Abstract
Objective
Previous studies highlighted a high prevalence of mental health issues among students during the COVID-19 pandemic, but there is no evidence from Russia. This study was aimed to examine the prevalence of somatic and psychological distress among Russian university students.
Method
The cross-sectional study was conducted in March-April 2021. The participants were university students from several regions of Russia (N = 1236). The Patient Health Questionnaire-15 and Depression, Anxiety, and Stress Scales-21 were used to measure the somatic and psychological distress.
Results
The prevalence of somatic burden, depression, anxiety, and stress was 72.2%, 54.7%, 63.4%, and 55.4%, respectively. Somatic burden, anxiety, and stress were more frequently observed in females and students with experience of COVID-19 disease compared to males and students without experience of COVID-19 disease.
Conclusions
These data illuminate the high prevalence and potential risk factors for somatic and psychological distress among Russian university students and determine the importance of psychoeducation and preventive measures in the Russian university environment.
Keywords: somatic burden, psychological distress, COVID-19 pandemic, psychosomatic medicine, Russian university students
Introduction
After the COVID-19 pandemic was announced in March 2020, governments around the world developed measures to prevent the SARS-CoV-2 infection. The strictest preventive measures applied to older persons, who had a higher risk of a severe or even mortal course of the disease. In further studies, younger age and student status were found to be risk factors for COVID-19-related stress.1-3 Many students were concerned about finances, future academic and career prospects,4 worried about their family health status and their learning assignments,5 showed low online learning satisfaction with poor self-efficacy, general anxiety, and fear of COVID-19.6 This prompted researchers to examine the impact of the pandemic on mental health among college and university students.
Numerous studies showed a high prevalence of mental health issues among students in various countries. In Italy, university students experienced moderate to severe levels of anxiety, depressive, and obsessive-compulsive symptomatology while 14% of them met the criteria for at least 1 mental health disorder.7 In an online survey in the France, 43% of university students had possible depressive symptoms and 39% had probable anxiety symptoms.8 Similar findings were obtained among 50% of UK university students with clinically significant anxiety and depressive symptoms.9 In cross-cultural comparisons, 72% of Czech college students reported somatic symptoms, 40% anxiety, and 52% depression, which was similar to 70% of Slovak college students complaining about somatic symptoms, 35% anxiety, and 47% depression.10 The incidence of somatic symptoms among Chinese college students was 35%, compared to 2% for primary school students,11 highlighting the serious impact of the COVID-19 pandemic on persons in adolescence and early adulthood.
In Russia, the pandemic also had a negative impact on the mental health of university students. Compared to the long period onset of the pandemic, students reported greater levels of depression, anxiety, and stress in the early days of the spread of COVID-19 in Russia and in the period before the implementation of containment measures.12 However, the prevalence of somatic and psychological distress among Russian university students is still unknown, despite evidence that during the pandemic, depressive symptoms are more pronounced among Russians than among Italians, Germans, and Spaniards.13
We aimed to examine the prevalence of somatic and psychological distress among Russian university students. This study expands previous findings and contributes to knowledge about student mental health during the COVID-19 pandemic.
Methods
Participants and procedure
The study population consisted of 1236 Russian university students. Participants were predominantly female (71.9%) and experienced COVID-19 disease (50.7%). The mean age of the sample was 19.57 (SD = 2.13).
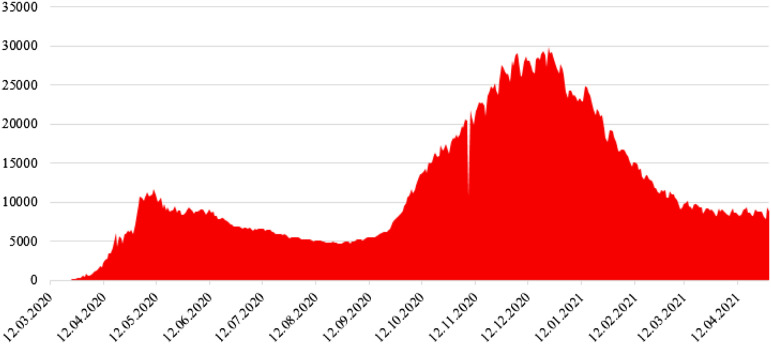
The data were collected in March-April 2021 after the Russian university students left the distance learning format. At this time there was a relative decline in the incidence of the SARS-CoV-2 infection in Russia (Figure 1). University employees announced opportunities for students to participate in this study. Students who responded to the announcement were invited into classrooms where they were given pens and paper versions of the questionnaire. All volunteers were not limited in time to complete the questionnaire, gave written informed consent, and received academic bonuses for participating in this study.
