Key Points
Question
What is the association between geospatial access to trauma center care and firearm injury mortality in a mature urban trauma system?
Findings
In this cohort study, among 10 105 people shot due to interpersonal violence in Philadelphia, Pennsylvania, from 2015 to 2021, longer predicted ground transport time was associated with an increase in risk-adjusted odds of death.
Meaning
Geospatial access to care is an important trauma system measure in urban environments; the findings in this study suggest that improvements in access to care may reduce deaths from gun violence.
This cohort study evaluates associations between geospatial access to trauma center care and mortality from firearm injury in Philadelphia, Pennsylvania.
Abstract
Importance
The burden of firearm violence in US cities continues to rise. The role of access to trauma center care as a trauma system measure with implications for firearm injury mortality has not been comprehensively evaluated.
Objective
To evaluate the association between geospatial access to care and firearm injury mortality in an urban trauma system.
Design, Setting, and Participants
Retrospective cohort study of all people 15 years and older shot due to interpersonal violence in Philadelphia, Pennsylvania, between January 1, 2015, and August 9, 2021.
Exposures
Geospatial access to care, defined as the predicted ground transport time to the nearest trauma center for each person shot, derived by geospatial network analysis.
Main Outcomes and Measures
Risk-adjusted mortality estimated using hierarchical logistic regression. The population attributable fraction was used to estimate the proportion of fatalities attributable to disparities in geospatial access to care.
Results
During the study period, 10 105 people (910 [9%] female and 9195 [91%] male; median [IQR] age, 26 [21-28] years; 8441 [84%] Black, 1596 [16%] White, and 68 other [<1%], including Asian and unknown, consolidated owing to small numbers) were shot due to interpersonal violence in Philadelphia. Of these, 1999 (20%) died. The median (IQR) predicted transport time was 5.6 (3.8-7.2) minutes. After risk adjustment, each additional minute of predicted ground transport time was associated with an increase in odds of mortality (odds ratio [OR], 1.03 per minute; 95% CI, 1.01-1.05). Calculation of the population attributable fraction using mortality rate ratios for incremental 1-minute increases in predicted ground transport time estimated that 23% of shooting fatalities could be attributed to differences in access to care, equivalent to 455 deaths over the study period.
Conclusions and Relevance
These findings indicate that geospatial access to care may be an important trauma system measure, improvements to which may result in reduced deaths from gun violence in US cities.
Introduction
Firearm violence is a public health crisis in the US. More than 120 000 people are shot annually, and 34 000 die from their injuries.1,2 Firearm injury due to interpersonal violence is a predominantly urban phenomenon.1 The burden of people shot in US cities has continued to rise, even more so since the arrival of SARS-CoV-2 has stressed vulnerable communities.3,4
Patients who have sustained gunshot wounds frequently require urgent surgical intervention. In these patients, rapid transport to a trauma center and early operative management are important determinants of survival.5,6 System-wide policies that minimize prehospital delays and prioritize scoop-and-run practices to expedite access to care for those shot can save lives.7,8 Conversely, delayed access to trauma center care is associated with worse mortality.9,10 While previous studies have characterized geospatial access to trauma resources as a trauma system measure,11,12,13,14,15 to our knowledge, the association of access to care with firearm injury mortality in an urban trauma system has not been comprehensively evaluated. As the epidemic of gun violence persists, quantifying the role of timely access to care may help to guide resource allocation with the goal of reducing deaths from firearm violence in US cities.
We hypothesized that delayed access to care is associated with worse survival for those shot due to gun violence, and that this association contributes to the observed rate of firearm homicide system wide. The objective of this study was to measure the association between geospatial access to trauma center care and mortality for those shot in Philadelphia, Pennsylvania, and to estimate the proportion of gun violence deaths that might be attributable to variable access to care.
Methods
Study Design
This was a retrospective cohort study including people injured due to firearm violence in Philadelphia between January 1, 2015, and August 9, 2021. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. The project was approved by the University of Pennsylvania Institutional Review Board, Philadelphia. All data were publicly available and deidentified; therefore informed consent was not required.
Data Sources
Mapping Data
Data used for mapping and geospatial analyses were derived from multiple sources. A base map of Philadelphia county was obtained from OpenDataPhilly.16 State-designated level 1 and 2 trauma centers in Philadelphia and surrounding counties were identified from the Pennsylvania Trauma System Foundation.17 A network data set of US streets obtained from ESRI ArcGIS StreetMap Premium18 was used for geospatial analyses of Philadelphia roads (eFigure in the Supplement).
