Abstract
Background:
To explore potential causes leading to the failure of the surgical reconstruction of sigmoid sinus wall in patients with pulsatile tinnitus.
Methods:
This study retrospectively analyzed pulsatile tinnitus patients with sigmoid sinus wall dehiscence and/or sigmoid sinus diverticulum, who underwent revision surgeries following the surgical reconstruction of the sigmoid sinus wall.
Results:
A total of 7 pulsatile tinnitus patients were included. After the first surgery, 5 of 7 patients showed varying degrees of remission in pulsatile tinnitus, but pulsatile tinnitus gradually recurred. The other 2 patients experienced no change in pulsatile tinnitus. Images after the first surgeries revealed that the surgical failure of Patients 1-5 was caused by incompleted elimination of sigmoid sinus wall dehiscence and sigmoid sinus diverticulum. Following revision surgeries, they all acquired great or complete resolution of pulsatile tinnitus. In Patient 6, an abnormal diploic vein entering the sigmoid sinus was overlooked during the first surgery for repairing sigmoid sinus wall dehiscence. As soon as the diploic vein was blocked during the revision surgery, the patient’s pulsatile tinnitus was alleviated significantly. Patient 7 had a recurrence of pulsatile tinnitus after transient improvement following the first surgery, and still experienced no change in pulsatile tinnitus after the revision surgery. However, after venous sinus stenting in the stenosis of transverse-sigmoid sinus junction, she got complete resolution of pulsatile tinnitus. It suggested that the unresolved stenosis of the venous sinus was the cause of the surgical failure.
Conclusions:
Both sigmoid sinus diverticulum and sigmoid sinus wall dehiscence are recommended to be resolved during surgery. Abnormal diploic veins and venous sinus stenosis are potential causes of pulsatile tinnitus.
Keywords: Pulsatile tinnitus, sigmoid sinus diverticulum, sigmoid sinus wall dehiscence, reconstruction, revision
Introduction
Tinnitus refers to the sensation of intra-aural or intracranial sound in the absence of an external sound source stimulation. According to its characteristics, tinnitus can be either pulsatile or non-pulsatile. Pulsatile tinnitus (PT) is present in approximately 4% of tinnitus patients,1 and the involved sound is generally produced by abnormal blood vessels in the head and neck. The rhythm of vascular PT is consistent with the patient’s heartbeat. According to the different types of blood vessels, vascular PT is either arterial or (more commonly) venous.
Studies have found that approximately 20% of patients with PT have related sigmoid sinus anomalies,2-4 which include sigmoid sinus wall dehiscence (SSWD) and sigmoid sinus diverticulum (SSD). In 2007, Otto et al5 surgically reconstructed the lateral wall of the sigmoid sinus to treat patients with SSD. We modified this method.6,7 The treatment results showed that for patients who had SSD and for patients with SSWD, treatment effectiveness rates were 80% and 70.4%, respectively.6,7 However, some patients who had transient improvement of their tinnitus and subsequent postoperative recurrence requested additional surgery. Thus far, there has been no relevant report.
In this study, we retrospectively analyzed a group of 7 PT patients with sigmoid sinus anomalies who had undergone revision surgeries. We explored the possible etiology of PT and aimed to improve the effectiveness of surgery.
Materials and Methods
Subjects
The study was approved by the Beijing Friendship Hospital, Capital Medical University of China (Approval no: 2018-P2-140-02) and carried out following the CARE guidelines. All participants signed an ethical committee–approved, informed consent form prior to the study. We retrospectively reviewed the records of PT patients who underwent 2 related surgeries for the reconstruction of the sigmoid sinus wall between December 2008 and October 2020. In total, 7 patients were included. We collected the following information about patients: sex, age of PT onset, side of PT, dominant sigmoid sinus (DSS), body mass index (BMI), pure tone audiometry (PTA), intracranial pressure, and imaging findings. Dominant sigmoid sinus was confirmed by computed tomography angiography (CTA) and digital subtraction angiography (DSA). The severity of tinnitus was assessed using the Tinnitus Handicap Inventory (THI) scale.
Surgical Procedure
We used a transmastoid approach to reconstruct the bone wall around the sigmoid sinus. The surgical methods have been described in detail previously.6,7 Briefly, a posterior auricular incision was made; a pedicled myoperiosteal flap was then created to expose the mastoid cortex. The bony shell surrounding SSD or SSWD was removed, and temporalis fascia was used to reconstruct the bone wall of the diverticulum or dehiscence according to the normal contour of the sigmoid sinus. Autologous bone powder was then used for lateral shaping, and the graft was fixed with a medical adhesive (FAL, Beijing Fuaile Co., Beijing, China). Finally, the mastoid process was covered with the pedicled myoperiosteal flap.
All patients were followed up regularly by telephone or via clinic visits. According to subjective descriptions of the patients, the effect of surgical treatment on PT was classified as complete resolution, partial resolution, or no change. The THI was used to assess each patient’s condition and postoperative changes during follow-up. Computed tomography angiography and PTA were performed only on patients who returned to the clinic.
