Abstract
Background:
Transosseous tunnel (TO) repair is considered the gold standard for patellar tendon rupture; however, suture anchor (SA) repair has emerged as a viable alternative in recent years. Although both these techniques are used widely in clinical practice, the most biomechanically optimal construct for patellar tendon repair remains unknown.
Purpose:
To examine published studies on the biomechanical properties of TO and SA fixation for patellar tendon repair in terms of ultimate load to failure and cyclic gap formation. The null hypothesis was that there would be no significant difference in either outcome measure between the groups.
Study Design:
Systematic review.
Methods:
A systematic review using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines was performed by searching PubMed, the Cochrane Library, and Embase to identify studies that analyzed the biomechanical properties of SA and TO techniques for repair of a ruptured patellar tendon. The search phrase implemented was “patellar tendon repair.” Meta-analysis was performed to provide a quantitative comparison of the 2 techniques with regard to ultimate load to failure and cyclic gap displacement. Weighted averages were calculated for all quantitative outcomes, and outcomes were summarized in a forest plot. A random-effects model was used to account for the heterogeneity among the included studies in the final statistical analysis.
Results:
Of 875 studies initially screened, the inclusion criteria were met by 7 studies, including 128 cadaveric specimens (66 SA, 62 TO). The pooled analysis from 6 studies reporting on gap displacement revealed a statistically significant difference in favor of SA versus TO fixation (P < .001). Pooled analysis from 7 studies reporting on ultimate load to failure did not reveal a statistically significant difference between the use of SA and TO for tendon repair (P = .465).
Conclusion:
Our systematic review revealed that the use of SA fixation for patellar tendon repair was associated with lower cyclic gap displacement when compared with TO fixation. There was no significant difference in ultimate load to failure between the repair techniques.
Keywords: patellar tendon, biomechanics, suture anchor, transosseous tunnel
Patellar tendon ruptures are devastating injuries that can cause significant functional impairment attributed to disruption of the knee extensor mechanism. Rupture of the patellar tendon typically occurs in male patients aged <40 years and is caused by sudden quadriceps contraction with the knee in a flexed position, leading to tensile overload of the extensor mechanism. 13,19 Disruption of the patellar tendon most commonly occurs at the inferior pole of the patella but can also occur at the midsubstance of the tendon or as a distal avulsion from the tibial tubercle, though this is much less common in adults. 22
Complete tears of the patellar tendon necessitate operative intervention to restore function of the extensor mechanism. Although midsubstance tendon ruptures can be managed with end-to-end primary repair, ruptures at the osteotendinous junction at the inferior pole of the patella can be addressed with either a transosseous tunnel (TO) technique or suture anchor (SA) fixation. The standard TO repair technique entails drilling 3 vertical transpatellar tunnels from inferior to superior and utilizing a running locked Krackow stitch to tension and secure the patellar tendon to its anatomic footprint at the inferior pole of the patella. Alternatively, SA repair typically uses a similar technique for tendon suturing, though bony fixation is achieved with SAs placed at the inferior pole of the patella rather than TOs. Substantial variability in the material and size of anchors and sutures has been reported for each repair technique. 2,5,10,12,14,16,18
Although some clinical data have been presented in favor of SA fixation, 15 there is currently no consensus for the construct that confers the most optimal biomechanical properties. 2,5,10,12,14,16,18 Multiple biomechanical studies have examined the properties of TO versus SA fixation for patellar tendon repair, with conflicting results. The purpose of this study was to conduct a systematic review of the literature to evaluate the biomechanical properties of TO versus SA fixation for patellar tendon repair. The null hypothesis was that there would be no difference in ultimate load to failure or cyclic gap displacement between the TO and SA techniques.
