Abstract
Objective:
Burnout is prevalent among vascular surgery trainees. Here we aim to identify modifiable risk factors for burnout in vascular surgery training, to facilitate the development of programs to enhance and sustain trainee well-being.
Methods:
The Association of Program Directors in Vascular Surgery issued the Annual Training survey in the fall of 2018 to all trainees. The survey contained items to assess frequency of burnout, as well as mentorship, training environment, and stress coping mechanisms using an abbreviated COPE (Coping Orientation to Problems Experienced) inventory.
Results:
Of 628 surveys issued, the response rate was 30% (n = 188). Respondents indicated that the majority of programs offer mentorship opportunities (n = 150 [83%]) that are longitudinal throughout the duration of training (n = 140 [77%]). Fifty-eight percent (n = 109) indicated there was an appropriate balance between learning and productivity in their program, with more respondents leaning toward too much clinical productivity (n = 57) and fewer toward too much learning (n = 19). Forty-five percent of respondents indicated feeling burnout at least weekly (n = 81). The burnout group was less likely to report an appropriate balance between clinical productivity and learning (49.4% vs 67.7%; P < .001), as well as a lower frequency of mentorship opportunities (72.1% vs 92.7%; P < .001). Certain coping skills were used more frequently in the burnout group, including self-distraction, disengagement, humor, self-blame, and substance use. In multivariate analysis, frequent use of self-blame conferred a 9.847-fold increased risk (95% confidence interval, 2.114–45.871) of burnout (P = .003), while feeling appropriately challenged by the faculty was significantly protective (odds ratio for burnout, 0.158; 95% confidence interval, 0.031–0.820; P = .03).
Conclusions:
The protective effect against vascular surgery trainee burnout conferred by the availability of mentorship suggests that an expansion and emphasis on mentorship in training may help to mitigate trainee burnout. Mentorship may also be a suitable channel to assess for an appropriate level of challenge, as well as for an appropriate balance between clinical productivity and learning that, when present, are also protective against burnout. Furthermore, the correlation between the frequent use of certain coping skills and burnout highlight this as an area for intervention, potentially through a combination of mentor modeling and formal training on healthy stress-related coping strategies.
Keywords: Resident education, Workforce, Database, coping
Burnout is a syndrome defined by emotional exhaustion, depersonalization, and a sense of low personal accomplishment.1 Physician burnout is linked to a number of consequences, among them negative patient outcomes and career attrition.2,3 In the most recent Society for Vascular Surgery Wellness Task Force report, 30% of practicing vascular surgeons met criteria for burnout.4
Within the residency track, data suggest that vascular surgery residency has lower rates of attrition than general surgery, with the most recent data demonstrating an attrition rate of 0.6% to 2.9% compared with 3.3% to 5.2% in general surgery, demonstrating that this pathway promotes retention of trainees.5 Still, in 2018, the Association of Program Directors in Vascular Surgery (APVDS) Annual Trainee Survey indicated that among fellowship and residency vascular surgery trainees, more than 60% feel burned out at least once a week. Nonmodifiable risk factors for burnout included older age and possessing an additional advanced degree.6 Other surveys indicated burnout among trainees to be related to lack of mentorship, lack of programmatic social events, and violation of duty-hour restrictions.7 These data suggest that trainee burnout is a complex syndrome with contributions from institutional organization, intrapersonal dynamics, family dynamics, mechanism of instruction, and limitations in time.
Despite the high retention rate in vascular surgery training, the high reported rate of burnout mirrors that of the general surgery training population, and so the focus on prevention of burnout remains pertinent.8 It will be imperative for vascular surgery program directors of both training modalities to model healthy behavior and motivate trainees to further promote retention within vascular surgery training. Such skills cultivated in training may also foster long-term retention in a vascular surgery career. Prior work has suggested that modifying coping mechanisms can improve performance under pressure.9 The objective of this study was to use the Annual Training Survey issued by the Association of Program Directors in Vascular Surgery Issues Committee to evaluate coping strategies as potentially modifiable risk factors for burnout among vascular surgery trainees to further guide program directors in this endeavor.
METHODS
The Association of Program Directors in Vascular Surgery (APDVS) fosters an annual trainee survey to understand issues relating to training in vascular surgery. The annual survey was distributed by e-mail to all active vascular trainees in both the 2-year fellowship and 0+5 integrated vascular residency in Accreditation Council for Graduate Medical Education-accredited programs in the United States during the 2018–2019 academic year. The APDVS Issues Committee survey is conducted annually and approved by APDVS leadership. Use of the data is only allowed by the Issues Committee and APDVS leadership.