Results
General Patient Information
The clinical characteristics of the patients are shown in Table 1. The mean age of the patients was 28.43 ± 5.83 years (range, 19-34 years). Ipsilateral distal transverse sinus stenosis in Patient 6 had a gradient of 10.9 cmH2O and a lumbar puncture was performed, with a cerebrospinal fluid pressure of 17.5 cmH2O. All 7 patients had normal otoscopic findings. Pure tone audiometry indicated that 2 patients had mild hearing loss at 250 and 500 Hz frequencies (Patients 2 and 5); the others had normal hearing.
Table 1.
Preoperative Patient Information
| Patient Number | Sex | Age of Onset (Year) | Side | DSS | BMI | THI | Imaging Findings |
| 1 | F | 31 | Right | Right | 25.59 | 58 | SSD + SSWD + high and dehiscent jugular bulb |
| 2 | F | 26 | Right | Right | 26.67 | 56 | SSD + SSWD |
| 3 | F | 23 | Left | Left | 22.46 | 38 | SSD + SSWD |
| 4 | F | 19 | Right | Right | 22.48 | 74 | SSD + SSWD + high and dehiscent jugular bulb |
| 5 | F | 33 | Right | Right | 25.16 | 60 | SSD + SSWD |
| 6 | F | 33 | Right | Right | 21.22 | 42 | SSWD + high jugular bulb + distal transverse sinus stenosis |
| 7 | F | 34 | Right | Right | 25.71 | 68 | SSD + SSWD + right internal carotid atherosclerosis + empty and expanded sella |
DSS, dominant sigmoid sinus in ipsilateral pulsatile tinnitus; BMI, body mass index; SSD, sigmoid sinus diverticulum; SSWD, sigmoid sinus wall dehiscence; THI, Tinnitus Handicap Inventory.
Surgical Outcomes
Relevant information about the operations is outlined in Table 2. Despite 2 operations, no major complications such as dizziness, headache, visual changes, or hearing loss were found. Common minor complications included persistent periauricular numbness, breakdown of the posterior auricular incision site, and ear fullness.
Table 2.
Surgical Outcomes in Patients with Pulsatile Tinnitus
| Patient Number | Date of First Surgery | First Surgical Outcome | Possible Reasons | Date of Second Surgery | Second Surgical Outcome | Loudness (%)# |
Follow-Up Duration After Second Surgery
(Month) |
|---|---|---|---|---|---|---|---|
| 1 | 2011/4 | No change | SSWD not resolved | 2012/12* | Partial resolution | 30 | 94 |
| 2 | 2011/8 | Slightly better, returned to baseline after 1 month | SSD partially eliminated, SSWD not resolved | 2013/10 | Partial resolution | 20 | 84 |
| 3 | 2011/9 | 50% better, returned to baseline after 3 weeks | SSD partially eliminated, SSWD not resolved | 2012/12* | Complete resolution | 0 | 94 |
| 4 | 2013/1* | Disappeared, returned to 90% after 1 day | SSD partially eliminated, SSWD not resolved | 2013/1* | Complete resolution | 0 | 93 |
| 5 | 2013/5* | 90% better, returned to baseline after 1 month | SSD partially eliminated, SSWD not resolved | 2014/7 | Complete resolution | 0 | 75 |
| 6 | 2017/1 | No change | Abnormal diploic vein | 2019/8 | Partial resolution | 20 | 14 |
| 7 | 2017/8 | Disappeared, returned to baseline after 3 months | SSWD and stenosis not resolved | 2018/1 | No change | 100 | 33 |
SSD, sigmoid sinus diverticulum; SSWD, sigmoid sinus wall dehiscence.
*Surgery was performed under local anesthesia. # Loudness level of second postoperative pulsatile tinnitus compared with that of preoperative pulsatile tinnitus (%).