Methods
A systematic review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. A search of the PubMed, Embase, and Cochrane Library databases was conducted up to October 29, 2021. The electronic search string was “patellar tendon repair.” Cadaveric studies were included that assessed the biomechanics of patellar tendon repair with SA versus TO fixation. Studies were excluded if they focused on the repair of other tendons (eg, quadriceps tendon) or if they evaluated techniques other than isolated SA or TO tunnel fixation (ie, construct augmentation with additional materials such as cable wire or polydioxanone suture cord augmentation). Clinical studies and studies not published in the English language were also excluded. Duplicate articles were subsequently filtered and removed. Published articles were identified and reviewed in a blinded fashion by 2 reviewers (C.I., S.S.) to assess study eligibility. In cases of discrepancy between reviewers, the senior author (H.G.) served as the final determination of study eligibility. Data extraction from each study was performed independently by 1 reviewer and then reexamined for accuracy by a separate reviewer. There was no need for funding or a third party to obtain any of the collected data.
The Quality Appraisal for Cadaveric Studies (QUACS) scale was used to evaluate cadaveric study methodology quality. 21 The scale consists of a checklist encompassing 13 items. Each is scored with either 0 points (no/not stated) or 1 point (yes/present). Points are assigned only if a criterion is met without any doubt, and a final percentage is given as the total score. Scores >75% are considered satisfactory.
Study outcomes were biomechanical, including ultimate load to failure (N) and cyclic gap formation (N/mm). When standard deviations were absent and only standard errors were reported, standard deviations were computed utilizing the methodology described in the Cochrane Handbook for Systematic Reviews of Interventions (Version 6.2.0). Weighted averages were calculated for all quantitative outcomes. The outcomes were summarized in a forest plot when data from ≥2 studies were available. Using a random-effects model, standardized mean differences with 95% CIs were calculated and embedded within the forest plot. A random-effects model was used to account for the heterogeneity among the included studies in the final statistical analysis. The degree of heterogeneity attributed to between-study characteristics was quantified using the I 2 statistic. Meta-analysis statistics and generation of forest plots figures were performed using OpenMetaAnalyst, which implements metaphor R console code.
Results
A total of 875 studies were screened by title and abstract to determine study eligibility based on the predefined criteria (Figure 1). Seven studies 2,5,10,12,14,16,18 with a total of 128 cadaveric specimens undergoing patellar tendon repair (66 SA, 62 TO) met the study criteria and were included for analysis (Table 1). Five studies 2,5,12,14,16 cited the mean ± SD cadaver age, which was 64.1 ± 6.1 years. One study did not note the mean cadaver age, 18 and 1 study utilized porcine specimens rather than human cadavers. 10 This animal study was part of the analysis because porcine models are commonly used in musculoskeletal biomechanics research, and porcine tendons have similar load characteristics to human tendons. 1 In all studies, the patellar tendon was transected at or near the inferior pole of the patella.
Figure 1.
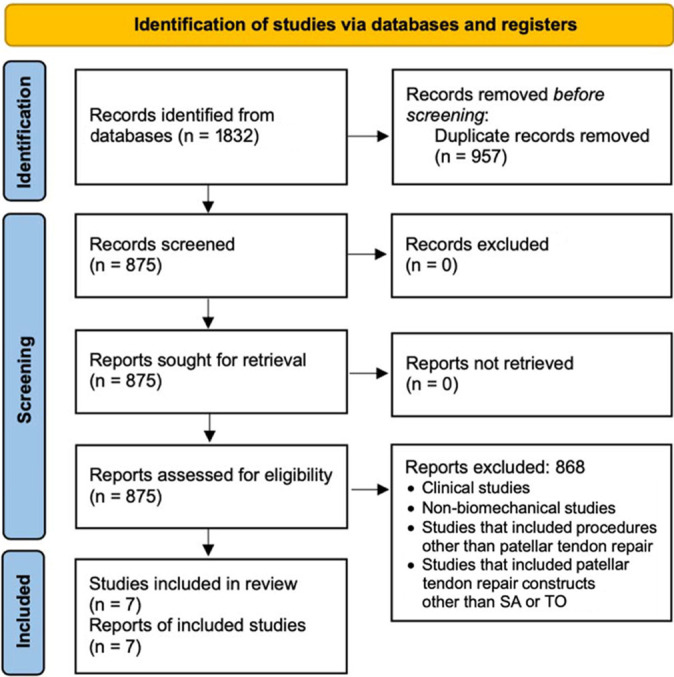
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram. SA, suture anchor; TO, transosseous tunnel.