To identify causative factors, questions were added to address motivation, mentorship, and stress coping. The final survey was reviewed by the APDVS Issues Committee, which includes program directors, associate program directors, and select trainees. A total of 21 multiple choice questions were included in the survey along with an open-ended option for commentary (Supplementary Fig, online only). This included an abbreviated COPE (Coping Orientation to Problems Experienced) inventory. Responses were recorded and compiled anonymously. All surveys were returned and submitted voluntarily without compensation or incentive. Lack of response or negative responses were not penalized and cannot be traced back to the individual or training program.
Statistical analysis.
Data were analyzed using both bivariate and multivariate analyses. Demographics and training characteristics were analyzed using the Fischer’s exact test for categorical variables and the t test for continuous variables. Graded variables for factors contributing to burnout were analyzed using the Fischer exact test. Questions that were found to be statistically significant as markers for high burnout were selected for a multivariate logistic regression model predictive of high burnout. The concordance index was identified and results were reported as odds ratios (ORs) with a 95% confidence interval (CI). All statistical tests were considered to be significant at a two-sided P value of less than .05. All analyses were performed using SAS software version 9.4 (SAS Inc., Cary, NC).
RESULTS
Demographics.
The 2018–2019 annual APDVS training survey was sent to a total of 628 vascular surgery trainees, 55% (n = 346) from integrated vascular surgery programs, 41.5% (n = 260) from vascular surgery fellowships, and 3.5% (n = 22) incoming fellows, with a response rate of 30% (n = 188; composed of 76 fellows and 112 integrated residents or recent graduates), comparable with prior published survey results.6,7,10 The survey respondents were 70.21% male (n = 132) and 28.72% female (n = 54). The median age of respondents was 30 years (range, 26–48 years). The majority (n = 172 [93.48%]) of respondents described their program as a quaternary/tertiary care center, and a majority (n = 175 [94.59%]) described their training program as academic.
Mentorship and training environment.
Mentorship has been identified as a key component of surgical training.11 Eighty-three percent of respondents (n = 150) indicated that their program has mentorship opportunities available. Furthermore, 77.35% (n = 140) indicated that this mentorship is longitudinal, continuing through the years of their training experience (Fig 1, A).
Fig 1.
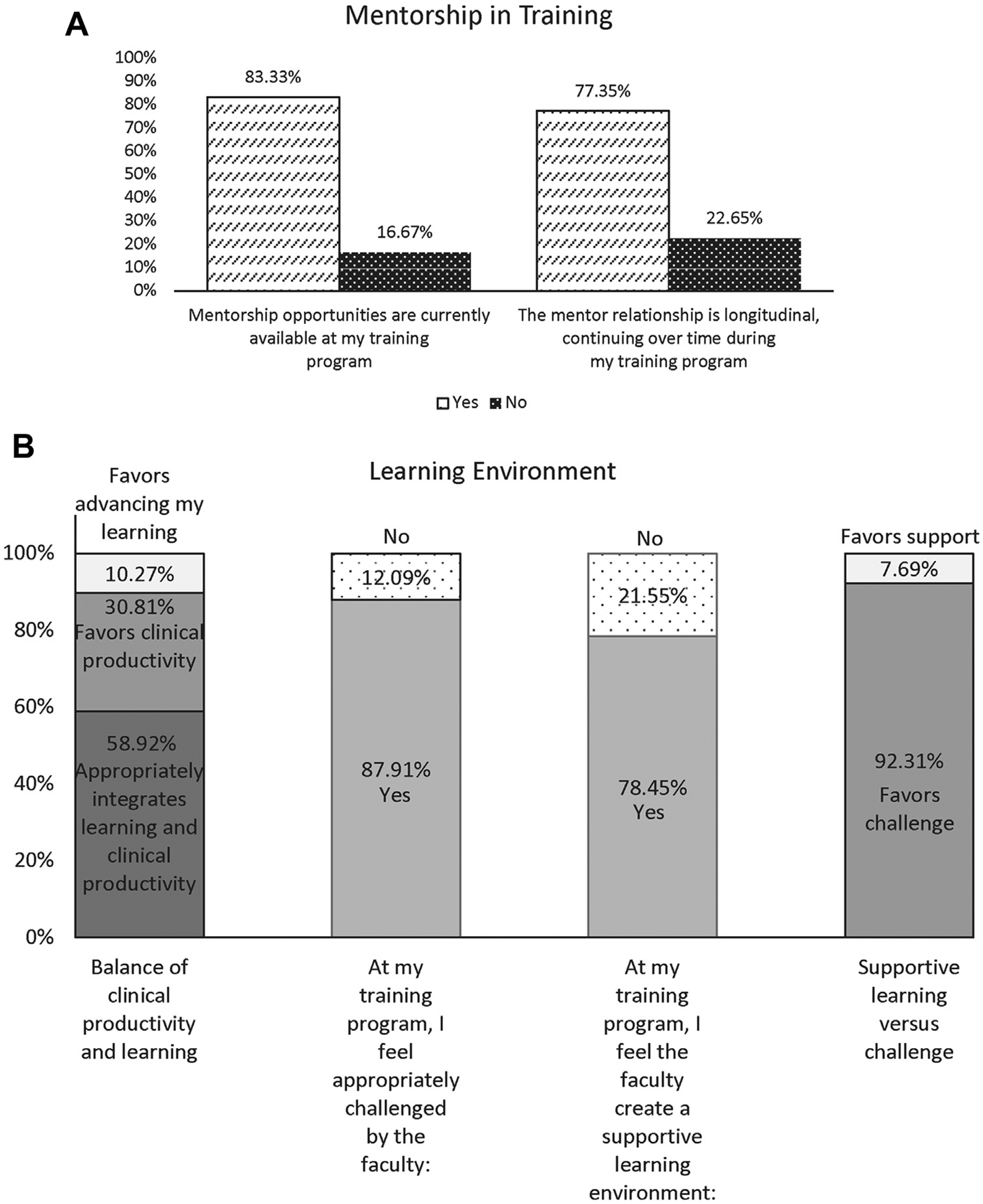