Case Presentation
Patient 1
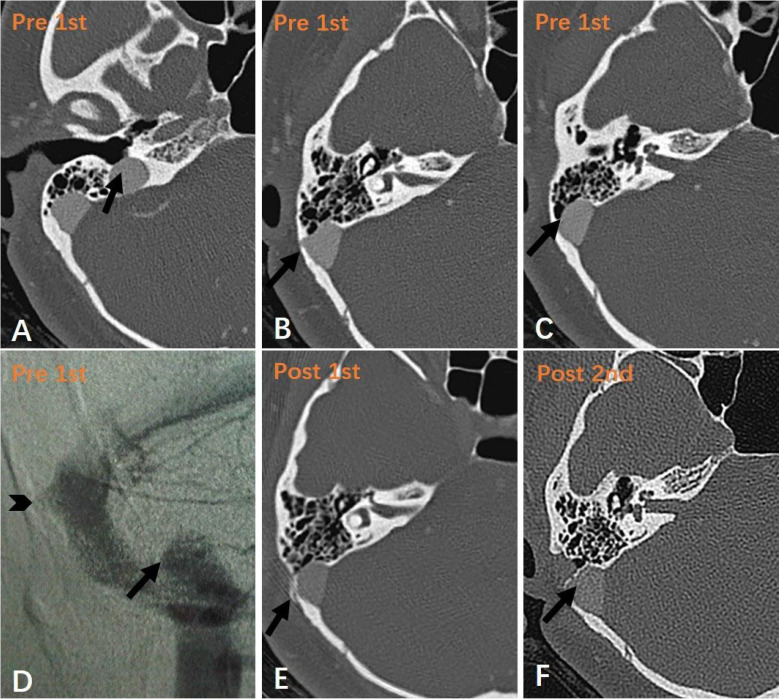
Patient 1 suffered from PT for 7 years. Computed tomography angiography and DSA showed SSD, SSWD, and a dehiscent jugular bulb on the right side of her sigmoid sinus (Figure 1A-D). The SSD was resolved completely during the first operation (Figure 1E), but she experienced no change in PT. During reconstruction of the SSWD in the second operation under local anesthesia (Figure 1F), the patient’s tinnitus resolved immediately. However, because she could not tolerate the continuation of the operation, the high and dehiscent jugular bulb was not resolved. Her symptoms improved markedly after the surgery; the loudness level was 30%, compared with that of the preoperative PT, and remained stable until the last followup.
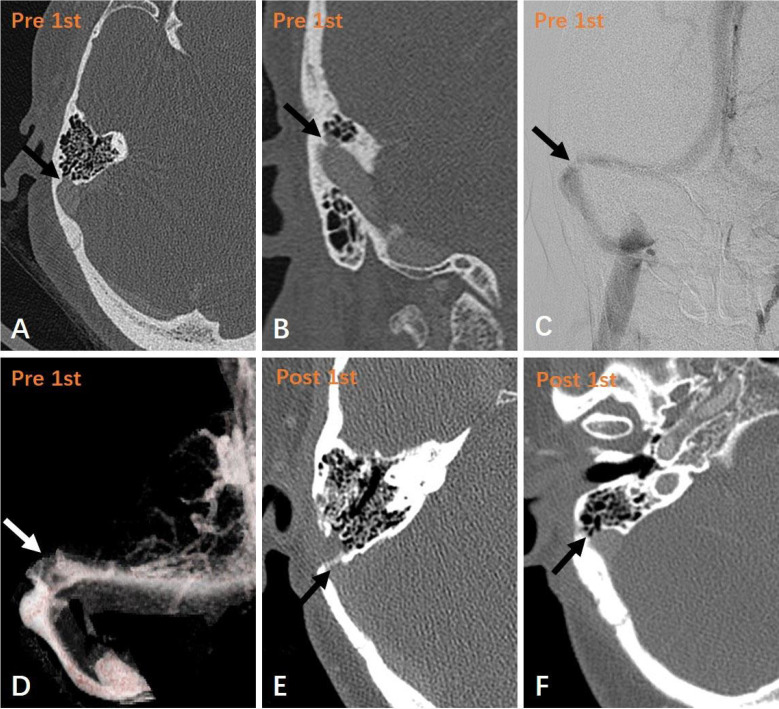
Figure 1. a-f.
(a-d), 1st preoperative; E, 1st postoperative; and F, 2nd postoperative images of Patient 1 who underwent two operations. (a), (b), and (c) show the high and dehiscent jugular bulb, SSD, and SSWD in axial CTA, respectively (arrows). (d) shows a DSA image of the right high jugular bulb (arrow) and SSD (arrowhead). The layer in (e) corresponds to that in B; the diverticulum is completely repaired (arrow). The layer in (f) corresponds to that in C; the dehiscence is completely repaired (arrow).