Table 1.
Specimens and Fixation Details of Included Studies a
| Lead Author (Year) | Sample Size | Cadaver Age, y b | SA Fixation | TO Fixation |
|---|---|---|---|---|
| Bushnell (2006) 2 | 18: 6 SA, 6 TO Ethibond, 6 TO FiberWire | 74 (59-68) | Two 5.0-mm corkscrew titanium anchors with FiberWire sutures | Three tunnels drilled, fixed with Ethibond or FiberWire suture |
| Ettinger (2013) 5 | 30: 10 titanium SA, 10 hydroxyapatite SA, 10 TO | 60 ± 11 | Two 5.5-mm anchors, titanium or hydroxyapatite, with Ultrabraid sutures | Three tunnels drilled, fixed with Ultrabraid suture |
| O’Donnell (2021) 14 | 10: 5 SA, 5 TO | 58.4 ± 22 | Two 5.0-mm titanium anchors with Ultrabraid sutures | Three tunnels drilled, fixed with Ultrabraid suture |
| Lanzi (2016) 10 | 24: 12 SA, 12 TO | Porcine specimens | Two 4.75-mm PEEK anchors with FiberWire sutures | Three tunnels drilled, fixed with FiberWire suture |
| Sherman (2019) 18 | 12: 6 SA, 6 TO | Not reported | Three double-loaded 4.5-mm biocomposite Corkscrew anchors with FiberWire sutures | Three tunnels drilled, fixed with FiberWire suture |
| Massey (2020) 12 | 20: 10 SA, 10 TO | 63.8 ± 8 | Two 4.75-mm biocomposite SwiveLock knotless suture anchors with suture tape | Three tunnels drilled, fixed with FiberWire suture |
| Ode (2016) 16 | 14: 7 SA, 7 TO | 64.3 (43-73) | Two 5.5-mm corkscrew PEEK anchors with FiberWire sutures | Three tunnels drilled, fixed with FiberWire suture |
a Manufacturers: Ethibond suture (Johnson & Johnson Medical Devices), FiberWire suture (Arthrex), Ultrabraid suture (Smith & Nephew), SwiveLock anchor (Arthrex), Corkscrew anchor (Arthrex). PEEK, polyetheretherketone; SA, suture anchor; TO, transosseous tunnel.
b Mean ± SD (range).
Ultimate load to failure (N) was reported in all 7 studies, whereas cyclic gap formation (N/mm) was noted in 6 studies. 2,5,10,12,14,18 Ode et al 16 reported gap formation results as a graphical representation but did not provide numerical values; therefore, these data could not be included in the meta-analysis. Although there was some variation among studies in terms of the methodology used for load-to-failure testing, the ultimate load to failure was consistently assessed after the evaluation of cyclic gap formation in all studies. Gap formation (N/mm) was recorded after at least 250 cycles in each study. Five studies 2,5,12,14,18 indicated data for gap formation at 250 cycles, whereas 1 study 10 examined gap formation data after 1000 cycles.
Methodologic Quality Assessment
The risk of bias and methodologic quality of the studies were assessed using the QUACS scale, 21 which was previously validated. The mean QUACS score was 80.2% (range, 76.9-84.6%). All 7 studies satisfied the threshold for a satisfactory level of methodologic quality (>75%) (Table 2).
Table 2.