Philadelphia Shooting Victims Data
Data for people injured due to gun violence were obtained from the Philadelphia Police Department’s registry of shooting victims.19 This data set includes individual-level data for all people shot as the result of interpersonal violence since 2015. Only shootings classified by police as criminal in nature were included; therefore, injuries resulting from self-harm were excluded. Variables captured include time and date, baseline demographic characteristics, documented wounds, indoor (vs outdoor) shooting location, and whether the injured person died. Geospatial coordinates were included, allowing for each shooting to be mapped. Race data were included in this study due to known race-based disparities in gun violence. Categories of race are presented in keeping with the manner they were recorded in police records. Asian and unknown race categories were consolidated as they represented 0.6% of the study population.
Study Population
All individuals 15 years and older who were shot as a result of interpersonal violence were included. Records for officer-involved shootings (n = 88) lacked location information and were therefore excluded.
Derivation of the Exposure: Geospatial Access to Trauma Center Care
The exposure was defined as the predicted ground transport time to the nearest trauma center. Shooting locations and trauma centers were mapped using ArcMap version 10.5 (ESRI ArcGIS). Network analysis was then performed to identify the nearest trauma center and calculate predicted transport time for each person shot. Network analysis uses road segment characteristics in a street network data set to determine geospatial relationships between points on the network. This technique has been previously demonstrated as a geospatial approach for the quantitative analysis of trauma center access.12 The closest facilities solver in ArcMap Network Analyst was used to determine the route to nearest trauma center along public roads for each person shot. Predicted transport time was estimated by applying time as the impedance along each route with emergency vehicle selected as the travel mode. In this way, predicted transport time represented the fastest possible travel time to the nearest trauma center for each person shot—a measure of geospatial access to trauma care.
The status of trauma centers in Philadelphia changed during the study period (eTable 1 in the Supplement). Specifically, the Trauma Center at Penn moved from the Hospital of the University of Pennsylvania to Penn Presbyterian Medical Center at noon on February 4, 2015; Lankenau Medical Center opened as a level 2 trauma center on September 1, 2016; and Hahnemann University Hospital closed as a level 1 trauma center on June 29, 2019. To account for these changes in trauma center location, predicted transport times were calculated separately for each intervening time period.
Outcome
The outcome was firearm injury mortality. Mortality information was recorded for each person shot in the Philadelphia Police Department’s registry. These data are updated with police homicide records and therefore account for changes to mortality status over time.
Potential Confounders
We considered several variables that might confound the measured association between predicted transport time and mortality. Baseline demographic characteristics (age, sex, and race), injury characteristics (anatomic location of gunshot wounds), and event characteristics (indoors vs outdoors shooting location, time of day, and season) were derived. Time of day was operationalized in 6-hour increments (midnight to 6 am, 6am to noon, noon to 6pm, and 6 pm to midnight). Season was operationalized as spring (March through May), summer (June through August), fall (September through November) and winter (December through February). The level of state trauma center designation (level 1 vs level 2) of the nearest trauma center was also considered.
Anatomic location of gunshot wounds was recorded for each person shot in the data set from police records. Because these data do not follow a standardized system for abstraction, wounds were grouped into broad anatomic categories: head, neck, torso, extremity, and multiple wounds. The derivation of these categories from available descriptors is provided in eTable 2 in the Supplement.
Age was the only variable missing in fewer than 1% of records (n = 58). Missing values were imputed using a multiple imputation technique.20
Statistical Analysis
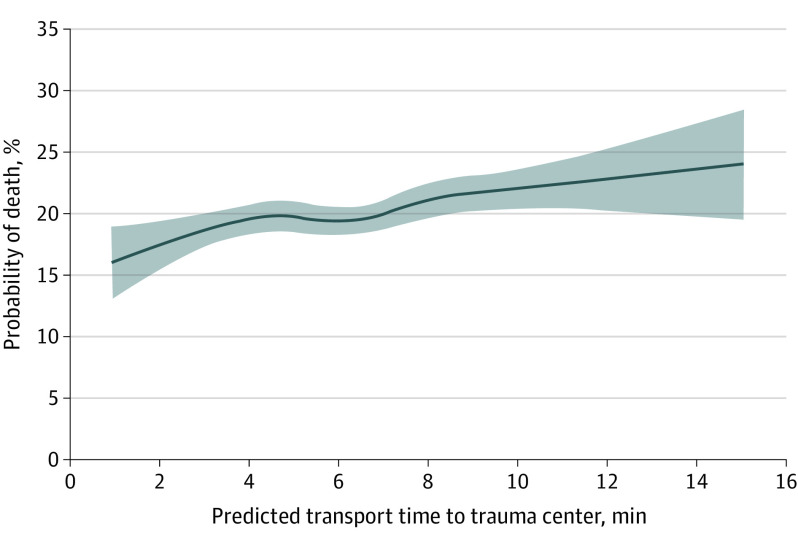
Univariable comparison was made between characteristics of fatal and nonfatal shootings. Wilcoxon rank sum and χ2 tests were used to compare median values and frequencies of categorical variables, respectively. The unadjusted probability of death after firearm injury was plotted as a function of increasing predicted transport time using locally estimated scatterplot smoothing.21
Two analytic approaches were then used to meet the stated study objectives. First, a hierarchical logistic regression model was used to estimate the risk-adjusted association between geospatial access to care and mortality at the individual level. To account for neighborhood-level characteristics not captured by fixed effects, the model included a random intercept term to account for clustering of shootings within zip codes.22,23 Potential confounders were evaluated for inclusion using a combination of the 10% change-in-estimate approach described by Mickey and Greenland24 and significance in univariable comparisons. The final model included variables that changed the exposure point estimate by more than 10% or differed significantly between fatal and nonfatal shootings. Multicollinearity was ruled out using the variance inflation factor and tolerance statistic. Model calibration was ensured using the Hosmer-Lemeshow goodness-of-fit test and model discrimination is reported using the C statistic. A sensitivity analysis was performed limiting the study cohort to those with gunshot injuries most likely to be life threatening and time sensitive: truncal (neck or torso) or multiple gunshot wounds.
