Abstract
Introduction
Autism refers to an early-onset neurodevelopmental condition with characteristic impairments and difficulties in practical living skills, which persist across the lifespan such that adults with autism often require substantial support and comprehensive care. Yet, mental health and other services are frequently unavailable for adults with autism despite considerable need for mental healthcare and individual, familial and socioeconomic burdens. This study will (1) examine current needs, barriers and burdens related to ineffective healthcare of adults with autism in Germany, (2) develop specific recommendations for a need-oriented mental healthcare model and (3) evaluate its future implementation.
Methods and analysis
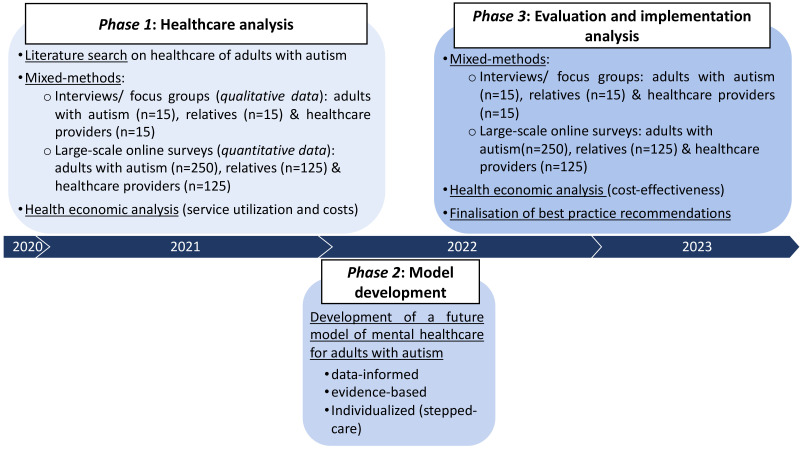
A mixed-methods design with three phases will be conducted. In phase 1, current mental healthcare for adults with autism will be assessed at three levels (individual, structural and professional) and from three perspectives (adults with autism, relatives and healthcare providers) using (1) focus groups/interviews (qualitative data) and (2) large-scale online surveys (quantitative data). Furthermore, service utilisation and related costs will be estimated. In phase 2, recommendations for a future healthcare model will be derived based on phase 1, considering the heterogeneous and complex needs within the autism spectrum and specifying indications for recommended services. In phase 3, these will again be evaluated by the three stakeholder groups using mixed-methods and analysed regarding feasibility of implementation and cost-effectiveness. Our study will, thus, contribute to a better translation of recommendations into practice to reduce disability, burden and costs related to ineffective healthcare and improve mental health outcomes for adults with autism and those who support them.
Ethics and dissemination
This study was approved by the Local Psychological Ethics Commission of the Center for Psychosocial Medicine at the University Medical Center Hamburg-Eppendorf (LPEK-0227). Findings will be disseminated via scientific meetings and peer-reviewed journals. Cooperating partners and associations will be informed about the study’s course and findings by regular newsletters and meetings.
Trial registration number
This study protocol was preregistered at the Open Science Framework (osf.io/5x8pg).
Keywords: health economics, adult psychiatry, mental health
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Systematic analysis of current mental healthcare for adults with autism in Germany addressing the perspectives and needs of people with autism, relatives and healthcare providers. Mixed-methods and health economic analyses to ensure a comprehensive picture and understanding of all perspectives.
Threefold systematic approach: (1) healthcare and needs analysis, (2) subsequent development of specific recommendations for all relevant stakeholders and of a need-oriented, personalised future model of care for adults with autism, (3) evaluation and analysis of future implementation.
Participatory research approach by (1) assessing the perspectives of those who are affected, (2) getting input and feedback from relevant stakeholders throughout all project phases, (3) engaging researchers with autism and clinical researchers, who also work in mental healthcare of adults with autism.
No direct implementation of the developed model within the course of the study. Future funding will be necessary to test implementation, clinical effectiveness and sustainability, for example, within a randomised controlled trial.
Introduction
Autism spectrum disorder, or simply autism, refers to an early-onset lifelong neurodevelopmental condition, which occurs at an estimated prevalence rate of about 1% up to 2%.1 2 Autism is characterised by impairments in social interaction and communication as well as restrictive and repetitive behaviours, including abnormalities in sensory information processing and difficulties in practical living skills.3 These impairments persist across adulthood such that adults with autism often require external, substantial support and comprehensive care across the lifespan.
Yet, autism as a traditionally conceived childhood disorder is commonly under-represented (ie, not diagnosed or treated) in general and mental healthcare services for adults despite considerable healthcare needs of adults with autism, as shown by increased rates of comorbid medical and mental health conditions, premature mortality or risk of suicide.4–8 Medically, autism has been associated with increased rates of various conditions including epilepsy, bowel or gastrointestinal disorders, diabetes, etc.5 6 8 In comparison, rates of mental health comorbidity were found to be particularly increased in adults with autism (ie, more than 80% of patients showed psychiatric comorbidity),8 including anxiety disorders and mood disorders as well sleep disturbances, attention-deficit/hyperactivity disorder (ADHD), and even psychosis.5 These conditions were related to reduced quality of life in adults with autism,9 10 suggesting a particular need for mental health services. Despite this need, observations of ineffective or cost-inefficient healthcare utilisation have been made for adults with autism with respect to primary or medical healthcare such as preventive services, gynaecology, urgent care or emergency department visits,7 8 11 12 as well as mental health services such as psychiatric, therapeutical, counselling, psychopharmacological or other supporting services.12–18 Medical and mental health comorbidities in adults with autism were associated with increased barriers to service use18 as well as healthcare expenditures.8 Analyses of autism-related mental healthcare expenditures using data from psychiatric outpatient clinics in Germany revealed costs comparable with those attributable to schizophrenia.19 Largest cost components arose from inpatient care, pharmacotherapy and occupational therapy, and costs varied as a function of gender, IQ and diagnosis. Asperger syndrome, despite being considered ‘high-functioning’, was associated with higher costs19 and higher unmet healthcare needs.18 Together this evidence highlights the intensity and complexity of healthcare needs associated with autism in adulthood and the pervasive need of a more efficient, extended healthcare system meeting those needs,20 as also emphasised by several national and international ‘autism strategies’ from all over Europe.