A, The majority of respondents indicated a presence of mentorship opportunities that were longitudinal in nature throughout the years of their training. B, Just more than one-half of respondents indicated that their programs were balanced between clinical productivity and learning, with those not balanced more often leaning toward clinical productivity. The large majority of respondents indicated their program was supportive with an appropriate level of challenge from the faculty.
Regarding the training environment, 58.92% of respondents (n = 109) replied that their program appropriately integrates learning and clinical productivity. A mere 10.27% (n = 19) replied that their program favors advancing learning over productivity, and 30.81% (n = 57) replied their program favors clinical productivity over learning. Overall, the vast majority (n = 160 [87.91%]) of respondents replied that they feel appropriately challenged in their training program. Additionally, the majority (n = 142 [78.45%]) endorsed that the faculty create a supportive learning environment. Of those who either indicated they did not feel appropriately challenged or felt the learning environment was not supportive (n = 48), the majority (n = 44 [92.3%]) responded that their program favored challenge over learning, and only 7.7% (n = 4) indicated their program favored learning over challenge (Fig 1, B).
Coping strategies.
To identify actionable targets to improve trainee burnout, our survey included an abbreviated COPE questionnaire to identify what coping strategies trainees are currently using to mitigate the stressors of training. Survey respondents were asked to rate the frequency of using various coping strategies with regard to their most recent major surgical complication (Supplementary Fig, online only, question 17). The percent of trainee respondents who indicated each frequency for each coping strategy can be seen in Fig 2. The most commonly used strategy was, “I’ve been thinking hard about what steps to take to prevent a complication from happening again,” followed by “I’ve been looking for something good in what is happening.” The least frequently used strategy was “I’ve been using alcohol or other drugs to make myself feel better,” with 76.14% (n = 134) indicating they “haven’t been doing this at all.”
Fig 2.
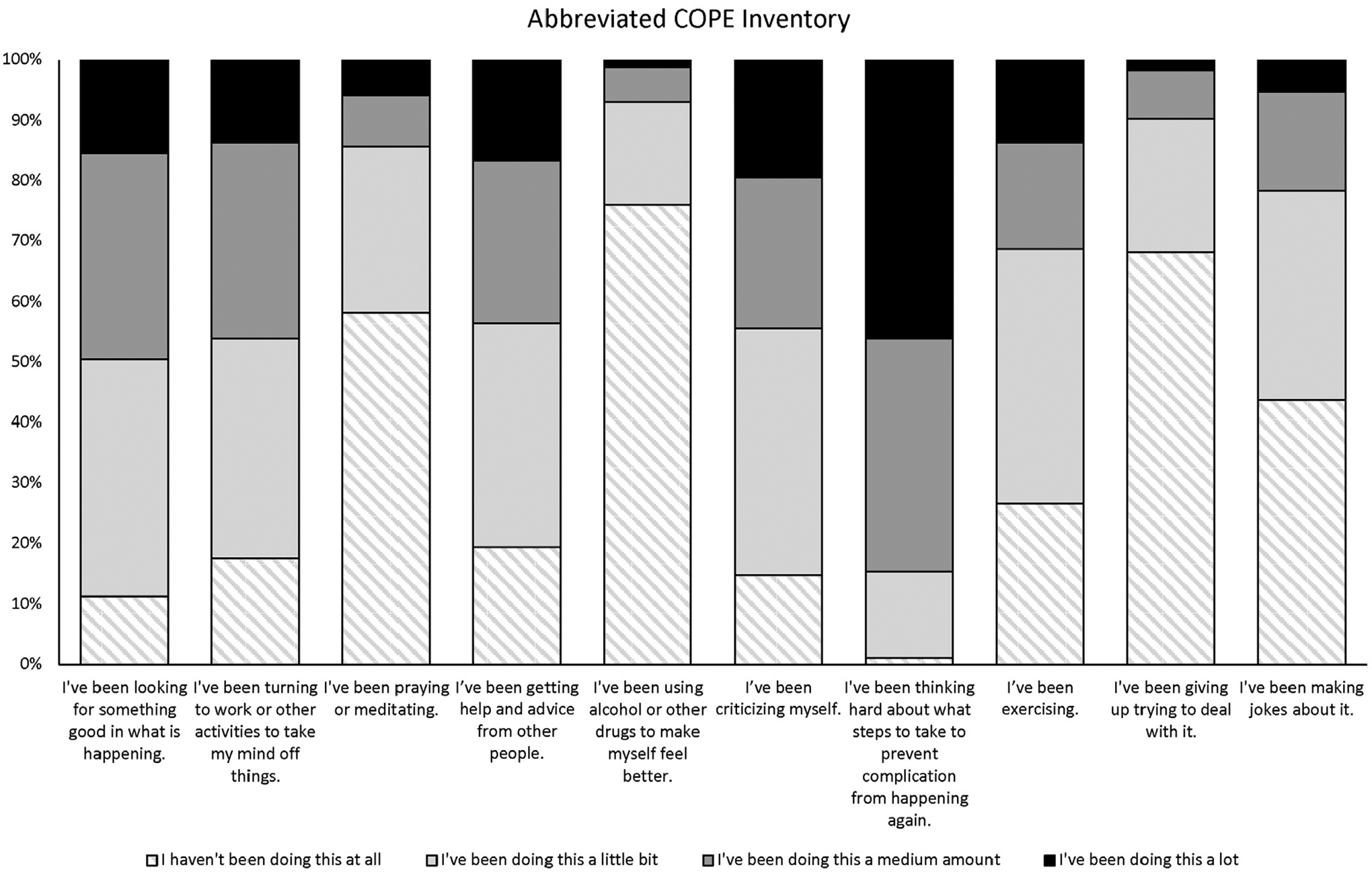
Respondents rated major coping strategies used by frequency.
Burnout.