Second, we estimated the proportion of shooting fatalities that might be attributable to variable access to care using the population attributable fraction. The population attributable fraction is an epidemiologic measure, defined as the fraction of all cases (in this study, shooting fatalities) in a population that could be attributed to a specific exposure (in this study, geospatial access to care) assuming a causal association.25 To accomplish this, concentric 1-minute service areas of increasing predicted transport time (≤1 minute to >15 minutes) were mapped. Case fatality rates were calculated for the populations of people shot within each service area. Mortality rate ratios were then estimated for each service area using a negative binomial model, with the fastest possible theoretical access to care (predicted transport time ≤1 minute) defined as the reference category. Mortality rate ratios were risk adjusted for the case mix within each category of access to care. The population attributable fraction was then calculated using the formula described by Rockhill et al26 and Miettinen27:
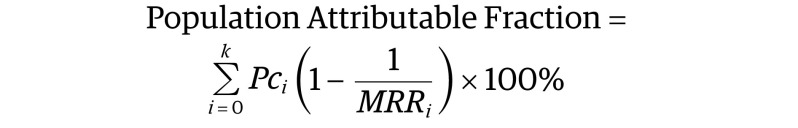 |
where Pci was the proportion of all shooting deaths that occurred in the ith service area of predicted ground transport time, and MRRi was the adjusted mortality rate ratio in the ith service area compared to the reference (i = 0; in this case, predicted transport time ≤1 minute). In this way, the number and proportion of shooting fatalities attributable to the association between variable access to care and mortality was estimated.
Mapping and geospatial analyses were performed using ArcMap version 10.5 (ESRI ArcGIS). Statistical analyses were performed using SAS statistical software version 9.4 (SAS Institute). Threshold for statistical significance was set to P < .05.
Results
During the study, period 10 105 people 15 years and older were shot in Philadelphia (910 [9%] female and 9195 [91%] male; median [IQR] age, 26 [21-28] years; 8441 [84%] Black, 1596 [16%] White, and 68 other [<1%], including Asian and unknown). Shootings occurred with greatest frequency during summer months (June through August; n = 3132 [31%]) and between the hours of 6 pm and midnight (n = 4244 [42%]). Most shootings occurred outdoors (n = 9599 [95%]). The median (IQR) predicted ground transport time was 5.6 (3.8-7.2) minutes. A total of 1999 individuals who were shot (20%) died.
Table 1 compares characteristics between fatal and nonfatal shootings. Head, torso, and multiple wounds were associated with fatality, as were indoor shootings and those that occurred during winter months. Figure 1 shows the plot of unadjusted probability of death as a function of increasing predicted transport time. Longer predicted ground transport time was associated with higher probability of mortality in a near linear fashion.
