines, such as leaving the middle seats unoccupied on airplanes to reduce COVID-19 risk [19, 20]. These measures were in response to studies suggesting increased SARS-CoV-2 transmission among passengers in confined spaces [21–28]; for example, in the early days of the COVID-19 outbreak when protective measures (such as wearing masks) were rare among passengers, Speake et al (2020) found flight-associated SARS-CoV-2 transmission on a domestic flight route in Australia and reported that the secondary infectious rate was about 9.8% in the midportion of the cabin [21]; Khanh et al (2020) found the attack rate of SARS-CoV-2 was 62% in business class on a 10-hour commercial flight [24]. On the contrary, some research observed that the risk of SARS-CoV-2 transmission on flights was very low [29, 30]. For example, no onward transmission was found on an airplane from China to Canada on 22 January 2020, carrying Canada’s first reported COVID-19 patient traveling from Wuhan [31, 32]. There might be complicated reasons, including different flight hygiene guidelines. However, drawing robust conclusions from studies employing small samples is especially hard, as they are constrained by the availability of travel and epidemiological data by different transportation sources. Therefore, the overall risk of transmission of SARS-CoV-2 in confined public transport (eg, airplane) remains unclear.
Using individual itinerary and detailed epidemiological data among confirmed COVID-19 patients and their close contacts across mainland China in the early days of the outbreak in 2020, we quantified the overall transmission risk of SARS-CoV-2 during domestic travel on hundreds of airplanes across seat locations and by joint travel (co-travel) time. To account for confounding relationships between passengers (eg, family or friends) and their potential SARS-CoV-2 infections at home or working places before or after travel, we also estimated the upper and lower bounds of transmission risk during the journey. The findings from this research can provide an improved evidence-base for tailoring travel interventions to reduce the transmission risk of SARS-CoV-2 in cabins during the resumption of socioeconomic activities and public transportation in the vaccination and post-pandemic era. It may also provide necessary parameters for the control of other infectious diseases in the future.
METHODS
Data Sources
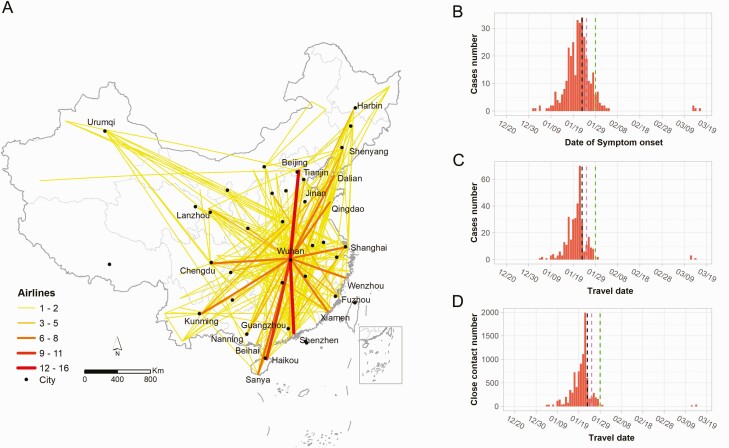
Since the COVID-19 outbreak has been first reported, the national and local Centers for Disease Control and Prevention (CDC) across China have conducted intensive epidemiological investigations to identify COVID-19 cases and close contacts as well as their travel history, according to the Diagnosis and Treatment Scheme for COVID-19 released by the National Health Commission of China [33]. A confirmed case was diagnosed with a positive result for SARS-CoV-2 nucleic acid by real-time reverse transcriptase polymerase chain reaction (RT-PCR) assay or high-throughput sequencing of nasal and pharyngeal swab specimens. Confirmed cases who reported to have a travel history of domestic flight during illness or within 14 days before symptom onset were recorded. Passenger lists who seated within three rows to the confirmed cases were then supplied by airlines. A total of 291 airplanes with confirmed COVID-19 cases on board flying between 81 cities were collected, from 4 January 2020 to 14 March 2020 (Figure 1). The date of travel, flight number, seat number, departure and arrival airports of cases and passengers as potential close contacts were collected to analyze the potential infectious risk of the disease. To measure the duration of travel, we searched flight timetables and flight types at the Variflight (www.variflight.com) and the Ctrip (www.ctrip.com). To understand the risk of SARS-CoV-2 transmission among travelers in transit before the wide implementation of nonpharmaceutical interventions in the early days of the outbreak, we focused on the individual-level transmission risk of COVID-19 among passengers on domestic flights, departing from Wuhan before the lockdown was implemented on 23 January 2020 (Figure 1). The flight dataset contained a total of 177 flights departing from Wuhan before the lockdown, of which Airbus and Boeing accounted for 37.9% (67) and 62.1% (110), respectively.
