Abstract
Introduction and importance
The oro-antral communication (OAC) is a pathological opening between the maxillary sinus and the oral cavity. When it does not close spontaneously or if it is not treated, it remains permeable and epithelializes to develop into an oro-antral fistula (OAF) and can cause maxillary sinusitis.
Cases presentation
The authors present through 5 clinical cases the different steps of the surgical protocols opting for the buccal fat pad flap and the advanced buccal flap to treat OAF/OAC.
Clinical discussion
Surgical closure of the OAC within 48 h is recommended to avoid complications. Several alternative techniques have been described over the years for the management of the OAC and OAF, with their advantages and limitations. The most commonly used surgical flaps are of two types: the advanced buccal flap and the buccal fat pad (BFP) flap.
Conclusion
The adequate availability of the advanced buccal flap and the buccal fat pad (BFP) flap in the majority of patients, the easy handling, the minimal donor site morbidity as well as the excellent blood supply make them perfect flaps for the closure of OAF/OAC. However, follow-up remains a key point and very important to avoid complications. The present case series was limited by the small number of patients and the authors recommend a study with larger groups.
Keywords: Case series, Oro-antral communications, Oro-antral fistula, Diagnosis, Advanced buccal flap, Buccal fat pad flap
Highlights
-
•
Surgical closure of the oro-antral communication within 48 hours is recommended to avoid complications.
-
•
Oro-antral fistula should be managed promptly by creating a barrier between oral cavity and maxillary sinus to prevent maxillary sinusitis.
-
•
Successful closure of oro-antral fistula or communication depends on compliance with the indications and surgical protocol.
-
•
Follow-up remains very important to avoid complications.
1. Introduction
Oroantral communications (OAC) are complications that frequently occur in oral and maxillofacial surgery. It is an unnatural pathological opening between the oral cavity and the maxillary sinus [1]. The proximity of the maxillary sinus during extraction of antral teeth, most often the upper molars and premolars, is the main reason for this complication (48 %). Interventions on cystic or tumoral pathologies (18.5 %), or following a trauma (7.5 %) can lead to the creation of an oral-sinus communication [2]. Other causes include osteoradionecrosis, infection, sinusitis, osteomyelitis, during implant surgery or following dehiscence after implant failure and sometimes as a complication of the Caldwell-Luc procedure [1], [3].
In the absence of sinus infection, most small OACs 1–2 mm in diameter heal spontaneously through blood clot formation and secondary healing [4]. However, bony defects >2 mm require adequate treatment within 24 h [3], [6], which consists of closure of the breach to ensure site tightness and avoid possible sinus infection. Larger OACs that go undiagnosed or untreated rarely heal, and when it does not close spontaneously, it remains permeable and epithelializes to develop into an oro-antral fistula [1]. This epithelialization usually occurs when the communication persists for at least 48 to 72 h [3], [5]. In addition, several situations can occur including alveolar; vestibular or palatal OAF [7].
If OAF/OAC is not properly treated, approximately 50 % of patients will develop sinusitis 48 h later, and 90 % of patients will develop sinusitis after 2 weeks of no treatment [6].
Typically, surgical techniques for OAF repair include local autogenous soft tissue flaps from buccal or palatal tissues, use of the buccal fat pad, tongue flaps, bone grafts, and/or alloplastic materials, such as hydroxyapatite, soft polymethylmethacrylate, resorbable collagen membranes, gold foil, and gold plates [4], [8], [9].
The choice of the appropriate treatment technique is based on a combination of several patient-related factors, such as age, medical comorbidities, sinus health, size and location of the defect, distance from adjacent tissues, and factors related to the dentist's experience and technical skills [8], [9].
Below, we present through clinical cases the different steps of surgical protocols opting for the buccal fat pad flap and the advanced buccal flap to treat OAF/OAC. These cases were reported according to the PROCESS 2020 criteria [10].
2. Method
The patients included in our work are those whose surgery was performed, between 2019 and 2022.by a resident doctor, in the department of surgical dentistry of the Center of Consultations and Dental Care of the University Hospital Ibn Sina in Rabat, Morocco.
The inclusion criteria were as follows:
-
•
Signs and symptoms of maxillary sinusitis.
-
•
Oroantral communication confirmed after the removal of an antral tooth
-
•
Persistence of an unhealed orifice after tooth extraction
Data recorded included gender, age, fistula location, fistula size, and complications. The criteria for successful and effective treatment were complete closure of the communication and restoration of the maxillary sinus.
Of the 5 patients, 2 were female and 3 were male. Their ages ranged from 20 to 45 years.
The dimensions of the OAF/OAC varied from 6 to 12 mm.
3. Clinical protocol and surgical procedure
3.1. Case 1
A 36-year-old woman, in good general health, referred by her dentist because of persistent air leakage in the right maxillary region, after treatment of sinusitis with Amoxicillin/Clavulanic Acid “Zamox®, 1 g/125 mg, comprimé, Laboratory BOTTU, Casablanca, Maroc” for 1 month.