In Germany, increased mental healthcare demands are also reflected in the recently growing number of specialised psychiatric outpatient clinics and other services addressing adults with autism or adults seeking diagnostic clarification of potential autism. These developments certainly represent major advancements. However, adults seeking autism diagnostics, post-diagnostic treatment or counselling, psychotherapy and other specialised or supportive services in Germany can be confronted with waiting times up to 2–3 years.14 21 22 Adults with autism seeking psychotherapy reported that the main reason for not receiving any or insufficient treatment was an expressed lack of professional expertise about autism.14 21 Accordingly, therapists also reported barriers due to limited training and experience, and low confidence with respect to treating autism despite high motivation for comprehensive care.23 In fact, diagnosis and treatment of autism indeed require qualified training, can be time-intensive and cost-intensive and often lack validated therapeutical manuals or instruments for use in adults with autism.20 Thus, lack of professional knowledge or training can be considered a major barrier. In addition, multiple other difficulties or barriers have been suggested, which prevent effective and efficient mental healthcare for adults with autism especially for those who struggle with comorbid mental or medical health problems.17
Barriers have been discussed at different levels, nationally24 as well as internationally25–31: at (1) an individual level due to autism-related social-communicative impairments, perceptual peculiarities or difficulties with practical skills of daily living (eg, when making appointments), (2) a system-related or structural level (eg, lack of services or reduced service accessibility across healthcare sectors for adults with autism), and (3) professional level (eg, lack of training/knowledge or stigma about adult autism). Yet, factors that facilitate healthcare for adults with autism have also been suggested (eg, appointment coordination via email, special stimulus-reduced waiting areas, autism-specific training for healthcare providers, shared decision-making, cooperation with relatives/partners, case managers or coordination of care through general practitioners, transition management, specialised medical care centres or financial facilitation for healthcare services).17 26
Among these facilitatory factors, transition management from a familiar and guided paediatric care system to a complex and self-managed care system for adults seems particularly important,12 32–34 considering autism to be a neurodevelopmental condition with limited flexibility and resistance to change. Assistance with transition could not only foster self-management of young adults with autism but also reduce potential burden of care for relatives. In fact, relatives typically compensate for the lack of assistance or services, thereby often facing extensive personal and financial burden35 36 and reduced health-related quality of life themselves.37 38 The amount of evidence on the consequences of an insufficient healthcare system for relatives of adults with autism—not only children—is limited. In addition, support from relatives might not always be available considering the increased age of adults with autism, difficult familial relations or high family concordance rates.39 With increasing prevalence rates of autism,40 however, a rising number of individuals with autism will be transitioning to adult healthcare and needing assistance to access the appropriate healthcare services. Interventions at several levels and assistance with respect to navigation within the healthcare system will also be required to reduce caregiver burden in autism.41
In sum, not only adults with autism but also their relatives and healthcare providers face barriers and are in need of extended services. Recognising autism as a lifelong condition will be a fundamental first step. Yet, in order to increase access, capacity and quality of care for adults with autism, it will be necessary to (1) systematically understand the factors that lead to poorer health status and ineffective healthcare by including the perspectives of all people involved in healthcare access for adults with autism,25 (2) operationalise individual levels of support, define necessary services and their indications, (3) make this information easily accessible to all relevant stakeholders, and (4) finally, implement evidence-based healthcare programmes for adults with autism. Previous evidence was helpful in identifying barriers and pointing to future directions. Many suggestions, however, have yet to find their way into healthcare politics and services, much less being implemented in routine practice. In addition, recommendations often lacked specifics or operationalisations with respect to the selection of services or interventions depending on the individual level of disability and required support (compare with the recent Lancet commission on the future of care in autism: ‘Crucial factors include understanding what works for whom and when, and what are some of the predictable needs and variations that need to be considered to support autistic individuals’42).
Thus, with the current study we seek to, first, systematically analyse current barriers, facilitators and unmet needs—including their economic and personal consequences—in mental healthcare of adults with autism in Germany at three relevant levels (individual, structural and professional) and from three relevant perspectives (adults with autism, relatives and healthcare providers). While the focus of the study is on mental healthcare (ie, particularly, diagnosis, therapy and supportive services), the study will also examine all health-related services relevant for adults with autism given the aforementioned complexity of the condition. Second, we seek to use these data to develop specific recommendations for a need-oriented, future model of mental healthcare and supporting services for adults with autism, which will consider the heterogeneity within the autism spectrum, different service needs and individual indications for services. Third, this model will be evaluated by the three stakeholder groups and analysed with respect to implementation in healthcare routines and cost-effectiveness. During all phases, the study will strengthen a participatory research approach by engaging autism-trained clinicians and adults with autism in the scientific process and by collaborating with autism-related, parental-related and service-related associations. The long-term aim of the study is to contribute to more effective mental healthcare for adults with autism by providing specific recommendations for clinical practice and healthcare policies, also improving mental health outcomes for adults with autism and those who support them.
Methods and analysis
This study protocol was written in adherence to the SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) checklist for study protocols for items applicable to the present protocol of a non-interventional, observational study.
