Abstract
Background
The COVID-19 outbreak has affected the aviation sector. The anxiety and fear caused by this newly emerging virus, whose effects are not fully known in the short and long term, may also cause problems in terms of flight safety. We aimed to evaluate fatigue and sleep problems associated with fear of COVID-19 during the early pandemic period in cabin crew.
Methods
This is a cross-sectional survey study consisting of 45 questions in total. Participants were cabin crew members on flight duty. An online questionnaire was sent to 2092 cabin crew in February–April 2021 via TASSA Cabin Crew Member's Association. The survey included questions about socio-demographic characteristics, flight times, flight types and COVID test history, as well as the international physical activity questionnaire-short form (IPAQ-SF), fatigue severity scale (FSS), Jenkins sleep scale (JSS) and fear of COVID-19 scale (FCV-19S).
Results
Out of 316 survey results obtained (response rate, 15%), 225 (71%) were included in the study, with a mean age (SD) of 32.54 (4.91) years, and 124 (55.1%) were women. According to IPAQ-SF, 27.6% of cabin crew were found to be inactive, 54.7% minimally active and 17.7% very active. According to FSS, pathological fatigue was found in 43.6%. The FSS score of the inactive group was higher than the others (Kruskal Wallis, p < 0.001). As the number of people living in the same house or flight time in the last 1 month increase, the fear of COVID-19 also increases (Spearman, p = 0.01 r = 0.171, and p = 0.049 r = 0.131). In addition, there was direct correlation between fear of COVID-19 and fatigue and sleep problems (Spearman, p = 0.001 r = 0.218, and p < 0.001 r = 0.26, respectively).
Conclusion
This study shows that fatigue and sleep problems increase as the fear of COVID-19 increases in cabin crew during the early pandemic period. Consequently, precautions and further studies are needed, as fatigue and sleep disorders may primarily be related to the anxiety, fear and uncertainty surrounding the COVID-19 pandemic.
Keywords: COVID-19, Coronavirus, Aviation, Safety, Cabin crew, Flight, Aerospace medicine
1. Introduction
SARS-CoV-2, which emerged in Wuhan, China in December 2019, spread worldwide and eventually evolved into the COVID-19 pandemic which has been shown to have the potential to create serious fear in the society [[1], [2], [3]]. While mild and moderate level of fear can prevent the spread of the virus by increasing adherence to precautions and supportive protection from the disease, an excessive level of fear reduces the person's quality of life and reduces work performance [2].
The cabin crew members represent certified individuals assigned by the airline company to carry out duties related to flight and passenger safety during flights [[4], [5], [6]]. Sleep disturbance, depression and fatigue are frequently noted in cabin crew. Likewise, diseases that can lead to chronic fatigue, such as cardiovascular disease and cancer, are disproportionately diagnosed despite having lower body mass index [7,8]. An outbreak that may cause anxiety and fear and render cabin crew more susceptible to fatigue can lead to disruption of certain tasks, as well as to reduced adherence to safety-related protocols. During pandemic period, various new tasks such as adherence to new hygiene protocols, control of passengers using face masks, and identification, isolation and notification of symptomatic passengers or other flight attendants were added to cabin crew duties, and potentially negatively affected their working conditions.
Therefore, studying how to COVID-19 pandemic affected cabin crew may be important for questions of flight safety [9]. Specifically, we aimed to evaluate of fatigue and sleep problems associated with fear of COVID-19 during early pandemic period in cabin crew.
2. Material and methods
This is a survey based cross-sectional study. The study population consisted of cabin crewmembers on flight duty. Crewmembers who were interested to participate in this study could fill out the survey online. This study was performed by following the tenets of the Declaration of Helsinki, and institutional review board approval was obtained from the local ethics committee (B.30.2.ODM.0.20.08/54).
2.1. Study population and design
Inclusion criteria of the study were, actively working as a cabin crewmember on flight duty, and having answered all questions in the questionnaire. Survey responses were excluded if respondents were retired, or provided abnormal or inconsistent responses on the questionnaire. Duplicate survey entries were also removed from analysis. The European Union Aviation Safety Agency (EASA) had created an information bulletin about COVID-19 for flight crews, and aviation institutions had shared it with all their employees on flight duty [10]. Consequently, all active cabin crewmembers were using mandatory face masks during this pandemic period in cabin.
