Abstract
Objectives
Action planning is a brief and effective behaviour change technique (BCT) to improve physical activity (PA) and diet behaviour (DB). This study aimed to identify critical BCTs and mechanisms of action (MoAs) to interpret the effectiveness of planning interventions based on the Health Action Process Approach (HAPA) model.
Design
Systematic review.
Data sources
PubMed, Web of Science, CINAHL (EBSCO), PsycINFO (EBSCO), Psychology and Behavioural Sciences Collection (EBSCO), psyARTICLES and Medline were searched for studies from January 1990 to September 2021 published in English.
Eligibility criteria
Experiment involving action planning intervention to improve PA or DB in community-dwelling adult patients with chronic conditions.
Data extraction and synthesis
Two reviewers independently coded the planning interventions into BCT combinations and MoA assemblies. Outcome was dichotomised according to the statistical power and Cohen’s d. The Cochrane risk of bias assessment tool and the Risk of Bias in Nonrandomized Studies–of Interventions assessment tool were used to assess the quality of randomised controlled trials (RCTs) and non-RCTs, respectively.
Results
From the 52 included studies, 46 BCTs were identified and linked to 21 MoAs. Long-term facilitators for planning intervention included ‘self-monitoring of behaviour’, ‘problem solving’, ‘instruction on how to perform the behaviour’ and ‘adding objects to the environments’. The three most frequently occurring MoAs were ‘intention’, ‘behavioural regulation’, ‘beliefs about capabilities’. The effective intervention groups had higher MoA scores that corresponded to the HAPA model constructs than the ineffective groups.
Conclusions
The findings from this review may inform scientific and effective planning intervention designs for community-dwelling people with chronic conditions in the future.
PROSPERO registration number
CRD42021241227.
Keywords: PUBLIC HEALTH, HEALTH SERVICES ADMINISTRATION & MANAGEMENT, Health informatics
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This review covered both randomised controlled trials (RCTs) and non-RCT research focusing on individuals with a variety of chronic diseases, resulting in a comprehensive analysis.
Both health outcome and behavioural outcome were taken into account to determine the effectiveness of action planning intervention.
The health action process approach model was used to conceptualise the key mechanisms of action.
Coding of interventions did not concern the intensity of each behaviour change technique.
Fidelity assessment failed to capture the degree of each fidelity item due to the dichotomous approach.
Introduction
It is well known that poor eating habits and physical inactivity are two major risk factors for non-communicable chronic diseases (NCDs), such as cardiovascular disease, type 2 diabetes mellitus (T2DM) and obesity,1 and improvements in physical activity (PA) and diet behaviour (DB) can significantly benefit community-dwelling patients with NCDs.2–4 In this patient population, there is an urgent need for effective behavioural interventions supported by theory and evidence, as they have less pre-existing PA, a greater sense of helplessness, less social support and more perceived barriers.5
Complex behavioural interventions with multiple components are gaining traction as a promising and important public health approach for encouraging these people to develop healthy eating habits and actively participate in sports. Their explosion has resulted in a plethora of categorical frameworks for aggregating intervention components. The Behaviour Change Technique Taxonomy version 1 (BCTTv1) is one of the most complete and systematic frameworks. It consists of an ‘extensive, consensually agreed upon, hierarchically structured’ set of 93 techniques aimed at changing health behaviours.6 BCTTv1 is of great value in synthesising and analysing complex behavioural interventions.
One effective behaviour change technique (BCT) popularised in PA or DB improvement is ‘action planning’. It is defined as ‘prompt detailed planning of behaviour performance, including context, frequency, duration and intensity’.6 A plan that specifies situational cues and sufficient action detail, such as ‘I intend to go jogging in the park on Monday at 11:00’ qualifies as an action plan. Several meta-analyses have confirmed the effectiveness of planning in improving PA7–9 and DB,7 9–11 and they identified that reinforcement,12 barrier management8 and monitoring11 were significant moderators. However, it is likely that some potential moderators have not yet been identified due to the absence of a theoretical and comprehensive synthesis of planning intervention components from the perspective of BCTs.
Theoretically, planning has been incorporated as one of the theoretical constructs into the Health Action Process Approach (HAPA) model. The model indicates that the process of health behaviour change involves two phases: motivational and volitional. Self-efficacy, outcome expectancy and risk perception are considered critical to promote intention formation (eg, ‘I intended to do more exercise.’) in the motivational phase, and planning is regarded as the watershed in intention conversion to action in the volitional phase, with self-efficacy moderating the effect.13 However, the contradictory results of previous studies regarding the predictability of planning suggest that there may be unspecified mechanisms in the health behaviour change process.14–17 For example, self-regulation13 18 and social support16 19 are frequently included as volitional constructs, and past habits were found to impair the intention–action association.20 21
To improve the theoretical understanding of the planning intervention, intervention reverse coding was conducted to identify the mechanisms contributing to the planning effect. It is identifying mechanisms of action (MoAs, the theoretical approach through which behaviour change occurs) that link to the BCTs used in an intervention through the theory and technique tool.22 The tool is based on an expert consensus22 and literature review23 that summarises existing connections between BCT and MoA. A previous study applied it to determine the most frequently used MoAs in a PA intervention programme.24 However, there is no review research that synthesises MoAs that occurred in the planning of interventions, which would advance the theoretical understanding of intervention effectiveness. By deconstructing the planning interventions into BCT combinations and MoA scores, this review aimed to (1) summarise the characteristics of BCT distribution and critical BCTs in PA and DB planning interventions targeting community-dwelling patients; and (2) enhance comprehension of the theoretical mechanisms underlying the efficacy of planning interventions based on the HAPA model.
Method
Patient and public involvement
No patients were involved.
Search strategy and study selection
The review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines,25 with the checklist available in online supplemental file 1. The protocol was registered in the International Prospective Register of Systematic Reviews (CRD42021241227). Seven electronic databases were searched, including PubMed, Web of Science, CINAHL (EBSCO), PsycINFO (EBSCO), Psychology and Behavioural Sciences Collection (EBSCO), psyARTICLES and Medline, for English-language studies published from January 1990 to September 2021. Online supplemental file 2 contains detailed information about the search strategy. Furthermore, manual searching was carried out via Google Scholar and the reference lists from previous meta-analyses.8 10–12
bmjopen-2021-058229supp001.pdf (2.9MB, pdf)
bmjopen-2021-058229supp002.pdf (58.2KB, pdf)
Inclusion and exclusion criteria
This review included both randomised controlled trials (RCTs) and non-RCTs. The inclusion criteria were presented according to ‘PICO’. Participants were adults who lived in the community and had at least one chronic condition (Participation). They received PA and/or DB planning intervention. Specifically, they were asked to create detailed action plans specifying when, where, and how to do things or to use an ‘if–then’ form to create specific behavioural plans to improve PA or DB (Intervention). There should be no planning intervention in the control group (Comparison). Physiological or behavioural outcomes (as measured by self-report questionnaires or wearable devices) were considered (Outcome). The exclusion criteria were as follows: (1) participants' plans did not qualify as action or coping plans; and (2) the intervention provider (eg, nurses, healthcare professionals, etc), rather than patients, was the research object.
Study selection and data extraction
The title, abstract, and full text were reviewed independently and concurrently by HL and DX. Disagreements were discussed and resolved with the assistance of a third reviewer (ND). HL extracted the following data from each included study: sample size, participant health status, intervention target (either PA or DB, or both), intervention delivery, rehabilitation, key outcome indicator and measuring method, follow-up time, and statistical power of outcome difference between planning intervention group and control. In studies with multiple outcome indicators, the behavioural outcome (eg, pedometer) was selected first, followed by the physiological outcome and finally the self-reported outcome. In the case of DB, the physiological outcome came first, followed by the self-reported behavioural outcome.
