Abstract
Introduction and importance
Myxoma is the commonest cardiac tumor in adults but is very rare in a newborn. The majority of myxoma arises from the interatrial septum. 75% of myxomas are found in the left atrium and 20% are found in the right atrium. Myxomas can be single or multiple. Multiple myxomas are usually associated with familial syndromes. Myxomas are generally not associated with another congenital heart defect except atrial septal defect. As myxomas are rare in newborns most of the knowledge is through various case reports.
Case presentation
We report a rare case of an 8-day-old neonate presenting with cyanosis and respiratory distress. Transthoracic echocardiography was suggestive of right atrial myxoma which was arising from the atrioventricular junction on the right side of an interatrial septum. It was associated with the total anomalous pulmonary venous connection. The patient underwent successful excision of myxoma and rerouting of the common venous chamber to the left atrium with an uneventful immediate postoperative course.
Clinical discussion
Cardiac myxomas are rare in newborns and their association with TAPVC even rare. Our patient had single atrial myxoma with TAPVC. The significance of this association is not clear. This association is mostly by chance. Probably it is the first case reported of its kind.
Conclusion
As myxomas are very rare in neonates, it is highly possible to miss other associated structural heart defects. Diagnosis of atrial myxoma can be suggested by echocardiogram but a definite diagnosis can only be confirmed by histology.
Keywords: Case report, Right atrial myxoma, Neonate, Total anomolus pulmonary venous connections (TAPVC), Severe pulmonary hypertension
Highlights
-
•
Mass in right atrium in a neonate
-
•
Rare association of atrial myxoma with total anamolous pulmonary venous connection in neonates
-
•
Probably the first case reported
1. Introduction
“Cardiac mass is defined as an abnormal structure within or immediately adjacent to the heart. The three basic types of cardiac masses are tumor, thrombus, or vegetation” [1]. Tumor, thrombus, and infective vegetation are important differential diagnoses. Cardiac tumors are rare in the pediatric population, out of which the majority are benign [2]. Benign cardiac tumors are classified as Rhybdomyoma, myxoma, fibroma, lipoma, and hemangioma. Rhybdomyoma is the commonest benign cardiac tumor in the pediatric population [3]. Myxomas are the commonest cardiac tumor in adults but very rare in neonates and fetuses [4]. Myxomas are known to have familial occurrences. Various syndromes like LAMB (Lentigines, Atrial myxoma, Mucocutaneous myxoma, and Blue naevi) and NAME (Naevi, Atrial myxoma, Myxoid neurofibromata, and Ephelides) are associated with myxomas. Myxoma with familial occurrences is usually multiple but can be solitary in a few patients. Myxomas are most commonly located in the left atrium and rarely in the right atrium [5]. Association of atrial myxoma with other congenital heart diseases is rare. We report a case of an 8-day neonate presenting with right atrial myxoma arising from interatrial septum associated with the total anomalous pulmonary venous connection (TAPVC). There was no family history of myxoma or another congenital heart disease. The patient was operated on for removal of RA mass and TAPVC repair. To our knowledge, this is the first case reported in neonates with right atrial myxoma and TAPVC.
Work reported was done in Acharya Vinoba Bhave Hospital, Sawangi(M) which is a tertiary care center in the Vidarbha region of Maharashtra. This is a rural hospital attached to the private medical college, Jawaharlal Nehru Medical College under DMIMS. Surgery was performed by a surgeon who had experience of 15 years in pediatric cardiac surgery. He worked as a professor and head of the department of CVTS for 5 years. The work reported is in line with the SCARE 2020 criteria [6]. Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
2. Case report
8 day old full term neonate presented with increased respiratory rate and bluish discoloration of nails and lips. The baby had been diagnosed with a right atrial mass on antenatal scans. There was no history of any congenital heart disease or atrial myxoma in the family. No history of any drug intake other than routine nutrient supplementation by mother. A screening transthoracic echocardiogram was done on the second day of life. It was suggestive of heterogeneous, pedunculated right atrial mass attached to interatrial septum approximately 10 × 8 mm with mild tricuspid regurgitation. Peak right ventricular systolic pressure was 61 mmHg suggestive of severe pulmonary hypertension. Screening echocardiogram of a family member were normal.