2.2. Questionnaire with scales
A questionnaire consisting of 45 questions created by our department of aerospace medicine was applied via Google Forms. The survey included questions about socio-demographic characteristics, flight times, flight types and COVID test history, as well as four internationally valid scales. All survey questions and scales are shown in Appendix 1. An online questionnaire was sent to 2092 cabin crew in February–April 2021 via TASSA, Cabin Crew Member's Association.
2.3. International physical activity questionnaire - short form (IPAQ-SF)
The IPAQ-SF was developed by the International Physical Activity Measurements Group to assess the physical activity and inactivity status of people aged 15–65 years [11]. The short form, as we used, consists of a total of 7 questions, questioning the amount of activity in the last 7 days. In the questions, the number of days of walking, moderate physical activity, and vigorous physical activity for 1 week, how many minutes a day is done on average, and how many hours are spent sitting on average per day are questioned. Calculations are made over MET (Metabolic Equivalent of Task), that is, the amount of energy consumed per unit time. In data analysis, MET-min/week score is calculated, and classification is made in this way. There are 3 physical activity levels in the classification. These were labeled as inactive/low, minimally active/moderate, and very active/high (Supplemantary).
2.4. Fatigue severity scale (FSS)
The FSS is a scale designed to calculate how tired a person has felt in the last 7 days, including the current day [12]. There are nine questions to express experienced fatigue. There are 7 options (1–7 pt) in each question and a value between 7 and 63 is obtained by adding the points marked by the person. The result of the scale is obtained by dividing the total value by 9. According to this result, values higher than 4 are considered pathological fatigue.
2.5. Jenkins sleep scale (JSS)
The Jenkins sleep scale was developed to assess sleep problems and was first applied to air traffic controllers and people recovering from cardiac surgery [13]. The test consists of 4 questions and each question has 6 options (0–5 pt). If the average score of the test is 4 pt or above, it is understood that there are about 15 nights or more with sleep problems in a month. The higher the score, the greater the sleep disturbance.
2.6. Fear of COVID-19 scale (FCV-19S)
The FCV-19S was designed to measure the fear of COVID-19 during the pandemic period [14]. The test consists of 7 questions with 5 options (1–5 pt) in each. The total result ranges from 7 to 35. The higher the result from the scale, the greater the fear of COVID-19 is considered.
2.7. Statistical analysis
Statistical analysis was performed using SPSS software, version 22.0 (IBM SPSS, Chicago, IL, USA). Descriptive statistical methods (mean, standard deviation) were used in the evaluation of the data. The categorical variables were analyzed using the chi-square test. Quantitative parameters were analyzed for distribution by the Shapiro-Wilk test for normality analysis. Due to the detected non-parametric distribution, the Mann-Whitney U test was used in the comparison of the two groups, while the Kruskal Wallis test was used for more than two groups. Post-hoc analysis was performed for pairwise group comparison of the parameters with significant results using the Kruskal Wallis test, and adjusted p values were indicated. Spearman test was used for correlation analysis. The main objective of the statistical analysis was to determine the relationship between fear of COVID-19 score and other parameters, especially fatigue and sleep disorder scores. The secondary objective is to determine the relationship between scales and questions about the pandemic changes (especially the 13th-16th). The evaluations were made at the 95% confidence interval, and the p-values of less than 0.05 were considered a statistically significant difference.
3. Results
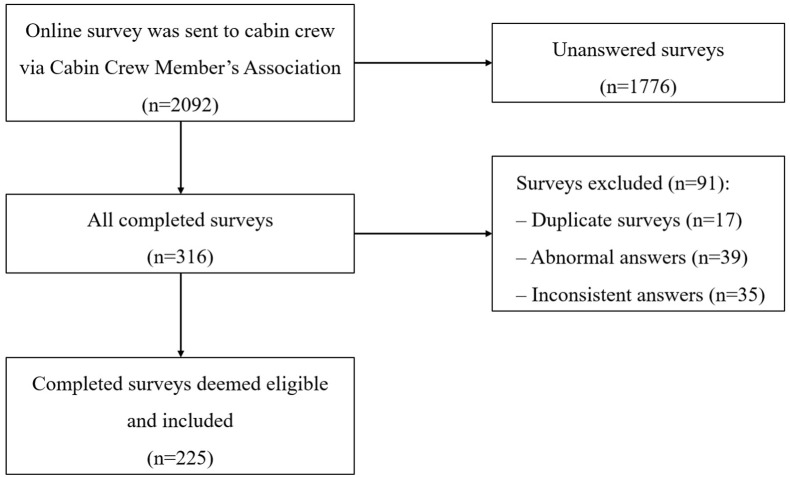
Respondents filled the surveys between 02.2021 and 04.2021. Out of 2092 invitations to participate, a total of 316 questionnaires were obtained (15% response rate). After excluding 91 responses from the study because of exclusion criteria, 225 questionnaires were included in this study (Fig. 1 ). The mean age (SD) was 32.54 (4.91) years, and 124 (55.1%) were female and 101 (44.9%) were male.