Risk of bias and fidelity assessment
RCT study quality was assessed using the Cochrane risk of bias assessment tool,26 which included the following domains: (1) random sequence generation, (2) allocation bias, (3) performance bias related to participant and intervention provider blinding, (4) attrition bias due to missing data, (5) detection bias and (6) reporting bias. In the final three domains, non-RCTs were also evaluated. Additionally, they were assessed for risk of baseline confounding due to one or more prognostic variables that predicted the intervention effect, selection bias due to participant inclusion/exclusion based on their characteristics and performance bias due to deviation from intended interventions using the Risk of Bias in Nonrandomized Studies–of Interventions assessment tools.27 Each item’s risk level was classified as ‘low risk’, ‘high risk’ or ‘uncertain’. Fidelity was assessed using modified Bellg et al28 criteria and a dichotomised assessment in terms of study design, provider training, treatment delivery and treatment receipt. Cohen’s kappa was used to assess inter-rater agreement in risk of bias and fidelity assessments.
Intervention coding and reverse coding
Two reviewers (HL and DX) completed the tutorial (http://www.bct-taxonomy.com, accessed on 23 January 2021) to qualify them of capacity for BCT coding. In addition, prior to formal coding, DX and HL independently coded 5% of the studies to ensure consistency. Inter-rater agreement in coding was determined by Cohen’s kappa value. Two coders were retrained and coded again if the kappa value was less than 80%. The remaining differences were resolved through discussion with a third reviewer (ND).
The coding result was vectorised, with ‘1’ indicating the presence of the BCT and ‘0’ indicating its absence. Inactive or undefined control groups were not coded. Following coding, the BCTs were mapped to MoAs using the theory and technique tool (an online interactive heatmap matrix retrieved on 23 January 2021, from https://theoryandtechniquetool.humanbehaviourchange.org/tool). Each MoA score was determined by the number of BCTs associated with that MoA, indicating the variety of BCTs used to modify behaviour according to this theoretical mechanism. This process was repeated for each intervention group, resulting in a matrix of MoA scores, with the row representing the score of a certain MoA for all groups and the column representing the scores of all MoAs within a certain group.
Intervention effectiveness coding
Because the outcome measurement and follow-up time were highly inconsistent, it was anticipated that quantitative estimation of planning intervention effectiveness would have low evidence power and a low reference value. Hence, intervention effectiveness was classified as ‘effective’, ‘ineffective’ or ‘inconclusive’ based on the effect size (ES) and statistical significance of the key indicator. Cohen’s d was used to calculate the magnitude of the ES by dividing the mean difference between the intervention and control groups by the SD.29 The rules for coding intervention effectiveness were as follows: if statistical power was significant (p>0.05), the ES of an ‘effective’ intervention should at least reach a small level (d>0.2) for physiological measurement or device-based measurements, or a medium level (d>0.5) for self-reported indicators, or it was coded as ‘ineffective’. If there was no information on the statistical power or ES, it was classified as ‘inconclusive’.
Data synthesis
Only the planning intervention groups from the included studies were included in the analysis. The occurrence rate of each BCT was calculated by dividing the number of groups that used this BCT by the total number of groups and was classified based on target behaviour, health condition and mode of delivery. The success rate of each BCT was calculated by dividing the number of effective groups that used this BCT by the total number of groups that used this BCT and was classified as long-term (ie, the follow-up period was longer than 3 months) and short-term (ie, the follow-up period was not longer than 3 months). Notably, only BCTs involved in more than 10% of studies were included in subsequent analyses.
The MoA scores for all planning intervention groups were displayed using the R software (V.3.6.1) heatmap drawing tool.30 MoA with an average score greater than 1 indicates that, on average, at least one specific BCT was used to improve health behaviour change via this mechanism. These MoAs were further conceptualised with the HAPA model. Descriptive analyses were then performed on the difference in MoA score between effective intervention groups and ineffective intervention groups for PA and DB outcomes.
Results
Study selection and study characteristics
A total of 52 studies were included in the analysis (figure 1). As shown in table 1, there were 45 RCTs31–75 and 7 quasi-experiments.76–82 Thirty-nine studies included PA planning interventions, and 37 included DB planning interventions. Ten trials included a rehabilitation period prior to action planning, eight of which occurred outside the hospital.41 47 50 51 56 58 62 78 Thirty-seven per cent of the studies targeted obese patients without metabolic syndrome (MS). The majority of studies administered the intervention via face-to-face sessions that were either individual based (58%) or individual and group based (29%). Nine studies provided merely online sessions.31 36 38 41 48 64 65 70 78 Three studies incorporated both individual sessions and online sessions based on computers37 68 or smartphone applications.72
Figure 1.
PRISMA flow diagram. From Moher et al.25 PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1.
Study characteristics
| Author | Published year | Study type | Intervention target | Health status | Intervention delivery | Rehabilitation |
| Almeida et al31 | 2015 | RCT | PA & DB | CVD | Computer session | None |
| Armitage et al32 | 2014 | RCT | DB | OB | Individual session | None |
| Armitage et al33 | 2017 | RCT | DB | OB | Individual session | None |
| Ayre et al34 | 2020 | RCT | DB | OB, DM | Individual session | None |
| Bélanger-Gravel et al35 | 2013 | RCT | PA | OB | Individual session | None |
| Breslin et al36 | 2019 | RCT | PA & DB | OB | Group session plus individual session | None |
| Broekhuizen et al37 | 2012 | RCT | PA & DB | FH | Computer session plus individual session | None |
| Cheung et al38 | 2017 | RCT | PA & DB | OB | Computer session | None |
| Christiansen et al39 | 2010 | RCT | PA | CBP | Individual session | None |
| de Freitas Agondi et al40 | 2014 | RCT | DB | HP | Individual session | None |
| Duan et al41 | 2018 | RCT | PA & DB | CVD | Computer session | Out-of-hospital |
| Gagnon-Girouard et al42 | 2010 | RCT | DB | OB with depression or eating disorder | Group session plus individual session | None |
| Groeneveld et al43 | 2011 | RCT | PA & DB | CVD | Individual session | None |
| Hayes et al44 | 2020 | RCT | DB | OB | Individual session | None |
| Igelström et al45 | 2014 | RCT | PA & DB | OB, OSAS | Individual session | None |
| Jackson et al46 | 2005 | RCT | DB | CVD | Individual session | None |
| Janssen et al47 | 2014 | RCT | PA & DB | CVD | Group session plus individual session | Out-of-hospital |