To build on our prior work, burnout was assessed with a single question, “I have felt burned out by my work (select one): A. Every day; B. A few times a week; C. Once a week; D. A few times a month; E. Once a month or less; F. A few times a year” (Supplementary Fig, online only, question 20). Respondents with burnout, that is, those who responded “at least once a week,” were compared with those with infrequent symptoms of burnout. The burnout group included 45% of respondents (n = 81), comparable to the previously published rates from prior surveys using the validated 7-item Physician Well-Being Index.6 No statistically significant difference was found between the groups with regard to gender, age, academic vs community program, or training level (Supplementary Table I, online only).
Differences in training environment were assessed, and coping strategies were stratified by presence or absence of burnout (Table I). The Fischer exact test identified a significant difference between burnout and no burnout groups in the balance between integrating learning and clinical productivity in the operating room, with 67.7% (n = 65) of the no burnout group responding that the balance was appropriate vs only 49.4% (n = 40) in the burnout group (P < .001). The burnout group was more likely to respond that the operating room favored clinical productivity, 45.7% (n = 37) vs 17.7% (n = 37) in the no burnout group. The burnout and no burnout groups also differed significantly in their response to feeling appropriately challenged by the faculty, with 95.8% (n = 92) of the no burnout group indicating they are appropriately challenged vs only 77.8% (n = 63) in the burnout group (P < .001). Furthermore, the groups differed in the reported supportiveness of the learning environment, as defined by the survey respondent, with only 11.6% (n = 11) of the no burnout group feeling unsupported vs 33.3% (n = 27) of the burnout group (P = .001).
Table I.
Univariate analyses of program factors for correlation with high burnout
| No burnouta | Burnouta | ||
|---|---|---|---|
| Questions | (n = 96) | (n = 81) | P valueb |
| At my training program, teaching in the operating room: | |||
| Appropriately integrates learning and clinical productivity | 65 (67.7) | 40 (49.4) | <.001 |
| Favors advancing my learning | 14 (15.6) | 4 (4.9) | |
| Favors clinical productivity | 17 (17.7) | 37 (45.7) | |
| At my program, I feel appropriately challenged by the faculty. | |||
| No | 4 (4.2) | 18 (22.2) | <.001 |
| Yes | 92 (95.8) | 63 (77.8) | |
| At my program, I feel the faculty create a supportive learning environment.c | |||
| No | 11 (11.6) | 27 (33.3) | .001 |
| Yes | |||
| Mentorship opportunities are currently available at my training program.c | |||
| No | 7 (7.3) | 22 (27.9) | <.001 |
| Yes | 89 (92.7) | 57 (72.1) | |
| The mentor relationship is longitude, continuing over time during my training program.d | |||
| No | 12 (12.5) | 28 (35.0) | .001 |
| Yes | |||
Values are number (%).