Figure 1.
Incidence of the SARS-CoV-2 infection in Russia from March 12, 2020 to April 30, 2021.
Instruments
Patient health questionnaire-15
The Patient Health Questionnaire-15 (PHQ-15) is a 15-item self-report measure assessing somatic burden via the list of symptoms (eg, stomach pain, chest pain, dizziness, heart pound or race, shortness of breath, trouble sleeping). Respondents rate their distress for each symptom on a scale from 0 (“not bothered”) to 2 (“bothered a lot”).14 Following Witthöft et al. (2013), we excluded item 4 (“… menstrual cramps or other problems with period”) due to gender-specific context and item 8 (“… fainting spells”) due to rare occurrence.15 The PHQ-15 cut-off scores of ≥5 represent signs of somatic burden. Within the current study, the Russian version of the PHQ-15 had good internal reliability (Cronbach’s alpha value for total score was .805).
Depression, anxiety, and stress scales-21 (DASS-21)
The Depression, Anxiety, and Stress Scales-21 (DASS-21) is a 21-item self-report measure assessing general psychological distress via 3 dimensions: depression (eg, “I felt down-hearted and blue”), anxiety (eg, “I felt scared without any good reason”), and stress (eg, “I felt that I was rather touchy”).16 Respondents rate the frequency of psychological symptoms on a scale from 0 (“never, or did not apply to me at all”) to 3 (“almost always, or applied to me very much, or most of the time”). The DASS-21 depression subscale cut-off scores of ≥10 represent signs of depression, the DASS-21 anxiety subscale cut-off scores of ≥8 represent signs of anxiety, and the DASS-21 stress subscale cut-off ≥ 15 represent signs of stress. We used the Russian version of the DASS-21, which has been verified for its psychometric properties.17 In this study, the DASS-21 had a good internal reliability for depression (Cronbach’s alpha value was .854), anxiety (Cronbach’s alpha value was .792), and stress subscales (Cronbach’s alpha value was .854).
Data analysis
Primarily, the prevalence of somatic burden, depression, anxiety, and stress was described. The Pearson’s χ2 was further used to examine differences in the prevalence of somatic and psychological distress between males and females, those who experienced and those who did not experience COVID-19 disease. All analyses were performed using SPSS 27.0.