Figure 1.
Number of passengers infected with COVID-19 and close contacts on airlines across mainland China, December 2019 to March 2020. A, Routes and numbers of domestic airlines, excluding flights arriving in Wuhan. B, Number of cases by date of symptom onset. C, Number of cases by date of travel. D, Number of close contacts by date of travel. Black vertical dashed line: the date of Wuhan lockdown on 23 January 2020. Purple vertical dashed line: the Lunar New Year Day on 25 January 2020. Green vertical dashed line: the highest-level (Level 1) public health emergence response implemented across all provinces in mainland China, as of 29 January 2020. Abbreviation: COVID-19, coronavirus disease 2019.
Definitions of Index Case and Close Contact
On an airplane, a passenger was defined as an index case if he or she (i) was confirmed with COVID-19 after the travel; (ii) had symptom onset within 14 days before travel or within 2 days after travel; and (iii) had the earliest date of symptom onset among passengers within 3 rows in the case where there was more than 1 case. Passengers within 3 rows of the index case seat were considered to be close contacts for estimating the upper bound of risk detailed below. Given an average incubation period of 5 days (range 2–14 days), secondary COVID-19 cases were defined as cases among close contacts who had symptom onset later than that of the index case and within 2–14 days after travel [34].
The relationship and contacts between passengers were important factors in determining the transmission risk of COVID-19 on airplanes, because family members, colleagues, or friends frequently co-travel and might have a higher transmission risk at home or in the workplace, as opposed to travel [35]. However, individual social network information was not available for this study. Therefore, to account for group travel among family or friends, we used 2 assumptions for estimating the upper bound and lower bound of infection risks on transport, respectively. For estimating the upper-bound risk, we assumed that there was no family or friend relationship between travelers, nor any contacts before and after the journey, to estimate the potential high risks (upper bound) of SARS-CoV-2 transmission during air travel. For estimating the lower bound of risk, passengers were assumed to be traveling with their family members or friends if a small group of passengers included 1 index COVID-19 patient and passengers seated immediately adjacent to this index patient shared the same departure and destination. Therefore, passengers fitting this definition were excluded from close contacts of the index patient to estimate the potential low risks (lower bound) of SARS-CoV-2 spread on airplanes.
Assessing Transmission Risks
The attack rate (AR) of a seat was calculated as the number of confirmed cases divided by the total number of close contacts that used the same seat location apart from index cases. Relative risk (RR) and χ2 tests were used to compare the risks between different seats. Fisher exact test was used when the χ2 approximation might be incorrect because of small sample sizes. The 95% confidence interval (CI) of estimated AR was estimated using Wilson binomial method. Risk ratio was calculated using Wald unconditional maximum likelihood estimation, and its 95% CI was estimated using Wald normal approximation. The number of secondary cases infected per index case during travel was also used as an effective reproduction number of COVID-19 transmission among passengers on airplanes, respectively.
Assessing the Impact of Co-Travel Time on COVID-19 Transmission
The duration of domestic flights departing from Wuhan was mostly around 2–3 hours and generally within 4 hours. To measure the relationship between co-travel time with the COVID-19 transmission risk on board, we grouped the co-travel times of airline passengers with an index case into three categories: 0–1.5 hours, 1.5–2.5 hours, and >2.5 hours. The χ2 tests were used to compare the risk between different co-travel time groups.
Sensitivity analyses were performed to assess the impact of different definitions of index cases and secondary cases and the impact of the definition of co-traveled family members or friends group by changing the group size (Supplementary Sensitivity Analyses).
All statistical analyses in this study were conducted using R version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
COVID-19 Prevalence Among Air Passengers
A total of 5797 airline passengers on 177 planes were included in this study during the early stage of COVID-19 outbreak departing from Wuhan city, from 4 January 2020 through 23 January 2020 before the lockdown in the city of Wuhan. Eventually, 209 airline travelers were later confirmed as COVID-19 cases within the 1–14 days following their travel.