High burnout was defined as feeling burned out by work once a week, a few times a week, or every day.
P values are from Fischer’s exact and bolded if < .05.
There was one missing response for these questions.
There was two missing response for this question.
Mentorship experience also differed between the burnout and no burnout groups. The no burnout group was more likely to report the availability of mentorship opportunities at their program 92.7% (n = 89) vs 72.1% (n = 57) in the burnout group (P < .001). The burnout group was also more likely to report the lack of longitudinal mentorship relationships, 35.0% (n = 28) vs 12.5% (n = 12) in the no burnout group (P = .001; Table I).
Coping skills, such as self-distraction, were compared between the two groups, and although some were found to be similarly used by both groups (Supplementary Table II, online only), others differed (Table II). When asked about turning to work or other activities to take their mind off things (self-distraction), the burnout group was more likely to respond, “I’ve been doing this a lot” at 21.0% (n = 17) vs 7.3% (n = 7) in the no burnout group (P = .02). The burnout group also was more likely to endorse using substances, with 33.3% (n = 27) reporting doing this a little, a medium amount or a lot vs only 15.6% (n = 15) of the no-burnout group (P = .02). Other coping skills that the burnout group was more likely to use (“I have been doing this a little/medium amount/a lot vs not at all”) included disengagement (“I’ve been giving up trying to deal with it”) at 43.2% (n = 35) vs 21.9% (n = 21) in the no-burnout group (P = .009); humor (“I’ve been making jokes about it”) at 60.5% (n = 49) in the burnout group vs 52.1% (n = 50) in the no-burnout group (P = .01); and self-blame (“I’ve been criticizing myself”) at 88.9% (n = 72) in the burnout group vs 80.2% (n = 77) in the no-burnout group (P < .0001). The burnout group was also significantly less likely to report being satisfied or very satisfied with their training program at only 60.5% (n = 49) vs 87.5% (n = 84) of the no-burnout group (P < .0001).
Table II.
Univariate analyses of coping mechanisms for correlation with burnout
| No burnouta | Burnouta | ||
|---|---|---|---|
| Questions | (n = 96) | (n = 81) | P valueb |
| I’ve been turning to work or other activities to take my mind off things. | |||
| I haven’t been doing this at all. | 23 (24.0) | 9 (11.1) | .02 |
| I’ve been doing this a little bit. | 36 (37.5) | 29 (35.8) | |
| I’ve been doing this a medium amount. | 30 (31.3) | 26 (32.1) | |
| I’ve been doing this a lot. | 7 (7.3) | 17 (21.0) | |
| I’ve been using alcohol or other drugs to make myself feel better. | |||
| I haven’t been doing this at all. | 81 (94.4) | 54 (66.7) | .02 |
| I’ve been doing this a little bit. | 12 (12.5) | 18 (22.2) | |
| I’ve been doing this a medium amount. | 3 (3.1) | 7 (8.6) | |
| I’ve been doing this a lot. | 0 (0) | 2 (2.5) | |
| I’ve been criticizing myself. | |||
| I haven’t been doing this at all. | 19 (19.8) | 9 (11.1) | <.0001 |
| I’ve been doing this a little bit. | 47 (49.0) | 24 (29.6) | |
| I’ve been doing this a medium amount. | 25 (26.0) | 19 (23.5) | |
| I’ve been doing this a lot. | 5 (5.2) | 29 (35.8) | |
| I’ve been giving up trying to deal with it. | |||
| I haven’t been doing this at all. | 75 (78.1) | 46 (56.8) | .009 |
| I’ve been doing this a little bit. | 16 (16.7) | 23 (28.4) | |
| I’ve been doing this a medium amount. | 5 (5.2) | 9 (11.1) | |
| I’ve been doing this a lot. | 0 (0) | 3 (3.7) | |
| I’ve been making jokes about it. | |||
| I haven’t been doing this at all. | 46 (47.9) | 32 (39.5) | .01 |
| I’ve been doing this a little bit. | 38 (39.6) | 23 (28.4) | |
| I’ve been doing this a medium amount. | 10 (10.4) | 19 (23.5) | |
| I’ve been doing this a lot. | 2 (2.1) | 7 (8.6) |
Values are number (%).