Table 1. Comparison of Characteristics Between Fatal and Nonfatal Shootings.
| Parameter | No. (%) | P value | |
|---|---|---|---|
| Fatal (n = 1999) | Nonfatal (n = 8106) | ||
| Baseline characteristics | |||
| Age, median (IQR), y | 28 (22-35) | 26 (21-33) | <.001 |
| Female | 154 (7.7) | 740 (9.1) | .045 |
| Male | 1845 (92.3) | 7366 (90.9) | |
| Racea | 1675 (83.8) | 6766 (83.5) | |
| Black | 1675 (83.8) | 6766 (83.5) | .62 |
| White | 308 (15.4) | 1288 (15.9) | |
| Otherb | 16 (0.8) | 52 (0.6) | |
| Injury characteristics | |||
| Head wound | 779 (39.0) | 586 (7.2) | <.001 |
| Neck wound | 29 (1.5) | 99 (1.2) | .41 |
| Torso wound | 474 (23.7) | 1568 (19.3) | <.001 |
| Extremity wound | 45 (2.3) | 3725 (46.0) | <.001 |
| Multiple wounds | 948 (47.4) | 2257 (27.8) | <.001 |
| Event characteristics | |||
| Indoor shooting | 199 (10.0) | 331 (4.1) | <.001 |
| Time of day | |||
| Midnight to 6 am | 473 (23.7) | 1807 (22.3) | .03 |
| 6 am to noon | 270 (13.5) | 997 (12.3) | |
| Noon to 6 pm | 482 (24.1) | 1867 (23.0) | |
| 6 pm to midnight | 774 (38.7) | 3435 (42.4) | |
| Season | |||
| Spring (Mar-May) | 495 (24.8) | 1986 (24.5) | <.001 |
| Summer (Jun-Aug) | 569 (28.4) | 2583 (31.9) | |
| Fall (Sept-Nov) | 465 (23.2) | 1955 (24.1) | |
| Winter (Dec-Feb) | 470 (23.5) | 1582 (19.5) | |
| Level of nearest trauma center | |||
| Level 1 (vs level 2) | 1856 (92.9) | 7597 (93.7) | .15 |
| Access to nearest trauma center | |||
| Predicted transport time, median (IQR), min | 5.7 (4.0-7.4) | 5.5 (3.8-7.2) | .002 |
Race data were included in this study due to known race-based disparities in gun violence. Categories of race are presented in keeping with the manner they were recorded in police records.
Other included Asian and unknown, consolidated because they represented 0.6% of the study population.
Figure 1. Unadjusted Association Between Increasing Predicted Transport Time to Nearest Trauma Center and Probability of Death for Individuals Shot.
Shading indicates 95% CIs.
Hierarchical Model for Shooting Fatality
Results of the multivariable logistic regression model for mortality are shown in Table 2. Model discrimination was excellent (C statistic, 0.81). Head, torso, and multiple wounds were independently associated with mortality, as were indoor and winter shootings. Extremity gunshot wounds were strongly associated with survival. After risk adjustment, predicted transport time to the nearest trauma center was significantly associated with shooting fatality. Specifically, each additional minute of predicted transport time was associated with a 3% increase in odds of death (odds ratio [OR], 1.03 per minute; 95% CI, 1.01-1.05).
Table 2. Multivariable Model for Shooting Fatality.
| Parameter | Odds of fatality (95% CI) |
|---|---|
| Access to nearest trauma center | |
| Predicted transport time (per 1-min increase) | 1.03 (1.01-1.05) |
| Baseline characteristics | |
| Age (per 1-y increase) | 1.01 (1.01-1.02) |
| Female sex (vs male) | 0.82 (0.66-1.02) |
| Injury characteristics | |
| Head wound | 5.10 (4.21-6.19) |
| Torso wound | 1.34 (1.05-1.70) |
| Extremity wound | 0.05 (0.04-0.08) |
| Multiple wounds | 1.45 (1.18-1.79) |
| Event characteristics | |
| Indoor shooting | 2.03 (1.62-2.54) |
| Time of day | |
| Midnight to 6 am | 1.15 (0.99-1.33) |
| 6 am to noon | 1.10 (0.92-1.32) |
| Noon to 6 pm | 1.07 (0.93-1.24) |
| 6 pm to midnight | 1 [Reference] |
| Season | |
| Summer (Jun-Aug) | 1 [Reference] |
| Fall (Sept-Nov) | 1.14 (0.98-1.33) |
| Winter (Dec-Feb) | 1.25 (1.07-1.47) |
| Spring (Mar-May) | 1.11 (0.96-1.30) |
Results of the sensitivity analysis in which the patient cohort was limited to truncal or multiple gunshot wounds (n = 4970) are shown in eTable 3 in the Supplement. The risk-adjusted association between access to care and mortality was no different among this cohort (OR, 1.03 per minute; 95% CI, 1.01-1.05).