Results
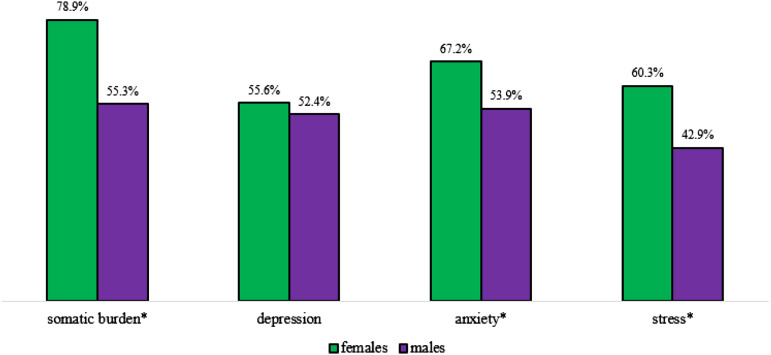
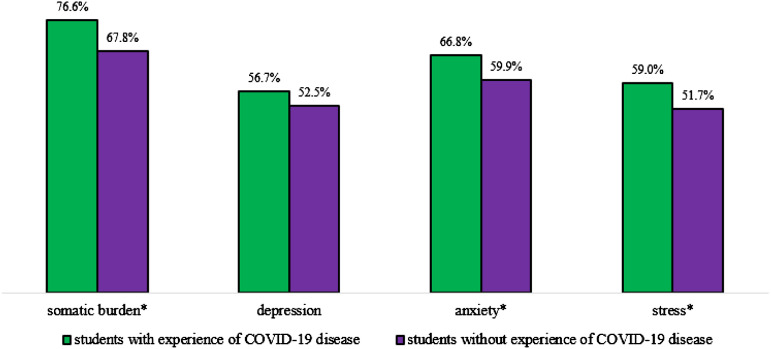
Signs of somatic burden was found in 72.2% of students, signs of depression in 54.7% of students, signs of anxiety in 63.4% of students, and signs of stress in 55.4% of students. Figures 2 and 3 illustrate prevalence of somatic and psychological distress by sex and experience of COVID-19 disease. Students with signs of somatic burden (χ2 (1) = 68.869, P < .001), anxiety (χ2 (1) = 18.929, P < .001), and stress (χ2 (1) = 30.420, P < .001) were more often females. Similar results were obtained with regard to the experience of COVID-19 disease. Students with signs of somatic burden (χ2 (1) = 11.767, P = .001), anxiety (χ2 (1) = 6.326, P = .012), and stress (χ2 (1) = 6.640, P = .010) were more often those who experienced COVID-19 disease. There were no differences in signs of depression by sex (χ2 (1) = .979, P = .322) and experience of COVID-19 disease (χ2 (1) = 2.234, P = .135).
Figure 2.
Prevalence of somatic and psychological distress among females and males. * statistically significant differences.
Figure 3.
Prevalence of somatic and psychological distress among students with and without experience of COVID-19 disease. * statistically significant differences.
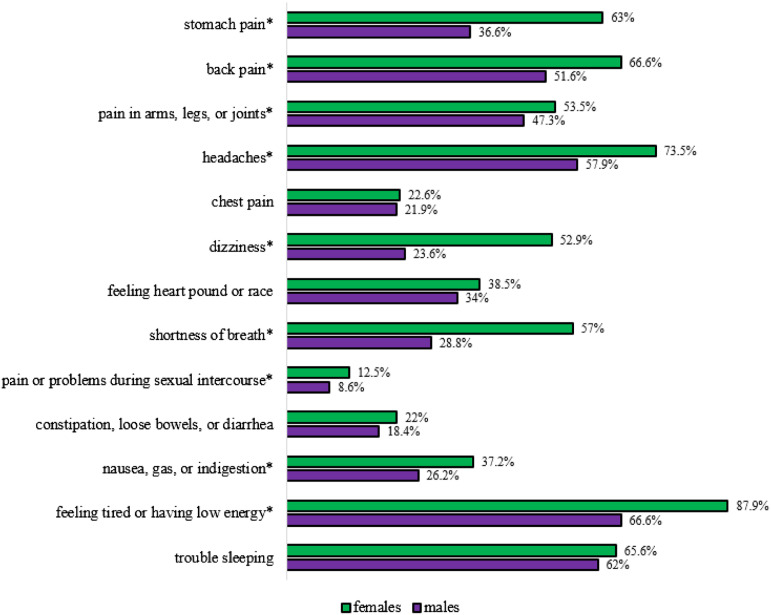
The sex-special prevalence of specific somatic symptoms is shown in Figure 4. Compared to males, females reported higher stomach pain (χ2 (1) = 73.312, P < .001), back pain (χ2 (1) = 23.950, P < .001), pain in arms, legs, or joints (χ2 (1) = 3.944, P = .047), headaches (χ2 (1) = 28.182, P < .001), dizziness (χ2 (1) = 34.415, P < .001), shortness of breath (χ2 (1) = 6.600, P = .010), pain or problems during sexual intercourse (χ2 (1) = 4.236, P = .040), nausea, gas or indigestion (χ2 (1) = 13.450, P < .073), and feeling tired or having low energy (χ2 (1) = 76.173, P < .001). There were no statistically significant differences in chest pain (χ2 (1) = .072, P = .789), feeling heart pound or race (χ2 (1) = 2.129, P = .145), constipation, loose bowels, or diarrhea (χ2 (1) = 1.951, P = .162), and trouble sleeping (χ2 (1) = 1.429, P = .232).