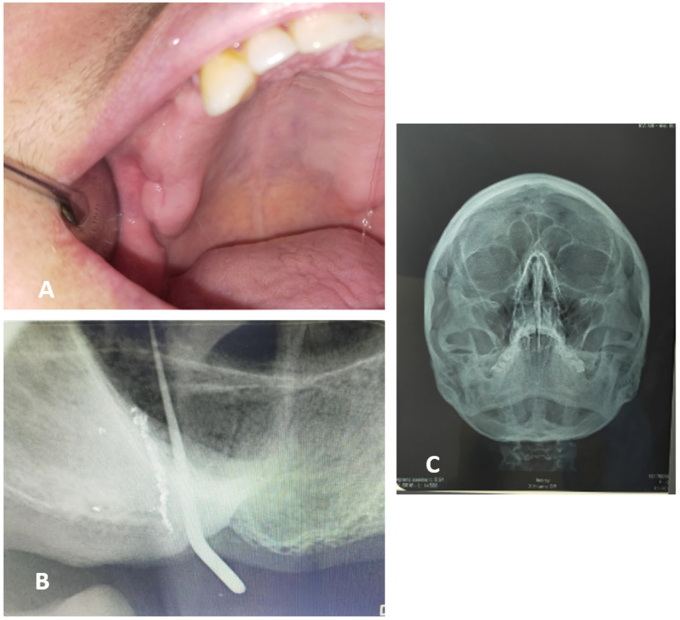
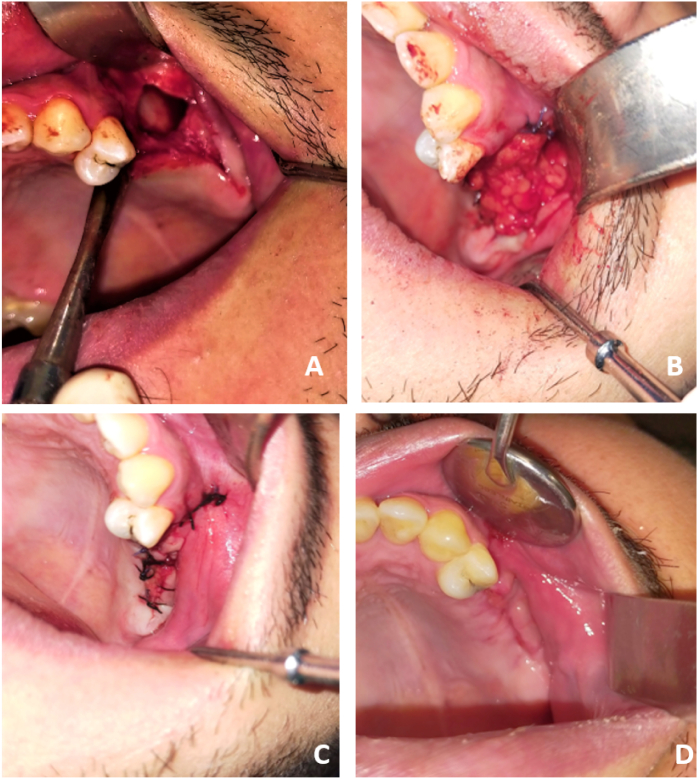
Endo-buccal examination showed the presence of an asymptomatic fistula of approximately 2 mm, with absence of pus and systemic inflammatory signs (Fig. 1A).
Fig. 1.
A: Endo-buccal view showing the intraoral fistula with absence of pus and systemic inflammatory signs. B: Retroalveolar cone in place showing the bone defect in the site, materialized by a perforation in the right maxillary sinus floor.C: Blandeau Incidence revealing the absence of anomaly in the right maxillary sinus.
A retroalveolar rediography with a cone introduced into the fistula revealed the bony defect in the site, materialized by a perforation in the floor of the right maxillary sinus, which confirmed the communication between the oral cavity and the right maxillary sinus. A blandeau scan was performed and revealed the absence of abnormality in the right maxillary sinus with a flaw in its floor (Fig. 1B/C).
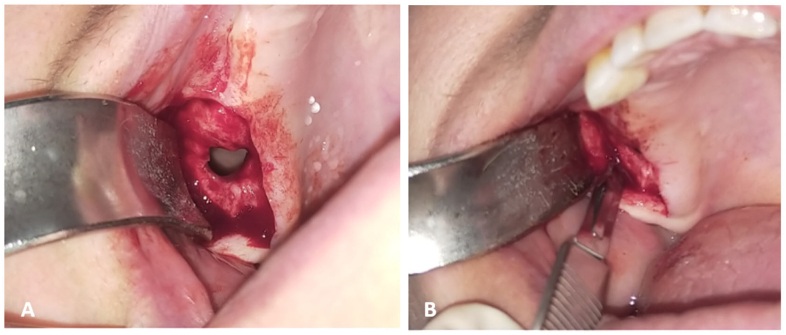
Under local anesthesia, the surgical procedure consisted of a crestal incision followed by a mesial discharge in the region of the upper right first molar. After raising the sinus, the diameter of the fistula appeared larger than its initial clinical size, approximately 12 mm (Fig. 2A). Then a horizontal incision over the periosteum and fascial cover to remove the BFP was made (Fig. 2B). The BFP was dragged into the fistula site, completely covering the defect, and then sutured with simple 3–0 resorbable silk sutures, without tension (Fig. 3A/B).
Fig. 2.
A: endo-buccal view showing the detachment of the full thickness flap, and highlighting a fistula larger than its initial clinical dimension. B: Horizontal incision on the periosteum and the fascial cover to remove the buccal fat pad.
Fig. 3.
A: the buccal fat pad pulled.B: Recovery of the fistula by the buccal fat pad sutured to the palatal bank. C: Control after 15 days. D: Control after 6 months.
The suture was removed after a 15-day postoperative period without complications; the patient had an advanced stage of mucosal epithelial tissue proliferation over the adipose tissue (Fig. 3C). Six months after the procedure, wound healing and complete closure of the defect, which was completely epithelialized, was observed (Fig. 3D).
3.2. Case 2
A 30-year-old patient, in good general health, referred to our surgical odontology department, complaining of pain in the left hemiface and persistence of an unhealed orifice, as well as fluid discharge through his nose and food entry through the communication due to an extraction of the left upper first molar seven months earlier.
The extraoral examination did not reveal any particularity. On intraoral examination, we noted stomatitis under prosthesis with the absence of 17, 16, 15, 14, 25, 26, 27, 28, and the presence of a fistula of approximately 4 mm at the level of the left alveolar ridge (Fig. 4A).
Fig. 4.