Fig. 1.
Collection of appropriate survey responses for the study.
The average total flight time (SD) was 5657.87 (5189.76) hours. The average flight times (SD) were 296.38 (192.33) hours, 39.75 (15.48) hours, and 13.6 (10.71) hours in the last year, month, and week, respectively. In the last 1 month, the most frequent flight types were 31.1% medium-haul (3–6 h), 28.9% short-haul (less than 3 h), 23.1% long-haul (6–12 h) and 16.9% ultra-long-haul (more than 12 h).
The average number of people (SD) sharing the household with the respondent were 1.48 (1.14). Presence of a chronic disease were reported 5 (2.22%), and 45 (20%) had a history of SARS-CoV-2 test positivity. Distribution of the various answers to questions 13–17 is shown in Table 1 .
Table 1.
Distribution of the various answers to question 13–17.
| Question No. | Content | Answers distribution | |||
|---|---|---|---|---|---|
| 13 | The state of fatigue compared to the pre-pandemic period | Yes, currently feeling more tired n = 95 (42.2%) |
No n = 88 (39.1%) |
Undecided n = 42 (18.7%) | |
| 14 | Future anxiety about health during the pandemic period | Yes n = 117 (78.7%) |
No n = 48 (21.3%) |
||
| 15 | Comparing the workload in the pandemic period with the previous | Increased n = 54 (24%) |
Not changed n = 58 (25.8%) | Decreased n = 113 (50.2%) | |
| 16 | The state of feeling helpless due to her/his profession | Yes n = 161 (71.6%) |
No n = 64 (28.4%) |
||
| 17 | The state of thinking that there is a high risk of contracting COVID-19 due to his/her profession | Yes n = 216 (96%) |
No n = 9 (4%) |
||
3.1. IPAQ-SF results
According to the results of IPAQ-SF, 62 (27.6%) respondents were found to be inactive, 123 (54.7%) were found to be minimally active, and 40 (17.7%) were found to be very active.
3.2. FSS results
Pathological fatigue (according to scale, more than 4 points was defined as pathological fatigue) was found in 98 (43.6%). The average FSS score (SD) in females was statistically significantly higher than male cabin crewmembers (4.48 [1.23] vs 3.97 [1.23], p = 0.004). The relationship between fatigue severity scores and answers to questions 13–16 is shown in Table 2 . A statistically significant difference was found between physical activity classes in terms of FSS score (Kruskal Wallis, p = 0.001) (Table 3 ). The FSS score of the inactive cabin crewmembers was statistically significantly higher than very active and minimally active members (post-hoc, adjusted p = 0.001 and p = 0.026, respectively). Also, a weak positive correlation was found between the FSS score and the daily sitting time (Spearman, p = 0.005, r = 0.188).
Table 2.
The relationship between scale scores and answers to questions 13–16.
