Abstract
Introduction and importance
Degenerative lumbar scoliosis is a prominent cause of adult spinal deformity with an increasing prevalence as the population ages. This pathology is associated with debilitating symptoms, including radicular back pain and lower extremity claudication. Surgical realignment of the spine and restoration of sagittal imbalance can reduce low back pain. Chronic sacroiliac dysfunction commonly causes low back radicular pain. We present a complicated case where stereotactic navigation facilitated an extensive fusion and decompression procedure for adult spinal deformity in an obese patient with multiple prior surgeries for scoliosis and sacroiliac joint pathology.
Case presentation
A 69-year-old, obese female with scoliosis refractory to multiple interventions presented with severe, radicular lower back pain. On examination of the right lower extremity (RLE), she had mild weakness (3/5 strength) and reduced sensation to light touch over its anterolateral aspect (dermatome L4). She was unable to perform single leg stance or tandem walk. Imaging revealed moderate mid-lumbar levoscoliosis, severe degenerative disc disease and facet hypertrophy changes in the setting of prior multilevel lumbar fusion, and consecutive nerve root impingement between L1 and L5 (worst at L3–4). DEXA scan was consistent with osteoporosis. The patient underwent lumbar laminectomy with posterior fusion of T10-ilium, transforaminal lumbar interbody fusion, osteotomy, and decompression using stereotactic navigation. The presence of SI titanium dowels from her previous SI fusion procedure posed a challenge with respect to achieving pelvic fixation.
Clinical discussion
Iliac screw placement is a critical adjunctive to lumbosacral fusion, notably for prevention of pseudoarthrosis; however, patients with prior SI fusion may present a biomechanical challenge to surgeons due to obstruction of the surgical site. The O-arm neuronavigation system was successfully used to bypass this obstruction and provide sacroiliac fixation in this procedure.
Conclusion
Stereotactic navigation (The O-arm Surgical Imaging System) can effectively be used to circumvent prior SI fusion in osteoporotic bone.
Keywords: Pelvic screw, Sacroiliac fusion, Osteoporosis, Spinal deformity, Stereotactic navigation, Case report
Highlights
-
•
Stereotactic navigation circumvents prior SI fusion in osteoporotic bone.
-
•
Case complexity indicates use of O-arm to obtain pelvic fixation.
-
•
Stereotactic navigation associated with benefits in posterior spinal surgery.
1. Introduction
Although its etiology is not entirely clear, degenerative scoliosis of the lumbar spine is a prominent cause of adult spinal deformity that often results from degenerative disc disease or osteoporosis [1]. Currently, the prevalence of degenerative scoliosis within the aged population is increasing, and degenerative de novo scoliosis often presents with spinal stenosis and its associated symptoms [2]. The associated degenerative pathology includes disc bulging, facet arthritis, and ligamentum flavum hypertrophy [2]. With respect to symptomatology, degenerative lumbar scoliosis most commonly presents with low back pain, leg pain, and spinal instability [3], [4]. More specifically, spinal stenosis and rotary vertebral subluxation induce claudication and/or radicular pain, while low back pain can be caused by disk degeneration, facet joint arthrosis, and/or decreased lumbar lordosis [5], [6]. Spinal realignment can reduce rotary subluxation and result in leg pain relief, while restoration of sagittal imbalance can contribute to low back pain relief [3], [5], [6]. As such, surgical approaches to treatment of degenerative lumbar scoliosis include a combination of spinal fusion with instrumentation, neural decompression, and correction of deformities [3]. Because of the multifaceted pathology of degenerative lumbar scoliosis, as well as its prevalence in elderly patients who often present with co-morbidities, these surgical approaches are associated with a high complication rate [3], [7].
In addition to degenerative lumbar scoliosis, chronic sacroiliac (SI) joint dysfunction is another common cause of chronic low back/buttock radicular pain [8]. In fact, its estimated prevalence is 15–30 % despite the fact that it is often overlooked as a cause of axial back pain that predominates in female patients [8]. SI joint dysfunction has a significant impact on quality of life and can be treated with both conservative management strategies and surgical approaches, with sacroiliac joint fusion (SIJF) emerging as a safe and effective option that may provide pain relief [9], [10].