A: Endo-buccal view showing the sub-prosthetic stomatitis and the intraoral fistula. B: Panoramic radiograph revealing a left bony defect at the extraction site, and also the presence of a perforation of the floor of the left maxillary sinus, which confirms the communication between the oral cavity and the left sinus. C: Blandeau Incidence revealing the presence of a left maxillary veiled sinus with a defect in its floor.
Panoramic radiograph revealed a left bony defect at the extraction site, and also the presence of a perforation of the floor of the left maxillary sinus, which confirms the communication between the oral cavity and the sinus (Fig. 4B).
A blandeau scan was performed and revealed a left maxillary veiled sinus with a defect in its floor. This led to the diagnosis of chronic sinusitis (Fig. 4C).
To treat the stomatitis under prosthesis an antifungal gel “Dactarin®, 2 %, gel, Laboratory JANSSEN CILAG, France” in local application during 10 days was prescribed.
For the management of the sinus flap, the patient was put on antibiotics by using amoxicillin/clavulanic acid as a molecule “Augmentin®, 1 g/125 mg, Sachet, Laboratory GlaxoSmithKline, France” for 10 days, analgesics level 2 “Codoliprane®, tablet, Casablanca Maroc”, sea water nasal spray “Sterimar®, nasal spray, Laboratory Fumouze, Levallois-Perret, France” and an oral antiseptic “Eludril®, moutwash, Pierre Fabre, Paris, France”. A surgery with BFP was decided to close the oro-antral fistula.
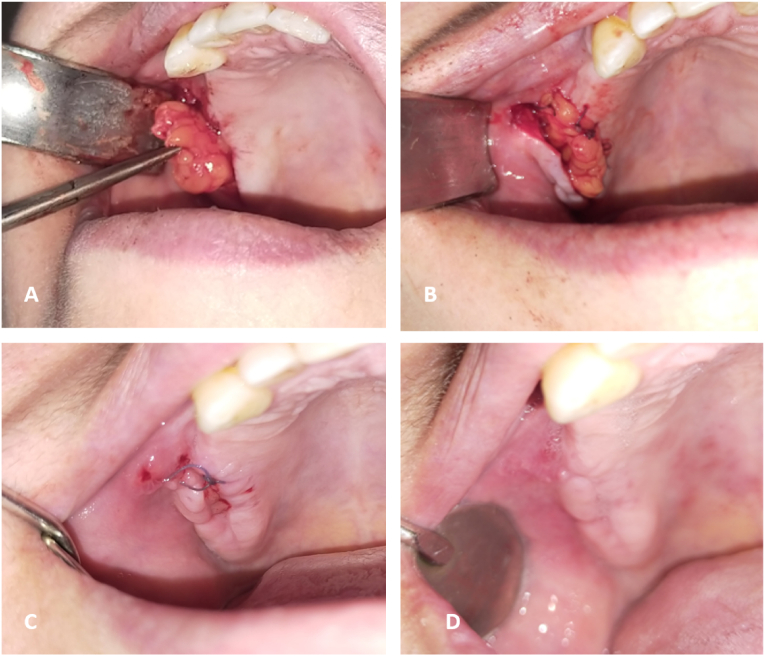
Under local anesthesia, a crestal incision with mesial discharge allowed the lifting of a mucoperisoteal flap and the exposure of a fistula with a diameter of approximately 12 mm. The epithelial tract and inflammatory tissue within the opening were completely removed and a cleaning and saline flushing of the site was performed (Fig. 5A). A horizontal incision over the periosteum and fascial covering to remove the bichat ball was made, the bichat ball was dragged to cover the bony defect and then sutured to the palatal margin (Fig. 5B). Hermetic sutures were performed to reposition the flap to its original position covering the BFP (Fig. 5C).
Fig. 5.
Removal of the tissue filling the maxillary sinus and rinsing with saline solution.B: Recovery of the fistula with the buccal fat pad pulled and sutured to the palatal margin. C: Covering of the Bichat's ball by the vestibular flap. D: Control after 1 month.
Antibiotics were continued for 10 days, as well as prednisolone 60 mg/day for 5 days, paracetamol and nasal decongestant.
The patient was seen again after 10 days (Fig. 5D). Healing was uneventful with closure of the OAF. At six months, good healing was noted with a return to normal.
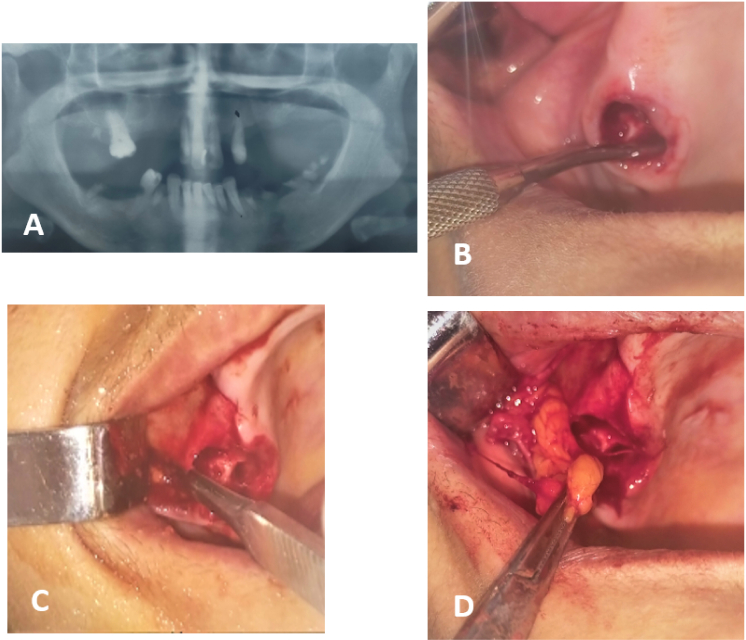
3.3. Case 3
A 45-year-old patient in good general health was referred to our department for extraction of 17,16,38,37, 35, 34, 44, 45,47. The X-ray showed the 16 antral (Fig. 6A/B). After removal of the 16, the oro-antral communication was confirmed and her management was performed by a BFP according to the technique described in the firsts cases reports (Fig. 7A/B/C/D). Follow-up of the patient after six months showed good healing without any complications.