Contribution of Variable Access to Care to Shooting Fatalities
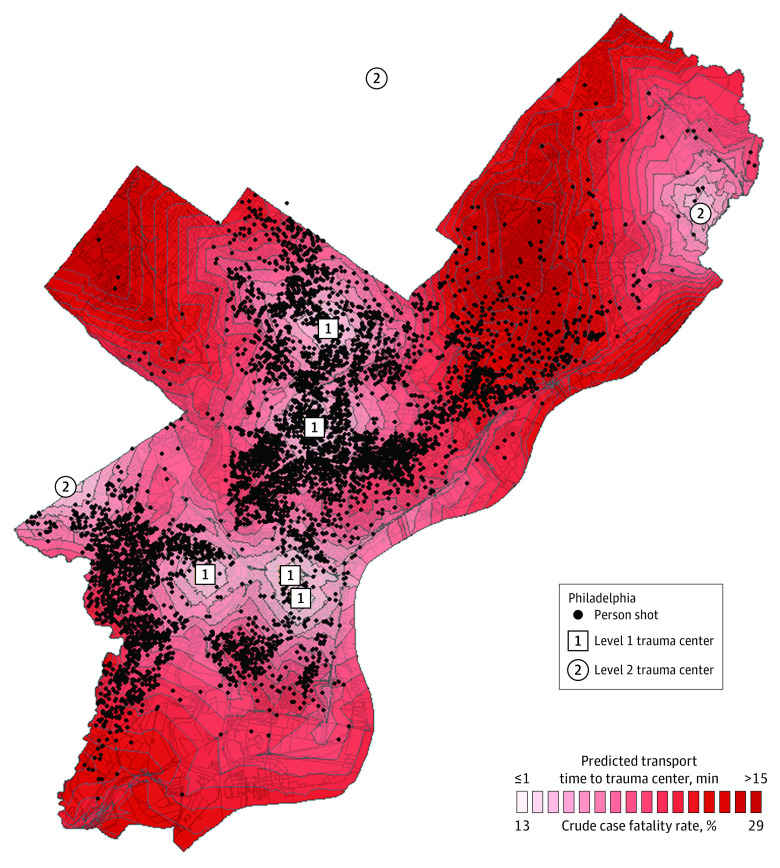
The population attributable fraction was calculated to estimate the proportion of shooting fatalities that could be attributable to variable access to care. Concentric 1-minute service areas of increasing predicted transport time are mapped in Figure 2. The case fatality rate for people shot increased from 13% (29 of 232 shootings) in the service area with quickest potential access to care (predicted transport time ≤1 minute) to 29% (7 of 24 shootings) in the service area with most delayed access to care (predicted transport time >15 minutes). Risk-adjusted mortality rate ratios estimated for shootings at increasing ranges of predicted ground transport time are shown in eTable 4 in the Supplement. The resulting population attributable fraction was 23%, equivalent to an estimated 455 fatalities during the study period.
Figure 2. Map Showing Concentric 1-Minute Service Areas of Increasing Predicted Ground Transport Time to Nearest Trauma Center for Individuals Shot in Philadelphia.
The case fatality rate of shootings increased from 13% in the service area of shortest predicted transport time (≤1 minute) to 29% in the service area of longest predicted transport time (>15 minutes).
Discussion
In this retrospective cohort study of people shot in Philadelphia, geospatial access to trauma care was significantly associated with survival. Specifically, each additional minute of predicted ground transport time to the nearest trauma center was associated with increased odds of mortality. An estimated 23% of observed fatalities could be attributed to this association owing to differences in access to care across the population of people shot.
These data provide new evidence that the variable nature of access to trauma center care matters in the struggle to reduce deaths from gun violence. Previous studies have evaluated the association of access to care with deaths from firearm injury. Crandall et al10 found that people shot more than 5 miles from trauma centers in Chicago, Illinois, in so-called trauma deserts, were more likely to die. Crandall et al9 later found that closure of an urban level 1 trauma center in Los Angeles, California, was followed by a rise in shooting fatalities in the surrounding catchment. Drawbacks to these studies were that they considered only straight-line distance as a dichotomized measure of access or the catchment area of a single hospital. In contrast, we evaluated the full spectrum of access to care as a continuous measure for all people shot using network analysis, a geospatial technique validated for quantifying access within trauma systems.12 Our findings therefore provide evidence that system-level interventions to improve access to definitive trauma care may result in a tangible reduction in firearm injury mortality.
We used the population attributable fraction to provide a meaningful estimate of the net contribution of the association between access to care and mortality to observed fatalities citywide. This analysis was important to account for variation in the geospatial distribution of shootings relative to trauma centers. For example, if the observed association were relatively minor, the contribution of disparities in access to care to observed fatalities would be small. Similarly, if few shootings occurred in neighborhoods with greater delays in access, this association would translate to few deaths. Rather, we estimated that 23% of fatalities were attributable to differences in access to trauma center care. It is important to note that this calculation assumes a causal relationship, which cannot be interpreted from this observational study. Furthermore, the estimate may be subject to residual confounding due to unmeasured factors. However, within these limitations, the findings suggest that local policy makers should consider investing in improved trauma center access as a systems approach to reducing deaths from gun violence in US cities.