QUACS Scores of the Included Studies a
| Study | QUACS Score, % |
|---|---|
| Bushnell (2006) 2 | 84.6 |
| Ettinger (2013) 5 | 76.9 |
| O’Donnell (2021) 14 | 84.6 |
| Lanzi (2016) 10 | 76.9 |
| Sherman (2019) 18 | 76.9 |
| Massey (2020) 12 | 76.9 |
| Ode (2016) 16 | 84.6 |
a Scores >75% are considered satisfactory. QUACS, Quality Appraisal for Cadaveric Studies.
Surgical Technique
Transosseous Fixation
All 7 studies implemented a similar surgical technique for TO fixation. Three vertical tunnels were drilled from inferior to superior, dividing the patella into equal quarters. Each study utilized the standard Krackow locking whipstitch technique to secure the tendon after appropriate tensioning. 8 Four studies 10,12,16,18 utilized No. 2 FiberWire sutures (Arthrex); 1 study 2 tested No. 5 Ethibond (Johnson & Johnson Medical Devices) and No. 2 FiberWire suture; and 2 studies 5,14 used No. 2 Ultrabraid sutures (Smith & Nephew). Sutures were passed through the transpatellar tunnels and tied at the superior pole of the patella.
SA Fixation
SA fixation for patellar tendon repair implemented a similar technique for tendon suturing. However, instead of passing the suture through transpatellar tunnels, SAs were fixed at the inferior patellar pole, securing the tendon to its native anatomic footprint. This technique entailed predrilling and/or tapping into the distal aspect of the patella and placing anchors with their accompanying sutures into the holes. Six studies 2,5,10,12,14,16 utilized 2 SAs for fixation, whereas 1 study 18 used 3 anchors. For studies utilizing 2 SAs, the anchors were placed just medial and just lateral to the center of the inferior pole, dividing the patella into approximately equal thirds. When 3 SAs were used, the anchors were placed in central, medial, and lateral locations, dividing the patella into quarters. 18 In 6 studies, 5,10,12,14,16,18 the sutures were affixed to the patellar tendon using the standard Krackow whipstitch method. 8 In 1 study, 2 the sutures were secured to the patellar tendon using a modified Mason-Allen technique. 2,11 Three studies 2,5,14 used titanium, while 2 studies 10,16 each used polyetheretherketone and biocomposite anchors. 12,18 One study 5 tested 2 groups separately with titanium and hydroxyapatite anchors. In terms of types of suture used, 4 studies 2,10,16,18 used anchors with No. 2 FiberWire sutures; 2 studies 5,14 used anchors with No. 2 Ultrabraid sutures; and 1 study 12 used knotless SAs and a single 2-mm suture tape (Arthrex) with 2 core sutures.
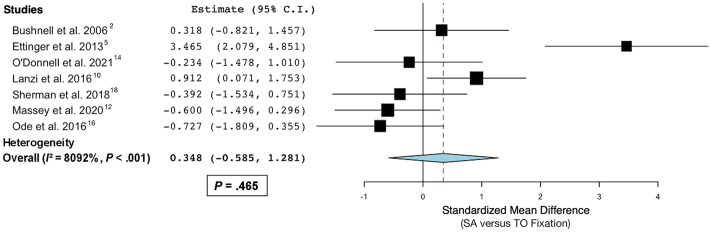
Ultimate Load to Failure
All studies evaluated ultimate load to failure of the patellar tendon repair construct. Two studies 5,10 concluded that SA fixation demonstrated higher ultimate load to failure than TO fixation, while the remaining 5 studies 2,12,14,16,18 concluded that there was no significant difference between the groups. The pooled analysis from 7 studies on ultimate load to failure did not reveal a statistically significant difference between SA and TO fixation (P = .465) (Figure 2).
Figure 2.
Forest plot demonstrating a standardized mean difference of ultimate load to failure between suture anchor (SA) and transosseous tunnel (TO) fixation for patellar tendon repair.