High burnout was defined as feeling burned out by work once a week, a few times a week, or every day.
P values are from Fischer’s exact and bolded if < .05.
To adjust for covariates, a multivariate analysis was performed to assess for factors associated with high burnout vs low burnout. Self-criticism was found to increase the risk for burnout (OR, 9.847; 95% CI, 2.114–45.871; P = .003), whereas feeling appropriately challenged by faculty was protective against burnout (OR, 0.158; 95% CI, 0.031–0.820; P = .03; Table III).
Table III.
Multivariable model for burnout
| Questiona | OR (95% CI) | P valueb |
|---|---|---|
| At my training program, teaching in the operating room: | ||
| Appropriately integrates learning and clinical productivity | Ref | .18 |
| Favors advancing my learning | 0.302 (0.060–1.517) | |
| Favors clinical productivity | 1.464 (0.548–3.912) | |
| At my program, I feel appropriately challenged by the faculty. | ||
| No | Ref | |
| Yes | 0.158 (0.031–0.820) | .03 |
| At my program, I feel the faculty create a supportive learning environment. | ||
| No | Ref | |
| Yes | 0.456 (0.157–1.329) | .15 |
| Mentorship opportunities are currently available at my training program. | ||
| No | ||
| Yes | 0.522 (0.093–2.923) | .46 |
| The mentor relationship is longitude, continuing over time during my training program. | ||
| No | Ref | |
| Yes | 0.789 (0.173–3.602) | .76 |
| I’ve been turning to work or other activities to take my mind off things. | ||
| I haven’t been doing this at all. | Ref | |
| I’ve been doing this a little bit. | 1.977 (0.629–6.217) | .35 |
| I’ve been doing this a medium amount. | 1.274 (0.387–4.197) | |
| I’ve been doing this a lot. | 3.153 (0.719–13.823) | |
| I’ve been criticizing myself. | ||
| I haven’t been doing this at all. | Ref | |
| I’ve been doing this a little bit. | 0.974 (0.303–3.133) | .003 |
| I’ve been doing this a medium amount. | 1.969 (0.573–6.774) | |
| I’ve been doing this a lot. | 9.847 (2.114–45.871) | |
| I’ve been making jokes about it. | ||
| I haven’t been doing this at all. | Ref | |
| I’ve been doing this a little bit. | 0.835 (0.353–1.977) | .73 |
| I’ve been doing this a medium amount. | 1.475 (0.452–4.806) | |
| I’ve been doing this a lot. | 2.039 (0.260–16.011) | |
CI, Confidence interval; OR, odds ratio.
All bivariable significant questions without empty cells were entered into the model.
Significant P values were bolded. The c index was 0.837 with the intercept being 1.7231.
Discussion.
Because prior work identified a high prevalence of burnout among vascular surgery trainees,6 our study aimed to identify modifiable risk factors for burnout in this population to facilitate a structured approach to improving trainee well-being. Burnout is a complex syndrome affected by all facets of life, including institutional organization, intrapersonal dynamics, family dynamics, mechanism of instruction, and limitations in time. We chose to focus this study on the intervenable factors potentially within the control of program directors and other faculty mentors. We identified that the learning environment—feeling appropriately challenged, appropriately integrating learning and clinical productivity, and having a supportive learning environment—protected against burnout. The opportunity for mentorship in a longitudinal fashion was found to be protective against burnout. Certain frequently used coping strategies emerged as risk factors for burnout, including self-distraction, substance use, self-criticism, disengagement, and humor. The no-burnout group also demonstrated a higher level of satisfaction with their training program.
A learning environment balanced in support and challenge driven by mentorship has previously been proposed as the cornerstone of a successful surgical residency.11,12 Our data support this finding, and that trainees who perceive that their training program balances learning and clinical productivity reported a lower rate of burnout. Furthermore, feeling appropriately challenged by the faculty emerged as strongly correlative with low burnout on multivariate analysis. A program that leans more heavily toward clinical productivity may not allow for trainees to complete adequate case preparation or receive appropriate supervision for their level of skill, and result in a high burden of administrative tasks delegated to the vascular surgery trainee. Conversely, a program that favors learning over productivity may not allow trainees to cultivate the necessary technical skill sets that require practice. Many of the factors that constitute the learning environment are part of the hidden curriculum, composed of the values held by the institution, the surgical attendings, and the health care staff, which are transmitted to the trainee informally.13 We intentionally did not define what constitutes an appropriate balance of learning and productivity, or what constitutes an appropriate level of challenge, but rather left it to the discretion of the respondent to define this variable. Future studies to better define how trainees perceive balance and challenge in training will also help identify targets for intervention. However, a multi-institutional survey-based study evaluating trainee workload satisfaction and learning environment found that the institution was a more significant factor than specialty.14 Further investigation into institutional and cultural factors that affect the surgical trainee learning environment may be warranted to clarify targets for intervention.