Attack Rate of COVID-19 Among Passengers
In total, 175 index cases traveling by airplane from Wuhan before its lockdown and the implementation of stringent interventions in China in 2020 were identified (Table 1). When estimating the upper bound of risk, 34 passengers among close contacts were considered to be infected on airplanes departing from Wuhan, respectively, with an AR of 0.60% (34/5622, 95% confidence interval [CI] .43–.84%). The median time lag from departure to symptom onset was 4.0 days (interquartile range 3.0–7.8). When estimating the lower bound of risk, the AR was 0.33% (18/5400, 95% CI .21–.53%), and each index case infected 0.10 (SD 0.32) passengers.
Table 1.
Coronavirus Disease 2019 (COVID-19) Transmission Risk Among Airplane Passengers Departing From Wuhan
| Characteristics | Upper Bound of Risk | Lower Bound of Risk |
|---|---|---|
| Date of travel | 4 January 2020 – 23 January 2020 | |
| No. of cases and close contacts | ||
| Total passengers | 5797 | |
| Close contacts | 5622 | 5400 |
| All cases | 209 | 209 |
| Index cases | 175 | 175 |
| Secondary cases | 34 | 18b |
| No. of airplanes | 177 (Airbus: 67; Boeing: 110) | |
| Reproduction number (SD)a | 0.19 (0.45) | 0.10 (0.32) |
| Attack rate by seat location, 95% CI | ||
| Overall | 0.60% (34/5622), .43–.84% | 0.33% (18/5400), .21–.53% |
| Aisle seats | 0.56% (11/1974), .31–1.00% | 0.53% (10/1884), .29–.97% |
| Middle seats | 0.71% (12/1692), .41–1.24% | .13% (2/1595), .03–.46% |
| Window seats | 0.56% (11/1956), .31%–1.00% | 0.31% (6/1921), .14–.68% |
| Seats adjacent to index cases | 9.20% (16/174), .57–14.4% | 1.32% (2/151), .37–4.70% |
| Seats not adjacent to index cases | 0.33% (18/5448), .21–.52% | 0.30% (16/5249), .19–.49% |
Abbreviations: CI, confidence interval; SD: standard deviation.
The overall effective reproduction number during travel was estimated as the number of secondary cases divided by the number of index cases in each setting.
By the definition of lower bound of risk, passengers seated immediately adjacent to an index patient were excluded from close contacts of the index patient to estimate the potential low risks.
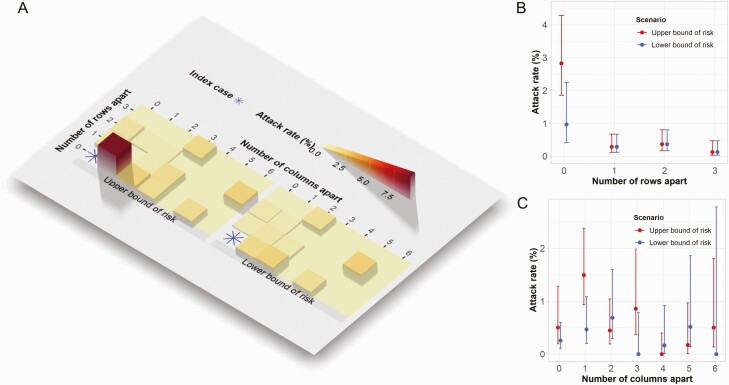
COVID-19 Transmission Risk by Seat Location in Cabin
The AR varied greatly by seat within 3 rows and 6 columns to the index patient seat (Figure 2). In the upper-bound risk estimation, the seats immediately adjacent to the index cases had the highest risk, with an AR of 9.2% (95% CI 5.7–14.4%). Compared to other seats, the relative risk (RR) of these seats was 27.8 (95%CI 14.4–53.7). Generally, passengers seated on the same row as the index case had a higher risk than passengers at other rows, with a RR of 10.6 (95% CI 5.3–21.1). However, ARs for the seats at 1–3 rows apart from the index patient showed no significant difference between each other (P > .05).
Figure 2.