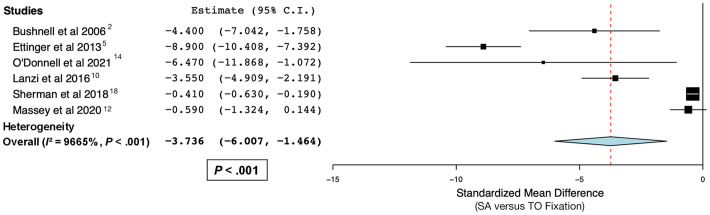
Gap Formation
Six studies evaluated gap formation of the patellar tendon repair construct and provided numerical data for inclusion in the meta-analysis. 2,5,10,12,14,18 These 6 studies concluded that SA fixation yielded less gap formation than TO fixation. The pooled analysis from 6 studies on gap formation revealed a statistically significant difference in favor of SA versus TO fixation for patellar tendon repair (P < .001) (Figure 3).
Figure 3.
Forest plot demonstrating a standardized mean difference of gap formation in favor of suture anchor (SA) vs transosseous tunnel (TO) fixation for patellar tendon repair.
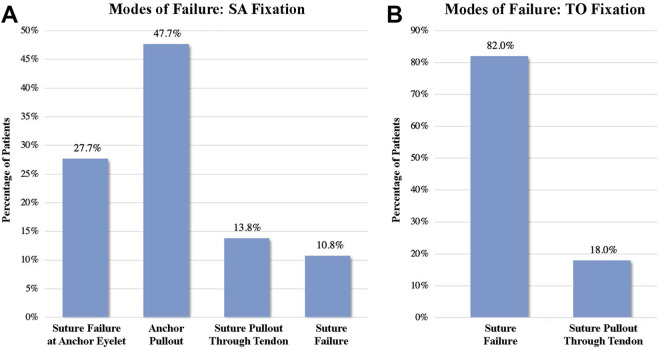
Mode of Failure
All 7 studies reported the mode of failure of each specimen in the SA and TO fixation groups. For the SA fixation group (n = 65), failure occurred by anchor pullout from bone (47.7%), suture failure at anchor eyelet (27.7%), suture pullout through tendon (13.8%), or suture failure/breakage (10.8%) (Figure 4A). For the TO fixation group (n = 61), failure occurred by suture failure (82%) or suture pullout through the tendon (18%) (Figure 4B).
Figure 4.
Modes of failure of the fixation groups: (A) suture anchor (SA) and (B) transosseous tunnel (TO).
Discussion
Upon evaluating the current literature for biomechanical properties of SA and TO fixation for patellar tendon repair, our findings suggest that SA fixation exhibits decreased cyclic gap formation when compared with TO fixation (P < .001), with no significant difference in ultimate load to failure found between the groups (P = .465).
Clinical outcomes after repair of acute patellar tendon rupture have typically been reported in small cohorts of patients, with failure rates ranging from 0% to 21%. 3,6,7,15,19 Thus, it is worthwhile to evaluate the biomechanical properties of various fixation constructs in an attempt to optimize a patellar tendon repair technique and maximize the chances for a successful outcome. A multitude of operative techniques have been described in the literature, including primary repair with the TO or SA technique as described in the current review, in addition to augmentation of repair constructs with cerclage wire, Dall-Miles cable, autografts, allografts, or synthetic grafts. 4,6 Within the context of comparing SA and TO fixation for patellar tendon repair, O’Dowd et al 15 presented clinical results from a retrospective review of 361 patients. SA repair demonstrated a significant decrease in rerupture rate as compared with TO repair, with no significant differences in overall reoperation rate or infection rate between the groups. This is the largest published study comparing SA and TO patellar tendon repair, and no randomized clinical trials have been conducted comparing the 2 groups thus far.