Study population
Three stakeholder perspectives will be assessed. We will recruit (1) adults with autism with varying degrees of needed support, (2) close relatives (first or second degree) or partners of adults with early-diagnosed and late-diagnosed autism, and (3) healthcare service providers throughout Germany. For qualitative data collection (ie, focus groups), we will primarily recruit providers of mental healthcare services with experience in treating patients or clients with autism in order to gain central information about the current state of mental healthcare, including barriers and needs, for adults with autism in Germany and to support coherent discussions. Primary care practitioners and paediatrists will also be recruited due to their particular role in transition and coordination of care. Given the often complex health status and broad service needs of adults with autism as well as supposed barriers throughout the care system (eg, due to lack of knowledge about autism), the large-scale online surveys will also include data from healthcare providers with various professional backgrounds and levels of experience with autism (from working in autism-specific services to more general services or no expertise in autism) in order to gather a more comprehensive and representative picture on barriers and needs with respect to treating adults with autism and to examine whether qualitatively identified barriers and needs also apply to different healthcare settings. Inclusion of different professional backgrounds and levels of experience with autism along with other relevant criteria (eg, geographical distribution, urban or countryside, etc) will be ensured by predefined recruitment strategies and collection of corresponding sociodemographic data via questionnaire in the recruitment and data collection process.
Participants with autism must be adults (18+ years) and must have a secured diagnosis of autism without intellectual disability (IQ >70), sufficient ability to provide informed consent and sufficient language skills to answer the questions. Participants with intellectual disability (IQ <70), insufficient German skills and ability to give informed consent will be excluded. Participants will be recruited throughout Germany using purposive, quota and snowball sampling via the study’s collaborating network of cooperating partners, publicly available contacts from autism-related associations (including self-help/ support and caregiver groups), healthcare associations (medical chambers, therapist associations, etc), local and countrywide outpatient clinics as well as social media. Participants will be informed in detail about the study and data protection in accordance with the General Data Protection Regulation, and informed consent will be obtained prior to participation. No expense allowance will be paid (with the exception of possible travel expenses for participation in interviews/focus groups).
Study design and data collection
The study will evolve over a period of 3 years (October 2020–September 2023). A three-phase design will be implemented (figure 1).
Figure 1.
Timeline and three study phases.
Phase 1: healthcare and needs analysis
First, a literature search on national and international evidence will be conducted in PubMed to identify previously published barriers, facilitators and needs related to healthcare and mental healthcare of adults with autism. Results will be used to develop guideline questions for qualitative data collection. Three interview guides will be developed, tailored to each stakeholder group. Participants’ experiences with healthcare or with provision of services/treatment of adults with autism will be assessed. Barriers, facilitators and needs in healthcare of adults with autism, especially with focus on mental healthcare (ie, diagnostics, therapy and assisting services), at individual, professional, and structural levels and recommendations for improving mental healthcare for adults with autism will be discussed. Guideline questions will be administered by trained researchers in semistructured one-on-one interviews with adults with autism (n=15) and structured focus groups with relatives/partners of adults with autism (n=15) as well as healthcare providers (n=15). All interviews and focus groups will be audio-recorded. An external, specifically transcription-qualified and bound-to-secrecy person will transcribe recordings verbatim. Because of the dynamics of the COVID-19 pandemic, interviews and focus groups will be conducted online enabled by an online video communication provider. To meet individual difficulties in communication and flexibility, participants with autism will also be given the chance to answer interview questions in a written format, via chat or phone. All qualitative data will be pseudonymised, that is, personal identifying information (eg, names) will be removed. Only pseudonymised data will be further analysed. All data will be stored on secured servers of the University Medical Center Hamburg-Eppendorf.
Second, for large-scale online surveys, open-ended and close-ended items (eg, implementing a 5-point Likert scale) on barriers and needs in mental healthcare of adults with autism will be generated through consented discussion in the research team based on qualitative results, that is, themes that emerged from interviews/focus groups. These items will be similarly assessed across stakeholder groups. The mixed-methods approach aims to obtain a complete set of information to develop specific recommendations for a future healthcare model for adults with autism. In addition, items specific to each group of participants will be included such as items related to service provision in professionals (eg, waiting times), related to informal care in relatives, and to service utilisation and comorbidities in adults with autism. Thus, separate online surveys will be developed for each stakeholder group (adults with autism; relatives of adults with autism; healthcare providers) that will be used to collect quantitative data in larger samples and provide an overview of the healthcare situation for adults with autism in Germany from multiple perspectives. Online surveys, that is, barrier-related and needs-related items, will be explored with respect to psychometric properties, such as content and construct validity, discriminability and internal consistency, for example, via correlational or exploratory factor analyses. We will also examine floor and ceiling effects using descriptive analyses. As proxy for acceptability, we will examine patterns of missing data or low response rates. In addition, standardised, psychometric questionnaires and patient-reported outcomes will be employed in participants with autism and relatives. They will be asked to complete questionnaires related to health-related quality of life (eg, EQ-5D-5L),43 disability/functioning (eg, WHO Disability Assessment Schedule 2.0)44 and a German version of the ‘barriers to healthcare’ questionnaire.29 Relatives will additionally be asked to rate their burden of care (eg, CarerQoL).45 These represent previously validated instruments with good overall validity and reliability.29 43–45 Moreover, in both groups, variables related to disease/healthcare history, utilisation of medical and non-medical services, and productivity losses will be collected (eg, days spent on sick leave, hospital days, physician contacts or informal care) through modified versions of the FIMA (Fragebogen zur Erhebung von Gesundheitsleistungen im Alter) and FIMPsy (Fragebogen zur Inanspruchnahme medizinischer und nicht medizinischer Versorgungsleistungen bei psychischen Erkrankungen) questionnaires.46 47
Person-identifying information will not be requested. Online surveys will be delivered countrywide by an online survey software in German based at protected servers. Separate survey versions will be provided to adults with autism (n=250), relatives (n=125) and healthcare providers (n=125). Participation will take place in a completely anonymised manner. Participants will be automatically assigned randomly generated IDs. Personal information entered in free text fields will be removed or anonymised. Data collection will be continuously monitored and managed by members of the research team.