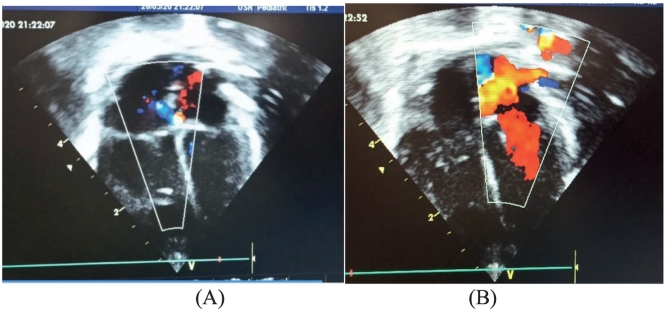
On day 8 of life, the patient was tachypneic and mildly cyanosed with SP02 84 % on room air on, ESM murmur with loud P2 was heard. Chest X-ray was suggestive of pulmonary plethora and mild cardiomegaly. A repeat transthoracic echocardiogram was done by a pediatric cardiologist which was suggestive of a right atrial mass 10 × 9 mm attached at an atrioventricular junction on the right side of the interatrial septum (Fig. 1), restrictive atrial septal defect (ASD) above the upper border of mass with the right to left shunt, dilated pulmonary arteries and severe pulmonary hypertension. 2 right-sided pulmonary veins form a common vein which drains into superior vena cava (SVC) and one pulmonary vein was draining to SVC directly (Fig. 2). Computed tomography (CT) was done for evaluation of left sided pulmonary veins. CT suggested right superior pulmonary vein and right inferior pulmonary vein form a common chamber that drains to the superior vena cava. Left-sided pulmonary vein joins to form a common vein which continues infradiaphragmatically to join to the portal vein. So the diagnosis of right atrial mass with mixed TAPVC with severe pulmonary hypertension was made and surgery was planned accordingly.
Fig. 1.

Large hyperechoic lesion from interatrial septum in right atrium (Preoperative).
Fig. 2.
A) Right sided pulmonary vein forming common and drain to SVC above SVC RA junction and one right sided vein entering to SVC directly. B) hyperechoic mass attached at atroventricular junction in right atrium and ASD shunting right to left.(This figure required colour image).
The heart was approached through a midline sternotomy. The baby was put on cardiopulmonary bypass with bicaval cannulation and aortic cannulation. The right Atrium was opened under cardioplegic arrest. Operative findings were thick pedunculated mass was attached to the interatrial septum at the atrioventricular junction. 2 Right-sided pulmonary veins form a common vein which drains to the superior vena cava and the right middle pulmonary vein joins separately to SVC. Left-sided pulmonary vein joins to form a vertical vein which joins to the portal vein infra diagrammatically. Individual pulmonary veins were normal. Right atrial mass around 10 × 10 mm was excised as much as possible. TAPVC was addressed next. Both common veins were routed to left atrium by augmenting it with pericardial patch. ASD was closed with a pericardial patch.
The postoperative course was uneventful. The baby was extubated after 24 h. A postoperative echocardiogram shows an unobstructed flow of a pulmonary vein to left atrium, small PFO was there shunting left to right (Fig. 3). Histology examination of a mass was suggestive of myxoma.
Fig. 3.
A) Postoperative image showing no residual mass, small PFO with left to right shunt. B) Unobstructed pulmonary venous flow to left atrium. (colour image required).
3. Discussion
Myxoma is rare in the pediatric population though it is commonest in adult. The usual site of the tumor is left atrium followed by the right atrium and ventricle or may be multifocal [7]. Association of atrial myxoma with congenital heart diseases other than atrial septal defect is usually not reported. There is only a single case reported by Mathur et al. suggesting association of TAPVC with a multiple myxoma in 18 year old female [8]. Significance of this association is considered to be mostly probability of chance.