The clinical results from the study by O’Dowd et al 15 are consistent with the biomechanical findings from the current meta-analysis. SA fixation confers decreased gap formation, which may in turn decrease failure rate, as was shown to be the case clinically. 9,17 Notably, it has been reported in the literature that patellar tendon gap formation of 3 to 5 mm is consistent with clinical failure. 9,17 The favorable gap formation properties of the SA fixation construct may be attributable to the stiffness of anchor fixation relative to suture fixation, although this metric was used in only 1 study, 12 which demonstrated no significant difference. Interestingly, the current biomechanical analysis did not reveal a difference in ultimate load to failure between SA and TO repair, despite a clinical difference in rerupture rate, as shown in the literature.
Another important consideration is the mode of failure of each construct. While TO repair can fail by either suture breakage or suture cutting through the tendon, SA fixation can additionally fail by anchor pullout, suture failure at the anchor eyelet, or, rarely, patellar fracture during insertion of the anchor. 2,5,16 This study found that for TO repair, the majority of specimens failed via suture breakage, while the most common mode of failure for the SA repair group was anchor pullout. While the clinical results by O’Dowd et al 15 were very informative, the mode of failure by which each rerupture occurred was not noted for either group.
In a clinical setting, SA fixation for patellar tendon repair necessitates less dissection and results in a shorter operating time for surgeons. 12 Coupled with the decreased rerupture rate shown clinically 15 and the favorable gap formation shown biomechanically, it can be considered that SA fixation may be more optimal for patellar tendon repair than for TO fixation. However, randomized controlled trials should be conducted to more rigorously evaluate the difference in outcomes between the groups.
Limitations
A limitation of this review was that only 7 studies were included; this may suggest that some of the conclusions drawn herein are not adequately powered. Additionally, the surgical techniques of SA and TO patellar tendon repair, while similar, were not identical across all studies, making direct comparison difficult. Furthermore, the techniques by which ultimate load to failure and gap formation were evaluated exhibited a degree of heterogeneity among studies; therefore, the results and our concomitant conclusions should be interpreted with caution. Additionally, cadaveric bone density must be taken into consideration, particularly for the SA groups, as SA fixation quality may be limited in lower density bone. 20 While 2 studies reported bone density parameters, 12,16 there were not enough available data to factor this into our analysis.
Conclusion
Our systematic review revealed that the use of SA fixation results in decreased cyclic gap formation when compared with TO repair, with no significant difference in ultimate load to failure between the groups. These findings may have meaningful clinical implications, coinciding with existing clinical data demonstrating a decreased failure rate for SA repair in comparison with TO repair for patellar tendon rupture.
Footnotes
Final revision submitted March 21, 2022; accepted June 6, 2022.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Bonney H, Colston BJ, Goodman AM. Regional variation in the mechanical properties of cortical bone from the porcine femur. Med Eng Phys. 2011;33(4):513–520. [DOI] [PubMed] [Google Scholar]
- 2. Bushnell BD, Byram IR, Weinhold PS, Creighton RA. The use of suture anchors in repair of the ruptured patellar tendon: a biomechanical study. Am J Sports Med. 2006;34(9):1492–1499. [DOI] [PubMed] [Google Scholar]
- 3. Bushnell BD, Tennant JN, Rubright JH, Creighton RA. Repair of patellar tendon rupture using suture anchors. J Knee Surg. 2008;21(2):122–129. [DOI] [PubMed] [Google Scholar]