| Kim and Utz48 | 2019 | RCT | PA & DB | DM | Smartphone application | None |
| Kwasnicka et al49 | 2020 | RCT | PA &DB | OB | Group session plus individual session | None |
| Luszczynska50 | 2006 | RCT | PA | Post-MI | Individual session | Out-of-hospital |
| Luszczynska et al51 | 2007 | RCT | DB | Post-MI | Individual session | Out-of-hospital |
| Luszczynska et al52 | 2007 | RCT | PA & DB | OB | Individual session | None |
| Miller et al53 | 2016 | RCT | PA & DB | DB | Group session plus individual session | None |
| Obara-Golebiowska and Brycz54 | 2015 | RCT | DB | OB | Group session plus individual session | None |
| Osborn et al55 | 2018 | RCT | PA & DB | SMI | Individual session | None |
| Rodgers et al56 | 2014 | RCT | PA | CLD | Individual session | Out-of-hospital |
| Rodrigues et al57 | 2013 | RCT | PA | CVD | Individual session | None |
| Scholz et al58 | 2007 | RCT | PA | CVD | Individual session | Out-of-hospital |
| Scholz et al59 | 2013 | RCT | DB | OB | Individual session | None |
| Silva et al60 | 2020 | RCT | PA | DM | Individual session | None |
| Sniehotta et al61 | 2005 | RCT | PA | CVD | Individual session | Hospital |
| Sniehotta et al62 | 2006 | RCT | PA | CVD | Individual session | Out-of-hospital |
| Sniehotta et al63 | 2011 | RCT | PA & DB | NCD | Individual session | None |
| Soureti et al64 | 2011 a | RCT | DB | OB | Computer session | None |
| Soureti et al65 | 2011b | RCT | DB | OB | Computer session | None |
| Stevens et al66 | 2001 | RCT | PA & DB | OB | Individual session | None |
| Ströbl et al67 | 2013 | RCT | PA & DB | NCD | Group session plus individual session | Hospital |
| Svetkey et al68 | 2008 | RCT | PA & DB | OB, HP, DLP | Computer session or individual session | None |
| Thoolen et al69 | 2009 | RCT | PA & DB | DM | Individual session | None |
| van Genugten et al70 | 2014 | RCT | PA & DB | OB | Computer session | None |
| Vinkers et al71 | 2014 | RCT | PA & DB | OB | Group session plus individual session | None |
| Wilczynska et al72 | 2019 | RCT | PA | OB, DM | Smartphone application plus individual session | None |
| Wooldridge et al73 | 2019 | RCT | PA | DM | Group session plus individual session | None |
| Zakrisson et al74 | 2019 | RCT | PA | COPD, CHF | Group session plus individual session | None |
| Zandstra et al75 | 2010 | RCT | DB | OB | Individual session | None |
| Dombrowski et al76 | 2016 | QE | PA & DB | OB | Individual session | None |
| Boekhout et al77 | 2018 | QE | PA | NCD | Computer session | None |
| Fleig et al78 | 2011 | QE | PA & DB | CVD | Computer session | Out-of-hospital |
| Göhner et al79 | 2012 | QE | PA & DB | OB | Group session plus individual session | None |
| Kivelä et al80 | 2020 | QE | PA & DB | NCD | Individual session | None |
| Leung et al81 | 2019 | QE | PA | DM, HP | Group session plus individual session | None |
| Richardson et al82 | 2012 | QE | PA | NCD | Group session plus individual session | None |
CBP, chronic back pain; CHF, chronic heart failure; CLD, chronic lung disease; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; DB, diet behaviour; DLP, dyslipidaemia; DM, diabetes mellitus; FH, familial hypercholesterolemia; HP, hypertension; NCD, non-communicable chronic disease; OB, obesity; OSAS, obstructive sleep apnoea syndrome; PA, physical activity; post-MI, post-myocardial infarction; QE, quasi-experiment; RCT, randomised controlled trial; SMI, severe mental illness.
Risk of bias and fidelity assessment
A substantial proportion of studies were evaluated with a high/unclear risk of performance bias (58%) and reporting bias (58%). Attrition bias and detection bias were high for 33% and 58% of the included studies, respectively. Seven RCTs were assessed with insufficient random sequence generation, and 18 showed insufficient concealment of allocations. Five non-RCTs had a high risk of baseline confounding, and three had significant selection bias. Only five trials were evaluated as having low risk in every domain.56 64 65
According to the fidelity assessment, 81% of studies had descriptions of standardised procedures for planning intervention, and 67% provided supplementary resources to aid participants in developing action plans. Less than half (44%) measured participants’ action plans. The quality of action plans was guaranteed in 54% of trials. Only 10 (19%) studies described planning intervention provider training. Online supplemental files 3 and 4 contain detailed information on the risk of bias and fidelity assessment within individual studies. The kappa values for risk of bias and fidelity were 0.87 and 0.95, respectively.
bmjopen-2021-058229supp003.pdf (63.6KB, pdf)
bmjopen-2021-058229supp004.pdf (66.1KB, pdf)
BCT coding
To improve coding consistency, a systematic review of 20 rehabilitation studies83 was used to summarise the common BCTs used in rehabilitation studies. The coding consistency kappa was 0.89. A total of 46 BCTs were identified from 52 studies (see online supplemental files 5 and 6 for details). In addition to action planning, the BCTs occurring in more than 10% of all groups and their occurrence rates were: (1) information about health consequences (78%); (2) behavioural goal setting (71%); (3) unspecified social support (69%); (4) problem solving (68%); (5) adding objects to the environment (56%); (6) instruction on how to perform the behaviour (53%); (7) self-monitoring of behaviour (52%); (8) feedback on behaviour (40%); (9) practical social support (37%); (10) self-monitoring of outcomes of behaviour (32%); (11) reduce negative emotions (31%); (12) pharmacological support (28%); (13) credible source (28%); (14) prompt/cues (28%); etc. These BCTs were referred to by serial numbers for ease of reference, for example, ‘(2)’ refers to ‘behavioural goal setting’ below.
bmjopen-2021-058229supp005.pdf (177.7KB, pdf)
bmjopen-2021-058229supp006.pdf (59.6KB, pdf)
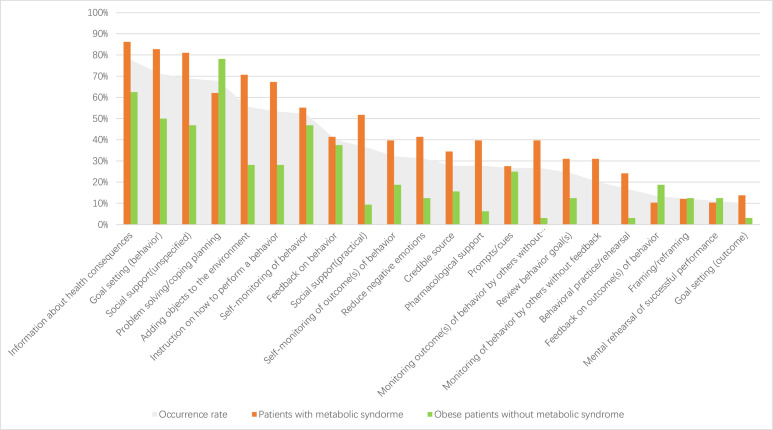
The planning interventions for patients with MS included an average of 12 BCTs, which was higher than the number of BCTs used in groups for obese patients without MS (7 BCTs on average, see figure 2). The top eight BCTs in terms of occurrence in patients with MS were (1), (2), (3), (5), (6), (4), (7) and (9). In terms of the occurrence in obese patients without MS, the top eight most popular BCTs in order were (4), (1), (2), (3), (7), (8), (5) and (6). ‘Practical social support’ was merely popular in patients with MS (52%), while ‘feedback on behaviour’ was only popular in obese patients without MS (38%).
Figure 2.
Distribution of BCTs for different health conditions. BCTs, behaviour change techniques.
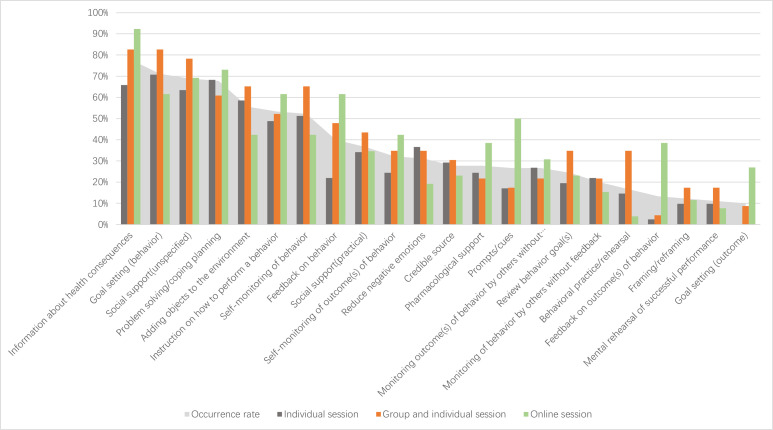
Individual session intervention, group plus individual session intervention, and online session intervention all identified averages of 9, 12, and 11 BCTs, respectively. As shown in figure 3, the top eight popular BCTs in group plus individual session interventions were (1), (2), (3), (5), (7), (4), (6) and (8) in order. The top eight common BCTs in individual session interventions were (2), (4), (1), (3), (5), (7), (6) and (11) in order. The top eight popular BCTs in order were (1), (4), (3), (2), (6), (8), (14) and (5). ‘Reduce negative emotions’ was simply common in individual session interventions (37%), and ‘prompts/cues’ was uniquely popular in online session interventions (50%).