Improved access to trauma care can be achieved in urban environments through various interventions, each with benefits and drawbacks. Police transport is one potential means. Since police are often first to arrive at the scene of a shooting, police transport results in quicker arrival at definitive care (so-called scoop-and-run) and fewer prehospital delays (so-called stay-and-play).7,28,29 The Philadelphia Police Department has practiced this under a directive with increasing frequency such that in 2018 nearly 80% of patients treated for gunshot wounds arrived by police transport.30,31 While implementing such a policy is challenging, police transport is associated with lower risk-adjusted mortality32 and anecdotal perceptions from patients, police, and trauma clinicians are that the practice saves lives.33
Another approach to improving access to care is to prioritize early notification. The response of police and emergency medical services to shootings is variable across an urban built environment. Use of acoustic sensor technology (eg, ShotSpotter) has been shown to hasten activation of emergency services and reduce both response and total prehospital times for patients transported by police or ambulance.34
Complementary to interventions that emphasize the prehospital system, optimizing the location of trauma resources represents another target for system-level improvement. Geospatial analysis provides a powerful means to identify discrepancies between injury locations and trauma center distribution.11,12,13,14,15 Bringing trauma care to shooting hotspots with poor access could shorten transport times and provide opportunities for rescuing people with time-sensitive injuries. This might take the form of building trauma capabilities at non-trauma hospitals or military treatment facilities.35 Taken together, each urban trauma system must be evaluated uniquely to determine where shortfalls exist and which approaches to improving access to care will yield the greatest population benefit.
Limitations
This study has several limitations. Perhaps most important is the potential for unmeasured confounding. Specifically, real-world data pertaining to prehospital times, mode of transport, injury diagnoses, destination hospital, or in-hospital course were not available. However, not all unmeasured variables are confounders. Confounding would occur only if these factors differed systematically across the spectrum of access to care. We have no evidence that such systematic differences in prehospital care or injury severity exist within the confined geographic area of urban Philadelphia. Furthermore, by accounting for clustering of shootings within zip codes in our hierarchical model, neighborhood-level differences in mortality risk due to unmeasured confounding would be further minimized. Therefore, it is unlikely that the observed association between access to care and mortality is due to confounding.
Second, the study exposure—predicted ground transport time to the nearest trauma center—is a geospatial measure that represents the fastest possible access to care. We are unable to know how close the system came to achieving this estimate for each person shot. However, while prehospital times and transport mode will vary, the geospatial estimate of access to care is likely a valid analog that is proportional to the real-world scenario.
Third, locations of death were not available for analysis. Therefore, the proportion of fatalities that occurred in the prehospital environment is unknown. While the opportunity to evaluate prehospital mortality would lend construct validity to our findings, there is no statistical or biological rationale for excluding these cases. On the contrary, prehospital deaths represent a natural extreme of delayed access to care in individuals with time-sensitive injuries and should be included in analyses such as ours that seek to make probabilistic estimates of mortality risk.
Fourth, while we included all people shot in our primary analysis, not all injuries are time sensitive. Therefore, the results of this analysis may not be generalizable to all patients. For example, gunshot wounds to the head are more likely to be fatal irrespective of timely access to care. For this reason, we performed a sensitivity analysis limited to individuals with penetrating truncal injuries or multiple gunshot wounds (excluding head wounds). The results were unchanged. Furthermore, the C statistic for our multivariable models exceeded 0.8, indicating excellent accuracy in predicting mortality irrespective of differing patterns of injury.
Fifth, the generalizability of our results to other cities is uncertain. Nearly 80% of individuals shot in Philadelphia are transported by police and the geographic density of trauma centers is high. Given that these system characteristics should reflect fast access to definitive care, our findings are more notable. This association is likely to be even more pronounced in urban trauma systems where characteristics are less favorable for quick access to care.