Attack rates of COVID-19 at different seats apart from index cases on airplanes for passengers departing from Wuhan, as of 23 January 2020. A, Attack rate per different seats. The seats of index cases were indicated at (row 0, column 0). B, Attack rate of seats by row apart from the index case. C, Attack rate of seats by column apart from the index case. Abbreviation: COVID-19, coronavirus disease 2019.
In terms of seat location on airplanes, that is, window, middle, and aisle seats, the middle seat had the highest AR (0.7%, 95% CI .4–1.2%), followed by the window seat (0.6%, 95% CI .3–1.0%) and the aisle seat (0.6%, 95% CI .3–1.0%) for the upper bound estimation, likely due to the fact that middle seats are exposed to individuals on either side, whereas window and aisle seats are exposed to only 1 individual. No significant difference in AR was found on seats between Airbus and Boeing airplanes (P = 1.0).
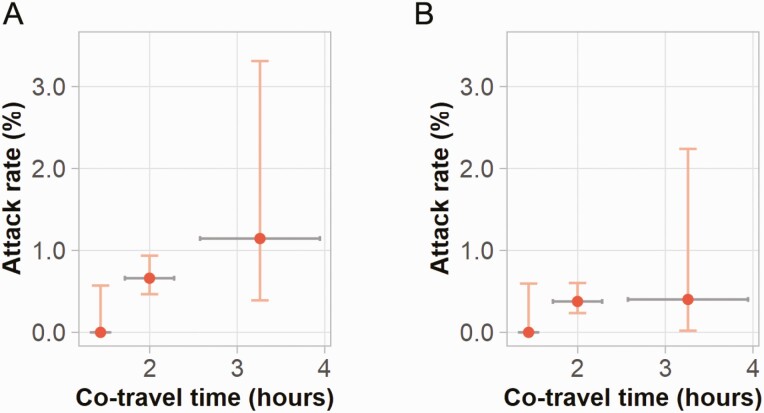
Effect of Co-Travel Duration on the Transmission Risk
Travel time among domestic airplane passengers departing from Wuhan ranged from 1.1 to 4.3 hours (mean 2.0, SD 0.5), with approximately 98% traveling <3 hours. On average, the upper bound of AR increased from 0.7% (95% CI .5–1.0%) to 1.2% (95% CI .4–3.3%) when the co-travel time increased from 2.0 hours to 3.3 hours (Figure 3), whereas the lower bound estimates of AR increased from a relatively low risk (0.0%, 95% CI .0–.6%) within 1.5 hours, to 0.4% (95% CI .02–2.2%) for a joint travel duration of 3.3 hours. However, due to the small number of secondary cases in different groups of co-travel time intervals, there was no significant difference between the estimated upper and lower bounds of ARs (P = .06).
Figure 3.
Relationships between COVID-19 attack rate and co-travel time on airplane departing from Wuhan, as of 23 January 2020. A, Upper bounds of attack rates on airplanes. B, Lower bounds of attack rates on airplanes. Vertical bars show 95% confidence interval of attack rate estimates; horizontal bars represent the standard deviation of co-travel time. Abbreviation: COVID-19, coronavirus disease 2019.
DISCUSSION
Although many studies have explored the impact of human mobility and relevant interventions on the spread of infectious diseases [1, 2, 36], our study comprehensively quantified the overall risk of SARS-CoV-2 transmission among individual air passengers. These findings inform transmission probability estimates of COVID-19 in confined environments, which could help to formulate targeted strategies to protect travelers and control the transmission of the disease. Based on anonymized individual case and passenger data on airplanes, our research showed that general transmission risk of SARS-CoV-2 among domestic passengers in the early days of outbreaks was relatively low on aircrafts, for both Boeing and Airbus airplanes. We further quantified the relationship between transmission risk and other travel factors, such as seat distance from an infectious individual and co-travel time.
We found that transmission of SARS-CoV-2 in cabins might have occurred, but the overall risk to a given individual was relatively low for domestic air travel in China, even under upper bound risk assumptions. Several factors might explain this: first, individuals are less likely to travel after illness onset, in particular severe infections. Second, the degree of infectivity among travelers may vary temporally. For example, some travelers infected with SARS-CoV-2 might be presymptomatic and still in the latent period of infection, defined as the period between exposure to the virus and the onset of infectiousness. Third, modern commercial airplanes are commonly equipped with high efficiency particulate air filters, which can effectively filter out 99.9% of dust, bacteria, and viruses with a particle size of >0.3 μm [37], thereby reducing transmission risk of respiratory infectious diseases [38–43]. When the air enters the passenger cabin, it undergoes high temperature disinfection and cooling. Aircraft cabin air conditioners can complete up to 20 air changes per hour, reducing the presence of virus-containing droplets and the risk of disease transmission in the cabin. Toward this, we found that the difference in risk was not significant by aircraft type within our analyses.