Phase 2: development of recommendations for a future healthcare model for adults with autism
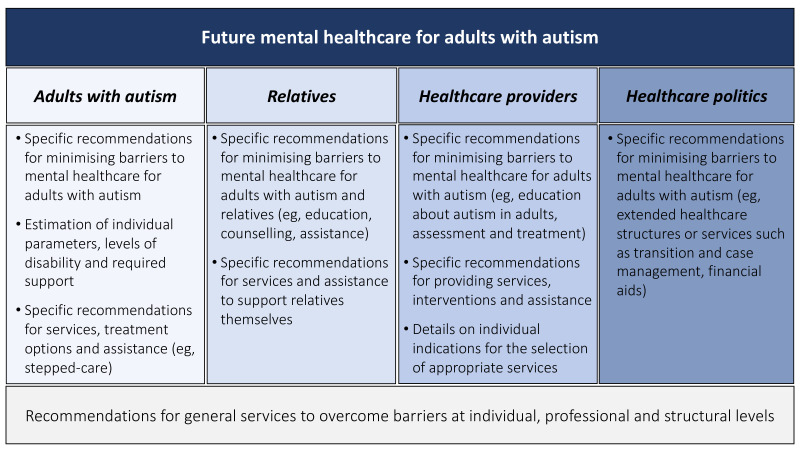
A literature search on possibly existing healthcare recommendations or implementation models for adults with autism and related conditions will be conducted in PubMed and Google and—together with the results from the mixed-methods data in phase 1—fed into the development of an extended, need-oriented mental healthcare model for adults with autism. This model will include recommendations for actions/interventions at different levels (individual, structural and professional) and will be addressed to the stakeholder groups (adults with autism; relatives of adults with autism; healthcare providers and policymakers/politics; figure 2). Given the heterogeneity of symptom severity, functional impairments, rates of comorbidity and needed support within the autism spectrum, a multiprofessional stepped or collaborative care approach as similarly proposed for psychosis or depression,48 might represent a possible framework for an alternative care model for adults with autism as opposed to current standard care (as also suggested by Lord et al42). Stepped mental healthcare for autism may range from low-level, evidence-based services (eg, educational programmes or information/consulting about autism and available treatment options, e-mental health) over mid-level (eg, improved diagnostics, autism-informed psychotherapy, occupational therapy or sociotherapy) to high-level services, which are often unavailable to adults with autism in Germany (eg, case managers, integrated care, medical healthcare centres, inpatient care). Recommendations for possible individual steps, services offered within each step and indications for services will be specified. Besides recommendations for adults with autism, the future healthcare model will also provide recommendations for relatives of adults with autism, healthcare providers and policymakers (figure 2). More specifically, relatives or partners who support an adult with autism are often in need of support themselves. Thus, the model will also include recommendations for relatives. Conversely, for healthcare providers, recommendations could include suggestions to advance knowledge about specific needs of adults with autism and promote awareness for these needs in different mental healthcare sections. For policymakers, recommendations will focus on extended services to reduce structural barriers. These will be underlined by the health-economic data collected within phases 1 and 3.
Figure 2.
Future model of mental healthcare for adults with autism: relevant stakeholders and target groups.
Phase 3: evaluation and implementation analysis
Methods will be analogous to phase 1 (mixed-methods, qualitative interviews/focus groups and quantitative online surveys with adults with autism, relatives of adults with autism and healthcare providers) with emphasis on evaluation and implementation of the developed recommendations for a future healthcare model. Based on the ‘Consolidated Framework for Implementation Research’, an implementation of the model will be explored to improve the feasibility of a potential implementation.49 The developed model and its components will be evaluated by all stakeholder groups in a structured evaluation process based on different dimensions such as acceptability, appropriateness, cost, feasibility and sustainability.50 In phase 3, participants from phase 1 will be re-recruited or, if this is not possible, comparable representatives will be invited. In addition, we will invite participants from other backgrounds such as healthcare politics/policies. Furthermore, participants will be, for example, asked to rate to what extent (1) barriers and needs identified during phase 1 will be addressed by the model, (2) whether suggested services are already implemented in standard German healthcare, (3) which services might be easier or more feasible to be implemented and (4) give feedback about service requirements (eg, indications, training, time/financial resources, personnel). The mixed-methods design (including open-ended questions during online surveys) will allow direct feedback and potential indications for modifications. In addition, standardised implementation-related questionnaires will be employed.51 As the model’s actual implementation is not part of the study, we would like to use this phase to gather enough information, including positive and critical aspects, for a potential implementation. Finally, based on the results of phase 3, the developed recommendations and model for improving healthcare for adults with autism will be reviewed and, if necessary, revised.
Sample sizes
Based on power calculation, a minimum of n=500 participants will be aimed at for each quantitative online survey. This sample size represents the minimum number of participants needed for group comparisons with at least medium effect sizes (d=0.50) at a power of 80% and an alpha error of 5%. Previously published related online surveys with participants with autism or caregivers have reported dropout rates of 15%–35% due to reasons such as incomplete or duplicate responses, failure to consent or to meet inclusion criteria.52 53 Thus, here to compensate for dropouts, participants will be over-recruited (ie, a dropout rate of 15% would correspond to 75 additional participants). The motivation to participate in scientific studies can be considered high in the autism community, particularly regarding participation in online surveys and research with impact to their everyday life. Yet, if recruitment targets are not met, the following steps will be taken to achieve planned sample sizes: extension of the data collection time window, increased networking as well as enhanced promotion of our research via associations, social media and community outreach.