Figure 3.
Distribution of BCTs for different intervention deliveries. BCTs, behaviour change techniques.
Intervention effectiveness coding
In summary, 47 groups contained PA planning interventions, of which 42 were available for effectiveness coding, while 43 groups contained DB planning interventions. Among the 46 BCTs identified, 24 occurred in more than 10% of the PA groups, and 21 occurred in more than 10% of the DB groups. The PA intervention group had an average of 11 BCTs, whereas the DB intervention group had an average of 8 BCTs. Janssen et al47 designed an intervention involving the maximum number of BCTs (N=25).
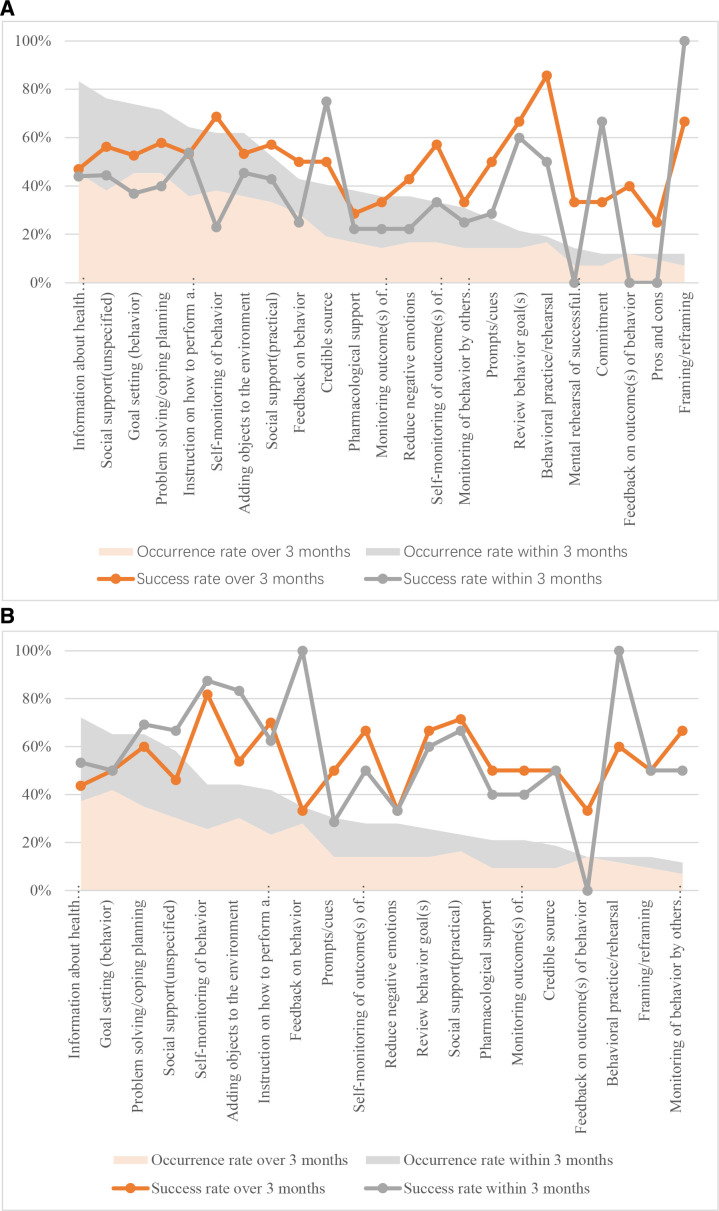
As shown in figure 4A, the top eight popular BCTs in the PA intervention groups were (1), (3), (2), (4), (6), (7), (5) and (9) in order. Except for (1), all popular BCTs had a success rate of more than 50% for long-term PA outcomes. However, only (4) and (5) had success rates above 50% for short-term PA outcomes. For the DB intervention groups, the top eight popular BCTs were (1), (2), (4), (3), (5), (7), (6) and (8). All of them had a success rate above 50% for short-term DB outcomes. However, only (4), (7), (6) and (5) had success rates above 50% for long-term DB outcomes. Overall, ‘self-monitoring of behaviour’, ‘problem solving’, ‘instruction on how to perform the behaviour’ and ‘adding objects to the environment’ were BCTs that were favoured by the planning interventions for both PA and DB long-term improvements.
Figure 4.
Occurrence and success rates of BCT in (A) physical activity and (B) diet behaviour planning intervention. BCTs, behaviour change techniques.
Mapping BCT to MoA
BCTs in the planning intervention groups corresponded to 21 MoAs, 11 of which scored higher than 1. In addition to ‘behavioural cueing’ (which corresponded to action planning), the top three MoAs in terms of occurrence were ‘intention’ (89%), ‘behavioural regulation’ (88%) and ‘beliefs about capabilities’ (87%). ‘Behavioural regulation’ was the highest scoring MoA, which was associated with an average of 1.6 BCTs. ‘Beliefs about capabilities’, ‘knowledge’ and ‘intention’ tied for second place, each with an average of 1.5 BCTs. A PA planning intervention involved an average of 8 MoAs, while a DB planning intervention involved an average of 11 MoAs. However, all MoAs in the PA planning interventions scored higher than those in the DB planning interventions.
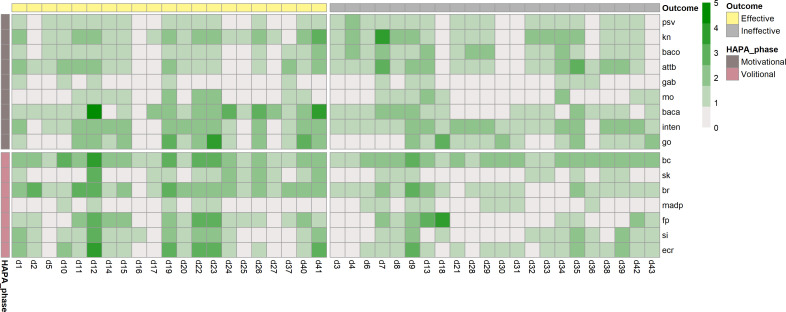
The results are displayed as heatmaps presenting the distribution of MoA scores (see figures 5 and 6). Table 2 displays the conceptualisation of the 11 MoAs that scored greater than 1 according to the HAPA model (columns 1 and 2), as well as their average scores for effective and ineffective planning interventions, distinguished by PA and DB outcomes (columns 4-7). Both effective and ineffective interventions covered both phases and all of the HAPA model’s constructs. In the motivational phase, however, effective interventions exhibited higher scores in MoAs corresponding to self-efficacy (ie, ‘beliefs about capabilities’) and intention (ie, ‘goals’) than ineffective interventions. In the volitional phase, all effective intervention MoAs scored higher than ineffective intervention MoAs.
Figure 5.
MoA score heatmap of physical activity planning intervention. HAPA, Health Action Process Approach; MoA, mechanism of action; psv, perceived susceptibility/vulnerability; kn, knowledge; baco, beliefs about concequences; attb, attitudes towards the behaviour; gab, general attitudes/beliefs; mo, motivations; baca, beliefs about capabilities; inten, intention; go, goals; bc, behaviour cueing; sk, skill; bc, behavioural regulation; madp, memory, attention and decision processes; fp, feedback processes; si, social influences; ecr, environmental context and resources.
Figure 6.