Our findings suggested the risk varied with joint travel time and seat distance to the index case, with the risk increasing by longer travel time. The effect of co-travel duration on COVID-19 transmission risk was also found in high-speed trains across the country [43]. Therefore, the transmission risk on international flights may also increase due to longer travel distance and time for the international journey. Additionally, there are several factors which might explain the higher risk we observed among travelers seated in the same row as index patients. First, droplets and aerosols produced by the index patient’s talking, coughing, and sneezing might be more likely to spread within the immediate vicinity, such as the same row [44, 45]. Furthermore, the seat backs between the front and rear rows might partially block the spread of the virus in the forward and backward positions. Second, each row of seats has an independent air-conditioning exhaust system that blows air from top to bottom and is filtered away from the bottom of the seat. This design could reduce the speed of air diffusion to the surroundings and thereby dilute the virus concentration [46]. Third, passengers in the same row might have more opportunities for social contact, especially if they are travelling with family members or friends. Finally, nonpharmaceutical interventions that were in place across China since late January 2020 have effectively contained the spread and further transmission of COVID-19 across the country [47, 48], subsequently reducing the infection risk among travelers. Further containment measures such as temperature screening at stations or airports, face mask usage, and travel restrictions for high risk areas might work synergistically to minimize transmission risk in transit [36]. The vaccine’s protective role has the potential to reduce the risk of transmission even further. To assess the impact of vaccination rates and protective measures on the risk of transmission on aircraft, more real-world data and complex scenario simulation designs are needed.
Our study was subject to a variety of limitations. First, due to the limitation of data availability, we only studied the risk of transmission within 3 rows (7 rows in total) in front of and behind the index case, and therefore did not consider possible transmission within a larger scope (including flight crews). However, previous studies showed that the seats within 3 rows to the index patients had the highest risk [49]. Second, as with other similar studies, we cannot accurately determine when and where the infection occurred due to recall bias from passenger reported information [46]. The information of whether passengers travelled together was also missed in the data. Cases may have been infected in other places before or after travel, such as in terminals, or during the boarding process. This might overestimate the risk of spreading COVID-19 on planes, although we accounted for this by employing 2 scenarios to estimate the interval of risk. Third, data on usage of personal protective equipment such as masks and goggles during the flight were not available to account for the impact of these interventions, although few passengers might use these measures before 23 January 2020 when the lockdown of Wuhan was in place. The provision of in-flight meals was also not considered due to the data availability. Fourth, due to the retrospective feature of this study, we did not quantify the risk of transmission by other modes of exposure on transportation, such as contact with contaminated surfaces in the restroom, or personnel changing seats. Fifth, due to the limited capacity of testing at the early stage of this outbreak, the links between index cases and secondary cases were not further examined by genome sequencing and phylogenetic analysis. Additionally, asymptomatic travelers might not be captured in this study, and transmission risk before the symptom onset might be overlooked [28, 50]. Finally, the difference in the size and cabin layout of aircrafts was not considered in the study, where first class cabins tend to have more space between passengers than economy cabins. Despite these, our findings contribute to improve our understanding of infectious disease transmission risk during traveling and to inform COVID-19 response efforts, lift travel restrictions and reopen economy in the vaccination and post-pandemic era.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. We thank staff members at disease control institutions, hospitals, and health administrations across China for field investigation, administration, and data collection. We also thank Prof Marc Lipsitch at the Harvard T.H. Chan School of Public Health for his insightful comments to improve this article. The data and code for plotting figures in this study have been made openly available for further use at https://github.com/maoguihu/TransmisionRiskOnAirplane-Train. The individual itinerary data of cases and passengers included in the current study are not publicly available because this would compromise the agreement with the data provider, but the information on the process of requesting access to the data that support the findings of this study are available from the corresponding author (wangjf@lreis.ac.cn).