Qualitative data will not be used for direct hypotheses testing so that sample size does not need to be based on power analyses. Here sample size (a total of N=−90) was chosen based on previously published recommendations.54
Data analyses
Qualitative data from phases 1 and 3 will be analysed according to the thematic analysis approach55 using the software MAXQDA. Deductive or theoretical categories based on previously published evidence relevant to each phase will drive the analyses. Because the study will focus on subjective experiences/perspectives, data analyses will be complemented by an inductive approach. Data analyses will be conducted by two trained researchers. Emerging themes, subthemes and codes related to barriers and needs in mental healthcare (phase 1) and evaluation/implementation of derived recommendations for extended care (phase 3) will be discussed by the two researchers and agreed upon by the research team. A third researcher will be consulted upon disagreement.
Quantitative data from online surveys in phases 1 and 3 will be exported to and analysed using the statistical software SPSS Statistics 27 and R. Before analyses, exported survey data will be manually checked by members of the research team. We will run descriptive statistical analyses and report frequencies/percentages, means/medians and SDs/IQRs separate for each stakeholder group on, if applicable: (1) sociodemographic data (eg, age, gender, education, employment status, profession), (2) clinical data (eg, diagnosis, comorbidities, service utilisation), (3) objective healthcare indicators (eg, waiting times for or distances of services), (4) subjective ratings on barriers and needs in mental healthcare (phase 1) or evaluative ratings on implementation of the developed care model (phase 3),49 50 and (5) scores on the implemented standardised questionnaires related to barriers to healthcare,29 health-related quality of life,43 disability and functioning,44 burden of care45 and implementation.51 Primary outcome will be service utilisation in the last 6 months as assessed in the online surveys and groups of adults with autism and relatives. In order to determine predictors of healthcare utilisation of adults with autism in Germany and, thus, also inform the development of an extended care model in phase 2 (eg, indications for services (cf. 42)) multiple regression analyses will be conducted. The following variables will be tested as potential predictors, that is, enabling or disabling healthcare utilisation: sociodemographic variables (eg, gender, age, education), autism diagnosis, symptom severity/level of required support according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition,3 comorbidity and experienced barriers to healthcare as operationalised by the score on the ‘barriers to healthcare’ questionnaire29 as well as by ratings from our own online survey. With respect to the latter, a factor analysis will be performed in order to identify underlying dimensions. Scores of factors with the highest variance will then be used as predictors for regression analyses. In secondary, more exploratory, analyses, we aim to test for mean differences between stakeholder groups on subjective ratings of barriers and needs in mental healthcare (phase 1) and evaluation/implementation of the developed need-oriented model (phase 3), using stakeholder group as independent variable and ratings as dependent variable employing parametric or non-parametric statistical tests depending on scale level and data distribution. Quantitative data will be tested statistically based on 95% CIs.
Health-economic analyses in phases 1 and 3 will be informed by a previously conducted systematic review of the literature on cost-of-illness and cost-effectiveness studies in autism. The systematic review will be carried out in agreement with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Standard databases such as Medline/PubMed and PsycInfo as well as reference lists will be searched for international studies in English or German. The search term will focus on “costs of illness”, “health expenditures”, “cost effectiveness” or “cost analysis”, “burden of illness”, “economic burden” and “autism spectrum disorders”, combined with Boolean operators. In phase 1, in addition to service utilisation, productivity losses in the last 6 months as well as out-of-pocket payments will be directly assessed in adults with autism. In addition, relatives will also be asked about aspects that might be related to their relative with autism, like informal care provision or reduced working time. To estimate direct costs, service utilisation will be evaluated in monetary terms using standardised unit costs.56 57 Indirect costs due to productivity losses (eg, due to incapacity to work) will be estimated with the human capital approach. The estimated costs for adults with autism will then be compared with the general German population, and excess costs will be calculated.58 Under the assumption that differences in sociodemographic covariates or comorbidities across groups are adjusted, the excess cost approach enables the analysis of all costs attributable to autism. Based on the skewed distribution of cost data, cost differences will be calculated using generalised linear models with gamma distribution and log-link function. Our findings will also be compared with other evidence on cost-of-illness in autism and other mental health conditions such as depression as common mental disorder, schizophrenia as disorder with similar prevalence or ADHD as other developmental disorder. In phase 3, health-economic analyses will focus on the evaluation of the potential costs and effects of the developed future healthcare model using health-economic modelling. The cost-effectiveness analysis will assess the incremental cost-effectiveness ratio of the developed healthcare model compared with the status quo. This is calculated as the ratio of the difference in costs (between healthcare intervention and status quo) to the difference in health effects of both respective groups. The costs are to be determined from a societal perspective, that is, in addition to purely medical costs, non-medical costs and monetarily assessed productivity losses will also be taken into account. As a measure of the health effects, that is, health-related quality of life, quality-adjusted life years (QALYs) will be estimated based on the findings from the EQ-5D-5L.43
Patient and public involvement
The stakeholders’ perspectives are systematically included given the mixed-methods design. Research will be undertaken in close collaboration with federal and local patient, parental and healthcare or autism-related organisations, from which we obtained collaboration agreements prior to submission to the funding agency as well as during the initial course of the study. Representatives of these organisations will be continuously informed over the course of the study via regular meetings and asked to provide feedback during each study phase. They will also be invited to participate in focus groups and qualitative interviews and asked to support further recruitment of study participants. Cooperation partners and all other study participants from focus groups and interviews will be offered to receive quarterly newsletters about the course and interim findings of the study. For all other participants (eg, who anonymously took part in the online surveys), information will be made publicly available on a project website. Participants will be given the possibility to express feedback or concerns via the project’s email address or direct contact to one of our (peer) researchers.
