Abstract
We present a single centre study describing the effect of awake prone position (PP) on oxygenation and clinical outcomes in spontaneously breathing patients with novel coronavirus disease (COVID-19). Between 1st March and 30th April 2020, forty eight of 138 patients managed outside of the critical care unit with facemask oxygen, high flow nasal oxygen (HFNO) or continuous positive airway pressure (CPAP), underwent PP. Prone position was associated with significant improvement in oxygenation, lower ICU admission, tracheal intubation, and shorter ICU length of stay. Lack of response to PP may be an indicator of treatment failure, requiring early escalation.
Keywords: Novel coronavirus disease 2019 (COVID-19), acute respiratory distress syndrome (ARDS), prone positioning (PP), Viral pneumonia, noninvasive ventilation
Introduction
The novel coronavirus disease (COVID-19) pandemic has generated significant pressures on capacity on intensive care units (ICUs), 1 resulting in many patients managed with high flow nasal oxygen (HFNO) and continuous positive airway pressure (CPAP) on general wards. Prone position in managing such patients was suggested in early publications from China. 2 Whilst it is clear that prone position improves oxygenation and is associated with lower mortality in mechanically ventilated patients, 3 , 4 very few studies have investigated the feasibility, safety and effectiveness of early application of prone position (PP) in awake non-intubated patients outside of the ICU. 5 , 6 We carried out a cohort study in hypoxaemic patients with respiratory failure due to COVID-19 to evaluate these, and report on patient centered outcomes.
Methods
This was a prospective, single centre cohort study at the Royal London Hospital (London, UK) between 1st March and 30th April 2020, with local Ethics approval. Verbal informed consent was obtained from each patient and data collected as part of the usual clinical care provided by the critical care outreach team (CCOT). All patients were considered for PP while being managed on general medical wards with face mask oxygen, HFNO or CPAP. Proned patients remained proned for as long as tolerated. Respiratory indices were monitored hourly and care escalated to critical care as required.
The effects of PP on oxygenation were described as change in ratio of arterial oxygen partial pressure (PaO2) to fraction of inspired oxygen (P/F ratio), and ratio of the peripheral capillary oxygen saturation (sats) to fraction of inspired oxygen (S/F ratio). Changes in respiratory rate, and work of breathing were evaluated pre, during and post pronation. Work of breathing was defined as visible vigorous breathing efforts produced by all respiratory muscles. Shortness of breath (SOB), the subjective experience of difficulty breathing, was self-reported by patients in a binary manner (yes/no). ICU admission, endotracheal intubation, ICU and hospital length of stay (LOS), secondary COVID-19 complications and 90-day mortality were also recorded.
Two-tailed Student’s t-test, analysis of variance (ANOVA) and chi-square or Fisher’s exact test were used for statistical analysis.
Results
From 138 patients enrolled, 46 patients were proned (PP). Reasons for not proning were patient confusion (37%), refusal/discomfort (14%), language (14%), high BMI (11%), need for intubation (n = 12, 13), or cardiovascular instability (n = 2, 3%).
The Table 1 shows the demographics of proned patients. Twelve patients (26%) could not tolerate PP longer than one hour. The remaining patients (n = 34, 74%) tolerated PP with a median time of 5 hours per session, and a frequency of 1 to 6 times per day. There were no differences in demographics or severity markers between the two groups.
Table 1.
Outcomes in the subgroups of PP patients who tolerated PP for >1 hour and those who were unable to (PP ≤ 1 h). The laboratory results refer to the time of first review by the Critical Care Outreach Team.