Although surgical treatments for pain associated with degenerative lumbar scoliosis and SI joint dysfunction have become fairly common, especially in the elderly population, we present a case that is particularly unique in complexity. The patient initially presented to us in a state of morbid obesity, making the decision to go forth with surgery tenuous. The patient was also osteoporotic and above all, had already undergone two lumbar laminectomies and one SI fusion, meaning there was already extensive hardware present in her spinal column. Because of the degree of complexity required for this procedure, an O-arm Surgical Imaging System, which allows for CT-quality multiplanar reconstructions and intraoperative guidance, was used to achieve pelvic fixation around the previous SI fusion [11]. This case report has been reported in line with the SCARE criteria [12].
2. Case description
A 69-year-old, obese female with scoliosis refractory to multiple surgeries and/or procedures including two lumbar laminectomies for neurogenic claudication, sacroiliac (SI) fusion, and a failed stimulation trial, presented with lower back and lower extremity pain. The patient described pain (6–8/10) as radiating and shooting/stabbing in character that was worse in the right lower extremity, extending from her buttock to her thigh and extending down into the lateral portion of her leg and wrapping around her anterior shin and ankle. The pain was not triggered by any precipitating event. She also described numbness and tingling in the same distribution as well as weakness of the right lower extremity. Additionally, her pain failed to remit following each of the aforementioned surgeries, and is only reduced by lying down, heat, and medications (Hydrocodone Bitartrate/Acetaminophen 10–350 mg every 4–6 h, Gabapentin 800 mg x3/day, and Robaxin 750 mg daily). Multiple epidural steroid injections and physical therapy following her prior surgery failed to provide pain relief. Following her most recent lumbar laminectomy (one year prior), her lower back pain worsened, and she experienced urinary retention (requiring intermediate length of time of self-catheterization) that eventually resolved. The patient also noted a change in posture over the course of her symptoms and reported that she has difficulty walking (RLE strength 3/5), requiring a 4-point walker. Prior to her operations she had been ambulatory without an assistive device. Upon presentation, her Oswestry Disability Index was 60 and her past medical history was unremarkable.
2.1. Examination
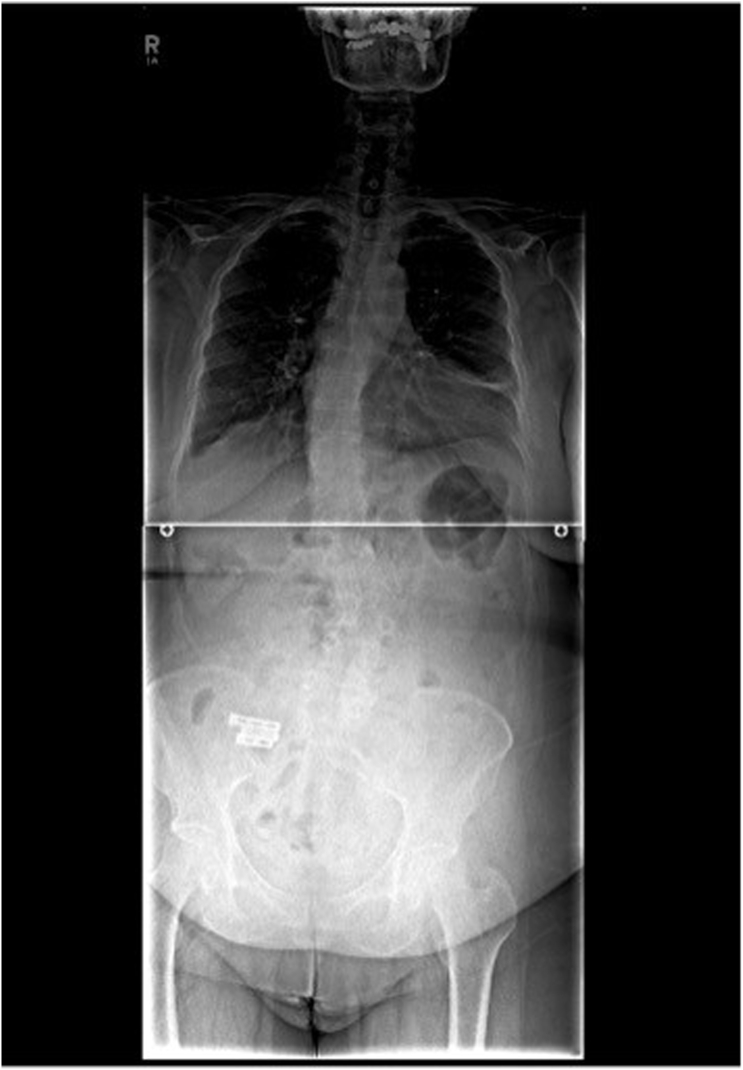
On examination, decreased sensation to light touch in the anterolateral aspect of the right lower extremity was noted. Patient was alert and oriented x3 with trace DTRs and exhibited some weakness of the right lower extremity, with no loss of upper extremity function and intact proprioception. She was unable to perform single leg stance (bilaterally) and tandem walk. Thoracolumbar spine X-ray and lumbar spine computed tomography (CT) revealed severe degenerative changes most notable for thoracolumbar degenerative scoliosis (right-sided deviation), spinal stenosis, and multilevel lumbar autofusion. Compared to lumbar MRI from a year prior, a probable interval right L3 laminectomy and partial right L3-4 facetectomy with increase in 5.3 cm anteroposteriorly (AP) irregular