Ethics and dissemination
Ethics approval and consent to participate
The study will be carried out in accordance with the WMA Declaration of Helsinki and has been approved by the Local Psychological Ethics Commission of the Center for Psychosocial Medicine of the University Medical Center Hamburg-Eppendorf (ref.# LPEK-0227). Study participation is voluntary and no foreseeable risks for participants result from the participation. Participants will be fully informed about the aims of the study, data collection, handling and storage. Written informed consent will be obtained before participation. Preserving principles of data sensitivity, data protection and confidentiality requirements will be met.
Dissemination
Findings will be disseminated via national and international scientific meetings and peer-reviewed journals in the field of autism and healthcare research. Cooperating partners and associations will be informed about the study’s course and findings by quarterly newsletters and biannual meetings. Study participants from focus groups and interviews will also receive quarterly newsletters about the progression and outcomes of the study. Information, including study information, posters and presentations, will also be disseminated via the project’s webpage.
Discussion
This study protocol outlines several urgent challenges related to mental healthcare for adults with autism in Germany. The study will provide a systematic analysis of the current state of healthcare for adults with autism, including barriers and requirements experienced by persons with autism themselves, but also their relatives and healthcare providers. The results will be used to facilitate a real-world, data-informed and evidence-based future model of mental healthcare for adults with autism, which seeks to overcome current barriers by developing specific practice recommendations at individual, structural and professional levels aiding all stakeholder groups. The model will provide suggestions for all involved stakeholders including policymakers.
Strengths and limitations
One strength of this study is that it aims to define individual characteristics that might be useful to assess a person’s need of support and provide specific treatment suggestions and indications for mental healthcare and other related services that are relevant for adults with autism (‘understanding what works for whom and when’).42 Another strength is that this study will evaluate the developed recommendations and model conceptions for future care with respect to implementation chances, acceptability, feasibility, sustainability, cost-effectiveness and other dimensions and prepare for a future implementation. As such, the current study goes beyond previously published analyses of healthcare and published suggestions for improvement of care for individuals with autism, adults in particular.
For a long time, research or healthcare politics have overlooked, neglected or ignored individuals with autism and their families in information and decision-making processes.52 59 Here, participatory research will be realised in a threefold fashion. First, results will be obtained by directly asking those who are affected (adults with autism, relatives and healthcare providers) about real-world experiences and their attitude towards the developed research. Second, researchers serving mental healthcare of adults with autism, and researchers with autism will conduct the study. Third, the research will be undertaken in close collaboration with patient, parental and healthcare organisations, which will be continuously informed over the course of the study and asked to provide feedback during each study phase.
One limitation of the study is that the developed mental healthcare model for adults with autism will not be practically applied during the course of the study. Future funding will be necessary to test implementation, clinical effectiveness and sustainability of the developed recommendations and services, for example, within a randomised controlled trial. This will allow for further refinement and specifics to foster large-scale implementation. Yet, as the study is funded by the German Federal Joint Committee—the highest decision-making body of the joint self-government of practitioners, hospitals and health insurance funds in Germany—this study will likely have a direct and immediate impact on healthcare policies and contribute to improving outcomes in people and families with autism and reducing individual, familial and socioeconomic burdens associated with a lack of services for adults with autism.
Supplementary Material
Footnotes
Contributors: HS is the main PI for the study. DS, AK, KV, ND and JP are co-PIs. They all conceptualised and designed the study. SD, PG, HK, PR and FE are research staff. SD is also a graduate student. ND and JP mainly drafted this manuscript. All authors participated, reviewed and edited the manuscript; all authors approved the final version of the manuscript.
Funding: This work was supported by the Innovation Fund of the German Federal Joint Committee (Gemeinsamer Bundesausschuss, G-BA, study 'BarrierefreiASS'/grant number: 01VSF19011 awarded to HS (PI)).
Disclaimer: The funding body had no role in the design of the study or in writing the manuscript, nor will they have a role in data collection, analyses or interpretation of data.
Competing interests: DS received honoraria for lectures from or has been an advisor to Janssen, ROVI, Lundbeck, Otsuka Pharma and Takeda. The remaining authors do not declare other competing interests.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Baio J, Wiggins L, Christensen DL, et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveill Summ 2018;67:1–23. 10.15585/mmwr.ss6706a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lundstrom S, Reichenberg A, Anckarsater H, et al. Autism phenotype versus registered diagnosis in Swedish children: prevalence trends over 10 years in general population samples. BMJ 2015;350:h1961. 10.1136/bmj.h1961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC, 2013. [Google Scholar]
- 4.Hirvikoski T, Mittendorfer-Rutz E, Boman M, et al. Premature mortality in autism spectrum disorder. Br J Psychiatry 2016;208:232–8. 10.1192/bjp.bp.114.160192 [DOI] [PubMed] [Google Scholar]