Conclusions
In this retrospective cohort study of individuals shot in a mature urban trauma system, each additional minute of predicted ground transport time to the nearest trauma center was associated with increased mortality. This association was estimated to contribute to 23% of fatalities owing to differences in access to care. These findings indicate that geospatial access to care may represent an important trauma system measure, improvements to which may result in reduced deaths from gun violence in US cities.
eFigure. Philadelphia roads map derived from network dataset of US streets
eTable 1. Trauma Centers in Philadelphia and Surrounding Counties
eTable 2. Derivation of Wound Locations from Wound Descriptors in Shooting Victims Dataset
eTable 3. Sensitivity Analysis: Multivariable model of cohort with penetrating truncal or multiple injuries
eTable 4. Calculation of the Population Attributable Fraction of Shooting Fatalities due to Variable Access to Trauma Care
References
- 1.Kaufman EJ, Wiebe DJ, Xiong RA, Morrison CN, Seamon MJ, Delgado MK. Epidemiologic trends in fatal and nonfatal firearm injuries in the US, 2009-2017. JAMA Intern Med. 2021;181(2):237-244. doi: 10.1001/jamainternmed.2020.6696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldstick JE, Zeoli A, Mair C, Cunningham RMUS. US firearm-related mortality: national, state, and population trends, 1999-2017. Health Aff. 2019;38(10):1646-1652. doi: 10.1377/hlthaff.2019.00258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chodos M, Sarani B, Sparks A, et al. Impact of COVID-19 pandemic on injury prevalence and pattern in the Washington, DC Metropolitan Region: a multicenter study by the American College of Surgeons Committee on Trauma, Washington, DC. Trauma Surg. 2021;6(1). doi: 10.1136/tsaco-2020-000659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beard JH, Jacoby SF, Maher Z, et al. Changes in shooting incidence in Philadelphia, Pennsylvania, between March and November 2020. JAMA. 2021;325(13):1327-1328. doi: 10.1001/jama.2021.1534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meizoso JP, Ray JJ, Karcutskie CA IV, et al. Effect of time to operation on mortality for hypotensive patients with gunshot wounds to the torso: the golden 10 minutes. J Trauma Acute Care Surg. 2016;81(4):685-691. doi: 10.1097/TA.0000000000001198 [DOI] [PubMed] [Google Scholar]
- 6.Swaroop M, Straus DC, Agubuzu O, Esposito TJ, Schermer CR, Crandall ML. Pre-hospital transport times and survival for hypotensive patients with penetrating thoracic trauma. J Emerg Trauma Shock. 2013;6(1):16-20. doi: 10.4103/0974-2700.106320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seamon MJ, Fisher CA, Gaughan J, et al. Prehospital procedures before emergency department thoracotomy: “scoop and run” saves lives. J Trauma. 2007;63(1):113-120. doi: 10.1097/TA.0b013e31806842a1 [DOI] [PubMed] [Google Scholar]
- 8.Winter E, Hynes AM, Shultz K, Holena DN, Malhotra NR, Cannon JW. Association of police transport with survival among patients with penetrating trauma in Philadelphia, Pennsylvania. JAMA Netw Open. 2021;4(1):e2034868. doi: 10.1001/jamanetworkopen.2020.34868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crandall M, Sharp D, Wei X, Nathens A, Hsia RY. Effects of closure of an urban level I trauma centre on adjacent hospitals and local injury mortality: a retrospective, observational study. BMJ Open. 2016;6(5):e011700. doi: 10.1136/bmjopen-2016-011700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crandall M, Sharp D, Unger E, et al. Trauma deserts: distance from a trauma center, transport times, and mortality from gunshot wounds in Chicago. Am J Public Health. 2013;103(6):1103-1109. doi: 10.2105/AJPH.2013.301223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown JB, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL. Geographic distribution of trauma centers and injury-related mortality in the United States. J Trauma Acute Care Surg. 2016;80(1):42-49. doi: 10.1097/TA.0000000000000902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Winchell RJ, Xu P, Mount LE, Huegerich R. Development of a geospatial approach for the quantitative analysis of trauma center access. J Trauma Acute Care Surg. 2019;86(3):397-405. doi: 10.1097/TA.0000000000002156 [DOI] [PubMed] [Google Scholar]
- 13.Jansen JO, Morrison JJ, Wang H, et al. Optimizing trauma system design: the GEOS (Geospatial Evaluation of Systems of Trauma Care) approach. J Trauma Acute Care Surg. 2014;76(4):1035-1040. doi: 10.1097/TA.0000000000000196 [DOI] [PubMed] [Google Scholar]
- 14.Horst MA, Jammula S, Gross BW, et al. Development of a trauma system and optimal placement of trauma centers using geospatial mapping. J Trauma Acute Care Surg. 2018;84(3):441-448. doi: 10.1097/TA.0000000000001782 [DOI] [PubMed] [Google Scholar]