Figure 4.
Prevalence of somatic symptoms among females and males. * statistically significant differences.
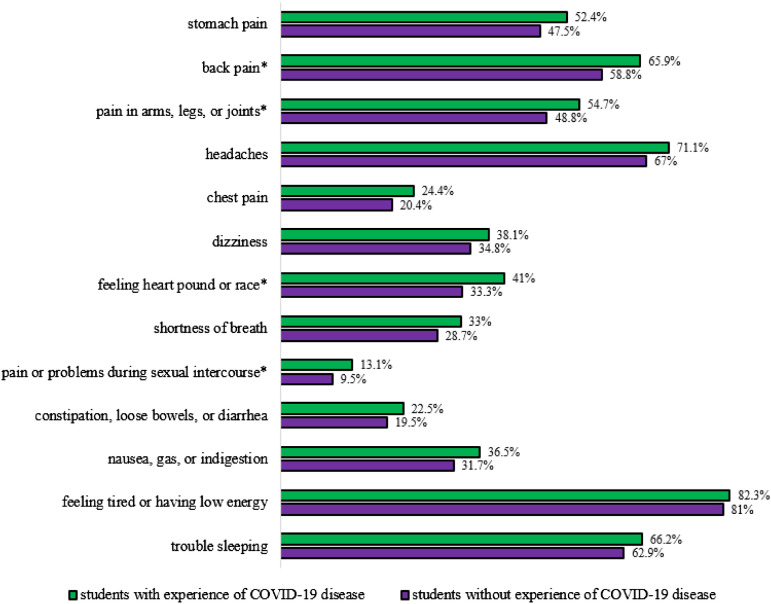
Prevalence of specific somatic symptoms among those students who experienced and did not experience COVID-19 disease is presented in Figure 5. Students with the experience reported higher back pain (χ2 (1) = 6.607, P = .010), pain in arms, legs, or joints (χ2 (1) = 4.360, P = .037), feeling heart pound or race (χ2 (1) = 7.749, P = .005), and pain or problems during sexual intercourse (χ2 (1) = 3.886, P = .049) than students without experience of the disease. There were no statistically significant differences in stomach pain (χ2 (1) = 1.882, P = .170), headaches (χ2 (1) = 2.476, P = .116), chest pain (χ2 (1) = 2.901, P = .089), dizziness (χ2 (1) = 1.458, P = .227), shortness of breath (χ2 (1) = 2.649, P = .104), constipation, loose bowels, or diarrhea (χ2 (1) = 1.616, P = .204), nausea, gas or indigestion (χ2 (1) = 3.208, P = .073), feeling tired or having low energy (χ2 (1) = .692, P = .406), and trouble sleeping (χ2 (1) = 1.469, P = .226) between students with and without experience of COVID-19 disease.
Figure 5.
Prevalence of somatic symptoms among students with and without experience of COVID-19 disease. * statistically significant differences.