Patients 2-5
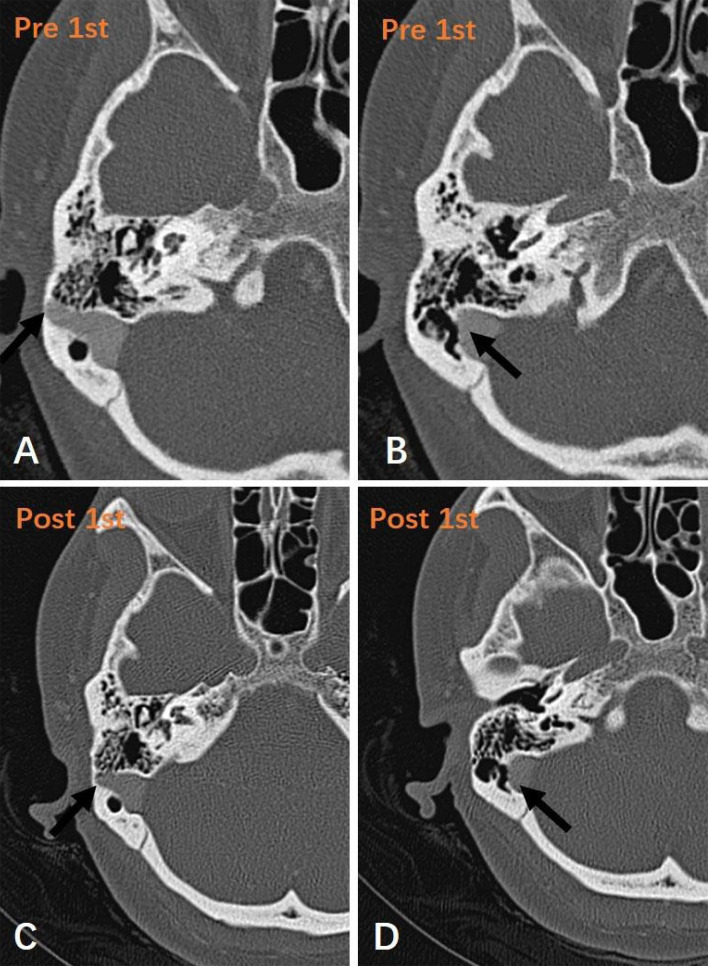
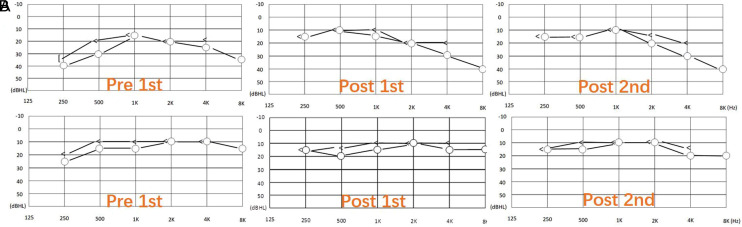
Patient 2 had a history of PT for almost 10 years, with progressive worsening. Preoperative CTA showed SSD and SSWD (Figure 2A, B). The first operation aimed to remove the diverticulum and reconstruct the sigmoid sinus wall. The patient reported a slight improvement in PT after the first operation, and her PT returned to preoperative baseline after 1 month. Postoperative CTA showed that the diverticulum had not been eliminated completely (Figure 2C) and the SSWD remained the same (Figure 2D). However, PTA showed improvement in ipsilateral low-frequency hearing loss (Figure 3A). During the second operation, after wide skeletonization and exposure of the diverticulum and SSWD, we removed the diverticulum and repaired the dehiscent sigmoid sinus wall. The patient experienced evident resolution of PT, which loudness level was 20% of preoperative PT. The treatment procedures in the other 3 patients (Patients 3, 4, and 5) were similar to those in Patient 2. The first operation partially removed SSD without repair of the SSWD. During the revision surgery, both SSD and SSWD were resolved, and all 3 patients achieved complete resolution of PT. Patient 5 also gained improvement in ipsilateral low-frequency hearing loss (250 Hz) (Figure 3B). The hearing remained normal after the second operation in these patients.
Figure 2. a-d.
(a), (b), 1st preoperative; and (c), (d), 1st postoperative images of Patient 2, who experienced slight resolution of PT after the first operation. (a) and (b) show the SSD and SSWD in axial CTA, respectively (arrows). (c) shows that the diverticulum is partially resolved in axial CTA (arrow). The layer in (d) corresponds to that in B; the SSWD remains the same (arrow).
Figure 3. a,b.
Pure tone audiograms show the pre- and postoperative hearing changes in PT after 2 surgeries. (a) represents Patient 2: before the first operation, air- and bone-conduction thresholds at 250 and 500 Hz were 40- and 35-dB, and 30- and 20-dB hearing level, respectively. After the first operation, air- and bone-conduction thresholds at 250 and 500 Hz were 15- and 15-dB, and 10- and 10-dB hearing level, respectively. After the second operation, low-frequency thresholds remained normal. (b) represents Patient 5: the first preoperative pure tone audiogram indicates that air- and bone-conduction thresholds at 250 and 500 Hz were 25- and 20-dB, and 15- and 10-dB hearing level, respectively. The first postoperative pure tone audiogram indicates that air- and bone-conduction thresholds at 250 Hz improved by 10 and 5 dB, respectively, but both decreased by 5 dB at 500 Hz. The second postoperative pure tone audiogram shows that the hearing threshold at 500 Hz recovered, and the other frequencies remained unchanged.