peripherally enhancing fluid collection along the operative bed and right paramedian posterior paraspinal soft tissues was noted (representing a postoperative collection). Additionally, MRI revealed significant circumferential epidural enhancement at the L3 level, and significant ill-defined soft tissue thickening and enhancements along the right L3-4 neuroforamen. Additional persistent significant dorsal epidural enhancement was present at L4 (likely epidural scar tissue). Ultimately, MRI was significant for mild-moderate mid-lumbar levoscoliosis and moderate-severe multilevel lumbar disc degeneration and facet hypertrophy with moderate L3-4 and mild L4-5 spinal stenosis. The result was nerve root impingement between L1-2 and L4-5 but worst at L3-4 (Fig. 1).
Fig. 1.
Pre-operative AP X-ray showing right-sided thoracolumbar scoliosis along with three titanium dowels.
Scoliosis X-rays supported the pathology evident on MRI (Fig. 1). Multiple vacuum discs and significant degeneration were noted on CT. Of note, DEXA scan showed a T-score value of <−2.5 which was suggestive of osteoporosis of the right hip, although her left hip and spine both demonstrated adequate bone health. Because of the concern regarding possible osteoporosis, an endocrinology consult was ordered; regardless, surgery was necessitated by her declining functional status.
2.2. Clinical course
The patient, whose BMI exceeded 35 on initial presentation, adhered to counseling and instructions to lose weight and reduce narcotic intake prior to surgery. She ultimately lost 25 pounds, reducing her BMI below 35 in a one-month span, after which it was determined she had achieved ample optimization for lumbar laminectomy with T10 to L4-L5 posterior spine instrumented fusion, transforaminal lumbar interbody fusion (TLIF), osteotomy, and decompression. Regardless, the presence of SI titanium dowels from her previous SI fusion procedure posed a challenge with respect to achieving pelvic fixation.
2.3. Operation
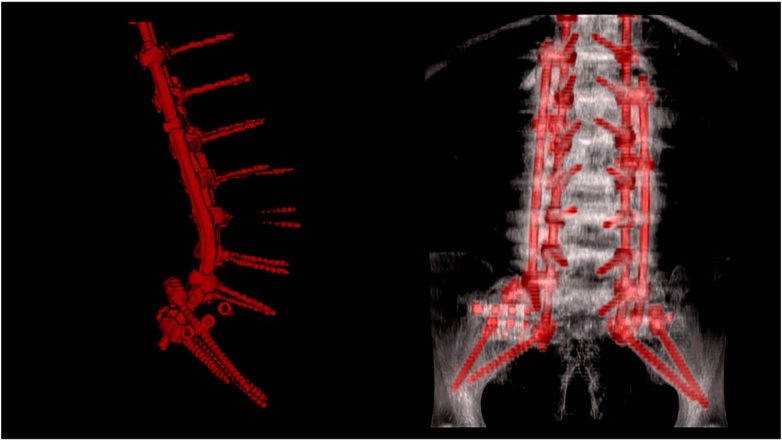
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request. This study is IRB exempt due to policy that permits reports of up to 3 individuals without IRB approval. Type 1 osteotomies were performed from T11-S1: a posterior Smith-Petersen column osteotomy approach was used with a high-speed burr to remove the ligamentum flavum, dorsal caudal lamina, and the superior and inferior articulating facet on the right and left foramen at each level. Following multilevel osteotomy, a decompression was performed over the area of the patient's worst stenosis: L3-L4. Next, spinal implants were placed: this involved sacroiliac fixation, iliac fixation bilaterally, and T10-S1 fixation bilaterally. A stereotactic navigation device was used in order to place the right-sided sacroiliac fixation around the prior implants within her sacral ilium, which were titanium implants blocking the trajectory. A combination of reduction screws and precontoured patient-specific rods were used to correct the adult spinal deformity, which was greater than 30 degrees in AP diameter. Additional satellite rods were then placed bilaterally, and decortication was performed from T10-S2. Autogenous autograft bone and bone morphogenic protein (BMP) was then laid over the T10-S2 regions. Neuromonitoring was stable thought the procedure with no issues (Fig. 2).