| Variables | PP ≤ 1h (n = 12) | PP > 1 h (n = 34) | |
|---|---|---|---|
| Age | 56 (30–79) | 56 (22–77) | p = 0.972 |
| SAPS (median, IQR) | 27 (12–38) | 25 (12–33) | p = 0.088 |
| CFS (median, IQR) | 2 (1–5) | 2 (1–4) | p = 0.084 |
| S/F ratio | |||
| – Pre | 146 (89–163) | 140 (92–249) | p = 0.666 |
| – During | 176 (135–248) | 185 (118–286) | p = 0.376 |
| – Post | 172 (118–277) | 189 (116–330) | p = 0.274 |
| Laboratory results (median, IQR) | |||
| – CRP mg/L | 176 (32–280) | 147 (41–324) | p = 0.630 |
| – Ferritin ng/mL | 7551 (489–28899) | 2373 (194–20357) | p = 0.087 |
| – D-dimer µg/mL | 16.3 (0.3–80) | 2.2 (0.4–16.2) | p = 0.213 |
| – Creatinine umol/L | 74 (40–165) | 70 (38–403) | p = 0.170 |
| ICU admission (number, %) | 10 (83) | 14 (41) | p = 0.011a |
| Intubation (number, %) | 10 (83) | 10 (29) | p = 0.001a |
| – ≤ 24 h | 0 | 2 (9) | p = 0.002a |
| ICU LOS (median, IQR) | 13 (5–26) | 5 (3–18) | p = 0.016a |
| Hospital LOS (median, IQR | 18 (6–34) | 13 (2–25) | p = 0.102 |
| 90-day mortality (number, %) | 5 (42) | 9 (26) | p = 0.325 |
CFS: Clinical Frailty Score; CRP: C-reactive protein; LOS: length of stay; SAPS II: Simplified Acute Physiology Score II; PP: prone position.
aStatistically significant.
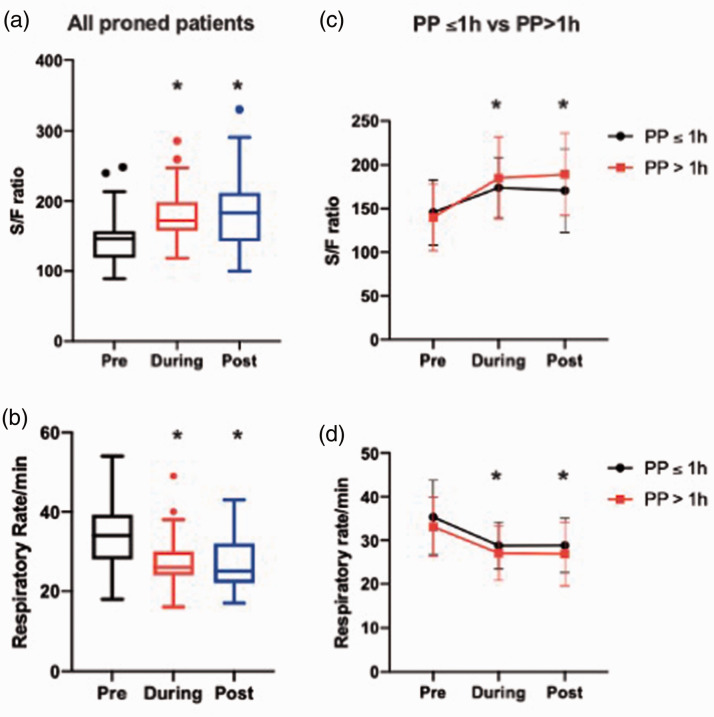
The majority of patients received HFNO prior to proning (n = 30), while the rest were on facemask O2 and moved to HFNO. Most patients were managed with HFNO after. Prone position resulted in significant improvement in oxygenation: P/F ratio (pre: 115 ± 43 mmHg vs post: 148 ± 70 mmHg, p = 0.025) and S/F ratio (pre: 141 ± 37 vs post: 188 ± 49, p < 0.001) (see Figure 1). Patients also had lower respiratory rate (RR) (pre: 34 ± 7 vs post: 25 ± 7 breaths per minute, p < 0.001), with lower work of breathing (WOB) (pre: 43 vs post: 16) and improvements in reported shortness of breath after PP (pre: 45 vs post: 19, p < 0.001). Changes were independent of oxygen delivery method.
Figure 1.
(a,b) Median and IQR for S/F ratio and respiratory rate among proned patients (PP) with COVID-19 respiratory failure. The values refer to PRE (1–2 hours before pronation), DURING, and POST (1–4 hours) after supination. (c,d) Changes in oxygenation and respiratory rate in proned patients who were able to tolerate PP for ≤1 hour and those able to tolerate >1 hour (mean ± SD). *denotes statistical significance (p < 0.0001 one-way ANOVA repeated measures for changes seen during proning and post supination compared to pre values).
Patients tolerating PP >1 hour had lower ICU admissions compared to those who were unable to tolerate proning for 1 h (PP ≤ 1h: 83% vs PP> 1 h: 41%, p = 0.011), required less invasive ventilation (PP ≤ 1h: 83% vs PP > 1h: 29%, p = 0.001), and had shorter median ICU length of stay (LOS) (PP ≤ 1h: 13 (5–26) vs PP > 1h: 5 (3–18) days, p = 0.016). But no difference in the hospital LOS or 90-day mortality rate. No adverse events of prone position were observed.