- 5.Croen LA, Zerbo O, Qian Y, et al. The health status of adults on the autism spectrum. Autism 2015;19:814–23. 10.1177/1362361315577517 [DOI] [PubMed] [Google Scholar]
- 6.Kohane IS, McMurry A, Weber G, et al. The co-morbidity burden of children and young adults with autism spectrum disorders. PLoS One 2012;7:e33224. 10.1371/journal.pone.0033224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nicolaidis C, Kripke CC, Raymaker D. Primary care for adults on the autism spectrum. Medical Clinics of North America 2014;98:1169–91. 10.1016/j.mcna.2014.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vohra R, Madhavan S, Sambamoorthi U. Comorbidity prevalence, healthcare utilization, and expenditures of Medicaid enrolled adults with autism spectrum disorders. Autism 2017;21:995–1009. 10.1177/1362361316665222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mason D, Mackintosh J, McConachie H, et al. Quality of life for older autistic people: the impact of mental health difficulties. Res Autism Spectr Disord 2019;63:13–22. 10.1016/j.rasd.2019.02.007 [DOI] [Google Scholar]
- 10.Mason D, McConachie H, Garland D, et al. Predictors of quality of life for autistic adults. Autism Research 2018;11:1138–47. 10.1002/aur.1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vohra R, Madhavan S, Sambamoorthi U. Emergency department use among adults with autism spectrum disorders (ASD). J Autism Dev Disord 2016;46:1441–54. 10.1007/s10803-015-2692-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ames JL, Massolo ML, Davignon MN, et al. Healthcare service utilization and cost among transition-age youth with autism spectrum disorder and other special healthcare needs. Autism 2021;25:705–18. 10.1177/1362361320931268 [DOI] [PubMed] [Google Scholar]
- 13.Schott W, Nonnemacher S, Shea L. Service use and unmet needs among adults with autism awaiting Home- and community-based Medicaid services. J Autism Dev Disord 2021;51:1188–200. 10.1007/s10803-020-04593-2 [DOI] [PubMed] [Google Scholar]
- 14.Lipinski S, Blanke ES, Suenkel U, et al. Outpatient psychotherapy for adults with high-functioning autism spectrum condition: utilization, treatment satisfaction, and preferred modifications. J Autism Dev Disord 2019;49:1154–68. 10.1007/s10803-018-3797-1 [DOI] [PubMed] [Google Scholar]
- 15.Croteau C, Mottron L, Dorais M, et al. Use, costs, and predictors of psychiatric healthcare services following an autism spectrum diagnosis: population-based cohort study. Autism 2019;23:2020–30. 10.1177/1362361319840229 [DOI] [PubMed] [Google Scholar]
- 16.Płatos M, Pisula E. Service use, unmet needs, and barriers to services among adolescents and young adults with autism spectrum disorder in Poland. BMC Health Serv Res 2019;19. 10.1186/s12913-019-4432-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maddox BB, Crabbe S, Beidas RS, et al. “I wouldn’t know where to start”: Perspectives from clinicians, agency leaders, and autistic adults on improving community mental health services for autistic adults. Autism 2020;24:919–30. 10.1177/1362361319882227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vogan V, Lake JK, Tint A, et al. Tracking health care service use and the experiences of adults with autism spectrum disorder without intellectual disability: a longitudinal study of service rates, barriers and satisfaction. Disabil Health J 2017;10:264–70. 10.1016/j.dhjo.2016.11.002 [DOI] [PubMed] [Google Scholar]
- 19.Hofer J, Hoffmann F, Dorks M. Health services use and costs in individuals with autism spectrum disorder in Germany: results from a survey in ASD outpatient clinics. J Autism Dev Disord 2021. (published Online First: 2021/03/18). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kamp-Becker I, Poustka L, Bachmann C, et al. Study protocol of the ASD-Net, the German research Consortium for the study of autism spectrum disorder across the lifespan: from a better etiological understanding, through valid diagnosis, to more effective health care. BMC Psychiatry 2017;17:206. 10.1186/s12888-017-1362-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lipinski S, Boegl K, Blanke ES, et al. A blind spot in mental healthcare? Psychotherapists lack education and expertise for the support of adults on the autism spectrum. Autism 2021;26:13623613211057973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gawronski A, Kuzmanovic B, Georgescu A. Expectations concerning psychotherapy of high-functioning adults with autism spectrum disorders]. Fortschr Neurol Psychiatr 2011;79:647–54. [DOI] [PubMed] [Google Scholar]
- 23.Brookman-Frazee L, Drahota A, Stadnick N, et al. Therapist perspectives on community mental health services for children with autism spectrum disorders. Adm Policy Ment Health 2012;39:365–73. 10.1007/s10488-011-0355-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dern S, Sappok T. Barriers to healthcare for people on the autism spectrum. Adv Autism 2016;2:2–11. 10.1108/AIA-10-2015-0020 [DOI] [Google Scholar]
- 25.Calleja S, Islam FMA, Kingsley J. Healthcare access for autistic adults a systematic review. Medicine 2020;99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mason D, Ingham B, Urbanowicz A, et al. A systematic review of what barriers and facilitators prevent and enable physical healthcare services access for autistic adults. J Autism Dev Disord 2019;49:3387–400. 10.1007/s10803-019-04049-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fenikilé TS, Ellerbeck K, Filippi MK, et al. Barriers to autism screening in family medicine practice: a qualitative study. Prim Health Care Res Dev 2015;16:356–66. 10.1017/S1463423614000449 [DOI] [PubMed] [Google Scholar]
- 28.Malik-Soni N, Shaker A, Luck H, et al. Tackling healthcare access barriers for individuals with autism from diagnosis to adulthood. Pediatr Res 2022;91:1028-1035. 10.1038/s41390-021-01465-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Raymaker DM, McDonald KE, Ashkenazy E, et al. Barriers to healthcare: instrument development and comparison between autistic adults and adults with and without other disabilities. Autism 2017;21:972–84. 10.1177/1362361316661261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nicolaidis C, Raymaker D, McDonald K, et al. Comparison of healthcare experiences in autistic and non-autistic adults: a cross-sectional online survey facilitated by an academic-community partnership. J Gen Intern Med 2013;28:761–9. 10.1007/s11606-012-2262-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nicolaidis C, Raymaker DM, Ashkenazy E, et al. "Respect the way I need to communicate with you": Healthcare experiences of adults on the autism spectrum. Autism 2015;19:824–31. 10.1177/1362361315576221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Freitag CM, Poustka L, Kamp-Becker I. Transition in autism spectrum disorders. Z Kinder Jug-Psych 2020;48:440–2. [DOI] [PubMed] [Google Scholar]