- 15.Brown JB, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL. Distance matters: effect of geographic trauma system resource organization on fatal motor vehicle collisions. J Trauma Acute Care Surg. 2017;83(1):111-118. doi: 10.1097/TA.0000000000001508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.OpenDataPhilly . Zip codes (2014). Accessed February 1, 2021. https://www.opendataphilly.org/dataset/zip-codes
- 17.Pennsylvania Trauma System Foundation . Find a trauma center (2021). Accessed February 1, 2021. https://www.ptsf.org/trauma-center/
- 18.ESRI . ArcGIS StreetMap premium (2021). Accessed February 1, 2021. https://www.openstreetmap.org/
- 19.OpenDataPhilly . Shooting victims (2021). Accessed February 1, 2021. https://metadata.phila.gov/#home/datasetdetails/5719551277d6389f3005a610/representationdetails/5719551277d6389f3005a614/
- 20.Yuan Y. Multiple imputation using SAS software. J Stat Softw. 2011;45(6):1-25. doi: 10.18637/jss.v045.i06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cohen R. An introduction to PROC LOESS for local regression: SAS Institute Inc., Cary, North Carolina, USA 1998. Accessed February 1, 2021. https://stats.idre.ucla.edu/wp-content/uploads/2016/02/loesssugi.pdf
- 22.Merlo J, Yang M, Chaix B, Lynch J, Råstam L. A brief conceptual tutorial on multilevel analysis in social epidemiology: investigating contextual phenomena in different groups of people. J Epidemiol Community Health. 2005;59(9):729-736. doi: 10.1136/jech.2004.023929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hubbard AE, Ahern J, Fleischer NL, et al. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology. 2010;21(4):467-474. doi: 10.1097/EDE.0b013e3181caeb90 [DOI] [PubMed] [Google Scholar]
- 24.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129(1):125-137. doi: 10.1093/oxfordjournals.aje.a115101 [DOI] [PubMed] [Google Scholar]
- 25.Mansournia MA, Altman DG. Population attributable fraction. BMJ. 2018;360:k757. doi: 10.1136/bmj.k757 [DOI] [PubMed] [Google Scholar]
- 26.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88(1):15-19. doi: 10.2105/AJPH.88.1.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miettinen OS. Proportion of disease caused or prevented by a given exposure, trait or intervention. Am J Epidemiol. 1974;99(5):325-332. doi: 10.1093/oxfordjournals.aje.a121617 [DOI] [PubMed] [Google Scholar]
- 28.Van Brocklin E. The trace: ’scoop and run’ can save lives. why don’t more police departments try it? Accessed July 1, 2021. https://www.thetrace.org/2018/11/scoop-and-run-gunshot-victim-police-transport/
- 29.Seamon MJ, Doane SM, Gaughan JP, et al. Prehospital interventions for penetrating trauma victims: a prospective comparison between advanced life support and basic life support. Injury. 2013;44(5):634-638. doi: 10.1016/j.injury.2012.12.020 [DOI] [PubMed] [Google Scholar]
- 30.Philadelphia Police Department . Directive 3.14. subject: hospital cases. Accessed July 1, 2021. https://www.phillypolice.com/assets/directives/D3.14-HospitalCases.pdf
- 31.Maher Z, Beard JH, Dauer E, et al. Police transport of firearm-injured patients-more often and more injured. J Trauma Acute Care Surg. 2021;91(1):164-170. doi: 10.1097/TA.0000000000003225 [DOI] [PubMed] [Google Scholar]
- 32.Band RA, Salhi RA, Holena DN, Powell E, Branas CC, Carr BG. Severity-adjusted mortality in trauma patients transported by police. Ann Emerg Med. 2014;63(5):608-614.e3. doi: 10.1016/j.annemergmed.2013.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jacoby SF, Branas CC, Holena DN, Kaufman EJ. Beyond survival: the broader consequences of prehospital transport by police for penetrating trauma. Trauma Surg. 2020;5(1):e000541. doi: 10.1136/tsaco-2020-000541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goldenberg A, Rattigan D, Dalton M, et al. Use of ShotSpotter detection technology decreases prehospital time for patients sustaining gunshot wounds. J Trauma Acute Care Surg. 2019;87(6):1253-1259. doi: 10.1097/TA.0000000000002483 [DOI] [PubMed] [Google Scholar]
- 35.Lee BC, McEvoy CS, Ross-Li D, et al. Building trauma capability: using geospatial analysis to consider military treatment facilities for trauma center development. Trauma Surg Acute Care Open. 2022;7(1):e000832. doi: 10.1136/tsaco-2021-000832 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Philadelphia roads map derived from network dataset of US streets
eTable 1. Trauma Centers in Philadelphia and Surrounding Counties
eTable 2. Derivation of Wound Locations from Wound Descriptors in Shooting Victims Dataset
eTable 3. Sensitivity Analysis: Multivariable model of cohort with penetrating truncal or multiple injuries
eTable 4. Calculation of the Population Attributable Fraction of Shooting Fatalities due to Variable Access to Trauma Care