- 4. Core M, Anract P, Raffin J, Biau DJ. Traumatic patellar tendon rupture repair using synthetic ligament augmentation. J Knee Surg. 2020;33(8):804–809. [DOI] [PubMed] [Google Scholar]
- 5. Ettinger M, Dratzidis A, Hurschler C, et al. Biomechanical properties of suture anchor repair compared with transosseous sutures in patellar tendon ruptures: a cadaveric study. Am J Sports Med. 2013;41(11):2540–2544. [DOI] [PubMed] [Google Scholar]
- 6. Gilmore JH, Clayton-Smith ZJ, Aguilar M, Pneumaticos SG, Giannoudis PV. Reconstruction techniques and clinical results of patellar tendon ruptures: evidence today. Knee. 2015;22(3):148–155. [DOI] [PubMed] [Google Scholar]
- 7. Kasten P, Schewe B, Maurer F, Gösling T, Krettek C, Weise K. Rupture of the patellar tendon: a review of 68 cases and a retrospective study of 29 ruptures comparing two methods of augmentation. Arch Orthop Trauma Surg. 2001;121(10):578–582. [DOI] [PubMed] [Google Scholar]
- 8. Krackow KA, Thomas SC, Jones LC. A new stitch for ligament-tendon fixation: brief note. J Bone Joint Surg Am. 1986;68(5):764–766. [PubMed] [Google Scholar]
- 9. Krushinski EM, Parks BG, Hinton RY. Gap formation in transpatellar patellar tendon repair: pretensioning Krackow sutures versus standard repair in a cadaver model. Am J Sports Med. 2010;38(1):171–175. [DOI] [PubMed] [Google Scholar]
- 10. Lanzi JT, Jr, Felix J, Tucker CJ, et al. Comparison of the suture anchor and transosseous techniques for patellar tendon repair: a biomechanical study. Am J Sports Med. 2016;44(8):2076–2080. [DOI] [PubMed] [Google Scholar]
- 11. Lee BG, Cho NS, Rhee YG. Modified Mason-Allen suture bridge technique: a new suture bridge technique with improved tissue holding by the modified Mason-Allen stitch. Clin Orthop Surg. 2012;4(3):242–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Massey PA, Myers M, McClary K, Brown J, Barton RS, Solitro GF. Biomechanical analysis of patellar tendon repair with knotless suture anchor tape versus transosseous suture. Orthop J Sports Med. 2020;8(10):2325967120954808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Matava MJ. Patellar tendon ruptures. J Am Acad Orthop Surg. 1996;4(6):287–296. [DOI] [PubMed] [Google Scholar]
- 14. O’Donnell R, Lemme NJ, Marcaccio S, et al. Suture anchor versus transosseous tunnel repair for inferior pole patellar fractures treated with partial patellectomy and tendon advancement: a biomechanical study. Orthop J Sports Med. 2021;9(8):23259671211022245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. O’Dowd JA, Lehoang DM, Butler RR, Dewitt DO, Mirzayan R. Operative treatment of acute patellar tendon ruptures. Am J Sports Med. 2020;48(11):2686–2691. [DOI] [PubMed] [Google Scholar]
- 16. Ode GE, Piasecki DP, Habet NA, Peindl RD. Cortical button fixation: a better patellar tendon repair? Am J Sports Med. 2016;44(10):2622–2628. [DOI] [PubMed] [Google Scholar]
- 17. Ravalin RV, Mazzocca AD, Grady-Benson JC, Nissen CW, Adams DJ. Biomechanical comparison of patellar tendon repairs in a cadaver model: an evaluation of gap formation at the repair site with cyclic loading. Am J Sports Med. 2002;30(4):469–473. [DOI] [PubMed] [Google Scholar]
- 18. Sherman SL, Black B, Mooberry MA, et al. Biomechanical evaluation of suture anchor versus transosseous tunnel patellar tendon repair techniques. J Knee Surg. 2019;32(8):825–832. [DOI] [PubMed] [Google Scholar]
- 19. Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am. 1981;63(6):932–937. [PubMed] [Google Scholar]
- 20. Volk WR, Yagnik GP, Uribe JW. Complications in brief: quadriceps and patellar tendon tears. Clin Orthop Relat Res. 2014;472(3):1050–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wilke J, Krause F, Niederer D, et al. Appraising the methodological quality of cadaveric studies: validation of the QUACS scale. J Anat. 2015;226(5):440–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yousef MAA. Combined avulsion fracture of the tibial tubercle and patellar tendon rupture in pediatric population: case series and review of literature. Eur J Orthop Surg Traumatol. 2018;28(2):317–323. [DOI] [PubMed] [Google Scholar]