Fig. 2.
3-D reconstruction of SI fusion demonstrating circumvention of new SI screws.
This patient had several factors which significantly enhanced the complexity of this case. First, she had been previously morbidly obese and underwent surgery at a BMI just under the threshold of 35, making the soft-tissue dissection deep and complicated. Additionally, her bone was osteoporotic and, therefore, the fixation was particularly challenging and required unusually long screws – which were also very large in diameter – for fixation and correction of her spinal deformity. Together, these two factors lengthened the surgery by approximately 2 h.
Furthermore, the lumbar laminectomy was performed over a region that exhibited heavy scarring and further complicated the procedure. There was a significant amount of complexity encountered when obtaining fixation of the patient's right pelvis, which required stereotactic guidance via O-arm. Because the implants were directly in the path of screw placement, additional care was required (as these screws were quite critical to the foundation of the construct).
3. Discussion
3.1. Observations
Placement of screws to achieve iliac and pelvic fixation is a critical adjunctive technique that can be performed during lumbar fusion. Often, lumbar fusions present with a risk of pseudoarthrosis during scoliosis surgery, particularly at the L5-S1 level, and fusion to the sacrum can prevent L5-S1 pseudoarthrosis [11]. Furthermore, inclusion of the ilium in lumbosacral fusion can lend superior fixation to lumbosacral fusion than can sacral fixation alone [11]. However, including the sacrum in an already long construct poses a difficult biomechanical challenge, which in our case, was further complicated by the presence of a previous SI fusion. Complications and/or drawbacks associated with iliac screw placement include the need for extensive dissection and offset connectors, long screw length and large diameter, and the potential for post-operative painful loosening of screws, which can require reoperation [13], [14], [15].
In order to reduce these complications, the combined use of sacral and iliac alar screws has been implemented and previously described. For example, 2-year follow-up results comparing 26 patients treated with S-2 alar iliac fixation for spinal deformity to 27 patients treated with conventional pelvic fixation demonstrated a reduced rate of deep infection and superior pelvic correction when S-2 alar iliac fixation was used [16]. Furthermore, Matteini reported beneficial outcomes associated with S-2 alar iliac fixation in which posterior decompression and fusion with instrumentation from T-10 to pelvis was used in a patient with post-laminectomy degenerative scoliosis [17]. However, unlike in our case, the pelvic fixation was not obstructed by prior SI fusion. In a unique case described by Laratta, pelvic fixation was performed despite the presence of obstruction from a titanium sacroiliac fusion implant, which was also responsible for obstruction in our case [18]. Like our patient, the patient in this study complained of right thigh and back pain and exhibited disability. The patient's past surgical history includes posterior T11-L5 fusion with instrumentation as well as right SI joint fusion. During surgery, obstruction occurred as a result of the prior SI joint implant. Methods discussed for traversing the obstruction included unilateral iliac wing fixation, placing a short screw that would end in the SI implant, unilateral S2-A1 fixation, burring through the SI implant, or removing the SI implant in a separate procedure [18]. Ultimately, S2-A1 fixation was performed. Unlike in our case, however, O-arm neuronavigation was not employed during the fixation.