Fig. 6.
A: panoramic radiograph showing the 18 antral in the maxillary sinus. B:Insertion of the curette after extraction of the 18 in the sinus showing the presence of a bucco-sinus communication. C: Horizontal incision on the periosteum and the fascial cover to remove the ball of bichat.
Fig. 7.
A/B: Recovery of the fistula with the Bichat ball pulled and sutured to the palatal margin. B: Covering of the Bichat's ball by the flap. C: Control after 1 month.
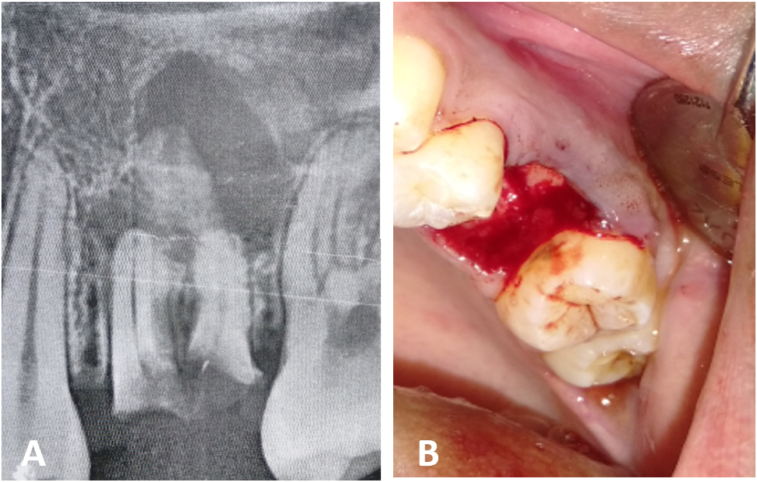
3.4. Case 4
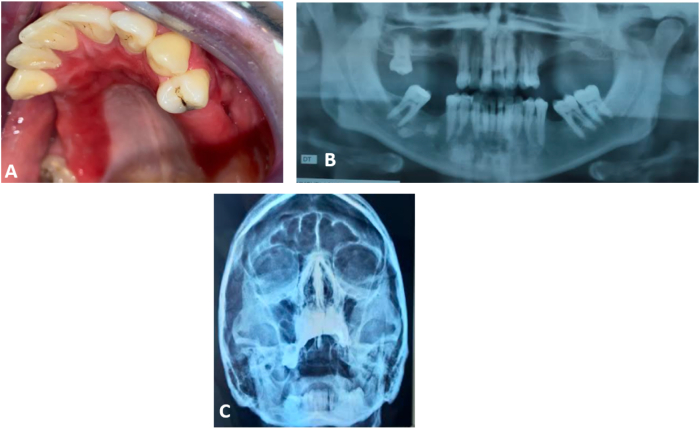
A 20-year-old patient in good general health was referred to our department for extraction of the residual roots of the 26. Retro alveolar X-ray showed the 26 antral with a periapical image of medium extent (Fig. 8A). After removal of the 26, the oro-antral communication was confirmed and its management was performed by a vestibular translation flap (Fig. 8B).
Fig. 8.
A: Retro alveolar showing the 26 antral in the maxillary sinus with a periapical image.B: Extraction of the 26.
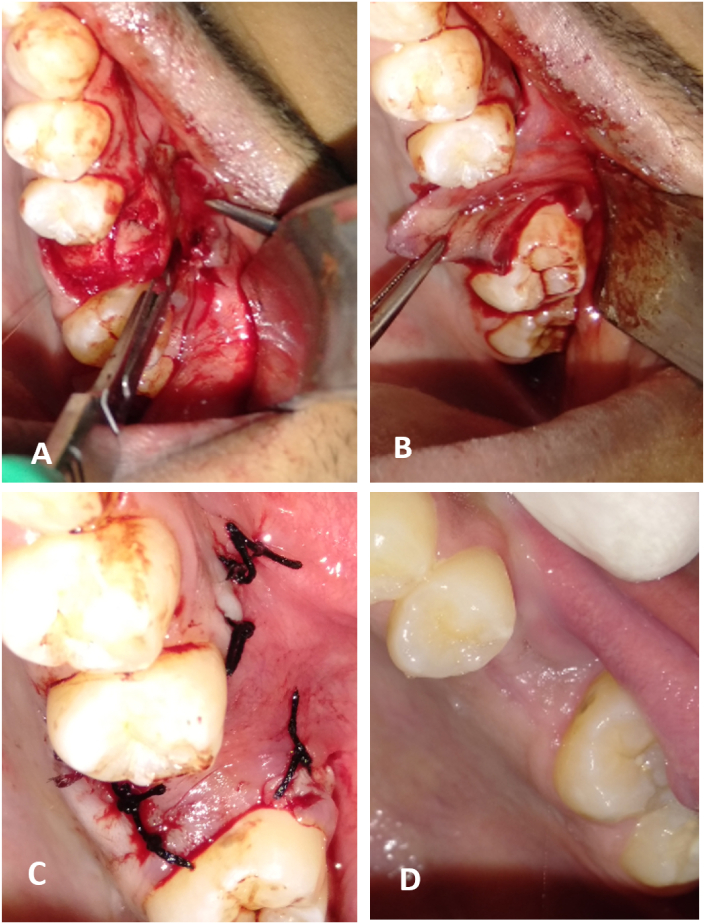
Under local anesthesia; two vertical trapezoidal release incisions were made. The broad-based mucoperiosteal flap was dragged and placed over the defect (Fig. 9A/B) and sutured to the palatal margins (Fig. 9C), and routine postoperative instructions with antibiotic and analgesic prescription were given to the patient. Healing was uneventful, and the patient's 1 year follow-up showed no recurrence (Fig. 9 D).