Financial sources. This study was supported by the National Science and Technology Major Project of China (grant numbers 2017ZX10201302 and 2016ZX10004222-009), the National Natural Science Foundation of China (grant numbers 41771434, 41531179, and 81773498), and the Bill & Melinda Gates Foundation (grant number INV-024911). A. J. T. is supported by funding from the Bill & Melinda Gates Foundation (grant numbers INV-002697, OPP1106427, OPP1032350, OPP1134076, and OPP1094793), the Clinton Health Access Initiative, the UK Department for International Development (DFID) and the Wellcome Trust (grant numbers 106866/Z/15/Z and 204613/Z/16/Z), and the EU H2020 (grant number MOOD 874850). N. R. is supported by funding from the Bill & Melinda Gates Foundation (grant number OPP1170969) and the Vodafone Institute; W. Y. is supported by funding from the Chinese Academy of Medical Sciences-Innovation Fund for Medical Sciences (grant number 2020-I2M-1-001).
Author contributions. M. H. designed the study, built the model, collected data, finalized the analysis, interpreted the findings, and wrote the manuscript. S. L. conceived the study, built the model, interpreted the findings, wrote and revised the manuscript. J. W. conceived and designed the study, interpreted the findings, and commented on and revised drafts of the manuscript. H. L., C. X., B. M., X. Z., Y. F., and Q. Y. collected data, interpreted the findings, and revised drafts of the manuscript. C. W. R., A. C., J. R. F., N. W. R., Z. L., W. Y., and A. J. T. interpreted the findings, and commented on and revised drafts of the manuscript. All authors read and approved the final manuscript.
Ethical approval. The collection and analysis of case and close contact data performed by the National Health Commission of China to investigate and control the COVID-19 outbreak was exempt from an ethical approval. All data were supplied and analyzed in an anonymous format, without access to personal identifying information.
Role of the funding source. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. The views expressed in this article are those of the authors and do not represent any official policy.
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Contributor Information
Maogui Hu, Institute of Geographic Sciences and Natural Resources Research, Chinese Academy of Sciences, Beijing, China.
Jinfeng Wang, Institute of Geographic Sciences and Natural Resources Research, Chinese Academy of Sciences, Beijing, China.
Hui Lin, China Academy of Electronics and Information Technology, Beijing, China.
Corrine W Ruktanonchai, WorldPop, School of Geography and Environmental Science, University of Southampton, Southampton, UK; Population Health Sciences, Virginia Tech, Blacksburg, Virginia, USA.
Chengdong Xu, Institute of Geographic Sciences and Natural Resources Research, Chinese Academy of Sciences, Beijing, China.
Bin Meng, Beijing Union University, Beijing, China.
Xin Zhang, Aerospace Information Research Institute, Chinese Academy of Sciences, Beijing, China.
Alessandra Carioli, WorldPop, School of Geography and Environmental Science, University of Southampton, Southampton, UK.
Yuqing Feng, Institute of Geographic Sciences and Natural Resources Research, Chinese Academy of Sciences, Beijing, China.
Qian Yin, Institute of Geographic Sciences and Natural Resources Research, Chinese Academy of Sciences, Beijing, China.
Jessica R Floyd, WorldPop, School of Geography and Environmental Science, University of Southampton, Southampton, UK.
Nick W Ruktanonchai, WorldPop, School of Geography and Environmental Science, University of Southampton, Southampton, UK; Population Health Sciences, Virginia Tech, Blacksburg, Virginia, USA.
Zhongjie Li, Divisions of Infectious Diseases, Chinese Center for Disease Control and Prevention, Beijing, China.
Weizhong Yang, School of Population Medicine and Public Health, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China.
Andrew J Tatem, WorldPop, School of Geography and Environmental Science, University of Southampton, Southampton, UK.
Shengjie Lai, WorldPop, School of Geography and Environmental Science, University of Southampton, Southampton, UK.
References
- 1. Jia JS, Lu X, Yuan Y, Xu G, Jia J, Christakis NA.. Population flow drives spatiotemporal distribution of COVID-19 in China. Nature 2020; 582:389–94. [DOI] [PubMed] [Google Scholar]
- 2. Wu JT, Leung K, Leung GM.. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet 2020; 395:689–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lai S, Floyd J, Tatem A.. Preliminary risk analysis of the spread of new COVID-19 variants from the UK, South Africa and Brazil. Available at: https://www.worldpop.org/events/covid_variants. Accessed 18 January 2021.