The learning environment has been proposed to affect many elements of surgical training, including the tone of the mentor-mentee relationships that are the cornerstone of surgical training. Our results identified the lack of mentorship opportunities and the lack of longitudinal mentorship as correlating with burnout among trainees. The implementation of longitudinal mentorship may vary by training paradigm, and further investigation to determine if trainee perception of mentorship varies between training program type. Surgical mentorship is the basis for learning more than simple technical proficiency but also communication skills, leadership, and commitment to practice, and likely reflects the origin of surgical training in the apprenticeship model which lent itself easily to close mentorship. In the modern surgical training paradigm, mentorship is most successful when mentees select their mentors and the relationship is continued over an extended period.15,16 A systematic review by Entezami et al17 identified 1091 unique articles on the subject of surgical mentorship, and of 38 that met inclusion criteria for review, most focused on the qualities of a mentor, the structure of the mentoring relationship, and overcoming barriers to mentoring. A focus on mentorship has been proposed as a way to address the growing physician shortage, as well as to improve the representation of under-represented groups in academic surgery.18,19 There are challenges to successful mentoring unique to surgical training, including time pressures for decision-making and affecting patient care.20 However, it is imperative to foster the mentor-mentee relationship by maintaining open lines of communication with a positive feedback cycle to cultivate the mentee’s potential.21 Mentorship will continue to be key to attracting and retaining a talented and well-trained future workforce in vascular surgery and should remain an explicit priority in training programs.
There are unique stressors of a surgical career that require a practicing surgeon be well equipped with coping strategies to be able to also enjoy its many benefits. In a survey of 47 general and vascular surgeons in the UK regarding their most recent major surgical complication, one-third reported significant traumatic stress 1 month after the incident, which correlated with the use of self-distraction as a coping mechanism.22 Our abbreviated COPE inventory included assessment for self-distraction, as well as for positive re-interpretation, planning, turning to spirituality, seeking social support, humor, self-blame, mental disengagement, and substance use. The most frequently used coping strategies were positive in nature. Although many coping strategies can be adaptive to some extent, we sought to identify which coping strategies correlated with burnout and were therefore more likely to represent maladaptive behavior. Respondents who reported less burnout were less likely to report using humor, self-blame, mental disengagement, or substance use. In particular, self-blame emerged as strongly correlative with high burnout in multivariate analysis. This result corresponds with findings of self-blame being a maladaptive coping mechanism adversely affecting performance in professional athletes.23 This represents an area of opportunity to improve well-being during training that can be carried over into practice as a surgical attending, by vascular surgery program directors, and faculty modeling positive coping strategies in the mentoring relationship, including the integration of a formal curriculum to foster awareness of adaptive stress management.
There are certain limitations to the interpretation of this study. As a voluntary survey, the results are subject to sample bias, although our response rate was on par with that reported in comparable surveys.6,7,10 Our outcome metric, namely, burnout, was defined subjectively by the user in this survey and, owing to the nature of surveys, the results may be subject to recall bias.
Taken together, these findings suggest that the majority of trainees feel their training program is balanced and supportive. The majority endorse having long-term mentoring opportunities available to them. Furthermore, trainees reporting less frequent burnout were less likely to use certain coping mechanisms, such as humor, disengagement, self-blame, or substance use. These findings present specific areas to structure improvements in vascular surgery training. Such improvements to training will help to produce a workforce that is well-equipped for the rigor of medical practice and that functions at peak performance throughout their careers.
Supplementary Material
Acknowledgments
The authors thank Niten Singh, MD, for his participation in the 2018–2019 APDVS Issue Committee, as well as his critical review of this manuscript. The authors also thank all members of the 2018–2019 APDVS Issues Committee for their involvement in designing and interpreting the survey results: Christopher Carsten, MD, Omid Jazaeri, MD, and Christine Shokrzadeh, MD.
K.E.H. was supported by NIH grant 1F32HL137292 during this project.
Footnotes
Author conflict of interest: none.
Presented at the Association for Program Directors in Vascular Surgery Spring Meeting, Chicago, Ill, March 30, 2019.