| Question No. | Content | Answer | FSS (pts) | JSS (pts) | FCV-19S (pts) |
|---|---|---|---|---|---|
| 13 | The state of fatigue compared to the pre-pandemic period | Yes, currently feeling more tired | 4.45 ± 1.13++ | 8.53 ± 6.09++ | 18.29 ± 6.26 |
| No | 3.49 ± 1.41 | 4.16 ± 3.98 | 16.41 ± 5.74 | ||
| Undecided | 4.18 ± 1.07 | 6.83 ± 4.42+ | 20.10 ± 6.43+ | ||
| 14 | Future anxiety about health during the pandemic period | Yes | 4.45 ± 1.13** | 6.87 ± 5.41* | 19.40 ± 5.59** |
| No | 3.50 ± 1.41 | 5.17 ± 5.25 | 12.33 ± 5.19 | ||
| 15 | Comparing the workload in the pandemic period with the previous | Increased | 4.27 ± 1.42 | 7.89 ± 5.59+ | 18.91 ± 6.85 |
| Not changed | 4.19 ± 1.19 | 6.71 ± 5.52 | 19.66 ± 6.31+ | ||
| Decreased | 4.35 ± 1.24 | 5.74 ± 5.16 | 16.50 ± 5.54 | ||
| 16 | The state of feeling helpless due to her/his profession | Yes | 4.54 ± 1.14** | 7.16 ± 5.60* | 19.44 ± 5.97** |
| No | 3.52 ± 1.24 | 4.86 ± 4.51 | 14.00 ± 5.05 |
FSS: Fatigue severity scale, JSS: Jerkins sleep scale, FCV-19S: Fear of COVID-19 scale, pts: points.
*: p < 0.05 and **: p < 0.001, Mann-Whitney U test, compared with other option.
+: p < 0.05 and ++: p < 0.001, Kruskal Wallis test post-hoc analysis, compared with the lowest option.
Table 3.
Comparison of physical activity classes in terms of fatigue scores.
| Inactive (n = 62) | Minimally active (n = 123) | Very active (n = 40) | p-value | ||
|---|---|---|---|---|---|
| FSS score | 4,66 ± 1,35 (4.94, 1.56–7) |
4,18 ± 1,24 (4.22, 1–7) |
3,79 ± 0,94 (3.89, 1.22–5.89) |
0.001* | |
| Inactive – very active | 0.001+ | ||||
| Inactive – minimally active | 0.026+ | ||||
| Very active – minimally active | 0.201+ | ||||
Mean ± standard deviation, additionally median, minimum and maximum values were given in parenthesis. p < 0.05 was considered statistically different.*Kruskal Wallis test. +Adjusted p values obtained by post-hoc analysis.
FSS: Fatigue severity scale.
3.3. JSS results
According to the JSS, the average sleep disorder score (SD) in respondents was calculated as 6.51 (5.41) points. While sleep disorder score was above 4 in 98 (44%) of the participants, it was 4 or below in 127 (56%). A statistically significant moderate positive correlation was found between sleep disorder and fatigue scores (Spearman, p < 0.001, r = 0.338). The relationship between sleep disorder scores and answers to questions 13–16 is shown in Table 2.
3.4. FCV-19S results
According to the FCV-19S, females had a higher score (SD) than males (18.92 [6.3] vs 16.63 [5.9], p = 0.01). A statistically significant positive correlation was found between FCV-19S score and JSS score, FSS score, number of people living together in the same house, and flight time in the last 1 month (Spearman, p < 0.001 r = 0.26; p = 0.001 r = 0.218; p = 0.01 r = 0.171; and p = 0.049 r = 0.131, respectively). The relationship between fear of COVID-19 scores and answers to questions 13–16 is shown in Table 2. Respondents who thought that they are at higher risk of contracting COVID-19 had a higher FCV-19S score (SD) compared to those who did not think so (18.16 [6.12] vs 11.44 [5.32], p = 0.002).
4. Discussion
In this study, fatigue and sleep problems associated with fear of COVID-19 were observed in cabin crew during the early pandemic period. Also, it was observed that the number of people living together in the same house and the flight time in the last month increased this fear proportionally. Although the physical activity levels determined do not have a direct effect on this fear, it was found to affect fatigue.
Events that threaten human health around the world, such as epidemics, affect social life, cause fear of death, create hopelessness and create economic uncertainty, causing not only physical but also mental health problems [15,16]. In the study conducted by El-Zoghby et al. during the pandemic period, 53.9% of people stated that they felt terrified and helpless, while Zhang et al. reported that this ratio is 46.7% [17,18]. In a study by Gill et al. in oncologists, 52% of the respondents stated that they felt anxiety or hopelessness [19]. However, this current study showed that 71.6% felt helpless during the pandemic period due to their profession and 78.7% were concerned about their health during the pandemic period. The reason why it is higher than other studies may be due to the cabin crew profession, the high contact with people, and the time spent in the aircraft cabin, a real indoor environment, with many people. Also, Wenn et al. stated that 59.5% of individuals in cabin crew reported abnormal levels of anxiety [20]. In the study of Wenn et al. they included 45 currently flying, 35 are grounded but doing alternate work, and 329 not working cabin crew. However, in this current study, the fact that only the cabin crew currently working on flight duty was included may explain this difference.