- 4. O’Toole Á, Hill V, Pybus OG, et al. . Tracking the international spread of SARS-CoV-2 lineages B.1.1.7 and B.1.351/501Y-V2. Available at: https://virological.org/t/tracking-the-international-spread-of-sars-cov-2-lineages-b-1-1-7-and-b-1-351-501y-v2/592. Accessed 24 January 2021. [DOI] [PMC free article] [PubMed]
- 5. Chang SL, Harding N, Zachreson C, Cliff OM, Prokopenko M.. Modelling transmission and control of the COVID-19 pandemic in Australia. Nat Commun 2020; 11:5710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gibbs H, Liu Y, Pearson CAB, et al. ; LSHTM CMMID COVID-19 working group. . Changing travel patterns in China during the early stages of the COVID-19 pandemic. Nat Commun 2020; 11:5012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wesolowski A, Zu Erbach-Schoenberg E, Tatem AJ, et al. . Multinational patterns of seasonal asymmetry in human movement influence infectious disease dynamics. Nat Commun 2017; 8:2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhao S, Zhuang Z, Ran J, et al. . The association between domestic train transportation and novel coronavirus (2019-nCoV) outbreak in China from 2019 to 2020: a data-driven correlational report. Travel Med Infect Dis 2020; 33:101568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhang XA, Fan H, Qi R-Z, et al. . Importing coronavirus disease 2019 (COVID-19) into China after international air travel. Travel Med Infect Dis 2020; 35:101620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Silverstein WK, Stroud L, Cleghorn GE, et al. . First imported case of 2019 novel coronavirus in Canada, presenting as mild pneumonia. Lancet 2020; 395:734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Eldin C, Lagier JC, Mailhe M, Gautret P.. Probable aircraft transmission of Covid-19 in-flight from the Central African Republic to France. Travel Med Infect Dis 2020; 35:101643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bogoch II, Watts A, Thomas-Bachli A, et al. . Pneumonia of unknown aetiology in Wuhan, China: potential for international spread via commercial air travel. J Travel Med 2020; 27:taaa008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chinazzi M, Davis JT, Ajelli M, et al. . The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 2020; 368: 395–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wells CR, Sah P, Moghadas SM, et al. . Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak. Proc Natl Acad Sci 2020; 117:7504–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. The World Bank. Available at: Air transport, passengers carried. Available at: https://data.worldbank.org/indicator/IS.AIR.PSGR. Accessed 27 June 2020.
- 16. Aschwanden C. Five reasons why COVID herd immunity is probably impossible. Nature 2021; 591:520–2. [DOI] [PubMed] [Google Scholar]
- 17. Yewdell JW. Individuals cannot rely on COVID-19 herd immunity: durable immunity to viral disease is limited to viruses with obligate viremic spread. PLoS Pathog 2021; 17:e1009509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lai S, Floyd J, Tatem A.. Preliminary risk analysis of the international spread of new COVID-19 variants, lineage B.1.1.7, B.1.351 and P.1. Available at: https://www.worldpop.org/events/covid_variants. Accessed 27 April 2021.
- 19. AirlineGeeks. Post-COVID-19 aviation industry: the middle seat. Available at: https://airlinegeeks.com/2020/05/30/41795/. Accessed 30 May 2020.
- 20. IATA. IATA calls for passenger face covering and crew masks-opposes onboard social distancing. Available at: https://www.iata.org/en/pressroom/pr/2020-05-05-01. Accessed 20 June 2020.