MoA score heatmap of diet behaviour planning intervention. HAPA, Health Action Process Approach; MoA, mechanism of action; psv, perceived susceptibility/vulnerability; kn, knowledge; baco, beliefs about concequences; attb, attitudes towards the behaviour; gab, general attitudes/beliefs; mo, motivations; baca, beliefs about capabilities; inten, intention; go, goals; bc, behaviour cueing; sk, skill; bc, behavioural regulation; madp, memory, attention and decision processes; fp, feedback processes; si, social influences; ecr, environmental context and resources.
Table 2.
Average mechanism of action scores for effective or ineffective planning intervention groups
| HAPA framework | Mechanism of action | Mechanism of action score | ||||
| Physical activity | Diet behaviour | |||||
| Motivation phase (goal setting) | Volitional phase (goal pursuit) | Effective (n=21) | Ineffective (n=21) | Effective (n=21) | Ineffective (n=22) | |
| Risk perception | Knowledge | 1.6 | 1.7 | 1.3 | 1.2 | |
| Outcome expectation | Beliefs about consequences | 1.0 | 1.0 | 0.8 | 1.0 | |
| Attitude towards the behaviour | 1.4 | 1.6 | 1.1 | 1.2 | ||
| Self-efficacy | Beliefs about capabilities | 1.9 | 1.5 | 1.7 | 0.9 | |
| Intention | Intention | 1.7 | 1.6 | 1.3 | 1.4 | |
| Goals | 1.4 | 1.2 | 1.3 | 0.9 | ||
| Planning | Behavioural cueing | 2.1 | 1.9 | 2.0 | 1.8 | |
| Action control | Behavioural regulation | 2.0 | 1.5 | 1.8 | 1.0 | |
| Self-efficacy | Feedback processes | 1.5 | 1.1 | 1.3 | 0.8 | |
| External support | Environmental context & resources | 1.7 | 1.4 | 1.3 | 1.0 | |
| Social influence | 1.4 | 1.3 | 1.0 | 0.7 | ||
HAPA, Health Action Process Approach.
Discussion
This study synthesised the BCT distributions and theoretical mechanisms in PA and/or DB planning interventions for community residents with chronic conditions. Overall, a total of 46 BCTs were identified from 52 included studies. There were 47 PA intervention groups and 43 DB intervention groups. ‘Self-monitoring of behaviour’, ’problem solving’, ‘instruction on how to perform the behaviour’ and ‘adding objects to the environment’ were identified as critical BCTs. ‘Behavioural regulation’, ‘beliefs about capabilities’ and ‘intention’ were considered key MoAs. The following sections will elaborate on the results from the perspective of BCT distribution, intervention effectiveness and MoA.
Features of BCT distribution in planning intervention
We found that a planning intervention contains an average of eight BCTs in addition to action planning. This number is greater for PA planning interventions compared with DB planning interventions, for patients with MS versus obese patients without MS, and for group and individual session interventions compared with other delivery modes.
The top eight most popular BCTs in general were information about health consequences, behavioural goal setting, unspecified social support, problem solving, adding objects to the environment, instruction on how to perform the behaviour, self-monitoring of behaviour and feedback on behaviour. However, differences were detected in the most popular BCTs for different target behaviours, disease populations and delivery modes. ‘Practical social support’ was only popular in PA planning interventions and interventions for patients with MS, and it was also identified as one of the key BCTs in previous reviews that synthesised the critical BCTs in PA interventions.84–86 ‘Feedback on behaviour’ was simply common in DB planning interventions and interventions aimed at obese patients without MS. Consistently, Cradock et al regarded it as one of the critical BCTs in DB interventions for patients with T2DM.87 In addition, we found that face-to-face sessions frequently use ‘reduce negative emotions’, and online sessions often use ‘prompts/cues’. The latter was also detected in a past review targeting mobile health application users. However, several previously identified BCTs failed to be captured in this review, for example, demonstration of behaviour,7 85 social comparison,87 information about others’ approval,85 credible source,84 etc. This may be due to different interventions and populations of interest. However, it is insufficient to merely know what BCTs are popular because they are not always the most effective ones.
Considering intervention effectiveness, ‘self-monitoring of behaviour’, ‘problem solving’, ‘instruction on how to perform the behaviour’ and ‘adding objects to the environment’ are long-term universal facilitators for planning intervention. ‘Goal setting (behaviour)’, ‘social support (unspecified)’ and ‘social support (practical)’ are specific facilitators of PA planning. This is the first review to identify the critical BCTs based on the popularity and intervention’s efficacy by target behaviour and follow-up period, thereby enhancing the practical and reference value. Nevertheless, it is essential to comprehend the underlying mechanisms to design an effective planning intervention with a credible theoretical foundation.
Interpretation of MoAs in planning intervention based on the HAPA model
The BCTs identified through planning interventions were primarily associated with 11 MoAs. They were conceptualised based on the HAPA model. We discovered that PA planning interventions are more diverse in BCT selection but less complex in potential theoretical mechanisms than DB planning interventions. The three mechanisms with the highest scores were ‘intention’, ‘behavioural regulation’ and ‘beliefs about capabilities’, which were also the three most prevalent. This indicates that they are the most frequently considered factors when designing PA or DB interventions for community-dwelling patients. A prior study also found that ‘beliefs about capabilities’ was the most frequently targeted theoretical domain in a PA intervention programme for patients with diabetes.24 Furthermore, effective intervention groups had higher MoA scores for action self-efficacy, maintenance self-efficacy and all other volitional constructs, which appear to be able to account for intervention effectiveness. This finding is also consistent with the connotation of the HAPA model. Schwarzer proposed that the integrity and interpretability of the HAPA model with regard to varying situations of behaviour change remain to be perfected.88 The findings of this review would be useful for enhancing the theoretical understanding and development of HAPA research, as well as for planning interventions to improve PA and DB in community-dwelling patients with chronic conditions.
Strengths and limitations
To the best of our knowledge, this is the first review identifying BCTs and MoAs in planning interventions aimed at improving PA and DB for community-dwelling patients with chronic conditions. The summary of the characteristics of BCTs in terms of various target behaviours, chronic conditions and intervention deliveries has practical significance. The conceptualisation of identified MoAs according to the HAPA model further improves the theoretical understanding of the intervention of interest.
Several limitations exist in this review. First, the MoA score was unable to reflect the actual impact of the interventions, and data on social cognitive indicators were not collected. Second, population and language restrictions in the inclusion criteria limit the generalisability of the findings. Third, the validity of intergroup comparisons of intervention components was compromised by the fact that the coding of intervention content only accounted for the variety, but not the intensity, of each BCT. Fourth, the inclusion of non-RCT studies and dichotomous coding of intervention effectiveness diminished the evidence power. Fifth, both the overall quality of the included studies and fidelity of the planning interventions were inadequate. Due to the dichotomous approach, the fidelity assessment failed to capture the degree of each fidelity item.
Implications for future research
To design an effective PA or DB planning intervention, intervention designers should apply the prevalent BCTs identified with long-term effects in this review and consider the target population and intervention delivery. In addition, we also encourage future intervention studies on phase-based planning interventions, structuring as BCTs, and elaborating processes in a structured form (eg, intensity, frequency and delivery), as well as measuring implementation fidelity. When analysing complex behavioural interventions in the future, it is advised that implementation factors be considered. In addition, it was suggested that data be collected on social cognitive indicators to determine the actual impact of BCTs on them.
Conclusions
In conclusion, the prevalent BCTs for planning interventions vary by target behaviour, chronic condition and intervention delivery. However, the most widely used BCTs are not always the most effective. To increase the success rate of exercise or diet planning interventions, it is best to employ BCTs that promote self-efficacy and volitional constructs of the HAPA model. The findings of this review may serve as an important reference for future research aimed at developing a rational and effective PA or DB intervention for individuals living in the community with chronic conditions.
Supplementary Material
Footnotes
Contributors: HL, MY, XM, NY and ND have made contributions to conceptualisation. HL and DX independently conducted the screening of literature, data extraction, intervention coding and quality assessment. HL completed the data analyses, visualisation and interpretation. MY, SH and ND made contributions to funding acquisition and supervision. Original draft was completed by HL, and was reviewed and approved by MY, XM, NY, HC, SH and ND. And HL was the guarantor of this work.
