A 34 year old previously healthy transgender male presented with a 7 day history of left ear pain, headache with intermittent right-sided weakness. Over 24 h, symptoms progressed with development of fever, right sided hemiparesis and inability to ambulate.
Investigations revealed hyponatremia (128 mmol/L, NR 133–145), elevated CRP (277.6 mg/L, NR 0–8) and leukocytosis (17.3 ×109 cells/L, NR 4.0–11.0). HIV testing was negative. Neurological examination showed meningismus and right-sided weakness with upper-motor neuron findings. CT-angiogram head showed left superior cerebral edema with multiple locules of gas (Fig. 1). Rapid Human Immunodeficiency Virus (HIV) testing was negative. Intravenous ceftriaxone, vancomycin, metronidazole and dexamethasone was initiated. Lumbar puncture (LP) was attempted but unsuccessful.
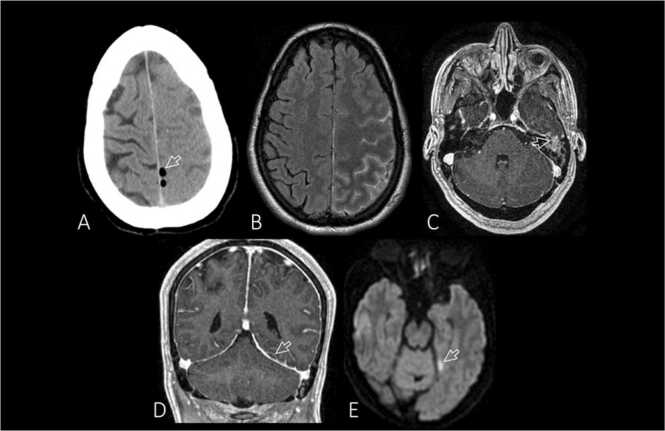
Fig. 1.
Otomastoiditis, meningitis and subdural empyema. Axial non-contrast CT (A) shows several small gas/air blebs located adjacent to the interhemispheric falx (arrow) in the extra-axial space. Axial post-gadolinium fluid-attenuated inversion recovery (FLAIR) (B), axial post-gadolinium T1-weighted (C), coronal post-gadolinium T1-weighted (D), and axial diffusion weighted imaging (DWI) (E) MRI images. MRI more fully characterized the infection and demonstrated the presence of a small subdural empyema. The FLAIR sequence shows hyperintense sulci involving the left cerebral hemisphere, suggesting meningitis in this clinical setting. The axial post-gadolinium sequence shows patchy enhancement of the left mastoid sinus (arrow) that had contiguous extension to involve the dura beneath the left temporal lobe. On the post-gadolinium coronal T1 weighted sequence, a small rim enhancing extra-axial collection is identified bordering the superior margin of the left tentorium (arrow). The left tentorium is thicker and has greater enhancement than on the right side. DWI is especially helpful and shows that this small extra-axial collection has restricted diffusion (arrowhead) that is characteristic of subdural empyema. A small intraluminal filling defect within a left-sided superior convexity cortical vein (not shown) indicated the added presence of non-occlusive cortical vein thrombosis.
Tonic clonic seizures developed 1 day after admission. A magnetic resonance image (MRI) of the brain and venogram showed venogram showed left-sided otomastoiditis, parietal cortical vein thrombosis, and subdural pus along the tentorium and posterior flax associated left hemispheric edema (Fig. 1). A LP under fluoroscopy revealed a pleocytosis (88 cells/μL, normal range 0–5) with 83 % neutrophils and elevated protein (0.66 g/L, normal range 0.15–0.45). CSF Bacterial and fungal cultures were negative and PCR for enterovirus, HSV, and VZV were negative. Multiplex nucleic acid amplification testing (BioFire FilmArray Meningitis Panel, bioMerieux) was positive for Streptococcus pneumoniae. The patient was treated with 6 weeks of ceftriaxone and metronidazole, with radiological improvement on follow-up imaging performed 1 month after presentation. Clinically, he improved with good neurological recovery, with full-strength by Medical Research Council (MRC) grading scale at 2-weeks post-admission.
Pneumococcal meningitis is the most common cause of community bacterial meningitis and a rare cause of pneumocephalus [1]. In the absence of prior head trauma or neurosurgery, spontaneous pneumocephalus is a rare complication of meningitis with few cases reported in the literature [1], [2]. This can be caused by a variety of microorganisms including aerobic gram negative bacilli, gas forming anaerobic bacteria, fungi and Streptococcus pneumoniae, especially in the context of an otogenic infection which allows air to enter the cranium [2], [3], [4]. Treatment is often conservative with broad-spectrum antimicrobials with adequate central nervous system penetration but requires close monitoring for neurological deterioration [1], [2], [3], [4]. Occasionally pneumocephalus can cause intracranial hypertension, leading to neurological deficits, alterations in consciousness and coma, requiring urgent surgical decompression [2], [3], [4]. In patients presenting with spontaneous pneumocephalus, consideration of meningitis within the differential diagnosis is important in initiating prompt and appropriate anti-microbial therapy. This dramatic presentation helps to illustrate the various and rare complications of pneumococcal meningitis, including pneumocephalus, cortical vein thrombosis, focal neurological deficits and seizures.
CRediT authorship contribution statement
Jordan Mah and Angela Lee conceived the work and drafted the manuscript. James Scott prepared the figure for publication. Jordan Mah, Deirdre Church, Angela Lee and James Scott critically revised the manuscript for important intellectual content and gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Ethical approval
N/A.
Consent
We have obtained patient consent.
Funding statement
The authors received no financial support for the writing of this case report.
Declaration of competing interests
The authors have no competing interests to declare.
References
- 1.Ciorba A., Berto A., Borgonzoni M., Grasso D.L., Martini A. Pneumocephalus and meningitis as a complication of acute otitis media: case report. Acta Otorhinolaryngol Ital. 2007;27:87. [PMC free article] [PubMed] [Google Scholar]
- 2.Markham J.W. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir. 1967;16(1):1–78. doi: 10.1007/BF01401900. [DOI] [PubMed] [Google Scholar]
- 3.Engel G., Fearon W.F., Kosek J.C., Loutit J.S. Pneumocephalus due to invasive fungal sinusitis. Clin Infect Dis. 2000;30:215–217. doi: 10.1086/313605/2/30-1-215-FIG001.GIF. [DOI] [PubMed] [Google Scholar]
- 4.Kim H.S., Kim S.W., Kim S.H. Spontaneous pneumocephalus caused by pneumococcal meningitis. J Korean Neurosurg Soc. 2013;53:249. doi: 10.3340/JKNS.2013.53.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]