The pathophysiology of fatigue is not well understood. However, fear and anxiety cause an increase in stress in the body. As a result, inflammatory response in anxiety and fear-related fatigue was consistently found to affect anxiety-related brain regions [21]. In the study conducted by Van Den Berg et al. on cabin crew, although sleep loss and circadian disruption were the main causes of fatigue, participants also blamed other key factors such as insufficient rest, high workload, work environment, and lack of company support and inadequate fatigue management training [6]. It has been emphasized that adequate rest is important not only for obtaining adequate sleep, but also for maintaining a work-life balance. Unlike before the pandemic, new in-cabin tasks such as personal protective equipment (PPE) usage control of “passengers” throughout the travel and warning of those who do not use it properly, distribution of PPE and hand disinfectant equipment to passengers at the entrance to the cabin have emerged. Also, COVID-19 documents needed to be filled before and after each trip [13]. In the study of Wen et al. on cabin crew during the COVID-19 period, the Flinders fatigue scale was applied and 63.5% fatigue was detected [4]. In this study conducted with FSS scores, fatigue was found to be 43.6% in the cabin crew. Furthermore, in the study of Castro et al. on cabin crew, it was reported that women were more affected by fatigue [22]. Similarly, in this study, the fatigue score of female cabin crewmembers was found to be statistically significantly higher than males. One possible explanation for this gender difference could be given by the more restful sleep of men [23]. In addition, gender inequalities regarding household responsibilities and child raising may be responsible for this difference in fatigue reported [23].
In the study of Castro et al. more fatigue was detected in medium and long-haul flights [22]. In the study of Aljurf et al. on pilots, no statistically significant results were found between the FSS score and total flight experience, long, medium, and short-haul flight rates in the last 12 months, and total flight hours in the last 1 week [24]. In this current study, no correlation was found between the most frequent flight type in the last month, total flight times in the last 1 year, 1 month, 1 week, and the FSS score.
When examining the relationship between fatigue and physical activity, many studies, meta-analyses, and systemic reviews concluded that physical activity reduces fatigue [[25], [26], [27]]. In this study, the FSS score of inactive people was found to be statistically significantly higher than very active and minimally active. A positive correlation was found between the fatigue score and the time spent sitting daily. Therefore, the inactive category within physical activity classes is more prone to fatigue. Even a minimally active level of exercise can protect against fatigue.
Poor sleep quality, sleep disturbances, and sleep deprivation are generally associated with fatigue [28]. In the study conducted by Reis et al. on pilots, 65.1% of the participants scored 4 and above on the JSS [29]. In our study, this rate was found to be 44% in cabin crew. In the same study conducted by Reis et al. on pilots, individuals were evaluated with JSS, and it was observed that fatigue increased if sleep disturbance increased [29]. In our study, a statistically significant positive correlation was found between fatigue scores and sleep disorder scores in cabin crew. In the review of Iwu et al. on prolonged COVID, it was reported that sleep disorders are among the complaints related to this period [30]. In the study of Huang et al., sleep-related problems were found in 26% of 1655 patients followed up after COVID-19 [31]. In this study, however, no statistically significant difference was found between the COVID-19 test history status information in terms of JSS score. Apart from these, cabin crew who answered like more tired and “undecided” about feeling more tired now, it is also a favorable finding that the sleep disorder score is higher than those who do not feel tired. Providing a briefing and relief related to COVID-19 that will contribute positively to the cabin crew, may eliminate this.