Discussion
Awake PP is safe and results in improved oxygenation and work of breathing in awake spontaneously breathing patients with COVID-19. PP was also associated with lower ICU admission and tracheal intubation. This effect was more pronounced in patients who were able to tolerate PP for longer than 1 hour, a finding which persisted after adjustment for age and pre-proning S/F ratio. The improvement in oxygenation and work of breathing was consistent with all modes of oxygen delivery (CPAP, HFNO and facemask).
Our findings in this small study are in keeping with other smaller observational studies that have shown the applicability of PP in conscious patients with ARDS and COVID-19.7–9 Whilst most studies have mainly shown improvement in oxygenation, our study showed that patients who were able to tolerate PP for more than 1 hour had less admission to ICU, reduced need for intubation and mechanical ventilation, and shorter ICU length of stay. This may be due to time-dependent effect of proning, 10 and/or may be an indicator of disease severity. Prone position could therefore be considered an early treatment and triage tool as part of a clinical algorithm for managing patients with COVID-19.
Acknowledgement
We would like to thank the Critical Care Outreach Team (Critical Care Department of the Royal London Hospital) and all the nursing staff and medical team for their hard work and support of patients throughout this study. Ann McGinley, Dr Julia Hadley and Professor Rupert Pearse reviewed the research proposal and supported the study locally. The Critical Care Outreach Team (Simon Nourse, Amanda Thomas, Alan Hurding, Siobhan O’Mahoney, Baldish Kaur, David Kirkpatrick, Ildiko Papp, Jane Ewing, Elizabeth Oteka) supported collection of data, provided training and clinical support to the nursing and medical team on the ward. Sr Ann McGinley, Dr Julia Hadley and Professor Rupert Pearse approved and supported the study locally. The Critical Care Outreach Team (Simon Nourse, Amanda Thomas, Alan Hurding, Siobhan O’Mahoney, Baldish Kaur, David Kirkpatrick, Ildiko Papp, Jane Ewing, Elizabeth Oteka) supported collection of data, provided training and clinical support to the nursing and medical team on the ward. Professor Rupert Pearse reviewed the manuscript.
Footnotes
Ethical approval: Ethical approval was granted by the Ethics Committee and the Barts life Science Data Committee of the Royal London Hospital, Barts Health NHS Trust.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Brigitta Fazzini https://orcid.org/0000-0003-3569-1203
Parjam Zolfaghari https://orcid.org/0000-0001-8700-2620
References
- 1.House N, Holborn H, Wc L. ICNARC report on COVID-19 in critical care. ICNARC Case Mix Programme database 22 May 2020.
- 2.Sun Q, Qiu H, Huang M, et al. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu province. Ann Intensive Care 2020; 10: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scaravilli V, Grasselli G, Castagna L, et al. Prone positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective study. J Crit Care 2015; 30: 1390–1394. [DOI] [PubMed] [Google Scholar]
- 4.Ding L, Wang L, Ma W, et al. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit Care 2020; 24: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sartini C, Tresoldi M, Scarpellini P, et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA 2020; 323: 2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elharrar X, Trigui Y, Dols A-M, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA 2020; 323: 2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Telias I, Katira BH, Brochard L. Is the prone position helpful during spontaneous breathing in patients with COVID-19? JAMA 2020; 323: 2265–2267. [DOI] [PubMed] [Google Scholar]
- 8.Ferrando C, Mellado-Artigas R, Gea A, et al.; COVID-19 Spanish ICU Network. For the COVID-19 Spanish ICU network. Awake prone positioning does not reduce the risk of intubation in COVID-19 treated with high-flow nasal oxygen therapy: a multicenter, adjusted cohort study. Crit Care 2020; 24: 597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly NL, Curtis A, Douthwaite S, et al. Effect of awake prone positioning in hypoxaemic adult patients with COVID-19. J Intensiv Care Soc. Epub ahead of print 24 September 2020. DOI:10.1177/1751143720961244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reutershan J, Schmitt A, Dietz K, et al. Alveolar recruitment during prone position: time matters. Clin Sci (Lond) 2006; 110: 655–663. [DOI] [PubMed] [Google Scholar]