Patient 6
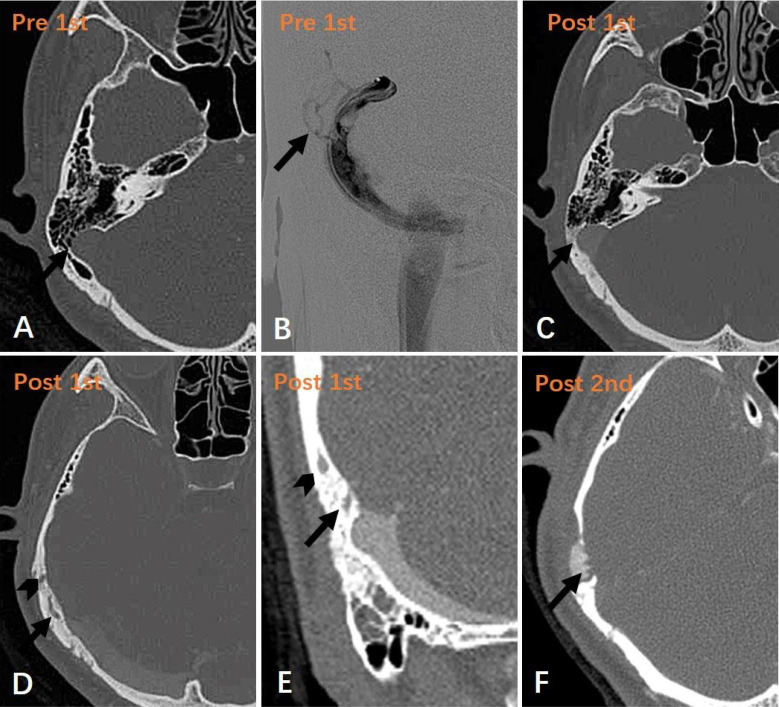
Patient 6 was admitted with a complaint of right-sided PT for more than 1 year. Computed tomography angiography images showed the anterior outer wall of the right sigmoid sinus had bone dehiscence in the range of 5-7 mm, with an ipsilateral high jugular bulb (Figure 4A, B). Although we reconstructed the bone wall surrounding the sigmoid sinus, the patient reported no change in PT. Postoperative CTA showed that the SSWD had been reconstructed (Figure 4C). After reanalysis of pre- and postoperative imaging findings, an abnormal diploic vein ring was found on DSA (Figure 4B). It was located in the adjacent region of the temporal and parietal bones and communicated with the superior curve of the sigmoid sinus (Figure 4D, E). When the abnormal diploic vein ring was blocked by a second operation (Figure 4F), the patient’s PT was alleviated immediately, such that its intensity was approximately 20% of the preoperative level. The patient’s symptoms have been stable during regular follow-up for 14 months.
Patient 7
Patient 7 developed vertigo and right-sided PT after a head injury 7 years prior to presentation to our hospital. After drug treatment, she experienced relief of vertigo, but no change in the PT, which had worsened in the previous 6 months. Computed tomography angiography indicated a typical right SSD (Figure 5A, B), with SSWD below it. On DSA and CTA, the transverse-sigmoid sinus transition was narrower on the right than on the left (Figure 5C, D). The first operation was to reconstruct the bone wall of the sigmoid sinus. The patient experienced complete resolution of PT, but PT recurred after 3 months. Postoperative CTA showed that the diverticulum had been resolved completely (Figure 5E). Considering the SSWD as a possible cause, a second surgery was performed to repair the SSWD (Figure 5F). However, the patient experienced no change in PT after the second surgery. The patient refused a postoperative CTA examination following the second surgery. She visited another hospital for further treatment 6 months later. Digital subtraction angiography records from that hospital showed a filling defect at the junction of the transverse sigmoid sinus, with a gradient of 4 mmHg between the distal transverse and proximal sigmoid sinuses. One stent (PRECISE 6 × 40 mm, Cordis Corporation) was placed at the transverse-sigmoid sinus transition. The patient’s PT was resolved without recurrence. Unfortunately, we did not acquire the related images.
Discussion
Sigmoid sinus diverticulum and SSWD are considered as common causes of venous PT.2-5,8 Mattox reported that SSD constituted 20% of venous-originating PT.2 According to imaging statistics, the incidences of SSWD and SSD in patients with PT were 86.4% and 34.3%, respectively; SSWD was the most frequent anomaly.9 The actual incidences may be higher than those reported in the literature.
In terms of the surgical technique for reconstruction of the SSW, the soft tissue graft (temporalis fascia) can also be inserted between the dura and the posterior fossa bony plate. This may be more reliable for removal of the SSD or for compression of the enlarged sigmoid sinus but may lead to thrombosis or intracranial hypertension, as well as other serious complications.8 In our patients, we used temporalis fascia to directly cover the external side of the diverticulum or defect to reconstruct the bone wall, which may have caused insufficient compression to the sigmoid sinus wall. Firmer materials, such as bone cement or bone chips, may be better than autologous bone dust in terms of minimizing recurrence of SSD or SSWD,10-13 particularly in subjects with transverse sinus stenosis with the jet-like venous flow.14
In the first patient, PT may be caused by multiple causes, including SSD, SSWD, high and dehiscent jugular bulb.15,16 The failure of complete resolution of PT was probably due to the remaining dehiscent jugular bulb. Jugular bulb resurfacing surgery is potentially effective for PT caused by dehiscent jugular bulb.17,18 Since the patient got marked resolution of PT following the second surgery, she opted not to undergo the jugular bulb resurfacing surgery.