In the study of Lu et al. on healthcare workers, it was found that personnel who had close contact with COVID-19 infected patients felt 1.4 times more fearful than other personnel participating in the study, but also experienced 2 times more anxiety and depression [32]. In this study, 96% of cabin crew thought that the risk of contracting COVID-19 was higher due to their profession. Nikopoulou et al. reported that using the FCV-19S and anxiety scales, fear and anxiety were correlated [33]. Apart from these, several studies have reported a higher fear of COVID-19 in women [34,35]. In this study, the FCV-19S score of female cabin crewmembers is statistically significantly higher than males. Also, using the FCV-19S, a statistically significant positive correlation was found between the COVID-19 fear score and the number of people living together in the same house and the flight time in the last 1 month. The increase in the number of people living together in the same house increases the COVID-19 fear score because of the anxiety of causing transmission of disease to a relative person within the home or vice versa. In a study conducted by Yang et al. on employees returning to work during the pandemic period, poor sleep quality was found to be associated with anxiety and depression [36]. Similarly, in this study, there was a statistically significant positive correlation between FCV-19S, JSS, and FSS scores. Apart from these, cabin crew who answered like “undecided” about feeling more tired now, it is also an interesting finding that the COVID-19 fear level is higher than those who do not feel tired. Providing a briefing or activities related to COVID-19 that will contribute positively to the cabin crew, who do not comment on their fatigue, may eliminate this undecided situation. In this study, there was no statistically significant difference between COVID-19 test status information and physical activity classes in terms of COVID-19 fear score.
4.1. Strengths and limitations
The main strength of this study is a blinded survey study conducted on cabin crew due to researchers have no name or commercial airline type information about any cabin crew. Also, another important strength is the use of internationally valid scales such as IPAQ-SF, JSS, FSS, and FCV-19S. To the best of our knowledge, this is the first study in which these scales were used in cabin crew during the early COVID-19 pandemic period.
The limitations of this study are that the study is cross-sectional online survey research and conducted between 02.2021 and 04.2021. Results may vary in face-to-face survey collaboration or at different times during the pandemic period. Also, this study was performed only on the cabin crew working in Turkish commercial airlines, therefore it may vary for different companies and pilots. Another important limitation to discuss is a likely selection bias. The response rate was low (15%) and a third of responses (29%) were removed. So, found proportion may be smaller than described in this standing. In addition, at the time of this survey, cabin crew had not yet been vaccinated in Turkey. In addition, during the early COVID-19 pandemic, all transmission routes and treatment options for COVID were not also fully revealed except vaccination. The fear of COVID-19, fatigue and sleep problems that we have detected may change after the vaccination is entirely completed. Apart from these, comparing these findings of physical activity, fatigue, and sleep with the non-pandemic period may be useful for further research. Thus, appropriate further studies are needed.
5. Conclusions
In summary, the COVID-19 pandemic has affected the aviation sector and also affected cabin crewmembers, one of the major elements of this sector. This study showed that fatigue and sleep problems associated with fear of COVID-19 were detected in the cabin crew who had a high risk of close contact with people even during the pandemic period. Furthermore, this study suggests fatigue and sleep disturbances are primarily related to the anxiety, fear and uncertainty surrounding COVID-19 pandemic. Additionally, this study shows that physical activity and exercise may contribute to the reduction of fatigue. Providing more info and psychosocial support to cabin crewmembers about COVID-19 and benefits of exercise may be beneficial for aviation safety and public health. Also, taking precautions and being prepared for possible future pandemic-like conditions can be effective by reducing the associated fear and anxiety. The aviation world was not fully prepared for this pandemic, but it should be prepared for the next. Further studies are needed.
Declarations
Institutional review board approval was obtained from the local ethics committee (B.30.2.ODM.0.20.08/54, Approval date: 29.01.2021). This study was accepted as Eda Sabaner's thesis for specialization in aerospace medicine, in the Department of Aerospace Medicine, Faculty of Medicine, Ondokuz Mayis University, Turkey. There is no relationship between authors and TASSA. TASSA provided free support to this study for contributing to science.
Declaration of interest
The authors report no conflict of interest for this research. The authors alone are responsible for the content and writing of this article.
Funding or financial support
No financial or funding support was received for this research.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Authors’ contributions
ES: Conceptualization, Methodology, Software, Formal analysis, Writing - Original Draft, Visualization; FK: Conceptualization, Methodology, Writing - Review & Editing, Supervision; EE: Conceptualization, Methodology, Writing - Review & Editing, Supervision.
Declaration of competing interest
All authors certify that they have no affiliations with or involvement in any organization with any financial interest or non-financial interest in the subject matter or materials discussed in this article. All authors approved of the final manuscript.
Acknowledgments
Special thanks to” TASSA, Cabin Crew Member's Association” for helping in the survey section, and to “Mehmet Cem Sabaner” for kindly helping with statistical analysis.
Footnotes
This study was conducted at the Department of Aerospace Medicine, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey with the online survey participation of TASSA, Turkey Cabin Crew Association.