Fig. 9.
A: Creation of a partial thickness vestibular flap. B: Flap traction. C: The flap is sutured hermetically to the palatal edge. D: Control after 1 year (healing of the surgical site).
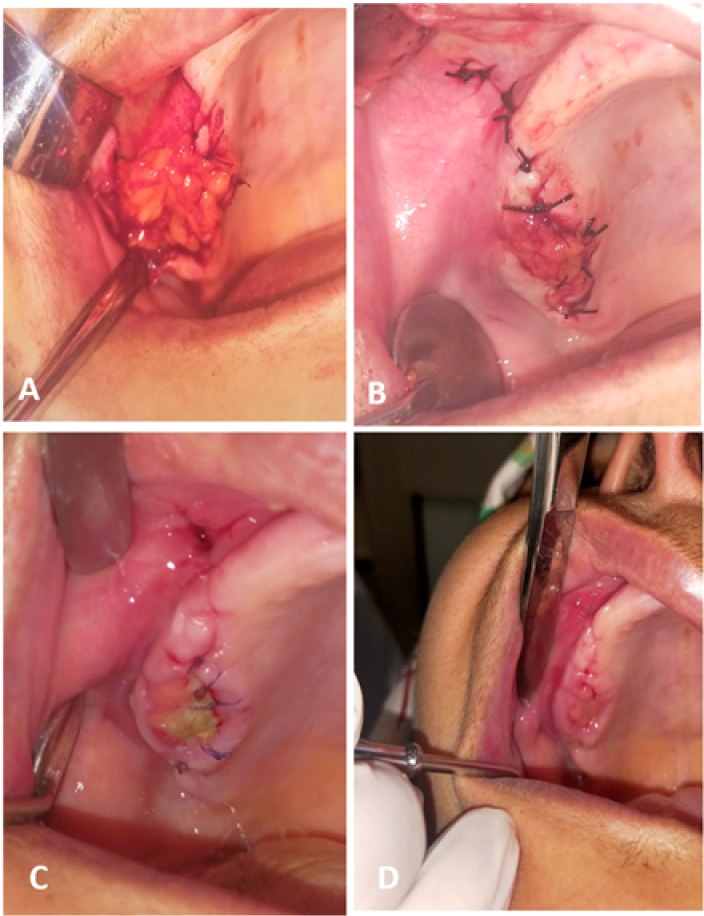
3.5. Case 5
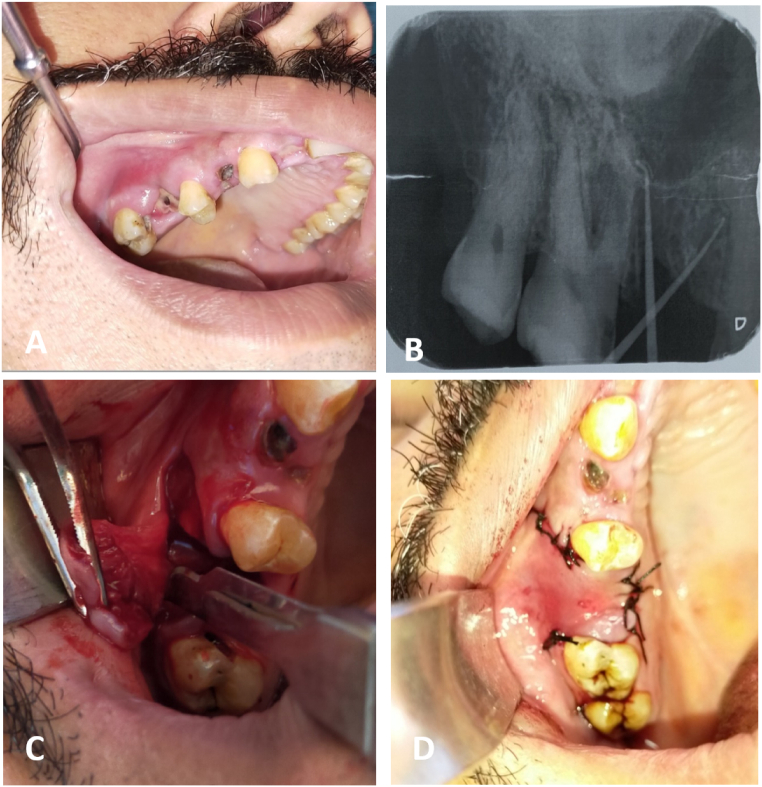
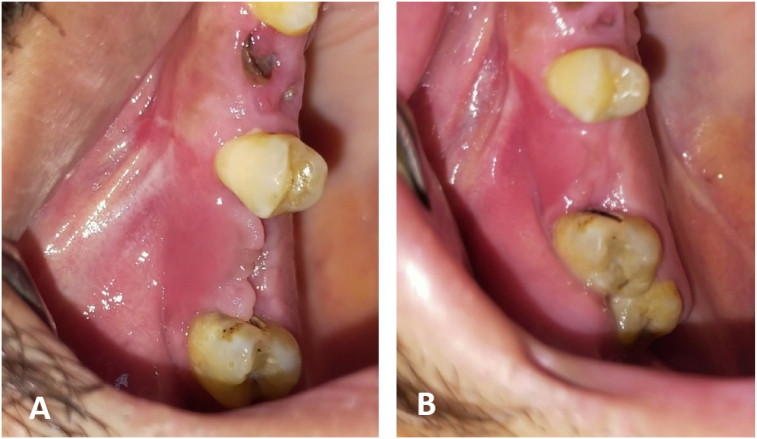
A 32-year-old patient in good general health complained of delayed healing after extraction of the 16 one month earlier. Clinical and radiographic examination revealed an oroantral fistula. There was no evidence of acute infection (Fig. 10A/B). However, the patient was started on antibiotics (amoxicillin/clavulanic acid “Augmentin®, 1 g/125 mg, Sachet, Laboratory GlaxoSmithKline, France” for 10 days), seawater nasal spray “Sterimar®, nasal spray, Laboratory Fumouze, Levallois-Perret, France” and an oral antiseptic for management of the sinus component. After 7 days, the patient underwent surgery with a vestibular translation flap using the technique described in the previous case (Fig. 10C/D). Healing was uneventful, and the patient's 1 year follow-up showed no recurrence (Fig. 11A/B).