Patients 2-5 were our early cases. Due to the lack of surgical experience and failure to expose the SSD/SSWD sufficiently, the treatment outcome of the first surgery was unsatisfactory. When both SSD and SSWD were resolved after the second surgery, patients achieved satisfactory effect. In some instances, it is difficult to identify the responsible anomaly (SSD, SSWD, or a combination). We recommend a complete resolution of both the SSD and SSWD during the operation.
In Patient 6, the abnormal vessel ring was likely formed by diploic veins, possibly with a petrosquamosal sinus connecting to the sigmoid sinus. We speculate that this may be associated with abnormal blood flow or abnormal hemodynamics. The diploic veins are lined by a single endothelial cell layer, have no vascular valves, and course in diploic channels.19 Diploic veins communicate with the emissary veins, dural sinuses, meninges, pericranial veins, and skull base. They act as a link between the extra- and intracranial venous systems.20 They may be part of the brain’s cooling and buffering systems,21 thus relieving acute elevations of intracranial pressure.22 Diploic veins are rarely evident under normal physiological conditions, but the diploic system may show enhanced flow in certain pathological states.23
Due to the lack of valves in diploic veins, the blood in these vessels can flow in 2 directions.19 In mice, the diploic venous flow is unidirectional; however, in some pathological states in humans, the blood flow may be reversed in the venous ring, making its directional flow uncertain. In addition, a diploic system with enhanced flow may cause PT. As technology advances, in vivo imaging techniques for the measurement of blood flow speed and direction may help to identify sites responsible for PT.19 In our study, the discovery of a diploic vein anomaly provides insight to understand the mechanism of PT. Although extremely rare, it is a potential cause of PT.
It is notable that the PT subsequently disappeared after one stent was placed in the ipsilateral distal transverse sinus in Patient 7. It indicates that there was some ongoing stenosis in the venous sinus. The presence of transverse sinus stenosis, a high jugular bulb, and ipsilateral venous outflow dominance, together with a deeper pituitary fossa, were more common in the PT group than in the asymptomatic group.24 Upstream venous sinus stenosis is often associated with SSD and is considered as a cause of SSD formation.25 Enhanced flow turbulence is observed at the distal end of the stenosis when the pressure gradient reached 10 mmHg across the sigmoid sinus stenosis.26 These studies suggest that SSD and distal transverse sinus stenosis may have synergistic effects on PT generation.
We found that although PT recurred at the preoperative level after the first operation, the low-frequency hearing of Patient 2 and Patient 5 remained normal (Figure 3). It seems difficult to explain with masking effects.10,27 Song also described a patient whose low-frequency hearing remained normal when tinnitus recurred 4.5 years after surgery.10 The other 5 patients suffered from PT but without any definite low-frequency hearing loss. Therefore, although low-frequency hearing loss and its normalization are objective signs of PT changes, subjective symptom assessment of PT is more important.
Based on the current understanding, we believe that the reasons for reoperation can be classified into the following categories: (1) the patients had multiple anomalies, but only part of them were fixed; (2) failing to recognize other causes; (3) insufficient understanding of venous sinus stenosis, it is still unknown what extent of stenosis could cause hemodynamic changes; and (4) Insufficient understanding of the spatial and stereoscopic structure of SSD/SSWD.
Some limitations of this study should be considered. First, it was a retrospective review based on clinical research at a single center. Although there were only 7 patients, this may be the largest number of revisions of surgical reconstruction of the sigmoid sinus wall in published literatures. Second, imaging data in some cases were incomplete for accurate assessment. Third, it is difficult to determine the causal relationship between sigmoid sinus-related anomalies and PT; the lesions may occur in asymptomatic patients or in the asymptomatic side of unilateral PT; and therefore the findings can only suggest a potential correlation. In the future, hemodynamic measurements may help to evaluate and quantify these interactions.28
Conclusion
SSD and SSWD often occur concurrently in patients with PT. They can be independent or mutual causes of PT. It is recommended to completely resolve both SSD and SSWD during surgery. Abnormal diploic veins and venous sinus stenosis are potential causes of PT.
Figure 4. a-f.
(a), (b), 1st preoperative; (c-e), 1st postoperative; and (f), 2nd postoperative images of Patient 6, who experienced great resolution of PT after two operations. (a) shows the SSWD and the “air on sinus” sign (arrow). (b) is a DSA image of the abnormal diploic vein loop in the squamous portion of the temporal bone (arrow). The layer in (c) corresponds to that in A; the dehiscence is repaired (arrow). (d) and (e) show the upper (arrowheads) and lower (arrows) branches of the vein loop in CTA. In (e), the root of the loop enters the anterolateral wall of the sigmoid sinus. In (f), axial CTA shows the abnormal diploic vein is sealed (arrow).
Figure 5. a-d.