Funding: This study was supported by the Key Research and Development Program of Ningxia Hui Autonomous of China (No. 2020BFG02002), the National Key Research and Development Program of China (No. 2020YFC2003403, 2020YFC2006405), and the Major Science and Technology Project in Hainan Province of China (No. ZDKJ2019012).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information. Data are available in a public, open access repository. Extra data can be accessed via the Dryad data repository at http://datadryad.org/ with the doi: 10.5061/dryad.m905qfv48
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Not applicable.
References
- 1.World Health Organization . Global status report on noncommunicable diseases 2014. Geneva, Switzerland: WHO, 2014. http://www.who.int/nmh/publications/ncd-status-report-2014/en/ [Google Scholar]
- 2.Ramezani-Jolfaie N, Mohammadi M, Salehi-Abargouei A. The effect of healthy Nordic diet on cardio-metabolic markers: a systematic review and meta-analysis of randomized controlled clinical trials. Eur J Nutr 2019;58:2159–74. 10.1007/s00394-018-1804-0 [DOI] [PubMed] [Google Scholar]
- 3.Chen L, Pei J-H, Kuang J, et al. Effect of lifestyle intervention in patients with type 2 diabetes: a meta-analysis. Metabolism 2015;64:338–47. 10.1016/j.metabol.2014.10.018 [DOI] [PubMed] [Google Scholar]
- 4.Lin X, Zhang X, Guo J, et al. Effects of exercise training on cardiorespiratory fitness and biomarkers of cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc 2015;4:e002014. 10.1161/JAHA.115.002014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jack K, McLean SM, Moffett JK, et al. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther 2010;15:220–8. 10.1016/j.math.2009.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (V1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- 7.Cradock KA, ÓLaighin G, Finucane FM, et al. Behaviour change techniques targeting both diet and physical activity in type 2 diabetes: a systematic review and meta-analysis. Int J Behav Nutr Phys Act 2017;14:1–17. 10.1186/s12966-016-0436-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bélanger-Gravel A, Godin G, Amireault S. A meta-analytic review of the effect of implementation intentions on physical activity. Health Psychol Rev 2013;7:23–54. 10.1080/17437199.2011.560095 [DOI] [PubMed] [Google Scholar]
- 9.Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta‐analysis of effects and processes. Adv Exp Soc Psychol 2006;38:69–119. 10.1016/S0065-2601(06)38002-1 [DOI] [Google Scholar]
- 10.Adriaanse MA, Vinkers CDW, De Ridder DTD, et al. Do implementation intentions help to eat a healthy diet? A systematic review and meta-analysis of the empirical evidence. Appetite 2011;56:183–93. 10.1016/j.appet.2010.10.012 [DOI] [PubMed] [Google Scholar]
- 11.Vilà I, Carrero I, Redondo R. Reducing fat intake using implementation intentions: a meta-analytic review. Br J Health Psychol 2017;22:281–94. 10.1111/bjhp.12230 [DOI] [PubMed] [Google Scholar]
- 12.Silva MAVda, São-João TM, Brizon VC, et al. Impact of implementation intentions on physical activity practice in adults: a systematic review and meta-analysis of randomized clinical trials. PLoS One 2018;13:e0206294. 10.1371/journal.pone.0206294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol 2008;57:1–29. 10.1111/j.1464-0597.2007.00325.x [DOI] [Google Scholar]
- 14.Barg CJ, Latimer AE, Pomery EA, et al. Examining predictors of physical activity among inactive middle-aged women: an application of the health action process approach. Psychol Health 2012;27:829–45. 10.1080/08870446.2011.609595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gutiérrez-Doña B, Lippke S, Renner B, et al. Self-efficacy and planning predict dietary behaviors in Costa Rican and South Korean women: two moderated mediation analyses. Appl Psychol 2009;1:91–104. 10.1111/j.1758-0854.2008.01001.x [DOI] [Google Scholar]
- 16.Parschau L, Barz M, Richert J, et al. Physical activity among adults with obesity: testing the health action process approach. Rehabil Psychol 2014;59:42–9. 10.1037/a0035290 [DOI] [PubMed] [Google Scholar]
- 17.Caudroit J, Stephan Y, Le Scanff C. Social cognitive determinants of physical activity among retired older individuals: an application of the health action process approach. Br J Health Psychol 2011;16:404–17. 10.1348/135910710X518324 [DOI] [PubMed] [Google Scholar]
- 18.Gholami M. Self-Regulation and Health Behavior Across the Life Span [PhD]. In: Erziehungswissenschaft und Psychologie, 2014. [Google Scholar]
- 19.Teleki S, Zsidó AN, Lénárd L, et al. Role of received social support in the physical activity of coronary heart patients: the health action process approach. Appl Psychol Health Well Being 2022;14:44–63. 10.1111/aphw.12290 [DOI] [PubMed] [Google Scholar]
- 20.Hagger MS, Polet J, Lintunen T. The reasoned action approach applied to health behavior: role of past behavior and tests of some key moderators using meta-analytic structural equation modeling. Soc Sci Med 2018;213:85–94. 10.1016/j.socscimed.2018.07.038 [DOI] [PubMed] [Google Scholar]
- 21.Zhang C-Q, Zhang R, Schwarzer R, et al. A meta-analysis of the health action process approach. Health Psychol 2019;38:623–37. 10.1037/hea0000728 [DOI] [PubMed] [Google Scholar]
- 22.Connell LE, Carey RN, de Bruin M, et al. Links between behavior change techniques and mechanisms of action: an expert consensus study. Ann Behav Med 2019;53:708–20. 10.1093/abm/kay082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carey RN, Connell LE, Johnston M, et al. Behavior change techniques and their mechanisms of action: a synthesis of links described in published intervention literature. Ann Behav Med 2019;53:693–707. 10.1093/abm/kay078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bourne JE, Ivanova E, Gainforth HL, et al. Mapping behavior change techniques to characterize a social cognitive theory informed physical activity intervention for adults at risk of type 2 diabetes mellitus. Transl Behav Med 2020;10:705–15. 10.1093/tbm/ibz008 [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 26.Higgins J, Thomas J, Chandler J. Cochrane handbook for systematic reviews of interventions [Internet. 2nd ed. Chichester UK: The Cochrane Collaboration, 2019. [Google Scholar]
- 27.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bellg AJ, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH behavior change Consortium. Health Psychol 2004;23:443–51. 10.1037/0278-6133.23.5.443 [DOI] [PubMed] [Google Scholar]
- 29.Cohen J. Statistical power analysis for the behavioral sciences. New York: Academic Press, 1977. [Google Scholar]
- 30.R: a language and environment for statistical. Vienna, Austria: R Foundation for Statistical Computing; 2021. [Google Scholar]
- 31.Almeida FA, Smith-Ray RL, Dzewaltowski DA, et al. An interactive computer session to initiate physical activity in sedentary cardiac patients: randomized controlled trial. J Med Internet Res 2015;17:e206. 10.2196/jmir.3759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Armitage CJ, Norman P, Noor M, et al. Evidence that a very brief psychological intervention boosts weight loss in a weight loss program. Behav Ther 2014;45:700–7. 10.1016/j.beth.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 33.Armitage CJ, Alganem S, Norman P. Randomized controlled trial of a volitional help sheet to encourage weight loss in the middle East. Prev Sci 2017;18:976–83. 10.1007/s11121-017-0807-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ayre J, Cvejic E, Bonner C, et al. Effects of health literacy, screening, and participant choice on action plans for reducing unhealthy snacking in Australia: a randomised controlled trial. PLoS Med 2020;17:e1003409. 10.1371/journal.pmed.1003409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bélanger-Gravel A, Godin G, Bilodeau A, et al. The effect of implementation intentions on physical activity among obese older adults: a randomised control study. Psychol Health 2013;28:217–33. 10.1080/08870446.2012.723711 [DOI] [PubMed] [Google Scholar]