The O-arm is a neuronavigation system that can provide computer-assisted stereotactic placement of screws, as previously described by Ray and colleagues [11]. They described the use of O-arm when placing S-2 alar screws in 18 patients, 8 of whom, like our patient, exhibited degenerative scoliosis. 10 of the procedures they described involved fusion of the lower thoracic spine (T9–10) to the pelvis, making them fairly similar to the procedure we performed. Although intraoperative navigation is now a popular and essential tool used by neurosurgeons for intracranial procedures [19], [20], [21], [22], there is not necessarily a need to include intraoperative image guidance in all spinal instrumentation procedures. During pelvic lumbar fixation, however, it allows for maximization of screw length and diameter and aids in determining proper trajectory when placing iliac screws [11]. Furthermore, it has been reported that use of O-arm intraoperative may reduce operative duration as well as intraoperative blood loss in complex procedures such as long thoracolumbar fusions. Additionally, studies have found that O-arm intraoperative navigation results in higher (99 %) accuracy of pedicle screw placement than the freehand method (94.1%) [23], [24]. Future studies are needed to fully identify the benefits of O-arm neuronavigation with respect of posterior instrumentation spine surgery.
4. Conclusions
In this case report, we present a unique case of pelvic fixation via iliac and pelvic screw placement around an obstruction resulting from a previous sacroiliac fusion in an obese, osteoporotic scoliosis patient. O-arm (The O-arm Surgical Imaging System), a technique involving stereotactic navigation for screw placement, was used to aid in placement of the screws around the previous SI fusion. Altogether, these factors provided for a challenging procedure and increased the operative duration by over 2 h.
Provenance and peer review
Not commissioned, externally peer reviewed.
Sources of funding
None declared.
Ethical approval
This study is IRB exempt due to policy that permits reports of up to 3 individuals without IRB approval.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Research registration
n/a
Guarantor
Nolan J. Brown, BS
Summary
We present a complicated case where stereotactic navigation facilitated an extensive fusion and decompression procedure for adult spinal deformity in a morbidly obese patient with multiple prior surgeries for scoliosis and sacroiliac joint pathology.
CRediT authorship contribution statement
Nolan J. Brown: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. Shane Shahrestani: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. Joshua S. Kurtz: Formal analysis, Methodology, Writing – review & editing. Ryan S. Beyer: Writing – review & editing. Martin H. Pham: Supervision, Validation, Visualization, Writing – review & editing. Joseph Osorio: Supervision, Validation, Visualization, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
There were no sources of funding for this work.
References
- 1.Daffner S.D., Vaccaro A.R. Adult degenerative lumbar scoliosis. Am. J. Orthop. (Belle Mead NJ) 2003;32(2):77–82. discussion 82. [PubMed] [Google Scholar]
- 2.Ploumis A., Transfledt E.E., Denis F. Degenerative lumbar scoliosis associated with spinal stenosis. Spine J. 2007;7(4):428–436. doi: 10.1016/j.spinee.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 3.Cho K.-J., Suk S.-I., Park S.-R., et al. Short fusion versus long fusion for degenerative lumbar scoliosis. Eur. Spine J. 2008;17(5):650–656. doi: 10.1007/s00586-008-0615-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grubb S.A., Lipscomb H.J., Suh P.B. Results of surgical treatment of painful adult scoliosis. Spine (Phila Pa 1976) 1994;19(14):1619–1627. doi: 10.1097/00007632-199407001-00011. [DOI] [PubMed] [Google Scholar]
- 5.Marchesi D.G., Aebi M. Pedicle fixation devices in the treatment of adult lumbar scoliosis. Spine (Phila Pa 1976) 1992;17(8 Suppl):S304–S309. doi: 10.1097/00007632-199208001-00016. [DOI] [PubMed] [Google Scholar]
- 6.Schwab F.J., Smith V.A., Biserni M., Gamez L., Farcy J.P., Pagala M. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976) 2002;27(4):387–392. doi: 10.1097/00007632-200202150-00012. [DOI] [PubMed] [Google Scholar]