This study was accepted as Eda Sabaner's thesis for specialization in Aerospace Medicine, in the Department of Aerospace Medicine, Faculty of Medicine, Ondokuz Mayis University, Turkey.
This research and paper not presented anywhere.
The authors report no conflict of interest for this research.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.tmaid.2022.102430.
Abbreviations
- PPE
Personal protective equipment
- IPAQ-SF
International physical activity questionnaire-short form
- FSS
Fatigue severity scale
- JSS
Jenkins sleep scale
- FCV-19S
Fear of COVID-19 scale
- TASSA
Cabin Crew Member's Association
- EASA
European Union Aviation Safety Agency
- MET
Metabolic Equivalent of Task
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Jee Y. WHO international health regulations emergency committee for the COVID-19 outbreak. Epidemiol Health. 2020;42 doi: 10.4178/epih.e2020013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajabimajd N., Alimoradi Z., Griffiths M.D. Impact of COVID-19 related fear and anxiety on job attributes: a systematic review. Asian J. Soc. Health. Behav. 2021;4(2):51–55. doi: 10.4103/shb.shb_24_21. [DOI] [Google Scholar]
- 3.Bielecki M., Patel D., Hinkelbein J., Komorowski M., Kester J., Ebrahim S., et al. Air travel and COVID-19 prevention in the pandemic and peri-pandemic period: a narrative review. Trav Med Infect Dis. 2021;39 doi: 10.1016/j.tmaid.2020.101915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wen C.C.Y., Nicholas C.L., Clarke-Errey S., Howard M.E., Trinder J., Jordan A.S. Health risks and potential predictors of fatigue and sleepiness in airline cabin crew. Int J Environ Res Publ Health. 2021;18:1–15. doi: 10.3390/ijerph18010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baruah R., Jayasankara Reddy K. Implication of emotional labor, cognitive flexibility, and relational energy among cabin crew: a review. Indian J Occup Environ Med. 2018;22:2–4. doi: 10.4103/ijoem.IJOEM_21_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van den Berg M.J., Signal T.L., Gander P.H. Fatigue risk management for cabin crew: the importance of company support and sufficien rest for work-life balance—a qualitative study. Ind Health. 2020;58:2–14. doi: 10.2486/indhealth.2018-0233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McNeely E., Gale S., Tager I., et al. The self-reported health of U.S. flight attendants compared to the general population. Environ Health. 2014;13(1):13. doi: 10.1186/1476-069X-13-13. https://doi:10.1186/1476-069X-13-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McNeely E., Mordukhovich I., Tideman S., Gale S., Coull B. Estimating the health consequences of flight attendant work: comparing flight attendant health to the general population in a cross-sectional study. BMC Publ Health. 2018;18(1):346. doi: 10.1186/s12889-018-5221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grout A., Leggat P.A. Cabin crew health and fitness-to-fly: opportunities for re-evaluation amid COVID-19. Trav Med Infect Dis. 2021;40 doi: 10.1016/j.tmaid.2021.101973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.European Aviation Safety Agency (EASA) 2020. pp. 1–13.https://www.easa.europa.eu/downloads/111913/en (Guidance on the management of crew members in relation to the COVID-19 pandemic). [Google Scholar]
- 11.Craig C.L., Marshall A.L., Sjöström M., Bauman A.E., Booth M.L., Ainsworth B.E., et al. International physical activity questionnaire: 12-Country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 12.Armutlu K., Cetisli Korkmaz N., Keser I., Sumbuloglu V., Irem Akbiyik D., Guney Z., et al. The validity and reliability of the Fatigue Severity Scale in Turkish multiple sclerosis patients. Int J Rehabil Res. 2007;30:81–85. doi: 10.1097/MRR.0b013e3280146ec4. [DOI] [PubMed] [Google Scholar]
- 13.Jenkins C.D., Stanton B.A., Niemcryk S.J., Rose R.M. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41:313–321. doi: 10.1016/0895-4356(88)90138-2. [DOI] [PubMed] [Google Scholar]