(a-d), 1st preoperative, and (e), (f), 1st postoperative images of Patient 7. (a) and (b) show the SSD in axial and coronal CTA, respectively (arrows). (c) and (d) respectively show DSA and computed tomography venography images of the right transverse-sigmoid sinus transition which was narrow (arrows). The layer in (e) corresponds to that in (a); the diverticulum is completely repaired (arrow). In (f), CTA shows the SSWD and “air on sinus” sign (arrow).
Footnotes
Ethics Committee Approval: Ethical committee approval was received from the Ethics Committee of Beijing Friendship Hospital, Capital Medical University of China (Approval no: 2018-P2-140-02).
Informed Consent: Written informed consent was obtained from all participants who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – Z.W., S.G.; Design – D.L., G.W., S.G.; Supervision – Z.W., S.G.; Funding – G.W., Z.W., S.G.; Data Collection and/or Processing – D.L., R.Z., W.L., N.C.; Analysis and/or Interpretation – R.Z., P.Z.; Literature Review – N.C., P.Z.; Writing – D.L., G.W., S.G.; Critical Review – Z.W., S.G.
Declaration of Interests: The authors declare that they have no competing interests.
Funding: This work was supported by grants from Beijing Hospital Authority Youth Program (QML20180101); National Natural Science Foundation of China (No.61931013 and NO.82171886); Zhangjiakou City Science and Technology Research Project (No.1821053D).
References
- 1. Madani G, Connor SE. Imaging in pulsatile tinnitus. Clin Radiol. 2009;64(3):319 328. 10.1016/j.crad.2008.08.014) [DOI] [PubMed] [Google Scholar]
- 2. Mattox DE, Hudgins P. Algorithm for evaluation of pulsatile tinnitus. Acta Otolaryngol. 2008;128(4):427 431. 10.1080/00016480701840106) [DOI] [PubMed] [Google Scholar]
- 3. Grewal AK, Kim HY, Comstock RH, Berkowitz F, Kim HJ, Jay AK. Clinical presentation and imaging findings in patients With pulsatile tinnitus and sigmoid sinus diverticulum/dehiscence. Otol Neurotol. 2014;35(1):16 21. 10.1097/MAO.0b013e31829ab6d7) [DOI] [PubMed] [Google Scholar]
- 4. Schoeff S, Nicholas B, Mukherjee S, Kesser BW. Imaging prevalence of sigmoid sinus dehiscence among patients with and without pulsatile tinnitus. Otolaryngol Head Neck Surg. 2014;150(5):841 846. 10.1177/0194599813520291) [DOI] [PubMed] [Google Scholar]
- 5. Otto KJ, Hudgins PA, Abdelkafy W, Mattox DE. Sigmoid sinus diverticulum: a new surgical approach to the correction of pulsatile tinnitus. Otol Neurotol. 2007;28(1):48 53. 10.1097/01.mao.0000247814.85829.f6) [DOI] [PubMed] [Google Scholar]
- 6. Wang GP, Zeng R, Ma XB, Liu ZH, Wang ZC, Gong SS. Surgical treatment of pulsatile tinnitus caused by the sigmoid sinus diverticulum: a preliminary study. Med (Baltim). 2015;94(21):e882. 10.1097/MD.0000000000000882) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zeng R, Wang GP, Liu ZH.et al. Sigmoid sinus wall reconstruction for pulsatile tinnitus caused by sigmoid sinus wall dehiscence: a single-center experience. PLoS ONE. 2016;11(10):e0164728. 10.1371/journal.pone.0164728) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eisenman DJ. Sinus wall reconstruction for sigmoid sinus diverticulum and dehiscence: a standardized surgical procedure for a range of radiographic findings. Otol Neurotol. 2011;32(7):1116 1119. 10.1097/MAO.0b013e31822a1c7d) [DOI] [PubMed] [Google Scholar]
- 9. Dong C, Zhao PF, Yang JG, Liu ZH, Wang ZC. Incidence of vascular anomalies and variants associated with unilateral venous pulsatile tinnitus in 242 patients based on dual-phase contrast-enhanced computed tomography. Chin Med J (Engl). 2015;128(5):581 585. 10.4103/0366-6999.151648) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Song JJ, Kim YJ, Kim SY.et al. Sinus wall resurfacing for patients with temporal bone venous sinus diverticulum and ipsilateral pulsatile tinnitus. Neurosurgery. 2015;77(5):709 717. 10.1227/NEU.0000000000000902) [DOI] [PubMed] [Google Scholar]
- 11. Kim CS, Kim SY, Choi H.et al. Transmastoid reshaping of the sigmoid sinus: preliminary study of a novel surgical method to quiet pulsatile tinnitus of an unrecognized vascular origin. J Neurosurg. 2016;125(2):441 449. 10.3171/2015.6.JNS15961) [DOI] [PubMed] [Google Scholar]