- 7.Pritchett J.W., Bortel D.T. Degenerative symptomatic lumbar scoliosis. Spine (Phila Pa 1976) 1993;18(6):700–703. doi: 10.1097/00007632-199305000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Darr E., Meyer S.C., Whang P.G., et al. Long-term prospective outcomes after minimally invasive trans-iliac sacroiliac joint fusion using triangular titanium implants. Med. Devices (Auckl) 2018;11:113–121. doi: 10.2147/MDER.S160989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dengler J.D., Kools D., Pflugmacher R., et al. 1-year results of a randomized controlled trial of conservative management vs. Minimally invasive surgical treatment for sacroiliac joint pain. Pain Physician. 2017;20(6):537–550. [PubMed] [Google Scholar]
- 10.Duhon B.S., Bitan F., Lockstadt H., et al. Triangular titanium implants for minimally invasive sacroiliac joint fusion: 2-year follow-up from a prospective multicenter trial. Int. J. Spine Surg. 2016;10:13. doi: 10.14444/3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ray W.Z., Ravindra V.M., Schmidt M.H., Dailey A.T. Stereotactic navigation with the O-arm for placement of S-2 alar iliac screws in pelvic lumbar fixation. J. Neurosurg Spine. 2013;18(5):490–495. doi: 10.3171/2013.2.SPINE12813. [DOI] [PubMed] [Google Scholar]
- 12.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Group S. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 13.Bridwell K.H. Utilization of iliac screws and structural interbody grafting for revision spondylolisthesis surgery. Spine (Phila Pa 1976) 2005;30(6 Suppl):S88–S96. doi: 10.1097/01.brs.0000155562.60754.62. [DOI] [PubMed] [Google Scholar]
- 14.Kuklo T.R., Bridwell K.H., Lewis S.J., et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976) 2001;26(18):1976–1983. doi: 10.1097/00007632-200109150-00007. [DOI] [PubMed] [Google Scholar]
- 15.Tsuchiya K., Bridwell K.H., Kuklo T.R., Lenke L.G., Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976) 2006;31(3):303–308. doi: 10.1097/01.brs.0000197193.81296.f1. [DOI] [PubMed] [Google Scholar]
- 16.Sponseller P.D., Zimmerman R.M., Ko P.S., et al. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine (Phila Pa 1976) 2010;35(20):1887–1892. doi: 10.1097/BRS.0b013e3181e03881. [DOI] [PubMed] [Google Scholar]
- 17.Matteini L.E., Kebaish K.M., Volk W.R., Bergin P.F., Yu W.D., O'Brien J.R. An S-2 alar iliac pelvic fixation. Technical note. Neurosurg Focus. 2010;28(3):E13. doi: 10.3171/2010.1.FOCUS09268. [DOI] [PubMed] [Google Scholar]
- 18.Laratta J.L., Lin J.D., Shillingford J.N., Hardy N.E., Reddy H., Lehman R.A. Obstructed spinopelvic fixation in the setting of a triangular titanium sacroiliac fusion implant: a case description. J. Spine Surg. 2017;3(4):732–735. doi: 10.21037/jss.2017.11.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnett G.H., Miller D.W., Weisenberger J. Frameless stereotaxy with scalp-applied fiducial markers for brain biopsy procedures: experience in 218 cases. J. Neurosurg. 1999;91(4):569–576. doi: 10.3171/jns.1999.91.4.0569. [DOI] [PubMed] [Google Scholar]
- 20.Greenfield J.P., Cobb W.S., Tsouris A.J., Schwartz T.H. Stereotactic minimally invasive tubular retractor system for deep brain lesions. Neurosurgery. 2008;63(4 Suppl 2):334–339. doi: 10.1227/01.neu.0000334741.61745.72. discussion 339–340. [DOI] [PubMed] [Google Scholar]
- 21.Grunert P., Muller-Forell W., Darabi K., et al. Basic principles and clinical applications of neuronavigation and intraoperative computed tomography. Comput. Aided Surg. 1998;3(4):166–173. doi: 10.1002/(SICI)1097-0150(1998)3:4<166::AID-IGS6>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 22.Mangano F.T., Limbrick D.D., Jr., Leonard J.R., Jr., Park T.S., Jr., Smyth M.D., Jr. Simultaneous image-guided and endoscopic navigation without rigid cranial fixation: application in infants: technical case report. Neurosurgery. 2006;58(4 Suppl 2) doi: 10.1227/01.NEU.0000205297.39862.33. discussion ONS-E377. [DOI] [PubMed] [Google Scholar]
- 23.Mattei T.A., Fassett D.R. Letter to the editor: the O-arm revolution in spine surgery. J. Neurosurg. Spine. 2013;19(5):644–647. doi: 10.3171/2013.5.SPINE13474. [DOI] [PubMed] [Google Scholar]
- 24.Silbermann J., Riese F., Allam Y., Reichert T., Koeppert H., Gutberlet M. Computer tomography assessment of pedicle screw placement in lumbar and sacral spine: comparison between free-hand and O-arm based navigation techniques. Eur. Spine J. 2011;20(6):875–881. doi: 10.1007/s00586-010-1683-4. [DOI] [PMC free article] [PubMed] [Google Scholar]