- 36.Breslin G, Sweeney L, Shannon S, et al. The effect of an augmented commercial weight loss program on increasing physical activity and reducing psychological distress in women with overweight or obesity: a randomised controlled trial. J Public Ment Health 2019;19:145–57. 10.1108/JPMH-08-2018-0055 [DOI] [Google Scholar]
- 37.Broekhuizen K, van Poppel MNM, Koppes LL, et al. No significant improvement of cardiovascular disease risk indicators by a lifestyle intervention in people with familial hypercholesterolemia compared to usual care: results of a randomised controlled trial. BMC Res Notes 2012;5:181. 10.1186/1756-0500-5-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheung KL, Schwabe I, Walthouwer MJL, et al. Effectiveness of a video-versus text-based computer-tailored intervention for obesity prevention after one year: a randomized controlled trial. Int J Environ Res Public Health 2017;14. 10.3390/ijerph14101275. [Epub ahead of print: 23 10 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Christiansen S, Oettingen G, Dahme B, et al. A short goal-pursuit intervention to improve physical capacity: a randomized clinical trial in chronic back pain patients. Pain 2010;149:444–52. 10.1016/j.pain.2009.12.015 [DOI] [PubMed] [Google Scholar]
- 40.de Freitas Agondi R, Cornélio ME, Rodrigues RCM, et al. Implementation intentions on the effect of salt intake among hypertensive women: a pilot study. Nurs Res Pract 2014;2014:196410. 10.1155/2014/196410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Duan YP, Liang W, Guo L, et al. Evaluation of a web-based intervention for multiple health behavior changes in patients with coronary heart disease in home-based rehabilitation: pilot randomized controlled trial. J Med Internet Res 2018;20:e12052–e. 10.2196/12052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gagnon-Girouard M-P, Bégin C, Provencher V, et al. Psychological impact of a "Health-at-Every-Size" intervention on weight-preoccupied overweight/obese women. J Obes 2010;2010:928097. 10.1155/2010/928097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Groeneveld IF, Proper KI, van der Beek AJ, et al. Short and long term effects of a lifestyle intervention for construction workers at risk for cardiovascular disease: a randomized controlled trial. BMC Public Health 2011;11:1–9. 10.1186/1471-2458-11-836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hayes JF, Balantekin KN, Graham AK, et al. Implementation intentions for weight loss in college students with overweight and obesity: a proof-of-concept randomized controlled trial. Transl Behav Med 2021;11:359–68. 10.1093/tbm/ibaa038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Igelström H, Helena I, Emtner M, et al. Tailored behavioral medicine intervention for enhanced physical activity and healthy eating in patients with obstructive sleep apnea syndrome and overweight. Sleep Breath 2014;18:655–68. 10.1007/s11325-013-0929-x [DOI] [PubMed] [Google Scholar]
- 46.Jackson C, Lawton R, Knapp P, et al. Beyond intention: do specific plans increase health behaviours in patients in primary care? A study of fruit and vegetable consumption. Soc Sci Med 2005;60:2383–91. 10.1016/j.socscimed.2004.10.014 [DOI] [PubMed] [Google Scholar]
- 47.Janssen V, De Gucht V, van Exel H, et al. A self-regulation lifestyle program for post-cardiac rehabilitation patients has long-term effects on exercise adherence. J Behav Med 2014;37:308–21. 10.1007/s10865-012-9489-y [DOI] [PubMed] [Google Scholar]
- 48.Kim SH, Utz S. Effectiveness of a social media-based, health literacy-sensitive diabetes self-management intervention: a randomized controlled trial. J Nurs Scholarsh 2019;51:661–9. 10.1111/jnu.12521 [DOI] [PubMed] [Google Scholar]
- 49.Kwasnicka D, Ntoumanis N, Hunt K, et al. A gender-sensitised weight-loss and healthy living program for men with overweight and obesity in Australian football League settings (Aussie-FIT): a pilot randomised controlled trial. PLoS Med 2020;17:e1003136. 10.1371/journal.pmed.1003136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Luszczynska A. An implementation intentions intervention, the use of a planning strategy, and physical activity after myocardial infarction. Soc Sci Med 2006;62:900–8. 10.1016/j.socscimed.2005.06.043 [DOI] [PubMed] [Google Scholar]
- 51.Luszczynska A, Scholz U, Sutton S. Planning to change diet: a controlled trial of an implementation intentions training intervention to reduce saturated fat intake among patients after myocardial infarction. J Psychosom Res 2007;63:491–7. 10.1016/j.jpsychores.2007.06.014 [DOI] [PubMed] [Google Scholar]
- 52.Luszczynska A, Sobczyk A, Abraham C. Planning to lose weight: randomized controlled trial of an implementation intention prompt to enhance weight reduction among overweight and obese women. Health Psychol 2007;26:507. 10.1037/0278-6133.26.4.507 [DOI] [PubMed] [Google Scholar]
- 53.Miller CK, Weinhold KR, Nagaraja HN. Impact of a worksite diabetes prevention intervention on diet quality and social cognitive influences of health behavior: a randomized controlled trial. J Nutr Educ Behav 2016;48:160–9. 10.1016/j.jneb.2015.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Obara-Golebiowska M, Brycz H. Strategies of return to self-regulation among obese people: Implementation of goal’s intention and motivation to weight reduction. Balt J Health Phys Act 2015;7:59–65. 10.29359/BJHPA.07.2.05 [DOI] [Google Scholar]
- 55.Osborn D, Burton A, Hunter R, et al. Clinical and cost-effectiveness of an intervention for reducing cholesterol and cardiovascular risk for people with severe mental illness in English primary care: a cluster randomised controlled trial. Lancet Psychiatry 2018;5:145–54. 10.1016/S2215-0366(18)30007-5 [DOI] [PubMed] [Google Scholar]
- 56.Rodgers WM, Selzler A-M, Haennel RG, et al. An experimental assessment of the influence of exercise versus social implementation intentions on physical activity during and following pulmonary rehabilitation. J Behav Med 2014;37:480–90. 10.1007/s10865-013-9503-z [DOI] [PubMed] [Google Scholar]
- 57.Rodrigues RCM, João TMS, Gallani MCBJ, et al. The "Moving Heart Program": an intervention to improve physical activity among patients with coronary heart disease. Rev Lat Am Enfermagem 2013;21 Spec No:180–9. 10.1590/S0104-11692013000700023 [DOI] [PubMed] [Google Scholar]
- 58.Scholz U, Sniehotta FF, Burkert S, et al. Increasing physical exercise levels: age-specific benefits of planning. J Aging Health 2007;19:851–66. 10.1177/0898264307305207 [DOI] [PubMed] [Google Scholar]
- 59.Scholz U, Ochsner S, Luszczynska A. Comparing different boosters of planning interventions on changes in fat consumption in overweight and obese individuals: a randomized controlled trial. Int J Psychol 2013;48:604–15. 10.1080/00207594.2012.661061 [DOI] [PubMed] [Google Scholar]
- 60.Silva MAVda, São-João TM, Cornelio ME, et al. Effect of implementation intention on walking in people with diabetes: an experimental approach. Rev Saude Publica 2020;54:103. 10.11606/s1518-8787.2020054002024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sniehotta FF, Scholz U, Schwarzer R, et al. Long-term effects of two psychological interventions on physical exercise and self-regulation following coronary rehabilitation. Int J Behav Med 2005;12:244–55. 10.1207/s15327558ijbm1204_5 [DOI] [PubMed] [Google Scholar]