Discussion
There are 2 key findings in this study. Firstly, the prevalence of somatic burden, depression, anxiety, and stress was 72.2%, 54.7%, 63.4%, and 55.4%, respectively. These findings showed that somatic and psychological distress among Russian university students were greater than among French,8 British,9 Chinese,11 Czech, and Slovak students.10 Importantly, this study was conducted during a lull in new cases of COVID-19 and transition from online learning to classroom learning, which would seem to have a positive effect on somatic and psychological well-being of Russian university students. This suggests that the high prevalence of somatic and psychological distress is a national characteristic of young Russians, as confirmed by pre-pandemic studies with Russian adolescents and their peers from other countries.18,19 Secondly, somatic and psychological distress varied by sex and experience of COVID-19 disease. Somatic burden, anxiety, and stress were more frequently reported by females and those who experienced COVID-19 disease compared to males and those who did not experience COVID-19 disease. These findings contribute to the knowledge that female sex and experience of COVID-19 disease are closely related to somatic and psychopathological responses to the pandemic.20-22
This study has limitations and future directions. The key limitation of this study is its cross-sectional nature, whereas the impact of the pandemic on somatic and psychological distress needs to be examined using a longitudinal design. Evidence for this comes from a study in which Spanish adults rated their psychological distress at the beginning, middle, and end of the forced confinement during the COVID-19 outbreak.23 Females reported significantly higher depressive, anxiety, stress, and avoidance symptoms than males at the beginning of the confinement, but over time the sex differences disappeared. Another limitation is that we used self-reports to determine the experience of COVID-19 disease. Some somatic symptoms are similar to those of COVID-19 disease, such as fatigue, dizziness, headache, diarrhea, nausea, and abdominal pain,24-26 which could lead students to mistakenly believe they are infected. Future directions may focus on the assessment of somatic and psychological distress among Russian university students based on data from medical examinations and dynamic observations.
In conclusion, this study highlighted the high prevalence and potential risk factors for somatic and psychological distress among Russian university students. It is hoped that these findings will form the basis of psychoeducation and preventive measures in the Russian university environment.
Footnotes
Author contributions: A.Z.: Conceptualization, Methodology, Formal analysis, Visualization, Writing - original draft, review & editing. S.B.: Data curation, Investigation. I.D.: Investigation, V.T.: Investigation. M.L.: Investigation. L.S.: Investigation. S.M.: Investigation. I.K.: Formal analysis. R.I.: Formal analysis. D.H.: Supervision, Writing - review & editing. M.K.: Supervision, Writing - review & editing.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by RFBR and NSFC (project No.20-515-55003) and partly by the Government contract of the Institute of Immunology and Physiology (АААА-А21-121012090090-9).
Ethical approval: This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board at the Chelyabinsk State University (Chelyabinsk, Russia).
Data availability: Data available in Supplementary materials.
ORCID iD
Alena Zolotareva https://orcid.org/0000-0002-5724-2882
References
- 1.Haesebaert F, Haesebaert J, Zante E, et al. Who maintains good mental health in a locked-down country? A French nationwide online survey of 11,391 participants. Health Place. 2020;66:102440. doi: 10.1016/j.healthplace.2020.102440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang X, Hegde S, Son C, et al. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. 2020;22:e22817. doi: 10.2196/22817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Werner AM, Tibubos AN, Mülder LM, et al. The impact of lockdown stress and loneliness during the COVID-19 pandemic on mental health among university students in Germany. Sci Rep. 2021;11:22637. doi: 10.1038/s41598-021-02024-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Appleby JA, King N, Saunders KE, et al. Impact of the COVID-19 pandemic on the experience and mental health of university students studying in Canada and the UK: a cross-sectional study. BMJ Open. 2022;12:e050187. doi: 10.1136/bmjopen-2021-050187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schiff M, Zasiekina L, Pat-Horenczyk R, et al. COVID-related functional difficulties and concerns among university students during COVID-19 pandemic: a binational perspective. J Community Health. 2021;46:667-675. doi: 10.1007/s10900-020-00930-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Nasa’h M, Al-Tarawneh L, Awwad FMA, et al. Estimating students’ online learning satisfaction during COVID-19: a discriminant analysis. Heliyon. 2021;7:e08544. doi: 10.1016/j.heliyon.2021.e08544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Di Consiglio M, Merola S, Pascucci T, et al. The impact of COVID-19 pandemic on Italian university students’ mental health: changes across waves. Int J Environ Res Public Health. 2021;18:9897. doi: 10.3390/ijerph18189897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le Vigouroux S, Goncalves A, Charbonnier E. The psychological vulnerability of French university students to the COVID-19 confinement. Health Educ Behav. 2021;48:123-131. doi: 10.1177/1090198120987128. [DOI] [PubMed] [Google Scholar]