Fig. 10.
A: Endobuccal view. B: Retro alveolar gutta cone in place showing a bone defect in the extraction site materialized by a perforation in the right maxillary sinus floor. C: Creation of a partial thickness vestibular flap. D: The flap is sutured hermetically to the palatal edge.
Fig. 11.
A: Control after 10 days. B: Control after 1 year (healing of the surgical site).
4. Results
Of all the patients we received for this surgery, two of them (case 1, case 5) had asymptomatic fistula, while, one patient had sinusitis (case 2), and 2 patients had OAC, which were confirmed immediately after extraction (case 4, case 3).
One week after surgery, all fistulas were visually evaluated, finding no opening or dehiscence of the operative sites. After one month, we performed the Valsalva test which concluded complete closure of the fistulas. As for case 2, the sinusitis recovered. Indeed, these results confirm that BFP and advanced buccal flap are effective in closing the OAF/OAC.
Post-operative follow-up was performed for a period ranging from 6 to 24 months. However, it is important to specify that all our patients were motivated for the follow-up.
5. Clinical discussion
The clinical diagnosis of OAC/OAF is usually based on subjective and objective findings, patients may be asymptomatic [11], but most complain of symptoms that may be acute or chronic. Acute symptoms include epistaxis, passage of fluid or air through the OAC/OAF, pain in and around the affected sinus area, voice alteration, and wheezing when speaking [2]. Chronic symptoms include alleviated pain, free drainage of fluids through the oral fistula, mucopurulent nasal discharge, antral polyps may be visualized through the defect at a later stage, postnasal drip, bad intraoral odor and taste, voice alterations and earache [9], [11].
The Valsalva test can be used by having the patient gently expel air against the closed nostrils while keeping the mouth open, the passage of air or blood at the postoperative site usually indicates the presence of an OAC/OAF [11]. However, a negative test does not rule out the possibility of an antral perforation. It should be noted that detection of small perforations is not always possible. Fogging of a mouth mirror placed at the orifice may also confirm the clinical diagnosis [11], [12].
To validate the clinical findings, radiological investigation of the OAC and OAF site is necessary [2], [11], [13], [14]. A panoramic radiograph and a blond CT scan can determine the size, location, and degree of sinus involvement [13].
It is essential to close the oro-antral fistula in a disease-free sinus environment to prevent exacerbation of the infection. Therefore, management of the sinus flap is the first step that should be performed and consists of a prescription for:
-
▪
Amoxicillin/Clavulanic acid for 10 days “Augmentin®, 1 g/125 mg, Sachet, France”.
-
▪
Corticosteroids for 8 days “Solupred® 20 mg, tablet, Casablanca, Morocco”.
-
▪
Anlgesics, level 2 “Codoliprane®, tablet, Casablanca, Maroc”.
-
▪
Sea water solution in nasal spray “Sterimar®, nasal spray, Levallois-Perret, France”.
-
▪
Oral antiseptic “Eludril®, moutwash, Paris, France”.
Patients with chronic sinusitis who do not respond to medical treatment will require surgical intervention such as endoscopic sinus surgery or the Caldwell-Luc procedure [1].
A rational decision-making process should be followed for OAC/OAF closure rather than haphazardly performing the available technique [13]. For this, several factors should be considered, the most important of which are the age, size, and location of the defect as well as its relationship to the adjacent teeth and the height of the alveolar ridge [15]. Usually, an OAF <2 mm in diameter closes spontaneously, but when there is more than >3 to 4 mm of defect, the opening persists and requires surgical closure. In addition clinically, the tract closure flap should be broad-based, well-vascularized, and the anastomosis site should be free of tension and located on the intact alveolar bone leaving at least 5 mm from the fistula margin [13]
In 1936. Rehrmann [16] described the vestibular sliding flap, which can be considered the oldest and most common surgical technique for the treatment of OAC. For the realization of this flap, two vertical diverging vestibular incisions from the extraction socket or the edges of the fistula orifice must be made. The resulting broad-based trapezoidal mucoperiosteal flap is pulled and placed over the defect and sutured to the palatal margins. The literature has reported high success rates (93 %) related to the sufficient vascularization provided by the wide base of this flap [14], [17]. Despite the high success rates, von Wowern [17] has shown that the reduction in sulcus depth after the Rehrmann method is permanent in half of the cases. The vestibular flap technique can be used successfully in the treatment of small and medium-sized communications, but in case of a defect displaced to the palatal area that requires greater flap sliding and consequently more vestibular depth loss this technique is contraindicated [14], [18].
Môczáir [19] described the closure of OAF\OAC by an alternative method that involves moving the vestibular flap of a tooth downstream. This technique produces negligible change in vestibular depth compared with the Rehrmann method, which may require additional vestibuloplasty in patients with prostheses [13], [14]. A disadvantage of this approach is that it can lead to gingival recession and periodontal disease because it requires a large amount of dentogingival detachment to facilitate the shift.
The BFP has the shape of a gutter with a vertical axis and a posterior concavity, it is a lobulated mass that lies in the masticatory and buccal spaces. Anatomically, it is bounded medially by the buccinator muscle, anterolaterally by the zygomatic arch, deep cervical fascia, and muscles of facial expression, and posteriorly by the parotid gland and mandibular ramus with attached masticatory muscles [20].
The BFP consists of a “body” and four extensions: buccal, pterygoid, deep temporal and superficial temporal. The body and buccal extension make up 50–70 % of the total weight of the BFP, approximately 9.5 g, regardless of the individual's weight [21].