Additional material for this article may be found online at www.jvascsurg.org.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
REFERENCES
- 1.Maslach C, Jackson S, Leiter M. The Maslach burnout inventory manual. In: Zalaquett CP, Wood RJ, editors. Evaluating stress: a book of resources. Lanham MD: The Scarecrow Press; 1997. p. 191–218. [Google Scholar]
- 2.Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med 2018;178: 1317–30. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 3.Hamidi MS, Bohman B, Sandborg C, Smith-Coggins R, de Vries P, Albert MS, et al. Estimating institutional physician turnover attributable to self-reported burnout and associated financial burden: a case study. BMC Health Serv Res 2018;18:851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coleman DMM, Money SR, Meltzer AJ, Wohlauer M, Drudi LM, Freischlag JA, et al. Vascular surgeon wellness and burnout - a report from the SVS Wellness Task Force. J Vasc Surg 2020. Nov 25. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 5.Chen H, Reddy RM, Palmer SW, Coleman DM, Hoch JR, DiMusto PD, et al. Attrition rates in integrated vascular and cardiothoracic surgery residency and fellowship programs. J Vasc Surg 2019;69:236–41. [DOI] [PubMed] [Google Scholar]
- 6.Hekman KE, Wohlauer MV, Magee GA, Shokrzadeh CL, Brown KR, Carsten CG 3rd, et al. Current issues and future directions for vascular surgery training from the results of the 2016–2017 and 2017–2018 Association of Program Directors in Vascular Surgery annual training survey. J Vasc Surg 2019;70:2014–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janko MR, Smeds MR. Burnout, depression, perceived stress, and self-efficacy in vascular surgery trainees. J Vasc Surg 2019;69: 1233–42. [DOI] [PubMed] [Google Scholar]
- 8.Elmore LC, Jeffe DB, Jin L, Awad MM, Turnbull IR. National survey of burnout among US general surgery residents. J Am Coll Surg 2016;223:440–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kent S, Devonport TJ, Lane AM, Nicholls W, Friesen AP. The effects of coping interventions on ability to perform under pressure. J Sports Sci Med 2018;17:40–55. [PMC free article] [PubMed] [Google Scholar]
- 10.Dalsing MC, Makaroun MS, Harris LM, Mills JL, Eidt J, Eckert GJ. Association of Program Directors in Vascular Surgery (APDVS) survey of program selection, knowledge acquisition, and education provided as viewed by vascular trainees from two different training paradigms. J Vasc Surg 2012;55:588–97; discussion: 598. [DOI] [PubMed] [Google Scholar]
- 11.Souba WW. Mentoring young academic surgeons, our most precious asset. J Surg Res 1999;82:113–20. [DOI] [PubMed] [Google Scholar]
- 12.Gofton W, Regehr G. Factors in optimizing the learning environment for surgical training. Clin Orthop Relat Res 2006;449:100–7. [DOI] [PubMed] [Google Scholar]
- 13.Gofton W, Regehr G. What we don’t know we are teaching: unveiling the hidden curriculum. Clin Orthop Relat Res 2006;449:20–7. [DOI] [PubMed] [Google Scholar]
- 14.Gruppen LD, Stansfield RB, Zhao Z, Sen S. Institution and specialty contribute to resident satisfaction with their learning environment and workload. Acad Med 2015;90(11 Suppl):S77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grantcharov TP, Reznick RK. Training tomorrow’s surgeons: what are we looking for and how can we achieve it? ANZ J Surg 2009;79: 104–7. [DOI] [PubMed] [Google Scholar]
- 16.Korentager R, editor. Mentoring and Modeling Professionalism: clinical care. American Council of Academic Plastic Surgeons Winter Retreat. Chicago, IL: Wolters Kluwer Health; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Entezami P, Franzblau LE, Chung KC. Mentorship in surgical training: a systematic review. Hand (N Y) 2012;7:30–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ford HR. Mentoring, diversity, and academic surgery. J Surg Res 2004;118:1–8. [DOI] [PubMed] [Google Scholar]
- 19.Franzblau LE, Kotsis SV, Chung KC. Mentorship: concepts and application to plastic surgery training programs. Plast Reconstr Surg 2013;131:837e–43e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pellegrini VD Jr. Mentoring during residency education: a unique challenge for the surgeon? Clin Orthop Relat Res 2006;449:143–8. [DOI] [PubMed] [Google Scholar]
- 21.Konstantakos AK. Surgical education and the mentor–student relationship. Curr Surg 2003;60:547–8. [DOI] [PubMed] [Google Scholar]
- 22.Pinto A, Faiz O, Bicknell C, Vincent C. Acute traumatic stress among surgeons after major surgical complications. Am J Surg 2014;208: 642–7. [DOI] [PubMed] [Google Scholar]
- 23.Timpka T, Jacobsson J, Dahlström Ö, Kowalski J, Bargoria V, Ekberg J, et al. The psychological factor ‘self-blame’ predicts overuse injury among top-level Swedish track and field athletes: a 12-month cohort study. Br J Sports Med 2015;49:1472–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