- 9.Chen T, Lucock M. The mental health of university students during the COVID-19 pandemic: an online survey in the UK. PLoS One. 2022;17:e0262562. doi: 10.1371/journal.pone.0262562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gavurova B, Ivankova V, Rigelsky M, et al. Somatic symptoms, anxiety, and depression among college students in the Czech Republic and Slovakia: a cross-sectional study. Front Public Health. 2022;10:859107. doi: 10.3389/fpubh.2022.859107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu S, Liu Y, Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatry Res. 2020;289:113070. doi: 10.1016/j.psychres.2020.113070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zinchenko YP, Shaigerova LA, Almazova OV, et al. The spread of COVID-19 in Russia: immediate impact on mental health of university students. Psychol Stud. 2021;66:291-302. doi: 10.1007/s12646-021-00610-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brailovskaia J, Cosci F, Mansueto G, et al. The association between depression symptoms, psychological burden caused by Covid-19 and physical activity: an investigation in Germany, Italy, Russia, and Spain. Psychiatry Res. 2021;295:113596. doi: 10.1016/j.psychres.2020.113596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL, Frank V, et al. A symptom checklist to screen for somatoform disorders in primary care. Psychosomatics. 1998;39:263-272. doi: 10.1016/S0033-3182(98)71343-X. [DOI] [PubMed] [Google Scholar]
- 15.Witthöft M, Hiller W, Loch N, et al. The latent structure of medically unexplained symptoms and its relation to functional somatic syndromes. Int J Behav Med. 2013;20:172-183. doi: 10.1007/s12529-012-9237-2. [DOI] [PubMed] [Google Scholar]
- 16.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335-343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- 17.Zolotareva AA. Psychometric examination of the russian version of the depression, anxiety, and stress scales-21. Psychological Journal. 2021;42:80-88. (in Russ.). doi: 10.31857/S0205959200017077-0. [DOI] [Google Scholar]
- 18.Brailovskaia J, Schönfel P, Zhang X, et al. A cross-cultural study in Germany, Russia, and China: are resilient and social supported students protected against depression, anxiety, and stress? Psychol Rep. 2018;121:265-281. doi: 10.1177/0033294117727745. [DOI] [PubMed] [Google Scholar]
- 19.Tingstedt O, Lindblad F, Koposov R, et al. Somatic symptoms and internalizing problems in urban youth: a cross-cultural comparison of Czech and Russian adolescents. Eur J Public Health. 2018;28:480-484. doi: 10.1093/eurpub/cky001. [DOI] [PubMed] [Google Scholar]
- 20.Ausín B, González-Sanguino C, Castellanos MÁ, et al. Gender-related differences in the psychological impact of confinement as a consequence of COVID-19 in Spain. J Gend Stud. 2021;30:29-38. doi: 10.1080/09589236.2020.1799768. [DOI] [Google Scholar]
- 21.Giudice V, Iannaccone T, Faiella F, et al. Gender differences in the impact of COVID-19 pandemic on mental health of Italian academic workers. J Pers Med. 2022;12:613. doi: 10.3390/jpm12040613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guerrini CJ, Schneider SC, Guzick AG, et al. Psychological distress among the U.S. general population during the COVID-19 pandemic. Front Psychiatry. 2021;12:642918. doi: 10.3389/fpsyt.2021.642918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fenollar-Cortés J, Jiménez Ó, Ruiz-García A, et al. Gender differences in psychological impact of the confinement during the COVID-19 outbreak in Spain: a longitudinal study. Front Psychol. 2021;12:682860. doi: 10.3389/fpsyg.2021.682860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hu Y, Sun J, Dai Z, et al. Prevalence and severity of corona virus disease 2019 (COVID-19): a systematic review and meta-analysis. J Clin Virol. 2020;127:104371. doi: 10.1016/j.jcv.2020.104371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infection: a systematic review and meta-analyses with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:611-627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smyk W, Janik M, Portincasa P, et al. COVID-19: focus on the lungs but do not forget the gastrointestinal tract. Eur J Clin Invest. 2020;50:13276. doi: 10.1111/eci.13276. [DOI] [PMC free article] [PubMed] [Google Scholar]