To make this flap, an incision is made in the posterior mucosa at the level of the zygomatic buttress, followed by a periosteal incision. The fascia enveloping the buccal fat pad is then incised. Gentle dissection with fine curved artery forceps is performed to expose the yellowish-colored buccal fat. The pedicled buccal fat pad flap is most often used for the closure of the OAF [3].
BFP have many advantages over other types of flaps. The anatomically favorable location; facilitates harvesting and minimal dissection is required to harvest and mobilize the flap [3]. The surgical procedure is simple and has shown a high success rate in various applications [22]. The high success rates of BFP flaps are attributed to a rich blood supply from the maxillary artery (buccal and deep temporal branches), superficial temporal artery (transverse facial branch), and facial artery (small branches) [23].
Postoperative sequelae to be expected with this surgery are pain, swelling, depression of the cheek after reconstruction has also been noted. Finally, trismus is usually reported after reconstruction using BFP. To alleviate this problem, mouth opening exercises can be performed starting on the 5th day after surgery [24].
The risk of failure is present after any surgical procedure. The most common reasons leading to failure after closure of oro-antral defects may be: inadequate preoperative treatment of a pre-existing sinus infection, insufficient vascularization of the flap used due to excessive tension, failure of the patient to follow postoperative advice or instructions given incorrectly by the practitioner [3]. Therefore, patients should be instructed not to eat hard foods. They should eat soft foods and drink liquid on the opposite side to avoid trauma to the surgical site. Intense physical activities that may increase the intrasinusoidal pressure should be avoided until recovery. Blowing the nose and sneezing with the mouth closed is prohibited for 2 weeks. The patient should open the mouth when coughing or sneezing. Patients should not roll their tongue over the suture line or flap for 07 days after surgery. The wound should be kept clean with warm saline mouthwashes. The use of straws or smoking is prohibited [3] [25].
.The palatal flap can also be used to resolve important communications without damaging the vestibular sulcus, although this procedure creates great morbidity due to the open area it creates in the palate. This open area requires a long period of postoperative care, generating enormous discomfort for the patient [18].
When establishing a treatment plan, one must take into account the patient's general condition, the presence of a medical history and specific needs, such as the existence of a long-term treatment that may have an effect on the body's functions and therefore influence dental management, or radiotherapy in the head and neck region. The age of the patient can also have an impact on the healing process, and the quantity and quality of the remaining tissue, the use of dentures or not, and the possibility of placing an implant in the affected site must be assessed. Although each flap technique has its own advantages and disadvantages, the choice depends largely on these factors and the success of a technique is related to the use of a flap with appropriate indications.
This study allowed us to evaluate our choice of the standard buccal flaps as a treatment technique for OAC/OAF. Indeed, this technique showed its effectiveness, since, all patients in the present study were satisfied, and also, a good healing was noted with a later return to normal.
This clearly shows that the buccal flaps is strongly indicated in the treatment of OAF and OAC, and remains a reference technique despite the appearance of new techniques, such as: autogenous bone grafts, allogenic materials, xenografts, flexible polymethylmethacrylate…etc.
The present case series was limited by the small number of patients, to remedy this, the authors recommend a study with larger groups.
In addition, in order to enrich the scientific field, we consider it useful to conduct further studies on the feasibility and efficacy of Platelet-Rich-Fibrin (PRF) in the treatment of OAF/OAC and also, to conduct a comparison of the results of our case series with this technique.
6. Conclusion
OAC/OAF is a common complication in oral surgery. Clinical and radiographic examinations are necessary to establish a diagnosis. It can be inferred from this article that OAC/OAF should be managed promptly by creating a barrier between the oral cavity and the maxillary sinus to prevent maxillary sinusitis. The buccal flap is suitable for closure of small and mesial defects and the FPB is suitable for closure of large posterior defects. A significant scientific contribution of this work is the follow-up that can be extended beyond 24 months. Other factors besides defect size, related to both the patient and the practitioner, are involved in the choice of treatment, but both techniques remain reliable, easy, and predictable options for CAO/OAF closure. The present case series was limited by the small number of patients and the authors recommend a study with larger groups.
Patient perspective
All patients were satisfied with the result after the treatment.
Funding sources
No sources funded this manuscript.
Ethical approval
All authors have read and complied with the journal's policy on ethical consent.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Registration of research studies
N/a.
Garantor
Asma Azzouzi
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Asma Azzouzi: Conceptualisation, Rédaction - Préparation du brouillon original, Rédaction - Révision et édition.
Lamiae Hallab: Méthodologie, Visualisation.