- 14.Ahorsu D.K., Lin C.Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addiction. 2020;1–9 doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) J Trauma Stress. 2005;18:39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Zoghby S.M., Soltan E.M., Salama H.M. Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. J Community Health. 2020;45:689–695. doi: 10.1007/s10900-020-00853-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in liaoning province, China: a cross-sectional study. Int J Environ Res Publ Health. 2020;17:2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gill S., Hao D., Hirte H., Campbell A., Colwell B. Impact of COVID-19 on canadian medical oncologists and cancer care: Canadian association of medical oncologists survey report. Curr Oncol. 2020;27:71–74. doi: 10.3747/co.27.6643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wen C.C.-Y., Nicholas C.L., Howard M.E., Trinder J., Jordan A.S. Understanding sleepiness and fatigue in cabin crew using COVID-19 to dissociate causative factors. Aerosp Med Hum Perform. 2022;93:50–53. doi: 10.3357/AMHP.5925.2022. [DOI] [PubMed] [Google Scholar]
- 21.Felger J.C. Imaging the role of inflammation in mood and anxiety-related disorders. Curr Neuropharmacol. 2018;16(5):533–558. doi: 10.2174/1570159X15666171123201142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Castro M., Carvalhais J., Teles J. Irregular working hours and fatigue of cabin crew. Work. 2015;51:505–511. doi: 10.3233/WOR-141877. [DOI] [PubMed] [Google Scholar]
- 23.Engberg I., Segerstedt J., Waller G., Wennberg P., Eliasson M. Fatigue in the general population- associations to age, sex, socioeconomic status, physical activity, sitting time and self-rated health: the northern Sweden MONICA study 2014. BMC Publ Health. 2017;17(1):654. doi: 10.1186/s12889-017-4623-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aljurf T.M., Olaish A.H., BaHammam A.S. Assessment of sleepiness, fatigue, and depression among Gulf Cooperation Council commercial airline pilots. Sleep Breath. 2018;22:411–419. doi: 10.1007/s11325-017-1565-7. [DOI] [PubMed] [Google Scholar]
- 25.Naczenski L.M., de Vries J.D., van Hooff M.L.M., Kompier M.A.J. Systematic review of the association between physical activity and burnout. J Occup Health. 2017;59:477–494. doi: 10.1539/joh.17-0050-RA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oberoi S., Robinson P.D., Cataudella D., Culos-Reed S.N., Davis H., Duong N., et al. Physical activity reduces fatigue in patients with cancer and hematopoietic stem cell transplant recipients: a systematic review and meta-analysis of randomized trials. Crit Rev Oncol Hematol. 2018;122:52–59. doi: 10.1016/j.critrevonc.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 27.Dreher M., Döβereck N., Lachtermann E. Physical activity and its effects on burnout syndrome: a systematic review. Laryngo-Rhino-Otol. 2020;99:121–131. doi: 10.1055/a-1071-1905. [DOI] [PubMed] [Google Scholar]
- 28.Caldwell J.A. Fatigue in aviation. Trav Med Infect Dis. 2005;3:85–96. doi: 10.1016/j.tmaid.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 29.Reis C., Mestre C., Canhão H., Gradwell D., Paiva T. Sleep complaints and fatigue of airline pilots. Sleep Sci. 2016;9:73–77. doi: 10.1016/j.slsci.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Iwu C.J., Iwu C.D., Wiysonge C.S. The occurrence of long COVID: a rapid review. Pan Afr Med J. 2021;38:1–12. doi: 10.11604/pamj.2021.38.65.27366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang C., Huang L., Wang Y., Li X., Ren L., Gu X., et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatr Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nikopoulou V.A., Holeva V., Parlapani E., Karamouzi P., Voitsidis P., Porfyri G.N., et al. Mental health screening for COVID-19: a proposed cutoff score for the Greek version of the fear of COVID-19 scale (FCV-19S) Int J Ment Health Addiction. 2022;20:907–920. doi: 10.1007/s11469-020-00414-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fitzpatrick K.M., Harris C., Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychol Trauma Theor, Res Pract Pol. 2020;12:S17–S21. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- 35.Broche-Pérez Y., Fernández-Fleites Z., Jiménez-Puig E., Fernández-Castillo E., Rodríguez-Martin B.C. Gender and fear of COVID-19 in a Cuban population sample. Int J Ment Health Addiction. 2022;20:83–91. doi: 10.1007/s11469-020-00343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang Y., Zhu J fu, Yang S yue, Lin H jiang, Chen Y., Zhao Q., et al. Prevalence and associated factors of poor sleep quality among Chinese returning workers during the COVID-19 pandemic. Sleep Med. 2020;73:47–52. doi: 10.1016/j.sleep.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.