- 12. Wang AC, Nelson AN, Pino C, Svider PF, Hong RS, Chan E. Management of sigmoid sinus associated pulsatile tinnitus: a systematic review of the literature. Otol Neurotol. 2017;38(10):1390 1396. 10.1097/MAO.0000000000001612) [DOI] [PubMed] [Google Scholar]
- 13. Newberry I, Highland J, DeTorres A, Gurgel R. Transmastoid hydroxyapatite resurfacing for sigmoid sinus wall anomalies causing pulsatile tinnitus. Ann Otol Rhinol Laryngol. 2021;130(8):885 891. 10.1177/0003489420987407) [DOI] [PubMed] [Google Scholar]
- 14. Amans MR, Haraldsson H, Kao E.et al. MR venous flow in sigmoid sinus diverticulum. AJNR Am J Neuroradiol. 2018;39(11):2108 2113. 10.3174/ajnr.A5833) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yoon BN, Lee TH, Kong SK, Chon KM, Goh EK. Management of high jugular bulb with tinnitus: transvenous stent-assisted coil embolization. Otolaryngol Head Neck Surg. 2008;139(5):740 741. 10.1016/j.otohns.2008.04.019) [DOI] [PubMed] [Google Scholar]
- 16. Sayit AT, Gunbey HP, Fethallah B, Gunbey E, Karabulut E. Radiological and audiometric evaluation of high jugular bulb and dehiscent high jugular bulb. J Laryngol Otol. 2016;130(11):1059 1063. 10.1017/S0022215116009166) [DOI] [PubMed] [Google Scholar]
- 17. Lee SY, Song SK, Park SJ.et al. Jugular bulb resurfacing with bone cement for patients with high dehiscent jugular bulb and ipsilateral pulsatile tinnitus. Otol Neurotol. 2019;40(2):192 199. 10.1097/MAO.0000000000002093) [DOI] [PubMed] [Google Scholar]
- 18. DeHart AN, Shaia WT, Coelho DH. Hydroxyapatite cement resurfacing the dehiscent jugular bulb: novel treatment for pulsatile tinnitus. Laryngoscope. 2018;128(5):1186 1190. 10.1002/lary.26711) [DOI] [PubMed] [Google Scholar]
- 19. Toriumi H, Shimizu T, Shibata M.et al. Developmental and circulatory profile of the diploic veins. Microvasc Res. 2011;81(1):97 102. 10.1016/j.mvr.2010.11.004) [DOI] [PubMed] [Google Scholar]
- 20. Rangel de Lázaro G, de la Cuétara JM, Píšová H, Lorenzo C, Bruner E. Diploic vessels and computed tomography: segmentation and comparison in modern humans and fossil hominids. Am J Phys Anthropol. 2016;159(2):313 324. 10.1002/ajpa.22878) [DOI] [PubMed] [Google Scholar]
- 21. Lachkar S, Dols MM, Ishak B, Iwanaga J, Tubbs RS. The diploic veins: a comprehensive review with clinical applications. Cureus. 2019;11(4):e4422. 10.7759/cureus.4422) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tsutsumi S, Nakamura M, Tabuchi T, Yasumoto Y, Ito M. Calvarial diploic venous channels: an anatomic study using high-resolution magnetic resonance imaging. Surg Radiol Anat. 2013;35(10):935 941. 10.1007/s00276-013-1123-3) [DOI] [PubMed] [Google Scholar]
- 23. García-González U, Cavalcanti DD, Agrawal A.et al. The diploic venous system: surgical anatomy and neurosurgical implications. Neurosurg Focus. 2009;27(5):E2. 10.3171/2009.8.FOCUS09169) [DOI] [PubMed] [Google Scholar]
- 24. Zhao P, Lv H, Dong C, Niu Y, Xian J, Wang Z. CT evaluation of sigmoid plate dehiscence causing pulsatile tinnitus. Eur Radiol. 2016;26(1):9 14. 10.1007/s00330-015-3827-8) [DOI] [PubMed] [Google Scholar]
- 25. Paramasivam S, Furtado S, Shigamatsu T, Smouha E. Endovascular management of sigmoid sinus diverticulum. Interv Neurol. 2016;5(1-2):76 80. 10.1159/000444507) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Signorelli F, Mahla K, Turjman F. Endovascular treatment of two concomitant causes of pulsatile tinnitus: sigmoid sinus stenosis and ipsilateral jugular bulb diverticulum. Case report and literature review. Acta Neurochir (Wien). 2012;154(1):89 92. 10.1007/s00701-011-1202-3) [DOI] [PubMed] [Google Scholar]
- 27. Hou ZQ, Han DY. Pulsatile tinnitus in perimenopausal period. Acta Otolaryngol. 2011;131(8):896 904. 10.3109/00016489.2011.567998) [DOI] [PubMed] [Google Scholar]
- 28. Liu Z, He X, Du R, Wang G, Gong S, Wang Z. Hemodynamic changes in the sigmoid sinus of patients with pulsatile tinnitus induced by sigmoid sinus wall anomalies. Otol Neurotol. 2020;41(2):e163 e167. 10.1097/MAO.0000000000002512) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a