Saliha Chbicheb: Supervision, Validation.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
References
- 1.Kwon M.S., Lee B.S., Choi B.J., Lee J.W., Ohe J.Y., Jung J.H., et al. Closure of oroantral fistula: a review of local flap techniques. J. Korean Assoc. Oral Maxillofac. Surg. 2020;46:58–65. doi: 10.5125/jkaoms.2020.46.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mainassara Chekaraou S., Benjelloun L., El Harti K. Management of oro-antral fistula: two case reports and review. Ann. Med. Surg. (Lond.) 2021 Sep;4(69) doi: 10.1016/j.amsu.2021.102817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khandelwal P., Hajira N. Management of oro-antral communication and fistula: various surgical options. World J. Plast. Surg. 2017 Jan;6(1):3–8. PMID: 28289607; PMCID: PMC5339603. [PMC free article] [PubMed] [Google Scholar]
- 4.Gheisari R., Hosein Zadeh H., Tavanafar S. Oro-antral fistula repair with different surgical methods: a retrospective analysis of 147 cases. J. Dent. (Shiraz) 2019 Jun;20(2):107–112. doi: 10.30476/DENTJODS.2019.44920. PMID: 31214638; PMCID: PMC6538900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Watzak G., Tepper G., Zechner W., Monov G., Busenlechner D., Watzek G. Bony press-fit closure of oro-antral fistulas: a technique for pre-sinus lift repair and secondary closure. J. Oral Maxillofac. Surg. 2005 Sep;63(9):1288–1294. doi: 10.1016/j.joms.2005.05.299. PMID: 16122592. [DOI] [PubMed] [Google Scholar]
- 6.Procacci P., Alfonsi F., Tonelli P., Selvaggi F., Menchini Fabris G.B., Borgia V., De Santis D., Bertossi D., Nocini P.F. Surgical treatment of oroantral communications. J. Craniofac. Surg. 2016 Jul;27(5):1190–1196. doi: 10.1097/SCS.0000000000002706. PMID: 27300451. [DOI] [PubMed] [Google Scholar]
- 7.Borgonovo A.E., Berardinelli F.V., Favale M., Maiorana C. Surgical options in oro-antral fistula treatment. Open Dent. J. 2012;6:94–98. doi: 10.2174/1874210601206010094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levine M.H., Spivakovsky S. Low quality evidence for treatment approaches for oro-antral communications. Evid. Based Dent. 2017 Oct 27;18(3):90–91. doi: 10.1038/sj.ebd.6401260. PMID: 29075025. [DOI] [PubMed] [Google Scholar]
- 9.Kiran Kumar Krishanappa S., Eachempati P., Kumbargere Nagraj S., Shetty N.Y., Moe S., Aggarwal H., Mathew R.J. Interventions for treating oro-antral communications and fistulae due to dental procedures. Cochrane Database Syst. Rev. 2018 Aug 16;8(8) doi: 10.1002/14651858.CD011784.pub3. PMID: 30113083; PMCID: PMC6513579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agha R.A., Sohrabi C., Mathew G., Franchi T., Kerwan A., O'Neill N., for the PROCESS Group The PROCESS 2020 guideline: updating consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) guidelines. Int. J. Surg. 2020;84:231–235. doi: 10.1016/j.ijsu.2020.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Bhalla N., Sun F., Dym H. Management of oroantral communications. Oral Maxillofac. Surg. Clin. North Am. 2021 May;33(2):249–262. doi: 10.1016/j.coms.2021.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Kretzschmar D.P., Kretzschmar J.L. Rhinosinusitis: a review from a dental perspective. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003;962:128–135. doi: 10.1016/S1079-2104(03)00306-8. [DOI] [PubMed] [Google Scholar]
- 13.Parvini P., Obreja K., Begic A., Schwarz F., Becker J., Sader R., Salti L. Decision-making in closure of oroantral communication and fistula. Int. J. Implant Dent. 2019 Apr 1;5(1):13. doi: 10.1186/s40729-019-0165-7. PMID: 30931487; PMCID: PMC6441669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belmehdi A., El Harti K. Management of oroantral communication using buccal advanced flap. Pan Afr. Med. J. 2019 Oct;3(34):69. doi: 10.11604/pamj.2019.34.69.19959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borgonovo A.E., Berardinelli F.V., Favale M., Maiorana C. Surgical options in the treatment of oro-antral fistula. Open Dent. J. 2012;6:94–98. doi: 10.2174/1874210601206010094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rehrman A. Eine Methode zur Schliessung von Kieferhölenperforationen. Dtsch Zahnärztl Wschr. 1936;39:1136–1138. [Google Scholar]
- 17.Von Wowern N. Closure of an oro-antral fistula with buccal flap: Rehrmann versus Moczar. Oral Surg.Int. J. 1982;113:156–165. doi: 10.1016/s0300-9785(82)80003-3. [DOI] [PubMed] [Google Scholar]
- 18.Akerzoul N., Chbicheb S., El wady W. Surgical closure of Oro-Antral Fistula (OAF) using buccal fat pad graft: a case report and review of literature. Int. J. Oral Health Med. Res. 2015;2(1):32–35. [Google Scholar]
- 19.Môczáir L. Nuovo methodo operatiopela chisura delle fistole del seno mascellase di origina dentale. Stomatology (Rome) 1930:281087–281088. [Google Scholar]
- 20.Rathod N., et al. Use of the temporal extension of the buccal fat pad for closure of oro-antral communications. Int. J. Oral Maxillofac. Surg. 2021 doi: 10.1016/j.ijom.2021.02.030. [DOI] [PubMed] [Google Scholar]
- 21.Batra H., Jindal G., Kaur S. Evaluation of different treatment modalities for closure of oro-antral communications and formulation of a rational approach. J. Maxillofac. Oral Surg. 2010 Mar;9(1):13–18. doi: 10.1007/s12663-010-0006-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang S., Jee Y.J., Ryu D.M. Reconstruction of large oral-antral defects using a pedicled buccal fat pad. Maxillofac. Plast. Reconstr. Surg. 2018;40(1):7. doi: 10.1186/s40902-018-0144-6. Published April 5, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park J., Chun B.D., Kim U.K., Choi N.R., Choi H.S., Hwang D.S. Versatility of the pedicled buccal fat pad flap for the management of oro-antral fistula: a retrospective study of 25 cases. Maxillofac. Plast. Reconstr. Surg. 2019;41(1):50. doi: 10.1186/s40902-019-0229-x. Published November 25, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhalla N., Sun F., Dym H. Management of oroantral communications. Oral Maxillofac. Surg. Clin. North Am. 2021 May;33(2):249–262. doi: 10.1016/j.coms.2021.01.002. Epub 2021 Mar 5 PMID: 33685787. [DOI] [PubMed] [Google Scholar]
- 25.Scattarella A., Ballini A., Grassi F.R., Carbonara A., Ciccolella F., Dituri A., et al. Treatment of oro-antral fistula with autologous bone grafting and application of a non-resorbable membrane. Int. J. Med. Sci. 2010:7267–7271. doi: 10.7150/ijms.7.267. [DOI] [PMC free article] [PubMed] [Google Scholar]