- 21. Speake H, Phillips A, Chong T, et al. . Flight-associated transmission of severe acute respiratory syndrome Coronavirus 2 corroborated by whole-genome sequencing. Emerg Infect Dis 2020; 26:2872–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pavli A, Smeti P, Hadjianastasiou S, et al. . In-flight transmission of COVID-19 on flights to Greece: an epidemiological analysis. Travel Med Infect Dis 2020; 38:101882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Freedman DO, Wilder-Smith A.. In-flight transmission of SARS-CoV-2: a review of the attack rates and available data on the efficacy of face masks. J Travel Med 2020; 27:taaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Khanh NC, Thai PQ, Quach HL, et al. . Transmission of SARS-CoV 2 during Long-Haul flight. Emerg Infect Dis 2020; 26:2617–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yang N, Shen Y, Shi C, et al. . In-flight transmission cluster of COVID-19: a retrospective case series. Infect Dis (Lond) 2020; 52:891–901. [DOI] [PubMed] [Google Scholar]
- 26. Chen J, He H, Cheng W, et al. . Potential transmission of SARS-CoV-2 on a flight from Singapore to Hangzhou, China: an epidemiological investigation. Travel Med Infect Dis 2020; 36:101816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hoehl S, Karaca O, Kohmer N, et al. . Assessment of SARS-CoV-2 transmission on an international flight and among a tourist group. JAMA Netw Open 2020; 3:e2018044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shen Y, Li C, Dong H, et al. . Community outbreak investigation of SARS-CoV-2 transmission among bus riders in Eastern China. JAMA Intern Med 2020; 180:1665–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Johnson HS. IATA: Risk of COVID-19 transmission inflight is low. in Travel Daily. Available at: https://www.traveldailymedia.com/iata-risk-of-covid-19-transmission-inflight-is-low. Accessed 7 October 2020.
- 30. Nebehay S. Risk of inflight spread of COVID-19 “very low”, not zero-WHO. in Reuters. Available at: https://www.reuters.com/article/health-coronavirus-airlines-who/risk-of-inflight-spread-of-covid-19-very-low-not-zero-who-idUSL8N2HD5BS. Accessed 27 October 2020.
- 31. Schwartz KL, Murti M, Finkelstein M, et al. . Lack of COVID-19 transmission on an international flight. CMAJ 2020; 192:E410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Glauser W. Communication, transparency key as Canada faces new coronavirus threat. CMAJ 2020; 192:E171–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. National Health Commission of China. Interim diagnosis and treatment of 2019 novel coronavirus pneumonia. 3rd ed. Available at: http://www.gov.cn/zhengce/zhengceku/2020-01/23/content_5471832.htm. Accessed 4 March 2020. [Google Scholar]
- 34. Lauer SA, Grantz KH, Bi Q, et al. . The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Internal Med 2020; 172: 577–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhang L, Peng Z, Ou J, et al. . Protection by face masks against influenza A(H1N1)pdm09 virus on trans-Pacific passenger aircraft, 2009. Emerg Infect Dis 2013; 19:1403–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kraemer MUG, Yang CH, Gutierrez B, et al. ; Open COVID-19 Data Working Group. . The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 2020; 368:493–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Leder K, Newman D.. Respiratory infections during air travel. Intern Med J 2005; 35:50–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Li Q, Guan X, Wu P, et al. . Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020; 382: 1199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Vogt TM, Guerra MA, Flagg EW, Ksiazek TG, Lowther SA, Arguin PM.. Risk of severe acute respiratory syndrome-associated coronavirus transmission aboard commercial aircraft. J Travel Med 2006; 13:268–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Guan WJ, Ni Z, Hu Y, et al. . Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med 2020; 382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. . Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 2020; 395:1973–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ.. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc Natl Acad Sci U S A 2020; 117:14857–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hu M, Hui L, Wang J, et al. . Risk of coronavirus disease 2019 transmission in train passengers: an epidemiological and modeling study. Clin Infect Dis 2021; 72:604–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Stadnytskyi V, Bax CE, Bax A, Anfinrud P.. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc Natl Acad Sci U S A 2020; 117:11875–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions: potential implications for reducing transmission of COVID-19. JAMA 2020; 323:1837–8. [DOI] [PubMed] [Google Scholar]
- 46. Mangili A, Gendreau MA.. Transmission of infectious diseases during commercial air travel. Lancet 2005; 365:989–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tian H, Liu Y, Li Y, et al. . An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science 2020; 368:638–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lai S, Ruktanonchai NW, Zhou L, et al. . Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 2020; 585:410–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Li Z, Chen Q, Feng L, et al. ; China CDC COVID-19 Emergency Response Strategy Team. . Active case finding with case management: the key to tackling the COVID-19 pandemic. Lancet 2020; 396:63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bae SH, Shin H, Koo HY, Lee SW, Yang JM, Yon DK.. Asymptomatic transmission of SARS-CoV-2 on evacuation flight. Emerg Infect Dis 2020; 26:2705–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.