- 62.Sniehotta FF, Scholz U, Schwarzer R. Action plans and coping plans for physical exercise: a longitudinal intervention study in cardiac rehabilitation. Br J Health Psychol 2006;11:23–37. 10.1348/135910705X43804 [DOI] [PubMed] [Google Scholar]
- 63.Sniehotta FF, Dombrowski SU, Avenell A, et al. Randomised controlled feasibility trial of an evidence-informed behavioural intervention for obese adults with additional risk factors. PLoS One 2011;6:e23040. 10.1371/journal.pone.0023040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Soureti A, Murray P, Cobain M, et al. Exploratory study of web-based planning and mobile text reminders in an overweight population. J Med Internet Res 2011;13:e118. 10.2196/jmir.1773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Soureti A, Murray P, Cobain M, et al. Web-based risk communication and planning in an obese population: exploratory study. J Med Internet Res 2011;13:e100. 10.2196/jmir.1579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stevens VJ, Obarzanek E, Cook NR, et al. Long-term weight loss and changes in blood pressure: results of the trials of hypertension prevention, phase II. Ann Intern Med 2001;134:1–11. 10.7326/0003-4819-134-1-200101020-00007 [DOI] [PubMed] [Google Scholar]
- 67.Ströbl V, Knisel W, Landgraf U, et al. A combined planning and telephone aftercare intervention for obese patients: effects on physical activity and body weight after one year. J Rehabil Med 2013;45:198–205. 10.2340/16501977-1095 [DOI] [PubMed] [Google Scholar]
- 68.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA 2008;299:1139–48. 10.1001/jama.299.10.1139 [DOI] [PubMed] [Google Scholar]
- 69.Thoolen BJ, de Ridder D, Bensing J, et al. Beyond good intentions: the role of proactive coping in achieving sustained behavioural change in the context of diabetes management. Psychol Health 2009;24:237–54. 10.1080/08870440701864504 [DOI] [PubMed] [Google Scholar]
- 70.van Genugten L, van Empelen P, Oenema A. Intervention use and action planning in a web-based computer-tailored weight management program for overweight adults: randomized controlled trial. JMIR Res Protoc 2014;3:e31. 10.2196/resprot.2599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vinkers CDW, Adriaanse MA, Kroese FM, et al. Efficacy of a self-management intervention for weight control in overweight and obese adults: a randomized controlled trial. J Behav Med 2014;37:781–92. 10.1007/s10865-013-9530-9 [DOI] [PubMed] [Google Scholar]
- 72.Wilczynska M, Lubans DR, Paolini S, et al. Mediating effects of the ‘eCoFit’ Physical activity intervention for adults at risk of, or diagnosed with, Type 2 diabetes. Int J Behav Med 2019;26:512–21. 10.1007/s12529-019-09800-8 [DOI] [PubMed] [Google Scholar]
- 73.Wooldridge JS, Ranby KW, Roberts S, et al. A couples-based approach for increasing physical activity among adults with type 2 diabetes: a pilot feasibility randomized controlled trial. Diabetes Educ 2019;45:629–41. 10.1177/0145721719881722 [DOI] [PubMed] [Google Scholar]
- 74.Zakrisson A-B, Arne M, Hasselgren M, et al. A complex intervention of self-management for patients with COPD or CHF in primary care improved performance and satisfaction with regard to own selected activities; a longitudinal follow-up. J Adv Nurs 2019;75:175–86. 10.1111/jan.13899 [DOI] [PubMed] [Google Scholar]
- 75.Zandstra EH, den Hoed W, van der Meer N, et al. Improving compliance to meal-replacement food regimens. forming implementation intentions (conscious IF-THEN plans) increases compliance. Appetite 2010;55:666–70. 10.1016/j.appet.2010.09.021 [DOI] [PubMed] [Google Scholar]
- 76.Dombrowski SU, Endevelt R, Steinberg DM, et al. Do more specific plans help you lose weight? examining the relationship between plan specificity, weight loss goals, and plan content in the context of a weight management programme. Br J Health Psychol 2016;21:989–1005. 10.1111/bjhp.12212 [DOI] [PubMed] [Google Scholar]
- 77.Boekhout JM, Berendsen BAJ, Peels DA, et al. Evaluation of a Computer-Tailored healthy ageing intervention to promote physical activity among single older adults with a chronic disease. Int J Environ Res Public Health 2018;15. 10.3390/ijerph15020346. [Epub ahead of print: 15 02 2018]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fleig L, Lippke S, Pomp S, et al. Intervention effects of exercise self-regulation on physical exercise and eating fruits and vegetables: a longitudinal study in orthopedic and cardiac rehabilitation. Prev Med 2011;53:182–7. 10.1016/j.ypmed.2011.06.019 [DOI] [PubMed] [Google Scholar]
- 79.Göhner W, Schlatterer M, Seelig H, et al. Two-year follow-up of an interdisciplinary cognitive-behavioral intervention program for obese adults. J Psychol 2012;146:371–91. 10.1080/00223980.2011.642023 [DOI] [PubMed] [Google Scholar]
- 80.Kivelä K, Elo S, Kyngäs H, et al. The effects of nurse-led health coaching on health-related quality of life and clinical health outcomes among frequent attenders: a quasi-experimental study. Patient Educ Couns 2020;103:1554–61. 10.1016/j.pec.2020.02.026 [DOI] [PubMed] [Google Scholar]
- 81.Leung AYM, Chau PH, Leung ISH, et al. Motivating diabetic and hypertensive patients to engage in regular physical activity: a multi-component intervention derived from the concept of photovoice. Int J Environ Res Public Health 2019;16:1219. 10.3390/ijerph16071219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Richardson J, Letts L, Chan D, et al. Monitoring physical functioning as the sixth vital sign: evaluating patient and practice engagement in chronic illness care in a primary care setting--a quasi-experimental design. BMC Fam Pract 2012;13:1–13. 10.1186/1471-2296-13-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Heron N, Kee F, Donnelly M, et al. Behaviour change techniques in home-based cardiac rehabilitation: a systematic review. Br J Gen Pract 2016;66:e747–57. 10.3399/bjgp16X686617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tomasone JR, Flood SM, Ma JK, et al. Physical activity self-management interventions for adults with spinal cord injury: part 1–A systematic review of the use and effectiveness of behavior change techniques. Psychol Sport Exerc 2018;37:274–85. 10.1016/j.psychsport.2018.01.012 [DOI] [Google Scholar]
- 85.Yang C-H, Maher JP, Conroy DE. Implementation of behavior change techniques in mobile applications for physical activity. Am J Prev Med 2015;48:452–5. 10.1016/j.amepre.2014.10.010 [DOI] [PubMed] [Google Scholar]
- 86.Kunstler BE, Cook JL, Freene N, et al. Physiotherapists use a small number of behaviour change techniques when promoting physical activity: a systematic review comparing experimental and observational studies. J Sci Med Sport 2018;21:609–15. 10.1016/j.jsams.2017.10.027 [DOI] [PubMed] [Google Scholar]
- 87.Cradock KA, ÓLaighin G, Finucane FM, et al. Diet behavior change techniques in type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 2017;40:1800–10. 10.2337/dc17-0462 [DOI] [PubMed] [Google Scholar]
- 88.Schwarzer R. Health action process approach (HAPA) as a theoretical framework to understand behavior change. Actualidades en Psicología 2016;30:119–30. 10.15517/ap.v30i121.23458 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-058229supp001.pdf (2.9MB, pdf)
bmjopen-2021-058229supp002.pdf (58.2KB, pdf)
bmjopen-2021-058229supp003.pdf (63.6KB, pdf)
bmjopen-2021-058229supp004.pdf (66.1KB, pdf)
bmjopen-2021-058229supp005.pdf (177.7KB, pdf)
bmjopen-2021-058229supp006.pdf (59.6KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information. Data are available in a public, open access repository. Extra data can be accessed via the Dryad data repository at http://datadryad.org/ with the doi: 10.5061/dryad.m905qfv48