Cardiac tumors may be diagnosed antenatally by anomaly scan. The cardiac tumor can present as arrhythmias, hydrops fetalis, and congestive cardiac failure in fetal life. Postnatally clinical features depend upon the size, location, shape, and mobility of the tumor [9]. Clinical presentation of cardiac myxomas is variable from asymptomatic to cyanosis, respiratory distress, arrhythmias, murmur and sudden death. Our patient had respiratory distress and cyanosis which could be attributed to TAPVC. In adult patients, myxoma may present with constitutional symptoms due to the release of interleukin 6 and tumor necrosis factor [10].
Echocardiography provides the diagnosis of mass along with its structural details like size, shape, location, site of attachment, valvular obstruction or regurgitation, cardiac contractility, and other associated congenital cardiac defects. As atrial myxoma in a neonate is so engrossing that other structural heart defects can be missed which happens in our case in the initial evaluation. Cardiac MRI can provide better details of myxomas but that facility was not available at our institute.
Surgical excision of myxoma was straightforward. Rerouting of the pulmonary venous chamber to the left atrium was uneventful. Histopathological examination of mass reveals scattered round cells dense irregular nuclei with loose myxoid stroma suggestive of myxoma.
4. Conclusion
Diagnosis of atrial myxoma can be suggested by echocardiogram but a definite diagnosis can only be confirmed by histology. Echocardiography alone suggests the diagnosis but search carefully for other associated structural cardiac lesion as it's very likely to miss other heart defects. There is a need for more reporting and study of this subject if myxoma in the neonate is associated with other congenital anomalies.
Sources of funding
No funding.
Ethical approval
N/A.
Consent
The authors obtained patient consent to use all the images presented.
Registration of research studies
N/A.
Guarantor
Dr. Shantanu Gomase
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Dr. Shantanu Gomase: Writing the paper.
Dr. Sachin Kuthe: Data collection and analysis.
Dr. Manish Sonkusale: Study concept.
Declaration of competing interest
The authors report no declarations of interest.
References
- 1.Otto C.M., editor. Textbook of Clinical Echocardiography. 5th ed. Elsevier Saunders; Philadelphia: 2013. Cardiac masses and potential cardiac source of embolus; pp. 395–417. [Google Scholar]
- 2.Arciniegas E., Hakimi M., Farooki Z.Q., Truccone N.J., Green E.W. Primarycardiac tumors in children. J. Thorac. Cardiovasc. Surg. 1980;79:582–591. [PubMed] [Google Scholar]
- 3.Uzun Orhan, Wilson Dirk G., Vujanic Gordon M., Parsons Jonathan M., De Giovanni Joseph V. Orphanet J. Rare Dis. 2007;2:11. doi: 10.1186/1750-1172-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beghetti M., Gow R.M., Haney I., Mawson J., Williams W.G., Freedom R.M. Pediatric primary benign cardiac tumours: a 15-year review. Am. Heart J. 1997;134:1107–1114. doi: 10.1016/s0002-8703(97)70032-2. [DOI] [PubMed] [Google Scholar]
- 5.Bulkley B.H., Hutchins G.M. Atrial myxomas: a fifty year review. Am. Heart J. 1979;97:639–643. doi: 10.1016/0002-8703(79)90193-5. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Reynen K. Cardiac myxomas. NE]M. 1995:1610–1617. doi: 10.1056/NEJM199512143332407. [DOI] [PubMed] [Google Scholar]
- 8.Mch Alok Mathur, et al. Multiple, multifocal myxomas pulmonary venous drainage with total anomalous. IJTCVS. 2005;21:40–41. [Google Scholar]
- 9.Peters P.J., Reinhardt S. The echocardiographic evaluation of intracardiac masses: a review. J. Am. Soc. Echocardiogr. 2006;19:230–240. doi: 10.1016/j.echo.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 10.Mendoza C.E., Rosado M.F., Bernal L. The role of interleukin-6 in cases of cardiac myxoma. Clinical features, immunologic abnormalities, and a possible role in recurrence. Tex. Heart Inst. J. 2001;28(1):3–7. PMID: 11330738; PMCID: PMC101121. [PMC free article] [PubMed] [Google Scholar]