- 33.King C, Merrick H, Le Couteur A. How should we support young people with ASD and mental health problems as they navigate the transition to adult life including access to adult healthcare services. Epidemiol Psychiatr Sci 2020;29:e90. 10.1017/S2045796019000830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Enner S, Ahmad S, Morse AM, et al. Autism: considerations for transitions of care into adulthood. Curr Opin Pediatr 2020;32:446–52. 10.1097/MOP.0000000000000882 [DOI] [PubMed] [Google Scholar]
- 35.Cadman T, Eklund H, Howley D, et al. Caregiver burden as people with autism spectrum disorder and attention-deficit/hyperactivity disorder transition into adolescence and adulthood in the United Kingdom. J Am Acad Child Adolesc Psychiatry 2012;51:879–88. 10.1016/j.jaac.2012.06.017 [DOI] [PubMed] [Google Scholar]
- 36.Rogge N, Janssen J. The economic costs of autism spectrum disorder: a literature review. J Autism Dev Disord 2019;49:2873–900. 10.1007/s10803-019-04014-z [DOI] [PubMed] [Google Scholar]
- 37.Boehm TL, Carter EW, Taylor JL. Family quality of life during the transition to adulthood for individuals with intellectual disability and/or autism spectrum disorders. Am J Intellect Dev Disabil 2015;120:395–411. 10.1352/1944-7558-120.5.395 [DOI] [PubMed] [Google Scholar]
- 38.Johnson N, Frenn M, Feetham S, et al. Autism spectrum disorder: parenting stress, family functioning and health-related quality of life. Fam Syst Health 2011;29:232–52. 10.1037/a0025341 [DOI] [PubMed] [Google Scholar]
- 39.Tick B, Bolton P, Happé F, et al. Heritability of autism spectrum disorders: a meta-analysis of twin studies. J Child Psychol Psychiatry 2016;57:585–95. 10.1111/jcpp.12499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matson JL, Kozlowski AM. The increasing prevalence of autism spectrum disorders. Res Autism Spectr Disord 2011;5:418–25. 10.1016/j.rasd.2010.06.004 [DOI] [Google Scholar]
- 41.Iadarola S, Pérez-Ramos J, Smith T, et al. Understanding stress in parents of children with autism spectrum disorder: a focus on under-represented families. Int J Dev Disabil 2019;65:20–30. 10.1080/20473869.2017.1347228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lord C, Charman T, Havdahl A, et al. The Lancet Commission on the future of care and clinical research in autism. Lancet 2022;399:271–334. 10.1016/S0140-6736(21)01541-5 [DOI] [PubMed] [Google Scholar]
- 43.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ustun TB, Kostanjesek N, Chatterji S. Measuring health and disability: manual for who disability assessment schedule (WHODAS 2.0) / edited by T.B. Üstün, N. Kostanjsek, S. Chatterji, J.Rehm. Geneva: World Health Organization, 2010. [Google Scholar]
- 45.Brouwer WBF, van Exel NJA, van Gorp B, et al. The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual Life Res 2006;15:1005–21. 10.1007/s11136-005-5994-6 [DOI] [PubMed] [Google Scholar]
- 46.Seidl H, Bowles D, Bock J-O, et al. [FIMA--questionnaire for health-related resource use in an elderly population: development and pilot study]. Gesundheitswesen 2015;77:46–52. 10.1055/s-0034-1372618 [DOI] [PubMed] [Google Scholar]
- 47.Grupp H, König H-H, Riedel-Heller S, et al. [FIMPsy - Questionnaire for the Assessment of Medical and non Medical Resource Utilisation in Mental Disorders: Development and Application]. Psychiatr Prax 2018;45:87–94. 10.1055/s-0042-118033 [DOI] [PubMed] [Google Scholar]
- 48.Watzke B, Heddaeus D, Steinmann M, et al. Effectiveness and cost-effectiveness of a guideline-based stepped care model for patients with depression: study protocol of a cluster-randomized controlled trial in routine care. BMC Psychiatry 2014;14:230. 10.1186/s12888-014-0230-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:50. 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011;38:65–76. 10.1007/s10488-010-0319-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lindig A, Hahlweg P, Christalle E, et al. Translation and psychometric evaluation of the German version of the organisational readiness for implementing change measure (oriC): a cross-sectional study. BMJ Open 2020;10:e034380. 10.1136/bmjopen-2019-034380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pellicano E, Dinsmore A, Charman T. What should autism research focus upon? community views and priorities from the United Kingdom. Autism 2014;18:756–70. 10.1177/1362361314529627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Weir E, Allison C, Baron-Cohen S. Autistic adults have poorer quality healthcare and worse health based on self-report data. Mol Autism 2022;13:23. 10.1186/s13229-022-00501-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guest G, Namey E, McKenna K. How many focus groups are enough? building an evidence base for Nonprobability sample sizes. Field methods 2017;29:3–22. 10.1177/1525822X16639015 [DOI] [Google Scholar]
- 55.Braun V, Clarke V. What can "thematic analysis" offer health and wellbeing researchers? Int J Qual Stud Health Well-being 2014;9:26152. 10.3402/qhw.v9.26152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bock JO, Brettschneider C, Seidl H, et al. Ermittlung standardisierter Bewertungssätze AUS gesellschaftlicher Perspektive für die gesundheitsökonomische evaluation. Gesundheitswesen 2015;77:53–61. [DOI] [PubMed] [Google Scholar]
- 57.Grupp H, König H-H, Konnopka A. Kostensätze Zur monetären Bewertung von Versorgungsleistungen bei psychischen Erkrankungen. Gesundheitswesen 2017;79:48–57. [DOI] [PubMed] [Google Scholar]
- 58.Grupp H, König H-H, Konnopka A. Health care utilisation and costs in the general population in Germany. Health Policy 2016;120:159–69. 10.1016/j.healthpol.2015.11.005 [DOI] [PubMed] [Google Scholar]
- 59.Pellicano E, Stears M, Autism B. Bridging autism, science and society: moving toward an ethically informed approach to autism research. Autism Res 2011;4:271–82. 10.1002/aur.201 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.